- 1Department of Orthopedics, Ningbo No. 6 Hospital, Ningbo, Zhejiang, China
- 2Ningbo Clinical Research Center for Orthopedics, Sports Medicine & Rehabilitation, Ningbo, Zhejiang, China
Objective: This study evaluated the clinical efficacy of a modified surgical technique—lateral crossed-tensioned Kirschner wires (K-wires) combined with external fixation—for treating supracondylar humeral fractures in school-aged children.
Methods: Between April 2022 and April 2023, 45 school-aged children (ages 6–13) with supracondylar humeral fractures were retrospectively included in this study. The modified surgical technique involving lateral crossed-tensioned K-wires combined with external fixation was employed to facilitate early functional recovery without the need for plaster immobilization. The postoperative follow-up included a radiographic evaluation, assessment of elbow joint functional recovery, and patient satisfaction surveys.
Results: All the patients were followed up for 6–18 months. Five patients developed pin site infections, which were successfully managed with routine care. No cases of non-union, K-wire migration, or dislocation were observed. Based on their Flynn scores, 93.3% of the patients achieved excellent elbow joint function at 1 month postoperatively, increasing to 97.8% at 3 months and remaining stable at 6 months. No instances of elbow varus deformity were observed during follow-up. The patients and their families reported high satisfaction levels and recommended this technique for similar fractures in other children.
Conclusions: The use of lateral crossed-tensioned K-wires combined with external fixation for supracondylar humeral fractures in children yields satisfactory results, promotes early functional recovery of the elbow joint, facilitates a quicker return to school activities, and improves patient satisfaction. This technique is a viable alternative for managing supracondylar humeral fractures in school-aged children.
Background
Supracondylar humeral fractures are among the most common pediatric fractures (1, 2). Inadequate management can result in severe complications, including elbow varus deformity and ischemic muscle contracture, compromising both function and cosmetics. Prompt reduction and fixation are critical for optimal outcomes (3). The conventional surgical approach—closed or limited open reduction followed by percutaneous crossed Kirschner wire (K-wire) fixation and plaster cast immobilization—is well-established. However, the optimal K-wire configuration remains controversial (4, 5), and biomechanical comparisons of different fixation techniques remain a key research focus.
A series of studies (6–9) have endorsed crossed K-wire fixation for its stability and clinical efficacy. However, complications such as fixation failure, fracture redisplacement, and persistent elbow varus deformity have been documented with K-wire fixation alone (10, 11). Fayssoux et al. (12) analyzed 14 complex humeral supracondylar fractures, with complications occurring in six cases. No significant difference in fixation loss was observed between the 14 cases and the remaining 408 cases of humeral supracondylar fracture in their cohort. Prolonged cast immobilization after routine K-wire fixation restricts early elbow motion, impeding daily activities and delaying return to school, which is a growing concern given patients’ preferences for a rapid recovery. Slongo et al. (13) investigated the use of external fixation for difficult reductions to avoid cast immobilization. However, the use of threaded fixation pins that are >2 mm in diameter risks an epiphyseal plate injury.
Herein, we describe a combined technique of percutaneous K-wire and external fixation for treating supracondylar humeral fractures in school-aged children. First, smooth, 2-mm non-threaded K-wires are used to minimize the risk of an epiphyseal plate injury. Second, external fixation secures the K-wires, reducing the risk of K-wire migration, fixation failure, and subsequent redisplacement or varus deformity. Third, external fixation ensures robust stability, facilitating early functional recovery and a quicker return to normal activities.
Patients and methods
Patients
Between April 2022 and April 2023, we retrospectively included 45 patients (from 182 consecutive cases) who were all treated with the modified surgical technique. Written informed consent was obtained from the patients’ legal guardians. The inclusion criteria were as follows: (1) Gartland type III supracondylar humeral fracture; and (2) age ≥6 years. The exclusion criteria were as follows: (1) age <6 years old or a non-Gartland III fracture; (2) an open or pathological fracture; and (3) polytrauma requiring multidisciplinary management. Data on the patients’ demographics (age and sex); complications (nerve injury, pin track infection, and/or fixation failure); elbow function recovery at 1, 3, and 6 months after surgery; cosmetic outcomes; and patient satisfaction scores were systematically gathered during the postoperative follow-up.
Surgical technique
All the surgical procedures were conducted under brachial plexus anesthesia with upper arm tourniquet control. A single pediatric orthopedic surgeon with 20 years of experience performed all the procedures to maintain technical consistency. Under C-arm fluoroscopic guidance, closed reduction was attempted first. Cases with successful reductions then proceeded directly to fixation. In the other cases, after two unsuccessful attempts, we performed medial elbow exposure with the following steps: (1) a medial skin and fascial incision; (2) ulnar nerve identification and protection; (3) periosteal elevation; and (4) fracture site debridement and reduction. The same fixation methods were employed for both open and closed reductions. Two 2.0-mm K-wires were first inserted percutaneously to stabilize the lateral humeral condyle, followed by a third 2.0 mm K-wire inserted from the medial epicondyle and advanced to exit at the proximal lateral fracture margin (Figure 1). During the medial K-wire placement, particular attention was paid to protecting the ulnar and radial nerves. Our technique involved manually stabilizing the ulnar nerve within its groove using the thumb while inserting the K-wire along the medial epicondyle axis using a power drill. A critical technical modification was implemented whereby once the K-wire penetrated the proximal cortical bone on the opposite side, we immediately switched from power drilling to manual hammering to advance the K-wire through the skin, thereby minimizing soft tissue trauma, particularly to the radial nerve. Following fluoroscopic confirmation of satisfactory fracture reduction and implant positioning, all three K-wires were connected to a mini external fixation system (Double Medical Technology Inc., Xiamen, China) under compression (Figure 2). After final verification of the reduction and fixation, the protruding K-wire ends were trimmed, eliminating the need for postoperative casting. This approach permitted the immediate initiation of pain-free active elbow flexion-extension exercises, which are not allowed after conventional percutaneous K-wire fixation (Figure 2).
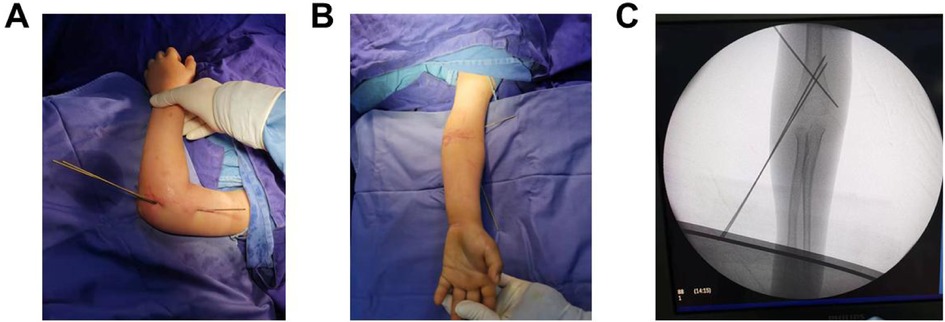
Figure 1. Initial percutaneous lateral crossed K-wire fixation after fracture reduction. (A) A lateral view of the affected side shows three percutaneously inserted K-wires. (B) The anteroposterior view of the affected side shows good restoration of the carrying angle of the elbow joint. (C) Fluoroscopic imaging confirms satisfactory fracture reduction, with optimal positioning and direction of the K-wires.
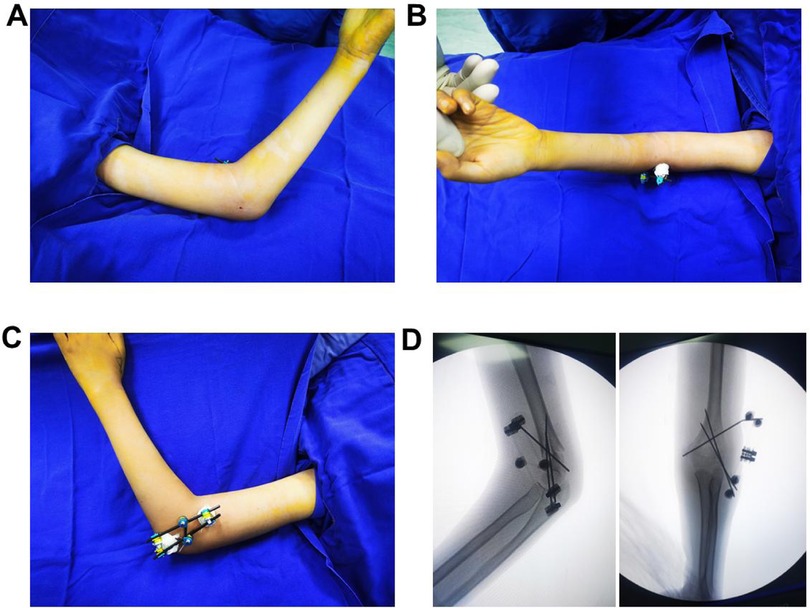
Figure 2. Postoperative confirmation of fracture reduction, proper implant positioning, and elbow joint stability. (A–C) The percutaneously inserted K-wires are positioned laterally to the elbow joint, with the external fixator securely in place. Only sterile dressings are applied to the distal ends of the K-wires, eliminating the need for postoperative plaster fixation and allowing the patient to begin early rehabilitation. (D) Fluoroscopic imaging confirms satisfactory fracture reduction, with optimal positioning and direction of the K-wires.
Postoperative management
The patients received routine pin site care and were instructed in finger and wrist exercises for symptom management. Furthermore, the patients were permitted elbow motion and encouraged to use the affected limb for daily activities (e.g., writing and eating). Radiographic follow-ups occurred at 1, 3, and 6 months postoperatively. At the 1-month follow-up, fixation removal was considered if callus bridging at the fracture site was visible, no local tenderness was present, and there was no pain with longitudinal compression. Elbow joint function was assessed during outpatient fixation removal. After the removal, the patients began active, non-weight-bearing exercises. Photographic assessment of cosmesis and patient satisfaction surveys were conducted 6 months after surgery as part of the follow-up protocol.
Statistical analysis
All the statistical analyses were performed using R software (version 4.3.1). Continuous variables are expressed as the mean ± standard deviation (SD), while categorical variables are presented as counts and percentages. Fisher's exact test was used for categorical variables. A two-tailed p-value <0.05 was considered statistically significant.
Results
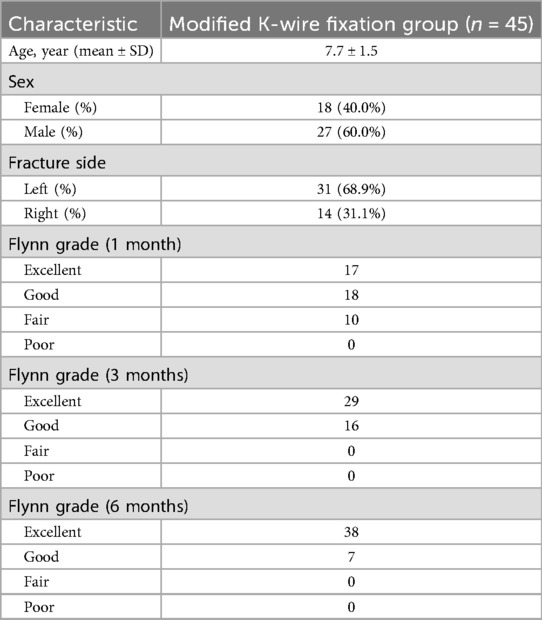
The cohort consisted of 45 patients (27 boys and 18 girls) aged 6–13 years old, with follow-up periods ranging from 6 to 18 months. Left-sided fractures predominated (31 cases, or 68.9%) compared to right-sided ones (14 cases, 31.1%). Extension-type fractures accounted for 93.3% (42 out of 45) of cases, with only three cases (6.7%) being flexion-type. Open reduction was required in 15.6% (seven out of 45) of the cases after failed closed reduction attempts. Preoperative nerve injuries occurred in 11 patients (six of the median nerve and five of the radial nerve), with complete resolution within 3 months. This elevated incidence likely reflects our selective inclusion of severe Gartland type III fractures. Skin infections at the pin sites occurred in five cases (11.1%), and all resolved with standard care. No cases of non-union, osteomyelitis, or fixation failure were observed. Notably, during the 6-month follow-up period, no patients in the modified technique cohort received a poor Flynn grading, demonstrating sustained clinical improvement (Table 1).
The functional outcomes, assessed via Flynn's grading system (14), demonstrated excellent results in 93.3% (42 out of 45) of the patients at the 1-month follow-up, improving to 97.8% (44 out of 45) by 3 months, a level that was maintained at 6 months (Figure 3). Postoperative parental satisfaction surveys showed that 91.1% (41 out of 45) would strongly recommend the treatment, citing excellent functional recovery as the primary reason. The cases of dissatisfaction were associated with either a skin infection or the need for open reduction.
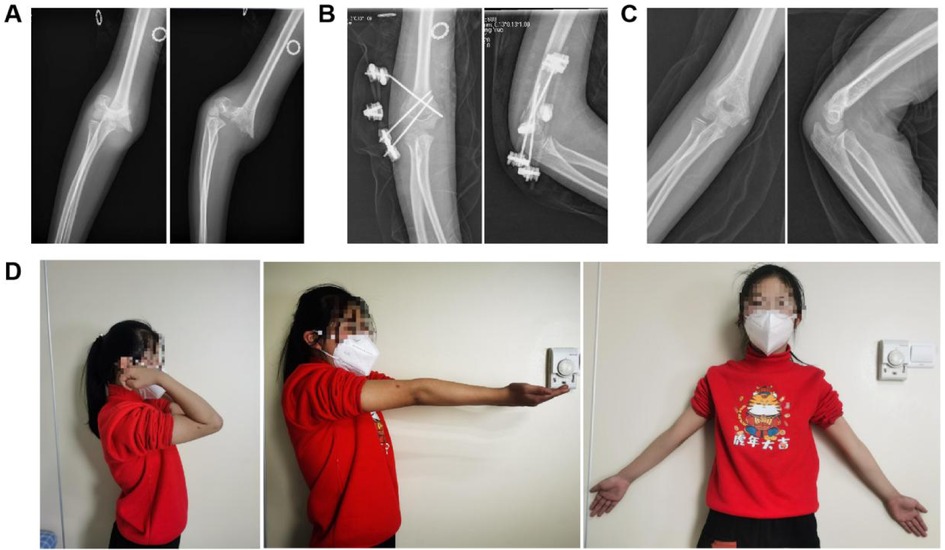
Figure 3. A case example of a 10-year-old girl with a right Gartland III supracondylar humerus fracture. (A) Preoperative radiographs, (B) 1-month postoperative radiographs, (C) 6-month postoperative radiographs, and (D) clinical photograph demonstrating symmetrical upper limb alignment.
Discussion
A supracondylar fracture of the humerus is the most prevalent type of pediatric elbow fracture (15, 16). Gartland type III fractures require surgical intervention, typically involving closed or open reduction, K-wire fixation, and plaster immobilization. Despite extensive research on K-wire configurations, a standardized clinical protocol remains undefined. Previous studies (7, 17) have suggested that two lateral K-wires and one medial K-wire provide optimal structural stability, and this is a widely endorsed approach. Nevertheless, conventional percutaneous K-wire fixation necessitates plaster cast immobilization, with reported risks of fixation failure, fracture redisplacement, and secondary cubitus varus deformity (18). Prolonged immobilization delays school-aged children's return to education and daily activities, posing substantial inconvenience. Even after cast removal, prolonged rehabilitation is needed to restore elbow joint function. Biomechanical research (19) has indicated that crossed K-wires lose stability under cyclic loading, making external fixation a viable alternative. Slongo et al. (13) pioneered external fixation as the primary treatment, avoiding postoperative plaster fixation. Liu (20) successfully replicated Slongo's technique in 11 older pediatric cases with supracondylar humerus fractures. While external fixation achieves reduction, it demands advanced surgical skills, as threaded wires may cause epiphyseal damage in children.
Traditional external fixation typically employs threaded pins over 2.0 mm in diameter, which carries a risk of epiphyseal damage. Given the severe consequences of an epiphyseal injury (21, 22), the use of threaded pins should be avoided in this region. The key challenge lies in balancing external fixation stability and avoiding iatrogenic epiphyseal harm. To address this, we proposed a modified technique that combines the crossed K-wire technique with lateral external compression fixation. This is especially advantageous for school-aged children who require prompt restoration of elbow joint function for fine motor tasks. The proposed fixation technique offers several benefits. First, the elimination of postsurgical plaster fixation allows for the rapid resumption of daily activities (e.g., writing and eating) and facilitates an earlier reintegration into social and educational settings. Second, the external fixation of the lateral crossed-tensioned K-wires prevents postoperative cubitus varus deformity. Third, smooth K-wires minimize the risk of epiphyseal injury compared to threaded pins. Patients treated with this technique in this study demonstrated earlier functional recovery and return to school, with high parental satisfaction.
This method also has limitations. First, open reduction is required if closed reduction fails. Our approach entails a medial incision to the elbow joint, improving ulnar nerve exposure and protection, and direct visualization during medial K-wire insertion lowers the risk of ulnar nerve injury (18). Second, this study lacks a comparison with traditional K-wire fixation and biomechanical testing. Future research should address these gaps.
For school-aged children with supracondylar humeral fractures requiring surgery, this technique achieves favorable therapeutic outcomes and high parental satisfaction. Lateral smooth cross-fixation with K-wires minimizes the risk of an epiphyseal plate injury. Moreover, rigid external fixation obviates the need for plaster casts, enabling early elbow mobilization and a quicker return to school activities. Therefore, we recommend this modified approach as an effective alternative treatment for supracondylar humeral fractures in school-aged children.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study involving humans was approved by the Academic Ethics Committee of the Ningbo No. 6 Hospital (2023-21K). This study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
HZhu: Data curation, Investigation, Writing – original draft. MW: Data curation, Writing – review & editing. CG: Writing – review & editing, Formal analysis, Investigation. HZhe: Supervision, Writing – review & editing, Data curation. JC: Writing – review & editing, Funding acquisition, Methodology, Project administration, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article.
Medical and Health Technology Plan Project of Zhejiang Province (No. 2024KY384) and the Ningbo Clinical Research Center for Orthopedics, Sports Medicine & Rehabilitation (No. 2024L004).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ma HL, Sun XW, Liu F, Hua ZT, Sun J, Zhang SC. Kirschner wire reconstruction of medial and lateral column periosteal hinge in the treatment of multidirectionally unstable supracondylar fracture of the humerus in children. Eur J Med Res. (2023) 28(1):585. doi: 10.1186/s40001-023-01560-2
2. Aparicio Martínez JL, Pino Almero L, Cibrian Ortiz de Anda RM, Guillén Botaya E, García Montolio M, Mínguez Rey MF. Epidemiological study on supracondylar fractures of distal humerus in pediatric patients. Rev Esp Cir Ortop Traumatol (Engl Ed). (2019) 63(6):394–9. English, Spanish. doi: 10.1016/j.recot.2019.07.001
3. Leitch KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified gartland type-IV fracture. J Bone Joint Surg Am. (2006) 88(5):980–5. doi: 10.2106/JBJS.D.02956
4. Ducić S, Bumbasirević M, Radlović V, Nikić P, Bukumirić Z, Brdar R, et al. Displaced supracondylar humeral fractures in children: comparison of three treatment approaches. Srp Arh Celok Lek. (2016) 144(1-2):46–51. doi: 10.2298/sarh1602046d
5. Lee S, Park MS, Chung CY, Kwon DG, Sung KH, Kim TW, et al. Consensus and different perspectives on treatment of supracondylar fractures of the humerus in children. Clin Orthop Surg. (2012) 4(1):91–7. doi: 10.4055/cios.2012.4.1.91
6. Feng C, Guo Y, Zhu Z, Zhang J, Wang Y. Biomechanical analysis of supracondylar humerus fracture pinning for fractures with coronal lateral obliquity. J Pediatr Orthop. (2012) 32(2):196–200. doi: 10.1097/BPO.0b013e318242a99a
7. Larson L, Firoozbakhsh K, Passarelli R, Bosch P. Biomechanical analysis of pinning techniques for pediatric supracondylar humerus fractures. J Pediatr Orthop. (2006) 26(5):573–8. doi: 10.1097/01.bpo.0000230336.26652.1c
8. Kao HK, Yang WE, Li WC, Chang CH. Treatment of gartland type III pediatric supracondylar humerus fractures with the kapandji technique in the prone position. J Orthop Trauma. (2014) 28(6):354–9. doi: 10.1097/BOT.0000000000000015
9. Kao HK, Lee WC, Yang WE, Chang CH. The posterior intrafocal pin improves sagittal alignment in gartland type III paediatric supracondylar humeral fractures. Injury. (2016) 47(4):842–7. doi: 10.1016/j.injury.2015.12.031
10. Sankar WN, Hebela NM, Skaggs DL, Flynn JM. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg Am. (2007) 89(4):713–7. doi: 10.2106/JBJS.F.00076
11. Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. (2002) 22(4):440–3. doi: 10.1097/01241398-200207000-00005
12. Fayssoux RS, Stankovits L, Domzalski ME, Guille JT. Fractures of the distal humeral metaphyseal-diaphyseal junction in children. J Pediatr Orthop. (2008) 28(2):142–6. doi: 10.1097/BPO.0b013e3181653af3
13. Slongo T, Schmid T, Wilkins K, Joeris A. Lateral external fixation–a new surgical technique for displaced unreducible supracondylar humeral fractures in children. J Bone Joint Surg Am. (2008) 90(8):1690–7. doi: 10.2106/JBJS.G.00528
14. Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. (1974) 56(2):263–72. doi: 10.2106/00004623-197456020-00004
15. Yang L, Yang P, Li L, Tang X. The outcome of loose bone fragments in pediatric supracondylar humerus fractures: a retrospective study. J Pediatr Orthop B. (2022) 31(1):12–7. doi: 10.1097/BPB.0000000000000837
16. Mulpuri K, Wilkins K. The treatment of displaced supracondylar humerus fractures: evidence-based guideline. J Pediatr Orthop. (2012) 32(Suppl 2):S143–52. doi: 10.1097/BPO.0b013e318255b17b
17. Kamara A, Ji X, Liu T, Zhan Y, Li J, Wang E. A comparative biomechanical study on different fixation techniques in the management of transverse metaphyseal-diaphyseal junction fractures of the distal humerus in children. Int Orthop. (2019) 43(2):411–6. doi: 10.1007/s00264-018-3968-x
18. Slongo T. Technik und biomechanik der Bohr-draht(kirschner-draht)-osteosynthese bei kindern [technique and biomechanics of kirschner wire osteosynthesis in children]. Oper Orthop Traumatol. (2020) 32(6):509–29. German. doi: 10.1007/s00064-020-00684-6
19. Weinberg AM, Castellani C, Arzdorf M, Schneider E, Gasser B, Linke B. Osteosynthesis of supracondylar humerus fractures in children: a biomechanical comparison of four techniques. Clin Biomech (Bristol). (2007) 22(5):502–9. doi: 10.1016/j.clinbiomech.2006.12.004
20. Liu S, Peng Y, Liu J, Ou Z, Wang Z, Rai S, et al. Small incision reduction and external fixation for the treatment of delayed over fourteen days supracondylar humeral fractures in children. Front Pediatr. (2022) 10:1039704. doi: 10.3389/fped.2022.1039704
21. Calvisi V, Romanini E, Staniscia D, Di Brigida G, Venosa M. Technical note: tibial spine avulsion treatment with arthroscopic reduction and internal fixation with kirschner wires in skeletally immature patients. Healthcare (Basel). (2023) 11(17):2404. doi: 10.3390/healthcare11172404
Keywords: supracondylar humeral fracture, school-aged children, crossed Kirschner wires, K-wire, external fixation
Citation: Zhu H, Wang M, Gao C, Zheng H and Cao J (2025) A modified surgical technique: lateral crossed-tensioned K-wires combined with external fixation for supracondylar humeral fractures in school-aged children. Front. Pediatr. 13:1681350. doi: 10.3389/fped.2025.1681350
Received: 7 August 2025; Accepted: 17 October 2025;
Published: 14 November 2025.
Edited by:
Xin Tang, Zhejiang University, ChinaReviewed by:
Weibin Du, Zhejiang Chinese Medical University, ChinaAbdallah Boukhentiche, Centre Hospitalo-Universitaire Benflis Touhami Batna, Algeria
Copyright: © 2025 Zhu, Wang, Gao, Zheng and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin Cao, Y2FvamluMTExQDE2My5jb20=
 Huanye Zhu
Huanye Zhu Mengyao Wang
Mengyao Wang Chao Gao
Chao Gao Huajiang Zheng1,2
Huajiang Zheng1,2 Jin Cao
Jin Cao