- 1School of Pharmacy, Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
- 2School of Medicine and Health Management, Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
- 3Division of Health Services Research, Department of Foundations of Medicine, New York University Long Island School of Medicine, Mineola, NY, United States
- 4School of Statistics and Mathematics, Zhongnan University of Economics and Law, Wuhan, China
- 5JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Shatin, NT, Hong Kong SAR, China
- 6School of Science, Hubei University of Technology, Wuhan, China
Introduction: Self-medication has a high prevalence in the middle-aged and elderly population in China. Despite the published evidence demonstrating the economic benefits of self-medication, limited research has addressed the relationship between self-medication and individual medical expenditures, especially within the Chinese population. This study examined the effect of self-medication on individual medical expenditures in China and analyzed the heterogeneity between outpatient and inpatient cases.
Methods: We conducted a panel data analysis using data from four waves of the China Health and Retirement Longitudinal Study (CHARLS). Two-part mixed-effect models were implemented to estimate the effect of self-medication on total outpatient and inpatient expenses and out-of-pocket (OOP) costs, where mixed-effects logit regression was used as the first part, and generalized linear mixed models with log link and gamma distribution was used as the second part.
Results: We identified 72,041 responses representing 24,641 individuals, of which 13,185 responses incurred outpatient expenses and 9,003 responses incurred inpatient costs. Controlling for all covariates, we found that self-medication behaviors were significantly associated with a higher probability of outpatient service utilization (OR = 1.250, 95% CI = 0.179 to 0.269; P < 0.001), but displayed no significant association with outpatient expenses. Respondents who had taken self-medication were less likely to use inpatient services (OR = 0.865, 95% CI = −0.201 to −0.089; P < 0.001), and their inpatient expenses were significantly reduced by 9.4% (P < 0.001). Inpatient OOP costs were significantly reduced by 10.7% (P < 0.001), and outpatient OOP costs were significantly increased by 11.3% (P < 0.001) among respondents who had self-medicated.
Conclusions: This study allowed us to identify the economic value of self-medication among the middle-aged and elderly population in China. Future work should guide the middle-aged and elderly to take responsible self-medication to reduce their economic burden.
1. Introduction
As a global public health issue, self-medication has become part of the healthcare system. The World Health Organization (WHO) defines it as the “selection and use of [herbal or chemical] medicines by individuals to treat self-recognized illnesses or symptoms” (1). The World Self-Medication Industry (WSMI) emphasizes responsible self-medication, describing it as “the practice whereby individuals treat their ailments and conditions with medicines which are approved and available without prescription, and which are safe and effective when used as directed” (2). Self-medication has positive effects on both personal health and healthcare systems; thus, it has attracted widespread attention in recent years (3, 4). With the improvement of the population's health literacy, self-medication has played an increasingly important role in the medical system.
Self-medication has become a common phenomenon that is widely practiced worldwide. As shown by previous studies, at least 43.8% of respondents self-medicated frequently in the United States (5), the prevalence of self-medication was approximately 25 % among older Europeans (6), and the prevalence rate in Spain was 12.7% (7). In developing countries, the prevalence of self-medication was 26.3% in Chile (8) and 76.3% in Brazil (9). Self-medication has a long history and a solid mass foundation in China (10). During the previous 12 months, 74.6% of respondents practiced self-medication (11). Furthermore, 45.4% of respondents would select self-medication if they felt physical discomfort during the 2 weeks preceding the survey, which was higher than the proportion who chose to “see the doctor” (12). Among the middle-aged and elderly people in China, the prevalence of self-medication during the previous month was 45.52% (13). Such a high prevalence has sparked a strong focus on self-medication among scholars.
Self-medication of middle-aged and elderly people shows particularity who seem to have a higher susceptibility to self-medicate (14). It is well established from a variety of studies that the elderly are the largest consumers of medicines in most countries (15, 16). The existing research recognizes that the elderly are one of the population groups with a higher prevalence of self-medication, resulting from a higher prevalence of diseases (17). On the one hand, age-related changes in pharmacokinetics and pharmacodynamics put the middle-aged and elderly at higher risk of medication than other age groups (18). On the other hand, their choices of medication are prone to be influenced by the surrounding environment. A wide variety of pharmaceutical products on the market, and the extensive publicity surrounding these products, often target the middle-aged and elderly (19). In this context, irresponsible self-medication by middle-aged and elderly people frequently occurs, with harmful consequences. All of these make self-medication by the middle-aged and elderly extremely complicated, which deserves major attention.
It is worth noting that self-medication has potential risks if taken inappropriately. Without proper consultation from healthcare professionals, self-medication increases the risk of drug abuse (20), consumption of inappropriate medication (21), and adverse drug events (22). In the meantime, the high proportion of sales of antibiotics without a prescription in China has been reported in the body of literature (23). Self-medication has exacerbated the abuse of antibiotics, which contributes to the development of antibiotic resistance. Despite its negative effects, the advantages of self-medication, especially the economic benefits, have been widely recognized. With the rapid growth of medical expenses, cost containment has gradually become a consensus in the healthcare system (24, 25). Previous research has shown that self-medication plays an active role in decreasing healthcare costs (26). Self-medication reduces the burden on healthcare services caused by minor and trivial ailments, leaving doctors with more energy to deal with patients in need (27). Self-medication reduces the need for clinic visits, thereby enabling cost reductions, which is the major cause of self-medication among patients (4, 28). Time saving is another factor that motivates patients to self-medicate (29, 30). Patients avoid spending travel time to the hospital and waiting in line for medical services at clinics or physicians' offices. Without a doubt, self-medication brings savings in costs and increased productivity (31). Studies have revealed that 45.5% of respondents performed self-medication to save money and 82% did so to save time (32).
Although many studies have explored the economic value of self-medication and affirmed its role in reducing medical expenditures (33–35), most quantitative studies concentrated on the national level or on certain diseases. Much of the research focused on the individual patient has been, up to now, descriptive in nature, and analyses of data about the savings in costs caused by self-medication from the perspective of patients are limited. This study conducted a panel data analysis using data from the 2011, 2013, 2015, and 2018 waves of the China Health and Retirement Longitudinal Study (CHARLS), and examined the effect of self-medication on individual medical expenditures among the middle-aged and elderly population in China. The heterogeneity between outpatient and inpatient cases was also analyzed. Our study quantified the effect of self-medication on savings in the cost of healthcare and its reduced burden on healthcare services. Our work also filled the gaps in the research on the middle-aged and elderly population in China. In the meantime, the CHARLS provided longitudinal data that delivered more accurate estimates.
2. Materials and methods
2.1. Data source
Our work is a longitudinal study based on data from four waves of the China Health and Retirement Longitudinal Study (CHARLS), namely 2011, 2013, 2015, and 2018. The CHARLS is a national population-based survey that includes assessments of social, economic, and health circumstances of community residents. The CHARLS collects high-quality data through face-to-face interviews with a structured questionnaire. The project, using multistage stratified probability-proportionate-to-size sampling, selected a nationally representative sample of Chinese residents aged 45 years and older. The data were collected from 28 provinces, 150 counties/districts, and 450 villages/urban communities across the country. The total sample size of the CHARLS baseline survey in 2011 was 17,708 individual respondents. Around 70% of the original 2011 sample participated in the follow-up survey throughout the following waves, and the response rate was over 86% (36). Detailed descriptions of the survey design and procedures can be found in in the original study documentation (37).
In this study, we included data from participants who had responded in “Module E: Health Care and Insurance”, and we excluded respondents who had missing values of dependent or independent variables. Respectively, 16,966, 16,946, 19,603, and 18,526 samples were included in Wave 1, 2, 3, and 4. In view of the statistical method used, the final analytical sample was not necessarily a balanced panel. A response from certain individuals might be excluded from our analyses while the rest of the responses from the same individuals might be included (38).
2.2. Study variables
2.2.1. Self-medication
In the CHARLS Waves 1, 2, and 3, the question about self-medication was: “How did you treat yourself during the past month?” The answer options included: (1) Consumed over-the-counter modern medicines; (2) Consumed prescription medicines; (3) Consumed traditional herbs or traditional medicines as treatment; (4) Consumed tonics/health supplements; (5) Used healthcare equipment; (6) Others; and (7) None. If the respondent chose consumed over-the-counter modern medicines, prescription medicines, or traditional herbs or traditional medicines as treatment, he was regarded as taking self-medication (13). In Wave 4, three types of medications were combined. The question about self-medication was: “Did you take any purchased medicine during the past month?” The respondents replied “Yes”, which indicated taking self-medication. These two definitions are consistent with the meaning of self-medication defined by the WHO (1).
2.2.2. Dependent variables
In the CHARLS, medical expenditure was self-reported as the total amount paid during 1 month preceding the survey date for outpatients or 1 year preceding the survey date for inpatients. Participants were asked about their outpatient expenditure via the following question: “How much did all the visits to medical facilities cost during the last month? (Include self-paid part and reimbursement part)”. These medical facilities were reported by participants as places they had visited in the last 4 weeks for outpatient treatment. The self-paid part was asked separately and defined as outpatient out-of-pocket (OOP) costs. Inpatient expenditure was asked via the following question: “What was the medical cost for all the hospitalizations you received during the past year? (Only include fees paid to the hospital, including ward fees but excluding wages paid to a hired nurse, transportation costs, and accommodation costs for yourself or family members).” The self-paid part of inpatient expenditure was defined as inpatient OOP costs.
2.2.3. Independent variables
We used Anderson's behavior model to select independent variables, including predisposing factors, enabling factors, and need factors (39). The classifications of the categorical variables were informed by published evidence. Predisposing factors included age, gender, marital status (40) (married = married with spouse present/cohabitated, and unmarried = married but not living with spouse temporarily for reasons such as work/separated/divorced/widowed/never married), and education status (41) (primary school and below and secondary school and above). Enabling factors included residential area (42) (rural and urban), socioeconomic status quartiles [annual per capita household consumption expenditure (43)], region (east, west, and center), and medical insurance schemes. Need factors consisted of self-rated health (very good, good, fair, poor, and very poor) and number of chronic diseases. Different medical insurance schemes were considered in our study, including Urban employee medical insurance (UEBMI), Urban resident medical insurance (URBMI), New rural cooperative medical insurance (NCMS), and Urban and rural resident medical insurance (URRBMI). Multiple/Other was indicated if the patient was a policyholder or primary beneficiary of more than one type of listed health insurance, or a policyholder or primary beneficiary of any insurance other than UEBMI, URBMI, NCMS, and URRBMI (44). Health behaviors such as smoking (yes and no) and drinking (often, sometimes, and never) were also considered.
2.3. Statistical analysis
Generally, medical expenditure is not normally distributed and shows more zero numbers. The two-part model (TPM) has been widely used for analyzing medical expenditure to address the problem of excess zeroes (45). The first part estimated the likelihood of an individual incurring any expenditure by a logit model. The second part was a generalized linear regression estimating medical expenditure among those with positive expenditure. The TPM with random effects could provide a method for analyzing repeated measurement data. Two-part mixed-effect models have been used to analyze longitudinal count data with excess zeros (46).
2.3.1. Part 1 – Selection equation: Mixed-effects logit regression
Selection equation, the first part of the two-part mixed-effect model, considered a binomial distribution – whether any medical expenditures was incurred (y > 0) or not (y = 0) – and implemented a mixed-effects logit regression to estimate the probability of medical service utilization. There is N number of participants, each of whom had multiple interviewed records. The probability function of medical service utilization was defined as:
Here, i = 1, …, N individuals, with the i individual having j = 1, …, ni interviewed records. The outcome (yij) was a binary response, where yij > 0 if medical expenditure was positive, and yij = 0 if otherwise. The outcome could be influenced by a set of fixed effects xij and random effects ui. βp1 were their associated regression coefficients for the Part 1 model. Considering no random slope, ui was the random intercept for each individual (47). For the logit regression, this function estimated the probability of (yij > 0).
2.3.2. Part 2 – Regression equation: Mixed-effects linear model with log link and gamma distribution
Conditional to any medical expenditure incurred (yij > 0), the intensity of medical expenditure could be fitted with a generalized linear mixed model (GLMM) called “regression equation”. The GLMM, an extension of the generalized linear model and mixed linear model, could process hierarchical data, making it suitable for the CHARLS database. Including random effects in the model addressed the problems of correlations, excessive dispersion, and heterogeneity among the data. The GLMM was also insensitive to missing data, which reduced the bias in the study's outcomes caused by data missing from the CHARLS database. The estimated intensity of medical expenditure was defined as:
Here, i = 1, …, N individuals, with the i individual having j = 1, …, ni interviewed records with positive expenditure. The outcome (yij) represented medical expenditure of each individual. βp2 were the associated regression coefficients for the Part 2 model and xij were set as fixed effects. Without considering any random slopes, Ui indicated the random intercept for each individual (47). The generalized linear mixed model was specified as log link and gamma distribution, which are commonly used in econometric analyses of medical expenditure due to their asymptotic properties for non-negative outcomes (48).
2.4. Statistical software
All statistical calculations were carried out using the R software (version 4.1.2; R Development Core Team, URL http://www.R-project.org, 2021). Generalized linear mixed models were performed using the library “glmmTMB”. The optimizer was considered to adjust the model.
3. Results
3.1. Sample characteristics
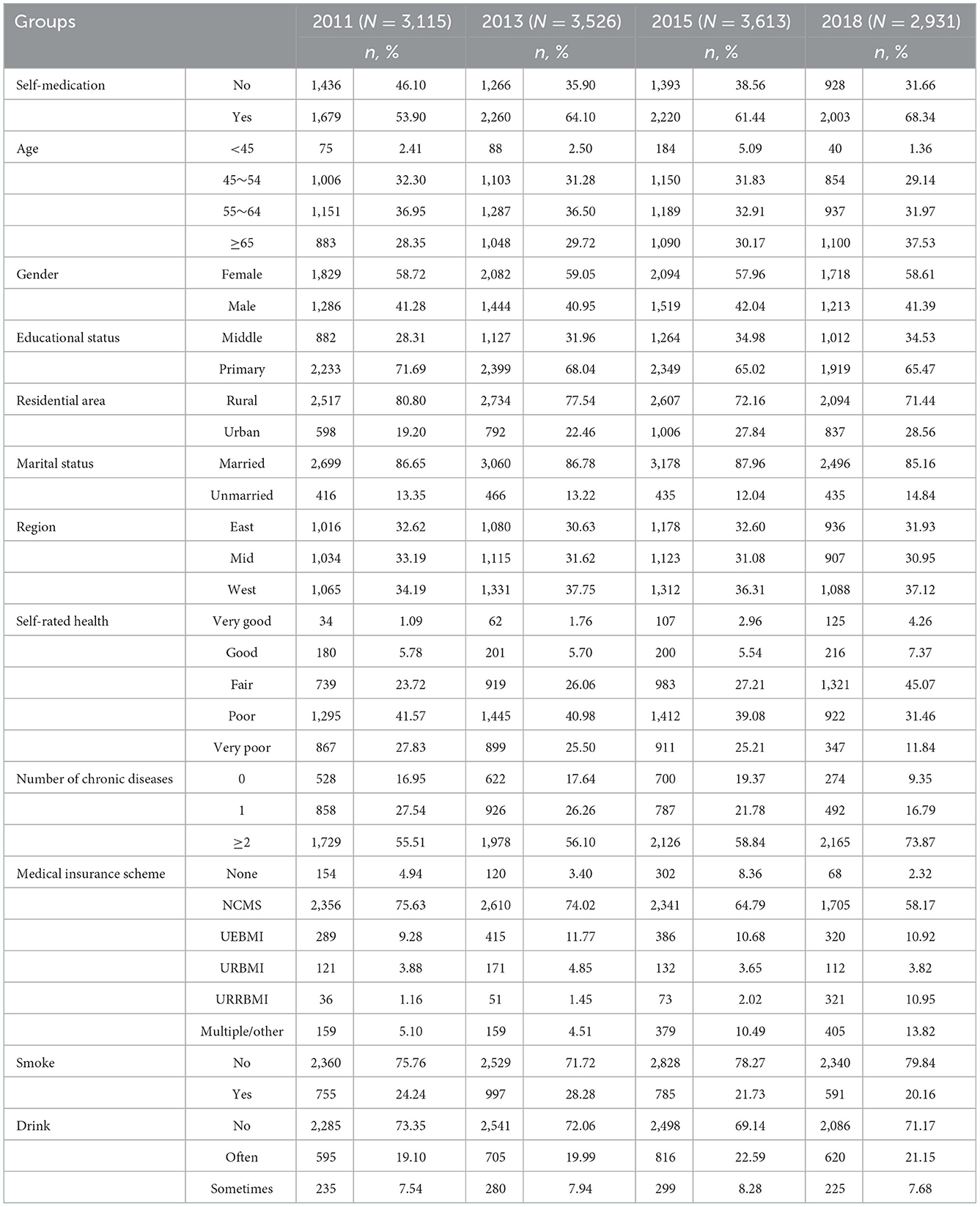
We identified 72,041 responses representing 24,641 individuals in the unbalanced panel data, of which 13,185 responses incurred outpatient expenses and 9,003 responses incurred inpatient costs. A total of 9,338 eligible individuals had incurred outpatient costs 1 month before the interview, and they generated 1–4 responses among the four waves. Table 1 summarizes the demographics of the included outpatients in different years. The individuals were aged 59.73 years on average and consisted of 41.43% men and 58.57% women. Of these, 8,162 (61.90%) respondents had taken self-medication 1 month before the interview. Women (59.00%) had performed more self-medication, same as the respondents that were married (87.18%), had attended primary school or below (66.93%), or were living in rural areas (74.78%).
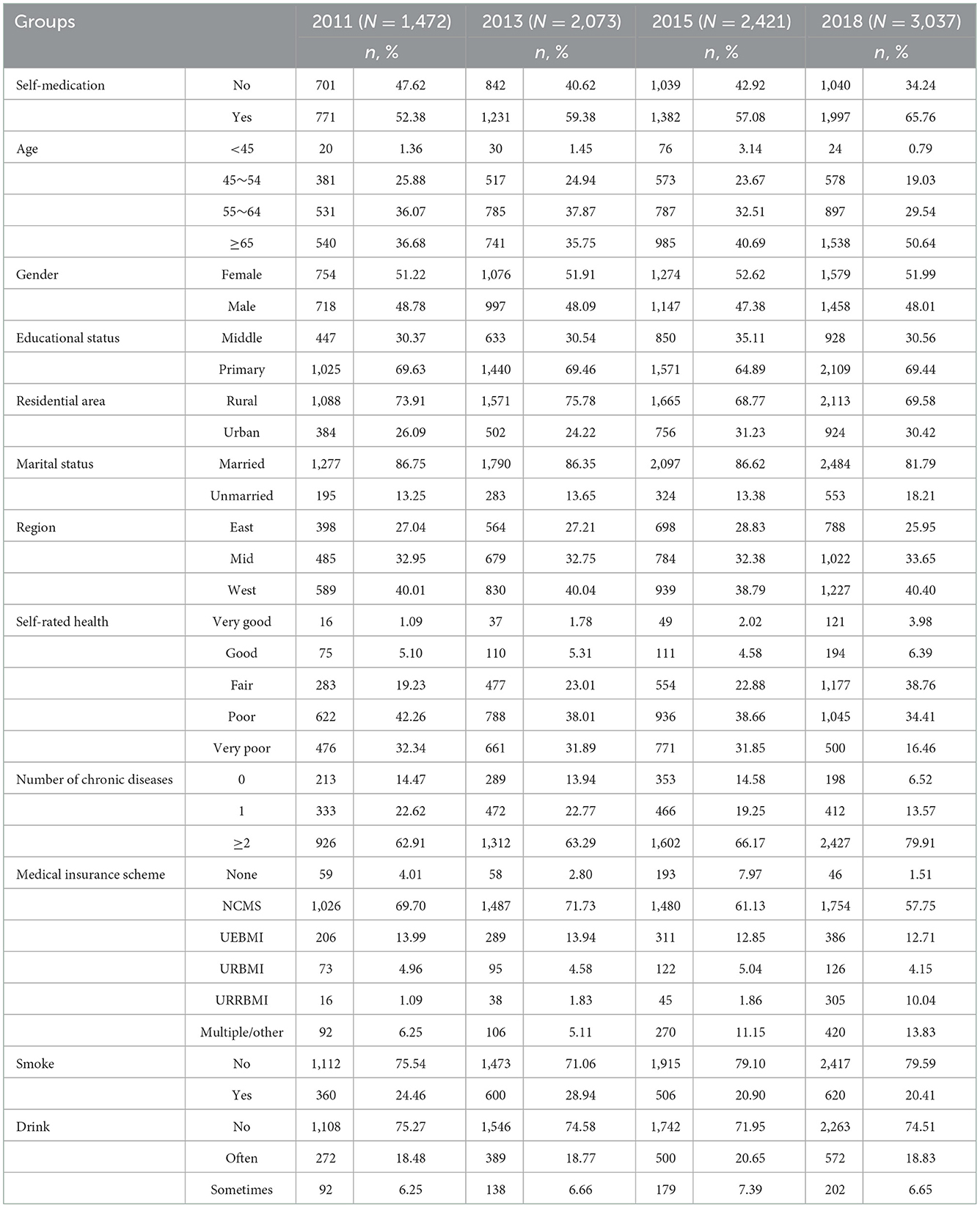
Among the four waves, we identified 9,003 responses representing 6,861 individuals that had incurred inpatient costs 1 year before the interview. Table 2 summarizes the demographics of the included inpatients over the 4 years. The respondents were aged 62.66 years on average and consisted of 47.98% men and 52.02% women. Of these, 5,381 (59.77%) respondents had taken self-medication 1 month before the interview.
3.2. Descriptive statistics
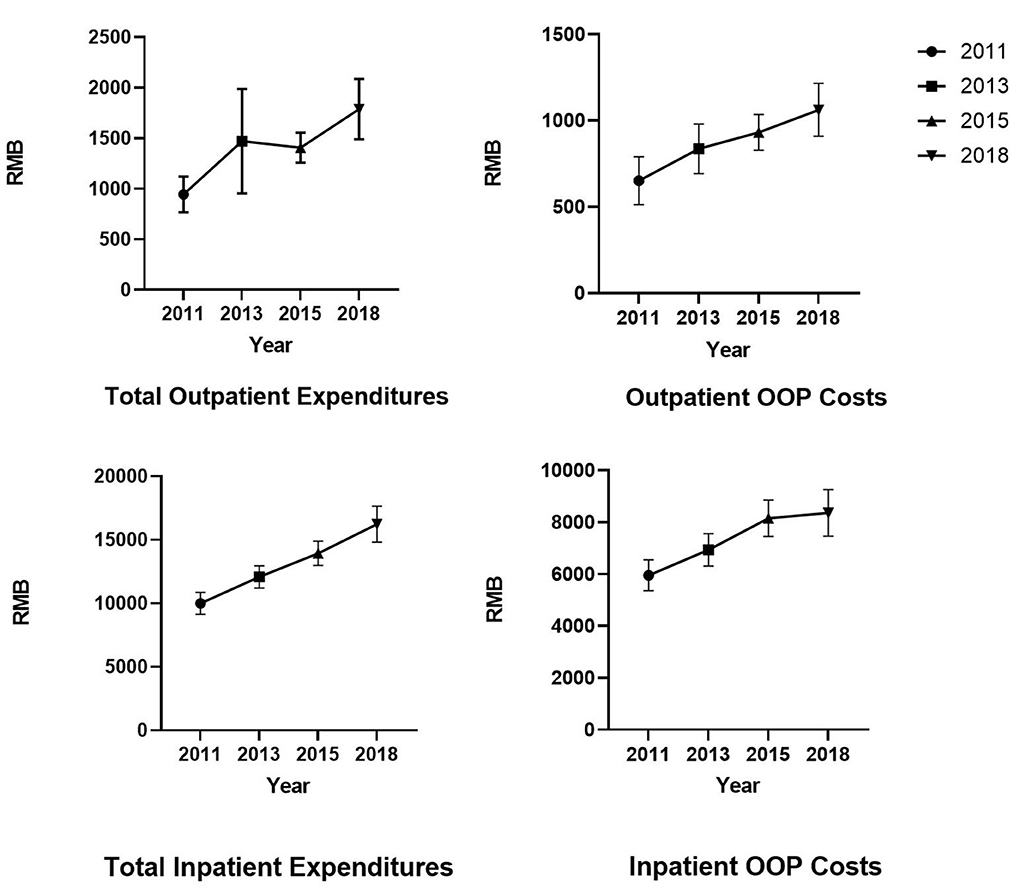
Figure 1 reports the mean of total medical expenditures and out-of-pocket (OOP) expenditure in different groups. Costs were adjusted to 2018 RMB using the consumer price index. The mean of monthly total outpatient costs in 2011, 2013, 2015, and 2018 was ¥944.61, ¥1,471.71, ¥1,407.68, and ¥1,789.23, respectively. The mean of annual total inpatient costs in 2011, 2013, 2015, and 2018 was ¥9,991.01, ¥12,068.57, ¥13,932.96, and ¥16,227.11, respectively. Although we used CPI to eliminate the effect of inflation, medical expenditure showed an increasing trend over the years. Regarding self-medication, patients who self-medicated had lower inpatient expenditures and OOP costs for inpatient care.
3.3. Two-part mixed-effects models
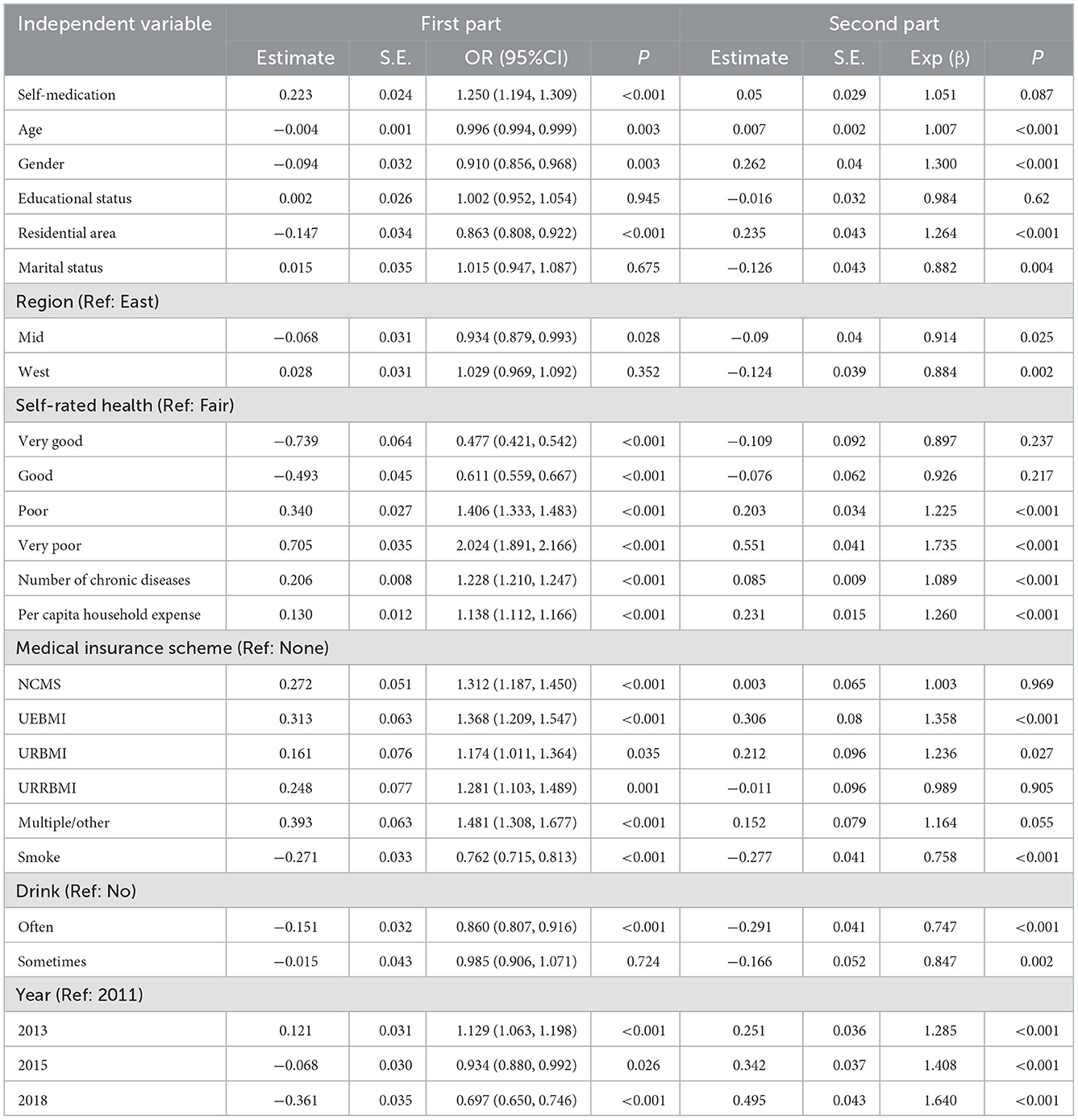
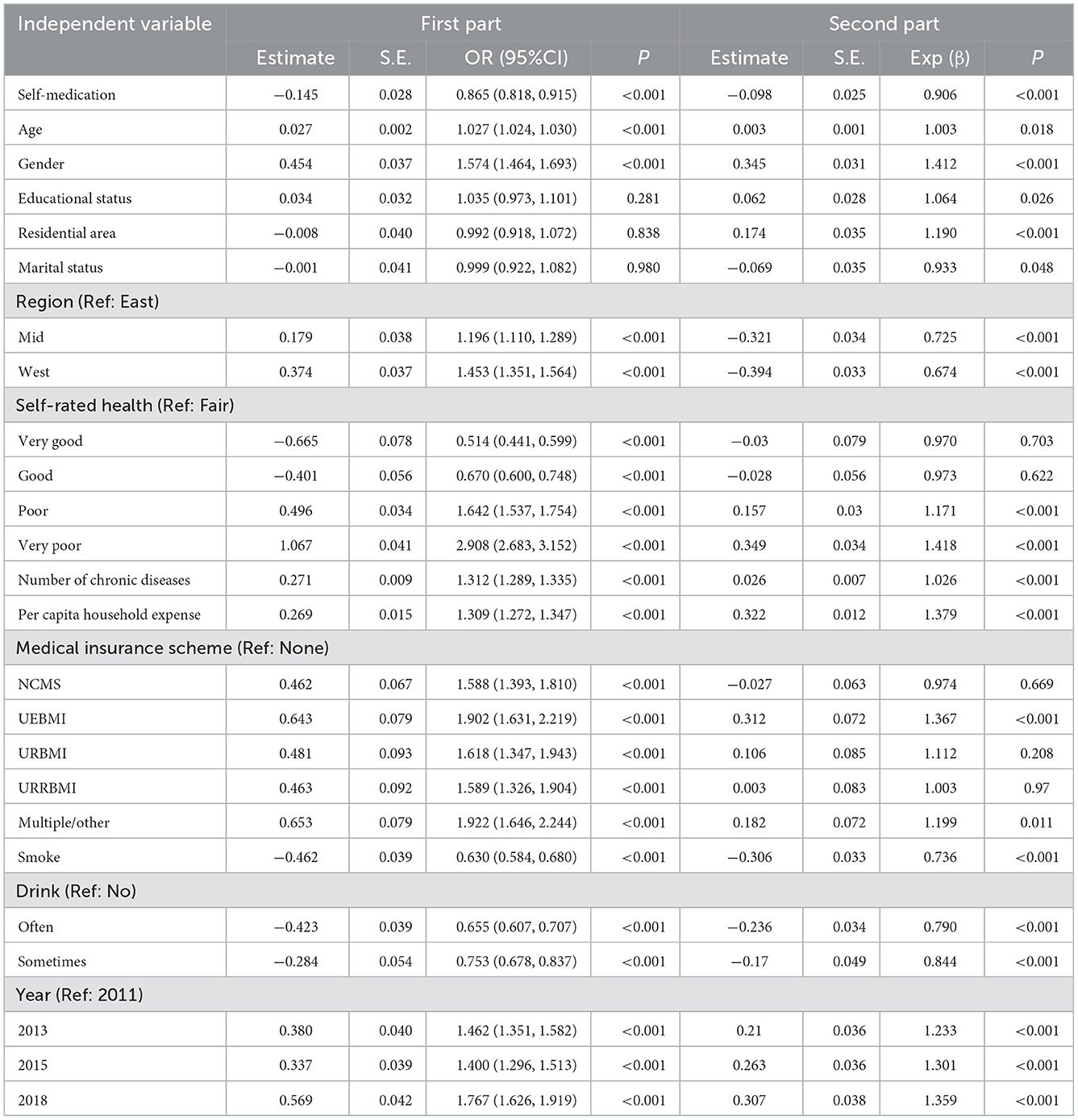
To evaluate the impact of self-medication on medical expenditures, this study applied two-part mixed-effects models. Logit regression was used as the first part and a gamma distribution and log link were performed for the second part. Outpatient expenditures are presented in Table 3 and inpatient expenditures in Table 4.
The estimator showed that self-medication behaviors were significantly associated with a higher probability of outpatient service utilization (OR = 1.250, 95% CI = 0.179 to 0.269; P < 0.001), but displayed no significant association with outpatient expenses (P = 0.087). Respondents who took self-medication were less likely to use inpatient services (OR = 0.865, 95% CI = −0.201 to −0.089; P < 0.001), and their inpatient expenses were significantly reduced by 9.4% (P < 0.001). The second part indicated a significant increase in healthcare expenditures with increasing age (P < 0.001; P = 0.018). Women had lower total medical expenditures compared with men (P < 0.001). Respondents living in non-rural areas were significantly associated with lower medical costs (P < 0.001), same as those living in central and western regions (P < 0.001, P < 0.001; P = 0.025, P = 0.002). Respondents who self-reported with “poor” and “very poor” health levels were found to have significantly higher medical expenditures (P < 0.001). With the increase in the number of chronic diseases, a significant increase in medical expense was also observed (P < 0.001). Regarding socioeconomic status, respondents with higher per capita household expenditure were significantly associated with higher medical costs (P < 0.001).
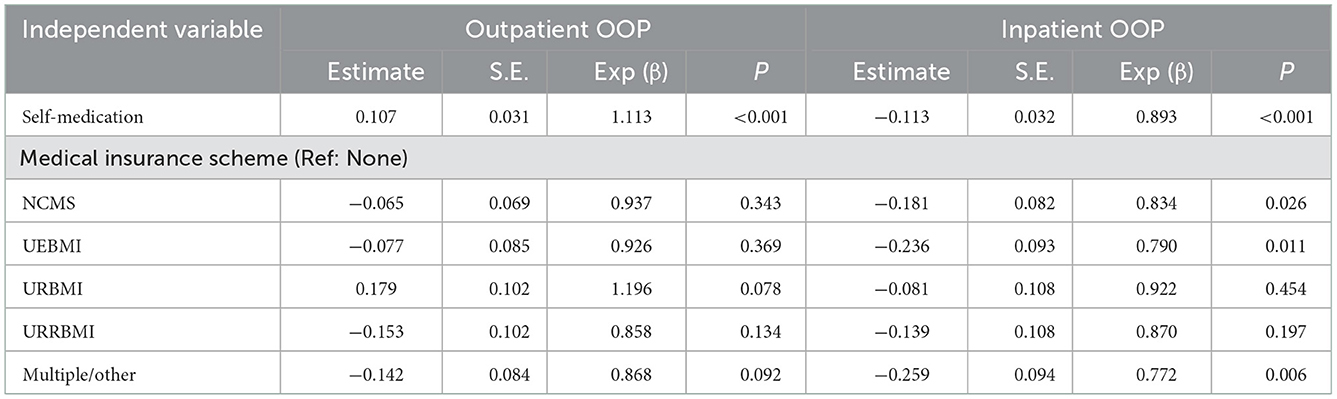
Table 5 shows that annual inpatient OOP costs were significantly reduced by 10.7% (P < 0.001) and monthly outpatient OOP costs were significantly increased by 11.3% (P < 0.001) in respondents who had taken self-medication. Nevertheless, the impact of medical insurance schemes on total costs and OOP costs showed great heterogeneity. Compared to the uninsured cases, all schemes increased total medical expenditure whether outpatient or inpatient, but statistically significant differences were only found in UEBMI (Poutpatient < 0.001; Pinpatient < 0.001) and Multiple/Other insurances (Pinpatient = 0.011). On the other hand, none of the schemes had a significant effect on outpatient out-of-pocket expenditures. In particular, the percentage savings for inpatient out-of-pocket expenditures were 21.0% (P = 0.011) in UEBMI, 16.6% (P = 0.026) in NCMS, and 22.8% (P = 0.006) in Multiple/Other insurances.
4. Discussion
This study was a longitudinal data analysis to investigate the impact of self-medication on the medical expenditures of middle-aged and elderly people in China. In our study, we tried to adopt an empirical approach to estimate the net effect of self-medication behavior on individual patient costs with four waves of data, and explored the heterogeneity of the effect on outpatient, inpatient, total costs, and out-of-pocket costs.
Prior studies showed that cost saving is the main reason for choosing self-medication (49). Additionally, the economic value of self-medication has been fully documented. The Consumer Healthcare Products Association (CHPA) indicated that self-medication reduced the frequency of doctor visits. Without self-medication and OTC (Over-the-Counter) medicines, 90% of consumers would have gone to the doctor instead (50). Each dollar spent on OTC medicines saves the U.S. healthcare system more than USD 7(33), and the availability of self-care medicines generates cost savings of more than USD 146 billion for the healthcare system annually in the US (51). The Association of the European Self-Medication Industry (AESGP) also reported that 1.2 billion minor health issues were self-managed every year with self-care products (35), with responsible self -medication accounting for a large proportion. This condition saved the healthcare systems and national economies EUR 34 billion (35). In Australia, the predicted value of switching 11 categories of current prescription medicines to OTC to promote self-medication resulted in savings of a further $1.1 billion for the healthcare system and almost $730 million for Medicare (34).
In terms of inpatient expenditures, comparable results were obtained in our study. We found that respondents who had self-medicated were less likely to use inpatient services, and their inpatient expenses were significantly reduced by 9.4%. Previous research showed that patients in pain who self-medicated with non-prescription medication were associated with significantly fewer hospitalizations experiences (52). Patients with hemophilia who took self-medication without prior consultation with a physician had an 89% reduction in the number of days they were hospitalized (53). To sum up, our results were consistent with fewer hospitalizations and shorter hospital stays. Furthermore, self-medication behaviors were associated with lower inpatient costs.
Although most studies reported that self-medication can reduce outpatient service utilization (50, 54, 55), we drew the unanticipated conclusion. The estimator indicated that self-medication behaviors were significantly associated with a higher probability of outpatient service utilization but showed no significant association with outpatient expenses. In general, self-medication serves as an alternative to absorb the demand of outpatient services. Patients choose self-medication to avoid visits to medical facilities because of various reasons, but it shows different characteristics among different age groups. A large proportion of the younger group performed self-medication because they felt the disease was too mild to require medical service (56). As regards older groups, the major diseases that led to self-treatment were recurrent and related to aging. Such diseases can often be well controlled by regular over-the-counter medication (57). Variance among groups provided a clue to explaining our unanticipated findings.
One possible explanation for the difference between outpatient and inpatient cases among the middle-aged and elderly population might be health awareness and health literacy. Engaging in self-care activities, such as self-medication, is generally considered as a consequence of health condition awareness (58). Respondents who self-medicated tended to be more health-conscious and more concerned about their own health status. This condition provided them with an advantage in comprehending the importance and methods of early disease detection and treatment (59). Respondents who had taken self-medication implemented better interventions in the early stages of the disease, which reduced the risk of chronic disease progression (60, 61). Possible consequences were an increase in outpatient utilization, due to early interventions, such as disease screening and return visits, and a decrease in inpatient utilization because of the effective control of chronic diseases. Despite these interesting results, the mechanism related to the heterogeneity between outpatient and inpatient cases remains speculative, which is limited by secondary data. Therefore, caution should be warranted in extrapolating the results to all patients. Further studies are required to provide more precise explanations by employing the prospective study design.
As far as the OOP costs were concerned, inpatient respondents showed similar results with total medical expenditure. Unexpectedly, outpatient OOP costs were significantly increased among respondents who had self-medicated. The results reminded us of the determinants of self-medicating behaviors. In developing countries, the main reasoning behind people self-medicating was a simple sign and symptom of disease (30), which was often associated with primary care utilization. The substitution relationship between self-medication and primary health care utilization provided a convenient approach to minor illnesses or health problems. However, when serious health problems arose, respondents were forced to turn to higher-tier hospitals. This meant the outpatient service utilization of respondents who had taken self-medication was likely inclined to non-primary care providers because of the substitution relationship. In China, visits to non-primary care providers showed higher patient cost-sharing, a policy that encouraged patients to seek primary care (62). Lower reimbursement rates resulted in higher out-of-pocket outpatient costs for the group we focused on.
Another significant aspect that deserved attention was medical insurance. In China, the government has developed a universal medical insurance system. The basic insurance system offered by the Chinese government consists of three schemes: UEBMI, which provides health insurance to formal-sector urban employees and retirees; URBMI, which aims to insure the urban residents not covered by the UEBMI, such as students and the self-employed; and NCMS, which is a voluntary medical insurance scheme targeting rural residents (44). In 2016, the State Council announced that it would integrate the NCMS and URBMI into URBMI (Urban and Rural Resident Basic Medical Insurance) to integrate fragmented medical insurance schemes and reduce inequity (63). We found that all schemes were significantly associated with a higher probability of medical service utilization, whether outpatient or inpatient. Medical insurances provided better financial protection for respondents, which lowered the barriers for individuals to seek healthcare services (64, 65). Thus, healthcare utilization by the insured increased accordingly (66), which was more similar to our results. In terms of out-of-pocket costs, different schemes reflected the heterogeneity. Almost all schemes played a role in reducing OOP costs, but they were not significant in outpatient cases. Three schemes were significantly associated with lower inpatient OOP costs, where the percentage savings for inpatient out-of-pocket expenditures were 21.0% in UEBMI, 16.6% in NCMS, and 22.8% in multiple/other insurances. The deficient reimbursement levels of medical insurance on outpatient care has been a problem in China's social health insurance schemes (44, 67). Meanwhile, the fragmentized social health insurance schemes operate in isolation, creating inequalities in the system across insurance programs (68). This situation was reflected in our findings: (1) UEBMI individuals provided the most generous benefit packages (65, 69); (2) A certain gap remains between the actual and expected goals of URRBMI (70), which was integrated from NCMS and URBMI; (3) Private health insurance (PHI) was an important supplement to the basic health insurance schemes (71).
Our research affirmed the economic value of self-medication among the middle-aged and elderly population in China. Responsible self-medication deserves to be promoted because it delivers significant benefits for both patients and healthcare systems. Given the risks of self-medication (72), reasonable guidance for residents is necessary in the future. Systematic public educational measures, such as public lectures, television, and online social networks, are necessary to reduce the harmful effects of improper self-medication. Regulations on drug instructions should be strengthened by relevant departments to provide accurate and understandable information on rational drug use.
At the same time, further studies are needed to evaluate the impact of self-medication on medical expenditure across different groups, such as children, women, and medical students.
5. Limitations
This study was limited in several ways. First, we were unable to judge the rationality of self-medication from the questionnaires that did not contain more details on the subjects' self-medication behavior. Although self-medication would cause adverse outcomes if taken inappropriately. Second, some of the variables were based on self-reporting and might be subject to recall bias, especially regarding medical expenditure. Medical expenditure has placed a significant cost burden on Chinese middle-aged and elderly people, as well as an enormous psychological burden. Therefore, the medical expenditure may have been over-reported to a certain extent (73). Finally, we excluded respondents that had utilized medical services but did not provide specific medical expenditure, which would bias the estimate of the probability of medical service utilization in the selection equations.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://opendata.pku.edu.cn/dataverse/CHARLS.
Author contributions
ZF and XS contributed to the conception and design of the study. ZZ performed the statistical analysis and wrote the first draft of the manuscript. DF and DZ wrote sections of the manuscript. DD and YL provided constructive suggestions in revising the manuscript. All authors contributed to the manuscript revision, read, and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China [Grant Nos.: 71804052 and 72274071], Scientific Research Project of Hubei Health Committee [Grant No.: WJ2021Q022], and the National Key Research and Development Program [Grant No.: 2020YFC2006500].
Acknowledgments
The authors thank the China Health and Retirement Longitudinal Study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. The role of the pharmacist in self-care and self-medication. World Health Organization Essential Drugs and Medicines Policy - WHO / EDM. (1998).
2. World Self-Medication Industry. The Story of Self-Care and Self-Medication, 40 years of progress (2010). Available online at: https://www.wsmi.org/resources/story-self-care-and-self-medication-40-years-progress (accessed April 28, 2022).
3. Chautrakarn S, Khumros W, Phutrakool P. Self-medication with over-the-counter medicines among the working age population in metropolitan areas of Thailand. Front Pharmacol. (2021) 12:726643. doi: 10.3389/fphar.2021.726643
4. Mortazavi SS, Shati M, Khankeh HR, Ahmadi F, Mehravaran S, Malakouti SK. Self-medication among the elderly in Iran: a content analysis study. BMC Geriatr. (2017) 17:198. doi: 10.1186/s12877-017-0596-z
5. Rajamma RK, Paswan AK, Pelton LE. Flipping the script: Consumers' propensity for self-medication. J Market Theory Pract. (2021) 29:448–62. doi: 10.1080/10696679.2020.1870240
6. Brandao GR, Teixeira L, Araujo L, Paul C, Ribeiro O. Self-medication in older European adults: Prevalence and predictive factors. Arch Gerontol Geriatr. (2020) 91:104189. doi: 10.1016/j.archger.2020.104189
7. Carmona-Torres JM, Cobo-Cuenca AI, Recio-Andrade B, Laredo-Aguilera JA, Martins MM, Rodriguez-Borrego MA. Prevalence and factors associated with polypharmacy in the older people: 2006-2014. J Clin Nurs. (2018) 27:2942–52. doi: 10.1111/jocn.14371
8. Vahedi S, Jalali FS, Bayati M, Delavari S. Predictors of Self-medication in Iran: A notional survey study. Iran J Pharm Res. (2021) 20:348–58. doi: 10.22037/ijpr.2020.113601.14394
9. Gama ASM, Secoli SR. Self-medication practices in riverside communities in the Brazilian Amazon Rainforest. Rev Bras Enferm. (2020) 73:e20190432. doi: 10.1590/0034-7167-2019-0432
10. Zhao Y, Ma S. Observations on the prevalence, characteristics, and effects of self-treatment. Front Public Health. (2016) 4:69. doi: 10.3389/fpubh.2016.00069
11. Wang R, Ma C, Jiang K, Li M, Ma S. Descriptions of self-treatment for the middle-aged and elderly in Shanxi, China. PLoS ONE. (2018) 13:e0198554. doi: 10.1371/journal.pone.0198554
12. Lei XS, Jiang H, Liu CJ, Ferrier A, Mugavin J. Self-Medication Practice and Associated Factors among Residents in Wuhan, China. Int J Environ Res Public Health. (2018) 15:69. doi: 10.3390/ijerph15010068
13. Wang Z, Guan X, Zhou Y, Han S, Yao P, Shi L. Prevalence and influence factors of self-medication in Chinese middle-aged and elderly people: evidence from 2011, 2013 and 2015 CHARLS panel data. J Chin Pharm Sci. (2019) 28:430–8. doi: 10.5246/jcps.2019.06.042
14. Jerez-Roig J, Medeiros LF, Silva VA, Bezerra CL, Cavalcante LA, Piuvezam G, et al. Prevalence of self-medication and associated factors in an elderly population: a systematic review. Drugs Aging. (2014) 31:883–96. doi: 10.1007/s40266-014-0217-x
15. Qato DM, Alexander GC, Conti RM, Johnson M, Schumm P, Lindau ST. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. Jama. (2008) 300:2867–78. doi: 10.1001/jama.2008.892
16. Francis SA, Barnett N, Denham M. Switching of prescription drugs to over-the-counter status: is it a good thing for the elderly? Drugs Aging. (2005) 22:361–70. doi: 10.2165/00002512-200522050-00001
17. Gao Z, Xu L, Qin W, Zhang J, Zhou J, Hu F, et al. Prevalence and associated factors of self-treatment among the elderly-a comparative study between empty and non-empty nesters in Shandong, China. Int J Environ Res Public Health. (2020) 17:7880. doi: 10.3390/ijerph17217880
18. Klotz U. Pharmacokinetics and drug metabolism in the elderly. Drug Metab Rev. (2009) 41:67–76. doi: 10.1080/03602530902722679
19. Flores VB, Benvegnú LA. Use of medicines by the elderly in Santa Rosa, Rio Grande do Sul State, Brazil. Cad Saude Publica. (2008) 24:1439–46. doi: 10.1590/S0102-311X2008000600024
20. Zawahir S, Lekamwasam S, Halvorsen KH, Rose G, Aslani P. Self-medication Behavior with antibiotics: a national cross-sectional survey in Sri Lanka. Expert Rev Anti Infect Ther. (2021) 19:1341–52. doi: 10.1080/14787210.2021.1911647
21. Bennadi D. Self-medication: A current challenge. J Basic Clin Pharm. (2013) 5:19–23. doi: 10.4103/0976-0105.128253
22. Locquet M, Honvo G, Rabenda V, Van Hees T, Petermans J, Reginster JY, et al. Adverse health events related to self-medication practices among elderly: a systematic review. Drugs Aging. (2017) 34:359–65. doi: 10.1007/s40266-017-0445-y
23. Gong Y, Jiang N, Chen Z, Wang J, Zhang J, Feng J, et al. Over-the-counter antibiotic sales in community and online pharmacies, China. Bull World Health Organ. (2020) 98:449–57. doi: 10.2471/BLT.19.242370
24. Keehan SP, Stone DA, Poisal JA, Cuckler GA, Sisko AM, Smith SD, et al. National health expenditure projections, 2016-25: price increases, aging push sector to 20 percent of economy. Health Aff (Millwood). (2017) 36:553–63. doi: 10.1377/hlthaff.2016.1627
25. Holle M, Wolff T, Herant M. Trends in the Concentration and Distribution of Health Care Expenditures in the US, 2001-2018. JAMA Netw Open. (2021) 4:e2125179. doi: 10.1001/jamanetworkopen.2021.25179
26. Ayalew MB. Self-medication practice in Ethiopia: a systematic review. Patient Prefer Adher. (2017) 11:401. doi: 10.2147/PPA.S131496
27. Ponte M, Wachs L, Serra A, Othatz L, Souto SM, Wachs A. Self medication and self prescription: relevance in daily medicine. Drug Safety. (2014) 37:835.
28. Wen Y, Lieber E, Wan D, Hong Y, A. qualitative study about self-medication in the community among market vendors in Fuzhou, China. Health Soc Care Community. (2011) 19:504–13. doi: 10.1111/j.1365-2524.2011.01009.x
29. Beyene KGM, Beza SW. Self-medication practice and associated factors among pregnant women in Addis Ababa, Ethiopia. Trop Med Health. (2018) 46:10. doi: 10.1186/s41182-018-0091-z
30. Shaghaghi A, Asadi M, Allahverdipour H. Predictors of self-medication behavior: a systematic review. Iran J Public Health. (2014) 43:136–46.
31. Noone J, Blanchette CM. The value of self-medication: summary of existing evidence. J Med Econ. (2018) 21:201–11. doi: 10.1080/13696998.2017.1390473
32. Jafari F, Khatony A, Rahmani E. Prevalence of self-medication among the elderly in Kermanshah-Iran. Glob J Health Sci. (2015) 7:360–5. doi: 10.5539/gjhs.v7n2p360
33. Consumer Healthcare Products Association. OTC Medicines Save the U.S. Healthcare System Money. (2019). Available online at: https://www.chpa.org/about-consumer-healthcare/infographics/otc-medicines-save-us-healthcare-system-money (accessed May 14, 2022).
34. Macquarie Centre for the Health Economy. The Value of OTC Medicines in Australia. (2014). Available online at: https://www.chpaustralia.com.au/Tenant/C0000022/Documents/Research/Value%20of%20OTC%20Medicines%20in%20Australia.pdf
35. Association of the European Self-Medication Industry. Self-Care in Europe: Economic and Social Impact on Individuals and Society. (2021). Available online at: https://aesgp.eu/articles/aesgp-releases-new-evidence-on-the-economic-and-social-value-of-self-care-in-europe
36. Zhang P, Jiang H, Chen W. Health shocks and changes in preventive behaviors: Results from the China Health and Retirement Longitudinal Study. Front Public Health. (2022) 10:954700. doi: 10.3389/fpubh.2022.954700
37. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
38. Jiang Y, Ni W. Association between supplemental private health insurance and burden of out-of-pocket healthcare expenditure in China: A novel approach to estimate two-part model with random effects using panel data. Risk Manag Healthc Policy. (2020) 13:323–34. doi: 10.2147/RMHP.S223045
39. Evashwick C, Rowe G, Diehr P, Branch L. Factors explaining the use of health care services by the elderly. Health Serv Res. (1984) 19:357–82.
40. Pan L, Li L, Peng H, Fan L, Liao J, Wang M, et al. Association of depressive symptoms with marital status among the middle-aged and elderly in Rural China-Serial mediating effects of sleep time, pain and life satisfaction. J Affect Disord. (2022) 303:52–7. doi: 10.1016/j.jad.2022.01.111
41. Lin L, Wang HH, Lu C, Chen W, Guo VY. Adverse childhood experiences and subsequent chronic diseases among middle-aged or older adults in china and associations with demographic and socioeconomic characteristics. JAMA Netw Open. (2021) 4:e2130143. doi: 10.1001/jamanetworkopen.2021.30143
42. Zhou J, Fang S. Association between undiagnosed hypertension and health factors among middle-aged and elderly Chinese population. Int J Environ Res Public Health. (2019) 16:1214. doi: 10.3390/ijerph16071214
43. Lei X, Smith JP, Sun X, Zhao Y. Gender differences in cognition in China and reasons for change over time: Evidence from CHARLS. J Econ Ageing. (2014) 4:46–55. doi: 10.1016/j.jeoa.2013.11.001
44. Zhang A, Nikoloski Z, Mossialos E. Does health insurance reduce out-of-pocket expenditure? Heterogeneity among China's middle-aged and elderly. Soc Sci Med. (2017) 190:11–9. doi: 10.1016/j.socscimed.2017.08.005
45. Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. (2004) 23:525–42. doi: 10.1016/j.jhealeco.2003.10.005
46. Zhao J, Zhao Y, Xiang L, Khanal V, Binns CW, Lee AH, et al. two-part mixed-effects model for analyzing clustered time-to-event data with clumping at zero. Comput Methods Programs Biomed. (2020) 187:105196. doi: 10.1016/j.cmpb.2019.105196
47. Hasan MZ, Story WT, Bishai DM, Ahuja A, Rao KD, Gupta S. Does social capital increase healthcare financing's projection? Results from the rural household of Uttar Pradesh, India. SSM - Populat Health. (2021) 15:100901. doi: 10.1016/j.ssmph.2021.100901
48. Nosyk B, Montaner JS, Yip B, Lima VD, Hogg RS. Antiretroviral drug costs and prescription patterns in British Columbia, Canada: 1996-2011. Med Care. (2014) 52:362–9. doi: 10.1097/MLR.0000000000000097
49. Haque M, Rahman NAA, McKimm J, Kibria GM, Azim Majumder MA, Haque SZ, et al. Self-medication of antibiotics: investigating practice among university students at the Malaysian National Defence University. Infect Drug Resist. (2019) 12:1333–51. doi: 10.2147/IDR.S203364
50. Consumer Healthcare Products Association. OTC Medicines Reduce Doctors Visits. (2019). Available online at: https://www.chpa.org/about-consumer-healthcare/infographics/otc-medicines-reduce-doctors-visits. (accessed May 14, 2022).
51. Consumer Healthcare Products Association. OTC Medicines Save Billions Annually. (2019). Available online at: https://www.chpa.org/about-consumer-healthcare/infographics/otc-medicines-save-billions-annually (accessed May 14, 2022).
52. Lee LJ, DiBonaventura MD, Kudel I, Schepart AL, Kellstein D. PSY51 - The incremental effect of over-the-counter medications on work productivity and health care resource utilization among adults with pain in the united states. Value in Health. (2016) 19:A250. doi: 10.1016/j.jval.2016.03.1074
53. Levine PH, Britten AF. Supervised patient-management of hemophilia: A study of 45 patients with hemophilia A and B. Annals of internal medicine. (1973) 78:195–201. doi: 10.7326/0003-4819-78-2-195
54. Millier A, Cohen J, Toumi M. Economic impact of a triptan Rx-to-OTC switch in six EU countries. PLoS ONE. (2013) 8:e84088. doi: 10.1371/journal.pone.0084088
55. Rankin PJ, Tsvetkova IV, Estus E, Nah N, Senne B. Managing Access to Dextromethorphan: Cost Implications of a Potential Over-the-Counter to Prescription-Only Conversion. (2016). Available online at: https://www.crai.com/insights-events/publications/managing-access-dextromethorphan-cost-implications-potential-over-counter-prescription/ (accessed May 14, 2022).
56. Flaiti MA, Badi KA, Hakami WO, Khan SA. Evaluation of self-medication practices in acute diseases among university students in Oman. J Acute Dis. (2014) 3:249–52. doi: 10.1016/S2221-6189(14)60056-1
57. Jiang Y, Wang Y, Li Y, Wang X, Ma C, Ma S. Prevalence, characteristics, and cost of self-treatment in the middle-aged and elderly: observations from Henan, China. Public Health. (2015) 129:597–600. doi: 10.1016/j.puhe.2015.02.005
58. Squiers L, Peinado S, Berkman N, Boudewyns V, McCormack L. The health literacy skills framework. J Health Commun. (2012) 17:30–54. doi: 10.1080/10810730.2012.713442
59. Lee SY, Arozullah AM, Cho YI. Health literacy, social support, and health: a research agenda. Soc Sci Med. (2004) 58:1309–21. doi: 10.1016/S0277-9536(03)00329-0
60. Galbraith L, Jacobs C, Hemmelgarn BR, Donald M, Manns BJ, Jun M. Chronic disease management interventions for people with chronic kidney disease in primary care: a systematic review and meta-analysis. Nephrol Dialysis Transplant. (2017) 33:112–21. doi: 10.1093/ndt/gfw359
61. Welte T, Vogelmeier C, Papi A. COPD early diagnosis and treatment to slow disease progression. Int J Clin Pract. (2015) 69:336–49. doi: 10.1111/ijcp.12522
62. Shen M, He W, Li L. Incentives to use primary care and their impact on healthcare utilization: Evidence using a public health insurance dataset in China. Soc Sci Med. (2020) 255:112981. doi: 10.1016/j.socscimed.2020.112981
63. Ren Y, Zhou Z, Cao D, Ma BH, Shen C, Lai S, et al. Did the Integrated Urban and Rural Resident Basic Medical Insurance Improve Benefit Equity in China? Value Health. (2022) 25:1548–58. doi: 10.1016/j.jval.2022.03.007
64. Ta Y, Zhu Y, Fu H. Trends in access to health services, financial protection and satisfaction between 2010 and 2016: Has China achieved the goals of its health system reform? Soc Sci Med. (2020) 245:112715. doi: 10.1016/j.socscimed.2019.112715
65. Zhou Y, Wushouer H, Vuillermin D, Ni B, Guan X, Shi L. Medical insurance and healthcare utilization among the middle-aged and elderly in China: evidence from the China health and retirement longitudinal study 2011, 2013 and 2015. BMC Health Serv Res. (2020) 20:654. doi: 10.1186/s12913-020-05522-w
66. Li Y, Malik V, Hu FB. Health Insurance In China: After Declining In The 1990s, Coverage Rates Rebounded To Near-Universal Levels By 2011. Health Aff (Millwood). (2017) 36:1452–60. doi: 10.1377/hlthaff.2016.1658
67. Dong W, Zwi AB, Bai R, Shen C, Gao J. Benefits associated with China's social health insurance schemes: trend analysis and associated factors since health reform. Int J Environ Res Public Health. (2021) 18:5672. doi: 10.3390/ijerph18115672
68. Liu GG, Vortherms SA, Hong X. China's health reform update. Annu Rev Public Health. (2017) 38:431–48. doi: 10.1146/annurev-publhealth-031816-044247
69. Su M, Zhou Z, Si Y, Wei X, Xu Y, Fan X, et al. Comparing the effects of China's three basic health insurance schemes on the equity of health-related quality of life: Using the method of coarsened exact matching. Health Qual Life Outc. (2018) 16:41. doi: 10.1186/s12955-018-0868-0
70. Wang Z, Chen Y, Pan T, Liu X, Hu H. The comparison of healthcare utilization inequity between URRBMI and NCMS in rural China. Int J Equity Health. (2019) 18:90. doi: 10.1186/s12939-019-0987-1
71. Wang Q, Zhang D, Hou Z. Insurance coverage and socioeconomic differences in patient choice between private and public health care providers in China. Soc Sci Med. (2016) 170:124–32. doi: 10.1016/j.socscimed.2016.10.016
72. Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self medication. Drug Safety. (2001) 24:1027–37. doi: 10.2165/00002018-200124140-00002
Keywords: self-medication, medical expenditure, middle-aged and elderly population, longitudinal study, two-part mixed-effect model, China
Citation: Zheng Z, Feng Z, Zhang D, Sun X, Dong D, Luo Y and Feng D (2023) Does self-medication reduce medical expenditure among the middle-aged and elderly population? A four-wave longitudinal study in China. Front. Public Health 10:1047710. doi: 10.3389/fpubh.2022.1047710
Received: 18 September 2022; Accepted: 16 December 2022;
Published: 11 January 2023.
Edited by:
Rebecca Masters, Public Health Wales NHS Trust, United KingdomReviewed by:
Ewelina Chawlowska, Poznan University of Medical Sciences, PolandEnver Envi Roshi, University of Medicine, Tirana, Albania
Haixia Liu, Binzhou Medical University, China
Copyright © 2023 Zheng, Feng, Zhang, Sun, Dong, Luo and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Da Feng,  ZmVuZ2RhQGh1c3QuZWR1LmNu
ZmVuZ2RhQGh1c3QuZWR1LmNu
 Zehao Zheng
Zehao Zheng Zhanchun Feng2
Zhanchun Feng2 Donglan Zhang
Donglan Zhang Xiaobo Sun
Xiaobo Sun Da Feng
Da Feng