- 1Department of Biostatistics, State Key Laboratory of Organ Failure Research, Ministry of Education, and Guangdong Provincial Key Laboratory of Tropical Disease Research, School of Public Health, Southern Medical University, Guangzhou, China
- 2Dermatology Hospital, Southern Medical University, Guangzhou, China
- 3Kirby Institute, New South Wales University, Sydney, NSW, Australia
- 4International Department of Nanjing No.13 Middle School, Nanjing, China
- 5University of North Carolina Project-China, Guangzhou, China
- 6Guangdong-Hong Kong-Macao Joint Laboratory for Contaminants Exposure and Health, Guangzhou, China
Background: HIV-positive men who have sex with men (MSM) tend to have high syphilis incidence. Our objective is to evaluate the prevalence of syphilis and determine the risk factors of syphilis among HIV-positive MSM.
Methods: A cross-sectional study with convenience sampling was performed among HIV-positive MSM in six cities of Guangdong Province from June 2020 to August 2021. Participants completed a survey including social-demographic characteristics, sexual behaviors and self-reported syphilis, chlamydia, gonorrhea, herpes, human papillomavirus statuses after HIV diagnosis. Multivariate logistic regression was used to determine the factors associated with syphilis and sexually transmitted diseases (STD).
Results: Among 944 HIV-positive MSM, 141 (14.9, 95% CI: 12.7–17.2%) men had syphilis and 220 (23.3, 95% CI: 20.6–26.0%) men had STD. Multivariate analysis indicated that MSM who met male sexual partners mainly through traditional meeting places (spa or bath house, sauna, foot or body massage parlor) in the last 6 months [adjusted Odds Ratio (aOR) = 2.91, 95% CI: 1.09–7.79], and who were diagnosed with herps after the HIV diagnosis (aOR = 3.79, 95% CI: 1.16–12.39) were more likely to have syphilis. In addition, MSM who met male sexual partners mainly through traditional meeting places in the last 6 month (aOR = 2.55, 95% CI: 1.01–6.42), and who had more than one male sexual partner in the last 6 months (aOR = 1.88, 95% CI: 1.17–3.02) were more likely to have STD.
Conclusions: The prevalence of syphilis and other STDs is relatively high among HIV-positive MSM in southern China. Routine syphilis screening as a part of HIV monitoring among HIV-positive MSM will have important epidemiological significance for the management of infected patients, and can help reduce the spread of syphilis.
Introduction
Human immunodeficiency virus (HIV) infection among men who have sex with men (MSM) was a significant public health challenge worldwide (1). HIV continued to disproportionately affect MSM living in China, despite the introduction of highly active antiretroviral therapies (2). By the end of 2019, there had been 962,809 people living with HIV (PLWH) in China, and male-to-male sexual contact had become one of the main routes of HIV transmission (23.3%) (3). In addition to HIV, MSM, including HIV-positive ones, were disproportionally affected by sexually transmitted diseases (STD), especially syphilis (4).
Previous studies have shown that the prevalence of syphilis has risen among HIV-positive MSM (2, 5, 6). Syphilis and HIV co-infection can pose considerable health burdens to HIV-positive MSM because syphilis can elevate HIV viral load and decreases CD4 count in HIV-positive patients, thus increasing the risk of HIV-transmission to their serodiscordant partners (7). The increasing number of syphilis cases highlights the importance of syphilis control in HIV-positive MSM, not just for the health of the HIV patient, but also for the prevention of further transmission of HIV and syphilis among uninfected MSM (8). Early detection and treatment of syphilis and other curable STD had become a major component of comprehensive HIV care programs (9). The US Centers for Disease Control (CDC) and Prevention recommends at least annual screening for syphilis for HIV-positive MSM (10). However, most regions in China did not provide syphilis screening services for HIV-positive people, and the testing rate of syphilis was only 37.1% in China (11). Therefore, there is an urgent need to improve routine syphilis screening in HIV-positive MSM in China, which is essential in understanding the driving force of syphilis among HIV-positive MSM.
There is an unique environment to conduct this study in Guangdong Province of China. First, as one of the most developed provinces in China, Guangdong province is one of the few provinces in China that provides regular syphilis screening for HIV-positive MSM. Also, Guangdong has the largest number of HIV-positive MSM in China (12). Second, Guangdong Province has an increasingly rapid prevalence of syphilis where the prevalence of syphilis is 24.7% among MSM (13). However, few studies have been conducted to determine the prevalence and risk factors of syphilis among HIV-positive MSM in Guangdong, previous studies only focused on one city or with small simple sizes. This study aims to evaluate the prevalence of syphilis and determine the risk factors of syphilis among HIV-positive MSM in Guangdong Province.
Methods
Study design and participants
This cross-sectional study was conducted from June 2020 to August 2021 using both online and offline surveys. The online survey was carried out through WenJuanXing (Changsha Ranxing Information Technology, China), an electronic survey platform that was widely used and provided anonymous surveys in China. The offline survey was performed at HIV treatment clinics. The online and offline surveys were both conducted in six cities (Guangzhou, Shenzhen, Zhuhai, Dongguan, Foshan, and Zhongshan) in Guangdong Province. Guangdong Province has been consistently ranked first in the nation for syphilis and other STDs incidence estimation over the last decade. These cities were chosen based on the high prevalence of STD and local sexually transmitted infection (STI)/HIV prevention capabilities.
All potential participants were screened for eligibility after signing an electronic informed consent. Chinese men were eligible to participate if they were (1) born as male, (2) aged over 18 years old, (3) ever engaged in anal or oral sex with a man, (4) newly diagnosed as HIV positive in the last 2 years (since May 2018) and (5) ever tested for syphilis after being diagnosed with HIV. Those participants who did not sign informed consent will be excluded.
Sample size
The primary outcome of our study was the prevalence of syphilis among HIV-positive MSM who had been tested for syphilis. A previous study reported that the prevalence of syphilis was 11.3% in China (2). We applied the two-sided confidence interval (CI) for One Proportion method to estimate a sample size of 655 for this study to produce a two-sided 95% CI and a width of 0.050. Therefore, at least 655 MSM need to be finally included in this study.
Data collection
Electronic questionnaires were used for data collection in this study. The questionnaire items in this study were created based on discussions with HIV and STI experts, HIV-positive MSM, and policy makers in China. We also piloted the survey with 20 volunteer HIV-positive MSM to test questionnaire items. The pilot data were not included in the final analysis.
The questionnaire data were collected using both online and offline surveys in this study. For the online survey, it was conducted by trained staffs from the CDC in each city. The staffs sent the survey link to potential participants through mobile phone text messages or WeChat (the most popular messaging app in China). The offline surveys were conducted by trained doctors at designated HIV treatment clinics in each city. Each potential participant was voluntarily subjected to an electronic questionnaire survey. All questionnaires were filled out by HIV-positive MSM themselves. The offline survey was also performed through the same questionnaire link as the online survey, which can avoid duplication of data. To minimize the risk of duplicate participation from the same person, we allowed each survey link to be accessed only once by a single IP address, phone number and WeChat account.
Measurements
Sociodemographic and behavioral variables
The collected information for social-demographic characteristics included gender, age, legal marital status, highest educational attainment, annual income (US dollar), and sexual orientation. Sexual behaviors included the number of male sexual partners and whether used condom frequently with male sex partners in the last 6 months. The main location to meet with the male sexual partners in the last 6 months was also recorded.
STD variables
STD variables included syphilis, chlamydia, gonorrhea, herpes, and human papillomavirus (HPV) statuses after HIV diagnosis. STD in this study was defined as the diagnosis of any of the following diseases in the past 2 years, syphilis, chlamydia, gonorrhea, herpes and HPV infection. These data were collected based on self-report.
Other variables
We also collected other variables including whether have had underlying diseases (diabetes, hypertension, tumor, pulmonary diseases, cardiac diseases, and kidney diseases) caused by HIV infection and the influence of Corona Virus Disease 2019 (COVID-19) on the HIV treatment.
Statistical analysis
Descriptive analysis was conducted to describe the demographic characteristics, sexual behaviors and STD. A series of univariate and multivariate logistic regressions were conducted to explore the factors associated with syphilis and STD, respectively. In the multivariate model, we adjusted for age, legal marital status, highest educational attainment, annual income and sexual orientation. These adjusted variables were chosen according to our previous experience. All analyses were conducted on SAS (Version 9.4, SAS Institute Inc., Cary, NC).
Results
Study participants characteristics
Overall, a total of 944 participants were recruited in this study. About half of the participants were between 26 and 35 years old (44.1%, 416/944) and had a College/Bachelor's or above degree (54.6%, 515/944). The majority of participants were never married (81.9%, 773/944) and gay, bisexual, and other MSM (GBMSM) (94.1%, 888/944). Around one-third of participants had an annual income between US dollar 5,001 and US dollar 10,000 (37.1%, 350/944) (Table 1).
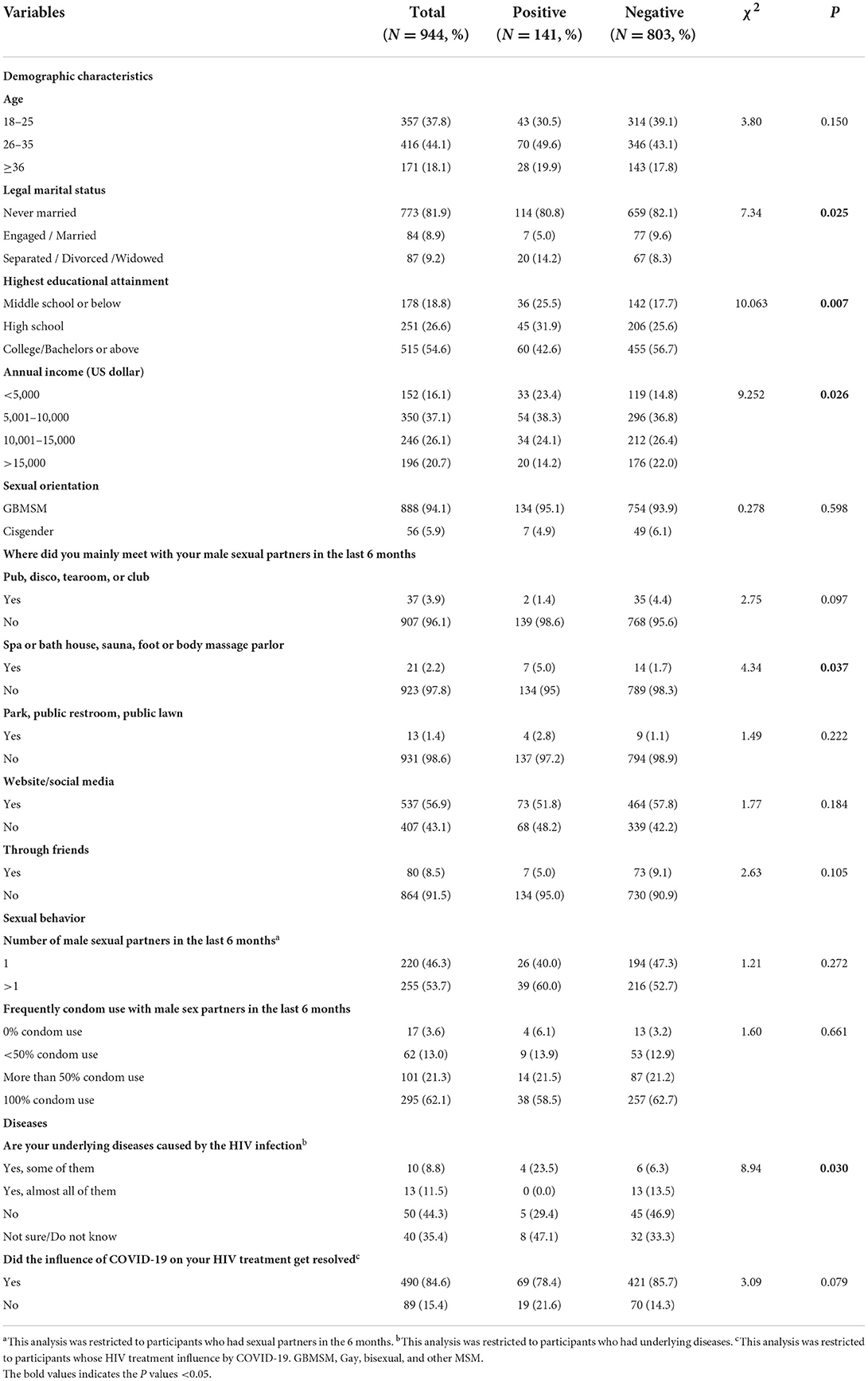
Table 1. Social-demographic and sexual behavioral characteristics among HIV-positive MSM in Guangdong Province from June 2020 to August 2021 (N = 944).
Sexual behaviors
About half of the participants had more than one sexual partner among 475 participants who had sexual partners in the last 6 months (53.7%, 255/475). The majority of the participants always used condom with male sex partners in the last 6 months (62.1%, 295/475). More than half of the participants sought sexual partners through website or social media (56.9%, 537/944) in the last 6 months (Table 1).
Prevalence of STD
In this study, we found that 14.9% of the participants were ever diagnosed with syphilis, 8.5% ever diagnosed with HPV, 1.4% ever diagnosed with herpes, 0.9% ever diagnosed with gonorrhea, 0.2% ever diagnosed with chlamydia and 23.3% ever diagnosed with STD in the past 2 years. In addition, 1.8% of the participants were ever diagnosed with two STDs and only three participants had more than two STDs in the last 2 years (Table 2).
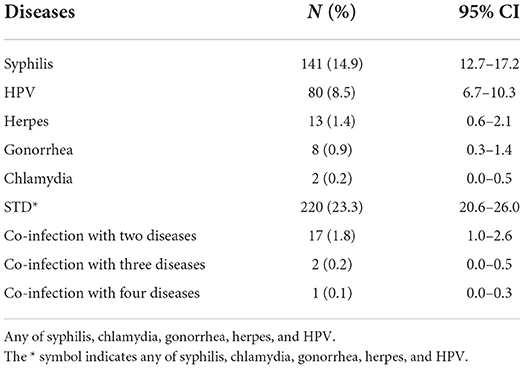
Table 2. Prevalence of STD among HIV-positive MSM in Guangdong Province from June 2020 to August 2021 (N = 944).
Factors associated with syphilis
After adjusted for age, marital status, education, annual income and sexual orientation, the multivariate logistic regression analysis indicated that the participants who met male sexual partners mainly through spa or bath house, sauna, foot or body massage parlor in the last 6 months [adjusted Odds Ratio (aOR) = 2.91, 95% CI: 1.09–7.79], who were diagnosed with herps after HIV diagnosis (aOR = 3.79, 95% CI: 1.16–12.39), and whose influence of COVID-19 on the HIV treatment was resolved (aOR = 1.91, 95% CI: 1.04–3.49) were more likely to be diagnosed with syphilis. The participants who had not underlying diseases caused by the HIV infection (aOR = 0.11, 95% CI: 0.01–0.92) were less likely to have syphilis (Table 3).
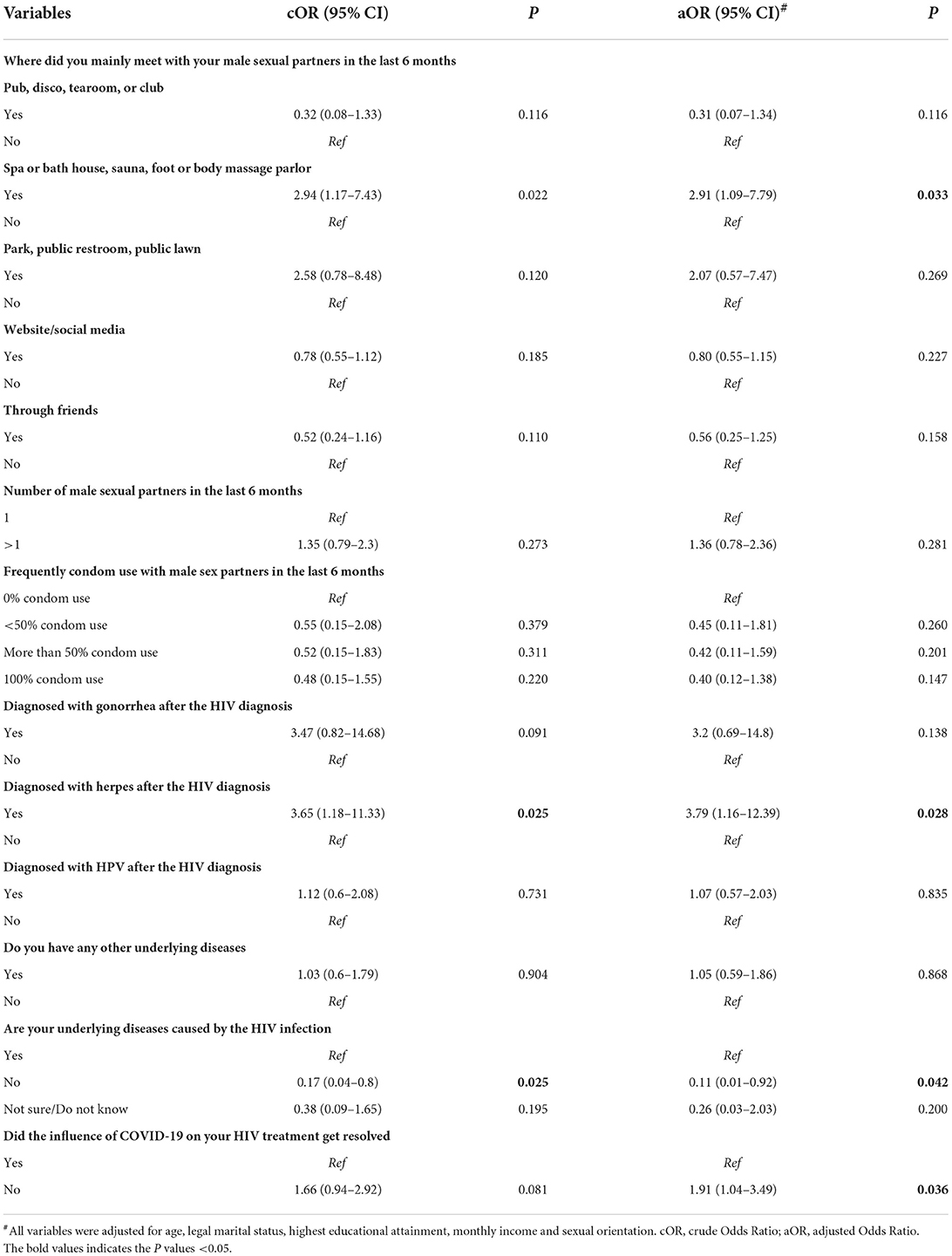
Table 3. Factors associated with syphilis among HIV-positive MSM in Guangdong Province from June 2020 to August 2021 (N = 944).
Factors associated with STD
After adjusted for age, marital status, education, annual income and sexual orientation, the multivariate logistic regression analysis indicated that the participants who met male sexual partners mainly through spa or bath house, sauna, foot or body massage parlor in the last 6 months (aOR = 2.55, 95% CI: 1.01–6.42), mainly through park, public restroom, public lawn in the last 6 months (aOR = 3.87, 95% CI: 1.19–12.57), and had more than one male sexual partner in the last 6 months (aOR = 1.88, 95% CI: 1.17–3.02) were more likely to have STD. The participants who had no underlying diseases caused by the HIV infection (aOR = 0.17, 95% CI: 0.03–0.90) were less likely to have STD (Table 4).
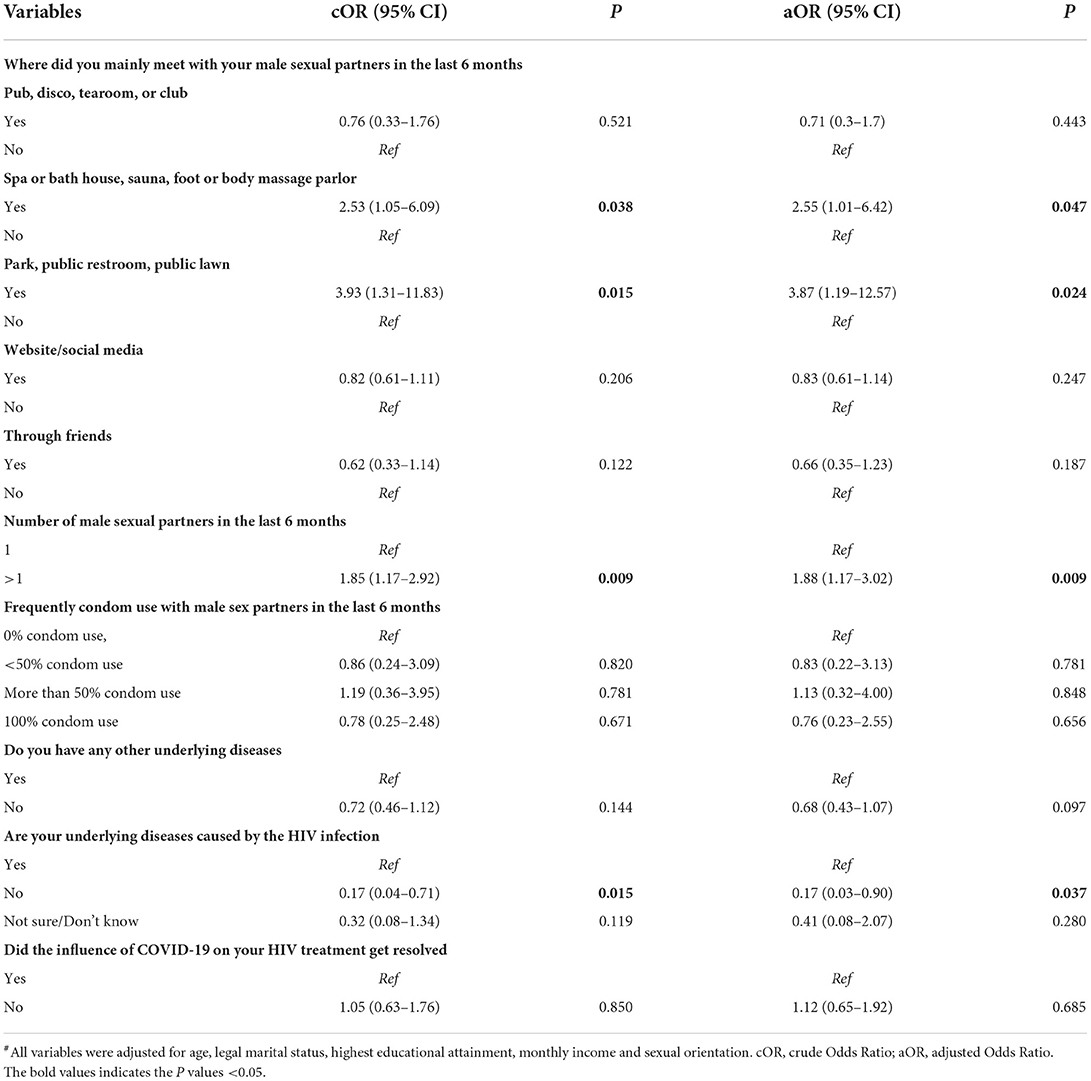
Table 4. Factors associated with STD among HIV-positive MSM in Guangdong Province from June 2020 to August 2021 (N = 944).
Discussion
Syphilis is a growing public health concern and the prevalence of syphilis is increasing among HIV-positive MSM in all countries over the world (14). This study expands the literature by focusing on a large number of HIV-positive MSM in China, exploring the prevalence and factors of syphilis, and describing the prevalence of other STDs. Our study suggests that the prevalence of syphilis and other STDs was relatively high, and seeking male sexual partners through traditional meeting places and reported a higher number of sexual partners were positively associated with syphilis and STD diagnoses among HIV-positive MSM in China.
We found that about one-seventh of HIV-positive MSM in Guangdong province had syphilis in the last 2 years. This prevalence of syphilis is higher than that reported in a previous study among HIV-positive MSM in China (2, 5), but lower than that previously reported in Turkey (4). There are several reasons for the high syphilis prevalence among HIV-positive MSM in our study. First, only 62.1% of participants used condoms consistently in this study, and the high prevalence was attributed to unprotected anal intercourse. Second, HIV impairs the immune system in ways that make it easier for syphilis to take hold (15). Third, poor awareness of syphilis prevention is also an important reason leading to high syphilis incidence among HIV-positive MSM (16). The high syphilis prevalence alongside highly risky sexual behaviors among HIV-positive MSM highlights the importance of syphilis control in China. A previous study has unveiled that frequent testing is a cost-effective way to reduce the potential onward transmission of syphilis (17). Hence, including routine syphilis testing as part of HIV monitoring in HIV-positive MSM can help reduce the duration of infectiousness and incidence of syphilis. Additionally, syphilis self-testing can help improve testing uptake among key populations and self-testing kits are also very easy to obtain online in China (18). It is also very necessary to promote syphilis self-testing among HIV-positive MSM in China.
We also observed that about one-fifth of the HIV-positive MSM have been diagnosed at least one of the listed STDs in the last 2 years in this study. This prevalence of STD is much higher than that reported in a previous study conducted among generally HIV-infected adults in China (19), and the results from a global meta-analysis among PLWH (20). Given the high prevalence of STD and the fact that many STI are asymptomatic infection, our findings highlight the necessity of carrying out regular STD testing among HIV-positive MSM, but the previous study demonstrated that the STD testing rate among HIV-positive MSM still remained low (10). To increase the STD testing, the US CDC launched a guideline to recommend MSM, especially HIV-positive MSM take at least one STD testing annually (21), yet such a guideline is not available in China. Hence, there is an urgent need to introduce national policies to demand MSM patients to be tested STD at least once per year, and to increase the frequency of testing depending on the patient's sexual activities. In addition, it is also necessary to ensure that medical providers can provide regular STD testing follow-up and consulting services for HIV-infected patients.
It was found that MSM who mainly seek male sexual partners through traditional meeting places such as spa or bathhouse, sauna, foot or body massage parlor were more likely to have syphilis. This is consistent with other studies in China (22). The previous study has evidenced that MSM among different venues (i.e., parks, public baths, bars/clubs, or internet) had different high-risk sexual behaviors and HIV/STI risks (23). Participants who seek sexual partners through traditional meeting places have more sexual partners and unprotected sexual behaviors. Comprehensive interventions including condoms and lubrication distribution, health education and providing counselors and special events related to safer-sex skills building need to be taken in traditional meeting places (24). This study also found that men with higher number of sexual partners have a higher risk of STI, which is consistent with other studies (25). Hence, this finding highlights the importance of enhancing sexual health services among HIV-positive MSM, especially those with a high prevalence of STD. In addition, we also found MSM whose influence of COVID-19 on the HIV treatment was resolved were more likely to be diagnosed with syphilis. Travel restrictions during the COVID-19 epidemic in China have impacted on the antiretroviral therapy of HIV-positive MSM (26). The participants whose influence of COVID-19 on the HIV treatment was resolved may have more high-risk behaviors. In order to reduce the negative impact on HIV-positive MSM, more attention should be paid to conducting health behavior education during the COVID-19 epidemic.
This study has several limitations. First, all the data were collected through self-report, the syphilis and other STDs prevalence were not determined by serum testing, which may result in information bias. Second, this study was a cross-sectional study. The cross-sectional nature of the design limits causal inference. Third, since HIV-positive MSM are a hard-to-reach population, we were not able to sample them randomly. However, our study has covered most HIV-positive MSM in Guangdong Province and the sample was representative. Fourth, this study recruited HIV-diagnosed MSM newly in the past 2 years, the results may not be able to generalize to other HIV-positive MSM over 2 years period.
Conclusion
The prevalence of syphilis and other STDs is relatively high among HIV-positive MSM in China. The finding of this study highlights the need to establish a national guideline for STD screening among HIV-positive MSM in China. Routine syphilis screening as part of HIV monitoring in HIV-positive MSM will have important epidemiological significance for the management of infected patients, and can help reduce the duration of infectiousness and incidence of syphilis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethical Committee of Guangzhou Center for Disease Control and Prevention (GZCDC-ER-P2019001). The patients/participants provided their written informed consent to participate in this study.
Author contributions
PZ, JZ, and WT wrote and reviewed the manuscript. WT and XF collected the data. ZY and JC helped analyze data. ZY and YZ helped collect the data and reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Numbers: 82173619 and 81773544), the Science and Technology Planning Project of Guangdong Province (Grant Number: 2020B1212030008), and Medical Scientific Research Foundation of Guangdong Province (Grant Numbers: B2021297 and B2022139).
Acknowledgments
We are very grateful to all the participants who participated in this study. Thanks to the Guangzhou CDC and Prevention for the support of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dong M, Peng B, Liu Z, Ye Q, Liu H, Lu X, et al. The prevalence of HIV among MSM in China: a large-scale systematic analysis. BMC Infect Dis. (2019) 19:1000. doi: 10.1186/s12879-019-4559-1
2. Chen L, Yang J, Ma Q, Pan X. Prevalence of active syphilis infection and risk factors among HIV-positive MSM in Zhejiang, China in 2015: a cross-sectional study. Int J Environ Res Public Health. (2019) 16:1507. doi: 10.3390/ijerph16091507
3. Zhengran C, Yunhui Z, Yalin Z, Jingjing Y, Zhijie S, Yongyi W, et al. Latest AIDS epidemic in global and China. Infect Dis Info. (2020) 33:501–3.
4. Köksal MO, Beka H, Evlice O, Çiftçi S, Keskin F, Başaran S, et al. Syphilis seroprevalence among HIV-infected males in Istanbul, Turkey. Revista Argentina de Microbiología. (2020) 52:266–71. doi: 10.1016/j.ram.2020.01.002
5. He H, Wang M, Zaller N, Wang J, Song D, Qu Y, et al. Prevalence of syphilis infection and associations with sexual risk behaviours among HIV-positive men who have sex with men in Shanghai, China. Int J Std AIDS. (2014) 25:410–9. doi: 10.1177/0956462413512804
6. Zhao YS, Su SL, Lv CX, Zhang XF, Lin L, Sun XG, et al. Seroprevalence of hepatitis C, hepatitis B virus and syphilis in HIV-1 infected patients in Shandong, China. Int J Std AIDS. (2012) (23):639–43. doi: 10.1258/ijsa.2012.011411
7. Polansky A, Levy I, Mor Z. Risk factors of syphilis co-infection among HIV-infected men who have sex with men in Tel-Aviv, Israel. AIDS Care. (2019) 31:1157–61. doi: 10.1080/09540121.2019.1612006
8. Refugio ON, Klausner JD. Syphilis incidence in men who have sex with men with human immunodeficiency virus comorbidity and the importance of integrating sexually transmitted infection prevention into HIV care. Expert Rev Anti Infect Ther. (2018) 16:321–31. doi: 10.1080/14787210.2018.1446828
9. US CDC. HIV Prevention Through Early Detection and Treatment of Other Sexually Transmitted Diseases - United States Recommendations of the Advisory Committee for HIV and STD Prevention. Available online at: https://www.cdc.gov/mmwr/preview/mmwrhtml/00054174.htm (accessed July 31, 1998).
10. Landovitz RJ, Gildner JL, Leibowitz AA. Sexually transmitted infection testing of HIV-positive medicare and medicaid enrollees falls short of guidelines. Sex Transm Dis. (2018) 45:8–13. doi: 10.1097/OLQ.0000000000000695
11. Lee N, Chen Y, Liu H, Li C, Li C, Ko W, et al. Increased repeat syphilis among HIV-infected patients: a nationwide population-based cohort study in Taiwan. Medicine. (2020) 99:e21132. doi: 10.1097/MD.0000000000021132
12. Lin P, Li Y, Tillman J. Guangdong Province: Trade Liberalization and HIV. HIV/AIDS China. (2019). p. 653–74. doi: 10.1007/978-981-13-8518-6_34
13. He WP, Ye XD, Tang SK, Zhuang JT, Liang RJ. The prevalence of HIV and syphilis and related factors among men who have sex with men in Guangzhou. Chin Prev Med. (2015) 16:684–8.
14. Kojima N, Klausner JD. An Update on the Global Epidemiology of Syphilis. Curr Epidemiol Rep. (2018) 5:24–38. doi: 10.1007/s40471-018-0138-z
15. Azbel L, Polonsky M, Wegman M, Shumskaya N, Kurmanalieva A, Asanov A, et al. Intersecting epidemics of HIV, HCV, and syphilis among soon-to-be released prisoners in Kyrgyzstan: implications for prevention and treatment. Int J Drug Policy. (2016) 37:9–20. doi: 10.1016/j.drugpo.2016.06.007
16. Wu X, Hong F, Lan L, Zhang C, Feng T, Yang Y. Poor awareness of syphilis prevention and treatment knowledge among six different populations in south China. BMC Public Health. (2016) 16:287. doi: 10.1186/s12889-016-2966-4
17. Zhao PZ, Wang YJ, Cheng HH, Zhang Y, Tang WM, Yang F, et al. Uptake and correlates of chlamydia and gonorrhea testing among female sex workers in Southern China: a cross-sectional study. BMC Public Health. (2021) 21:1477. doi: 10.1186/s12889-021-11526-w
18. Wang C, Cheng W, Li C, Tang W, Ong JJ, Smith MK, et al. Syphilis self-testing: a nationwide pragmatic study among men who have sex with men in China. Clin Infect Dis. (2020) 70:2178–86. doi: 10.1093/cid/ciz603
19. Wang XB, Tucker JD, Yang L, Zheng H, Zhang F, Cohen MS, et al. Unsafe sex and STI prevalence among HIV-infected adults in Guangzhou, China: opportunities to deamplify sexual HIV transmission. AIDS Behav. (2013) (17):1137–43. doi: 10.1007/s10461-012-0322-y
20. Kalichman SC, Pellowski J, Turner C. Prevalence of sexually transmitted co-infections in people living with HIV/AIDS: systematic review with implications for using HIV treatments for prevention. Sex Transm Infect. (2011) 87:183–90. doi: 10.1136/sti.2010.047514
21. Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. (2015) 64:1–137.
22. Das A, Li J, Zhong F, Ouyang L, Mahapatra T, Tang W, et al. Factors associated with HIV and syphilis co-infection among men who have sex with men in seven Chinese cities. Int J Std AIDS. (2015) 26:145–55. doi: 10.1177/0956462414531560
23. Yun K, Xu J, Leuba S, Zhu Y, Zhang J, Chu Z, et al. Development and validation of a personalized social media platform–based HIV incidence risk assessment tool for men who have sex with men in China. J Med Internet Res. (2019) 21:e13475. doi: 10.2196/13475
24. Binson D, Woods WJ, Pollack L, Paul J, Stall R, Catania JA. Differential HIV risk in bathhouses and public cruising areas. Am J Public Health. (2001) 91:1482–6. doi: 10.2105/AJPH.91.9.1482
25. Barbee LA, Dhanireddy S, Tat SA, Marrazzo JM. Barriers to bacterial sexually transmitted infection testing of HIV-infected men who have sex with men Engaged in HIV primary care. Sex Transm Dis. (2015) 42:590–4. doi: 10.1097/OLQ.0000000000000320
Keywords: men who have sex with men, human immunodeficiency virus, syphilis, sexually transmitted diseases, risk factors
Citation: Zhao P, Yang Z, Zhang Y, Chen J, Fu X, Tang W and Zhou J (2022) Prevalence of syphilis and risk factors among HIV-positive men who have sex with men in Guangdong province. Front. Public Health 10:1025221. doi: 10.3389/fpubh.2022.1025221
Received: 22 August 2022; Accepted: 26 October 2022;
Published: 09 November 2022.
Edited by:
Francisco Antunes, Universidade de Lisboa, PortugalReviewed by:
Weibin Cheng, Guangdong Second Provincial General Hospital, ChinaZhenzhou Luo, Shenzhen Nanshan Center for Chronic Disease Control, China
Copyright © 2022 Zhao, Yang, Zhang, Chen, Fu, Tang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiming Tang, d2VpbWluZ190YW5nQG1lZC51bmMuZWR1; Jiyuan Zhou, emhvdWppeXVhbjU0NjBAaG90bWFpbC5jb20=
 Peizhen Zhao
Peizhen Zhao Ziying Yang
Ziying Yang Ye Zhang
Ye Zhang Jinmei Chen
Jinmei Chen Xuezhen Fu4
Xuezhen Fu4 Weiming Tang
Weiming Tang Jiyuan Zhou
Jiyuan Zhou