- 1Research Center for Public Health and Nutrition, Research Organization for Health, National Research and Innovation Agency, Bogor, Indonesia
- 2Regional Research and Development Agency South Sumatra Province, Palembang, Indonesia
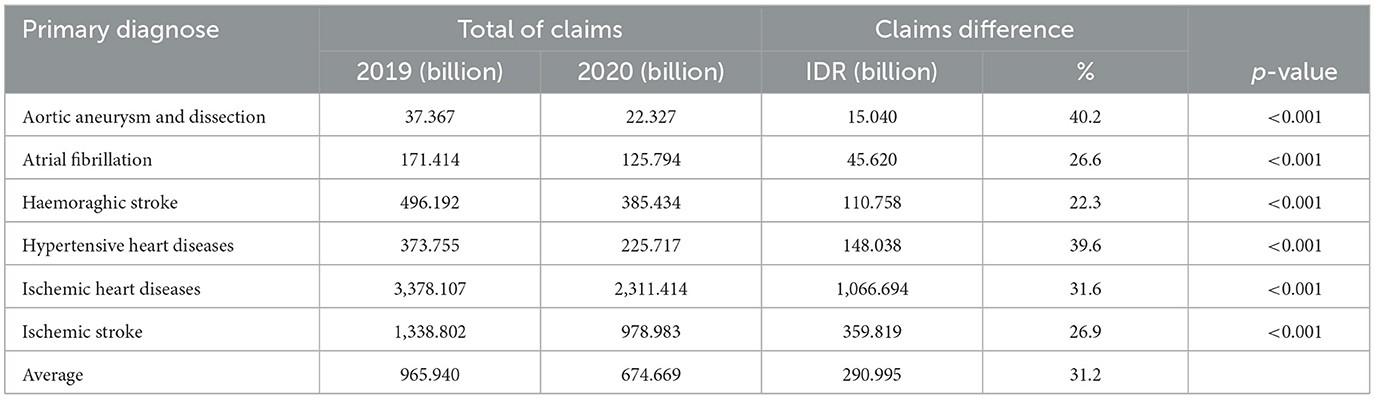
The disease burden related to non-communicable diseases is a major public health problem in Indonesia. About one-third of all deaths in Indonesia are caused by cardiovascular disease. This study describes the cost of cardiovascular disease from claims data for Advanced Referral Health Facilities at BPJS Kesehatan before and during the COVID-19 pandemic. We analyzed claims data on the National Health Insurance system managed by BPJS. The data comes from referral health facilities throughout Indonesia in 2019 and 2020. Cardiovascular service claims data by sex and age group were analyzed descriptively and with different tests between years. There was a decrease in the number of patients accessing cardiovascular services at referral health facilities for all genders, age groups, and types of main diagnoses, by around 27.8%, from 933,017 (2019) to 673,801 (2020). There was a significant decrease in total claims for all types of cardiovascular disease during the COVID-19 pandemic compared to before, especially the reduction in aneurysms and aortic dissection (40.2%) and hypertensive heart disease (39.6%). The decline also occurred in all sexes and age groups, with an average percentage decline of 31.2%. Our findings show that the reduction in the cost of cardiovascular disease claims goes hand in hand with the decrease in the number of cardiovascular patient visits. To guarantee treatment for cardiovascular disease patients during the COVID-19 pandemic, BPJS can maximize the telemedicine services that have been built. The organizer of the National Health Insurance program in Indonesia has developed a JKN mobile application that has the potential for telemedicine services guaranteed by JKN. On the other hand, BPJS needs to limit promotive and preventive budgets related to CVD so that it does not become a potential catastrophic financing.
Introduction
Globally, non-communicable diseases (NCDs) contribute to more than 60% of disability-adjusted life years (DALYs), 70% of deaths, and more than 80% of years of living with a disability. Cardiovascular diseases, which comprise ischemic heart disease, stroke, heart failure, peripheral arterial disease, and other heart and vascular conditions, represent 24% of NCD-associated DALYs and are the leading cause of global death and a major contributor to decreased quality of life (1, 2). In Indonesia, the burden of the disease related to non-communicable diseases is a major public health problem. About one-third of all deaths in Indonesia are caused by cardiovascular disease, with stroke and coronary heart disease being the main causes (3). In the last 10 years (2007–2017), there has been an increase in the burden of non-communicable diseases from 63% to 72%.
COVID-19 is a pandemic disease characterized by a respiratory infection caused by the coronavirus. It has spread worldwide since December 2019. The development of COVID-19 cases in Indonesia has been relatively fast since the first positive case was detected on 2 March 2020 (4). Patients with cardiovascular disease are more susceptible to infection and exacerbation of SARS-CoV-2 (5). Hypertension, diabetes, and atherosclerotic cardiovascular are independently associated with severe COVID-19 and, together with age and male sex, can be informative for predicting the risk of severe COVID-19 (6). In most cases, cardiovascular disease is a preventable condition that may be managed by reducing or eliminating a number of risk factors, such as hypertension, diabetes, dyslipidemia, obesity, smoking, insufficient physical activity, a poor diet, and alcohol use. In developing countries, lifestyles have changed dramatically due to rapid urbanization, which is characterized by an increase in poor diets and the adoption of sedentary lifestyles (7, 8).
The pandemic has harmed health services, including the difficulty of access to health facilities, lack of health personnel, and the social restrictions imposed. The movement of people has also become limited, not only healthy people but also sick people. One of the services that have fallen drastically is diagnosing and treating non-communicable diseases, with 69% of countries reporting this disorder (9). It is evident from an online survey in Indonesia in August–October 2020 that 20.4% of respondents reduced their routine use of health services (10).
The Social Security Administering Body, which was established through Law no. 24 of 2011, is a form of National Health Insurance providing Universal Health Coverage for all Indonesian people (11). The National Health Insurance Program is for all Indonesian residents, including foreigners who have worked for a minimum of 6 (six) months in Indonesia, and who have paid contributions. The number of participants reached 224,149,019 people in 2019 and 222,461,906 people in 2020 (12). This agency manages both outpatient and inpatient health services at first-level facilities and advanced referral facilities registered with Social Security Administering Body For Health (BPJS Kesehatan). The first-level facilities include Puskesmas, doctor's practice, Pratama clinic, and class D Pratama hospital. Advanced Level Referral Health Facilities include main clinics, general hospitals, and special hospitals. Payment for health services at hospitals uses the Indonesian Case Base Groups (INACBGs) system based on submitting claims from hospitals, both outpatient and inpatient (13).
Cancer and heart disease occupy the first and second catastrophic costs in National Health Insurance Program financing in Indonesia. In 2019, around 18.5% of the total National Health Insurance Program financing was catastrophic health financing (14, 15). During the pre-COVID-19 period, the health social security fund administered by the Social Security Administering Body experienced a budget deficit, and in the end, the government had to issue an allocation to cover the deficit (16). One of the contributors to the deficit is the adverse selection phenomenon, especially in people with catastrophic diseases, such as cardiovascular diseases. People with catastrophic diseases tend to register and take advantage of services managed by BPJS. Since it is well known that catastrophic diseases require large costs and long-term treatment (17). With no difference in financing pattern before the COVID-19 period (18), the Social Security Administering Body experienced a financial surplus during the pandemic (19).
The overall impact of the National Health Insurance Program contribution adjustment and low healthcare utilization has resulted in a financial surplus of the National Health Insurance fund. The National Health Insurance administrator management still needs to anticipate the period when the government announced that the COVID-19 pandemic has ended since that is the start of the COVID-19 financing under the National Health Insurance scheme (20). Considering the characteristics of cardiovascular diseases as catastrophic diseases and pandemic conditions, we would like to examine or know the pattern of cardiovascular disease financing in the period before and during the COVID-19 pandemic.
Materials and methods
Study design
This cross-sectional study was a secondary data analysis using the National Health Insurance claims data to describe patterns of visits and cardiovascular claims under the National Health Insurance Scheme.
Setting and data source
We analyzed data claims of the National Health Insurance managed by the Health Social Security Administration. We collected the data on outpatient and inpatient claims (in IDR) from all Advanced Level Referral Health Facilities (FKRTL) that collaborated with BPJS in Indonesia (34 provinces) in 2019 (before COVID-19) and 2020 (during COVID-19). In 2019, there were a total of 2,459 FKRTL and a total of 2,507 FKRTL that collaborated with The Social Security Administering Body (21). These claims data were payments by The Social Security Administering Body to service provider hospitals based on the Indonesia Case-Based Group (INA-CBG), which was equivalent to the local Diagnosis-Related Group (DRG). Expensive drugs, such as anticancer drugs, were not bundled with the goal of better predicting their use. Patients received full coverage for drugs identified in the national formulary at public hospitals (22).
Participants
The participants in this study were all patients suffering from cardiovascular diseases and utilizing BPJS services in 2019 and 2020. These patients were scattered among all hospitals that cooperate with BPJS in Indonesia. Patients consisted of all genders (male and female) and all age groups (0–80+ years).
Variable
Our data are not in the form of individual data but rather aggregate data for groups of individuals according to sex, age group, and type of disease. The claims data that we analyze are service claims data (main diagnosis) of cardiovascular disease based on the International Statistical Classification of Diseases and Related Health Problem Tenth Revisions (ICD-X) code, which includes aortic aneurysm and dissection (I71), atrial fibrillation (I48), hypertensive heart diseases (I11), hemorrhagic stroke (I619), ischemic stroke (I64), and ischemic heart diseases (I20, I21, I22, I23, I24, and I25). These disease codes are included in the criteria for diseases of the circulatory system (https://icd.who.int/browse10/2019/en#/).
Data management and analysis
Cardiovascular disease claims data were analyzed descriptively by adding up patients who had access to FKRTL according to sex characteristics, age group, and type of disease in 2019 and 2020 (Table 1). We calculated the difference in claims used by patients according to the characteristics of the type of disease in 2019 and 2020. From this difference in claims, we calculated the percentage and tested the difference in claims using the Wilcoxon test with a value limit of α = 0.05 (Table 2). Data claims were not normally distributed, so to enforce the different claim tests based on characteristics, we use Wilcoxon analysis (23). We calculated the difference in claims used by patients according to sex and disease characteristics in 2019 and 2020. From the difference in claims, we calculated the percentage (Table 3). This percentage was calculated as the difference in claims (in rupiahs) divided by the total claims in 2019 (in rupiahs), multiplied by 100%. All analyses were performed using the SPSS software.
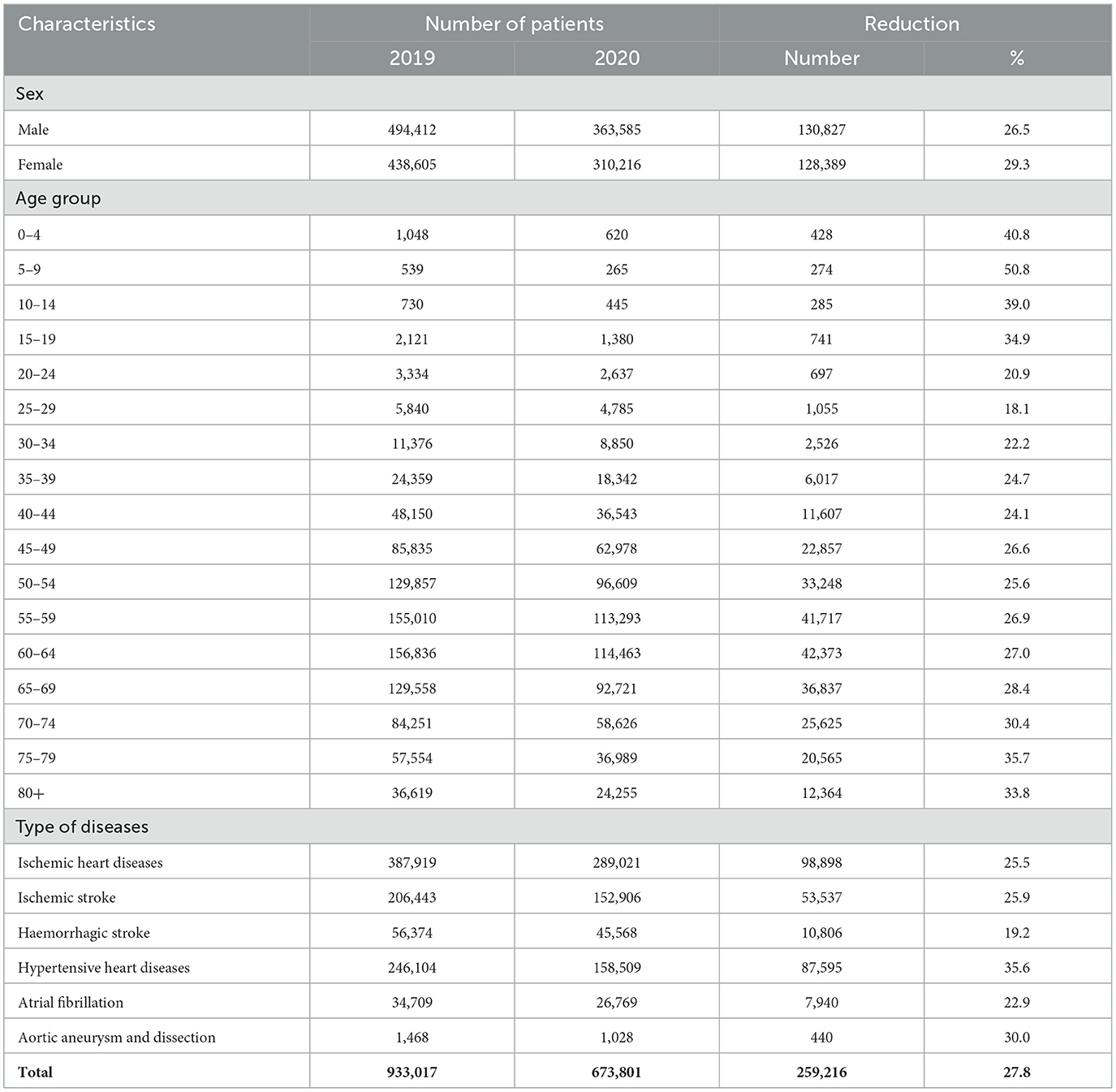
Table 1. Characteristic of cardiovascular disease patients in National Health Insurance claims, Indonesia, 2019–2020.
Results
The data analyzed in this study are claims data for several types of cardiovascular disease in 2019 and 2020 from all FKRTLs in Indonesia. Table 1 shows the number of patients who accessed cardiovascular services at FKRTL; in 2019, it was 933,017 people and decreased to 673,801 patients in 2020. In 2019 and 2020, more male patients accessed cardiovascular services in hospitals than female patients. When viewed from the percentage decrease, women (29.3%) are slightly higher than men (26.5%).
In 2019, the number of patients aged 0–4 years was more than those aged 5–14 years. In these 2 years, the number of patients will increase with increasing age upto 64 years. The number of patients will decrease again at the age of 65 years to more than 80 years. The number of patients decreased in all age groups from 2019 to 2020. However, looking at the percentage decrease in the number of patients, the 0–19 years and 70+ years experienced a 30–50% decrease.
The highest number of patients in 2019 and 2020 were cases of ischemic heart disease, followed by hypertensive heart diseases and ischemic stroke. The number of patients per type of disease decreased from 2019 to 2020. However, if we look at the percentage decrease in the number of patients, hypertensive heart diseases (35.6%) and aortic aneurysm and dissection (30.0%) patients experienced the most declines. Meanwhile, the number of hemorrhagic stroke patients decreased the least, less than one-fifth from 2019.
Ischemic heart disease and ischemic stroke dominated the largest total claims for treatment costs in 2019 (Table 2). The same pattern was also seen during the 2020 COVID-19 pandemic. There was a significant decrease in total claims for all types of cardiovascular disease during the COVID-19 pandemic compared to before the 2019 pandemic. The average decline for each of the six cardiovascular disease claims was 290,995 billion, with an average percent decrease of 31.2%. However, looking at the percentage of the largest decrease, it is in the case of aortic aneurysm and dissection, which is 40.2%, followed by hypertensive heart diseases with a 39.6% reduction in claim costs. Meanwhile, the lowest percentage decrease in total claims was in cases of hemorrhagic stroke, which did not decrease by a quarter of the cost before COVID-19 (22.3%).
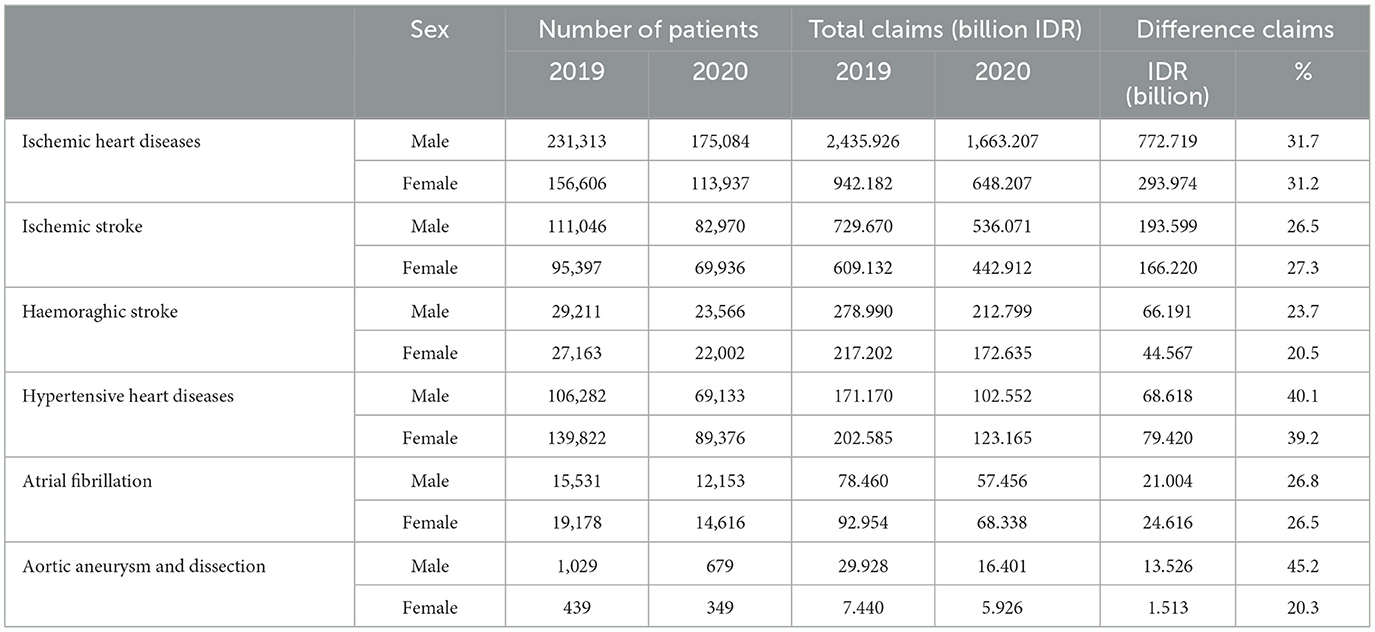
Table 3 shows the difference in the cost of NCD claims by gender from 2019 to 2020. Based on the nominal cost, the biggest decrease is the treatment of ischemic heart disease in male and female patients, followed by an ischemic stroke in male and female patients. However, in the case of hypertensive heart disease, the cost reduction was more for female patients than male patients. The smallest nominal decrease was in aortic aneurysm and dissection cases in women, followed by men.
However, when viewed from the percentage of costs, the largest percentage decrease was in the cost of aortic aneurysm and dissection in men (45.2%), followed by the percentage decrease in the cost of hypertensive heart disease in men (40.1%) and in women (39.2%). The lowest percentage of reduction in financing was aortic aneurysm and dissection in women (20.3%) and hemorrhagic stroke in women (20.5%).
Discussion
This study indicates that visits and claims of cardiovascular disease patients between before and after the COVID-19 pandemic showed a decrease, with a 31.2% decrease in claims. This decline in inpatient visits to health facilities also occurred in other countries. In Singapore, the COVID-19 pandemic was associated with a 9.3% reduction in doctor visits and inpatient visits and a 2.7% decrease in the likelihood of being diagnosed with a chronic condition (24). In Colombia, compared to 2019–2020, total emergency health services decreased from 83,925 to 71,611, with 133 per 100,000 person-months (25).
The decline in cardiovascular patient visits in Indonesia can be caused by various things, including decreased community mobility due to social distancing policies with changing policy methods ranging from Large-Scale Social Restrictions (PSBB) to Community Activity Restrictions (PPKM) with different levels in each region (26). This condition is in line with the BPJS report, which stated that there was a surplus in non-COVID-19 disease financing during the pandemic due to decreased health service utilization (20).
During the COVID-19 pandemic, National Health Insurance was in a surplus condition. This condition was not only caused by the decrease in utilization rates during the COVID-19 pandemic but also by several factors that contributed to the National Health Insurance surplus, namely adjustments to National Health Insurance rates, improvements in strategic purchasing in health services, and improvement in service quality (27, 28).
Furthermore, some people choose to be vigilant so as not to contract COVID-19 and choose to do activities and work at home, although some are less vigilant (3). This condition is also supported by the Indonesian association of specialist doctors who warn the public to postpone hospital visits if they are not in an urgent condition (29).
The COVID-19 pandemic has not only impacted public health but has also affected the Indonesian economy, education, and social life. One of the economic impacts occurred due to the implementation of PPKM and PSBB policies, namely government policies that prohibit people from congregating and carrying out activities outside the home. People are required to remain in their houses. With this regulation, community activities, employees, workers, and factory workers are forced to be sent home or reduced time for work and to terminate employment, causing unemployment (30, 31). When unemployment occurs, income automatically decreases dramatically. One of the reasons for this decline in income is the ability to pay health insurance premiums. The Health Social Security Administration data show that during the COVID-19 pandemic, the participation coverage rate dropped significantly (28).
Based on gender, the decrease in cardiovascular patient visits was more in female cardiovascular patients. More male patients access cardiovascular services in hospitals than female patients (32). Female heart disease patients are more likely to receive less treatment than male patients. Moreover, public health conditions generally focus more on the life cycle of women and breast cancer (33). During the COVID-19 pandemic, naturally, women tend to be more careful not to contract the coronavirus than men, so they choose to postpone visits even though they are sick.
The average cost per type of disease based on age has consistently decreased after the COVID-19 pandemic with the same pattern. Younger groups are generally healthier; and costs are concentrated among fewer individuals (34). This is one of the reasons why the financing of heart disease is getting bigger as the age group increases both in 2019 and 2020. At a young age, patients with cardiovascular disease have an ideal body fat composition and muscle mass and assume that their disease condition will be better. They have worsened when contracting the coronavirus in the hospital, thus choosing to postpone visits (35, 36). In contrast to older adults with cardiovascular disease who lose weight, most lose lean mass, which may contribute to an increased risk of cardiovascular events following weight loss, as body fat composition and muscle mass change with age, it is more urgent to visit health facilities consistently (37).
The phenomenon of a decrease in visits and a decrease in claims for National Health Insurance patients in cases of cardiovascular disease is not a reduction in the financing but is a pseudo-reduction, and there is a threat of an explosion in claims cases in future (38). Not to mention the condition of people's mental pressure from a wave of job loss cases, increasing poverty and unhealthy lifestyles threaten future cardiovascular disease cases (39, 40). A healthy lifestyle so as not to be exposed to expensive diseases is a substantial way to control the financing of cardiovascular disease.
A study in California in 2021 showed that during the COVID-19 pandemic, cardiovascular disease patients preferred telemedicine instead of attending health services which also aimed to control the cost of heart disease (41). This condition of using telemedicine is more common in developed countries (42). Meanwhile, in Indonesia, non-communicable disease control policies in this pandemic era have encountered more obstacles. More people delay visits to health facilities and wait for guidelines for visiting health facilities from expert doctors and specialists. The legal umbrella for telemedicine regulation has not yet been widely developed in Indonesia. Health facilities develop different telemedicine models by utilizing telecommunication application features, such as chatting or telephone to communicate with patients.
On the other hand, the Health Social Security Administration, as the operator of the National Health Insurance program in Indonesia, has developed a JKN mobile application that has the potential for telemedicine services to be guaranteed by the National Health Insurance (JKN). The advantages of the current Mobile JKN application are teleconsultation, the development of online prescribing, online queues, and health education for JKN participants (43). Technology-based screening, historical recording of participant claims history, and real-time data based on best practices are the directions for future development of the JKN program implemented by the Korean state since the COVID-19 pandemic (44). All of these efforts are carried out to prevent a spike in high-cost claim cases in future and prepare for another upcoming pandemic by strengthening the mobile JKN application. The Government of the Republic of Indonesia has also developed crowdfunding regulations for low-cost disease cases, so it is hoped that more savings will be made to prepare for financing claims for cardiovascular cases in future (45, 46). The next task of the Government and the community is to invite more people to adopt a healthy lifestyle to avoid cardiovascular disease and not aggravate existing disease conditions so that they do not become a burden on claims in future.
This study uses secondary data derived from the cost of health service claims from all hospitals in Indonesia. Secondary data are the given data; therefore, specific information cannot be obtained as complete as primary data.
The advantage of the study using national data is BPJS Health claims data so that it can describe financing conditions nationally. Meanwhile, the limitation of this study is the secondary data that are the given data; therefore, specific information cannot be obtained as complete as primary data. The available covariate adjustment factors are limited to the patient's age and sex. Further studies need to provide more adjustment factors to get a more accurate value of the difference in the claims, such as regional variations, service utilization time (months), and types of referral facilities.
Conclusion
There has been a decrease in claims for cardiovascular care costs from before the COVID-19 pandemic, both in general and for all genders and age groups. Our findings show that the reduction in the cost of cardiovascular disease claims goes hand in hand with the decrease in the number of cardiovascular patient visits. Taking into account the factor of social restrictions during COVID-19, which affected the number of visits, when social restrictions are lifted or life returns to normal, the possibility of CVD visits will be the same as before COVID-19. Going forward, JKN needs to expand the scope of promotional and preventive services, especially for catastrophic diseases such as CVD, thereby reducing the burden on JKN in future. Health facilities that work with JKN need to prepare for better health service management in dealing with a pandemic, including digitizing services for patients, including CVD patients.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the raw data for this research cannot be accessed by the public. This is in accordance with data owner regulations (Social Security Administering Body for Health) that claims data is confidential and may not be consumed by the public. Officially we made a request on a clear proposal to the Data Management Division before the data delivered and used for our analysis and developing the manuscript. Requests to access these datasets should be directed to bnVncmFoZW5pX3dwQHlhaG9vLmNvbQ==.
Ethics statement
This study had received ethical approval from the Health Research Ethics Committee, National Institute of Health Research and Development (HREC-NIHRD) with a letter number LB.02.01/2/KE.241/2021, on May 06, 2021. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
WPN, ER, and TR: conceptualization, methodology, writing—original draft, and writing—review and editing. RM: methodology, data curation, formal analysis, writing—original draft, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
The research was funded by NIHRD MOH and the publication fee was paid by the Regional Research and Development Board of South Sumatra.
Acknowledgments
The authors would like to express gratitude to BPJS Kesehatan (Social Security Administering Body for Health), Indonesia, who gave us the claims data of the JKN program that we used in our research. We also thank our best friend Nunik Kusumawardani, PhD, who has provided guidance during the research and is currently resting peacefully in heaven.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: a systematic review. BMC Public Health. (2018) 18:1–11. doi: 10.1186/s12889-018-5806-x
2. Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. (2019) 74:2529–32. doi: 10.1016/j.jacc.2019.10.009
3. Purnama SG, Susanna D. Hygiene and sanitation challenge for COVID-19 prevention in Indonesia. Kesmas. (2020) 15:6–13. doi: 10.21109/kesmas.v15i2.3932
4. WHO. Coronavirus Disease 2019 (COVID-19) Situation Report-42 Data as Reported by 10 AM CET 02 March 2020. World Health Organization (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200302-sitrep-42-covid-19.pdf?sfvrsn=224c1add_2 (accessed March 21, 2022).
5. Xu J, Xiao W, Liang X, Shi L, Zhang P, Wang Y, et al. A meta-analysis on the risk factors adjusted association between cardiovascular disease and COVID-19 severity. BMC Public Health. (2021) 21, 1533. doi: 10.1186/s12889-021-11051-w
6. Matsushita K, Ding N, Kou M, Hu X, Chen M, Gao Y, et al. The relationship of COVID-19 severity with cardiovascular disease and its traditional risk factors: a systematic review and meta-analysis. Glob Heart. (2020) 15:1–14. doi: 10.5334/gh.814
7. Ciumărnean L, Milaciu MV, Negrean V, Oră?an OH, Vesa SC, Sălăgean O, et al. Cardiovascular risk factors and physical activity for the prevention of cardiovascular diseases in the elderly. Int J Environ Res Public Health. (2022) 19:207. doi: 10.3390/ijerph19010207
8. Alhabib KF, Batais MA, Almigbal TH, Alshamiri MQ, Altaradi H, Rangarajan S, et al. Demographic, behavioral, and cardiovascular disease risk factors in the Saudi population: results from the prospective urban rural epidemiology study (PURE-Saudi). BMC Public Health. (2020) 20:1–14. doi: 10.1186/s12889-020-09298-w
9. WHO. Pulse Survey on Continuity of Essential Health Services During the COVID-19 Pandemic. Geneva: WHO (2020).
10. Rahayu S, Cahyani RA, Utomo B, Syarief S. Impact of COVID-19 pandemic on health services utilization in Indonesia. Working Paper (2021).
11. Minister of Law and Human Rights of the Republic of Indonesia. Law Number 24 of 2011 concerning the Healthcare and Social Security Agency. Law Number 24 of 2011 Indonesia (2011).
12. The Healthcare Social Security Agency. The Healthcare and Social Security Agency 2020 program management report and 2020 financial report. (2021). Available online at: https://Bpjs-Kesehatan.Go.Id/ (accessed March 21, 2022).
13. Indonesian Ministry of Health. Regulation of the Minister of Health of the Republic of Indonesia Number 28 of 2014 Concerning Guidelines for Implementation of the National Health Security Program. Number 28 of 2014 2014 p. 2004-6.
14. Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Suparmi, Achadi EL, et al. Universal health coverage in Indonesia: concept, progress, and challenges. Lancet. (2019). 393:75–102. doi: 10.1016/S0140-6736(18)31647-7
15. Kumalasari ND, Rahem A, Presley B, Setiawan E. Direct medical cost analysis among coronary heart disease and heart failure outpatients at one hospital. J Manage Pharm Pract. (2019) 9:38170. doi: 10.22146/jmpf.38170
16. Nugraheni WP, Zahroh AH, Hartono RK, Nugraha RR, Chun CB. National health insurance deficit in Indonesia: identification of causes and solutions for resolution. Glob J Health Sci. (2020) 12:58. doi: 10.5539/gjhs.v12n13p58
17. Asyrofi D, Ariutama I. Deficit of health social security fund in national health insurance program: a case study of BPJS Kesehatan. J Ekon Stud Pembangunan. (2019) 11:116–30. doi: 10.17977/um002v11i22019p116
18. Indonesian Ministry of Health. Amendment to the Regulation of the Minister of Health Number 52 of 2016 Concerning Health Service Rates Standards in the Implementation of the Health Insurance Program. Indonesian Ministry of Health (2016).
19. BPJS Kesehatan. 2020 Health DJS Cashflow Surplus, Satisfaction with the JKN Program Increases. BPJS Kesehatan (2021).
20. Mukti AG, Jaya C, Suhard RL. Current condition of social security administrator for health (BPJS Kesehatan) in Indonesia: contextual factors that affected the national health insurance. Med J Indonesia. (2022) 31:87–90. doi: 10.13181/mji.com.226296
22. Ng JYS, Ramadani RV, Hendrawan D, Duc DT, Kiet PHT. National health insurance databases in Indonesia, Vietnam and the Philippines. Pharmacoecon Open. (2019) 3:517–26. doi: 10.1007/s41669-019-0127-2
23. Lee SW. Methods for testing statistical differences between groups in medical research: statistical standard and guideline of life cycle committee. Life Cycle. (2022) 24:2. doi: 10.54724/lc.2022.e1
24. Ahn S, Kim S, Koh K. Changes in healthcare utilization, spending, and perceived health during COVID-19: a longitudinal study from Singapore. SSRN Electron J. (2020) 2020:13715. doi: 10.2139/ssrn.3695416
25. Grunau B, Helmer J, Lee S, Acker J, Deakin J, Armour R, et al. Decrease in emergency medical services utilization during early stages of the COVID-19 pandemic in British Columbia. Can J Emerg Med. (2021) 23:237–41. doi: 10.1007/s43678-020-00062-y
26. Yanti B, Wahyudi E, Wahiduddin W, Novika RGH, Arina YMD, Martani NS, et al. Community knowledge, attitudes, and behavior towards social distancing policy as prevention transmission of COVID-19 in Indonesia. J Admin Kesehatan Indonesia. (2020) 8:4. doi: 10.20473/jaki.v8i2.2020.4-14
27. COVID-19 Health System Response Monitor Republic of Indonesia (2021). Available online at: http://apps.who.int/iris/ (accessed February 26, 2023).
28. Sparrow R, Dartanto T, Hartwig R. Indonesia under the new normal: challenges and the way ahead. Bull Indones Econ Stud. (2020) 56:269–99. doi: 10.1080/00074918.2020.1854079
29. Widysanto A, Kurniawan A, Pratama N, Lugito H, Yuniarti M, Gunawan C, et al. Experience of using tocilizumab for treatment in Indonesian patients with severe COVID-19. Cytokine. (2021) 138:1–4. doi: 10.1016/j.cyto.2020.155393
30. Fajar M, Rizky Prasetyo O, Fajar M, Prasetyo OR, Nonalisa S. Forecasting Unemployment Rate in the time of COVID-19 pandemic using google trends data (Case of Indonesia) new criteria view project indikator official view project forecasting unemployment rate in the time of COVID-19 pandemic using google trends data (Case of Indonesia) statistics indonesia (Badan Pusat Statistik). Int J Sci Res. (2020) 6:29–33.
31. Susilawati S, Falefi R, Purwoko A. Impact of COVID-19's pandemic on the economy of Indonesia. BIRCI-J. (2020) 3:1147–56. doi: 10.33258/birci.v3i2.954
32. Russo V, Cassini R, Caso V, Donno C, Laezza A, Naddei M, et al. Nursing teleconsultation for the outpatient management of patients with cardiovascular disease during COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:1–10. doi: 10.3390/ijerph18042087
33. Woodward M. Cardiovascular disease and the female disadvantage. Int J Environ Res Public Health. (2019) 16:1165. doi: 10.3390/ijerph16071165
34. Peters DJ. Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. J Rural Health. (2020) 36:446–56. doi: 10.1111/jrh.12477
35. Choi S, Kim K, Kim SM, Lee G, Jeong SM, Park SY, et al. Association of obesity or weight change with coronary heart disease among young adults in South Korea. JAMA Intern Med. (2018) 178:1060–8. doi: 10.1001/jamainternmed.2018.2310
36. Giannouchos TV, Biskupiak J, Moss MJ, Brixner D, Andreyeva E, Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med. (2021) 40(January):20–6. doi: 10.1016/j.ajem.2020.12.009
37. Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. (2018) 3:280–7. doi: 10.1001/jamacardio.2018.0022
38. Seiffert M, Brunner FJ, Remmel M, Thomalla G, Marschall U, L'Hoest H, et al. Temporal trends in the presentation of cardiovascular and cerebrovascular emergencies during the COVID-19 pandemic in Germany: an analysis of health insurance claims. Clin Res Cardiol. (2020) 109:1540–8. doi: 10.1007/s00392-020-01723-9
39. Bin Y, Andrew S, Li-Jung C, Yi-Huei C, Ching-Heng L, Po-Wen K. Social isolation, loneliness, and all-cause mortality in patients with cardiovascular disease: a 10-year follow-up study. Psychosom Med. (2020) 82:208–14. doi: 10.1097/PSY.0000000000000777
40. Verma AK, Prakash S. Impact of COVID-19 on environment and society. Int J Biol Innov. (2020) 9:7352–63. Available online at: www.mutagens.co.in/jgb/vol.09/05/090506.pdf
41. Uscher-Pines L, Sousa J, Jones M, Whaley C, Perrone C, McCullough C, et al. Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA. (2021) 325:1106–7. doi: 10.1001/jama.2021.0282
42. Yagi N, Suzuki S, Nagai K, Tanaka T, Nagahama T, Arita T, et al. Current status of oral anticoagulant adherence in Japanese patients with atrial fibrillation: A claims database analysis. J Cardiol. (2021) 78:150–6. doi: 10.1016/j.jjcc.2021.02.007
43. The Healthcare Social Security Agency. Pandemic Covid-19 Dorong Inovasi Layanan Digital BPJS Kesehatan. (2021). Available online at: https://bpjs-kesehatan.go.id/bpjs/post/read/2021/2066/Pandemi-Covid-19-Dorong-Inovasi-Layanan-Digital-BPJS-Kesehatan (accessed November 24, 2021).
44. Yoo SM, Chung SH, Jang WM, Kim KC, Lee JY, Kim SM. New obligations of health insurance review and assessment service: Taking full-fledged action against the covid-19 pandemic. J Prev Med Public Health. (2021) 54:17–21. doi: 10.3961/jpmph.20.594
Keywords: COVID-19, cardiovascular disease, financing, National Health Insurance, Indonesia
Citation: Nugraheni WP, Retnaningsih E, Mubasyiroh R and Rachmawati T (2023) Effects of the COVID-19 pandemic on cardiovascular disease financing in Indonesia (JKN claims data analysis 2019–2020). Front. Public Health 11:1148394. doi: 10.3389/fpubh.2023.1148394
Received: 20 January 2023; Accepted: 06 March 2023;
Published: 31 March 2023.
Edited by:
Al Asyary, University of Indonesia, IndonesiaReviewed by:
Meita Veruswati, Universitas Muhammadiyah Prof. Dr. Hamka, IndonesiaFirdaus Hafidz, Gadjah Mada University, Indonesia
Copyright © 2023 Nugraheni, Retnaningsih, Mubasyiroh and Rachmawati. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ekowati Retnaningsih, ZWtvd2F0aS5wZW5lbGl0aUBnbWFpbC5jb20=
 Wahyu Pudji Nugraheni
Wahyu Pudji Nugraheni Ekowati Retnaningsih2*
Ekowati Retnaningsih2* Rofingatul Mubasyiroh
Rofingatul Mubasyiroh Tety Rachmawati
Tety Rachmawati