- 1Department of Epidemiology and Biostatistics, School of Public Health, Peking University, Beijing, China
- 2Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing, China
- 3Institute for Global Health and Development, Peking University, Beijing, China
- 4National Health Commission Key Laboratory of Reproductive Health, Peking University, Beijing, China
Background: The reluctance of individuals to obtain solid vaccine-induced immunity represents a fundamental challenge to containing the spread of SARS-CoV-2, including its highly mutated variants. We aimed to assess vaccination acceptance and associated factors for the COVID-19 vaccine booster dose among elderly people (≥60 years old) in China, providing a theoretical and practical reference for universal vaccination policy.
Methods: A national anonymous survey was conducted in mainland China from May 25 to June 8, 2022, using a stratified random sampling method. Individuals 60 years of age and above were the target population. A chi-squared test and Cochran-Armitage test for trend were used to compare and examine vaccine acceptance rates by characteristics. Via a backward stepwise method, multivariable logistic regression models were established to assess factors associated with booster dose acceptance. Two-sided P < 0.05 was considered statistically significant.
Results: Of 3,321 eligible participants, 82.8% (95% CI: 81.5–84.1%) were willing to receive COVID-19 vaccine booster shots. Concerns about contraindications (38.3%), vaccine safety (32.0%), and limited movement (28.0%) were the main reasons for vaccine hesitancy. Nearly one-third still believed that the booster dose was unnecessary after receiving the initial vaccination. Older adults with a low level of perceived barriers (aOR = 1.86, 95% CI, 1.03–3.38), a high level of perceived benefit (aOR = 2.31, 95% CI, 1.38–3.87), and higher cues to action (moderate, aOR = 2.22, 95% CI, 1.39–3.56; high, aOR = 5.46, 95% CI: 3.44–8.67) were more likely to accept the booster dose. Other major factors affecting the booster dose acceptance rate were occupation, time spent on social media, vaccination history, and a high knowledge score for COVID-19 and vaccines. In addition, for those over 70 years of age, rising awareness of susceptibility could be a better gateway for improving their willingness to get vaccinated.
Conclusions: A total of 82.8% of recruited older adults were willing to receive the booster dose. Acceptance behaviors were closely related to occupation, time spent on social media, vaccination history, knowledge factors, perception of barriers, and benefit, as well as action cues. Targeted public health measures are a priority for improving the vaccination coverage of valid immunity among the elderly population, not only to prevent infection and poor prognosis caused by emerging variants but also to reduce the huge disease and economic burden caused by the long-term sequelae after SARS-CoV-2 infection.
Introduction
As a salient example of an infectious disease with profound economic, social, and health implications, coronavirus disease 2019 (COVID-19) has directly affected the health of 628.6 million people as of October 26, 2022, and has caused 6.6 million deaths (1, 2). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) changes over time, and Omicron (B.1.1.529) is the dominant variant at the time of publication (3, 4). With multiple spike mutations and high transmissibility and immune escape, it outcompeted former variants soon after it was first detected in November 2021 (3, 4). Undoubtedly, promoting the global uptake of initial COVID-19 vaccines and booster doses has become an urgent issue worldwide, and is closely related to the formation of herd immunity (5, 6). According to data released by the United Nations Population Division, the global population aged 60 years and above was 1.08 billion in 2021, accounting for 13.7% of the global population (7). The elderly population is a key factor in the fight against COVID-19. Recently, BA.4 and BA.5 subvariants have emerged as the dominant strains and have higher transmissibility and immune escape ability than previous Omicron subvariants (8). Given the high risk of contracting SARS-CoV-2 and poor prognosis, older adults are confronted by the need to achieve solid immunity via the initial COVID-19 vaccine or the booster dose (9, 10). Moreover, a recent cohort study suggested that older age and multiple underlying diseases were risk factors for the development of long COVID-19, while valid vaccination may reduce the chance of long-term sequelae (11).
The reluctance of people to obtain solid vaccine-induced immunity represents a fundamental challenge to containing the spread of SARS-CoV-2 (12, 13). According to a report about the fifth wave of COVID-19 in Hong Kong, China, people aged 60 or above accounted for 96% of all deaths, and 88% of the deaths were people that were either unvaccinated or received only one dose of COVID-19 vaccine (14). However, only 32.3% of the world's population has received booster doses against COVID-19, as of October 8, 2022 (15). The Joint Prevention and Control Mechanism of the State Council claimed that, as of November 4, 2022, 31.6% of the elderly (≥60 years old) in China have yet to receive booster shots (16). Another critical issue that needs to be highlighted is that the overall level of effective antibodies produced by older people after vaccination was lower than that produced by younger adults (10, 17). Obviously, identifying misperceptions that fuel vaccine hesitancy and creating effective communication strategies are global public health priorities (12, 13, 18). The health belief model (HBM) is a health education model that can change people's behavior by intervening in people's perception, attitude, and belief (19–21). Individual health beliefs, cues to action, and behavioral constraints (demographic characteristics, knowledge level, etc.) constitute a complete HBM (22–24). Individual health belief refers to an individual's thoughts on health and disease, including recognizing the severity of the disease and their susceptibility (perceived severity and susceptibility), understanding the benefit of taking preventive measures and obstacles in the process (perceived benefit and barriers), and an individual's judgment about his ability to perform a certain action (self-efficacy). Action cues refer to factors that prompt people to take preventive measures, including reminders from medical staff. Combining motivation theory, cognitive theory, and expectancy-value theory, the HBM was used to predict people's preventive health behaviors and implement health education (25, 26). In recent years, HBM has been widely used to predict and explain the acceptance of vaccines against COVID-19, measles, human papillomavirus, etc., among different populations and its influencing factors (27–32). Combining the findings across studies, people with high perceived susceptibility, high perceived severity, high perceived benefit, and high levels of action cues were more likely to get vaccinated. The level of perceived barriers was generally inversely related to vaccination intention (27–32).
The entire medical community has invested enormous efforts in developing and delivering COVID-19 vaccines, and vaccination campaigns among adults are in full swing, such as in China. The Chinese government has continued to encourage older people to get vaccinated, especially for booster shots (33, 34). Communities have also launched a series of campaigns to increase vaccination rates among older people (33–35). Given the current more infectious variant, decreased vaccine-induced antibody titers, and the special social status of elderly individuals, vaccination intention and influencing factors of the elderly were essential for promoting vaccination coverage. However, few studies have targeted the elderly population (≥60 years old). Although our previous study shows that 93.7% of Chinese adults were willing to receive a third dose, only 81.7% (67/82) of people over the age of 50 have exhibited a willingness to take the vaccine (19). Obviously, owing to the small sample size of elderly people, previous results are of limited significance and are not sufficient to guide practical efforts for improving vaccine coverage in the elderly population. Therefore, we conducted a new survey based on the original study and targeted people aged 60 and above in China with the aim of identifying factors that can fuel vaccine acceptance and provide theoretical and practical references for universal vaccination policy.
Methods
Study design, population, and sampling
This national anonymous cross-sectional survey was conducted in mainland China via an online platform called Wen Juan Xing (Changsha Ranxing Information Technology Co., Ltd., Hunan, China). Covering at least 2.6 million registered members in China, we could easily reach an authentic, diverse, and representative sample (21, 36). Questionnaires were distributed via the internet to the potential target groups in the sample bank of this professional data science company. Our inclusion criteria were as follows: (1) Chinese citizens; (2) ≥60 years old; (3) people who agreed to participate in this survey; and (4) completed the survey between May 25, 2022 and June 8, 2022. To recruit enough representative respondents, we randomly sampled potentially eligible subjects in 31 provinces according to the proportion of adults aged 60 and above reported in the Seventh National Census (37). For people who did not respond to the questionnaire, the platform conducted further random sampling and sent questionnaires according to the preset requirements, ensuring that sufficient and high-quality samples were obtained.
Integrating the findings of previous studies and expert opinions, we set the rate of COVID-19 vaccine booster acceptance as 87% (P = 0.87) among older people (38, 39). PASS software 15.0 (NCSS LLC., Kaysville, U.T., USA) was used to calculate the minimum sample size with an acceptance rate of 87%, an α of 0.05, and a two-sided confidence interval width of 0.2p (0.174), using the exact (Clopper-Pearson) method. After quality control and manual check procedures to exclude invalid questionnaires, a total of 3,321 eligible respondents were ultimately included in our analyses (Supplementary Table S1).
Questionnaire design
The questionnaire was constructed and revised by a panel of experts, including one public health expert and two epidemiologists specializing in infectious diseases (Supplementary material 2). We performed a presurvey before it was officially released to test the validity of the questionnaire (Bartlett's test of sphericity, P < 0.001). The reliability of this questionnaire (only for the scales in the questionnaire) was confirmed by Cronbach's alpha coefficient by different dimensions (all α > 0.75). Each question was followed by a reminder that all answers were supposed to reflect the reality and true thoughts of those older adults.
The primary outcome was the acceptance rate of the COVID-19 vaccine booster, defined as the proportion of participants who answered “yes” when asked whether they were willing to receive the COVID-19 vaccine booster dose if available. If a respondent had any concerns or reluctance, the questionnaire would automatically jump to the specific reasons for hesitation.
Sociodemographic characteristics and health status of the sample population were investigated, including region, age, sex, marital status, education level, occupation, income, history of chronic disease, and COVID-19 vaccination. The amount of time people spent checking the news about COVID-19 or vaccines on social media each day and people's satisfaction with the government's response to COVID-19 were also obtained.
For knowledge factors, we set six and four questions to determine the knowledge level of the elderly on COVID-19 and COVID-19 vaccines, respectively. Sources of SARS-CoV-2 infection, common symptoms, transmission routes, high-risk groups, self-protection measures, and herd susceptibility were the investigational scope of the former aspect, with a total of 19 scores. Scores of “0–6,” “7–13,” and “14–19” represented a “low,” “moderate,” and “high” degree, respectively. For the knowledge on COVID-19 vaccines component, we mainly focused on price, time for booster vaccination, immunity induced by vaccines, and adverse reactions after vaccination. Each correct choice received 1 point, and a total of four scores were assigned to this part. Then, all respondents were divided into three groups (score 0–1, 2–3, and 4) from low to high.
As one of the most common theories reflecting individual behavior change, the HBM is an organic combination of motivation theory, cognitive theory, and expectancy-value theory, which has been widely used to explain public attitudes toward vaccines and predict people's vaccination behavior (19–21). Considering the strong correlation between different factors of the original HBM, “self-efficacy” was not included in the adjusted HBM of our study. We chose five dimensions in our final questionnaire, including perceived susceptibility (two items), perceived severity (two items), perceived barriers (three items), perceived benefit (three items), and cues to action (three items). All questions were answered as either “very concerned/agree,” “concerned/not sure,” and “not concerned/disagree” through a three-point Likert scale, and scores of 3, 2, and 1 were assigned to the above answers in descending order. Finally, an individual's grade in each dimension was divided into “low,” “moderate,” and “high” in ascending order based on their total points.
Data analysis
We performed descriptive analyses to summarize the characteristics of the recruited population by frequencies and percentages. The independent Chi-squared test and Cochran-Armitage test for trend were used to compare the differences between groups stratified by the abovementioned characteristics. To identify factors that influence vaccination willingness, multivariable logistic regression analyses were performed in different groups of participants, including three age groups (≥60 years old, 60–69 years old, and ≥70 years old) and those who had not yet received the booster dose. All independent variables were added to our multivariable models, and adjusted odds ratios (aORs) and 95% CIs were calculated via a backward stepwise method (P < 0.2). The Hosmer and Lemeshow test was used to assess the goodness of model fitting. All statistical analyses in this study were conducted using SPSS 26.0 (IBM SPSS Inc., NY, USA) and R 4.1.3 (AT&T Bell Lab., Auckland, New Zealand), and two-sided P < 0.05 was considered statistically significant.
Results
Participant characteristics
A total of 3,321 respondents were eventually included in our analyses (Table 1), and 1,097 (33.0%) were aged 70 or above. Among them, 1,731 (52.1%) were female, 926 (27.9%) lost their spouses, 1,987 (59.9%) did not have a high school degree, and more than 80% were satisfied with the government's response to COVID-19. A total of 9.7% of them had never been vaccinated, even with a single dose. Of all the participants, 82.8% (95% CI, 81.5–84.1%) were willing to receive COVID-19 vaccine booster shots (Table 1). People who were younger, lived with spouses, had a higher education level, or had a vaccination history were more likely to accept. Additionally, the more time spent on social media following content about COVID-19 and vaccines, the higher the vaccination willingness (Ptrend < 0.05). Significant differences in vaccine acceptance were not found between groups stratified by region, sex, occupation, and economic condition (all P > 0.05).
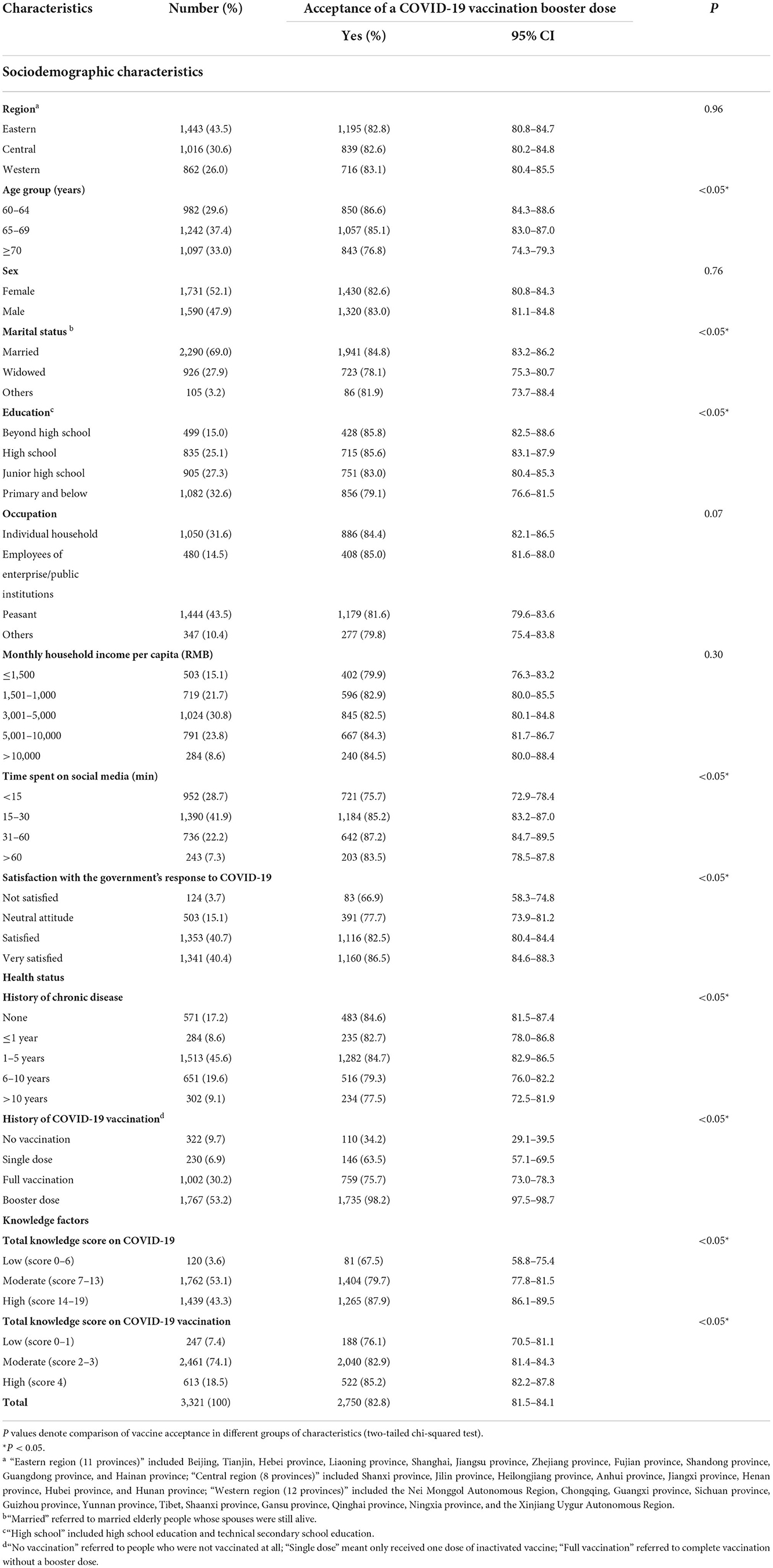
Table 1. Acceptance of a COVID-19 vaccine booster dose among older adults in China by demographic characteristics (n = 3,321).
Comparison of COVID-19 vaccine booster dose acceptance based on HBM
Concerns about the susceptibility of themselves and family members to SARS-CoV-2 infection indicated a higher acceptance rate of the booster dose among the older population (P < 0.05) (Table 2). On the “perceived severity” dimension, group differences between participants who agreed that their infection would cause severe illness or put their family at risk and participants who disagreed were not statistically significant (P > 0.05). Elderly people who believed in the safety and effectiveness of COVID-19 booster shots showed higher acceptance rates of 83.20% (81.90–84.50%) and 83.80% (82.40–85.10%), respectively. Similar results were exhibited for the dimension of the perceived benefit of the COVID-19 booster shot. Based on the analysis of five dimensions of the HBM, the higher the perception of susceptibility, benefit, and cues to action, the higher the vaccination acceptance rate among the elderly (all Ptrend < 0.05).

Table 2. Comparison of the acceptance rate of the COVID-19 vaccine booster dose based on the health belief model among the elderly population in China (n = 3,321).
Factors related to COVID-19 vaccine booster dose acceptance
For all 3,321 participants, our multivariable logistic regression indicated that the main factors related to COVID-19 vaccine booster dose acceptance were occupation, time spent on social media, and higher knowledge scores on COVID-19 and vaccines (Table 3). Vaccination history (single dose, aOR = 3.45, 95% CI, 2.33–5.10; full vaccination, aOR = 14.94, 95% CI, 11.16–20.01) significantly promoted vaccination. In addition, older adults with a low level of perceived barriers (low, aOR = 1.86, 95% CI, 1.03–3.38), a high level of perceived benefit (high, aOR = 2.31, 95% CI, 1.38–3.87), and higher cues to action (moderate, aOR = 2.22, 95% CI, 1.39–3.56; high, aOR = 5.46, 95% CI, 3.44–8.67) were more likely to accept the booster shots. However, occupation and knowledge scores for COVID-19 were no longer considered as the influential factors for participants aged 60–69 (Table 3). For individuals 70 years of age or older, high perceived susceptibility (high, aOR = 2.07, 95% CI, 1.15–3.73) and cues to action (high, aOR = 5.29, 95% CI, 2.40–11.68) indicated a higher vaccination willingness. The results of univariable logistic regression models of these three groups are shown in Supplementary Table S2.
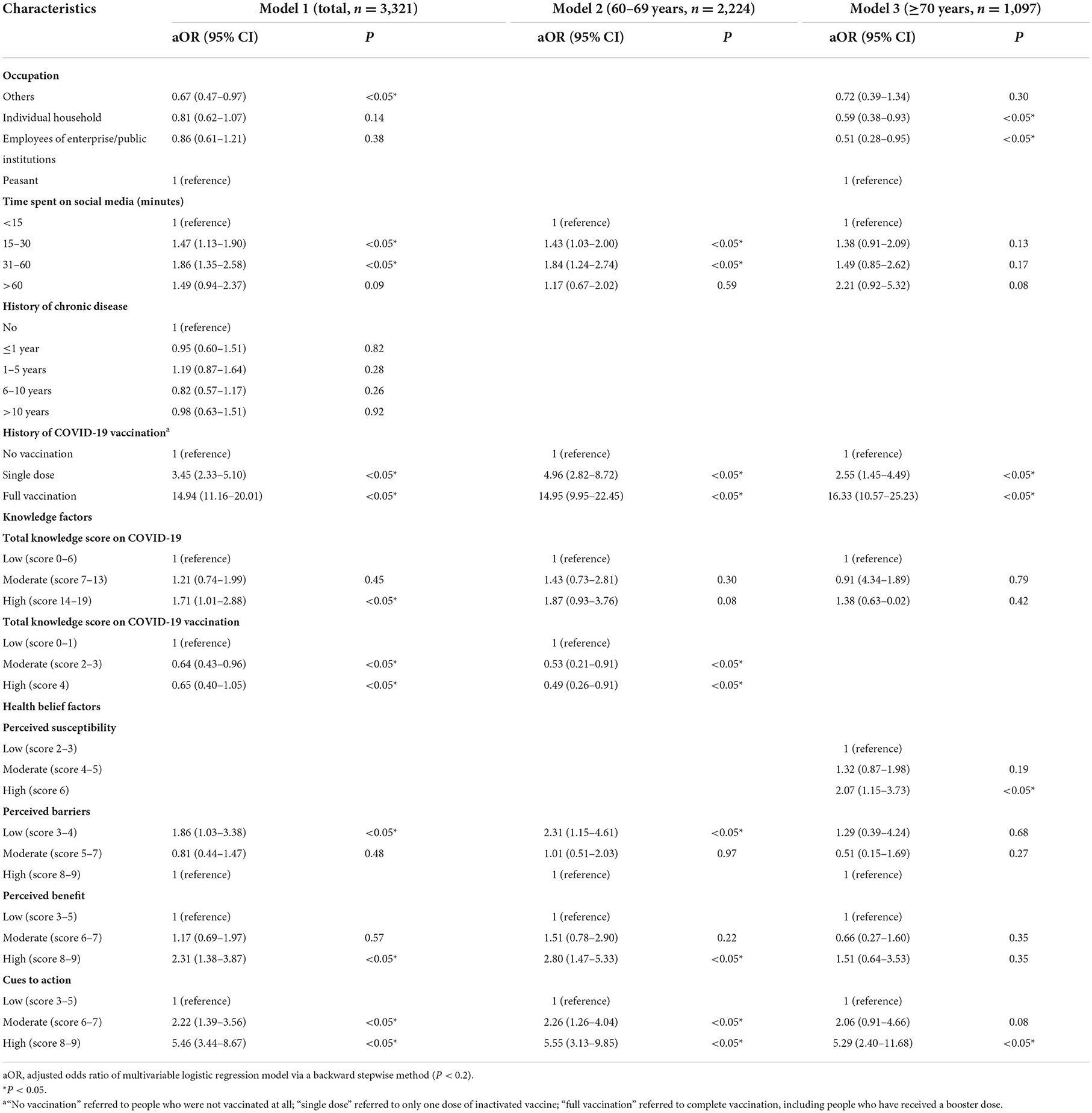
Table 3. Multivariable logistic regression of the factors associated with the acceptance of a COVID-19 vaccine booster dose among older people (n = 3,321).
Among the 1,554 participants who did not receive booster shots, 65.3% showed a willingness to receive the booster vaccination. A higher level of perceived benefit (high, aOR = 2.17, 95% CI, 1.18–4.01) and cues to action (moderate, aOR = 2.01, 95% CI, 1.16–3.49; high, aOR = 4.37, 95% CI, 2.56–7.43) indicated a higher willingness to receive a booster dose among those elderly people. Additionally, occupation, time spent on social media, and vaccination history could also affect the attitudes of elderly people toward booster vaccination (Figure 1).
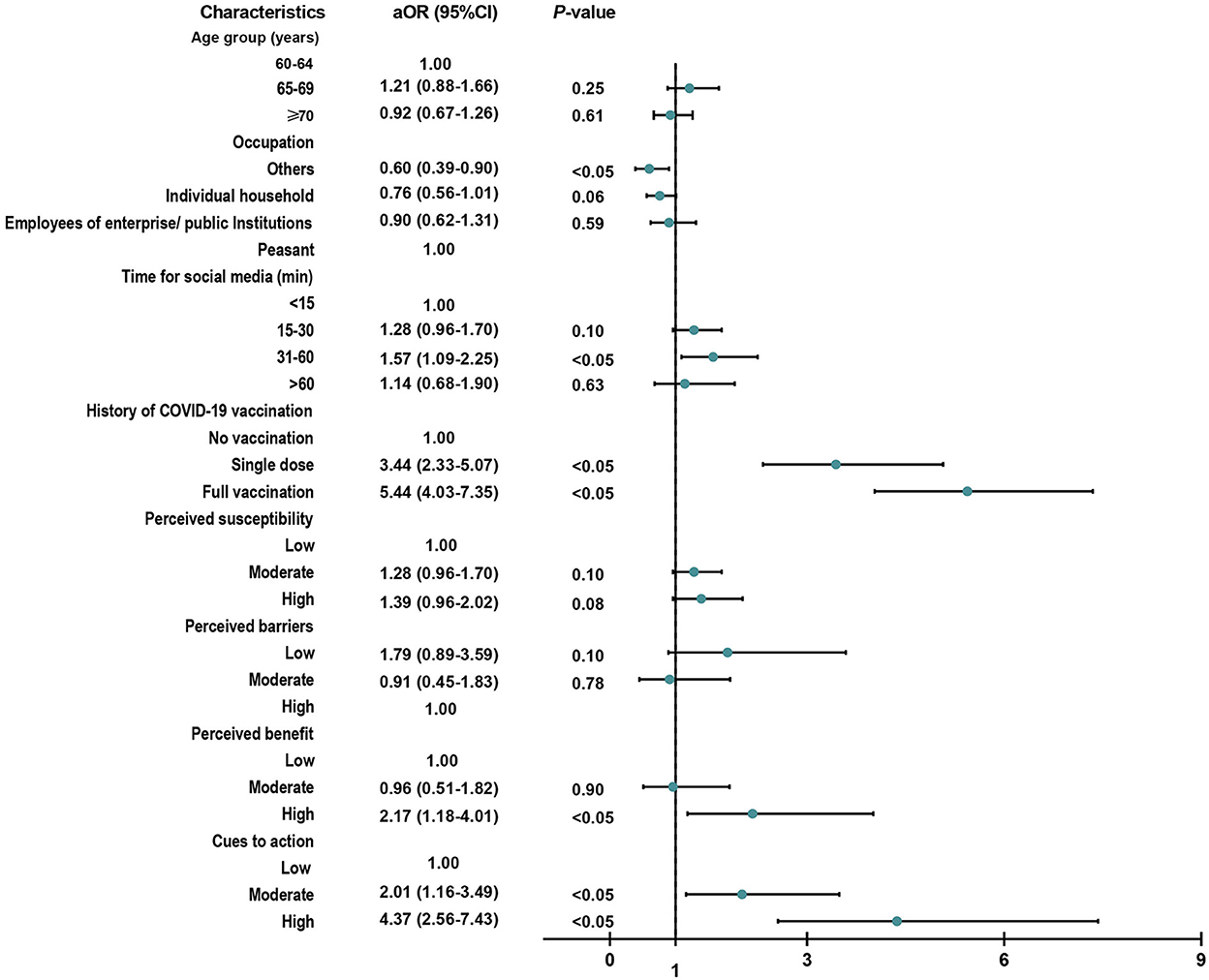
Figure 1. Factors related to vaccination acceptance among 1,554 participants who did not receive booster shots. aOR, adjusted odds ratio of multivariable logistic regression model via a backward stepwise method (P < 0.2).
Reasons for COVID-19 booster dose vaccine hesitancy stratified by age
Among the 571 (17.2%) participants who were reluctant or refused to receive the booster dose, nearly one-third were still unaware of the importance of booster shots, believing that it was unnecessary to receive a booster dose as they had already received one or two doses of the initial vaccination (Figure 2). A total of 38.3, 32, and 28% hesitated due to their concerns about contraindications, vaccine safety, and limited movement, respectively. Worrying about whether they were eligible for booster shots due to their existing diseases was a non-negligible reason for people aged 70 years or above. When ranking the four factors (social media, and advice from children, medical staff, and friends) that influence the elderly's vaccination willingness, 43.4% agreed that advice from children was the most important factor, while 32.7% supported advice from medical staff (Figure 3).
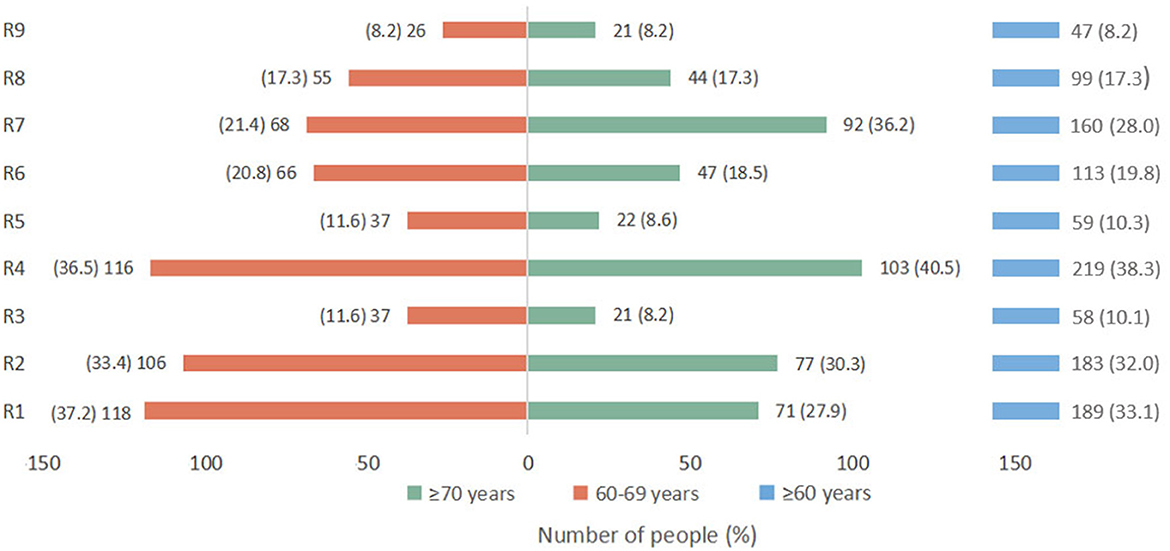
Figure 2. Reasons for responding “no” or “not sure” when asked about willingness to accept the COVID-19 vaccine booster dose (n = 571). “R1,” one or two doses of COVID-19 vaccines are already sufficient and a third dose is unnecessary; “R2,” the safety of the COVID-19 vaccine is not clear; “R3,” the efficacy of the COVID-19 vaccine is not clear; “R4,” severe illness and ineligibility for vaccination; “R5,” believing that they are healthy enough to fight COVID-19; “R6,” COVID-19 in China is well under control and there is no need to vaccinate; “R7,” limited movement; “R8,” believing that the vaccination process is complicated and time consuming; “R9,” other reasons.
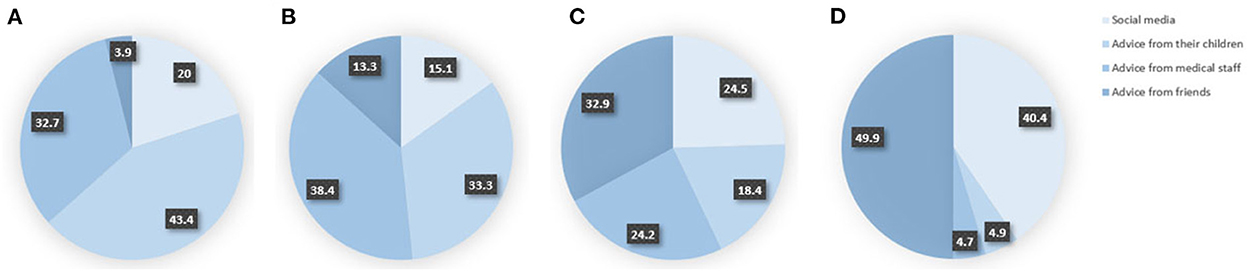
Figure 3. Ranking of the influence degree of four factors on the willingness of the elderly to receive the booster vaccination. (A) The most important, (B) the second most important, (C) the third most important, and (D) the least important.
Discussion
As a high-risk population with poor prognosis after infection, older adults are the key population for follow-up booster vaccination. We found that, of the 3,321 participants recruited, 82.8% (95% CI, 81.5–84.1%) were willing to receive COVID-19 vaccine booster shots. Concerns about contraindications, vaccine safety, and limited movement were the main reasons for vaccine hesitancy. Factors related to vaccine acceptance rate were occupation, time spent on social media, vaccination history, knowledge factors, and perception of barriers and benefit, as well as action cues. For the over 70s, increasing their awareness of susceptibility could be a better gateway for improving vaccination acceptance. Given the current global epidemic situation and the prevalence of highly infectious variants, it is likely that the subsequent second and third booster shots or vaccines against specific variants will soon be administered globally (40). Older adults have been prioritized for protection against severe illness and death through vaccination during this pandemic. Accordingly, our findings can help agencies develop targeted strategies to provide longer lasting immunity and greater protection against the evolving SARS-CoV-2 variants, which is important for the health of the elderly and the population as a whole.
Based on our study, 82.8% of 3,321 participants recruited were willing to receive COVID-19 vaccine booster shots. As the high-risk group for severe illness and death after SARS-CoV-2 infection, 87.6 million people (33.2%) aged 60 years and above in China have yet to receive booster shots as of August 10, 2022 (16). To date, very few studies have specifically focused on intentions to receive booster shots and the influencing factors among older adults, so our results can only be compared with specific subgroups of several existing studies (20, 39, 41). A large-scale nationwide survey conducted in China found that only 10.56% (30/284) of older adults (≥60 years old) were hesitant about receiving a booster shot (38), whereas in Jordan and Bangladesh (≥50 years old), the rates were 35.0 and 44.6%, respectively (20, 41). In addition, time spent on social media tracking news about COVID-19 and vaccines was also associated with vaccination acceptance (42). Our study also reflected the positive effect of vaccination history on receiving the booster shots, which was consistent with previous studies (19, 21, 39). Another surprising result was that, among older adults, the higher the knowledge scores on COVID-19 vaccines, the lower the willingness to take booster shots. More efforts are needed to regulate social media content and filter out misinformation (42, 43). The role of official social media in disseminating health information should be strengthened (42, 43).
Moreover, the HBM attempted to explain and predict the intention and behavior of the elderly with regard to receiving the COVID-19 vaccine booster shot from five dimensions (19–21). According to our multivariable analysis, people with low perceived barriers (model 1, aOR = 1.86, 95% CI, 1.03–3.38; model 2, aOR = 2.31, 95% CI, 1.15–4.61) and high perceived benefit (model 1, aOR = 2.31, 95% CI, 1.38–3.87; model 2, aOR = 2.80, 95% CI, 1.47–5.33) showed higher vaccination intention, which was generally consistent with previous studies (30, 44–46). However, for the perception of severity, none of our models found an association with vaccination willingness (all P > 0.05). Multiple studies have shown that higher perceived severity is negatively associated with vaccine hesitancy (38, 46, 47). For the over 70s, improving their awareness of susceptibility to SARS-CoV-2 variants could be a better gateway for making them more receptive to the vaccine. Of all the models, high action cues proved to have the most significant effect on vaccination willingness (all P < 0.05), which highlighted the importance and advantages of families and healthcare workers encouraging vaccination for eligible older persons. Similar results can also be verified (13, 19). Although the overall acceptance of COVID-19 booster shots among the elderly (≥60 years old) in China is relatively higher than that in other countries, efforts should also be made to remove barriers to vaccination given the large population base.
According to our results, nearly one-third of the elderly were still unaware of the importance of booster shots, believing a booster dose was unnecessary. According to a report on the fifth wave of COVID-19 in Hong Kong, China, people aged 60 years or more accounted for 96% of all deaths, and the mortality rate was 0.7% for those who were unvaccinated and 0.02% for those who had received two or three doses (14). Another concern is that the overall levels of effective antibodies produced by older people after vaccination are relatively lower than those produced by younger people (10, 17). We found that for those over 70 years of age, worrying about whether they were eligible for the booster shots due to their pre-existing severe or chronic diseases in acute phase was a non-negligible reason (40.5%, 103/254). As risk factors for SARS-CoV-2 infection and poor prognosis, comorbidities such as hypertension, diabetes, cardiovascular disease, and chronic respiratory disease are more common in older people (9, 10). Advanced age was also a risk factor for the disease (9, 10). Patients with well-controlled chronic diseases are generally considered eligible for vaccination (48). People with other medical conditions should consult health professionals in detail to determine whether they are contraindicated for vaccination (48). Regarding safety and effectiveness, data from the US, Germany, and South Korea all confirmed that prioritizing the most elderly for COVID-19 vaccination could save the most lives and surprisingly maximize remaining life expectancy (49).
We must recognize a practical problem, that is, the longer it takes to achieve herd immunity, the longer it will take for normal economic development to resume (12, 18, 50) and more people will likely face more complex situations. Our findings will help the assessment of older adults' attitudes toward the booster dose and exploration of the associated factors influencing their vaccination behavior, which could provide theoretical and practical implications for subsequent immunization strategies in older populations. However, this study also had some limitations. First, as with other online surveys, selection bias may exist. The accessibility of online surveys for the elderly was an inescapable problem as questionnaires were answered only by internet users. However, given the current global epidemic and the endless stream of variants, vaccine hesitation, especially in the elderly population, is a serious threat to people's lives and health. Considering the current requirements of epidemic prevention and control, we chose to conduct an online survey via a specialized data science company with a personal information database. We set up tips at the end of each question, repeatedly emphasizing that the subjective questions were supposed to be answered by the elderly independently. Second, people's acceptance of the booster dose was measured only by using the self-report questionnaire, and we were unable to assess it via a standard scale. In addition, our results need to be extrapolated with caution because of the differences in countries and theoretical models, and we also hope that large-scale offline surveys with more participants will be implemented as soon as feasible.
Conclusions
In this nationwide cross-sectional study, 82.8% of recruited older adults were willing to receive the COVID-19 vaccine booster dose. Acceptance behaviors were closely related to occupation, time spent on social media, vaccination history, knowledge factors, perception of barriers and benefit, and action cues. Concerns about contraindications, vaccine safety, and limited movement were the main reasons for vaccine hesitancy. In the current situation, promoting vaccination coverage of valid immunity among the elderly population is quite urgent, not only to prevent infection, severe illness, and death caused by emerging variants but also to reduce the huge disease and economic burden caused by the long-term sequelae of COVID-19.
Data availability statement
The datasets presented in this article are not readily available because the data will be further used in the following articles and research, and are not publicly available at this time. Requests to access the datasets should be directed to JL, anVlbGl1QGJqbXUuZWR1LmNu.
Ethics statement
This study met the requirements of the Declaration of Helsinki and was approved by the Institutional Review Board of Peking University (IRB00001052-21126). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization: CQ, MD, and WY. Methodology and analysis, visualization, and writing—original draft preparation: CQ. Review and editing: LT, WY, MD, QL, and ML. Supervision: JL. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers 72122001, 72211540398, and 71934002), the National Key Research and Development Project of China (grant numbers 2021ZD0114101, 2021ZD0114104, and 2021ZD0114105), the National Statistical Science Research Project (grant number 2021LY038), the Fundamental Research Funds for the Central Universities supported by Global Center for Infectious Disease and Policy Research and Global Health and Infectious Diseases Group of Peking University (grant number 202204), and the National Science and Technology Project on Development Assistance for Technology, Developing China-ASEAN Public Health Research and Development Collaborating Center (grant number KY202101004).
Acknowledgments
We would like to express our sincere gratitude to all the participants who enrolled in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.986916/full#supplementary-material
References
1. Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. (2021) 397:61–7. doi: 10.1016/s0140-6736(20)32228-5
2. University JH. COVID-19 Dashboard. Available online at: https://coronavirus.jhu.edu/map.html (accessed October 26, 2022).
3. Tracking SARS-CoV-2 variants. Available online at: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed July 01, 2022).
4. Reynolds CJ, Pade C, Gibbons JM, Otter AD, Lin K-M, Sandoval DM, et al. Immune boosting by B.1.1.529 (Omicron) depends on previous SARS-CoV-2 exposure. Science. (2022) 2022:eabq1841. doi: 10.1126/science.abq1841
5. Rauch S, Jasny E, Schmidt KE, Petsch B. New vaccine technologies to combat outbreak situations. Front Immunol. (2018) 9:1963. doi: 10.3389/fimmu.2018.01963
6. McDermott A. Core concept: herd immunity is an important-and often misunderstood-public health phenomenon. Proc Natl Acad Sci USA. (2021) 118:e2107692118. doi: 10.1073/pnas.2107692118
7. Dynamics, UNDoEaSAP,. Word Population Prospects 2022. Available online at: https://population.un.org/wpp/Download/Standard/Population/ (accessed October 23, 2022).
8. Mohapatra RK, Kandi V, Sarangi AK, Verma S, Tuli HS, Chakraborty S, et al. The recently emerged BA4 and BA5 lineages of Omicron and their global health concerns amid the ongoing wave of COVID-19 pandemic—Correspondence. Int J Surg. (2022) 103:106698. doi: 10.1016/j.ijsu.2022.106698
9. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
10. Ramasamy MN, Minassian AM, Ewer KJ, Flaxman AL, Folegatti PM, Owens DR, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. (2021) 396:1979–93. doi: 10.1016/s0140-6736(20)32466-1
11. Azzolini E, Levi R, Sarti R, Pozzi C, Mollura M, Mantovani A, et al. Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers. JAMA. (2022). doi: 10.1001/jama.2022.11691
12. Greenwood B. The contribution of vaccination to global health: past, present and future. Philos Trans R Soc Lond B Biol Sci. (2014) 369:20130433. doi: 10.1098/rstb.2013.0433
13. Bartoš V, Bauer M, Cahlíková J, Chytilová J. Communicating doctors' consensus persistently increases COVID-19 vaccinations. Nature. (2022) 606:542–9. doi: 10.1038/s41586-022-04805-y
14. Smith DJ, Hakim AJ, Leung GM, Xu W, Schluter WW, Novak RT, et al. COVID-19 mortality and vaccine coverage—Hong Kong Special Administrative Region, China, January 6, 2022–March 21, 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:545–8. doi: 10.15585/mmwr.mm7115e1
15. COVID-19 Vaccine Boosters Administered. Available online at: https://ourworldindata.org/covid-vaccinations (accesed October 26, 2022).
16. Joint Joint Prevention and Control Mechanism of The State Council (June 28 2022). Available online at: http://www.gov.cn/xinwen/gwylflkjz208/index.htm (accessed November 08, 2022).
17. Feikin DR, Higdon MM, Abu-Raddad LJ, Andrews N, Araos R, Goldberg Y, et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: results of a systematic review and meta-regression. Lancet. (2022) 399:924–44. doi: 10.1016/s0140-6736(22)00152-0
18. Jarrett C, Wilson R, O'Leary M, Eckersberger E, Larson HJ. Strategies for addressing vaccine hesitancy—a systematic review. Vaccine. (2015) 33:4180–90. doi: 10.1016/j.vaccine.2015.04.040
19. Qin C, Wang R, Tao L, Liu M, Liu J. Acceptance of a third dose of COVID-19 vaccine and associated factors in China based on health belief model: a national cross-sectional study. Vaccines (Basel). (2022) 10:89. doi: 10.3390/vaccines10010089
20. Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, et al. COVID-19 vaccine hesitancy among the adult population in Bangladesh: a nationwide cross-sectional survey. PLoS ONE. (2021) 16:e0260821. doi: 10.1371/journal.pone.0260821
21. Qin C, Wang R, Tao L, Liu M, Liu J. Association between risk perception and acceptance for a booster dose of COVID-19 vaccine to children among child caregivers in China. Front Public Health. (2022) 10:834572. doi: 10.3389/fpubh.2022.834572
22. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. (1988) 15:175–83. doi: 10.1177/109019818801500203
23. Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. (1984) 11:1–47. doi: 10.1177/109019818401100101
24. Cummings KM, Jette AM, Rosenstock IM. Construct validation of the health belief model. Health Educ Monogr. (1978) 6:394–405. doi: 10.1177/109019817800600406
25. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. (1974) 2:328–35. doi: 10.1177/109019817400200403
26. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. (2015) 30:566–76. doi: 10.1080/10410236.2013.873363
27. Chen H, Li X, Gao J, Liu X, Mao Y, Wang R, et al. Health belief model perspective on the control of COVID-19 vaccine hesitancy and the promotion of vaccination in China: web-based cross-sectional study. J Med Internet Res. (2021) 23:e29329. doi: 10.2196/29329
28. Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, et al. Health belief model, theory of planned behavior, or psychological antecedents: what predicts COVID-19 vaccine hesitancy better among the Bangladeshi adults? Front Public Health. (2021) 9:711066. doi: 10.3389/fpubh.2021.711066
29. Suess C, Maddock J, Dogru T, Mody M, Lee S. Using the Health Belief Model to examine travelers' willingness to vaccinate and support for vaccination requirements prior to travel. Tour Manag. (2022) 88:104405. doi: 10.1016/j.tourman.2021.104405
30. Tao L, Wang R, Han N, Liu J, Yuan C, Deng L, et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi-center cross-sectional study based on health belief model. Hum Vaccin Immunother. (2021) 17:2378–88. doi: 10.1080/21645515.2021.1892432
31. Vermandere H, van Stam MA, Naanyu V, Michielsen K, Degomme O, Oort F. Uptake of the human papillomavirus vaccine in Kenya: testing the health belief model through pathway modeling on cohort data. Global Health. (2016) 12:72. doi: 10.1186/s12992-016-0211-7
32. Zambri F, Perilli I, Quattrini A, Marchetti F, Colaceci S, Giusti A. Health Belief Model efficacy in explaining and predicting intention or uptake pertussis vaccination during pregnancy. Ann Ist Super Sanita. (2021) 57:167–73. doi: 10.4415/ann_21_02_09
33. Joint Joint Prevention and Control Mechanism of The State Council (September 29 2022). Available online at: http://www.gov.cn/xinwen/gwylflkjz208/index.htm (accessed October 08, 2022).
34. Council, tJPaCMotS,. Effective Prevention of Severe Illness: China Continues to Encourage the Elderly to Get Vaccinated. Available online at: http://www.gov.cn/xinwen/2022-04/07/content_5683922.htm (accessed October 08, 2022).
35. Council, tJPaCMotS,. Heartwarming Measures to Encourage Elderly People to Get Vaccinated Against COVID-19. Available online at: http://www.gov.cn/xinwen/2022-05/07/content_5689000.htm (accessed October 08, 2022).
36. Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines (Basel). (2020) 8:482. doi: 10.3390/vaccines8030482
37. Bulletin of the Seventh National Population Census (No. 5). Available online at: http://www.stats.gov.cn/tjsj/zxfb/202105/t20210510_1817181.html (accessed July 01, 2022).
38. Wu J, Li Q, Silver Tarimo C, Wang M, Gu J, Wei W, et al. COVID-19 vaccine hesitancy among Chinese population: a large-scale national study. Front Immunol. (2021) 12:781161. doi: 10.3389/fimmu.2021.781161
39. Tung TH, Lin XQ, Chen Y, Zhang MX, Zhu JS. Willingness to receive a booster dose of inactivated coronavirus disease 2019 vaccine in Taizhou, China. Expert Rev Vaccines. (2022) 21:261–7. doi: 10.1080/14760584.2022.2016401
40. Regev-Yochay G, Gonen T, Gilboa M, Mandelboim M, Indenbaum V, Amit S, et al. Efficacy of a fourth dose of Covid-19 mRNA vaccine against omicron. N Engl J Med. (2022) 386:1377–80. doi: 10.1056/NEJMc2202542
41. Rababa'h AM, Abedalqader NN, Ababneh M. Jordanians' willingness to receive heterologous prime-boost COVID-19 vaccination and vaccine boosters. Eur Rev Med Pharmacol Sci. (2021) 25:7516–25. doi: 10.26355/eurrev_202112_27452
42. Wang R, Qin C, Du M, Liu Q, Tao L, Liu J. The association between social media use and hesitancy toward COVID-19 vaccine booster shots in China: a web-based cross-sectional survey. Hum Vaccine Immunother. 2022:1-10. doi: 10.1080/21645515.2022.2065167
43. Elbarazi I, Al-Hamad S, Alfalasi S, Aldhaheri R, Dubé E, Alsuwaidi AR. Exploring vaccine hesitancy among healthcare providers in the United Arab Emirates: a qualitative study. Hum Vaccine Immunother. (2021) 17:2018–25. doi: 10.1080/21645515.2020.1855953
44. Wang R, Tao L, Han N, Liu J, Yuan C, Deng L, et al. Acceptance of seasonal influenza vaccination and associated factors among pregnant women in the context of COVID-19 pandemic in China: a multi-center cross-sectional study based on health belief model. BMC Pregnancy Childbirth. (2021) 21:745. doi: 10.1186/s12884-021-04224-3
45. Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. (2020) 14:e0008961. doi: 10.1371/journal.pntd.0008961
46. Baccolini V, Renzi E, Isonne C, Migliara G, Massimi A, De Vito C, et al. COVID-19 vaccine hesitancy among italian university students: a cross-sectional survey during the first months of the vaccination campaign. Vaccines (Basel). (2021) 9:vaccines9111292. doi: 10.3390/vaccines9111292
47. Ikiişik H, Akif Sezerol M, Taşçi Y, Maral I. COVID-19 vaccine hesitancy: A community-based research in Turkey. Int J Clin Pract. (2021) 75:e14336. doi: 10.1111/ijcp.14336
48. COVID-19 Vaccines Technical Guidence (Version 1). Available online at: http://www.nhc.gov.cn/xcs/yqfkdt/202103/c2febfd04fc5498f916b1be080905771.shtml (accessed June 23, 2022).
49. Goldstein JR, Cassidy T, Wachter KW. Vaccinating the oldest against COVID-19 saves both the most lives and most years of life. Proc Natl Acad Sci USA. (2021) 118:e2026322118. doi: 10.1073/pnas.2026322118
Keywords: COVID-19, vaccination, booster dose, hesitancy, old people
Citation: Qin C, Yan W, Du M, Liu Q, Tao L, Liu M and Liu J (2022) Acceptance of the COVID-19 vaccine booster dose and associated factors among the elderly in China based on the health belief model (HBM): A national cross-sectional study. Front. Public Health 10:986916. doi: 10.3389/fpubh.2022.986916
Received: 05 July 2022; Accepted: 22 November 2022;
Published: 15 December 2022.
Edited by:
Bijaya Kumar Padhi, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Francesco Andrea Causio, Università Cattolica del Sacro Cuore, ItalyRitika Kaur, Apollo Speciality Hospitals, Chennai, India
L. E. Cua Ngoc, Walailak University, Thailand
Copyright © 2022 Qin, Yan, Du, Liu, Tao, Liu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jue Liu, anVlbGl1QGJqbXUuZWR1LmNu
 Chenyuan Qin
Chenyuan Qin Wenxin Yan
Wenxin Yan Min Du
Min Du Qiao Liu1
Qiao Liu1 Liyuan Tao
Liyuan Tao Min Liu
Min Liu Jue Liu
Jue Liu