- 1Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
- 2College of Medicine, King Saud University, Riyadh, Saudi Arabia
- 3Psychiatry and Psychosomatic Medicine, Department of Psychiatry, College of Medicine, King Saud University, Riyadh, Saudi Arabia
In recent years, the global burden of diabetes distress has increased significantly worldwide, imposing mental health issues on patients and the healthcare system. Hence, this study aimed to estimate the prevalence of diabetes distress and determine its psychosocial predictors among Saudi adults with type 2 diabetes mellitus (T2DM). This cross-sectional, observational study was conducted at Diabetes Clinics, Tertiary Care Academic Medical Center, King Saud University Medical City, Riyadh, Saudi Arabia. The survey questionnaire was distributed to 423 participants. The sample size was 384, where the prevalence of diabetes distress was 48.5%. Based on 5% precision and a confidence interval of 95%, the response rate was 78.25% (334 respondents), among which 61.4% of respondents were females, the remaining 38.6% were males, and the mean age was 56.39 years. The mean scores for the Saudi Arabian Diabetes Distress Scale-17 (SADDS-17) subdomains including emotional burden, physician-related distress, regimen-related distress, and interpersonal distress were 2.63 ± 1.29, 2.31 ± 1.44, 2.48 ± 1.16, and 2.23 ± 1.24, respectively. Based on the World Health Organization Quality of Life Assessment Instrument, Short Version (WHOQOL-BREF) transformed scores, the quality of life was recorded as 62.7%. There was a statistically significant positive correlation between the Hospital Anxiety and Depression Scale (HADS) score (r = 0.287, p < 0.01) and the total SADDS-17 scores. The Patient Health Questionaire (PHQ) 15 scores showed significant positive correlations with the total SADDS-17 scores (r = 0.288, p < 0.01) and each of the four subdomains. Our present study revealed that diabetes distress prevalence is alarmingly high among patients in Saudi Arabia, Riyadh. Our findings provide evidence that physical symptoms, quality of life, depression, and anxiety are the notable predictors of diabetes distress.
Introduction
Diabetes mellitus (DM) is a severe threat and a most critical public health challenge; based on the International Diabetes Federation (IDF) statistics, it is affecting 463 million people in 2019 worldwide, and this number will be increased astoundingly to 700 million (10.9%) by 2045 (IDF Diabetes Atlas, 2019). The estimated prevalence of DM in the Middle East and North Africa is 55 million in 2019 (IDF Diabetes Atlas, 2019). In particular, the prevalence of DM ranged from 25.4 to 31.6% among Saudi adults and there has been a staggering emergence of both type 1 and 2 diabetes (Al-Daghri et al., 2011; Alqurashi et al., 2011; Al-Rubeaan et al., 2015).
Diabetes is a heterogeneous disorder compounded by the breakdown of multiple systems with a high risk for cerebrovascular disease, coronary artery disease, renal failure, and foot amputation (Papatheodorou et al., 2018). Prevention and treatment of diabetes and its complications is one of the crucial factors, which worsens patients’ mental health and develops depressive and anxiety symptoms (Bădescu et al., 2016; Naicker et al., 2017). Anxiety and depression are more prevalent among patients with type 2 diabetes mellitus (T2DM) than in the general population (Tran et al., 2021). It is estimated that one in every four T2DM patients has faced depression (Khaledi et al., 2019). Regardless of their depression symptoms, persons with type 2 diabetes benefit from self-management support intervention. A text messaging strategy reduced depression symptoms in patients with an A1c of less than 8.5 percent at baseline (Mayberry et al., 2021). The links between defense mechanisms, depression, and health-related quality of life point to the possibility of personification and protagonization, which may arise over time as diabetes symptoms become more intrusive. The favorable relationship between defensive techniques and well-being measures needs to be viewed with caution (Martino et al., 2020). In addition, a counseling intervention that was successful in achieving a long-term shift in physical activity and sedentary behavior increased psychological well-being and quality of life considerably (Balducci et al., 2019); even though patients with diabetes who had symptoms of depression, but which was not clinical depression, experienced an emotional burden related to diabetes distress (Fisher et al., 2007). Compared with major depressive disorder (MDD) and depressive symptoms in diabetics, the estimated prevalence of diabetes distress was a higher percentage in the US (18%) (Fisher et al., 2008, 2010), China (42.15%) (Zhou et al., 2017), and Malaysia (49.2%) (Chew et al., 2016).
Diabetes distress is a hidden negative emotional condition caused by worries, fears, and frustrations in patients with diabetes, which is mainly associated with poorer management (Ali et al., 2006; Fisher et al., 2007, 2008, 2010). Diabetes distress is more persistent than anxiety and affective disorders (Ali et al., 2006; Fisher et al., 2007, 2008, 2010) and had a cyclical relationship between depressive symptoms and diabetes distress (Ali et al., 2006; Fisher et al., 2007, 2008, 2010). Insulin treatment had a higher prevalence of diabetes distress than oral hypoglycemic agents or diet modification (Delahanty et al., 2007). Diabetes distress is better accounted for by non-clinical factors, including coping styles and social support rather than the clinical indicators (Karlsen et al., 2012). However, a positive correlation between the hemoglobin A1c (HbA1c) and diabetes distress has been reported by several studies. Female patients who have had MDD, or experienced more negative events are at high risk of becoming distressed over time (Fisher et al., 2007, 2008, 2010).
In recent years, the global burden of diabetes distress has increased significantly worldwide, imposing mental health issues on patients and the healthcare system. In particular, high rates of T2DM are observed among the Saudi population. Unfortunately, there is little to no information related to diabetes distress in the Saudi population. This notion could open new research in psychosocial predictors associated with diabetes distress in Saudi Arabia. Hence, this study aimed to estimate the prevalence of diabetes distress and determine its psychosocial predictors among Saudi adults with T2DM.
Materials and Methods
Design and Participants
This cross-sectional, observational study was conducted at Diabetes Clinics, Tertiary Care Academic Medical Center (concealed text), Saudi Arabia. It is a university-affiliated government hospital that delivers free DM healthcare services, and patients benefited from rural areas and all over the country. Participants were selected using convenience sampling of adults with T2DM (age ≥ 18 years) between December 2016 and April 2017, and who could fluently read and understand Arabic. The exclusion criteria included patients who were suffering from type 1 diabetes, severe comorbid medical illnesses, severe diabetes complications, or psychiatric diseases (psychosis or dementia), and pregnant or lactating females. The participants were interviewed by trained interviewers after getting their written informed consent. Ethical approval was obtained from the research ethics committee at King Saud University.
Sample Size
The sample size was 384, where the prevalence of diabetes distress was 48.5%. Based on 5% precision and a confidence interval of 95%, we calculated the sample size using the single proportion sample size formulae [n = Z2αP(1-P)/d2]. The survey questionnaire was distributed to 423 participants, with a non-response rate of 10%. The response rate was 78.25% (334 respondents); among these, 61.4% of respondents were females, the remaining 38.6% were males, and the mean age was 56.39 years.
Measurements
A committee composed of two psychiatrists, an epidemiologist, and two family medicine physicians reviewed each component of the study’s questionnaire to ensure the relevance and applicability of each question and tested on 30 participants before the final application.
The study questionnaire distributed to participants included a socio-demographic section that contained the medical record number, which was used to acquire clinical, biochemical, medication data, and past medical history. The next part of the questionnaire included the following scales:
The Diabetes Distress Scale (DDS-17) consists of 17 items divided into four domains that describe possible diabetes-related problems such as emotional burden (EB), physician-related distress (PD), regimen-related distress (RD), and interpersonal distress (ID). Based on the items scoring from 1 to 6, the scale was depicted as no distress to severe distress. The scores represent distress experienced over the last month. Scores were averaged by dividing the summed scores of each participant’s responses by the number of items in the scale. Based on their average scores, participants were categorized into two diabetes distress groups (low [<3], high [≥3]) (Polonsky et al., 2005).
The Saudi Arabian Diabetes Distress Scale (SADDS-17) was first validated and translated into the Arabic language (Batais et al., 2021). Two bilingual native Arabic speakers translated this scale after gaining Lawrence Fisher’s permission (Fisher et al., 2012). One speaker had medical expertise and another speaker knew the goal of the study. After this, two researchers back-translated the Arabic into an English version in order to assess the validity of each item. A committee of two psychiatrists, an epidemiologist, and two-family medicine physicians were then formed to finalize the Arabic version of DDS-17 by adapting it to the Saudi culture.
The Hospital Anxiety and Depression Scale (HADS) tool consists of 14 items, which are divided into two halves that evaluated anxiety and depression levels among participants. Each question had a range of four answers that described the severity of the exact point. A total score of 0–7 was considered within the normal range, a score of 8–10 was regarded as a borderline abnormal range, while a score within 11–21 was considered in the abnormal range. Permission to use a previously validated Arabic version of this scale was obtained (Malasi et al., 1991).
The Visual Analogue Scale (VAS) is a visual self-evaluation tool that was used to evaluate participants’ compliance with diabetes management (Finitsis et al., 2016). The participants viewed a horizontal line containing small vertical lines numbered sequentially from 0 to 10, representing a range from non-compliant to fully compliant. Based on the earlier studies (Zeller et al., 2008; Alosaimi et al., 2016, 2017), participants who had scores of great than or equal to 8 were considered an adherent group and used medicine as per doctor’s instructions; scores less than 8 represent the non-adherent group.
The World Health Organization Quality of Life Assessment Instrument, Short Version (WHOQOL-BREF) scale contains 26 items that evaluate the participants’ quality of life in four domains such as physical health, psychological health, social relationships, and environment during the past 2 weeks of their lives (WHOQOL, 2021). WHOQOL-BREF is a subset from the WHOQOL 100. However, it has no representative intervals. Scores in this scale are transformed into a value between 0 and 100, reflecting the lowest and highest possible scores, respectively. Prior permission to use the validated Arabic version of WHOQOL-BREF was obtained (Ohaeri and Awadalla, 2009).
Patient Health Questionnaire (PHQ-15) is a scale that contains 15 items evaluating somatic symptoms perceived by patients. Answers to questions include 0, not bothered at all; 1, bothered a little; and 2, bothered a lot. The total score is calculated and ranges from 0 to 30, reflecting the severity of symptoms as minimal, low, medium, or high level (Questionnaire). Permission was obtained to use the validated Arabic version (AlHadi et al., 2017).
The Summary of Diabetes Self- Care Activities (SDSCA) is a scale that contains eight items that measure the frequency of specific diabetes self-management activities in the past week. The categories included were diet, exercise, blood sugar testing, and foot care. Permission was obtained to use the validated Arabic version (AlJohani et al., 2016).
Statistical Analysis
Descriptive statistics for continuous variables were reported as mean ± standard deviation (SD), while categorical variables were reported as frequencies. Statistical comparisons between different groups were made using independent samples t-test, one-way ANOVA for diabetes distress score, and chi-square test for the level of diabetes distress. Bivariate correlations were performed to find the associations between diabetes distress scores and the socio-demographic, clinical, and biochemical data. To identify independent variables, multivariate logistic regression analysis was conducted on the significant variables from the bivariate analysis. All the tests were two-tailed, and statistical significance was set at p < 0.05 or p < 0.01. All analysis was performed in SPSS software v21.
Results
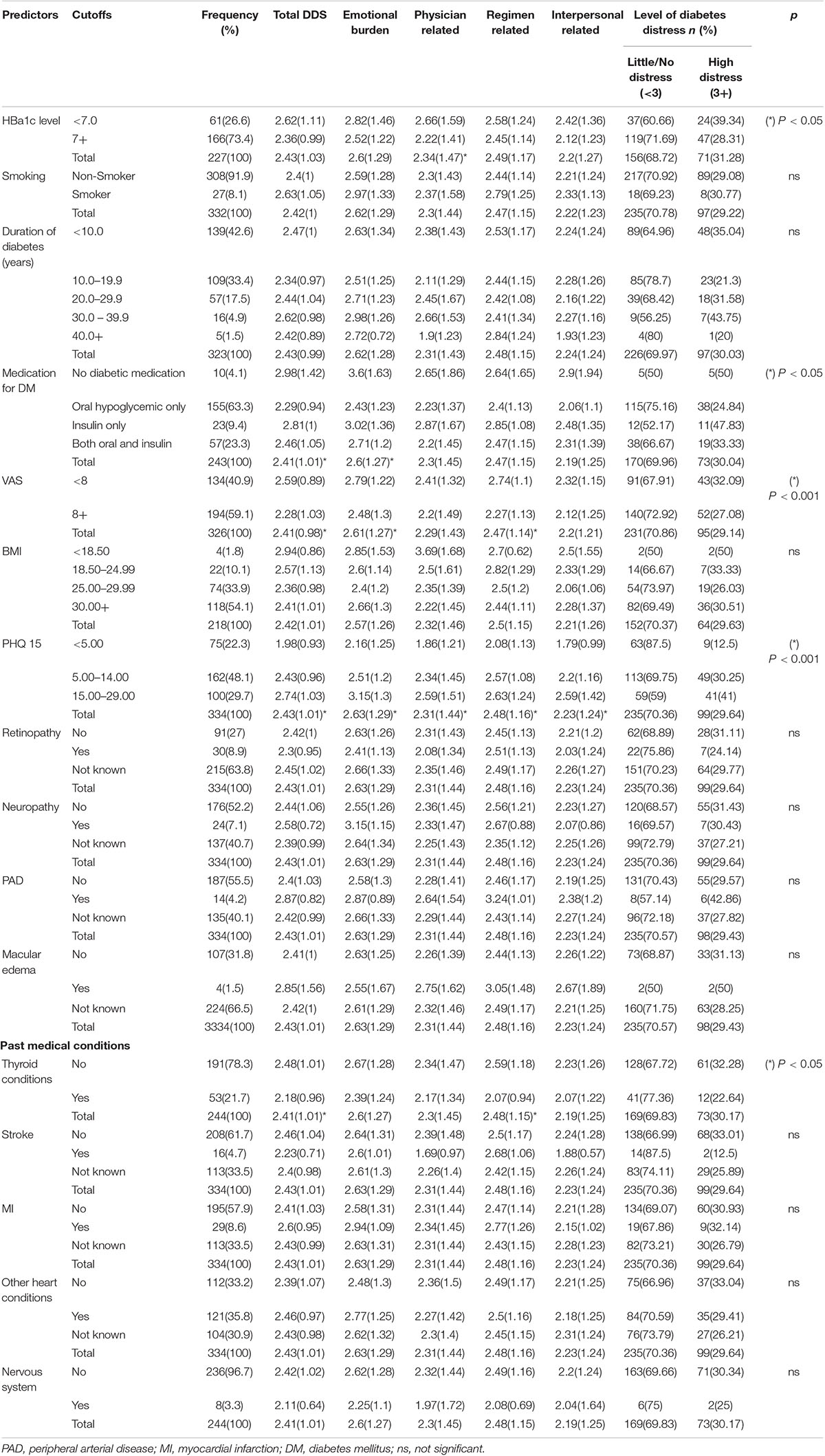
The response rate was 78.25% (334 respondents); among these, 61.4% of respondents were females, the remaining 38.6% were males, and the mean age was 56.39 years (SD = 10.21 years). The participants’ socio-demographic analysis showed 91.9% non-smokers, 67% married, and 54.2% unemployed. The average total diabetes distress score was 2.43 ± 1.01, with the emotional burden domain being the highest at 2.63 ± 1.29 (Table 1).
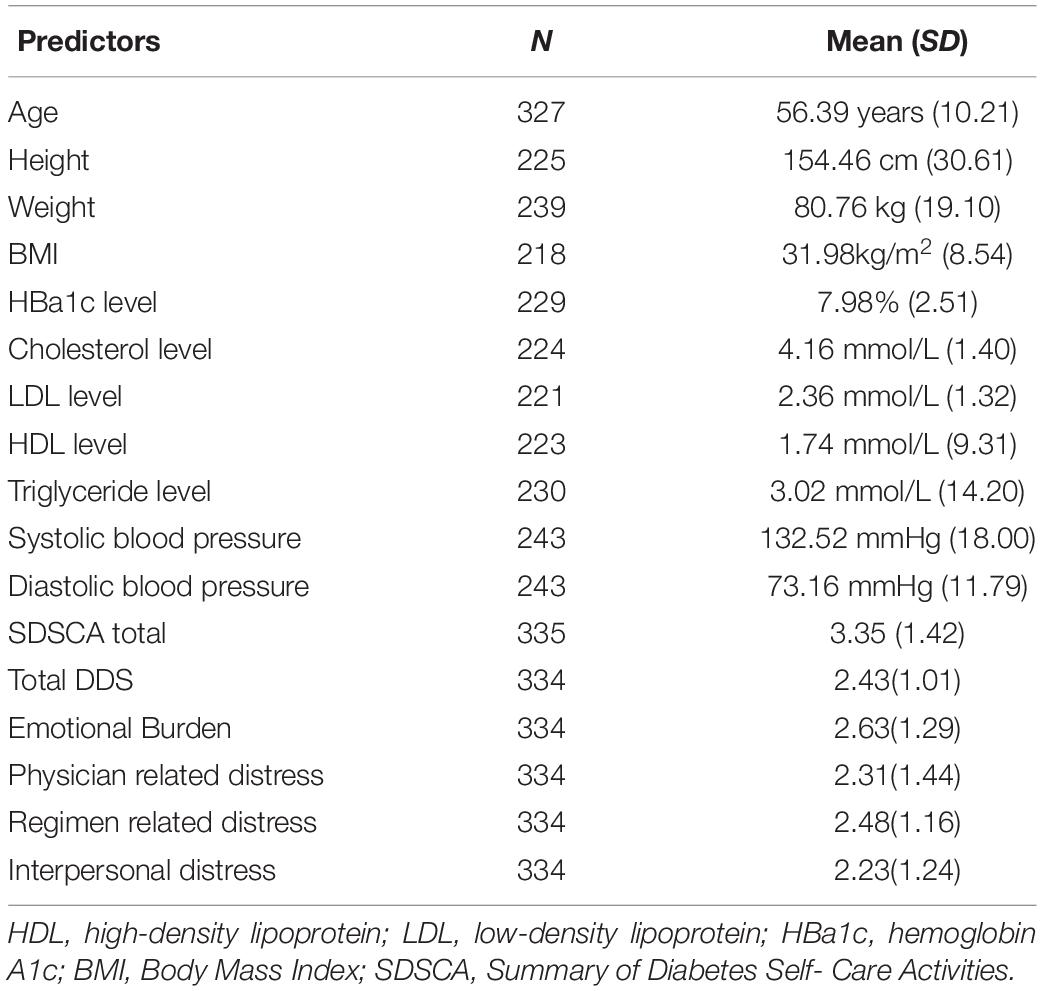
Table 1. Summary of descriptive statistics of socio-demographics, clinical factors, diabetes distress, and its domains.
The mean scores for the SADDS-17 subdomains, including emotional burden, physician-related distress, regimen-related distress, and interpersonal distress, were 2.63 ± 1.29, 2.31 ± 1.44, 2.48 ± 1.16, and 2.23 ± 1.24, respectively (Table 1). The average body-mass index (BMI) of participants was 31.98 (8.54 kg/m2), and the majority (63.3%) were on oral hypoglycemics treatment.
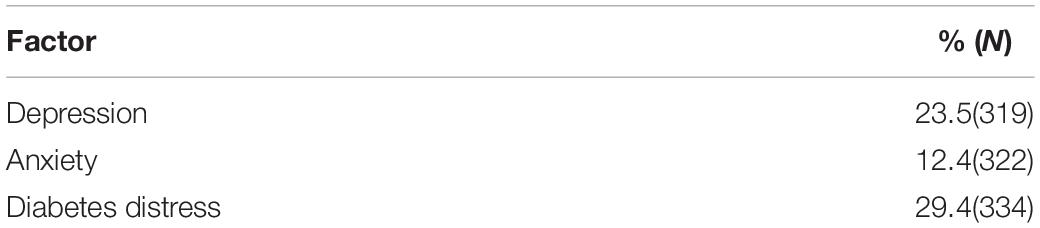
The respondents’ prevalence of diabetes distress was 29.4%, as calculated from total SADDS-17 scores. The distribution of participants across the four subdomains is shown in Figure 1. The prevalence of anxiety and depression were 12.4 and 23.5%, respectively, as estimated from the HADS scores (Table 2). Based on the WHOQOL-BREF transformed scores, the quality of life was recorded as 62.7%.
The respondents’ mean prevalence of diabetes distress among different groups revealed 2.81 ± 1.14 for the 15,000–20,000 SAR average monthly family income group, 2.64 ± 0.96 for the singles group in social status, 2.57 ± 0.98 for the businessman group in occupation, 2.52 ± 1.03 for the 5–9 family members under care group, 2.51 ± 1.12 for the bachelor’s degree group in educational level, 2.47 ± 1.04 for the 41–60 years age group, and 2.47 ± 1.04 for the female group in gender (Table 3).
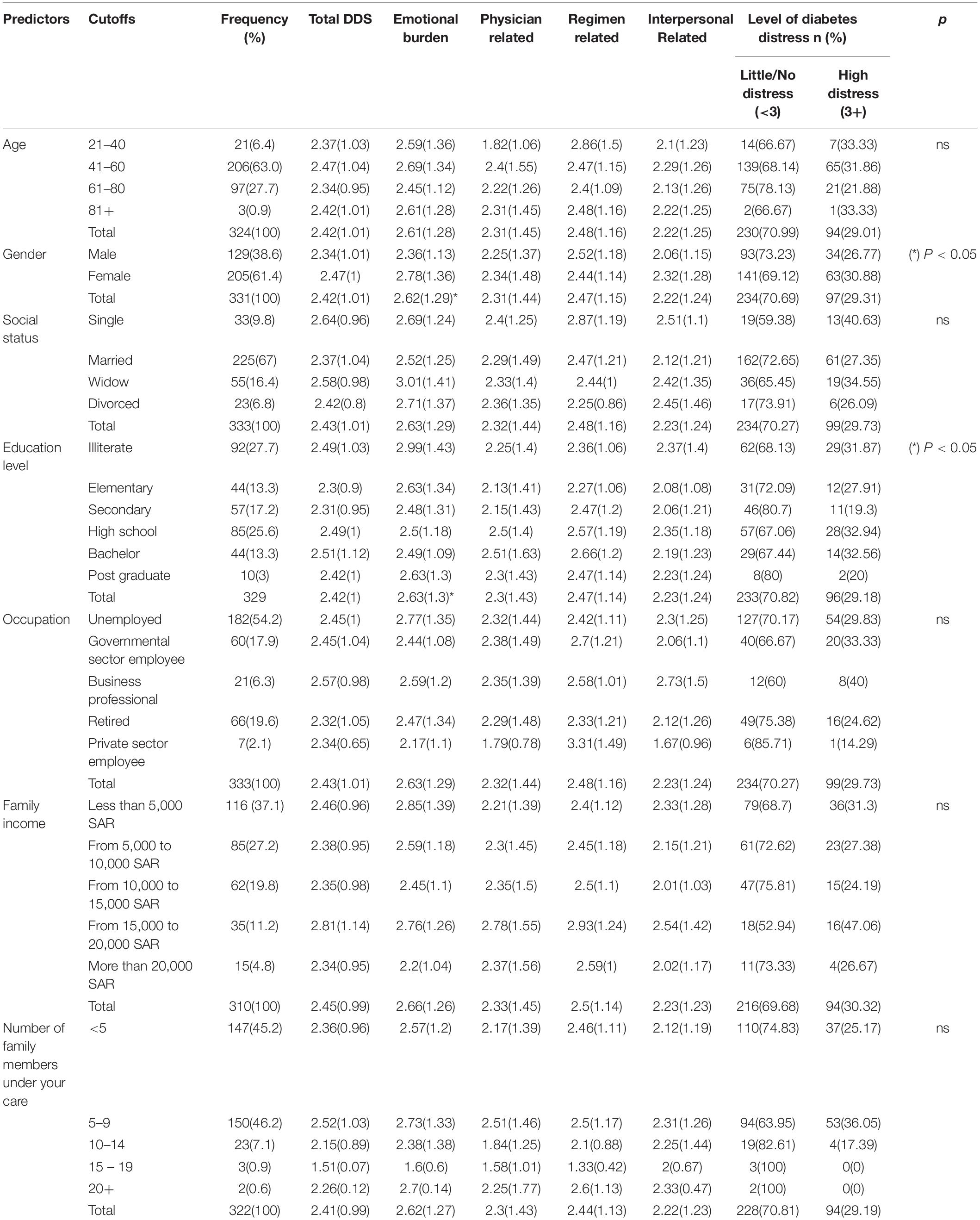
Table 3. Summary of univariate analysis between diabetes distress scores and socio-demographic characteristics.
In addition, the highest percentages of diabetes distress symptoms were recorded among the no diabetes medication group (50%), family income group of 15,000–20,000 SAR (47.06%), the singles group (40.63%) in social status, and business professional group (40%) in occupation (Tables 3, 4).
The univariate analysis results between diabetes distress scores and socio-demographic characteristics are shown in Table 3. Education level and gender were revealed to be significantly associated with emotional burden related to diabetes distress. However, no association was revealed between the other variables (age, social status, occupation, family income, number of family members under your care) and any of the DDS subdomains (Table 3).
In the clinical variables, higher diabetes distress levels were observed in the no diabetes medication group (2.98 ± 1.42), underweight (<18.5) in BMI group (2.94 ± 0.86), the smokers’ group (2.63 ± 1.05), and the 30–39 years duration of DM group (2.62 ± 0.98) (Table 4). Table 4 shows a univariate analysis between distress scores and clinical characteristics. The medication of DM, VAS scores, and PHQ 15 scores exhibited a significant association with total DDS and emotional burden related to diabetes distress. Thyroid conditions showed a significant association with emotional burden related to diabetes distress. HBA1c level and PHQ 15 scores revealed a significant association with physician-related diabetes distress. VAS scores, thyroid conditions, and PHQ 15 scores showed a significant association with regimen-related diabetes distress. PHQ 15 scores showed an association with interpersonal-related diabetes distress. However, there was no association between other clinical variables (BMI, smoking, duration of diabetes, retinopathy, neuropathy, PAD, macular, edema, thyroid conditions, stroke, MI, other heart conditions, nervous system), and any of the DDS sub-domains.
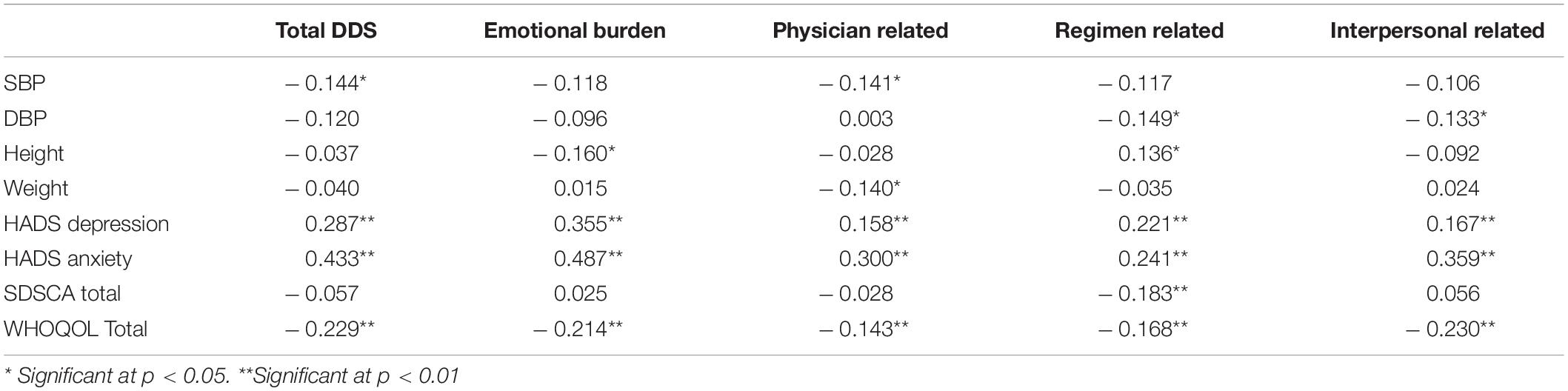
A statistically significant positive correlation between the HADS scale score (r = 0.287, p < 0.01) and the total SADDS-17 scores (r = 0.433, p < 0.01) related to the depression and anxiety and significant positive correlation with the other four sub-domains of SADDS-17 (Table 5).
A statistically significant negative correlation was seen between the systolic blood pressure (SBP) with the total SADDS-17 (r = −0.144, p < 0.05) and physician-related distress (r = −0.141, p < 0.05). Similarly, there was a significant negative correlation between diastolic blood pressure (DBP) with regimen-related distress (r = −0.149, p < 0.05) and interpersonal-related distress (r = −0.149, p < 0.05). A significant negative correlation was revealed between height and emotional burden distress (r = −0.16, p < 0.05) and between weight and physician-related distress (r = −0.14, p < 0.05).
The PHQ15 scores showed significant positive correlations with the total SADDS-17 scores (r = 0.288, p < 0.01) and each of the four subdomains. On the contrary, WHOQOL scores revealed significant negative correlations (r = −0.229, p < 0.01) with the SADDS-17 scores (Table 5). The SDSCA scores showed a significant negative correlation with regimen-related distress (r = −0.183, p < 0.01).
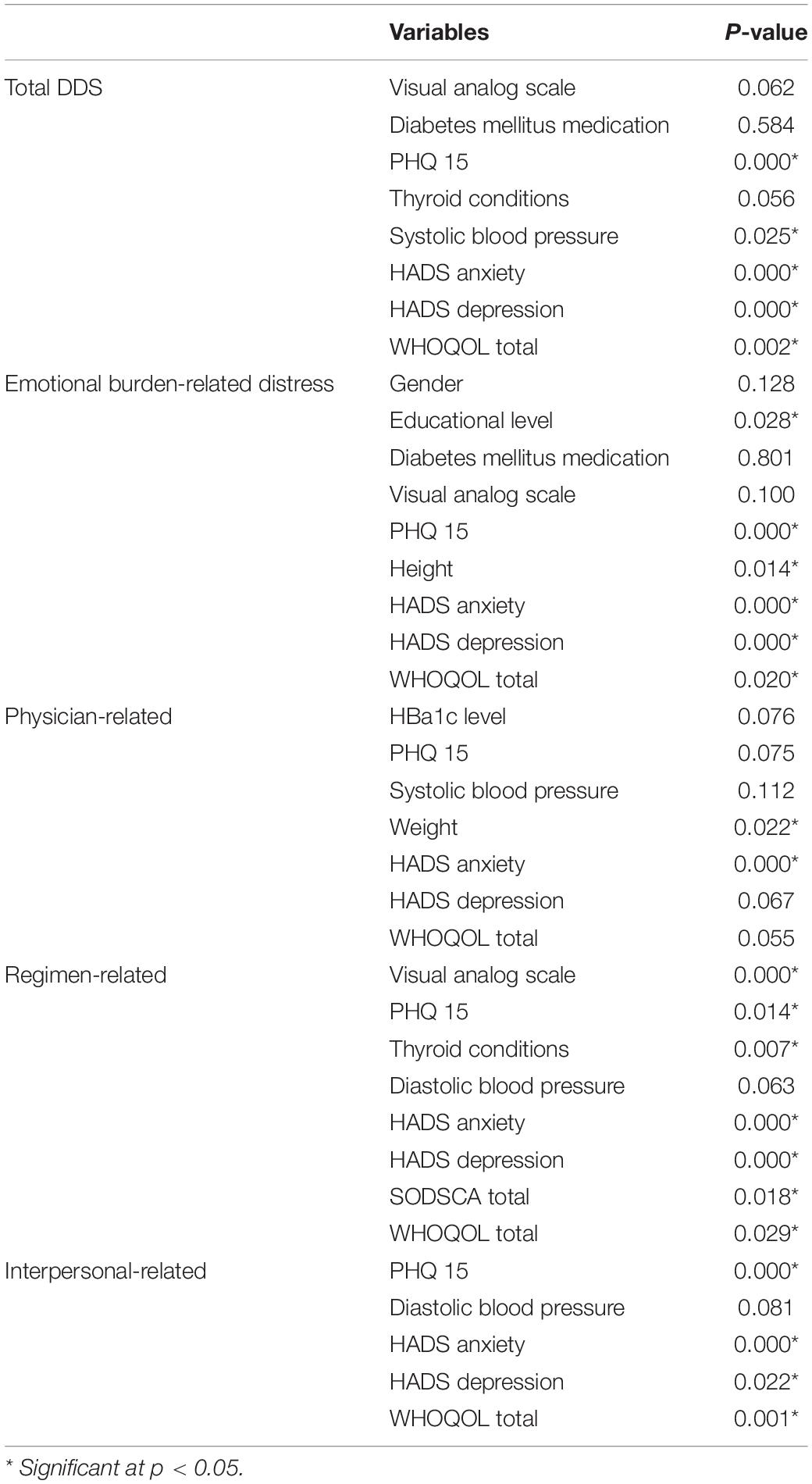
Among all variables associated with the total diabetes distress scores, PHQ 15 scores, SBP, HADS anxiety and depression scores, and WHOQOL total scores were shown to be independent variables. In the variables associated with the emotional burden, PHQ 15 scores, SBP, HADS anxiety and depression scores, and WHOQOL total scores were revealed as independent variables. For variables associated with physician-related diabetes distress, weight, and HADS anxiety scores were shown to be independent variables. Similarly, in the variables associated with regimen-related diabetes distress, VAS scores, PHQ 15 scores, thyroid conditions, HADS anxiety and depression scores, SDSCA total scores, and WHOQOL total scores were identified as the independent variables. Finally, the variables associated with interpersonal-related diabetes distress, PHQ 15 scores, HADS anxiety and depression scores, and WHOQOL total scores were revealed as independent variables (Table 6).
Discussion
Diabetes distress is a common health problem worldwide. The present findings demonstrated that 29.4% of people with diabetes had high distress, consistent with a recent systematic review and meta-analysis, where females were a higher proportion (Perrin et al., 2017). However, the prevalence of diabetes distress was relatively a little higher than in other local studies in Taif (25%) and Jazan (22.3%) cities (Aljuaid et al., 2018; Alzughbi et al., 2020). Consistent with an earlier study, the emotional burden had the highest impact on measuring diabetes distress (2.63 ± 1.29) among the four SADDS-17 subdomains (Onyenekwe et al., 2020).
In line with a previous study (Forsander et al., 2017), gender is the major factor influencing the levels of diabetes distress (emotional burden). Our findings indicate that females appeared particularly vulnerable, which may need more attention and support against diabetes distress. In parallel, a meta-analysis showed that females had higher diabetic distress than males and indicated that gender is the major socio-demographic factor associated with diabetes distress levels (Perrin et al., 2017).
The status of occupation plays a significant role in the development of depression and anxiety. People who are unemployed are more likely to experience anxiety and depression. The relationship between unemployment, depression, and anxiety can be described in two ways: sociological and economic. Individuals who are unemployed lack sociological functions such as time structure, status and identity, social contacts, participation in common goals, and consistent activity (Palizgir et al., 2013; Nordenmark and Strandh, 2016). In our study, over half of the individuals (54.2%) were unemployed, although this finding was unexpectedly unrelated to diabetes distress. Our findings contradict prior research, which revealed that unemployed people had higher levels of diabetes-related distress than employed people, ranging from 70 to 83.1% (Palizgir et al., 2013; Ramkisson et al., 2016; Dogra et al., 2017).
Our findings revealed that the illiterate group registered the highest emotional burden distress at 2.99 ± 1.43. Many studies suggested an inversely proportional relationship between the patients’ educational levels and diabetes distress levels. Those with low educational levels are more likely to experience more distress (van Bastelaar et al., 2010; Papelbaum et al., 2011; Graue et al., 2012; Baradaran et al., 2013). Similarly, another report indicated that the odds of becoming distressed over time were higher at a lower educational level (Fisher et al., 2009). Studies have also reported that low education leads to poor knowledge about the illness and its complications, which increases the risk of poor dietary habits, poor compliance to medication, and fewer health check-ups (Gahlan et al., 2018). Interestingly, consistent with the above findings, in our study, participants’ educational level revealed a notable influence on the level of diabetes distress (emotional burden). On the contrary, Wardian and Sun have reported that education was not significantly related to diabetes distress due to the lack of variation in education levels (Wardian and Sun, 2014). However, diabetes education requires individuals to increase self-efficacy and management of diabetes distress.
Consistent with previous findings (Fisher et al., 2008; van Bastelaar et al., 2010), HBA1c levels and diabetes distress had a significant negative correlation, and patients with higher (>7) HBA1c were experiencing lesser distress. On the contrary, a positive correlation between depression and HbA1c levels among diabetes patients was reported (Papelbaum et al., 2011), which may require further detailed investigation.
In line with prior international reports (Aikens, 2012), the influence of DM medication regimens on the level of diabetes distress was statistically significant at (p < 0.05). Previous quantitative research suggested that insulin-treated T2DM patients have experienced significantly higher diabetes distress, particularly regimen-related distress (Baek et al., 2014). In parallel, patients treated with insulin in our study had the highest amount of regimen-related distress at 2.85 ± 1.08. Surprisingly, the study indicated that insulin distress could take multiple forms, such as acute, sub-acute, or chronic insulin distress (Kalra and Balhara, 2018). However, in our present study, patients without any DM medication had the highest total diabetes distress (2.98 ± 1.42) than other medication groups.
Martino et al. (2019) looked at the impact of anxious and depressive symptoms, time since T2DM diagnosis, and metabolic control on health-related quality of life (HRQoL), focusing on physical and mental component summaries. In a chronic condition like T2DM, both anxiety levels and time since diagnosis play a predictive role in HRQoL. Higher Physical Component Summary (PCS) values, which indicate a superior HRQoL in the physical component, were linked to lower anxiety levels and a shorter period since T2DM diagnosis. Furthermore, greater Mental Component Summary (MCS) values, which indicate a superior HRQoL in the mental component, were linked to a reduction in anxiety and depression symptoms, but not to diabetes duration or metabolic control (Martino et al., 2019). Moreover, Bai et al. (2018) reported that both anxiety and depression were strongly correlated with diabetes distress. Anxiety has been attributed to fear of insulin injection and is common among people with diabetes (Abu Hassan et al., 2013). In this context, an extreme level of fear of self-injection is associated with high levels of diabetes distress, low general well-being, and psychological comorbidity, as well as poor adherence to the diabetes treatment regimen (Mollema et al., 2001; Abu Hassan et al., 2013). In agreement with the above findings, our finding showed a strong positive correlation between anxiety scores and the level of diabetes distress (r = 0.433, p < 0.01).
The total diabetes distress scores and sub-scales revealed a significant positive correlation with participants’ depressive scores as calculated from the HADS scale. The total DDS score showed (r = 0.287, p < 0.01) that depression was an independent variable to the total SADDS-17. Furthermore, Baradaran et al. (2013) reported a high percentage of diabetes distress patients diagnosed with depression. Adequate studies indicated a significant correlation between diabetes distress and depression symptoms among DM patients (Fisher et al., 2010; Chew et al., 2016).
Among past medical conditions, thyroid conditions had a statistically significant (p < 0.05) influence on the level of diabetes distress, which attribute to the close link between thyroid conditions and depressive symptoms. In agreement with our study, the clinical report indicated that patients with thyroid disorders are more prone to develop depression than those without thyroid disorders (Hage and Azar, 2012).
An independent strong negative correlation was revealed between WHOQOL-BREF scores related to the quality of life and the total diabetes distress scores (r = −0.229, p < 0.01). Inconsistent with our study, Morisky et al. (2008) reported that lower health-related quality of life was strongly associated with a higher level of emotional distress, which indicated that quality of life important predictor of diabetes distress.
The PHQ15 scores showed a significant positive correlation with the total SADDS-17 (r = 0.288, p < 0.01) and all four subdomains. Furthermore, we found an independent variable for the total SADDS-17 and its subdomains except (physician-related distress). Most interestingly, to the best of our knowledge, the relation between somatic symptoms and diabetes distress has not been addressed yet. However, it could be attributed to the link between somatic symptoms and quality of life. Alosaimi et al. indicated that the severity of somatic symptoms is correlated with a low quality of life (Alosaimi et al., 2019). Zhu et al. (2012) reported that an independent association exists between PHQ15 scores and depressive symptoms.
The SDSCA scores revealed a significant negative correlation with the regimen-related level of diabetes distress (r = −0.183, p < 0.05). Khan and Choudhary (2018) reported that high levels of diabetes distress might be attributed to reduced self-care management (Devarajooh and Chinna, 2017). We believe that fewer worries could be achieved if patients with diabetes are more adherent to self-care (exercise, dietary habits, blood glucose monitoring, and foot care); hence, less regimen-related diabetes distress could be experienced.
Limitations and Recommendations
Because the present study was a cross-sectional study, it has the following limitations that are mainly related to the study design. First, the temporal relationship between diabetes distress and certain factors could not confirm causality. Second, because this study used a convenience sample method from a single institute, the results cannot be applied to the entire Saudi Arabian population. Response bias may have occurred as a result of the sampling procedure. In order to resolve these limitations, further studies on a wider national scale are required to estimate the magnitude of diabetes distress in Saudi, as well as the use of more diversified approaches.
Conclusion
Our present study revealed that diabetes distress prevalence is alarmingly high among patients in Saudi Arabia, Riyadh. Our findings provide evidence that physical symptoms, quality of life, depression, and anxiety are notable predictors of diabetes distress.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Research Ethics Committee at King Saud University. The participants provided their written informed consent to participate in the study.
Author Contributions
MAB and FDA designed the study. AFA, AAA, OAA, MKA, KSA, AMA, and MTA facilitated data gathering. MAB, FDA, AFA, AAA, OAA, MKM, KSA, AMA, and MTA performed the data analysis and drafted the manuscript. All authors contributed to the interpretation of results and the revision of the manuscript, as well as approving the final manuscript.
Funding
This work was supported by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abu Hassan, H., Tohid, H., Amin, R. M., Long Bidin, M. B., Muthupalaniappen, L., and Omar, K. (2013). Factors influencing insulin acceptance among type 2 diabetes mellitus patients in a primary care clinic: a qualitative exploration. BMC Fam. Pract. 14:164. doi: 10.1186/1471-2296-14-164
Aikens, J. E. (2012). Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care 35, 2472–2478. doi: 10.2337/DC12-0181
Al-Daghri, N. M., Al-Attas, O. S., Alokail, M. S., Alkharfy, K. M., Yousef, M., Sabico, S. L., et al. (2011). Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region. Saudi Arabia (Riyadh cohort 2): a decade of an epidemic. BMC Med. 9:76. doi: 10.1186/1741-7015-9-76
AlHadi, A. N., AlAteeq, D. A., Al-Sharif, E., Bawazeer, H. M., Alanazi, H., AlShomrani, A. T., et al. (2017). An arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann. Gen. Psychiatry 16:32. doi: 10.1186/S12991-017-0155-1
Ali, S., Stone, M. A., Peters, J. L., Davies, M. J., and Khunti, K. (2006). The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabet. Med. 23, 1165–1173. doi: 10.1111/J.1464-5491.2006.01943.X
AlJohani, K., Ge, K., and Pd, S. (2016). Psychometric evaluation of the summary of diabetes self-care activities-arabic (SDSCA-Arabic): translation and analysis process. J. Transcult. Nurs. Off. J. Transcult. Nurs. Soc. 27, 65–72. doi: 10.1177/1043659614526255
Aljuaid, M. O., Almutairi, A. M., Assiri, M. A., Almalki, D. M., and Alswat, K. (2018). Diabetes-related distress assessment among type 2 diabetes patients. J. Diabetes Res. 2018:7328128. doi: 10.1155/2018/7328128
Alosaimi, F., Labani, R., Almasoud, N., Alhelali, N., Althawadi, L., and AlJahani, D. (2019). Associations of foot ulceration with quality of life and psychosocial determinants among patients with diabetes; a case-control study. J. Foot Ankle Res. 12:57. doi: 10.1186/S13047-019-0367-5
Alosaimi, F. D., AlMulhem, A., AlShalan, H., Alqazlan, M., Aldaif, A., Kowgier, M., et al. (2017). Psychosocial predictors of patient adherence to disease-modifying therapies for multiple sclerosis. Patient Prefer. Adherence 11, 513–518. doi: 10.2147/PPA.S129678
Alosaimi, F. D., Asiri, M., Alsuwayt, S., Alotaibi, T., Bin Mugren, M., Almufarrih, A., et al. (2016). Psychosocial predictors of nonadherence to medical management among patients on maintenance dialysis. Int. J. Nephrol. Renovasc. Dis. 9:263. doi: 10.2147/IJNRD.S121548
Alqurashi, K. A., Aljabri, K. S., and Bokhari, S. A. (2011). Prevalence of diabetes mellitus in a Saudi community. Ann. Saudi Med. 31, 19–23. doi: 10.4103/0256-4947.75773
Al-Rubeaan, K., Al-Manaa, H. A., Khoja, T. A., Ahmad, N. A., Al-Sharqawi, A. H., Siddiqui, K., et al. (2015). Epidemiology of abnormal glucose metabolism in a country facing its epidemic: SAUDI-DM study. J. Diabetes 7, 622–632. doi: 10.1111/1753-0407.12224
Alzughbi, T., Badedi, M., Darraj, H., Hummadi, A., Jaddoh, S., Solan, Y., et al. (2020). Diabetes-Related Distress and Depression in Saudis with Type 2 Diabetes. Psychol. Res. Behav. Manag. 13:453. doi: 10.2147/PRBM.S255631
Bădescu, S., Tătaru, C., Kobylinska, L., Georgescu, E., Zahiu, D., Zăgrean, A., et al. (2016). The association between Diabetes mellitus and Depression. J. Med. Life 9, 120.
Baek, R. N., Tanenbaum, M. L., and Gonzalez, J. S. (2014). Diabetes burden and diabetes distress: the buffering effect of social support. Ann. Behav. Med. 48, 145–155. doi: 10.1007/S12160-013-9585-4
Bai, X., Liu, Z., Li, Z., and Yan, D. (2018). The association between insulin therapy and depression in patients with type 2 diabetes mellitus: a meta-analysis. BMJ Open 8:e020062. doi: 10.1136/BMJOPEN-2017-020062
Balducci, S., D’Errico, V., Haxhi, J., Sacchetti, M., Orlando, G., Cardelli, P., et al. (2019). Effect of a behavioral intervention strategy on sustained change in physical activity and sedentary behavior in patients with type 2 diabetes: the IDES_2 randomized clinical trial. JAMA 321, 880–890. doi: 10.1001/JAMA.2019.0922
Baradaran, H. R., Mirghorbani, S.-M., Javanbakht, A., Yadollahi, Z., and Khamseh, M. E. (2013). Diabetes distress and its association with depression in patients with type 2 diabetes in Iran. Int. J. Prev. Med. 4:580.
Batais, M. A., Alosaimi, F. D., AlYahya, A. A., Aloofi, O. A., Almashouq, M. K., Alshehri, K. S., et al. (2021). Translation, cultural adaptation, and evaluation of the psychometric properties of an Arabic diabetes distress scale. Saudi Med. J. 42, 509–516. doi: 10.15537/smj.2021.42.5.20200286
Chew, B.-H., Vos, R., Mohd-Sidik, S., and Rutten, G. E. H. M. (2016). Diabetes-related distress, depression and distress-depression among adults with type 2 diabetes mellitus in malaysia. PLoS One 11:e0152095. doi: 10.1371/JOURNAL.PONE.0152095
Delahanty, L. M., Grant, R. W., Wittenberg, E., Bosch, J. L., Wexler, D. J., Cagliero, E., et al. (2007). Association of diabetes-related emotional distress with diabetes treatment in primary care patients with Type 2 diabetes. Diabet. Med. 24, 48–54. doi: 10.1111/J.1464-5491.2007.02028.X
Devarajooh, C., and Chinna, K. (2017). Depression, distress and self-efficacy: the impact on diabetes self-care practices. PLoS One 12:e0175096. doi: 10.1371/JOURNAL.PONE.0175096
Dogra, P., Prasad, S. R., and Subhashchandra, J. S. (2017). Assessment of depression and diabetes distress in type 2 diabetes mellitus patients in a tertiary care hospital of South India. Int. J. Res. Med. Sci. 5, 3880–3886. doi: 10.18203/2320-6012.IJRMS20173696
Finitsis, D. J., Pellowski, J. A., Huedo-Medina, T. B., Fox, M. C., and Kalichman, S. C. (2016). Visual analogue scale (VAS) measurement of antiretroviral adherence in people living with HIV (PLWH): a meta-analysis. J. Behav. Med. 396, 1043–1055. doi: 10.1007/S10865-016-9770-6
Fisher, L., Hessler, D. M., Polonsky, W. H., and Mullan, J. (2012). When is diabetes distress clinically meaningful?: establishing cut points for the diabetes distress scale. Diabetes Care 35, 259–264. doi: 10.2337/DC11-1572
Fisher, L., Mullan, J. T., Arean, P., Glasgow, R. E., Hessler, D., and Masharani, U. (2010). Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care 33, 23–28. doi: 10.2337/DC09-1238
Fisher, L., Mullan, J. T., Skaff, M. M., Glasgow, R. E., Arean, P., and Hessler, D. (2009). Predicting diabetes distress in patients with Type 2 diabetes: a longitudinal study. Diabet. Med. 26, 622–627. doi: 10.1111/J.1464-5491.2009.02730.X
Fisher, L., Skaff, M. M., Mullan, J. T., Arean, P., Glasgow, R. E., and Masharani, U. (2008). A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with Type 2 diabetes. Diabet. Med. 25, 1096–1101. doi: 10.1111/J.1464-5491.2008.02533.X
Fisher, L., Skaff, M. M., Mullan, J. T., Arean, P., Mohr, D., Masharani, U., et al. (2007). Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care 30, 542–548. doi: 10.2337/dc06-1614
Forsander, G., Bøgelund, M., Haas, J., and Samuelsson, U. (2017). Adolescent life with diabetes—Gender matters for level of distress. Experiences from the national TODS study. Pediatr. Diabetes 18, 651–659. doi: 10.1111/PEDI.12478
Gahlan, D., Rajput, R., Gehlawat, P., and Gupta, R. (2018). Prevalence and determinants of diabetes distress in patients of diabetes mellitus in a tertiary care centre. Diabetes Metab. Syndr. 12, 333–336. doi: 10.1016/J.DSX.2017.12.024
Graue, M., Haugstvedt, A., Wentzel-Larsen, T., Iversen, M. M., Karlsen, B., and Rokne, B. (2012). Diabetes-related emotional distress in adults: reliability and validity of the Norwegian versions of the Problem Areas in Diabetes Scale (PAID) and the Diabetes Distress Scale (DDS). Int. J. Nurs. Stud. 49, 174–182. doi: 10.1016/J.IJNURSTU.2011.08.007
Hage, M., and Azar, S. T. (2012). The link between thyroid function and depression. J. Thyroid Res. 2012, 590648. doi: 10.1155/2012/590648
IDF Diabetes Atlas (2019). IDF Diabetes Atlas, 9th Edn. Available online at: https://www.diabetesatlas.org/en/ (accessed October 28, 2021).
Kalra, S., and Balhara, Y. P. S. (2018). Insulin distress. U.S. Endocrinol. 14, 27–29. doi: 10.17925/USE.2018.14.1.27
Karlsen, B., Oftedal, B., and Bru, E. (2012). The relationship between clinical indicators, coping styles, perceived support and diabetes-related distress among adults with type 2 diabetes. J. Adv. Nurs. 68, 391–401. doi: 10.1111/J.1365-2648.2011.05751.X
Khaledi, M., Haghighatdoost, F., Feizi, A., and Aminorroaya, A. (2019). The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. 56, 631–650. doi: 10.1007/S00592-019-01295-9
Khan, A., and Choudhary, P. (2018). Investigating the association between diabetes distress and self-management behaviors. J. Diabetes Sci. Technol. 12, 1116–1124. doi: 10.1177/1932296818789721
Malasi, T. H., Mirza, I. A., and El-Islam, M. F. (1991). Validation of the hospital anxiety and depression scale in arab patients. Acta Psychiatr. Scand. 84, 323–326. doi: 10.1111/J.1600-0447.1991.TB03153.X
Martino, G., Caputo, A., Bellone, F., Quattropani, M. C., and Vicario, C. M. (2020). Going Beyond the visible in type 2 diabetes mellitus: defense mechanisms and their associations with depression and health-related quality of life. Front. Psychol. 11:267. doi: 10.3389/FPSYG.2020.00267
Martino, G., Catalano, A., Bellone, F., Russo, G. T., Vicario, C. M., Lasco, A., et al. (2019). As Time goes by: anxiety negatively affects the perceived quality of life in patients with type 2 diabetes of long duration. Front. Psychol. 10:1779. doi: 10.3389/FPSYG.2019.01779
Mayberry, L. S., Nelson, L. A., and Gonzalez, J. S. (2021). Adults with type 2 diabetes benefit from self-management support intervention regardless of depressive symptoms. J. Diabetes Complications 35, 108024–108024. doi: 10.1016/J.JDIACOMP.2021.108024
Mollema, E. D., Snoek, F. J., Adèr, H. J., Heine, R. J., and van der Ploeg, H. M. (2001). Insulin-treated diabetes patients with fear of self-injecting or fear of self-testing: psychological comorbidity and general well-being. J. Psychosom. Res. 51, 665–672. doi: 10.1016/S0022-3999(01)00229-X
Morisky, D. E., Ang, A., Krousel-Wood, M., and Ward, H. J. (2008). Predictive validity of a medication adherence measure in an outpatient setting. J. Clin. Hypertens. (Greenwich). 10:348. doi: 10.1111/J.1751-7176.2008.07572.X
Naicker, K., Øverland, S., Johnson, J. A., Manuel, D., Skogen, J. C., Sivertsen, B., et al. (2017). Symptoms of anxiety and depression in type 2 diabetes: associations with clinical diabetes measures and self-management outcomes in the Norwegian HUNT study. Psychoneuroendocrinology 84, 116–123. doi: 10.1016/J.PSYNEUEN.2017.07.002
Nordenmark, M., and Strandh, M. (2016). Towards a sociological understanding of mental well-being among the unemployed: the role of economic and psychosocial factors. Sociology 33, 577–597. doi: 10.1017/s003803859900036x
Ohaeri, J. U., and Awadalla, A. W. (2009). The reliability and validity of the short version of the WHO Quality of Life Instrument in an Arab general population. Ann. Saudi Med. 29, 98–104. doi: 10.4103/0256-4947.51790
Onyenekwe, B. M., Young, E. E., Nwatu, C. B., Okafor, C. I., and Ugwueze, C. V. (2020). Diabetes Distress and Associated Factors in Patients with Diabetes Mellitus in South East Nigeria. Dubai Diabetes Endocrinol. J. 26, 31–37. doi: 10.1159/000508706
Palizgir, M., Bakhtiari, M., and Esteghamati, A. (2013). Association of depression and anxiety with diabetes mellitus type 2 concerning some sociological factors. Iran. Red Crescent Med. J. 15:644. doi: 10.5812/IRCMJ.12107
Papatheodorou, K., Banach, M., Bekiari, E., Rizzo, M., and Edmonds, M. (2018). Complications of Diabetes 2017. J. Diabetes Res. 2018:3086167. doi: 10.1155/2018/3086167
Papelbaum, M., Moreira, R. O., Coutinho, W., Kupfer, R., Zagury, L., Freitas, S., et al. (2011). Depression, glycemic control and type 2 diabetes. Diabetol. Metab. Syndr. 3:26. doi: 10.1186/1758-5996-3-26
Perrin, N. E., Davies, M. J., Robertson, N., Snoek, F. J., and Khunti, K. (2017). The prevalence of diabetes-specific emotional distress in people with Type 2 diabetes: a systematic review and meta-analysis. Diabet. Med. 34, 1508–1520. doi: 10.1111/DME.13448
Polonsky, W. H., Fisher, L., Earles, J., Dudl, R. J., Lees, J., Mullan, J., et al. (2005). Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care 28, 626–631. doi: 10.2337/DIACARE.28.3.626
Ramkisson, S., Pillay, B. J., and Sartorius, B. (2016). Diabetes distress and related factors in South African adults with type 2 diabetes. J. Endocrinol. Metabol. Diabetes South Afr. 21, 35–39. doi: 10.1080/16089677.2016.1205822
Tran, N.-N., Nguyen, V.-Q., Vo, H.-L., Hoang, T.-P.-N., Bui, V.-S., and Nguyen, V.-T. (2021). Depression among patients with type 2 diabetes mellitus: evidence from the Northeast region of Vietnam. Diabetes Metab. Syndr. Clin. Res. Rev. 15:102293. doi: 10.1016/J.DSX.2021.102293
van Bastelaar, K. M. P., Pouwer, F., Geelhoed-Duijvestijn, P. H. L. M., Tack, C. J., Bazelmans, E., Beekman, A. T., et al. (2010). Diabetes-specific emotional distress mediates the association between depressive symptoms and glycaemic control in Type 1 and Type 2 diabetes. Diabet. Med. 27, 798–803. doi: 10.1111/J.1464-5491.2010.03025.X
Wardian, J., and Sun, F. (2014). Factors associated with diabetes-related distress: implications for diabetes self-management. Soc. Work Health Care 53, 364–381. doi: 10.1080/00981389.2014.884038
WHOQOL (2021). Measuring Quality of Life| The World Health Organization. Available online at: https://www.who.int/tools/whoqol (accessed October 28, 2021).
Zeller, A., Ramseier, E., Teagtmeyer, A., and Battegay, E. (2008). Patients’ self-reported adherence to cardiovascular medication using electronic monitors as comparators. Hypertens. Res. 31, 2037–2043. doi: 10.1291/HYPRES.31.2037
Zhou, H., Zhu, J., Liu, L., Li, F., Fish, A. F., Chen, T., et al. (2017). Diabetes-related distress and its associated factors among patients with type 2 diabetes mellitus in China. Psychiatry Res. 252, 45–50. doi: 10.1016/J.PSYCHRES.2017.02.049
Keywords: prevalence, diabetes distress, psychosocial predictors, type 2 diabetes, Saudi adults
Citation: Batais MA, Alfraiji AF, Alyahya AA, Aloofi OA, Almashouq MK, Alshehri KS, Almizel AM, Alotaibi MT and Alosaimi FD (2021) Assessing the Prevalence of Diabetes Distress and Determining Its Psychosocial Predictors Among Saudi Adults With Type 2 Diabetes: A Cross-Sectional Study. Front. Psychol. 12:759454. doi: 10.3389/fpsyg.2021.759454
Received: 07 September 2021; Accepted: 12 November 2021;
Published: 22 December 2021.
Edited by:
Mariagrazia Di Giuseppe, University of Pisa, ItalyReviewed by:
Federica Bellone, University of Messina, ItalyGiorgia Varallo, Istituto Auxologico Italiano, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Italy
Copyright © 2021 Batais, Alfraiji, Alyahya, Aloofi, Almashouq, Alshehri, Almizel, Alotaibi and Alosaimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed A. Batais, drmohammed34@gmail.com; Mbatais@ksu.edu.sa
†ORCID: Mohammed A. Batais, orcid.org/0000-0001-6766-7553; Abdulaziz F. Alfraiji, orcid.org/0000-0002-5405-5045; Abdulrahman Abdullah Alyahya, orcid.org/0000-0001-6667-4495; Ouf Abdullatif Aloofi, orcid.org/0000-0002-4169-0699; Mohammad Khalid Almashouq, orcid.org/0000-0002-4739-0611; Khalid Saeed Alshehri, orcid.org/0000-0003-4840-0698; Abdulrahman Mohammed Almizel, orcid.org/0000-0003-2016-4224; Fahad D. Alosaimi, orcid.org/0000-0003-1027-5836
 Mohammed A. Batais
Mohammed A. Batais Abdulaziz F. Alfraiji
Abdulaziz F. Alfraiji Abdulrahman Abdullah Alyahya
Abdulrahman Abdullah Alyahya Ouf Abdullatif Aloofi
Ouf Abdullatif Aloofi Mohammad Khalid Almashouq
Mohammad Khalid Almashouq Khalid Saeed Alshehri
Khalid Saeed Alshehri Abdulrahman Mohammed Almizel
Abdulrahman Mohammed Almizel Mohammed Taraheeb Alotaibi2
Mohammed Taraheeb Alotaibi2 Fahad D. Alosaimi
Fahad D. Alosaimi