- 1Tasmanian School of Medicine, College of Health and Medicine, University of Tasmania, Hobart, TAS, Australia
- 2Public Health Services, Department of Health, Hobart, TAS, Australia
Massive open online courses (MOOCs) have emerged as an innovative educational technology relevant to and affecting higher education, professional development, and lifelong learning. This paper introduces the principles of MOOCs and reviews the development of these platforms over time. We reflect upon the considerable investment by institutions to develop, deliver and promote such courses, particularly in public health. While open to interpretation, the inherent power, influence, and effectiveness of MOOCs is unquestionable. The potential contribution of MOOCs to public health education is immense, with almost universal reach and access. However, apart from research into participant engagement and knowledge, MOOC-related research and evaluation continue to lag with the rapid proliferation of these courses in response to emerging challenges, as seen with the Coronavirus Disease 19 (COVID-19) pandemic. This makes analyzing the contribution of MOOCs to public health education, health promotion and community programs challenging. This perspective article provides a robust rationale for the necessity of MOOCs and their utility in upskilling health professionals and the general public. It builds on current knowledge to comprehensively explore the factors influencing the development, and application of MOOCs.
Introduction
Public health is an interdisciplinary field concerned with understanding and influencing the population's health and wellbeing. While public health professionals assume various roles and responsibilities, the workforce must profoundly understand population health, including the social and ecological determinants of health. Public health education seeks to advance knowledge of public health evidence and interventions and aims to develop skills to address public health issues and influence change at a population level. Most public health schools offer interdisciplinary and multidisciplinary programs to support career preparation therefore drawing on and developing partnerships with non-traditional public health disciplines is necessary to tackle complex problems, with recent examples from engineering in humanitarian action (1) and urban health (2). However, there is considerable variation in public health competency frameworks and curricula content worldwide (3). This is reflective of geographic and cultural variability and the responsiveness of educational institutions and governments to factors impacting public health globally. By leveraging the efficiencies in content delivery, massive open online courses (MOOCs) can promote awareness of public health challenges as well as global issues. According to Meinert et al. (4), MOOCs may be a sustainable method for increasing citizen engagement in global concerns and health-related issues devised around health behavior research. Organizational MOOCs aimed at increasing knowledge and self-management of health issues can potentially improve health promotion and literacy (5, 6). High-quality content can be delivered to a large audience and updated with evidence from the latest scientific studies, which is not always possible with face-to-face instruction.
The Coronavirus Disease 19 (COVID-19) pandemic has stretched many health services across the globe. Given the rising costs of health and social care systems in many countries (7, 8), there is a need for new, improved, and accessible web-based resources and information to assist with health prevention and care. The flexible MOOC platform complements the increasing move to working from home, supported by many organizations and sectors since the COVID-19 pandemic. In addition, MOOCs provide on-demand learning opportunities in a rapidly changing workplace (9), making them attractive to small organizations that may lack the scale to invest in formal in-house training (10). The personal and professional gains are self-evident from MOOC participation and are well-described by authors such Blum et al. (11) and Chesniak et al. (12). We recognize the need for more rigorous research on MOOCs and their effectiveness and intended outcomes in the public health context. The aim of this perspective article is to review the current application of MOOCs across various disciplines and consider emerging trends and future potential for MOOCs in public health education.
The evolution of MOOCs
The original aim of the MOOC was to offer a self-organized learning experience in a field of study facilitated by experts in the area (13). It was introduced over 20 years ago as a revolution in education for its “disruptive content delivery method” by testing new pedagogical approaches and technological tools (13). MOOCs addressed potential barriers to educational engagement, by offering free access, and flexibility through their information and communications technologies (ICT)-based structure (14, 15). A course could include a few participants to as many as several thousand, actively engaging at their convenience (16). Learning on an online platform represented an alternative to face-to-face instruction while still offering collaborative learning with interactive forums. MOOCs have since grown steadily in popularity, driven by expanding internet access (17, 18). In 2019, an estimated 110 million individuals enrolled in an online course (19, 20), doubling to 220 million in 2021 (21). Consequently, millions of learners have engaged in non-traditional learning platforms promoting their new skills by signaling these learning successes to a broader community.
Since their inception, MOOCs have evolved into two types of courses: the Connectivist MOOC (cMOOC) and the Extended MOOC (xMOOC) (22). The main focus of cMOOCs is the creation and generation of knowledge, whereas the xMOOCs are content-based and focus on disseminating knowledge (23). Variations exist around the delivery of knowledge and skills development, depending on the discipline. While conceptual and quantitative descriptive studies of MOOCs in the disciplines of education, computer science, and engineering dominate, the educational approaches are practice-based and readily converge with the science and art of public health (24). For example, branches of public health, such as epidemiology, lend themselves to independent study. In contrast, other public health branches, such as biostatistics, which are simulation-based or have short answers, may use machine-scoreable assessments (25). Some MOOCs are designed to create an authentic learning experience by allowing participants to develop projects or blogs with other students to form social learning groups (26). McAuley et al. (14) proposed that the MOOC model would provide an ecosystem for exploring how individuals may develop the knowledge, skills, and attitudes they need to thrive in an economy. The model would also allow individuals the opportunity to join the community of practice at their own pace (16). This vision reflected the pedagogical principles of professional development, independence, and lifelong learning.
MOOCs in public health education
Many universities and colleges worldwide use MOOCs to provide a “flipped classroom” model for improved learning (27, 28). This approach has seen MOOCs gain traction in healthcare education, including medicine, pharmacy, and nursing (29–32). The MOOC technology has been a welcome method to supplement and augment medical training and inter-professional learning, which was necessary during the COVID-19 pandemic (33, 34). The COVID-19 pandemic has increased the demand for and provision of public health education.
The numerous Australian, US and UK universities that supported the emergence of MOOCs continue to provide central coordination and multiple MOOC offerings (35). The Organization for Economic Co-operation and Development (OECD) noted that the introduction of MOOCs undoubtedly generated a potential alternative pathway to traditional higher education qualifications (36). They have also shown to be an impetus for innovation, facilitating new approaches in education, including healthcare, by allowing diverse organizations to enter the higher education market (37). Figures from the MOOC aggregator site “Class Central” indicate that more than 900 universities globally launched free online courses using popular platforms such as FutureLearn and Coursera in 2021, with many governments launching their country-specific MOOC platforms (38). However, substantial variations of content and complexity exist between these platforms, particularly in course specialization and degrees and certificates awarded for courses (39).
A review of MOOCs in health education during the COVID-19 lockdown in 2021 by Dolores et al. (40) reported that 117 MOOCs, delivered by different platforms, were targeted at the general population, with the majority aimed at health promotion, food and nutrition, and mental health. Content delivery using MOOCs could provide a flexible modality to reflect the dynamic nature of public health if locally relevant (41). In addition, the potentially high number of course participants presents an opportunity to bring together a uniquely diverse group of people, allowing course cohorts to obtain a global and systems perspective which is an important component of public health education (42, 43). We note limited research examining the value of MOOCs as a platform for the delivery of public health education, reflected by a paucity of literature other than the reporting the numbers of participants.
Future trends of MOOCs in public health education
The earliest MOOC developments in public health education were recorded by the Johns Hopkins Bloomberg School of Public Health (JHSPH) during its 2012–2013 academic year. The school's decision to offer MOOCs was based on its already extensive experience with online and open education (44). This innovative approach served as a marketing element for JHSPH, offering a taster experience for a full degree program and attracting those ready and able to pursue formal coursework. In addition, it developed the potential to forge new partnerships with other universities and organizations, highlighting the growing interest in public health outside traditional degree programs.
MOOCs have materialized as effective tools for scaling-up education (45). McAuley et al. (14), viewed MOOCs as a reflection of a society where citizens are active agents in knowledge creation and dissemination processes. This implies that “digital citizenry” reflects the ability of citizens to connect, innovate, and reconfigure the known into new knowledge (14). MOOCs can also complement more traditional courses by simultaneously propagating information to many participants. McAuley and his team (14) had foreseen that training and educating large numbers of people in digital learning would be effective tools to produce change on a large scale. MOOCs offer a platform to support the tenet of public health promotion, which endeavors to connect people to improve health and wellbeing.
The personalization of MOOCs is a growing trend aimed at improving learners' individual experiences (46). Researchers such as Lambert (47) note that many organizations and educators have created public health programs for disadvantaged groups and communities to provide supportive, equitable, and targeted education. Examples include research training for health professionals in low- and middle-income countries (LMICs) (48) and One Health education in Kakuma refugee camp in Kenya (49). MOOCs can be directed to help the most vulnerable, such as the “Talk-to-Me” MOOC intervention for suicide prevention and mental health education among tertiary students (50). MOOC content developed in collaboration with stakeholders, a design process coined as co-creation, offers a viable method of developing course material tailored to the needs of a specific population group, such as the MOOC to Improve Digital Health Literacy in Pregnant and Lactating Women (51). Digital health literacy (DHL) has been referred to as a “super social determinant of health,” (52) and the use of MOOCs to improve DHL skills of health care professionals (53) can be an effective strategy, with an opportunity to employ the process of co-creation in its design and development (54).
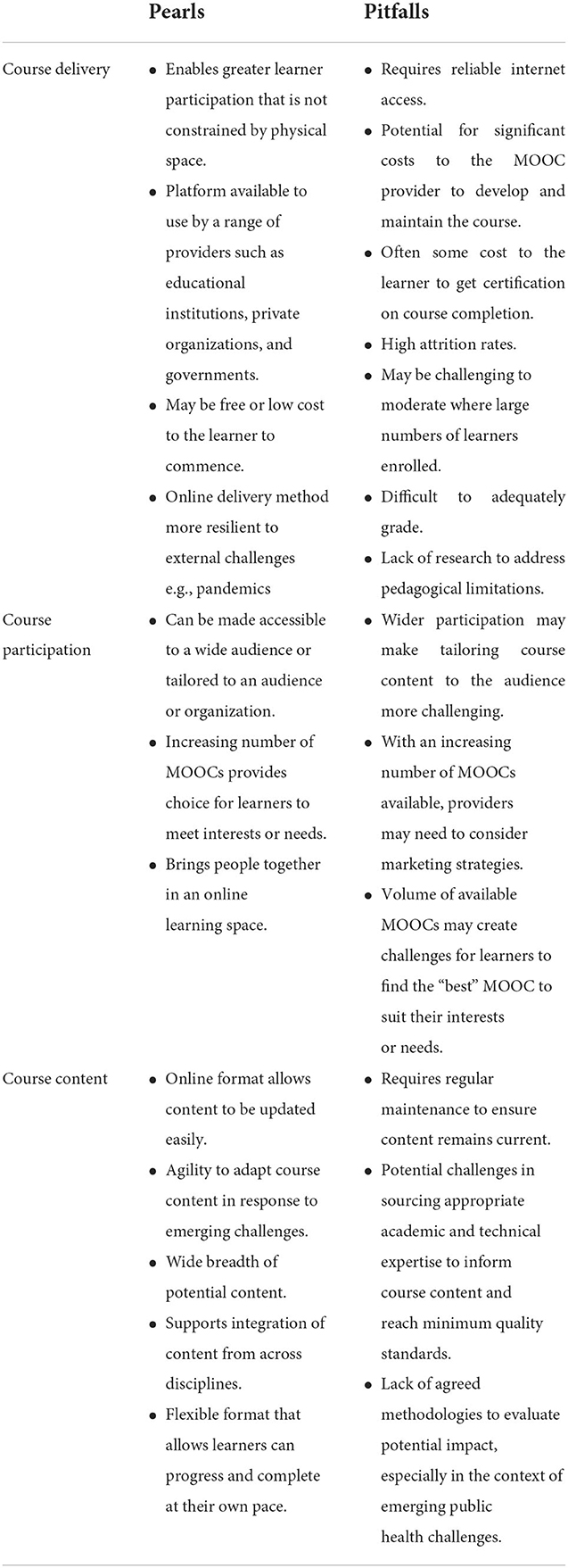
Targeted training outside traditional degree programs facilitates higher efficiency for higher education systems, including continuing professional development programs (19). This often fulfills labor markets' needs and improves economic diversification and competitiveness by retaining workforce (9, 55). For example, during the COVID-19 crisis, universities offered new micro-credentialing in public health for school-based professionals (56), and the Imperial College of London School of Public Health delivered MOOCs that were freely available to all NHS staff (57). MOOCs created to support skill development have proven to be popular, with higher enrolment and completion rates for courses that target work-related skills (58, 59) compared to the low completion rates of courses with more general content (60). However, the limited research in this area suggests the true effect of such credentials in various labor markets is unknown (61). Nevertheless, digital badges, micro-credentials, and certificates are promoted as an alternative to the more traditional credentials offered by higher education institutions (19). Fees associated with the more advanced MOOCs that offer certificates and micro-credentialing appear to be a significant departure from the original aim of MOOCs. Yet these changes have extended the reach of traditional higher education institutes to new students across the globe (62). Despite the challenges and complex nature of content, design and delivery of public health MOOCs, the desire to share knowledge and expertise is evident. We summarize our pearls and pitfalls in Table 1.
MOOCs for public health professionals
Health professionals increasingly access MOOCs to support their professional development (63). MOOCs offer a platform for high-quality reskilling and upskilling opportunities, particularly those targeted at continuing professional education (64) as well as supporting job seekers to attain sustainable employment opportunities. Globally, public health systems play a crucial role in addressing workforce retention by preparing for evolving capability needs (65), and continuing education opportunities for the public health workforce are essential. For example, MOOCs have leveraged access to education by healthcare workers in many LMICs, where they lack access to quality improvement training and basic skills in healthcare delivery (66, 67).
The interdisciplinary field of public health does not have a single preferred training modality (68), therefore, the scope and modality in MOOC preferences are influenced by design, delivery, and organizational support. Archer et al. (68) found that programs could influence the engagement of full-time employees by designing courses with clearly articulated purposes and benefits. The public health workforce was generally more engaged in completion if the course certification was aligned to competencies; the course content had practical application and was shorter, allowing them to complete the course quickly. Universities around the world reported high response rates to interest in public health and the necessity to gain professional public health skills. The impact of the COVID-19 pandemic on employers left many to reconsider their training choice and mode of upskilling and reskilling (69–71). For many countries, providing public health information and upskilling healthcare workers to all disciplines was necessary, as the COVID-19 emergency response required a surge in staff for pandemic preparedness, education, planning, logistics, and operations (72–74). The pandemic has been a powerful test of the online learning model and of organizational ability to respond quickly and effectively by expanding the range and delivery of training programs, from undergraduate programs to community-based health promotion education (38, 75).
Local public health MOOCs–An example from Tasmania
The COVID-19 pandemic challenged health systems globally, requiring them to respond with an integrated, multidisciplinary approach to preparedness, prevention, and management. Despite a whole of government response, Australia's federal division of power allowed policy formulation and innovation to occur at the state level, reflecting the impact of the pandemic for local communities. Tasmania's COVID-19 response aimed to contain the virus, minimize transmission, and protect vulnerable people and groups. This necessitated a range of evolving measures, including lockdowns and restricted travel, which had significant consequences on individuals and communities, including economic, social and psychological impacts.
The island state of Tasmania is isolated from the rest of Australia, with a limited public health workforce. It soon became evident that building a robust, skilled workforce was essential to an effective response. To advance existing expertise, close skill gaps and build surge capacity, creative solutions were explored to target and engage a large audience and deliver online training. As a result of agile leadership, a public health MOOC was developed in collaboration with the University of Tasmania and Public Health Services, Department of Health Tasmania (76). This MOOC aimed to provide initial training in contact tracing and active surveillance to support the development of a surge-ready workforce in Tasmania. It included an introduction to COVID-19, a summary of its epidemiology and prevention, and an overview of the public health response in Tasmania, including local systems and processes. These skills were applied through case studies and mock contact tracing interviews.
Global public health MOOCs
One of the most successful MOOCs during the COVID-19 pandemic was delivered by the World Health Organization (WHO) through their interactive platform, OpenWHO (77). OpenWHO was developed by the WHO Health Emergencies Programme in partnership with Hasso Plattner Institute (HPI) in 2017 (78). It offered a range of life-saving content on various disease outbreaks and general material for frontline responders, healthcare workers and the general public. Before the COVID-19 pandemic, OpenWHO provided 18 different disease courses; by 2021, there were 38 courses focused on the COVID-19 response alone (79). Additionally, the number of learners increased from 140,000 users in 2019 to 7 million enrolments, with a significant increase in female engagement and diversity in the geographical location and user characteristics (80).
The OpenWHO course creation process is unique, devised to be current and up-to-date with acute health emergencies, with WHO technical experts providing resources and guidance online in real-time (81). Course material is free, with unlimited access, and delivered in low-bandwidth formats accessible via mobile or desktop devices. In addition, OpenWHO courses are offered in multilingual formats and local languages of communities affected by particular outbreaks, including one in sign language (82). George et al. (83) acknowledge that this has facilitated “the rapid, global sharing of life-saving knowledge to the audiences who need it, when they need it, in formats and languages they can understand.”
Similarly, other United Nations (UN) agencies and programs responded to the COVID-19 pandemic with innovative learning solutions for individuals, organizations and institutions via its many platforms. UN agencies and programs produce various courses in partnership with numerous organizations, with courses offered through different platforms, as seen through the work of The United Nations Institute for Training and Research (UNITAR) and United Nations Information Centers(UNRIC) (84, 85). The benefit of partnership-based programs is the possibility of combining discipline experts in training and development with experts in substantive areas and local contexts. Courses are accessible to the public and professionals in different languages and free of charge. Some courses run several times a year, and a few provide certification. Concurrently, the partnerships provide a mechanism to deliver a broad range of contemporary public health content, including sustainable development and human rights, climate change, nutrition and food security, young people, and their mental health (84, 85).
Conclusion
Open online learning courses have grown substantially in recent years, with millions of new users enrolled (18). Class Central recorded 194,000 listed courses in the past 10 years, with micro-credentialing and MOOC-based degrees doubling in numbers from previous years (18). Our local experience of the COVID-19 pandemic demonstrated the opportunity to be agile in our response and adapt courses to local contexts and emerging needs, aligning them with participants' needs and experiences, and technological and financial resources. MOOCs developed in response to emerging challenges in public health require content to be regularly evaluated, updated, and improved. We have outlined the complex nature of content, design and delivery of public health MOOCs; however, it is evident that there is a need for agreed methodologies and guidelines that support robust evaluation to ensure homogeneity between studies. This includes standardization of reporting and process of data and a focus on evaluating outcomes, including knowledge, competencies and skills to examine MOOCs' benefits, effectiveness and impact in public health. More targeted research is required to better understand the role of MOOCs in public health education and health improvement to maximize their potential impact, especially in the context of emerging challenges.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SB and KM contributed to the conception and design of the article. SB wrote the first draft of the manuscript. KM and RP wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This research was awarded publication funding from the Tasmanian School of Medicine Research Committee.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Smith J, Tran AL, Compston P. Review of humanitarian action and development engineering education programmes. Eur J Eng Educ. (2020) 45:249–72. doi: 10.1080/03043797.2019.1623179
2. Hudson L, Wolff A, Gooch D, Van Der Linden J, Kortuem G, Petre M, et al. Supporting urban change: using a MOOC to facilitate attitudinal learning and participation in smart cities. Comput Educ. (2019) 129:37–47. doi: 10.1016/j.compedu.2018.10.012
3. Coombe L, Severinsen C, Robinson P. Practical competencies for public health education: a global analysis. Int J Public Health. (2020) 65:1159–67. doi: 10.1007/s00038-020-01459-3
4. Meinert E, van Velthoven M, Alturkistani A, Murray KA, Sabatier P, Car J. Cost measurements in production and delivery of a massive open online course (MOOD) for teaching the relationship between human health and climate change: a case study. IADIS IJWI. (2019) 17:14–27. doi: 10.33965/ijwi_2019172102
5. Zubala A, Lyszkiewicz K, Lee E, Underwood LL, Renfrew MJ, Gray NM. Large-scale online education programmes and their potential to effect change in behaviour and practice of health and social care professionals: a rapid systematic review. Interact Learn Environ. (2019) 27:797–812. doi: 10.1080/10494820.2018.1465438
6. Liyanagunawardena TR, Williams SA. Massive open online courses on health and medicine: review. J Med Internet Res. (2014) 16:e191. doi: 10.2196/jmir.3439
7. World Health Organization (WHO). Public Spending on Health: A Closer Look at Global Trends. (2019). Available online at: https://apps.who.int/iris/bitstream/handle/10665/276728/WHO-HIS-HGF-HF-WorkingPaper-18.3-eng.pdf (accessed April 22, 2022).
8. World Health Organization (WHO). Countries are Spending More on Health, But People are Still Paying Too Much Out of Their Own Pockets. (2019). Available online at: https://www.who.int/news-room/detail/20-02-2019-countries-are-spending-more-on-health-butpeople-are-still-paying-too-much-out-of-their-own-pockets (accessed June 2, 2022).
9. Santandreu Calonge D, Aman Shah M, Riggs K, Connor M. MOOCs and upskilling in Australia: a qualitative literature study. Cogent Educ. (2019) 6:1687392. doi: 10.1080/2331186X.2019.1687392
10. Hamori M. MOOCs at work: what induces employer support for them? Int J Hum Resour Manag. (2021) 32:4190–214. doi: 10.1080/09585192.2019.1616593
11. Blum ER, Stenfors T, Palmgren PJ. (2020). Benefits of massive open online course participation: deductive thematic analysis. JMIR. (2020) 22:e17318. doi: 10.2196/17318
12. Chesniak OM, Drane D, Young C, Hokanson SC, Goldberg BB. Theory of change models deepen online learning evaluation. Eval Program Plann. (2021) 88:101945. doi: 10.1016/j.evalprogplan.2021.101945
13. Rambe P, Moeti M. Disrupting and democratizing higher education provision or entrenching academic elitism: towards a model of MOOCs adoption at African universities. Educ Technol Res Dev. (2017) 65:631–51. doi: 10.1007/s11423-016-9500-3
14. McAuley A, Stewart B, Siemens G, Cormier D. Massive open online courses. Digital ways of knowing and learning The MOOC model for digital practice University of Prince Edward Island (Hrsg) Charlottetown, Canada. (2010). Available online at: https://www.oerknowledgecloud.org/archive/MOOC_Final.pdf (accessed on April 2, 2022).
15. Yuan L, Powell S. MOOCs Open Education: Implications for Higher Education. A white paper, JISC CETIS. (2013). Available online at: http://publications.cetis.ac.uk/2013/667 (accessed April 12, 2022).
16. Bonafini F, Chae C, Park E, Jablokow K. How much does student engagement with videos and forums in a MOOC affect their achievement? Online Learn J. (2017) 21:223–40. doi: 10.24059/olj.v21i4.1270
17. Zhu MN, Sari AR, Lee MM. A comprehensive systematic review of MOOC research: research techniques, topics, and trends from 2009 to 2019. Etr D-Educ Tech Res. (2020) 68:1685–710. doi: 10.1007/s11423-020-09798-x
18. Liu C, Zou D, Chen X, Xie H, Chan WH. A bibliometric review on latent topics and trends of the empirical MOOC literature (2008–2019). Asia Pac Educ Rev. (2021) 22:515–34. doi: 10.1007/s12564-021-09692-y
19. Kato S, Galán-Muros V, Weko T. The Emergence of Alternative Credentials. OECD Education Working Paper. (2020). Available online at: https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=EDU/WKP(2020)4&docLanguage=En (accessed April 12, 2022).
20. Shah D. By The Numbers: MOOCs in 2019. Class Central. (2018). Available online at: https://www.classcentral.com/report/tag/mooc-roundup-2019/ (accessed June 5, 2022).
21. Shah D. Class Central's Best Online Courses of the Year (2021 Edition) Class Central. (2021). Available online at: https://www.classcentral.com/report/best-free-online-courses-2021/ (accessed June 23, 2022).
22. Knox J. Massive open online courses (MOOCs). In M. A. Peters (ed.), Encyclopaedia of educational theory and philosophy. Singapore: Springer (2015). Available online at: https://link.springer.com/referenceworkentry/10.1007/978-981-287-588-4_219
23. Margaryan A, Bianco M, Littlejohn A. Instructional quality of massive open online courses (MOOCs). Comput Educ. (2015) 80:77–83. doi: 10.1016/j.compedu.2014.08.005
24. Sezgin S, Sevim Cirak N. The role of MOOCs in engineering education: an exploratory systematic review of peer-reviewed literature. Comput Appl Eng Educ. (2021) 29:950–68. doi: 10.1002/cae.22350
25. Shah D. A Decade of MOOCs: A Review of MOOC Stats Trends in 2021 Class Central. (2021). Available online at: https://www.classcentral.com/report/moocs-stats-and-trends-2021/ (accessed June 23, 2022).
26. Fasimpaur K. Massive and open. Learn Lead Technol. (2013) 40:12–7. Available online at: https://files.eric.ed.gov/fulltext/EJ1015163.pdf (accessed June 23, 2022).
27. Muñoz-Merino PJ, Ruipérez-Valiente JA, Delgado Kloos C, Auger MA, Briz S, De Castro V, et al. Flipping the classroom to improve learning with MOOCs technology. Comput Appl Eng Educ. (2017) 25:15–25. doi: 10.1002/cae.21774
28. Kloos CD, Muñoz-Merino PJ, Alario-Hoyos C, Ayres IE, Fernández-Panadero C. Mixing and blending MOOC technologies with face-to-face pedagogies. In: IEEE Global Engineering Education Conference (EDUCON). Tallinn (2015). doi: 10.1109/EDUCON.2015.7096090
29. Goldberg L, Crocombe L. Advances in medical education and practice: role of massive open online courses. Adv Med Educ Pract. (2017) 8:603–9. doi: 10.2147/AMEP.S115321
30. Maxwell WD, Fabel PH, Diaz V, Walkow JC, Kwiek NC, Kanchanaraksa S, et al. Massive open online courses in US healthcare education: practical considerations and lessons learned from implementation. Curr Pharm Teach Learn. (2018) 10:736–43. doi: 10.1016/j.cptl.2018.03.013
31. Swigart V, Liang Z. Digital resources for nursing education: open courseware and massive open online courses. Int J Nurs Sci. (2016) 3:307–13. doi: 10.1016/j.ijnss.2016.07.003
32. Rao R, Hawkins M, Ulrich T, Gatlin G, Mabry G, Mishra C. The evolving role of public health in medical education. Front Public Health. (2020) 8:251. doi: 10.3389/fpubh.2020.00251
33. Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In vivo. (2020) 34:1603–11. doi: 10.21873/invivo.11950
34. Mahajan R, Gupta P, Singh T. Massive open online courses: concept and implications. Indian Pediatr. (2019) 56:489–95. doi: 10.1007/s13312-019-1575-6
35. Longstaff E. The prehistory of MOOCs: inclusive and exclusive access in the cyclical evolution of higher education. J Organ Transform Soc Chang. (2014) 11:164–84. doi: 10.1179/1477963314Z.00000000028
37. Silén-Lipponen M, Koponen L, Korhonen U, Myllymäki M. Using a massive open online course (MOOC) to promote infection prevention and control learning in healthcare education. Int J Infect Control. (2022) 18:1–9. doi: 10.3396/ijic.v18.21667
38. Shah D, Pickard L, Ma R. Massive List of MOOC Platforms Around The World in 2022. (2022). Available online at: https://www.classcentral.com/report/mooc-platforms/ (accessed June 23, 2022).
39. Ayoub A, Amin R, Wani ZA. Contribution of developed countries towards MOOCs: an exploration and assessment from a representative platform Coursera. AAOU. (2020) 15:251–62. doi: 10.1108/AAOUJ-03-2020-0016
40. Dolores-Maldonado G, Cañari-Casaño JL, Montero-Romainville R, Malaga G. Massive open online course (MOOC) opportunities in health education (HE) in a mandatory social isolation context. F1000Res. (2022) 10:322. doi: 10.12688/f1000research.52049.2
41. Firmansyah M, Timmis S. Making MOOCs meaningful and locally relevant? investigating IDCourserians-an independent, collaborative, community hub in Indonesia. Res Pract Technol Enhanc Learn. (2016) 11:11. doi: 10.1186/s41039-016-0032-6
42. Kim W, Watson W, Watson S. Student perceptions of learning in three MOOCs: a case study of attitudinal change instruction. Educ Media Int. (2016) 53:168–83. doi: 10.1080/09523987.2016.1236890
43. Coronado F, Beck AJ, Shah G, Young JL, Sellers K, Leider JP. Understanding the dynamics of diversity in the public health workforce. J Public Health Manag Pract. (2020) 26:389–92. doi: 10.1097/PHH.0000000000001075
44. Gooding I, Klaas B, Yager JD, Kanchanaraksa S. Massive open online courses in public health. Front Public Health. (2013) 1:59. doi: 10.3389/fpubh.2013.00059
45. OECD. Innovating Education and Educating for Innovation: The Power of Digital Technologies and Skills. Paris: OECD Publishing (2016).
46. Sunar AS, Abdullah NA, White S, Davis H. Personalization in MOOCs: a critical literature review. In: International Conference on Computer Supported Education, Springer. (2015). Available online at: https://link.springer.com/chapter/10.1007/978-3-319-29585-5_9 (accessed July 14, 2022).
47. Lambert SR. Do MOOCs contribute to student equity and social inclusion? a systematic review 2014–18. Comput Educ. (2020) 145:103693. doi: 10.1016/j.compedu.2019.103693
48. Launois P, Maher D, Certain E, Ross B, Penkunas MJ. Implementation research training for learners in low- and middle-income countries: evaluating behaviour change after participating in a massive open online course. Health Res Policy Syst. (2021) 19:59. doi: 10.1186/s12961-021-00703-3
49. Bolon I, Mason J, O'Keeffe P, Haeberli P, Adan HA, Karenzi JM, et al. One health education in Kakuma refugee camp (Kenya): from a MOOC to projects on real world challenges. One Health. (2020) 10:100158. doi: 10.1016/j.onehlt.2020.100158
50. Milbourn B, Black MH, Afsharnejad B, Snyman Z, Baker-Young E, Thompson C, et al. The “Talk-to-Me” MOOC intervention for suicide prevention and mental health education among tertiary students: protocol of a multi-site cross-over randomized controlled trial. Contemp Clin Trials. (2022) 112:106645. doi: 10.1016/j.cct.2021.106645
51. Álvarez-Pérez Y, Perestelo-Pérez L, Rivero-Santanta A, Torres-Castaño A, Toledo-Chávarri A, Duarte-Díaz A, et al. Co-creation of massive open online courses to improve digital health literacy in pregnant and lactating women. Int J Environ Res Public Health. (2022) 19:913. doi: 10.3390/ijerph19020913
52. Sieck CJ, Sheon A, Ancker JS, Castek J, Callahan B, Siefer A. Digital inclusion as a social determinant of health. NPJ Digit Med. (2021) 4:1–3. doi: 10.1038/s41746-021-00413-8
53. Longhini J, Rossettini G, Palese A. Digital health competencies among health care professionals: systematic review. J Med Internet Res. (2022) 24:e36414. doi: 10.2196/36414
54. Perestelo-Perez L, Torres-Castaño A, Álvarez-Pérez Y, Toledo Chávarri A. Wägner A, Perello M, et al. IC-health project: development of MOOCs to promote digital health literacy: first results and future challenges. Sustainability. (2020) 12:6642. doi: 10.3390/su12166642
55. Castaño-Muñoz J, Rodrigues M. Open to MOOCs? Evidence of their impact on labour market outcomes. Comput Educ. (2021) 173:104289. doi: 10.1016/j.compedu.2021.104289
56. University University of Montana Contact Tracing Active Monitoring. (2020). Available online at: https://www.umt.edu/public-community-health-sciences/ph-news/new_micro-credential-_public_health_for_school-based_professionals.php (accessed February 16, 2022).
57. Imperial College of London. Imperial has Launched Three Free Massive Open Online Courses (MOOCs) on Public Health for All NHS Staff. (2022). Available online at: https://www.imperial.ac.uk/news/236394/imperial-launches-free-online-public-health/ (accessed June 10, 2022).
58. Radford AW, Robles J, Cataylo S, Horn L, Thornton J, Whitfield K. The employer potential of MOOCs: a mixed-methods study of human resource professionals' thinking on MOOCs. Int Rev Res Open Dis. (2014) 15:1–25. doi: 10.19173/irrodl.v15i5.1842
59. Weinhardt JM, Sitzmann T. Revolutionizing training and education? Three questions regarding massive open online courses (MOOCs). Human Resour Manag Rev. (2019) 29:218–25. doi: 10.1016/j.hrmr.2018.06.004
60. Kizilcec RF, Kambhampaty A. Identifying course characteristics associated with sociodemographic variation in enrollments across 159 online courses from 20 institutions. PLoS ONE. (2020) 15:e0239766. doi: 10.1371/journal.pone.0239766
61. Rivas MJ, Baker RB, Evans BJ. Do MOOCs make you more marketable? An experimental analysis of the value of MOOCs relative to traditional credentials and experience. AERA Open. (2020) 6:1–16. doi: 10.1177/2332858420973577
62. Fain P. On-ramps and off-ramps: Alternative credentials and emerging pathways between education and work: Inside Higher Ed (2018) 1–78.
63. Duncan A, Premnazeer M, Sithamparanathan G. Massive open online course adoption amongst newly graduated health care providers. Adv Health Sci Educ Theory Pract. (2022) 27:919–30. doi: 10.1007/s10459-022-10113-x
64. Monteiro EP, Gomide HP, Remor E. Massive open online course for Brazilian healthcare providers working with substance use disorders: curriculum design. BMC Med Educ. (2020) 20:240. doi: 10.1186/s12909-020-02162-w
65. Dinkin P, Kumar P, Laboissiere M, Parthasarathy R, Lurie E, Wilson M. Care for the Caretakers: Building the Global Public Health Workforce Mckinsey Company. (2022). Available online at: https://www.mckinsey.com/industries/public-and-social-sector/our-insights/care-for-the-caretakers-building-the-global-public-health-workforce?cid=eml-web (accessed June 12, 2022).
66. Scott KW, Dushime T, Rusanganwa V, Woskie L, Attebery C, Binagwaho A. Leveraging massive open online courses to expand quality of healthcare education to health practitioners in Rwanda. BMJ Open Qual. (2019) 8:e000532. doi: 10.1136/bmjoq-2018-000532
67. Nieder J, Nayna Schwerdtle P, Sauerborn R, Barteit S. Massive open online courses for health worker education in low- and middle-income countries: a scoping review. Front Public Health. (2022) 10:891987. doi: 10.3389/fpubh.2022.891987
68. Archer A, Berry I, Bajwa U, Kalda R, Di Ruggiero E. Evidence synthesis-Preferred modalities for delivering continuing education to the public health workforce: a scoping review. Health Promot Chronic Dis Prev Can. (2020) 40:116. doi: 10.24095/hpcdp.40.4.03
69. White I, Rittie T. Upskilling and reskilling: the impact of the COVID-19 pandemic on employers and their training choices. Research Report National Centre for Vocational Education Research (NCVER). (2022). Available online at: https://apo.org.au/node/316205 (accessed June 5, 2022).
70. Engberg M, Bonde J, Sigurdsson ST, Moller K, Nayahangan LJ, Berntsen M, et al. Training non-intensivist doctors to work with COVID-19 patients in intensive care units. Acta Anaesthesiol Scand. (2021) 65:664–73. doi: 10.1111/aas.13789
71. Monteverde E, Bosque L, Klappenbach R, Balina J, Lartigue B, Aran MI, et al. Nonintensivist training to increase the staff capacity of intensive care units during COVID-19 pandemic surge in Argentina. Disaster Med Public Health Prep. (2021) 1–7. doi: 10.1017/dmp.2021.282
72. Longhini J, De Colle B, Rossettini G, Palese A. What knowledge is available on massive open online courses in nursing and academic healthcare sciences education? a rapid review. Nurse Educ Today. (2021) 99:104812. doi: 10.1016/j.nedt.2021.104812
73. Rossettini G, Turolla A, Gudjonsdottir B, Kapreli E, Salchinger B, Verheyden G, et al. Digital entry-level education in physiotherapy: a commentary to inform Post-COVID-19 future directions. Med Sci Educ. (2021) 31:2071–83. doi: 10.1007/s40670-021-01439-z
74. Longhini J, Rossettini G, Palese A. Massive open online courses for nurses' and healthcare professionals' continuous education: a scoping review. Int Nurs Rev. (2021) 68:108–21. doi: 10.1111/inr.12649
75. Scarpetta S, Quintini G, Mullock. Skill Measures to Mobilize the Workforce During the Covid19 Crisis. OECD, Paris. (2020). Available online at: http://www.oecd.org/coronavirus/policy-responses/skill-measures-tomobilise-the-workforce-during-the-Covid-19-crisis-afd33a65/Australia (accessed July 12, 2022).
76. University University of Tasmania COVID-19 Contact Tracing Active Monitoring. (2020). Available online at: https://publichealth.mooc.utas.edu.au/ (accessed July 12, 2022).
77. WHO. Welcome to OpenWHO. (2022). Available online at: https://openwho.org (accessed April 18, 2022).
78. Rohloff T, Utunen H, Renz J, Zhao Y, Gamhewage G, Meinel C. OpenWHO: Integrating Online Knowledge Transfer into Health Emergency Response. EC-TEL (Practitioner Proceedings). (2018). Available online at: http://ceur-ws.org/Vol-2193/paper3.pdf (accessed April 8, 2022).
79. Utunen H, Van Kerkhove MD, Tokar A, O'Connell G, Gamhewage GM, Fall IS. One year of pandemic learning response: benefits of massive online delivery of the world health organization's technical guidance. JMIR Public Health Surveill. (2021) 7:e28945. doi: 10.2196/28945
80. WHO. Now 7 Million Enrolments Strong: Join the OpenWHO.org Learning Community. (2022). Available online at: https://www.who.int/news/item/11-08-2022-now-7-million-enrolments-strong-join-the-openwho.org-learning-community (accessed September 12, 2022).
81. Utunen H, George R, Ndiaye N, Tokar A, Attias M, Gamhewage G. Delivering WHO's life-saving information in real-time during a pandemic through an online learning platform: evidence from global use. Public Health Inform. (2021) 281:969–73. doi: 10.3233/SHTI210322
82. Utunen H, Ndiaye N, Piroux C, George R, Attias M, Gamhewage G. Global reach of an online COVID-19 course in multiple languages on OpenWHO in the first quarter of 2020: analysis of platform use data. J Med Internet Res. (2020) 22:e19076. doi: 10.2196/19076
83. George R, Utunen H, Attias M, Sy M, Ndiaye N, Piroux C, et al. An analysis of the growth in uptake of OpenWHO's online learning resources for COVID-19. Stud Health Technol Inform. (2020) 272:284–7. doi: 10.3233/SHTI200550
84. The United Nations Institute for Training Research. (UNITAR). Available online at: https://www.unitar.org/free-and-open-courses (accessed July 12, 2022).
85. United Nations Information Centres (UNRIC). Available online at: https://unric.org/en/sharpen-your-skills-during-lockdown-with-united-nations-e-learning-courses/ (accessed July 12, 2022).
Keywords: MOOCs, public health, education, professional, workforce, practice
Citation: Bettiol S, Psereckis R and MacIntyre K (2022) A perspective of massive open online courses (MOOCs) and public health. Front. Public Health 10:1058383. doi: 10.3389/fpubh.2022.1058383
Received: 30 September 2022; Accepted: 25 November 2022;
Published: 14 December 2022.
Edited by:
Cathleen Elizabeth Willging, Pacific Institute for Research and Evaluation, United StatesReviewed by:
Priscilla Robinson, La Trobe University, AustraliaGiacomo Rossettini, University of Genoa, Italy
Copyright © 2022 Bettiol, Psereckis and MacIntyre. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvana Bettiol, cy5iZXR0aW9sQHV0YXMuZWR1LmF1
 Silvana Bettiol
Silvana Bettiol Rhea Psereckis2
Rhea Psereckis2