- 1NSW Office of Preventive Health, Liverpool, NSW, Australia
- 2Sydney School of Public Health, Sydney Medical School, University of Sydney, Sydney, NSW, Australia
- 3NHMRC Centre of Research Excellence in the Early Prevention of Obesity in Childhood, Sydney School of Public Health, University of Sydney, Sydney, NSW, Australia
- 4Charles Perkins Centre, University of Sydney, Sydney, NSW, Australia
- 5Prevention Research Collaboration, Sydney School of Public Health, University of Sydney, Sydney, NSW, Australia
Background: Childhood obesity is an important public health issue. Approximately 20% of 2–4 year olds are overweight or obese, meaning 1 in 5 Australian children start school above a healthy weight. In the state of New South Wales (NSW) the combined prevalence of childhood overweight and obesity is significantly higher among children from low socioeconomic status backgrounds and children from regional, rural and remote areas. This paper describes implementation of a healthy eating and active play program (Munch & Move) for center-based early childhood education and care (ECEC) services aimed at influencing healthy behaviors in young children in NSW, Australia. It shows changes over time including a focus on disadvantaged, Aboriginal and remote communities. It also discusses the challenges and future opportunities for the program.
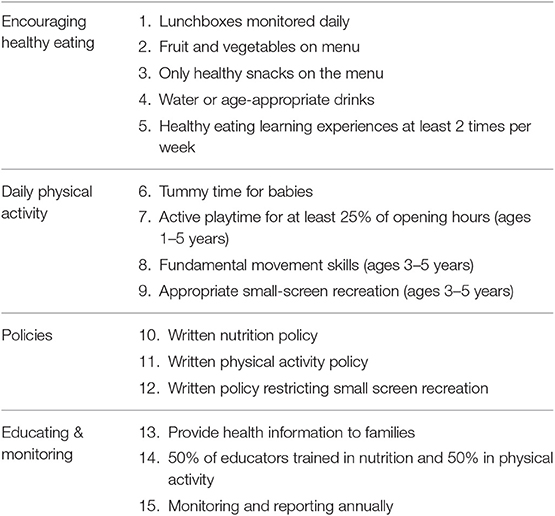
Methods: Routine data in relation to service delivery (reach) and implementation indicators are collected by Local Health District staff. Fifteen implementation indicators (known as practices) were introduced to monitor the implementation of Munch & Move (six related to promoting and encouraging healthy eating, four related to improving physical activity, two related to small screen recreation; and three related to quality of service delivery).
Results: As of 30 June 2017, 88.4% of ECEC services have staff trained in Munch & Move. Of the 15 practices related to promoting and encouraging healthy eating, increasing physical activity and improving the quality of service delivery 13 practices saw significant improvements between 2012 and 2017. This was consistent for services with a high proportion of Aboriginal children and for services in disadvantaged and remote communities. There has been a statistically significant increase in the proportion (37.6–81.0%, p < 0.0001) and type of ECEC services (preschools 36.1–81.3%, p < 0.0001, long day care 38.6–81.0%, p < 0.0001, and occasional care 34.0–74.6%, p < 0.0001) that have implemented the program since 2012 as well as in services with a high proportion of Aboriginal children (33.6–85.2% p < 0.0001), services in disadvantaged communities (37.4–83.3% p < 0.001), and services in remote communities (27.8–59.4% p < 0.0139).
Discussion: This paper demonstrates that Munch & Move has seen large improvements in the delivery of training, practice achievements and program adoption in ECEC services across NSW including services in disadvantaged and remote communities and that have a higher proportion of Aboriginal children.
Background
Childhood obesity is one of the most important public health issues facing Australia. Approximately 20% of 2–4 year olds are overweight or obese (1), meaning 1 in 5 Australian children start school above a healthy weight (2). A study conducted in New South Wales (NSW) found the combined prevalence of overweight and obesity among primary school children was significantly higher among children from low socioeconomic status (SES) backgrounds (35%) than children from high SES backgrounds (18.9%) and the prevalence significantly increased among children from regional, rural, and remote areas from 17.4% in 2010 to 21.1% in 2015 (2). Children from Aboriginal and Torres Strait Islander (Indigenous) communities are also more likely to be overweight or obese than non-Indigenous children (30% compared with 25%) (3).
Early childhood is an important period to establish healthy eating and physical activity behaviors (4, 5), and provides a critical time to implement obesity prevention initiatives. Children spend a significant amount of time in early childhood settings including preschools, long day care and family day care services (6). These services present an opportunistic setting to promote and establish good healthy eating and physical activity habits. They also provide a setting where the organizational infrastructure required for health promotion activities is available and responsive to program implementation. The Get Up & Grow guidelines in Australia (7) and the Early Childhood Obesity Prevention Policies in United States (8) are specific guidelines and recommendations which have been developed to promote healthy environments for young children and prevent obesity in early childhood. The World Health Organization (WHO) strongly recommends that guidance on, and support for key obesity prevention behaviors in early childhood be provided to ensure children grow appropriately and develop healthy habits (9). The WHO implementation plan recommends that settings like child care create healthy food environments and incorporate physical activity into daily routines (10). The plan outlines key elements for implementation of programs including capacity building, advocacy, expanding the knowledge base, mobilizing resources and most importantly, monitoring and accountability.
The Munch & Move program is a key state-wide healthy eating and active play program aimed at influencing the healthy eating and physical activity environments of young children aged from birth to 5 years. Munch & Move is designed to build capacity in center-based early childhood education and care (ECEC) services (preschools, long day care, and occasional care) to promote and encourage children's healthy eating and physical activity and reduce small screen recreation in young children, as well as influence policies and practices in the service. The program aligns with the key elements of the WHO implementation plan (10).
Evidence shows that regulation and educational workshops and training for child care providers on nutrition, physical activity and screen-time behaviors increased knowledge, improved center policies and reduced body mass index for children in child care centers in the United States (11, 12). In Australia, obesity prevention interventions in preschools have shown significant positive changes in children's food intake, movement skills, indicators of weight status, and reduction in the prevalence of overweight and obesity (13–16). A written physical activity policy, structured staff-led physical activity and staff participating in active play have also been associated with higher levels of physical activity in preschools (16). It has also been demonstrated through initial implementation of Munch and Move in pre-schools that it is a feasible, acceptable, and appropriate way to build knowledge and skills of early childhood professionals (17).
There are two aims of this paper. The first is to describe training and implementation of the Munch & Move program over time with a focus on implementation in disadvantaged, Aboriginal and remote communities. The second aim is to discuss the challenges and future opportunities for the program.
Methods
Description of the Munch & Move Program
Munch & Move was launched in July 2008 initially targeting children from 3 to 5 years of age attending preschools in NSW. In 2010 the program was scaled-up to be state-wide and inclusive of long day care and occasional care services covering children aged from birth to 5 years (18). More information on the Munch & Move program is provided on the NSW Healthy Kids website (www.healthykids.nsw.gov.au/campaigns-programs/about-munch-move.aspx). To create an environment that is supportive of healthy eating and physical activity Munch & Move is based on six health promoting key messages–encourage and support breastfeeding, choose water as a drink, choose healthier snacks, eat more fruit and vegetables, get active each day and turn off the screen and get active.
Munch & Move offers professional development training for early childhood educators to implement a fun, play-based approach to supporting healthy eating and physical activity habits in young children. It also offers practical resources (i.e., resource manual, poster, instructional videos for fundamental movement skills and a music CD) to support service policies and practices, support visits and regular contact from Local Health District (LHD) health professionals and fact sheets to communicate the key messages with families (18). The program is implemented using a “whole-of-service” health promotion approach (10, 19) which means bringing together directors, management, educators, staff, children, and families to create an environment that is supportive of healthy eating and physical activity. The program is strongly aligned to the National Quality Framework (NQF) (7) and in particular to children's health and safety, which outlines specific standards relating to the provision of healthy food and drinks, and the promotion of physical activity through planned and spontaneous experiences (20, 21).
Program training is delivered to early childhood educators working in ECEC services by an early childhood registered training organization. From July 2008 to April 2015 362 full day face-to-face workshops were delivered and from July 2015 to June 2017 training was delivered via 51 “live” webinar series consisting of four 2 h modules as this was seen to be more flexible and accessible for educators. The objective of the training is to provide early childhood educators with information on the Munch & Move key messages, the Australian Dietary Guidelines and Physical Activity and Sedentary Behavior Recommendations, how to engage children in healthy eating related learning experiences, how to increase the amount of physical activity children engage in and how to develop their fundamental movement skills. Ongoing LHD support allows the program to be tailored to the needs of the local community and each individual service for example local workshops on healthy eating experiences and resources for Aboriginal families.
Description of the Early Childhood Education and Care Context
As of September 2017 there were 3,753 approved ECEC services (excluding family day care and outside school hours care) in NSW (22) which is a significant increase from 2012 where there were around 2,600 (23). Of these there were 38 (1%) services located in remote locations and 1,945 (51.8%) services in low SES areas (24). In NSW there were ~596,234 children aged 0–5 years (25) and ~390,790 attended an ECEC service (6).
Evaluation and Monitoring Framework
The monitoring framework on which this paper is based is described in Farrell et al. (26) It includes routine data collected by LHDs in relation to service delivery indicators (i.e., number and classification of ECEC services across NSW and number trained in Munch & Move). It also includes implementation indicators (i.e., number of practices achieved and not achieved by services).
Because the prevalence of childhood obesity is higher in disadvantaged, Aboriginal and remote communities, the implementation of Munch & Move is also monitored and reported for these three types of communities. Disadvantaged communities are those communities located in the two most disadvantaged communities as measured by the Socio-economic Index for Areas [SEIFA quintiles 1 and 2] (27). Aboriginal communities are those communities with a high proportion of Aboriginal children in their care (10% or more children identified as being from Aboriginal background). Communities are classified as being remote based on their postcode (defined by the Accessibility/Remoteness Index of Australia [ARIA] classifications) (28).
Dodds et al. conducted a validation study of certain measures to implement and monitor obesity prevention policies and practices (29). Fifteen program adoption indicators (known as practices) were modified from this validated instrument and introduced to monitor the implementation of Munch & Move across NSW and to inform LHD service delivery. The monitoring framework for center-based ECEC services includes four domains and 15 practices, as detailed in Table 1.
To ensure consistent data collection by LHDs a monitoring guide was developed. It includes detailed practices and questions to measure achievement (see Table S1).
Data Sources and Analysis
A list of approved ECEC services across NSW was obtained from a government regulatory agency and is updated by LHDs on a regular basis. This list includes service name and license code, service type (i.e., preschool, long day care), local government area, contact details and opening days and hours. Practice data was initially collected via a computer assisted telephone interview (CATI) through self-reporting by a service representative. Subsequent data has been collected by trained health promotion officers through regular scheduled support visits, where data were collected through observation and conversations with the service representative.
Data on practices were collected using the monitoring guide (see Table S1). Data are stored in the NSW Health Population Health Information Management System (PHIMS). This system enables monitoring and reporting of the implementation of Healthy Children Initiative programs (30).
From July 2012 to June 2016 program adoption was measured and reported with reference to the number of services achieving 70% (or more) of the practices that were relevant for their particular service. From July 2016 to June 2017 the benchmark was increased to drive continuous quality improvement of program implementation. The new benchmark was the number of services achieving 80% (or more) of the practices that are relevant for their particular service.
Data Analysis
Data were reported as percentages (%) or proportion of the total of ECEC services achieving training, practice achievement, and program adoption targets. Chi-squared tests for differences in proportion were used to ascertain differences between data collection points as well as difference of training, practice and adoption measures between type of service and priority groups. Data analysis was performed using Microsoft Excel 2013. Differences were regarded as statistically significant at the p < 0.05 level.
Results
Data relating to training has been collected since July 2008 and monitoring of program implementation has been collected since July 2012.
Training
Trained is defined as attendance at a workshop or completion of a webinar series. As of 30 June 2017, 88.4% (n = 3,328) of center-based ECEC services had staff trained in Munch & Move (e.g., at least one staff had attended a workshop or completed a webinar series). There were variations between the type of services that had taken part in the training, with a significantly higher proportion of preschools having their staff trained (n = 830, 92.0%) compared to long day care (n = 2,424, 87.6%, chi-squared = 11.959, p = 0.0005) and other center-based services (n = 17, 56.7%, chi-squared = 26.080, p < 0.0001), which included distance learning, early intervention, and mobile services. For occasional care services 90.5% (n = 17) of staff were trained and this was not significantly different from preschool (chi-squared = 0.051, p = 0.8219 or long day care services (chi-squared = 0.131, p = 0.7176).
The proportion of ECEC services whose staff had undergone training was significantly higher for services with a higher proportion of Aboriginal children (n = 255, 95.3%, chi-squared = 11.416, p = 0.0007) and for services in disadvantaged communities (n = 1369, 92.8%, chi-squared = 21.506, p < 0.0001) when compared to the NSW average. Services in remote communities also had higher training attendance (n = 34, 94.1%) when compared to the NSW average, however, this was not significantly different (chi-squared = 1.071, p = 0.3008).
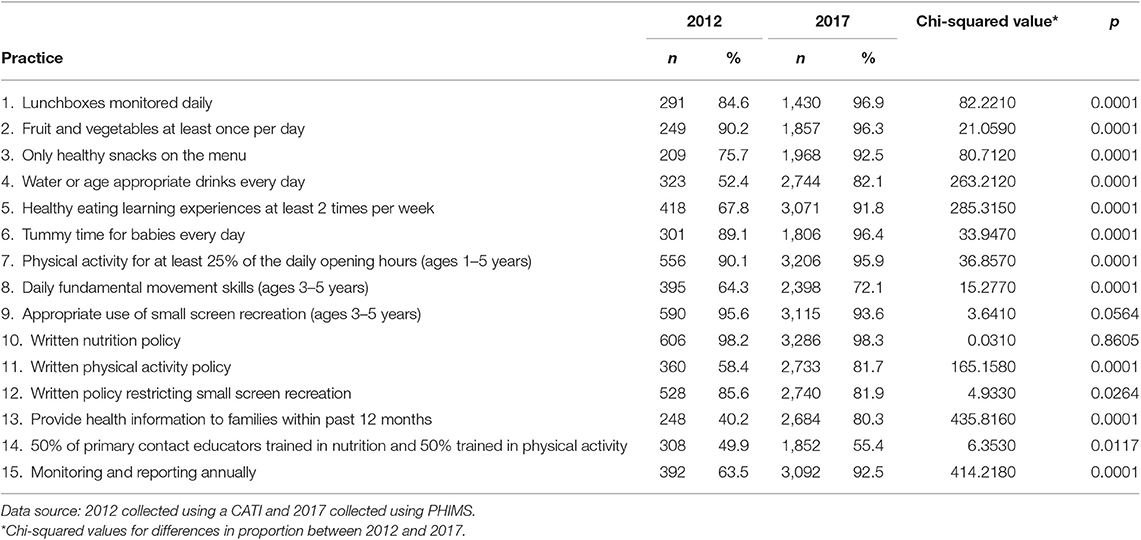
Practice Achievement Over Time
Practice achievement is defined as “met” in accordance with the monitoring guide. There have been substantial increases in practice achievements made by ECEC services since 2012 (Table 2). Of the 15 practices there were significant improvements in 13 practices between 2012 and 2017. There were only two practices where no significant differences occurred and these were having a written nutrition policy (already at 98%) and having 50% of primary contact educators trained in nutrition and physical activity. Two practices that already had relatively high levels of achievement in 2012 but decreased in 2017 were related to small screen recreation, namely appropriate use of small screen recreation and a written policy restricting small screen recreation.
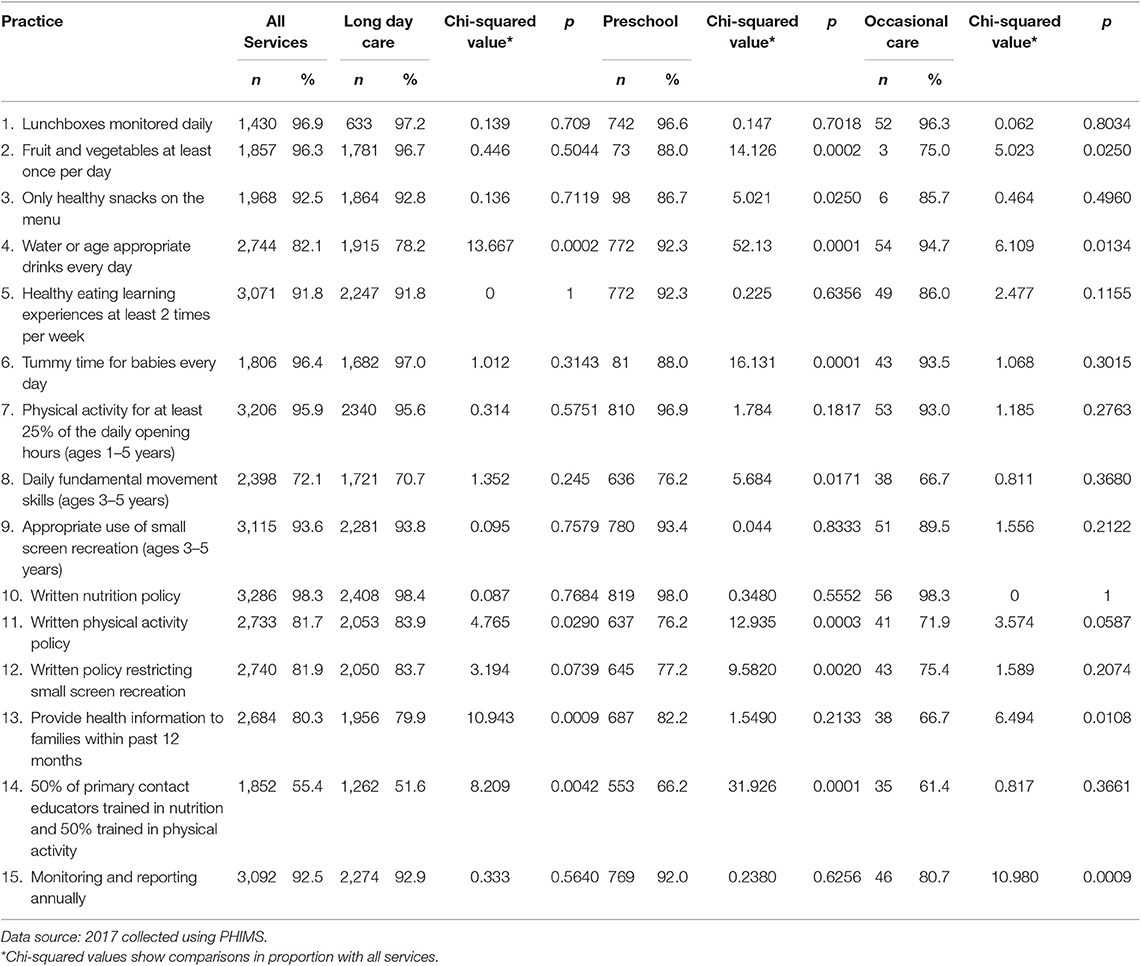
Practice Achievement Across Service Type
Practice achievements across type of service were fairly consistent, with some notable exceptions (Table 3). When compared to “All Services,” long day care services were significantly less likely to provide water or age appropriate drinks and to have 50% of contact educators trained in nutrition and physical activity. Long day care services were significantly more likely than “All Services” to have a written physical activity policy. Preschools were significantly more likely than “All Services” to provide water or age appropriate drinks every day, to provide daily fundamental movement skills and to have 50% of primary contact educators trained in nutrition and physical activity. However, they were significantly less likely than “All Services” to provide daily fruit and vegetables, only have healthy snacks, provide daily tummy time for babies and to have written policies for physical activity and restricting small screen recreation. Occasional care services were significantly more likely than “All Services” to provide water or age appropriate drinks every day, but significantly less likely to provide fruit and vegetables at least once a day, provide health information to families and undertake annual monitoring and reporting.
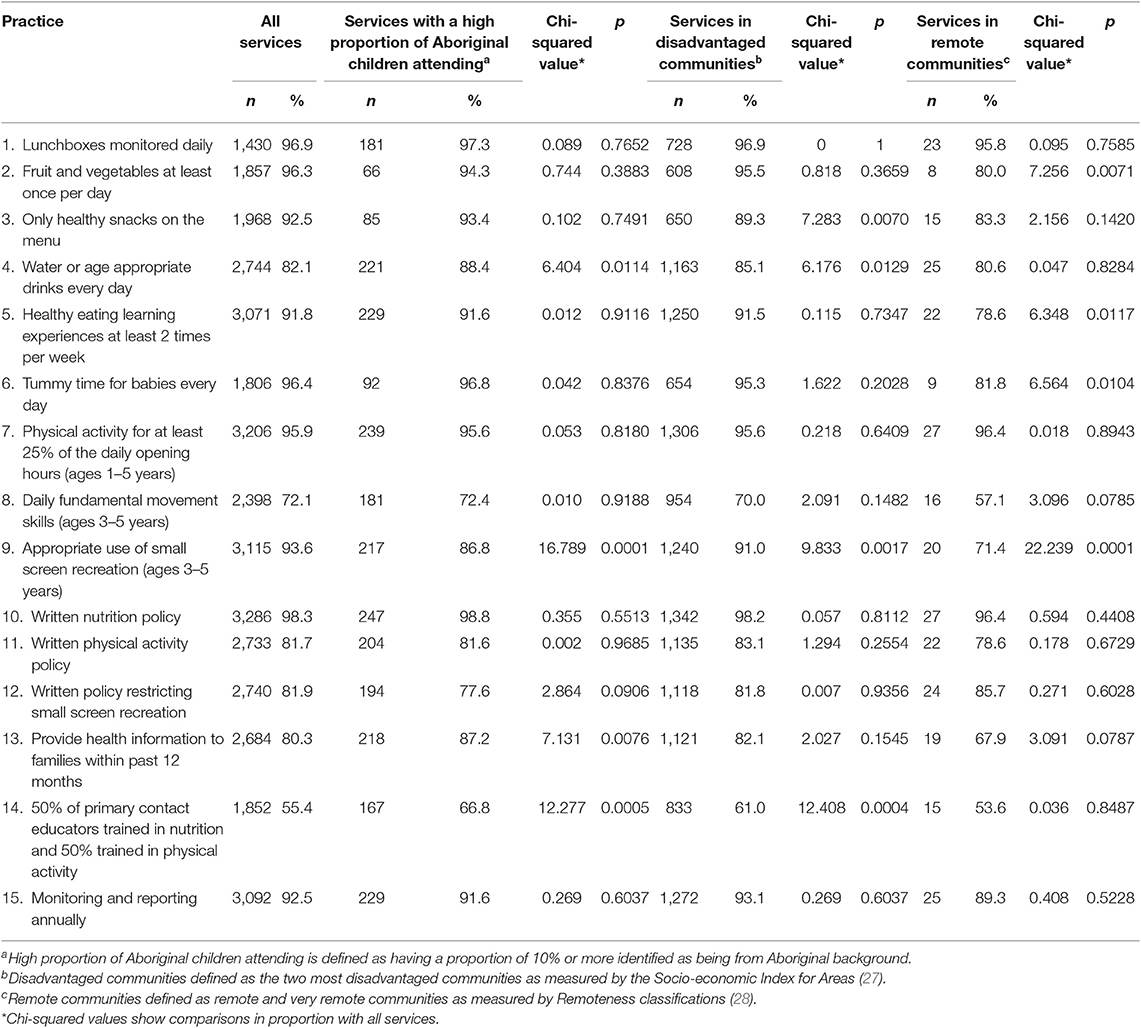
Practice Achievement by Priority Population Group
Practice achievements across ECEC services with a high proportion of Aboriginal children, services in disadvantaged communities, and services in remote communities had some significant differences when compared with “All Services” (Table 4). Services with a high proportion of Aboriginal children were significantly more likely than “All Services” to provide water or age appropriate drinks daily, provide health information to families and to have 50% of primary contact educators trained in nutrition and physical activity, However, these services were significantly less likely than “All Services” to have appropriate use of small screen recreation. Services in disadvantaged communities were significantly more likely than “All Services” to provide water or age appropriate drinks daily and to have 50% of primary contact educators trained in nutrition and physical activity, but significantly less likely to offer only healthy snacks and have appropriate use of small screen recreation. Services in remote communities were significantly less likely than “All Services” to offer fruit and vegetables daily, have healthy eating learning experiences at least twice a week, provide daily tummy time for babies and have appropriate use of small screen recreation.
Program Adoption
Program adoption is reported with reference to the number of services achieving a defined per cent of the practices that are relevant for their particular service. There has been a statistically significant increase in the proportion and type of ECEC services that have implemented Munch & Move since state-wide monitoring was introduced in 2012. In 2012 the total services across NSW achieving 70% (or more) of the practices was 37.6% and by June 2016 this increased to 81.0% (chi-squared = 1356.513, p < 0.0001). For preschools it increased from 36.1 to 81.3% (chi-squared = 366.865, p < 0.0001), for long day care it increased from 38.6 to 81.0% (chi-squared = 947.856, p < 0.0001), and for occasional care it increased from 34.0 to 74.6% (chi-squared = 19.095, p < 0.0001).
As of 30 June 2017, 71.6% (2,687/3,601) of ECEC services had achieved 80% (or more) of the program practices. Due to the proportion of practices to be achieved increasing from 70 to 80%, the proportion of services adopting the program between 2016 (81.0%) and 2017 (71.6%) decreased slightly; corresponding decreases in program adoption were seen for preschools (77.7%), long day care (69.8%), and occasional care services (66.7%).
There has been a statistically significant increase in the proportion of ECEC services within priority population groups that have implemented Munch & Move. From 2012 to 2016 services with a high proportion of Aboriginal children increased from 33.6 to 85.2% (chi-squared = 136.947, p < 0.0001), services in disadvantaged communities increased from 37.4 to 83.3% (chi-squared = 628.551, p < 0.0001) and services in remote communities increased from 27.8 to 59.4% (chi- squared = 6.053, p = 0.0139).
From 2016 to 2017 there was a decrease for ECEC services with a high proportion of Aboriginal children (81.2%) and disadvantaged communities (76.4%). This decrease was because of the change in the benchmark. However, program adoption for services in remote communities increased to 66.7% despite the change in the benchmark.
Discussion
This paper has described the training and implementation of the Munch & Move program over time with a focus on implementation in disadvantaged, Aboriginal and remote communities. The Munch & Move program has influenced the healthy eating and physical activity environments in NSW ECEC services. Our findings are consistent with the Nutrition and Physical Activity Self Assessment for Child Care intervention conducted in the USA and the Romp & Chomp intervention conducted in Victoria, Australia. They support the notion that early interventions targeting ECEC services (i.e., educator knowledge and support to change service policies and practices) can create opportunities to improve children's health and well-being (12, 31).
Based on the literature, multi-component, multi-level early childhood education interventions with parental engagement are most likely to be effective for obesity prevention (32). Therefore, sustained implementation of Munch & Move in ECEC services is likely to be effective in supporting children to establish healthy eating and physical activity behaviors and contribute to preventing overweight and obesity. A recent analysis has shown that while there has been no increase in the prevalence of overweight and obesity in all primary school children in NSW, among 5–6 year olds this prevalence decreased from 23.9% in 2010 to 17.5% in 2015 (2). In addition, the prevalence of overweight and obesity in kindergarten children in regional, rural, and remote areas decreased from 17.4% in 2010 to 15.5% in 2015 and for low SES it decreased from 29.1% in 2010 to 27.8% in 2015.
Attendance at training across NSW is high, and is significantly higher in preschools than in long day care and occasional care services. This may be due to the program initially being available only for preschools who have therefore had longer to access training. Training is also high among priority population groups which may be a reflection of local prioritization of program delivery to these groups and access to a free program in varying training modes (i.e., workshops and webinar series).
Increases in program implementation, measured by practice achievement, have also occurred between 2012 and 2017. Some practices such as having a nutrition policy were achieved early on as they had been part of the regulations prior to the introduction of the NQF. The practice for staff on-training did not change significantly and this could be due to high staff turnover in ECEC services. The two practices that decreased during this period were related to screen time and this may be due to the increased availability and use of screens in services for educational purposes. Practice achievement across the different service types was similar and the differences may be reflective of the organizational structures (i.e., food and drinks provided by the service or by family in lunchboxes), qualifications of staff working in these service types (i.e., all educators working in preschools must have teaching qualifications so training of 50% of staff in nutrition and physical activity is not seen as necessary) and the regulation framework (i.e., occasional care services do not come under the NQF so may not have documented reporting). Practice achievement among priority population groups was significantly higher except for the appropriate use of small screen devices. ECEC services in remote communities were also less likely to offer fruit and vegetables daily, to offer only healthy snacks and to have healthy eating learning experiences at least twice a week.
This analysis reports that the reach and program adoption by ECEC services in disadvantaged and remote communities and those services with a higher proportion of Aboriginal children was similar. This demonstrates equitable program implementation, particularly for the most vulnerable communities. These results are consistent with a study conducted by Yoong et al. (33) that found adoption of best-practice healthy eating and physical activity practices did not vary by locality and SES.
Challenges and Future Opportunities for the Program
The second aim of this paper was to discuss the challenges and future opportunities for the program. Munch & Move has high universal reach and program adoption and this may be due to a number of effective key intervention components outlined in the Romp & Chomp intervention evaluation and the WHO implementation plan (10, 31). These components include capacity building of early childhood educators through professional development, training, and resources accompanied by ongoing LHD support leading to organizational change over time; the introduction of the NQF in 2012 which provides a policy imperative for services and parent education materials (31).
A strength of the Munch & Move program is that once an ECEC service is trained they are supported by a health promotion officer from their LHD through visits, local workshops and newsletters for both the service and their families. This allows flexibility in the ongoing support provided to meet the service and community needs. Also, the monitoring guide used to collect the data is based on a modified validated tool (29).
However, there are some limitations of the data. This evaluation of Munch & Move reflects the “real world,” not a research trial and uses routine monitoring data which relies on self-reported data from ECEC services rather than direct observations which may contain reporter bias. Further, the data used for this paper includes a combination of two data sources (CATI and PHIMS) and inherent within this process is the limitation of comparing data from different sources.
Consistent with the WHO implementation plan (10) the NSW government recognizes the importance of obesity prevention and this is evident through the delivery of NSW Government's Premier Priorities Childhood Overweight and Obesity Delivery Plan (34) and the NSW Healthy Eating and Active Living Strategy: Preventing overweight and obesity in New South Wales 2013–2018 (35). The Munch & Move program is one of the key initiatives that focuses on early childhood. In order to achieve the Premier's target, Munch & Move will continue to provide training and support to early childhood educators and their services across NSW including the reengagement of family day care services along with monitoring of program implementation through strengthened practices for center-based ECEC services.
In conclusion, the Munch & Move has seen large improvements in the delivery of training, practice achievements and program adoption in ECEC services across NSW including services in disadvantaged and remote communities and that have a higher proportion of Aboriginal children. These improvements create important opportunities to improve children's health and well-being, and should contribute to the prevention of childhood overweight and obesity. Future research could consider assessing the direct impact of programs such as Munch & Move on individual child health and well-being outcomes.
Ethics Statement
The consent procedures were approved by the University of Sydney Ethics Project Number 2018/205.
Author Contributions
AG and CI-H designed the monitoring framework of Munch & Move. AG and SM prepared the draft manuscript. SM, BO'H, and BM performed the data analysis. All authors provided feedback on drafts and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank all NSW Ministry of Health State Program Managers and Project Officers—Peta Lucas, Rhonda Matthews, Kym Buffet, Lara Hernandez and Anthea Leslie, the 15 Local Health District Health Promotion Teams, the early childhood education and care services involved in the Munch & Move program, the Early Childhood Training and Research Centre, and the PHIMS team.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00034/full#supplementary-material
Abbreviations
SES, socioeconomic status; NSW, New South Wales; ECEC, early childhood education and care; LHD, Local Health District; NQF, National Quality Framework; CATI, Computer Assisted Telephone Interview; PHIMS, Population Health Information Management System.
References
1. Australian Bureau of Statistics. National Health Survey: First Results, 2014–15 (ABS 4364.0.55.001). Canberra, ACT: Australian Bureau of Statistics (2015) [updated 2018 Aug 27]. Available online at: www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.001 (accessed September 19, 2018)
2. Hardy LL, Mihrshahi S, Drayton BA, Bauman A. NSW Schools Physical Activity and Nutrition Survey (SPANS) 2015: Full Report. North Sydney, NSW: NSW Department of Health (2016).
3. Australian Institute of Health and Welfare. A Picture of Overweight and Obesity in Australia 2017. Canberra, ACT: AIHW (2017).
4. Tonge KL, Jones RA, Hagenbuchner M, Nguyen TV, Okely AD. Educator engagement and interaction and children's physical activity in early childhood education and care settings: an observational study protocol. BMJ Open. (2017) 7:e014423. doi: 10.1136/bmjopen-2016-014423
5. Wen LM, Baur LA, Simpson JM, Rissel C, Wardle K, Flood VM. Effectiveness of home based early intervention on children's BMI at age 2: randomised controlled trial. BMJ. (2012) 344:e3732. doi: 10.1136/bmj.e3732
6. Australian Bureau of Statistics. Childhood Education and Care, Australia, June 2014 (ABS 44020DO006_201406). Canberra ACT: Australian Bureau of Statistics; 2014 [updated 2018 Aug 27; cited 2018 Feb 7]. Available online at: www.abs.gov.au/ausstats/abs@.nsf/mf/4402.0
7. Commonwealth Department of Health and Ageing. Get Up & Grow: Healthy Eating and Physical Activity for Early Childhood. Canberra, ACT: Commonwealth of Australia (2013).
8. Committee on Obesity Prevention Policies for Young Children. Early Childhood Obesity Prevention Policies. In: Birch LL, Parker L, Burns A, editors. Washington, DC: Institute of Medicine (2011).
9. World Health Organization. Report of the Commission on Ending Childhood Obesity. Geneva: World Health Organization (2016).
10. World Health Organization. Report of the Commission on Ending Childhood Obesity. Implementation Plan: Executive Summary. Geneva: World Health Organization (2017).
11. Van Stan S, Lessard L, Dupont Phillips K. The impact of a statewide training to increase child care providers' knowledge of nutrition and physical activity rules in Delaware. Child Obes. (2013) 9:43–50. doi: 10.1089/chi.2012.0057
12. Alkon A, Crowley AA, Neelon SE, Hill S, Pan Y, Nguyen V, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children's body mass index. BMC Public Health. (2014) 14:215. doi: 10.1186/1471-2458-14-215
13. Zask A, Adams JK, Brooks LO, Hughes DF. Tooty Fruity Vegie: an obesity prevention intervention evaluation in Australian preschools. Health Promot J Austr. (2012) 23:10–5. doi: 10.1071/HE12010
14. Hardy LL, King L, Kelly B, Farrell L, Howlett S. Munch and Move: evaluation of a preschool healthy eating and movement skill program. Int J Behav Nutr Phys Act. (2010) 7:80. doi: 10.1186/1479-5868-7-80
15. de Silva-Sanigorski A, Elea D, Bell C, Kremer P, Carpenter L, Nichols M, et al. Obesity prevention in the family day care setting: impact of the Romp & Chomp intervention on opportunities for children's physical activity and healthy eating. Child Care Health Dev. (2011) 37:385–93. doi: 10.1111/j.1365-2214.2010.01205.x
16. Bell LK, Hendrie GA, Hartley J, Golley RK. Impact of a nutrition award scheme on the food and nutrient intakes of 2- to 4-year-olds attending long day care. Public Health Nutr. (2015) 18:2634–42. doi: 10.1017/S1368980014003127
17. Farrell L, King L, Hardy L, Howlett S. Munch and Move in Preschools - Summary Report on Implementation and Evaluation Phase 1 (2008 – 2009). Sydney, NSW: Prevention Research Collaboration, University of Sydney (2009).
18. Lockeridge A, Innes-Hughes C, O'Hara BJ, McGill B, Rissel C. Munch & Move: Evidence and Evaluation Summary. North Sydney, NSW: NSW Ministry of Health (2015).
19. NSW Health Department. Health Promotion With Schools: A Policy for the Health system. North Sydney, NSW: NSW Health Department (2000).
20. Australian Children's Education & Care Quality Authority. Guide to the National Quality Standard (2011). Available online at: www.acecqa.gov.au (accessed November 1, 2011).
21. NSW Ministry of Health. NSW Healthy Kids - About Munch & Move Sydney. North Sydney, NSW: NSW Ministry of Health; 2018 [updated 2018 Aug 27]. Available online at: www.healthykids.nsw.gov.au/campaigns-programs/about-munch-move.aspx (accessed September 26, 2018)
22. Australian Children's Education & Care Quality Authority. NQF Snapshot Q3 2017: A Quarterly Report From the Australian Children's Education and Care Quality Authority. Sydney, NSW: ACECQA (2017).
23. Department of Education Employment and Workplace Relations. Child Care Update, June Quarter 2012. Commonwealth of Australia (2012).
24. Australian Children's Education & Care Quality Authority. National Quality Standard Data [Internet]. Canberra, ACT: ACECQA (2018). Available online at: www.acecqa.gov.au/nqf/snapshots (accessed March 7, 2018).
25. Australian Bureau of Statistics. Australian Demographic Statistics (ABS 31010DO002_201706). Canberra, ACT: Australian Bureau of Statistics (2017) [updated 2018 Sep 9]. Available online at: www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 (accessed February 7, 2018).
26. Farrell L, Lloyd B, Matthews R, Bravo A, Wiggers J, Rissel C. Applying a performance monitoring framework to increase reach and adoption of children's healthy eating and physical activity programs. Public Health Res Pract. (2014) 25:e2511408. doi: 10.17061/phrp2511408
27. Australian Bureau of Statistics. Information paper: An Introduction to Socio-Economic Indexes for Areas (SEIFA). Canberra, ACT: Australian Bureau of Statistics (2006) [updated 2008 Mar 26]. Available online at: www.abs.gov.au/ausstats/abs@.nsf/mf/2039.0 (accessed February 7, 2018)
28. Australian Institute of Health and Welfare. Rural, Regional and Remote Health: A Guide to Remoteness Classifications. Canberra, ACT: AIHW (2004).
29. Dodds P, Wyse R, Jones J, Wolfenden L, Lecathelinais C, Williams A, et al. Validity of a measure to assess healthy eating and physical activity policies and practices in Australian childcare services. BMC Public Health. (2014) 14:572. doi: 10.1186/1471-2458-14-572
30. Green A, Innes-Hughes C, Rissel C, Mitchell J, Milat A, Williams M, et al. Codesign of the Population Health Information Management System to measure reach and practice change of childhood obesity programs. Public Health Res Pract. (2018) 28:2831822. doi: 10.17061/phrp2831822
31. de Silva-Sanigorski AM, Bell AC, Kremer P, Park J, Demajo L, Smith M, et al. Process and impact evaluation of the Romp & Chomp obesity prevention intervention in early childhood settings: lessons learned from implementation in preschools and long day care settings. Child Obes. (2012) 8:205–15. doi: 10.1089/chi.2011.0118
32. Ward DS, Welker E, Choate A, Henderson KE, Lott M, Tovar A, et al. Strength of obesity prevention interventions in early care and education settings: a systematic review. Prev Med. (2017) 95(Suppl):S37–52. doi: 10.1016/j.ypmed.2016.09.033
33. Yoong SL, Finch M, Nathan N, Wiggers J, Lecathelinais C, Jones J, et al. A longitudinal study assessing childcare services' adoption of obesity prevention policies and practices. J Paediatr Child Health. (2016) 52:765–70. doi: 10.1111/jpc.13252
34. NSW Ministry of Health. Premier's Priority: Reduce Overweight and Obesity Rates of Children by 5% Over 10 Years. North Sydney, NSW: NSW Ministry of Health (2016)
Keywords: childhood obesity, early childhood, health promotion, healthy eating, physical activity
Citation: Green AM, Mihrshahi S, Innes-Hughes C, O'Hara BJ, McGill B and Rissel C (2020) Implementation of an Early Childhood Healthy Eating and Physical Activity Program in New South Wales, Australia: Munch & Move. Front. Public Health 8:34. doi: 10.3389/fpubh.2020.00034
Received: 26 March 2018; Accepted: 03 February 2020;
Published: 21 February 2020.
Edited by:
Alison Fildes, University of Leeds, United KingdomReviewed by:
Scott B. Teasdale, University of New South Wales, AustraliaCihad Dundar, Ondokuz Mayis University, Turkey
Copyright © 2020 Green, Mihrshahi, Innes-Hughes, O'Hara, McGill and Rissel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amanda M. Green, YW1hbmRhLmdyZWVuQGhlYWx0aC5uc3cuZ292LmF1
 Amanda M. Green
Amanda M. Green Seema Mihrshahi
Seema Mihrshahi Christine Innes-Hughes1
Christine Innes-Hughes1 Blythe J. O'Hara
Blythe J. O'Hara Bronwyn McGill
Bronwyn McGill