- 1Department of Cardiology, First Hospital of China Medical University, Shenyang, China
- 2Department of Clinical Epidemiology, Institute of Cardiovascular Diseases, First Hospital of China Medical University, Shenyang, China
- 3Department of Clinical Epidemiology, Shengjing Hospital of China Medical University, Shenyang, China
Objective: Cumulative evidence indicates that education plays a major role in predicting cardiovascular risk factors. In this study, we intend to examine the possible relationship between education status and mortality in a large general subject from rural China.
Methods: Adult hypertensive subjects (n = 5,227, age = 57.22 ± 10.18 years; 49.1% men) were recruited from general population surveys (Northeast China Rural Cardiovascular Health Study). Their educational status was categorized into two groups as follows: (1) Low education (illiterate or lower than primary school) and (2) medium-high education (higher than primary school). Cardiometabolic comorbidities, related cardiovascular risk factors, and echocardiographic measurements were analyzed in both groups.
Results: Less educated hypertensive subjects had significantly higher prevalence of obesity, diabetes, dyslipidemia, and left ventricular hypertrophy than medium-high educated hypertensive subjects. In the medium-high educated subjects, a significant increase in left ventricular ejection fraction and lower rate of antihypertensive medication was found. Cox proportional hazards analysis indicated that medium-high education was independently associated with all-cause mortality (hazard ratio = 0.76; 95% confidence interval, 0.58, 0.99; P = 0.043) and cardiovascular mortality (hazard ratio = 0.65; 95% confidence interval, 0.44, 0.96; P = 0.028).
Conclusion: Education may act as the best predictor of all-cause and cardiovascular mortality in rural hypertensive subjects. This finding suggests that in rural areas, education is likely to represent a cardiovascular specific risk factor and should be evaluated in the strategies of hypertension.
Introduction
With the development of economy in rural areas, cardiovascular risk factors, such as hypertension, dyslipidemia, diabetes, and obesity have become a major disease burden, and account for a large proportion of mortality worldwide (1). Until 2013, in rural Chinese areas, the prevalence of lipid abnormality was 47.8, 13.8, 25.7, and 30.7% for total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG), respectively and the prevalence of hypertension was 51.1% (53.9% for men and 48.7% for women) (2, 3). Large cohort studies have demonstrated that high blood pressure (BP), as the major remediable risk factor, increased the risk of heart failure, atrial fibrillation, chronic kidney disease, heart valve diseases, aortic syndromes, and dementia, in addition to coronary heart disease and stroke (4–8). Although frequently asymptomatic, hypertension is associated with the cardiovascular disease (CVD) causation and is the leading cause of death globally (9, 10). Clinical trials have demonstrated that there is a decrease in mortality with reduction in BP, which emphasizes the importance of hypertension prevention (8). Moreover, BP reduction effectively reduces the overall burden of CVDs, significantly lowering the incidence of myocardial infarction, congestive heart failure, and cerebrovascular disease (11).
In 2020, The American Heart Association (AHA), in conjunction with the National Institutes of Health (NIH), reported the most up-to-date statistics related to heart disease, stroke, and cardiovascular risk factors (12). They present the AHA's My Life Check—Life's Simple 7 which includes the following: be active, maintain a healthy weight, learn about cholesterol, no smoking or use smokeless tobacco, eat a heart-healthy diet, keep blood pressure healthy, and learn about blood sugar and diabetes mellitus (12). Except for those factors mentioned above, in recent years, socio-economic status (SES) has gradually gained more attention and has been considered as an important factor for the development of CVDs. Among them, education status has been proved to be a useful indicator of SES and important predictor of CVD, and total and cardiovascular mortality (13, 14). Rural subjects from China have unique SES characters for example, compared with urban citizens, rural residents have relatively lower annual income, poor medical support, and higher rate of chronic diseases (15–20). Among those characters mentioned previously, the typical one is that lower educational status.
It is important to improve cardiovascular risk prediction to effectively prevent CVDs. Previous studies designed to estimate the possible effect of education on cardiovascular risk in hypertensive subjects suggested that education might serve as the best predictor of cardiovascular risk (21). Nevertheless, these studies enrolled participants from urban or developed areas who had relatively higher educational status than their rural counterparts. Besides, no study has evaluated whether education was able to predict cardiovascular mortality or all-cause mortality in hypertensive participants. To reduce cardiovascular mortality in rural areas of China, we need to identify useful predictors and develop useful strategies to control it. Hence, this study was designed to evaluate the impact of education on cardiovascular events (CVEs), and cardiovascular and all-cause mortality in rural hypertensive subjects.
Materials and methods
Subjects and methods
The Northeast China Rural Cardiovascular Health Study (NCRCHS) is a community-based prospective cohort study carried out in rural areas of Northeast China. The design and inclusion criteria of the study have been described previously (22). The study was approved by the Ethics Committee of China Medical University (Shenyang, China AF-SDP-07-1, 0-01). In brief, a multi-stage, stratified, and random cluster sampling design was adopted. In the first stage, Dawa, Zhangwu, and Liaoyang countries were selected from the eastern, southern, and northern regions of Liaoning Province. In the second stage, one town was randomly selected from each county (total of 3 towns). In the third stage, 8–10 rural villages from each town were randomly selected. In total, 26 rural villages were included. All eligible permanent residents (aged ≥35 years) were invited from each village to participate in the study. Participants who were pregnant, had a malignant tumor, or had mental disorders were excluded (23). For each participant, detailed information was collected at baseline. In 2015 and 2017, participants were invited to attend a follow-up study. Of the 11,956 subjects, 1,256 participants were not included due to missing contact information, and 10,349 participants (86.6%) completed at least one follow-up visit. The median follow-up was 4.66 years. Written informed consent was obtained from all participants. Complete information on co-variables was required at the baseline visit for inclusion in the current analyses. In the present study, we enrolled hypertensive subjects. Therefore, 5,227 participants out of 10,349 were enrolled in the present study.
All hypertensive subjects were divided into two groups according to their educational status as follows: (1) ‘Low educational group' consisting of 2,925 subjects (60% females) with a mean age of 60.52 ± 9.62 years who were illiterates or with an educational status of lower than primary school. (2) ‘Medium-high educational group' consisting of 2,302 subjects (38.9% females) with a mean age of 53.02 ± 9.29 years with higher than primary school education level, including high school, college, or above.
Measurements
For all subjects, clinical examination, including medical history, anthropometry, BP measurement, Doppler echocardiology, and fasting collection of blood were conducted for determining biological parameters. All this has been described in detail in previous studies (22, 24, 25). Weight and height were measured in participants with light weight clothing and without shoes. Waist circumference was measured at the umbilicus using a non-elastic tape. Body mass index (BMI, weight in kilograms divided by the square of height) and waist-to-hip ratio (WHR) were calculated. BP was assessed thrice in participants seated, after at least 5 min of rest using a standardized automatic electronic sphygmomanometer (HEM-907; Omron, Tokyo, Japan). Hypertension was defined as a systolic blood pressure (SBP) of ≥140 mmHg and/or a diastolic blood pressure (DBP) of ≥90 mmHg, and/or use of antihypertensive medications (11). Additionally, we evaluated the status of smoking and drinking. Fasting blood samples were collected in the morning from participants who fasted for at least 12 h. Fasting plasma glucose (FPG), TC, LDL-C, HDL-C, and TG were analyzed enzymatically.
Echocardiographic examination
All subjects underwent an M-mode and B-mode echocardiographic examination according to standardized procedures previously described (26). Left ventricular mass (LVM) and left ventricular mass index (LVMI) were calculated using data from echocardiographic examination. LVM was normalized for body surface area. Left ventricular hypertrophy (LVH) was defined as LVM index ≥115 g/m2 in men and 99 g/m2 in women (27, 28).
Adjudication of endpoints
The median follow-up was 4.66 years. The first participant was enrolled in January 2012, whereas the last follow-up date was December 2017. A series of irregular follow-up visits were conducted. The follow-up time was determined as the interval period from the date of randomization to the date of death, the date of last visit, or the last recorded clinical event of participants still alive, whichever occurred first (29). The primary outcome of this study was cause-specific mortality and cardiovascular cause mortality. An incident CVE was defined as a composite of new onset stroke or coronary heart disease (CHD) during the follow-up period. The specific incidences of stroke and CHD were also determined. For all participants reporting possible diagnoses or death, all available clinical information was collected, including medical records and death certificates. All materials were independently reviewed and adjudicated by the end-point assessment committee. Stroke was defined according to the WHO Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) criteria. CHD was defined as the diagnosis of hospitalized angina, hospitalized myocardial infarction, CHD death, or any revascularization procedure (30).
Statistical analysis
Descriptive statistics were calculated for all the variables, including continuous variables reported as mean ± standard deviations (SD) and categorical variables reported as numbers and percentages. Cox proportional hazards models were used to identify the associations between educational status and mortality with hazard ratios (HRs) and 95% confidence intervals (CIs) calculated. The related confounders were selected based on previous studies and their possible associations with cardiovascular mortality and all-cause mortality in clinical practice (21, 31, 32). All statistical analyses were performed using SPSS version 17.0 software, and P-values < 0.05 were considered statistically significant.
Results
All hypertensive subjects were sub-divided into two groups according to their educational status, namely low educational and medium-high educational groups. There were 2,925 subjects with low education (55.96%), whereas 2,302 with medium-high education (44.04%). The results revealed that hypertensive subjects with medium-high education had significantly younger age and lower proportion of females than those with low education (Table 1). Besides, subjects with higher education had relatively higher value of BMI and DBP, whereas lower value of SBP, TC, and LDL-C than subjects with low education. Unexpectedly, the prevalence of current smoking (38.0 vs. 32.9%, P < 0.001) and drinking (30.9 vs. 20.1%, P < 0.001) were significantly higher among medium-high education subjects compared with low education subjects. Participants with low education had relatively higher proportion of low annual income compared with medium-high education participants (≤5,000 CNY/year: 18.0 vs. 10.0%). Additionally, the rate of empty-nest subjects was significantly higher in the low education group than the high education group (48.2 vs. 32.2%, P < 0.001).
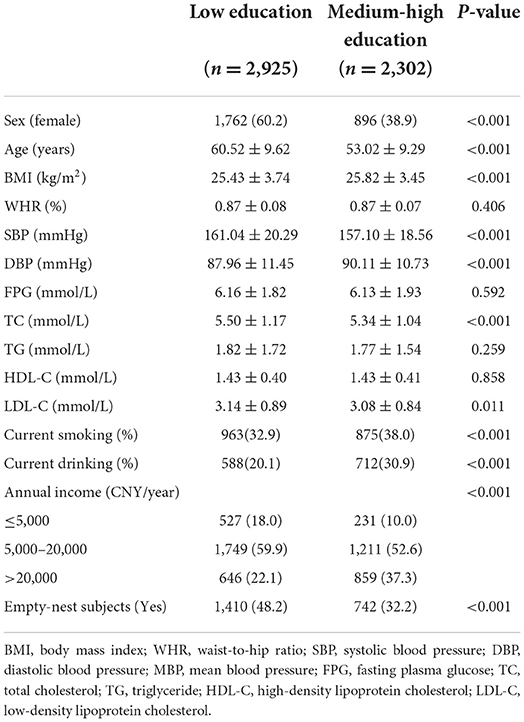
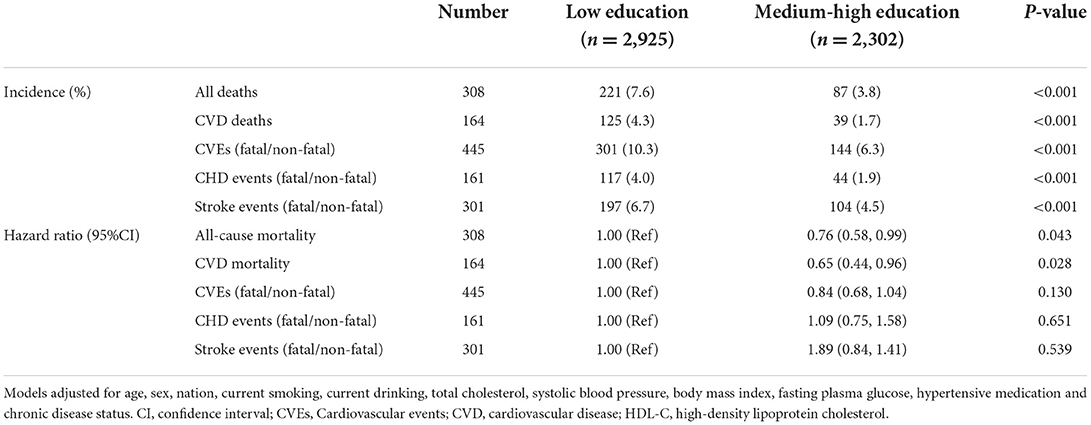
Table 1. Clinical characteristics in hypertensive subdivided at baseline according to educational status.
Table 2 showed that participants with low educational status had significantly higher prevalence of diabetes (17.1 vs. 14.9%, P = 0.02), dyslipidemia (82.2 vs. 77.9%, P < 0.001), and LVH (21.8 vs. 12.4%, P < 0.001) than participants with medium-high educational status. The prevalence of antihypertensive treatment was significantly higher in low educational group compared with medium-high educational group (32.8 vs. 26.1%, P < 0.001). In contrast, participants with medium-high education had relatively higher prevalence of obesity (57.5 vs. 52.2%, P < 0.001) and higher value of left ventricular ejection fraction (62.75 ± 3.89 vs. 61.95 ± 4.23, P < 0.001) than participants with low educational status. In terms of the prevalence of abdominal obesity, MetS, and E/A ratio, no significant differences were observed between the low educational and medium-high educational groups.

Table 2. Prevalence of comorbidities and echocardiographic parameters in hypertensives subdivided according to educational status.
Table 3 exhibits the Cox proportional hazard analysis after adjusting for possible confounders. Data showed that 308 deaths occurred from all-cause during follow-up. Participants with low education had remarkably higher incidence of all-cause mortality than those with medium-high education (7.6 vs. 3.8%, P < 0.001). Similarly, the incidence of CVD deaths was significantly higher in low education groups compared with medium-high education groups (4.3 vs. 1.7%, P < 0.001). Compared with the low education group, medium-high education group was associated with lower all-cause mortality (hazard ratio: 0.76, 95%CI, 0.58, 0.99, P = 0.043). In addition, 164 deaths attributed to CVDs and medium-high education was effective predictor of CVD deaths (hazard ratio: 0.65, 95%CI, 0.44, 0.96, P = 0.028). We also retrieved fatal and non-fatal CVEs. There were 161 CHD and 301 stroke events. Compared with low education group, the incidence of CVEs (10.3 vs. 6.3%, P < 0.001), CHD events (4.0 vs. 1.9%, P < 0.001), and stroke events (6.7 vs. 4.5%, P < 0.001) were significantly lower in medium-high education group. However, after adjusting for possible confounders, educational status was neither effective predictor of CVEs nor CHD events/stroke events.
Discussion
The present study, for the first time, confirmed the association between educational status and mortality in hypertensive subjects from rural areas of China. The major novel finding of this study was that diabetes, dyslipidemia, LVH, and antihypertensive medications were higher in hypertensive subjects with less education than those with medium-high education, whereas obesity was more likely to be seen among higher educational subjects. This finding indicated that education has close relationship with important cardiovascular risk factors. Besides, after adjusting for possible confounders, relatively higher educational status was associated with lower incidence of all-cause mortality and cardiovascular mortality among hypertensive subjects.
The China Hypertension Survey reported a high prevalence of hypertension (23.2%) and prehypertension (41.3%) in the general population of China (33). Besides, there were no significant differences in hypertension prevalence between urban and rural residents (23.4 vs. 23.1%, P = 0.819) (33). This suggested that hypertension was not only prevalent among the urban population, but also among the rural population. Hypertension, especially uncontrolled and untreated hypertension, was associated with increased risk of total and cardiovascular mortality among general hypertensive population (34, 35). However, the possible confounders of the hypertension related cardiovascular mortality and all-cause mortality remain unclear. Therefore, it is necessary to determine the possible confounders that might be relevant to all-cause mortality and cardiovascular mortality among rural hypertensive subjects. In the present study, we enrolled subjects aged ≥35 years and the mean age was 57.21 ± 10.78 years (from 35 to 92 years) at baseline. The nine-year compulsory education in China started in 1986. Earlier, in rural areas of China, only few subjects could afford education, especially women. Data from our study inferred that in total 56.0% of hypertensive subjects (66.3% of women; 45.3% for men; P < 0.001) had primary or below school education. This result was significantly higher than previous studies held in rural or urban areas of China (33, 36). One possible reason could be that the previous studies enrolled general population. Hence, the average age was lower in these samples, which infers that younger subjects who were more likely to have better educational status were recruited. The relationship between educational levels and hypertension has been well-proved. Previous studies indicated that hypertensive subjects with poorly controlled BP are represented by low education level (37, 38). To our knowledge, this is the first study intended to evaluate the association of low education with all-cause mortality and cardiovascular mortality in rural hypertensive participants. The novel finding of the present study was that all-cause mortality and cardiovascular mortality were higher in less educated subjects than medium-high educated hypertensive subjects. This finding was in line with the previous literature data, and indicated that education is an important predictor of cardiovascular mortality and all-cause mortality (39–41). Woodward et al. analyzed nearly 90,000 general subjects and claimed that those with a primary education had an increased risk of CVD, cardiovascular mortality, and all-cause mortality compared with individuals with a tertiary education (42). In contrast, higher education was associated with increased alcohol consumption and inversely related to smoking, BP, cholesterol levels, and diabetes (42). However, in our study, subjects with medium-high education showed a relatively higher rate of current drinking and smoking but lower cholesterol levels.
There might be some possible explanations that were relevant to this association between low educational status and cardiovascular or all-cause mortality. First, in our study, we identified that hypertensive subjects with low education status tended to have higher rate of low annual income that those with medium-high education (18.0 vs. 10.0%, P < 0.05). Besides, low education subjects were more likely to be empty-nest subjects (48.2 vs. 32.2%, P < 0.001). These results indicated that low education subjects were unable to meet the basic needs of life and were unlikely to get enough social support from their relatives. Second, our results indicated that the prevalence of diabetes, dyslipidemia, and LVH were relatively higher among low educational status than among medium-high educational status, which suggested that more cardiovascular risk factors are associated with low education status. It has been proved that individuals with low education tend to have an increased number of CVD risk factors (43). Hu et al. found that almost half of the increased risk of incident acute myocardial infarction in low education groups was explained by the traditional risk factors (44). Third, among the enrolled participants, subjects with low educational status were older, which might explain the higher incidence of all-cause mortality and cardiovascular mortality than those with medium-high educational status. Even with these estimations, the definite mechanisms underlying the remainder of the increased risk correlated with low education remains to be determined. In addition to the relationship between educational status and cardiovascular/all-cause mortality, it has been demonstrated that low educational subjects were more likely to be associated with cardiometabolic factors, particularly diabetes, dyslipidemia, lower LVEF, and LVH. This was in line with previous studies (45, 46). In low education participants, it is possible to detect strong markers of systolic function impairment, including a significant reduction in LVEF, and of the prevalence of LVH.
One interesting finding of our study was that the antihypertensive treatment rate was significantly higher in low education group than in medium-high education group. This is in contrast with previous studies claiming that low education might adversely influence self-seeking behavior or access to healthcare. Previous studies confirmed that among hypertensives with poor BP control, a considerable group is represented by low education (37, 38). Even though participants with low education had relatively higher rate of antihypertensive treatment, the SBP was still higher among this group than the medium-high education group. This finding had been proved by other previous study which also reported that persons with low levels of education were more frequently treated than hypertensive subjects with higher levels of education (21). One possibility for this phenomenon might be due to the more awareness of non-drug approaches to lowering BP. They were more willingly to decrease BP by modifying lifestyle factors but not drug therapy (47). However, the relationship between education level and drug treatment of hypertension was not clearly elucidated in the literature. As for the possible reasons of this controversy, it might be relevant to the medication adherence. Even though there was a higher rate of antihypertensive treatment in low education group, subjects with low education might have a relatively lower levels of adherence which are associated with worse BP control, and adverse outcomes (48, 49). There were validated objective (e.g., pharmacy fill, electronic monitoring) and subjective (e.g., self-report) measures for assessing medication adherence (50). However, in our present study, we did not collect data about medication adherence. Therefore, further study was warranted in order to confirm this possibility. Another interesting finding of our study was that the incidence of obesity was relatively low in the low education group. A meta-analysis found that study region, age groups, gender, and observation period could affect the relationship between education and overweight/obesity (51). In our study, the mean age in low education group was higher compared with medium-high education group. As the age increased, the rate of obesity decreased simultaneously. This might partially account for the low incidence of obesity in low education participants. Besides, Mosli et al. found that individuals who had the highest income bracket with low levels of education might have greater odds of obesity (52). This indicates that the synergistic effect of income and education might lead to changes in the relationship between education and obesity. In our study, low education participants had relatively lower annual income compared with medium-high education (annual income ≤5,000 CNY/year: 18.0 vs. 10%).
Results of the present study concluded that low educational status at baseline was associated with high incidence of mortality. Since the educational status at baseline cannot be altered, it seemed that there was no way to control this risk factor to reduce mortality. However, that was not the case. To better control all-cause mortality and cardiovascular mortality, we should understand that it is not the actual educational status that affected the health. In fact, it is the relevant health knowledge or healthy lifestyle derived from education that played an important role in all-cause mortality and cardiovascular mortality. We can use education intervention to make up for the low education status. A previous study aimed to evaluate the effectiveness of a health education intervention in improving hypertension knowledge, prevention, and self-care practices among older hypertensive residents. This study confirmed that community-based health education intervention targeting old adults can increase hypertensive knowledge, and improve prevention and self-care practices of hypertension (53). Therefore, even though we cannot change the baseline education status, we can restrict mortality through community educational intervention.
Limitations
Inevitably, there are certain limitations to the present study. (1) The study only evaluated whether subjects had antihypertensive medication. It did not list specific drugs that were used in the study. (2) The recruited subjects were from one province of northeast China, therefore, the findings cannot be generalized to all subjects across the country. (3) The definitions of diabetes, dyslipidemia, and MetS were based on a single blood test which might have bias. (4) Although we had controlled for a range of common confounders, the possibility of unmeasured and residual confounding might have contributed to the risk of mortality, which might distort the associations observed in this study. (5) Data about medication, specific kinds of antihypertensive medication, and other related factors were not included in the present study which caused the inability to elucidate the possible reasons for relative higher rate of antihypertensive treatment in low education group compared to medium-high education group.
Conclusion
Our data clearly indicates a definite association between low educational status and mortality, which emphasizes the importance of education. To some extent, this finding has a significant guiding effect on policy making, and this policy should ensure that people from rural areas with health problems are not deprived due to educational opportunities. More community-based health educational interventions are encouraged to better control cardiovascular risk and mortality.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of China Medical University (Shenyang, China AF-SDP-07-1, 0-01). All procedures were performed in accordance with ethical standards. Written consent was obtained from all participants after they had been informed of the objectives, benefits, medical items and confidentiality agreement regarding their personal information. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SY contributed to the data collection, analysis, and interpretation. XG and HY contributed to data collection. GL and SY contributed to the data analysis. YS contributed to the study conception and design. All authors read and approved the final version of the manuscript.
Funding
This study was supported by grants from the National Key Research and Development Program from the Ministry of Science and Technology of China (Project Grant # 2018 YFC 1312400 and Sub-project Grant # 2018 YFC 1312403) and the China Medical University Youth Backbone Program project funds (grant no. QGZ2018037).
Acknowledgments
We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. (2004) 364:937–52. doi: 10.1016/S0140-6736(04)17018-9
2. Sun GZ, Li Z, Guo L, Zhou Y, Yang HM, Sun YX. High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. Lipids Health Dis. (2014) 13:189. doi: 10.1186/1476-511X-13-189
3. Li Z, Guo X, Zheng L, Yang H, Sun Y. Grim status of hypertension in rural China: results from Northeast China Rural Cardiovascular Health Study 2013. J Am Soc Hypertens. (2015) 9:358–64. doi: 10.1016/j.jash.2015.02.014
4. Ho JE, Enserro D, Brouwers FP, Kizer JR, Shah SJ, Psaty BM, et al. Predicting heart failure with preserved and reduced ejection fraction: the international collaboration on heart failure subtypes. Circ Heart Fail. (2016) 9:1161–70. doi: 10.1161/CIRCHEARTFAILURE.115.003116
5. Emdin CA, Anderson SG, Salimi-Khorshidi G, Woodward M, MacMahon S, Dwyer T, et al. Usual blood pressure, atrial fibrillation and vascular risk: evidence from 4.3 million adults. Int J Epidemiol. (2017) 46:162–72. doi: 10.1093/ije/dyw053
6. Rahimi K, Mohseni H, Kiran A, Tran J, Nazarzadeh M, Rahimian F, et al. Elevated blood pressure and risk of aortic valve disease: a cohort analysis of 5.4 million UK adults. Eur Heart J. (2018) 39:3596–603. doi: 10.1093/eurheartj/ehy486
7. Emdin CA, Rothwell PM, Salimi-Khorshidi G, Kiran A, Conrad N, Callender T, et al. Blood pressure and risk of vascular dementia: evidence from a primary care registry and a cohort study of transient ischemic attack and stroke. Stroke. (2016) 47:1429–35. doi: 10.1161/STROKEAHA.116.012658
8. Perumareddi P. Prevention of hypertension related to cardiovascular disease. Prim Care. (2019) 46:27–39. doi: 10.1016/j.pop.2018.10.005
9. Patel P, Ordunez P, DiPette D, Escobar MC, Hassell T, Wyss F, et al. Improved blood pressure control to reduce cardiovascular disease morbidity and mortality: the standardized hypertension treatment and prevention project. J Clin Hypertens. (2016) 18:1284–94. doi: 10.1111/jch.12861
10. Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2015) 386:2287–323. doi: 10.1016/S0140-6736(15)00128-2
11. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. (2003) 289:2560–72. doi: 10.1097/00132578-200307000-00027
12. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. (2020) 141:e139–596. doi: 10.1161/CIR.0000000000000746
13. Steffen PR, Smith TB, Larson M, Butler L. Acculturation to Western society as a risk factor for high blood pressure: a meta-analytic review. Psychosom Med. (2006) 68:386–97. doi: 10.1097/01.psy.0000221255.48190.32
14. Reddy KS, Prabhakaran D, Jeemon P, Thankappan KR, Joshi P, Chaturvedi V, et al. Educational status and cardiovascular risk profile in Indians. Proc Natl Acad Sci USA. (2007) 104:16263–8. doi: 10.1073/pnas.0700933104
15. Ma C, Song Z, Zong Q. Urban-rural inequality of opportunity in health care: evidence from China. Int J Environ Res Public Health. (2021) 18:7792. doi: 10.3390/ijerph18157792
16. Chen L, Shen W. Spatiotemporal differentiation of urban-rural income disparity and its driving force in the Yangtze River Economic Belt during 2000–2017. PLoS ONE. (2021) 16:e0245961. doi: 10.1371/journal.pone.0245961
17. Li Q, Guo J, Cao XQ, Yuan X, Rao KQ, Zheng Z, et al. Trend of non-communicable disease mortality for three common conditions in the elderly population from 2002 to 2010: a population-based study in China. Chronic Dis Transl Med. (2015) 1:152–7. doi: 10.1016/j.cdtm.2015.06.006
18. Liu L. Rural-Urban Disparities in Cardiovascular Disease Mortality Among Middle-Age Men in China. Asia Pac J Public Health. (2020) 32:436–9. doi: 10.1177/1010539520956446
19. Gong W, Wei X, Liang Y, Zou G, Hu R, Deng S, et al. Urban and rural differences of acute cardiovascular disease events: a study from the population-based real-time surveillance system in Zhejiang, China in 2012. PLoS ONE. (2016) 11:e0165647. doi: 10.1371/journal.pone.0165647
20. Yan R, Li W, Yin L, Wang Y, Bo J. Cardiovascular diseases and risk-factor burden in urban and rural communities in high-, middle-, and low-income regions of China: a large community-based epidemiological study. J Am Heart Assoc. (2017) 6.
21. Di Chiara T, Scaglione A, Corrao S, Argano C, Pinto A, Scaglione R. Education and hypertension: impact on global cardiovascular risk. Acta Cardiol. (2017) 72:507–13. doi: 10.1080/00015385.2017.1297626
22. Yu S, Guo X, Yang H, Zheng L, Sun Y. An update on the prevalence of metabolic syndrome and its associated factors in rural northeast China. BMC Public Health. (2014) 14:877. doi: 10.1186/1471-2458-14-877
23. Li Z, Guo X, Zheng L, Sun Z, Yang H, Sun G, et al. Prehypertension in rural northeastern China: results from the northeast China rural cardiovascular health study. J Clin Hypertens. (2014) 16:664–70. doi: 10.1111/jch.12378
24. Li T, Li G, Guo X, Li Z, Yang J, Sun Y. Predictive value of echocardiographic left atrial size for incident stoke and stroke cause mortality: a population-based study. BMJ Open. (2021) 11:e043595. doi: 10.1136/bmjopen-2020-043595
25. Li T, Li G, Guo X, Li Z, Yang J, Sun Y. The influence of diabetes and prediabetes on left heart remodeling: a population-based study. J Diabetes Complic. (2021) 35:107771. doi: 10.1016/j.jdiacomp.2020.107771
26. Yu S, Guo X, Yang H, Sun Y. Combination of hyperuricemia and metabolic syndrome is an independent and powerful predictor for left ventricular hypertrophy in rural Chinese. Ann Endocrinol. (2015) 76:264–71. doi: 10.1016/j.ando.2015.01.002
27. Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. (1977) 55:613–8. doi: 10.1161/01.CIR.55.4.613
28. Cuspidi C, Facchetti R, Sala C, Bombelli M, Negri F, Carugo S, et al. Normal values of left-ventricular mass: echocardiographic findings from the PAMELA study. J Hypertens. (2012) 30:997–1003. doi: 10.1097/HJH.0b013e328352ac39
29. Chen Y, Li G, Guo X, Ouyang N, Li Z, Ye N, et al. The effects of calculated remnant-like particle cholesterol on incident cardiovascular disease: insights from a general Chinese population. J Clin Med. (2021) 10:3388. doi: 10.3390/jcm10153388
30. Gaye B, Canonico M, Perier MC, Samieri C, Berr C, Dartigues JF, et al. Ideal cardiovascular health, mortality, and vascular events in elderly subjects: the three-city study. J Am Coll Cardiol. (2017) 69:3015–26. doi: 10.1016/j.jacc.2017.05.011
31. Arrich J, Lalouschek W, Müllner M. Influence of socioeconomic status on mortality after stroke: retrospective cohort study. Stroke. (2005) 36:310–4. doi: 10.1161/01.STR.0000152962.92621.b5
32. Notara V, Panagiotakos DB, Kogias Y, Stravopodis P, Antonoulas A, Zombolos S, et al. The impact of educational status on 10-year (2004–2014) cardiovascular disease prognosis and all-cause mortality among acute coronary syndrome patients in the Greek Acute Coronary Syndrome (GREECS) longitudinal study. J Prev Med Public Health. (2016) 49:220–9. doi: 10.3961/jpmph.16.005
33. Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in china: results from the china hypertension survey, 2012–2015. Circulation. (2018) 137:2344–56. doi: 10.1161/CIRCULATIONAHA.117.032380
34. Gu Q, Dillon CF, Burt VL, Gillum RF. Association of hypertension treatment and control with all-cause and cardiovascular disease mortality among US adults with hypertension. Am J Hypertens. (2010) 23:38–45. doi: 10.1038/ajh.2009.191
35. Huynh QL, Reid CM, Chowdhury EK, Huq MM, Billah B, Wing LM, et al. Prediction of cardiovascular and all-cause mortality at 10 years in the hypertensive aged population. Am J Hypertens. (2015) 28:649–56. doi: 10.1093/ajh/hpu213
36. Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. (2017) 135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250
37. Wrobel MJ, Figge JJ, Izzo JL Jr. Hypertension in diverse populations: a New York State Medicaid clinical guidance document. J Am Soc Hypertens. (2011) 5:208–29. doi: 10.1016/j.jash.2011.05.003
38. Lynch J, Smith GD, Harper S, Hillemeier M. Is income inequality a determinant of population health? Part 2. U.S. National and regional trends in income inequality and age- and cause-specific mortality. Milbank Quart. (2004) 82:355–400. doi: 10.1111/j.0887-378X.2004.00312.x
39. Andersson T, Pikkemaat M, Schiöler L, Hjerpe P, Carlsson AC, Wändell P, et al. The impact of diabetes, education and income on mortality and cardiovascular events in hypertensive patients: a cohort study from the Swedish Primary Care Cardiovascular Database (SPCCD). PLoS ONE. (2020) 15:e0237107. doi: 10.1371/journal.pone.0237107
40. Khaing W, Vallibhakara SA, Attia J, McEvoy M, Thakkinstian A. Effects of education and income on cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol. (2017) 24:1032–42. doi: 10.1177/2047487317705916
41. Mesceriakova-Veliuliene O, Kalediene R, Sauliune S. Changes in inequalities of mortality by education level in Lithuania between 2001 and 2014. Public Health. (2020) 182:88–94. doi: 10.1016/j.puhe.2020.02.010
42. Woodward M, Peters SA, Batty GD, Ueshima H, Woo J, Giles GG, et al. Socioeconomic status in relation to cardiovascular disease and cause-specific mortality: a comparison of Asian and Australasian populations in a pooled analysis. BMJ Open. (2015) 5:e006408. doi: 10.1136/bmjopen-2014-006408
43. Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. (1992) 82:816–20. doi: 10.2105/AJPH.82.6.816
44. Hu B, Li W, Wang X, Liu L, Teo K, Yusuf S. Marital status, education, and risk of acute myocardial infarction in Mainland China: the INTER-HEART study. J Epidemiol. (2012) 22:123–9. doi: 10.2188/jea.JE20100175
45. Gupta R, Kaul V, Agrawal A, Guptha S, Gupta VP. Cardiovascular risk according to educational status in India. Prev Med. (2010) 51:408–11. doi: 10.1016/j.ypmed.2010.08.014
46. Gupta R, Deedwania PC, Sharma K, Gupta A, Guptha S, Achari V, et al. Association of educational, occupational and socioeconomic status with cardiovascular risk factors in Asian Indians: a cross-sectional study. PLoS ONE. (2012) 7:e44098. doi: 10.1371/journal.pone.0044098
47. de Gaudemaris R, Lang T, Chatellier G, Larabi L, LauwersCancès V, Maître A, et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension. (2002) 39:1119–25. doi: 10.1161/01.HYP.0000018912.05345.55
48. Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. (2009)119:3028–35. doi: 10.1161/CIRCULATIONAHA.108.768986
49. Krousel-Wood M, Holt E, Joyce C, Ruiz R, Dornelles A, Webber LS, et al. Differences in cardiovascular disease risk when antihypertensive medication adherence is assessed by pharmacy fill versus self-report: the Cohort Study of Medication Adherence among Older Adults (CoSMO). J Hypertens. (2015) 33:412–20. doi: 10.1097/HJH.0000000000000382
50. Peacock E, Krousel-Wood M. Adherence to antihypertensive therapy. Med Clin North Am. (2017) 101:229–45. doi: 10.1016/j.mcna.2016.08.005
51. Kim TJ, Roesler NM, von dem Knesebeck O. Causation or selection – examining the relation between education and overweight/obesity in prospective observational studies: a meta-analysis. Obes Rev. (2017) 18:660–72. doi: 10.1111/obr.12537
52. Mosli HH, Kutbi HA, Alhasan AH, Mosli RH. Understanding the interrelationship between education, income, and obesity among adults in Saudi Arabia. Obes Facts. (2020) 13:77–85. doi: 10.1159/000505246
53. Ozoemena EL, Iweama CN, Agbaje OS, Umoke PCI, Ene OC, Ofili PC, et al. Effects of a health education intervention on hypertension-related knowledge, prevention and self-care practices in Nigerian retirees: a quasi-experimental study. Arch Public Health. (2019) 77:23. doi: 10.1186/s13690-019-0349-x
Keywords: education, hypertension, mortality, cardiovascular, rural
Citation: Yu S, Guo X, Li G, Yang H, Zheng L and Sun Y (2022) Low educational status correlates with a high incidence of mortality among hypertensive subjects from Northeast Rural China. Front. Public Health 10:951930. doi: 10.3389/fpubh.2022.951930
Received: 24 May 2022; Accepted: 08 August 2022;
Published: 25 August 2022.
Edited by:
Aliya Naheed, International Centre for Diarrhoeal Disease Research (ICDDR), BangladeshReviewed by:
Md. Ariful Islam, International Centre for Diarrhoeal Disease Research (ICDDR), BangladeshNantu Chakma, International Centre for Diarrhoeal Disease Research (ICDDR), Bangladesh
Copyright © 2022 Yu, Guo, Li, Yang, Zheng and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingxian Sun, c3VueWluZ3hpYW5jbXUxaEAxNjMuY29t
 Shasha Yu1
Shasha Yu1 Yingxian Sun
Yingxian Sun