- 1Department of Child and Family Development, San Diego State University, San Diego, CA, United States
- 2Child and Adolescent Services Research Center, San Diego, CA, United States
- 3San Diego State University Research Foundation, San Diego State University, San Diego, CA, United States
- 4Department of Psychology, San Diego State University, San Diego, CA, United States
- 5Institute for Behavioral and Community Health, San Diego State University, San Diego, CA, United States
Background: A large and growing percentage of medically underserved groups receive care at federally qualified health centers (FQHCs). Care coordination is an evidence-based approach to address disparities in healthcare services. A partnered FQHC established a care coordination model to improve receipt and quality of healthcare for patients most at risk for poor health outcomes. This care coordination model emphasizes identification and support of behavioral health needs (e.g., depression, anxiety) and two evidence-based behavioral health programs needs were selected for implementation within the context of this care coordination model. Implementation Mapping is a systematic process for specifying the implementation strategies and outcomes. The current case study describes the application of Implementation Mapping to inform the selection and testing of implementation strategies to improve implementation of two behavioral health programs in a Care Coordination Program at a partnered FQHC.
Methods: We applied Implementation Mapping to inform the development, selection and testing of implementation strategies to improve the implementation of two evidence-based behavioral health programs within a care coordination program at a partnered FQHC.
Results: Results are presented by Implementation Mapping task, from Task 1 through Task 5. We also describe the integration of additional implementation frameworks (The Consolidated Framework for Implementation Research, Health Equity Implementation Framework) within the Implementation Mapping process to inform determinant identification, performance and change objectives development, design and tailoring of implementation strategies and protocols, and resulting evaluation of implementation outcomes.
Conclusions: The current project is an example of real-world application of Implementation Mapping methodology to improve care outcomes for a high priority population that is generalizable to other settings utilizing similar care models and health equity endeavors. Such case studies are critical to advance our understanding and application of innovative implementation science methods such as Implementation Mapping.
Introduction
Profound disparities in accessing and receiving quality healthcare exist for Hispanic or Latino/a individuals, likely contributing to the unequal rates of health issues spanning multiple health areas (e.g., health status, acute and chronic diseases, behavioral health) (1–4). Among these are higher rates of behavioral health conditions and unmet mental health needs when compared to White individuals, conferring vulnerability to further medical and behavioral health problems, preventable morbidity, and societal cost (1, 5). These care disparities have immense public health implications given that the Hispanic or Latino/a population represents the largest and most rapidly growing minority population in California and the United States (6). Efforts to promote equitable and effective care are critical to improve the health of this increasing population and diminish the associated public health impact. Given both the prevalence of behavioral health conditions and substantial public health impact, behavioral health represents a key target within healthcare and health equity efforts.
Federally qualified health centers (FQHCs) play a significant role in the care provision of largely underserved populations, especially Hispanic or Latino/a individuals. FQHCs are funded to provide health care, including primary care and related services, in underserved areas to offset multiple barriers (e.g., geographic, cultural) in care access and utilization. Data suggest that traditionally marginalized individuals, including lower income, racial and ethnic minority or uninsured individuals, comprise a large and increasing portion of those served by FQHCs (7). Further, Hispanic or Latino/a individuals comprise as much as 38% of those served by FQHCs (8, 9), making FQHCs uniquely positioned to promote health and healthcare equity for this population. Importantly, the prevalence of behavioral health conditions among patients are higher in FQHCs compared to other settings (10), with data suggesting that behavioral health conditions such as depression or anxiety were the third most frequent condition seen in FQHCs in 2020 (11). These higher rates of behavioral conditions further underscore the importance of ensuring FQHCs are equipped to address the behavioral health needs of patients served as part of the broader care provision model.
Care coordination is an evidence-based care model that is increasingly implemented to improve care equity, including in FQHCs (12–14). Defined as a person-centered, interdisciplinary approach to integrating healthcare, care coordination models involve case managers to integrate and support patient care, including services from primary care and other care specialists, patient education and treatment management, adjustment, and follow-up (12–14). Care Coordinators identify the specific needs of patients and the services they are receiving to ensure communication across the multiple service providers and to provide patient education and support surrounding treatment goals and recommendations (15–19). Such models can help bridge key care gaps to improve health equity and are increasingly recommended given their effectiveness for patients with co-occurring medical and behavioral health conditions (19, 20). Indeed, a focus on behavioral health needs is a key qualification area for care coordination accreditation models (21). Further, data support the effectiveness of collaborative care models in treating depression among low-income and minority communities, including Hispanic or Latino/a individuals (19, 22).
In 2017, a partnered FQHC implemented a care coordination model to support health promotion among most at-risk patients. Given the location along the US-Mexico border, most patients served are Hispanic or Latino/a, living at or below 200% of the federal poverty line, and/or largely uninsured. Consistent with broader accreditation standards, behavioral health conditions are a qualifying condition for the care coordination program as well as a prioritized health target of the broader organization. Training in evidence-based behavioral health programs is provided as part of this program, including training in two well recognized and federally and locally prioritized evidence-based practices (EBPs), Mental Health First Aid (23–25) and the Adverse Childhood Experiences Screener (26). Mental Health First Aid is an educational program to increase mental health literacy, reduce stigma, and support mental health service navigation. Through didactic training, implementers are provided with a broad knowledge of behavioral health conditions and basic skills in recognizing, approaching and providing initial support for behavioral health problems (23). The Adverse Childhood Experiences Screener is a short questionnaire used to rapidly identify and assess patients that may be at risk for poor health outcomes due to childhood trauma (26). To optimize implementation and effectiveness of these programs and improve both implementation and patient health outcomes, we applied Implementation Mapping to support an effort to expand and support implementation of behavioral health EBPs within the context of this Care Coordination program serving patients with chronic health condition (e.g., Diabetes, hypertension) at the partnered FQHC.
Implementation Mapping
Informed by the Intervention Mapping process and implementation science, Implementation Mapping provides step-by-step guidance for selecting and designing implementation strategies to guide implementation efforts (27). Implementation Mapping details five sequential tasks: (1) conduct a needs assessment; (2) identify implementation outcomes and performance objectives, identify determinants, and create matrices of change objectives; (3) identify and select theoretical methods implementation strategies; (4) create implementation protocols and materials; and (5) evaluate implementation. Consistent with the Intervention Mapping process on which it was based, Implementation Mapping facilitates implementation strategy development and selection that appropriately consider and address contextual needs and determinants, thereby optimizing implementation outcomes (27). In the current case study, Implementation Mapping in conjunction with broader implementation frameworks, including those specifying key health equity domains, will allow for identification of organizational and provider specific strategies to support EBP implementation and consider key implementation and care equity barriers (e.g., stigma, limited awareness) common to implementing behavioral health programs in settings like the partnered FQHC (28–30).
The purpose of this manuscript is to present a case study featuring the application of Implementation Mapping as part of a study that aims to examine the implementation and expansion of an existing, community-initiated health equity effort within a FQHC located along the US-Mexico border. In combination with relevant health equity and determinant implementation frameworks, we utilized the Implementation Mapping process to inform the development, selection and testing of different strategies to expand and enhance the implementation of evidence-based behavioral health programs within the Care Coordination program at a partnered FQHC.
Methods
This study is supported as part of the NIMHD-funded San Diego State HealthLINK Center for Transdisciplinary Health Disparities Research (U54MD012397; PIs: Ayala, Wells) aiming to enhance community capacity and improve infrastructure to advance minority health and health disparities. This project focuses on adapting and developing behavioral health evidence-based practice components and corresponding implementation strategies to expand and facilitate delivery of existing evidence-based behavioral health programs implemented within an existing care coordination model at a FQHC. This study was conducted in collaboration with key stakeholders at the FQHC, particularly those involved with the Care Coordination program, and investigators who have extensive experience working with Hispanic or Latino/a communities (E.A.). These individuals provided input and guidance for the design and selection of implementation strategies. This study was approved from the Institutional Review Board (IRB) at the academic institution as well as the ad-hoc IRB at partnered FQHC. Informed consent was obtained from all participants in the current project.
Guiding Implementation Frameworks
In addition to the Implementation Mapping Process, we applied the Consolidated Framework for Implementation Research [CFIR; (31)] to guide the current study. We selected CFIR given the interest in examining organizational level determinants, specification of key implementation determinants, and utility in prior programs conducted in FQHCs applying the Implementation Mapping process [e.g., (32)]. Given the specific emphasis on health equity in the current project, we also applied the Health Equity Implementation Framework [HEIF; (33, 34)] to enable examination of key implementation determinants that may explain the social determinants of health. Specifically, we integrated the three health equity domains detailed within this framework into our application of CFIR.
Results for the Application of Implementation Mapping
Implementation Mapping Task 1: Conduct a Needs Assessment
The first aim of this study consisted of a sequential mixed-methods (quan-QUAL) needs assessment to identify care coordinator perspectives regarding: (1) client service and Care Coordinator training needs related to behavioral health; (2) implementation determinants for selected evidence-based behavioral health programs; and (3) necessary modifications or enhancements to selected evidence-based behavioral health programs. We also assessed perceptions regarding existing and potentially relevant implementation strategies via our initial quantitative survey. The selected implementation frameworks (CFIR, HEIF) guided data collection, analyses, and interpretation, including application to iteratively develop and refine a qualitative focus group guide and codebook applied to conduct and analyze focus groups through in-depth coding. Consistent with the HEIF, for example, we included an explicit emphasis on culturally relevant factors and determinants through specific focus group questions, probes, and codebook. We also included questions pertaining to the CFIR constructs of behavioral health knowledge and beliefs and compatibility of existing evidence-based behavioral health programs such as “Given your experience with these programs, how well do these programs fit with or are appropriate for [the needs of your patients, your role as a care coordinator, the realities of your organization]?” We then included an additional probe assessing for the HEIF health equity domain of cultural relevance, including the fit or acceptability of these practices with the culture, beliefs, preferences and/or language of the largely Hispanic or Latino/a patients served.
Participants included Care Coordinators (n = 8 or 50% of the broader population of Care Coordinators at the FQHC) who participated in the initial web-based survey and subsequent virtual focus group; the pilot project lead (K.D.) with experience in mixed-methods needs assessment and qualitative methods led the focus groups. Each focus group lasted approximately 45 min and were conducted in English via secure videoconferencing software (i.e., HIPAA-compliant Zoom). The majority of participants were female (75%), with a Bachelor's (63%) or Associate's (38%) Degree. All identified as Mexican or of Mexican descent and reported delivering care coordination services in English and Spanish. The pilot project lead (K.D.) also conducted two informational interviews with FQHC leaders to gather necessary information regarding evidence-based practice decision making and identification of relevant processes and resources. Qualitative data were initially analyzed using rapid assessment process (35, 36), with findings categorized following each focus group in alignment with focus group guide domains specified by CFIR and HEIF. We (K.D. and T.H.) conducted subsequent in-depth consensus coding, applying an iteratively developed codebook informed by a priori and emergent themes and the guiding frameworks. The codebook contained definitions of the codes and guidelines for use. We integrated both quantitative and qualitative types to examine complementarity and expansion (37).
Results from our needs assessment indicated multilevel determinants spanning the organizational, implementer and end recipient or patient levels, including perceived client service and Care Coordinator training needs, for consideration. This suggested a need for multilevel performance objectives to best address these needs and achieve outcomes (see Task 2). Findings indicated limited behavioral health knowledge among both patients and Care Coordinators as well as Care Coordinator limited self-efficacy addressing or assessing behavioral health concerns and implementing behavioral health EBPs. Importantly and consistent with HEIF, our results also indicated several culturally relevant factors or determinants that were raised several times throughout both focus groups. This included the cultural stigma commonly associated with behavioral health and behavioral health treatments within the Mexican culture. A poor match between care practices or recommendations and cultural values was also described. For example, several participants described preferences or beliefs regarding alternative or traditional treatments among their patients frequently limit or impeded adherence to additional treatment recommendations. At the organizational level, limited collaboration between Care Coordinators and behavioral health providers as well as challenges related to the availability of behavioral health services emerged as barriers to EBP implementation. Results also indicated several relevant strategies to address these determinants, including ongoing, dynamic behavioral health trainings, additional culturally relevant and tailored behavioral health educational materials for both patients and Care Coordinators and increased collaboration between Care Coordination and behavioral health. Following analyses, we shared our results with our FQHC partners to aid further contextualization and interpretation and used them to inform identification of relevant outcomes, performance objectives and change objectives (Task 2) as well as selection and design of implementation strategies (Task 3).
In collaboration with our FQHC partners, our needs assessment also informed and confirmed those involved in the implementation of the evidence-based program and those required to support execution of the corresponding implementation plan. We confirmed that Care Coordinators would be the primary program implementers given the alignment between the evidence-based program target of behavioral health and workload responsibilities and expectations surrounding behavioral health for Care Coordinators. Care Coordination and organizational leaders would facilitate execution of the implementation strategies identified in Task 2. While the initial evidence-based behavioral health trainings would be facilitated by the research team, trainings were designed to be sustainable such that Care Coordination leaders can continue to facilitate and conduct these trainings following the completion of the study.
Implementation Mapping Task 2: Identify and State Adoption and Implementation Outcomes, Performance Objectives, Determinants, and Change Objectives
As mentioned, Task 1 findings aided the identification of relevant implementation outcomes, performance objectives corresponding to each identified implementation outcome, determinants of each performance objective, and change objectives mapped onto identified performance objectives and determinants. In collaboration with FQHC partners, we identified relevant implementation outcomes as well as necessary performance objectives to achieve these outcomes. The project lead and coordinator then reviewed the preliminary needs assessment findings to identify multilevel determinants relative to these performance objectives. Importantly, our Task 1 needs assessments identified several determinants, especially those pertaining to broader outer context or community-level, that while relevant, were deemed not directly relevant to our stated performance objectives and outside the scope of the current project. Thus, these were not included among our final determinants. This included barriers not directly related to behavioral health needs such as social service offerings (e.g., food distributions) or cultural food preferences that were incompatible with broader medical care or medically-related Care Coordination goals (e.g., limiting high carb such as those common in non-perishable foods).
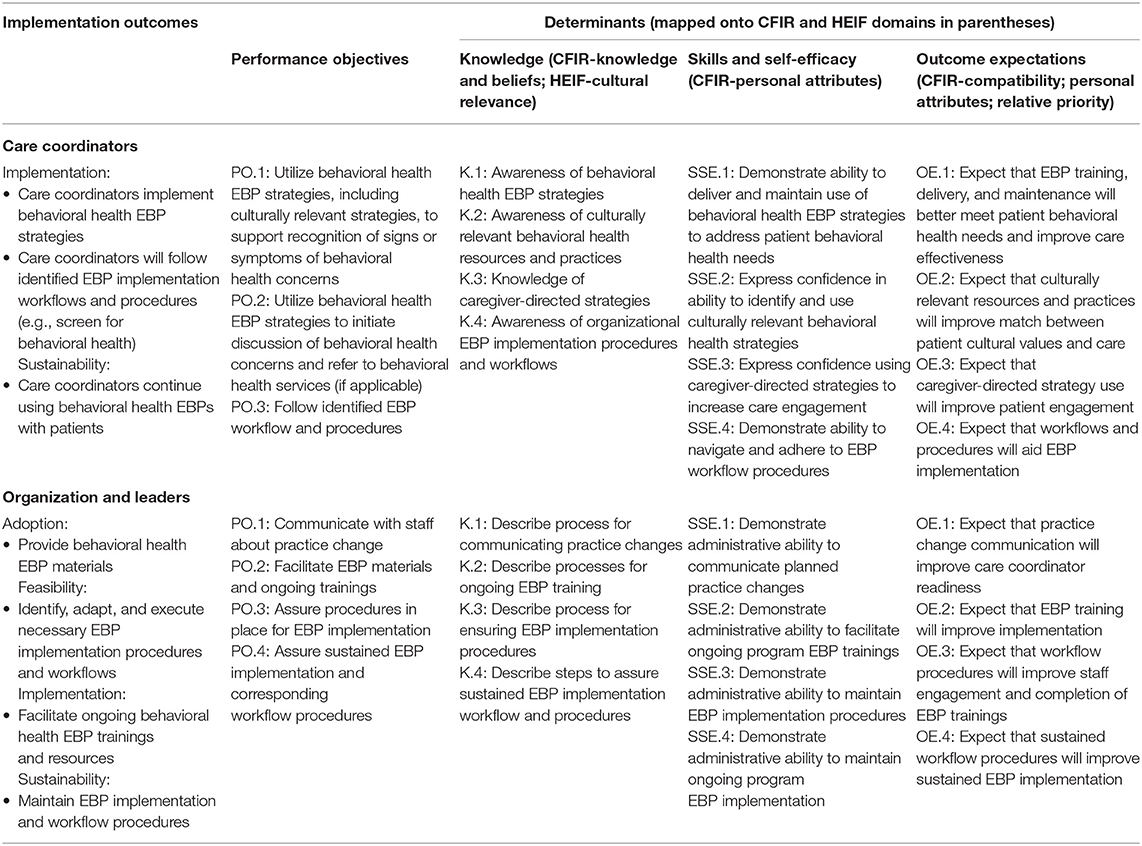
Determinants were also informed by broader CFIR and HEIF health equity domains to ensure alignment with our guiding implementation theories. For example, our needs assessment findings suggested limited knowledge and efficacy surrounding behavioral health. Consistent with the CFIR inner context domains Knowledge and Beliefs and Personal Attributes, this contributed to our specification of behavioral health knowledge and efficacy determinants. Additionally, and consistent with the HEIF health equity domain of culturally relevant factors, we identified knowledge and self-efficacy related to culturally relevant resources and practices as important determinants of stated performance objectives. Finally, we identified change objectives tied to each performance objective and determinant selected. See Table 1 for summary of implementation outcomes, performance objectives and relevant determinants.
Implementation Mapping Task 3: Change Method and Implementation Strategy Selection and Design
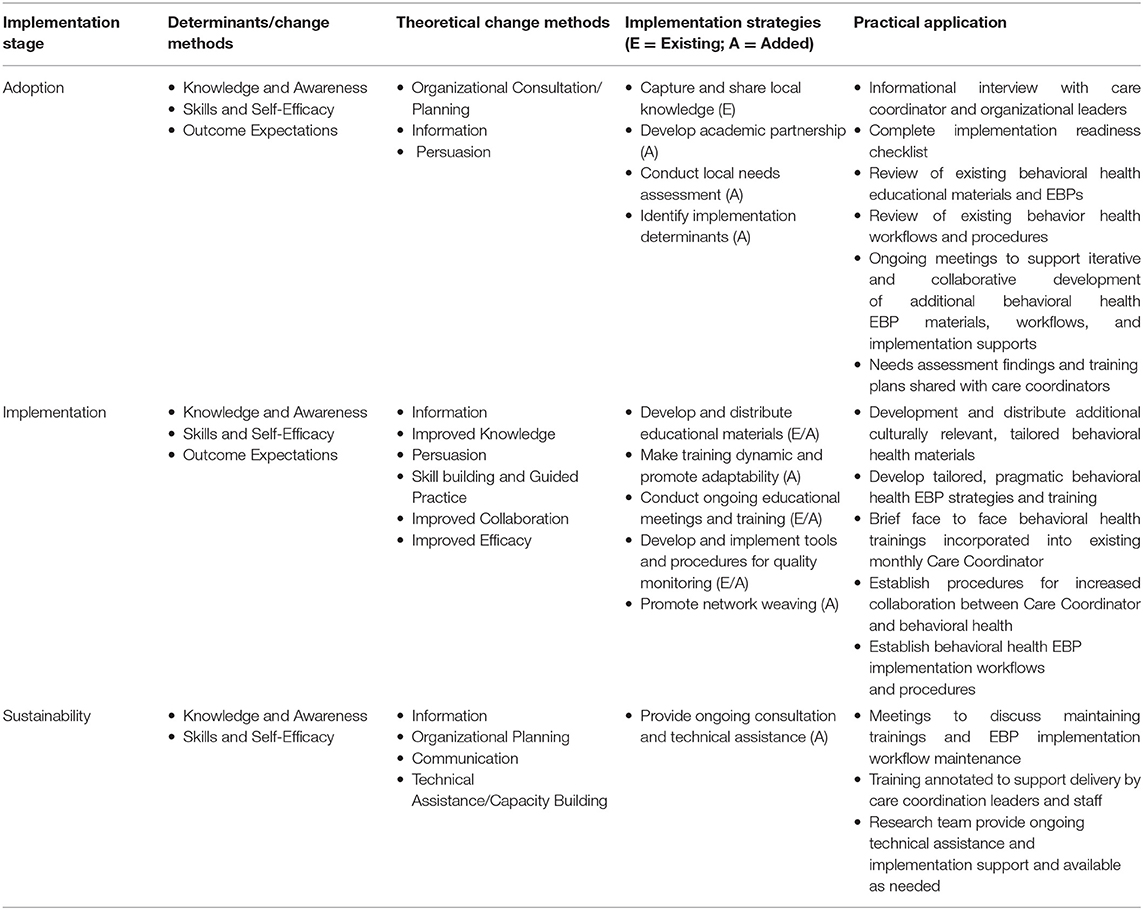
To complete this task, we first developed and selected theoretical change methods expected to target the determinants and change objectives identified in Task 2. This informed the subsequent, iterative selection of implementation strategies that appropriately operationalized our change methods. As in prior Tasks, this process was done in collaboration with our FQHC partners. We began by considering the implementation determinants and change objectives identified in Task 2 and referred to specific Task 1 quantitative results regarding Care Coordinators perspectives of relevant implementation strategies. This led to the development of specific theoretical change methods, informed by our guiding CFIR and HEIF implementation frameworks as well as literature regarding causal theories in implementation science [e.g., (38)]. For example, given the identified role of knowledge and knowledge change in promoting successful adoption and implementation, this was hypothesized as a key change method. To operationalize these change methods, we then developed and selected a list of possible implementation strategies. Informed by CFIR, we then prioritized those methods and strategies that would address implementation determinants toward achieving outcomes across multiple inner context levels, including providing information via training and educational materials targeting behavioral health knowledge and efficacy. We iteratively refined our implementation strategies following feedback from our community partner, including feedback regarding fit and feasibility within their organization (Table 2).
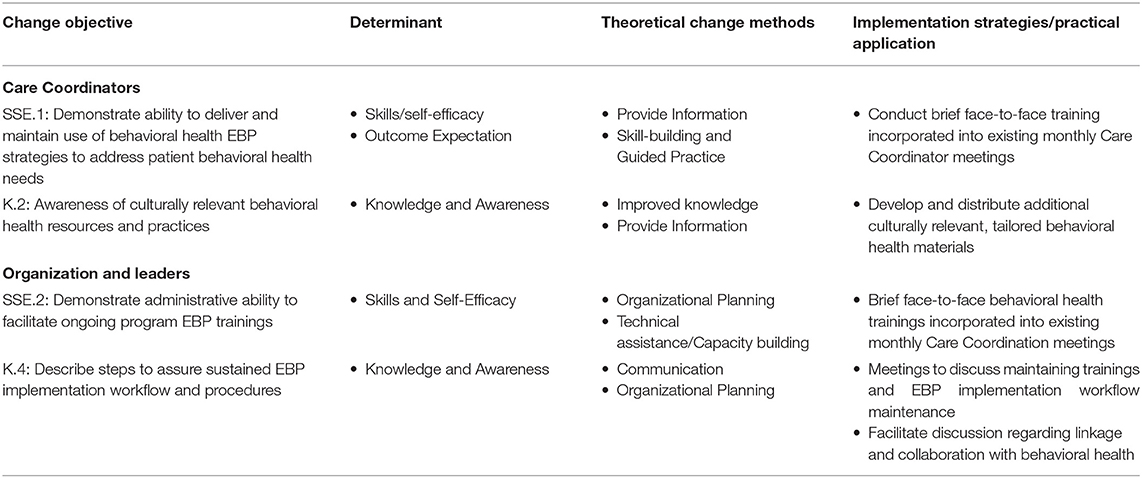
Table 2. Sample change objectives with corresponding implementation determinants, methods and implementation strategies.
During our design, selection, and refinement of implementation strategies, we were mindful of the specific implementation context and parameters within the partnered FQHC. For example, we considered but ultimately did not include the specific strategies of identifying implementation champions and/or quality monitoring to operationalize our change methods of Skill-building, Guided Practice, and Capacity Building but did not select these as they did not optimally fit with the specific structure and roles of the care coordination program, including Care Coordinator workload expectations and responsibilities. Additionally, we developed and tailored strategies to ensure complementarity with existing strategies utilized. For instance, the partnered FQHC conducted trainings for the selected behavioral health EBP materials with Care Coordinators as well as distributed behavioral health educational materials. To complement these strategies, we designed additional behavioral health educational materials targeting improved behavioral health knowledge and efficacy. Given the health equity focus within this project and consistent with the HEIF, strategies were designed or tailored to address or include culturally relevant factors such as patient beliefs, preferences, and treatment or care expectations. For example, educational materials developed aimed to destigmatize behavioral health and detail what the patient could expect from behavioral health services. To expand on existing EBP trainings, we designed ongoing, dynamic and adaptable trainings that were tailored to the specific needs (e.g., health care needs, cultural) of patients served. Trainings will be supplemented with ongoing implementation support and consultation as needed. Table 3 details the specific implementation strategies selected.
Implementation Mapping Task 4: Implementation Protocol and Materials
We finalized the process of identifying and developing implementation strategies (Task 3) to create an implementation protocol. It details the implementation strategies and practical applications, or those more detailed aspects of the implementation strategies, we designed to create change in the implementation determinants and change objectives identified in Task 2. We expect these implementation determinants and change objectives to drive achievement of the performance objectives and influence the specified implementation outcomes. Development of the protocol, activities and materials occurred in collaboration with our community partners to enhance the contextual fit within the organization as well as improve identified implementation strategies. To optimize feasibility and sustainability for example, we designed our ongoing trainings to be brief and pragmatic to permit incorporation into existing Care Coordinator team meetings (vs. requiring identification of additional training time). Psychoeducational and training topics were selected and/or developed to address patient and Care Coordinator behavioral health needs as well as normalize and destigmatize behavioral health. Sample topics included what to expect from behavior health services for patients, evidence-based stress management, coping strategies and patient engagement strategies, psychoeducation for setting behavioral health-oriented treatment goals, and psychoeducation for addressing and preventing secondary trauma. Further, we annotated all materials to enable ongoing delivery by partnered Care Coordinator leaders and/or staff as needed.
Implementation Mapping Task 5: Evaluate Implementation Outcomes
Implementation evaluation is planned as part of an ongoing preliminary pilot test of the selected EBP components and implementation protocol within the context of the partnered Care Coordinator program. Evaluation of identified strategies and associated impact on determinants and implementation outcomes is planned using a mixed-methods (quan->QUAL) approach. Initial quantitative measures will assess feasibility, acceptability, and appropriateness, as well as Care Coordinator knowledge and efficacy surrounding behavioral health using existing measures [e.g., Feasibility of Intervention Measure, Acceptability of Intervention Measure and Intervention Appropriateness measure (39); adapted evidence-based practice knowledge and confidence measure (40)] tailored for the current study. Qualitative interviews will expand on quantitative data regarding implementation outcomes as well as explore participating Care Coordinator perspectives' regarding programmatic impact on patient-level determinants and outcomes. Again, data collection and analyses will be guided by CFIR and the HEIR. Similar to our Task 1 needs assessments, questions will assess the compatibility of the developed evidence-based behavioral health practices and strategies as well as implementation strategies, including questions such as “You mentioned in the survey that you found the specific strategy of [insert strategy identified in quantitative survey here] as helpful. Can you tell us how you found this helpful?” with the specific probes regarding the cultural relevance and/or fit of this strategy with patients. We anticipate analyzing data using similar methods as in our Task 1 mixed-methods needs assessment.
Discussion
Implementation Mapping has the potential to respond to the need for enhanced methods to design, tailor, test, and evaluate implementation strategies in service of improving effective care delivery and outcomes in community settings (41). Indeed, prior work as well as the work included within this special issue highlight its utility in applying this approach to develop and test implementation strategies to improve the translation of effective care practices (27, 32). The current work presented a case study of ongoing work to apply Implementation Mapping to inform implementation strategy development to expand an existing community-initiated health equity initiative at a partnered FQHC.
A particular strength of the Implementation Mapping approach is the systematic approach to developing and tailoring implementation strategies and materials that begins with articulating desired outcomes and works in a stepwise, linked fashion toward describing behaviors and behavioral determinants associated with those outcomes. This allowed for facile application of this process as part of community-identified implementation effort where outcomes, especially service outcomes, were already selected and prioritized. In the current project, that included improving the health outcomes, especially behavioral health outcomes, of patients served in the Care Coordination program. An additional strength of this approach is the ease of incorporation of additional implementation science frameworks within the Implementation Mapping process. Given the explicit focus on health equity and organizational implementation determinants in the current study, for example, the application of CFIR and health equity domains from the HEIF was necessary for the current project. Finally, the current project demonstrates the immense utility of applying the Implementation Mapping to advance health equity implementation efforts given the strong emphasis on identifying and addressing implementation determinants, including those contributing to ongoing healthcare inequities, throughout each stepwise task.
This case study also underscored the importance of incorporating strong community partnerships as part of the Implementation Mapping process. The continued input and feedback obtained from our partners and leaders at the FQHC was invaluable to our application of Implementation Mapping, particularly during the selection and design of implementation strategies and methods (Task 3) to assure the feasibility and appropriateness within their organizational context and existing implementation strategies. The value added of involving community stakeholders is consistent with its role as an integral component of implementation and consideration as best practice for implementation research (42, 43). Community engagement adds additional value as part of implementation science methodologies such as Implementation Mapping through by assuring that the continued development and application of these methodologies align with community originated implementation initiatives such as the care coordination program of interest in the current study.
We noted some limitations to Implementation Mapping process, namely the time intensive nature of this process. As noted, the application of this process spanned multiple months, which is consistent with similar work noting a similar timeline as well as large number of individuals involved (32, 44). While these limitations certainly do not outweigh the immense benefits resulting from this process, the time and resources necessary may preclude its use in projects that may otherwise greatly benefit but lack these resources, including community-initiated implementation projects. Future directions include additional application of Implementation Mapping, especially within the context of rapid implementation projects or those applying more rapid implementation methods to better understand its use and utility in such projects.
Conclusions
There is a need for more systematic selection, design, specification, and testing of implementation strategies, including methods and tools to support doing so, to maximize the successful translation of EBPs. Implementation Mapping represents a practical method that has the potential to advance our use and understanding of implementation strategies. The current study provides a case study of the application of Implementation Mapping to an applied, community-partnered project aiming to examine the implementation and expansion of an existing, community-initiated health equity effort within a FQHC. It may provide useful insights for future work aiming to apply the Implementation Mapping process to support further health equity implementation efforts.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by San Diego State University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KD and TH wrote sections of the manuscript. KD and EA participated in the development of implementation mapping process. All authors reviewed and edited the manuscript.
Funding
Research reported in this manuscript was supported by the National Institute on Minority Health and Health Disparities, part of the National Institutes of Health, under award number U54MD012397. KD was also supported by a National Institute of Mental Health Career Development Award K23 MH115100.
Author Disclaimer
The research content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to acknowledge and thank our FQHC organizational partners for their engagement, guidance, support, and generous collaboration on this project.
References
1. Flores G. Racial and ethnic disparities in the health and health care of children. Pediatrics. (2010) 125:e979. doi: 10.1542/peds.2010-0188
2. U. S. Department of Health and Human Services National Center for Health Statistics. Health, United States, 2016 - With Chartbook on Long Term Trends in Health. Hyattsville, MD: U. S. Department of Health, and Human Services National Center for Health Statistics (2016).
3. National Centre for Health Statistics. Health, United States, 2015: Special Feature on Racial and Ethnic Health Disparities. National Centre for Health Statistics (2016).
4. Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. (2009) 31:99–112. doi: 10.1093/epirev/mxp008
5. U. S. Department of Health and Human Services. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: US Public Health Service: Substance Abuse and Mental Health Services Administration (2001). p. 1–204.
6. Bureau USC. U.S. Census Bureau Projections Show a Slower Growing, Older, More Diverse Nation a Half Century From Now. Suitland, MD: U.S. Census Bureau Publication (2012).
7. Nath JB, Costigan S, Hsia RY. Changes in demographics of patients seen at federally qualified health centers, 2005-2014. JAMA Internal Med. (2016) 176:712–4. doi: 10.1001/jamainternmed.2016.0705
8. Rosenbaum S, Paradise J, Rossier Markus A, Sharac J, Tran C. The George Washington University Health Sciences Research Commons Geiger Gibson/RCHN Community Health Foundation Research Collaborative Health Policy Management 1-2017 Part of the Community Health Preventive Medicine Commons, Health Medical Community Health Centers: Recent growth the role of the ACA. The Henry J. Kaiser Family Foundation (2017). Available online at: hsrc.himmelfarb.gwu.edu/sphhs_policy_ggrchnhttp://kff.org/medicaid/issue-brief/community-health-centers-recent-growth-and-the-role-of-the-aca/ (accessed January 30, 2017).
9. Geiger Gibson/RCHN and Community Health Foundation Research Collaborative. The Toll Taken on Poor Communities: Community Health Centers in the First Year of the COVID-19 Pandemic. Milken Institute School of Public Health (2021).
10. Burke BT, Miller BF, Proser M, Petterson SM, Bazemore AW, Goplerud E, et al. A needs-based method for estimating the behavioral health staff needs of community health centers. BMC Health Serv Res. (2013) 13:245. doi: 10.1186/1472-6963-13-245
11. Health Resources and Services Administration - Bureau of Primary Health Care: Uniform Data System Report. (2020). Available online at: https://bphc.hrsa.gov/sites/default/files/bphc/datareporting/pdf/2020-uds-manual.pdf (accessed February 01, 2022).
12. Duan-Porter W, Ullman K, Majeski B, Miake-Lye I, Diem S, Wilt TJ. Care coordination models and tools-Systematic review and key informant interviews. J Gen Intern Med. (2021). doi: 10.1007/s11606-021-07158-w. [Epub ahead of print].
13. Grubbs SS, Polite BN, Carney J, Bowser W, Rogers J, Katurakes N, et al. Eliminating racial disparities in colorectal cancer in the real world: It took a village. J Clin Oncol. (2013) 31:1928–30. doi: 10.1200/JCO.2012.47.8412
14. White RO, DeWalt DA, Malone RM, Osborn CY, Pignone MP, Rothman RL. Leveling the field: addressing health disparities through diabetes disease management. Am J Manag Care. (2010) 16:42–8.
15. National Coalition on Care Coordination. Policy Brief: Implementing Care Coordination in the Patient Protection and Affordable Care Act. National Coalition on Care Coordination (2014).
16. Parsons PL, Slattum PW, Thomas CK, Cheng JL, Alsane D, Giddens JL. Evaluation of an interprofessional care coordination model: Benefits to health professions students and the community served. Nurs Outlook. (2021) 69:322–32. doi: 10.1016/j.outlook.2020.09.007
17. Kangovi S, Mitra N, Grande D, Long JA, Asch DA. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Affairs. (2020) 39:207–13. doi: 10.1377/hlthaff.2019.00981
18. Landers S, Levinson M. Mounting evidence of the effectiveness and versatility of community health workers. Am J Public Health. (2016) 106:591–2. doi: 10.2105/AJPH.2016.303099
19. Smith S, Wallace E, O'Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochr Database Syst Rev. (2016) 3:CD006560. doi: 10.1002/14651858.CD006560.pub3
20. Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight-Eily LR, et al. Collaborative care to improve the management of depressive disorders: A community guide systematic review and meta-analysis. Am J Prevent Med. (2012) 42:525–38. doi: 10.1016/j.amepre.2012.01.019
21. HRSA Accreditation Patient-Centered Medical Home Recognition Initiative. Bureau of Primary Health Care. (2021). Available online at: https://bphc.hrsa.gov/qualityimprovement/clinicalquality/accreditation-pcmh/index.html (accessed February 1, 2022).
22. Angstman KB, Phelan S, Myszkowski MR, Schak KM, DeJesus RS, Lineberry TW, et al. Minority primary care patients with depression. Med Care. (2015) 53:32–7. doi: 10.1097/MLR.0000000000000280
23. Kitchener BA, Jorm AF. Mental health first aid training for the public: Evaluation of effects on knowledge, attitudes and helping behavior. BMC Psychiatry. (2002) 2:1–6. doi: 10.1186/1471-244X-2-10
24. Kitchener BA, Jorm AF, Kelly C, First Aid Australia. Mental health First Aid Manual. Parkville VIC: Mental Health First Aid Australia (2016).
25. Mental Health First Aid USA. (2021). Available online at: http://www.mentalhealthfirstaid.org/cs/ (accessed February 01, 2022).
26. Wade R, Becker BD, Bevans KB, Ford DC, Forrest CB. Development and evaluation of a short adverse childhood experiences measure. Am J Prevent Med. (2017) 52:163–72. doi: 10.1016/j.amepre.2016.09.033
27. Fernandez ME, ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: Using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:1–15. doi: 10.3389/fpubh.2019.00158
28. Knaak S, Patten S. A grounded theory model for reducing stigma in health professionals in Canada. Acta Psychiatrica Scandinavica. (2016) 134:53–62. doi: 10.1111/acps.12612
29. Knaak S, Patten S, Ungar T. Mental illness stigma as a quality-of-care problem. Lancet Psychiatry. (2015) 2:863–4. doi: 10.1016/S2215-0366(15)00382-X
30. Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthcare Manag Forum. (2017) 30:111–6. doi: 10.1177/0840470416679413
31. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
32. Highfield L, Valerio MA, Fernandez ME, Eldridge-Bartholomew LK. Development of an implementation intervention using intervention mapping to increase mammography among low income women. Front Public Health. (2018) 6:300. doi: 10.3389/fpubh.2018.00300
33. Woodward EN, Matthieu MM, Uchendu US, Rogal S, Kirchner JE. The health equity implementation framework: Proposal and preliminary study of hepatitis C virus treatment. Implement Sci. (2019) 14:1–18. doi: 10.1186/s13012-019-0861-y
34. Woodward E, Singh RS, Ndebele-Ngwenya P, Castillo AM, Dickson K, Kirchner J. A practical guide to incorporating health equity domains in implementation frameworks. Implement Sci Commun. (2020) 5:1–16. doi: 10.21203/rs.3.rs-32704/v1
36. Hamilton AB. Qualitative Methods in Rapid Turn-Around Health Services Research. (2013). Available online at: www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/780-notes.pdf (accessed February 01, 2022).
37. Palinkas LA, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, Landsverk J. Mixed method designs in implementation research. Adm Policy Ment Health. (2011) 38:44–53. doi: 10.1007/s10488-010-0314-z
38. Williams NJ, Beidas RS. Annual research review: the state of implementation science in child psychology and psychiatry: a review and suggestions to advance the field. J Child Psychol Psychiatry. (2019) 60:430–50. doi: 10.1111/jcpp.12960
39. Weiner BJ, Lewis CC, Stanick C, Powell BJ, Dorsey CN, Clary AS, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. (2017) 12:3. doi: 10.1186/s13012-017-0635-3
40. Lau AS, Brookman-Frazee L. The 4KEEPS study: identifying predictors of sustainment of multiple practices fiscally mandated in children's mental health services. Implement Sci. (2016) 11:31. doi: 10.1186/s13012-016-0388-4
41. Powell BJ, Fernandez ME, Williams NJ, Aarons GA, Beidas RS, Lewis CC, et al. Enhancing the impact of implementation strategies in healthcare: a research agenda. Front Public Health. (2019) 7:1–9. doi: 10.3389/fpubh.2019.00003
42. Brookman-Frazee L, Stahmer A, Stadnick N, Chlebowski C, Herschell A, Garland AF. Characterizing the use of research-community partnerships in studies of evidence-based interventions in children's community services. Adm Policy Ment Health Ment Health Serv Res. (2016) 43:93–104. doi: 10.1007/s10488-014-0622-9
43. Drahota A, Meza RD, Brikho B, Naaf M, Estabillo JA, Gomez ED, et al. Community-academic partnerships: a systematic review of the state of the literature and recommendations for future research. Milbank Quart. (2016) 94:163–214. doi: 10.1111/1468-0009.12184
44. Ibekwe LN, Walker TJ, Ebunlomo E, Ricks KB, Prasad S, Savas LS, et al. Using implementation mapping to develop implementation strategies for the delivery of a cancer prevention and control phone navigation program: a collaboration with 2-1-1. Health Promot Pract. (2022) 23:86–97. doi: 10.1177/1524839920957979
Keywords: Implementation Mapping, care coordination, federally qualified health center, evidence-based practice, implementation strategy
Citation: Dickson KS, Holt T and Arredondo E (2022) Applying Implementation Mapping to Expand a Care Coordination Program at a Federally Qualified Health Center. Front. Public Health 10:844898. doi: 10.3389/fpubh.2022.844898
Received: 29 December 2021; Accepted: 28 February 2022;
Published: 24 March 2022.
Edited by:
Gill Ten Hoor, Maastricht University, NetherlandsReviewed by:
Lynn N. Ibekwe, Harvard University, United StatesGerjo Kok, Maastricht University, Netherlands
Copyright © 2022 Dickson, Holt and Arredondo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kelsey S. Dickson, a2RpY2tzb25Ac2RzdS5lZHU=
 Kelsey S. Dickson
Kelsey S. Dickson Tana Holt
Tana Holt Elva Arredondo4,5
Elva Arredondo4,5