- 1Department of Pediatrics, Faculty of Medicine, Kuwait University, Kuwait City, Kuwait
- 2Department of Population Health, Dasman Diabetes Institute, Kuwait City, Kuwait
- 3Department of Pediatrics, Al-Farwaniya Hospital, Kuwait City, Kuwait
Background: With the rapid transmission of COVID-19 globally, countries have implemented strict governmental measures and social distancing rules that aimed to minimize the spread of the virus. School closures, quarantine orders, and social isolation, coupled with a surge in family stress and lack of peer interactions, are probable causes of mental health complications and psychological symptoms faced by children. This study aims at comparing the HRQoL of children and adolescents with type 1 diabetes (T1D) and affected by COVID-19 infection (personal or familial) and those who were not affected by COVID-19.
Materials and methods: A random sample was selected from children and adolescents diagnosed with T1D at the six major governmental diabetes centers in Kuwait. To measure HRQoL, parent-proxy and self-reports from the Pediatric Quality of Life Inventory (PedsQLTM) 3.0 Diabetes Module were used.
Results: A sample of 455 children and adolescents with T1D diabetes (44.6% male participants and 41.98% affected by COVID-19 infection) was studied. The total score of the HRQoL self-reports was significantly higher compared with parent-proxy reports (79.06 ± 15.19 vs. 73.79 ± 15.17, p < 0.01). Children reported significantly higher HRQoL scores in the “treatment I” domain and “worry” domain and lower scores in the “diabetes” symptoms domain, compared with their parents' reports (p < 0.01). In the COVID-19-affected group, a major difference was noticed between the total scores of children and parent-proxy reports (77.04 ± 15.81 vs. 72.80±14.90, p = 0.047). The affected children reported significantly lower scores in “diabetes” symptoms (59.50) (p < 0.01) and higher scores in the “treatment I” domain (81.43) than their parent-proxy reports (72.05) (p < 0.01).
Conclusion: This is the first report on the health-related quality of life of children with T1D in Kuwait during the COVID-19 era. Parents' or caregivers' experience of caring for their children was negative, as they worried, and reported poorer HRQoL compared with their children's perceptions. There is a need to empower healthcare professionals to support parents and caregivers of children with chronic diseases such as T1D in promoting self-management, enhancing physical and psychological wellbeing, treatment adherence, and continuous health education during pandemics of any kind.
Introduction
The COVID-19 pandemic has undoubtedly impacted all areas of the global population's daily lives, both physically and mentally, making it a worldwide healthcare disaster. With the rapid transmission of COVID-19 globally, countries have implemented strict governmental measures and social distancing rules that aimed to minimize the spread of the virus. School closures, quarantine orders, and social isolation, coupled with a surge in family stress and lack of peer interactions, are probable causes of mental health complications and psychological symptoms faced by children (1, 2). A recent meta-analysis using data from 80,879 youths globally, to investigate the pandemic's effect on mental health, reported a pooled prevalence estimate of clinically elevated depression and anxiety: 25.2% for children and 20.5% for adolescents. Compared with pre-pandemic estimates, the prevalence of depression and anxiety symptoms during COVID-19 has doubled (1). Mental health problems, particularly hyperactivity and peer problems, as well as psychosomatic complaints, such as sleeping problems and headaches, were also experienced by children during the pandemic (3).
Children with chronic illnesses faced additional challenges during the COVID-19 pandemic, including hindrance to accessing inpatient and outpatient clinical care. These limitations in care may have negatively impacted children with type 1 diabetes (T1D) since diabetes pediatric centers shifted to telemedicine (4). Families with children and adolescents with T1D were forced to change their approach to disease management as health services and delivery became significantly disrupted (4, 5). This may have resulted in delayed diabetes diagnosis, delayed insulin delivery, more episodes of diabetic ketoacidosis (DKA) and hyperglycemia, and admission to the pediatric intensive care unit (PICU); families also experienced fear of contracting COVID-19 infection while obtaining care (6). Furthermore, COVID-19 infection itself in individuals with preexisting diabetes has been associated with higher rates of hospitalization and admission to the intensive care unit (7, 8). These might indeed have a negative impact on an infected child's mental health and wellbeing. It might be also safe to assume that COVID-19 infection in a close family member might have a negative impact on the child, as the role of family dynamics and functioning influence diabetes management behavior and metabolic control (9).
Within and beyond the context of the pandemic, children with T1D face daily challenges, such as intensive therapeutic insulin regimes, dietary restrictions, and necessary physical activity (10). These children are also prone to the development of profound feelings of uncertainty, fear, or irritability that are a result of home confinement and disruptions in normal routine, which may ultimately influence their diabetes management (4, 11). These factors in combination make it imperative to address the emotional state of this population and assess their health-related quality of life (HRQoL) during the pandemic.
The assessment of HRQoL is crucial in clinical trials and healthcare as it measures the impact of diseases or disabilities on the mental, physical, and social dimensions of a patient's health (12, 13). Diabetes-specific HRQoL measurement instruments are critical for the assessment of symptoms and problems relevant to people living with diabetes, as well as the person's adherence to diabetes self-management (14, 15). Considering the obstacles of accessing healthcare and diabetes management as well as the emotional consequences resulting from the COVID-19 pandemic, it may be expected that pediatric patients with T1D have impaired HRQoL.
One objective of this study was to compare the HRQoL of children and adolescents (aged 2–18 years) with T1D and affected by COVID-19 infection (personal or familial) and those who were not affected by COVID-19. An additional objective is to measure the similarities and differences between the children's and parents' HRQoL reports during the COVID-19 pandemic.
2. Methods
2.1. Study design and subjects
Starting in January 2021, a random sample was selected from children and adolescents diagnosed with T1D between January 2011 and January 2020 at the six major governmental diabetes centers in Kuwait. Children aged 2–18 years who met the inclusion criteria: diabetes duration for at least 1 year, resident of Kuwait during the pandemic for at least 6 months, and Arabic-speaking parents and children, were included. Participants with other comorbidities (such as developmental delay and chronic renal disease) apart from T1D and its complications, and parents who refused to participate were excluded.
A total of 656 families were approached; of these, 586 (89.3%) were eligible while 70 (10.6%) did not meet the inclusion criteria; among those eligible, 455 (77.6%) agreed to participate. Of the 455 families, 116 fathers, 334 mothers, and 3 legal guardians were interviewed. A total of 203 boys and 252 girls were enrolled, including 49 children aged 2–4 years, 74 children aged 5–7 years, 204 children aged 8–12 years, and 128 children aged 13–18 years at the time of interview; these age groups correspond with the HRQoL instrument's age categories.
2.2. Data collection
Interviews were performed from January to October 2021, after parental consent and child assent were obtained. Most families participated over the phone or via a web-based platform (n = 433), but 22 families were directly interviewed during clinical visits. The PedsQLTM 3.0 Diabetes Module Arabic version, a validated questionnaire for children, was used to assess diabetes-specific HRQoL (16, 17). Before completion of the PedsQLTM 3.0 forms, baseline data were retrieved from parents or caregivers regarding demographic characteristics, diabetes-related history, and COVID-19 infection history. Glycemic status was obtained from medical records in terms of glycated hemoglobin (HbA1c) within 3 months of the recruitment. Optimal control was defined as HbA1c of < 7% as per the 2018 International Society of Pediatric and Adolescent Diabetes (ISPAD) guidelines, and HbA1C of above 9.0% was considered high risk (18). The study protocol was approved by the Standing Committee for Coordination of Health and Medical Research (Ethics Review Committee) at the Ministry of Health (MoH) of Kuwait (Reference No. 1588/2020).
2.3. PedsQLTM 3.0 Diabetes module
The 28-item module is composed of five scales: (1) diabetes symptoms (11 items), (2) treatment barriers I (4 items), (3) treatment adherence II (7 items), (4) worry (3 items), and (5) communication (3 items). The module is designed for four age groups: parent-proxy reports for toddlers (2–4 years), parent-proxy and child self-reports for young children (5–7 years), school-age children (8–12 years), and teenagers (13–18 years). The PedsQLTM items follow the five-point Likert scale from 0 (never) to 4 (almost always) for all age groups, except for young children (aged 5–7 years), which follows a three-point scale: 0 (not at all), 2 (sometimes), and 4 (a lot). To calculate the health-related quality of life (HRQoL), items were reverse-scored and linearly transformed on a scale from 0 to 100 (0 = 100, 1 = 75, 2 = 50, 3 = 25, and 4 = 0), and the sum of all items was divided over the number of items answered to calculate the total score. Higher scores indicate better HRQoL (19, 20).
The original PedsQLTM 3.0 Diabetes module was translated into Arabic and validated on children with T1D and their parents/caregivers at Kuwait University, Kuwait, based on the linguistic validation guidelines of the PedsQLTM Quality of Life Questionnaire and approved by MAPI Research Trust, on behalf of Dr. James W. Varni, the copyright owner of PedsQLTM (17, 21).
2.4. Procedure
In preparation for the study, a comprehensive well-established data collection sheet was developed. Research assistants were trained as interviewers. Following patient identification, a pilot phase was implemented over a 1-month period to test the procedures with a convenient sample of 50 families. The interview process and data collection forms were adjusted after the pilot phase.
The interviews took 20–25 min. The survey consisted of five sections: personal information, diabetes history, COVID-19-related history, COVID-19 family history, and the PedsQL 3.0 questionnaires. The answers were documented by the interviewers based on parents'/children's responses.
To ensure proper enrollment, COVID-19 status in children was confirmed through the Pediatric COVID-19 Registry (PCR-Q8) in Kuwait (MoH Reference No. 2020/1233), a national registry that records all cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in children in the country since the start of the pandemic in February 2020.
2.5. Statistical analysis
Statistical analysis was conducted using STATA software 13.1 (STATA Corp, College Station, TX). Continuous variables were expressed as median and interquartile ranges (IQR), as they were non-normally distributed. The Kruskal–Wallis test was used to test for differences in the continuous variables. The HRQoL scores were expressed as mean and standard deviation (SD). Unpaired t-tests were used to compare total and dimension-specific HRQoL scores between groups (e.g., no COVID-19 infection vs. COVID-19 infection).
3. Results
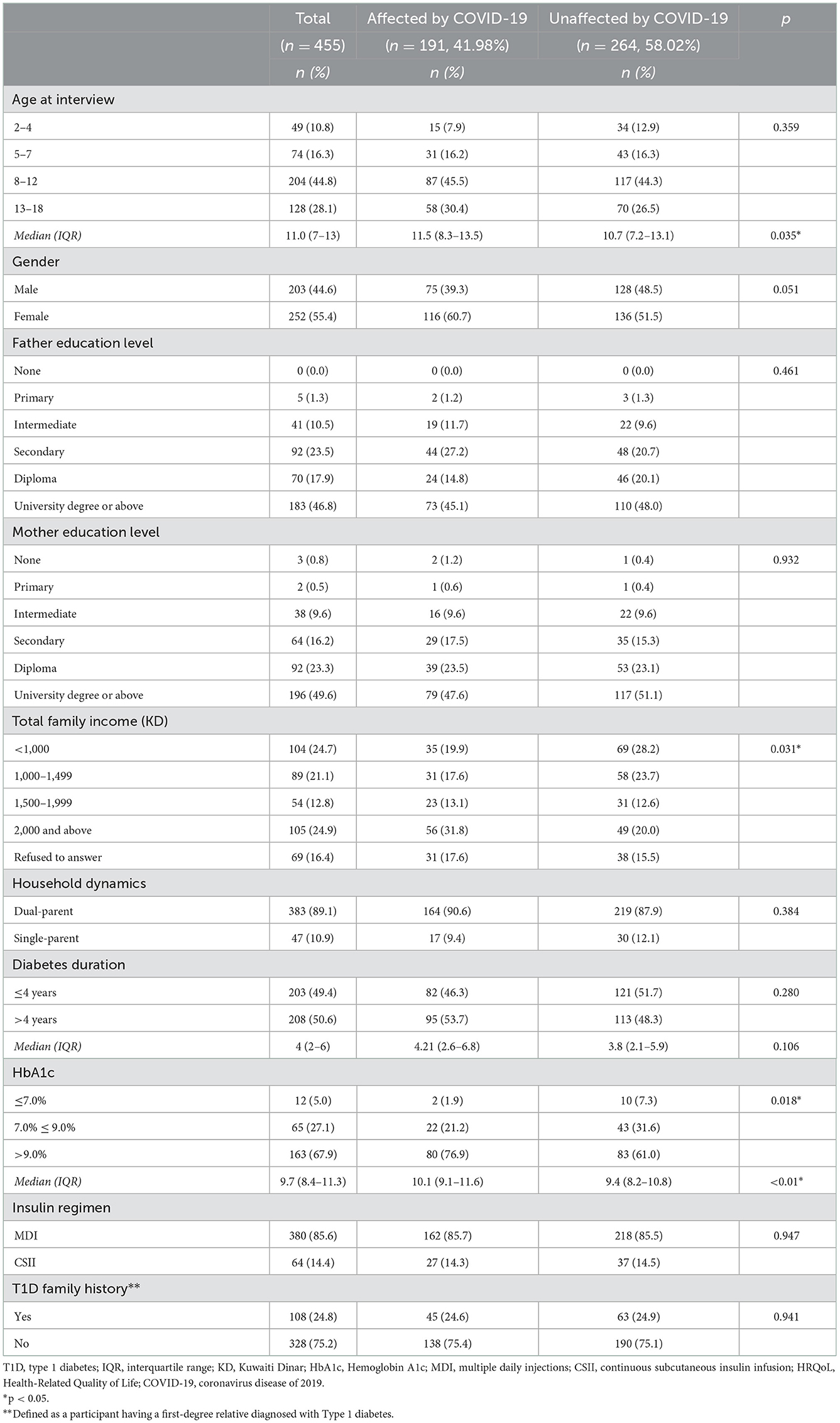
A total of 455 children and adolescents [203 (44.6%) male participants and 252 (55.4%) female participants] with T1D were included. The baseline characteristics of study participants and COVID-19 infection status are shown in Table 1. Among the participants, 191 (41.98%) children were affected by COVID-19. Children who had had COVID-19 were significantly older at the time of the study than those who had not (11.5 vs. 10.7 years, p = 0.035). The majority (31.8%) of the COVID-19-affected children were from families with incomes of 2,000 KD (equivalent to approximately €6,000) and above (p = 0.031). The majority (76.9%) of the children affected by COVID-19 had glycemic control in the high-risk category (p = 0.018), with a significantly higher HbA1c than those who had not been infected with COVID-19 [10.1 (9.1;11.6) vs. 9.4 (8.2;10.8), p < 0.01]. Children who had and had not been affected by COVID-19 were not different in terms of gender, parents' education, household dynamics, diabetes duration, insulin regimen, or family history of T1D. HRQoL was collected for 620 participants based on 165 child self-reports and 455 parent-proxy reports from the PedsQL™ 3.0 Diabetes module. A total of 260 participants were affected by COVID-19, of which 69 were children and 191 were parents. A total of 360 participants not affected by COVID-19 responded to the HRQoL questionnaire, of which 96 were children and 264 were parents.
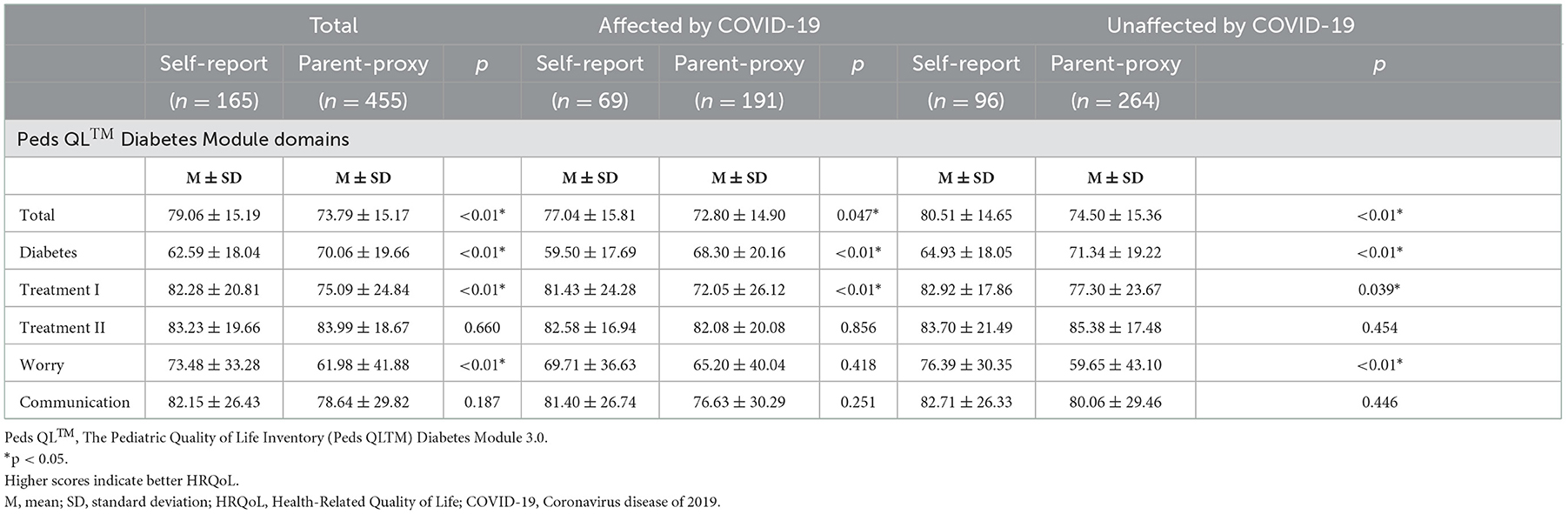
Table 2 describes the self-reports and parent-proxy reports of total and domain-specific HRQoL scores of the whole study population. The mean ± SD total HRQoL score of the self-report was significantly higher compared with those of the parent-proxy reports (79.06 ± 15.19 vs. 73.79 ± 15.17, p < 0.01). Children reported significantly higher scores than their parents in the “treatment barriers I” and “worry” domains (p < 0.01). However, children reported a significantly lower score (62.59 ± 18.04) in the “diabetes” symptoms domain than their parent-proxy reports (70.06 ± 19.66, p < 0.01).
In the COVID-19-affected group, there was a significant difference between the total self-reported HRQoL (77.04) and the parent-proxy HRQoL score (72.80) (p = 0.047). The COVID-19-affected children reported a significantly lower HRQoL score in the “diabetes” symptoms domain in comparison to parent-proxy reports (59.50 vs. 68.30, p < 0.01). However, they reported a significantly higher score in the “treatment barriers I” domain (81.43) than their parent-proxy reports (72.05) (p < 0.01).
Similar to the COVID-19-affected group, children unaffected by COVID-19 reported higher total HRQoL scores (80.51) compared with their parents (74.50) (p < 0.01). Furthermore, parent-proxies in the unaffected COVID-19 group consistently reported significantly lower scores compared with self-reports in the “treatment barriers I” domain (p = 0.039). The children unaffected by COVID-19 also reported a significantly lower score in the “diabetes” symptoms domain than their parent-proxy reports, similar to the COVID-19 affected group (64.93 ± 18.05 vs. 71.34 ± 19.22, p < 0.01).
Table 3 compares the self-report and parent-proxy reports of the affected and unaffected groups (by COVID-19). There was no significant difference between the two groups with regard to self-reports in total or domain-specific scores. However, the parents of COVID-19-affected children reported a significantly lower score in the “treatment barriers I” domain than the unaffected group (72.05 ± 26.12 vs. 77.30 ± 23.67, p = 0.026). Although marginally significant (p = 0.068), parents in the COVID-19-affected group reported lower scores in the “treatment adherence II” domain compared with parents unaffected by COVID-19 (82.08 ± 20.08 vs. 85.38 ± 17.48, p = 0.068).
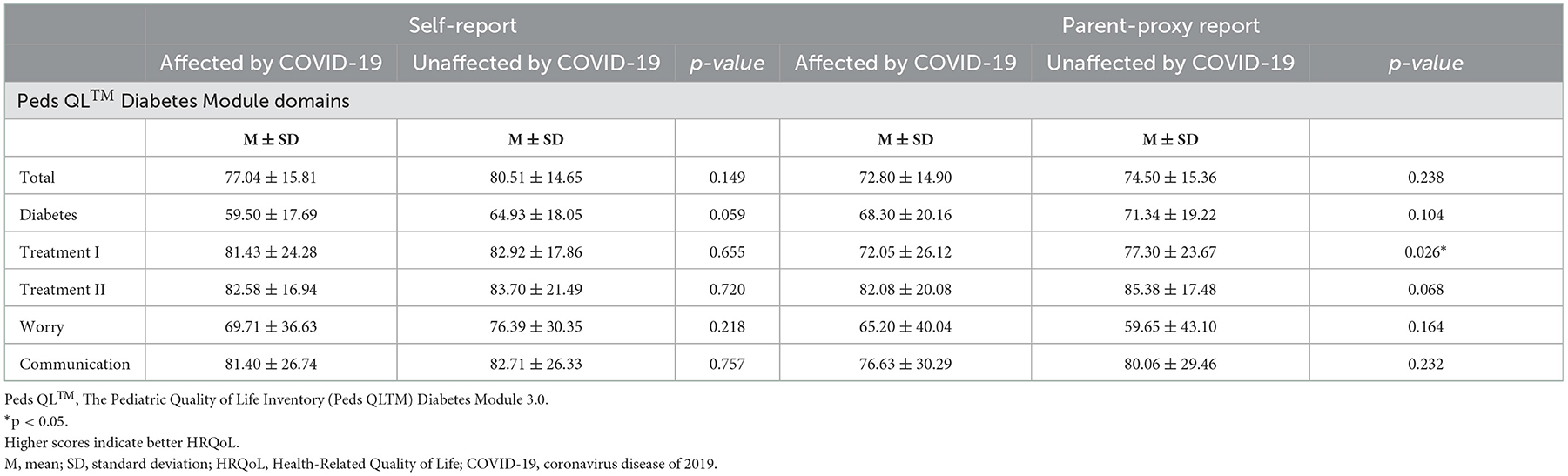
Table 3. Comparison of self-reports and parent-proxy reports for those affected vs. unaffected by COVID-19.
4. Discussion
This study aimed to evaluate the HRQoL of children and adolescents with T1D based on parent-proxy reports using the PedsQL™ 3.0 Diabetes module during the COVID-19 pandemic. This information may provide insights into how experiences of disease management during the COVID-19 pandemic may have been perceived differently by children and their parents. We further compared HRQoL reports from children and parent-proxies who had been affected with COVID-19 infection (personal or familial) with those unaffected.
We found that, regardless of COVID-19 infection status, children and adolescents with T1D reported higher scores (indicating better HRQoL) in the total HRQoL, “treatment barriers I,” and “worry” domains, compared with their parents. Furthermore, children and adolescents in both groups reported lower scores in the “diabetes symptoms” domain, indicating poorer HRQoL. In those affected by COVID-19, parents reported significantly worse HRQoL in “treatment barriers I” and marginally worse HRQoL in the “treatment adherence II” domain, compared with parents whose children were unaffected by COVID-19 infection.
Regardless of being affected or unaffected by COVID-19, parents of children with T1D during the pandemic reported worse HRQoL than what children reported. This finding is consistent with other studies published before the pandemic on children who suffer from T1D and obesity in Kuwait, and children with diabetes in Saudi Arabia (16, 22, 23). In Kuwait, Abdul-Rasoul et al. found that parents of children with T1D reported worse HRQoL than their children (16). Studies in Italy and Norway also showed that parents of children with T1D perceived a lower total quality of life compared with their children (20, 24). This might be attributed to the burden of the disease, the complexity of management, and concern for their child's lifestyle and future (16, 23, 25). Our study demonstrated that such discrepancy between the parents' reports and their children's reports on HRQoL continues to exist during the pandemic. It is therefore warranted to suggest incorporating an assessment of HRQoL during a pandemic to provide support, if needed, by facilitating open communication between children and their families, identifying points of concern from both sides, and planning for joint intervention.
In both groups, parent and child perception of diabetes symptoms, treatment barriers and adherence, worry about sleep quality, anger management, and hypoglycemic episodes were significantly different, consistent with the findings from Kuwait, Saudi Arabia, and Italy (16, 23, 24). The discrepancy in several of the domains indicates the importance of collecting information from the viewpoint of both child and parent, to better understand the impact of disease on HRQoL. The reduced quality of life in the “diabetes symptoms” domain in the children's report may be attributed to more personal effects of diabetes on the child's experiences with the disease.
This study also found that COVID-19-affected parents experienced worse HRQoL in the “treatment barrier” domain, compared with their unaffected counterparts. Treatment barriers include, for example, feeling pain when getting a finger prick or taking an insulin shot, feeling embarrassed about treatment, arguing with parents, or difficulty in caring for their diabetes. To this end, this is the first report that evaluates HRQoL between COVID-19-affected and unaffected children with T1D. Parents' added fear and worry regarding COVID-19 infection in the child or a family member adds to the challenges of managing diabetes and compliance with therapy during such stressful periods (26). The parental burden of management of a chronic condition such as T1D could also be amplified due to the lack of knowledge in relation to dealing with T1D during the pandemic, especially when infected with the infection itself (24–26). Infection control measures implemented by health authorities has led to limited interactions between children with T1D and their healthcare providers, which might indeed contribute to the lack of guidance during the pandemic period (27).
Our study is one of the first reports on HRQoL in children with T1D during the COVID-19 pandemic, regionally or internationally. To conduct the study, we used a validated translated questionnaire, with a disease-specific module, to assess the HRQoL of children and adolescents. There are a number of limitations in the current study. We can only generalize to Arabic speakers in Kuwait, as the data collection instruments were available in Arabic for the current study. The study was cross-sectional; therefore, it cannot provide information on changes in HRQoL over time, or before or after being affected by COVID-19.
5. Conclusion
This is the first report on the health-related quality of life of children with T1D in Kuwait during the COVID-19 era. Parents' or caregivers' experience of caring for their children was negative, as they worried, and reported poorer HRQoL compared with their children's perceptions. There is a need to empower healthcare professionals to support parents and caregivers of children with chronic diseases such as T1D in promoting self-management, enhancing physical and psychological wellbeing, treatment adherence, and continuous health education during pandemics of any kind. Longitudinal studies on the effect of the COVID-19 pandemic on children and youth with T1D are necessary to enhance our understanding of the effects of the pandemic on disease management, glycemic control, day-to-day activities, and patients' wellbeing. Future studies could also add new insights by comparing the experiences of children and adolescents with and without diabetes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Committee at the Ministry of Health of Kuwait. Written/verbal consents were provided by legal guardians or next of kin.
Author contributions
DA-A was responsible for planning, designing, data managing, conducting the study, and writing the manuscript. TA, FO, and FA-J collected data and recruited patients. DK participated in directing the reported work, data management, critically reviewed the manuscript, and participated in the discussions. TA, DA-A, and DK carried out data analysis and interpretation of the results. TA, FO, SQ, and FA-J contributed to the writing of the manuscript. HA-K participated in the planning, data management, and conducting of the study. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to acknowledge the children and their families who participated in this study. Furthermore, we would like to acknowledge Kuwait University and Dasman Diabetes Institute for the support provided to the investigators and authors during all phases of this project. We would also like to acknowledge the MAPI institute. Finally, we would like to acknowledge Solveig Argeseanu Cunningham for her expert review of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. (2021) 175:1142–50. doi: 10.1001/jamapediatrics.2021.2482
2. Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. (2020) 174:898–900. doi: 10.1001/jamapediatrics.2020.1619
3. Ravens-Sieberer U, Kaman A, Erhart M, Devine J, Schlack R, Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatry. (2021) 2021:1–11. doi: 10.2139/ssrn.3721508
4. Danne T, Lanzinger S, de Bock M, Rhodes ET, Alonso GT, Barat P, et al. A worldwide perspective on COVID-19 and diabetes management in 22,820 children from the SWEET project: diabetic ketoacidosis rates increase and glycemic control is maintained. Diabetes Technol Ther. (2021) 23:632–41. doi: 10.1089/dia.2021.0110
5. Passanisi S, Pecoraro M, Pira F, Alibrandi A, Donia V, Lonia P, et al. Quarantine due to the COVID-19 pandemic from the perspective of pediatric patients with type 1 diabetes: a web-based survey. Front Pediatr. (2020) 2020:491. doi: 10.3389/fped.2020.00491
6. Al-Abdulrazzaq D, Alkandari A, Alhusaini F, Alenazi N, Gujral UP, Narayan KMV, et al. Higher rates of diabetic ketoacidosis and admission to the paediatric intensive care unit among newly diagnosed children with type 1 diabetes in Kuwait during the COVID-19 pandemic. Diabetes Metab Res Rev. (2022) 38:e3506. doi: 10.1002/dmrr.3506
7. McGurnaghan SJ, Weir A, Bishop J, Kennedy S, Blackbourn LA, McAllister DA, et al. Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland. Lancet Diab Endocrinol. (2021) 9:82–93. doi: 10.1016/S2213-8587(20)30405-8
8. Diedisheim M, Dancoisne E, Gautier J-F, Larger E, Cosson E, Fève B, et al. Diabetes increases severe COVID-19 outcomes primarily in younger adults. J Clin Endocrinol Metab. (2021) 106:e3364–e8. doi: 10.1210/clinem/dgab393
9. Solowiejczyk J. The family approach to diabetes management: Theory into practice toward the development of a new paradigm. Diab Spectrum. (2004) 17:31–6. doi: 10.2337/diaspect.17.1.31
10. Control D, Group CTR. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New Engl J Med. (1993) 329:977–86. doi: 10.1056/NEJM199309303291401
11. Rochmah N, Faizi M, Hisbiyah Y, Triastuti IW, Wicaksono G, Endaryanto A. Quality of life differences in pre-and post-educational treatment in type 1 diabetes mellitus during COVID-19. Diab Metab Synd Obesity Targets Therapy. (2021) 14:2905. doi: 10.2147/DMSO.S313575
12. Arab-Zozani M, Hashemi F, Safari H, Yousefi M, Ameri H. Health-related quality of life and its associated factors in COVID-19 patients. Osong Public Health Res Perspect. (2020) 11:296. doi: 10.24171/j.phrp.2020.11.5.05
13. Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL. The PedsQL™ in type 1 and type 2 diabetes: reliability and validity of the Pediatric Quality of Life Inventory™ generic core scales and type 1 diabetes module. Diabetes Care. (2003) 26:631–7. doi: 10.2337/diacare.26.3.631
14. Varni JW, Delamater AM, Hood KK, Driscoll KA, Wong JC, Adi S, et al. Diabetes management mediating effects between diabetes symptoms and health-related quality of life in adolescents and young adults with type 1 diabetes. Pediatr Diabetes. (2018) 19:1322–30. doi: 10.1111/pedi.12713
16. Abdul-Rasoul M, AlOtaibi F, Abdulla A, Rahme Z, AlShawaf F. Quality of life of children and adolescents with type 1 diabetes in Kuwait. Medical principles and practice. (2013) 22:379–84. doi: 10.1159/000347052
17. Abdul-Rasoul M, AlOtaibi F, AlMahdi M, AlKandari H. Reliability and validity of the Arabic version of the PedsQLTM 4.0 generic ore scales and PedsQLTM 3.0 diabetes module. J Diab Mellit. (2012) 2:301–7. doi: 10.4236/jdm.2012.23047
18. DiMeglio LA, Acerini CL, Codner E, Craig ME, Hofer SE, Pillay K, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatr Diab. (2018) 27:105–14. doi: 10.1111/pedi.12737
19. Varni JW, Seid M, Rode C. PedsQL: Measurement model for the pediatric quality of life inventory Version. Med Care. (1998) 4:126–39. doi: 10.1037/t65932-000
20. Kalyva E, Malakonaki E, Eiser C, Mamoulakis D. Health-related quality of life (HRQoL) of children with type 1 diabetes mellitus (T1DM): self and parental perceptions. Pediatr Diabetes. (2011) 12:34–40. doi: 10.1111/j.1399-5448.2010.00653.x
21. Varni JW,. Linguistic validation of the PedsQL—a Quality of Life Questionnaire. Mapi Research Institute (2002). Available online at: https://www.pedsql.org/PedsQL-Linguistic-Validation-Guidelines.doc (accessed August, 2022).
22. Boodai SA, Reilly JJ. Health related quality of life of obese adolescents in Kuwait. BMC Pediatr. (2013) 13:1–5. doi: 10.1186/1471-2431-13-105
23. AlBuhairan F, Nasim M, Al Otaibi A, Shaheen NA, Al Jaser S, Al Alwan I. Health related quality of life and family impact of type 1 diabetes among adolescents in Saudi Arabia. Diabetes Res Clin Pract. (2016) 114:173–9. doi: 10.1016/j.diabres.2016.01.001
24. Nardi L, Zucchini S, D'Alberton F, Salardi S, Maltoni G, Bisacchi N, et al. Quality of life, psychological adjustment and metabolic control in youths with type 1 diabetes: a study with self-and parent-report questionnaires. Pediatr Diabetes. (2008) 9:496–503. doi: 10.1111/j.1399-5448.2008.00414.x
25. Graue M, Wentzel-Larsen T, Hanestad B, Båtsvik B, Søvik O. Measuring self-reported, health-related, quality of life in adolescents with type 1 diabetes using both generic and disease-specific instruments. Acta Paediatr. (2003) 92:1190–6. doi: 10.1111/j.1651-2227.2003.tb02483.x
26. Odeh R, Gharaibeh L, Daher A, Kussad S, Alassaf A. Caring for a child with type 1 diabetes during COVID-19 lockdown in a developing country: Challenges and parents' perspectives on the use of telemedicine. Diabetes Res Clin Pract. (2020) 168:108393. doi: 10.1016/j.diabres.2020.108393
Keywords: children, type 1 diabetes, health-related quality of life, PedsQLTM Diabetes Module, COVID-19
Citation: Al-Abdulrazzaq D, Khalifa D, Alqaisi T, Al-Juailla F, Othman F, Qabazard S and Al-Kandari H (2022) Health-related quality of life of children and adolescents with type 1 diabetes during the COVID-19 pandemic in Kuwait. Front. Public Health 10:1056967. doi: 10.3389/fpubh.2022.1056967
Received: 29 September 2022; Accepted: 25 November 2022;
Published: 23 December 2022.
Edited by:
Pei Wang, Fudan University, ChinaReviewed by:
Arlette Setiawan, Universitas Padjadjaran, IndonesiaValeria Di Onofrio, University of Naples Parthenope, Italy
Copyright © 2022 Al-Abdulrazzaq, Khalifa, Alqaisi, Al-Juailla, Othman, Qabazard and Al-Kandari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dalia Al-Abdulrazzaq,  ZGFsaWEuYWxhYmR1bHJhenphcUBrdS5lZHUua3c=
ZGFsaWEuYWxhYmR1bHJhenphcUBrdS5lZHUua3c=
†ORCID: Dalia Al-Abdulrazzaq orcid.org/0000-0002-4613-865X
 Dalia Al-Abdulrazzaq
Dalia Al-Abdulrazzaq Doaa Khalifa2
Doaa Khalifa2 Fatima Al-Juailla
Fatima Al-Juailla Fouzeyah Othman
Fouzeyah Othman