- 1College of Sports Science, Jishou University, Jishou, Hunan, China
- 2Department of Orthopaedic Surgery, Shanxi Medical University Second Affiliated Hospital, Taiyuan, China
- 3Second Clinical Medical College, Shanxi Medical University, Taiyuan, China
- 4Department of Nursing, Peking University Shenzhen Hospital, Shenzhen, China
- 5School of Nursing, Nanjing University of Chinese Medicine, Nanjing, Jiangsu, China
- 6College of Nursing, Weifang University of Science and Technology, Weifang, Shandong, China
- 7School of Nursing, Nanchang University, Nanchang, Jiangxi, China
- 8Digestive Endoscopy Center, The First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, China
Purpose: Chronic low back pain (CLBP) is an aging and public health issue that is a leading cause of disability worldwide and has a significant economic impact on a global scale. Treatments for CLBP are varied, and there is currently no study with high-quality evidence to show which treatment works best. Exercise therapy has the characteristics of minor harm, low cost, and convenient implementation. It has become a mainstream treatment method in clinics for chronic low back pain. However, there is insufficient evidence on which specific exercise regimen is more effective for chronic non-specific low back pain. This network meta-analysis aimed to evaluate the effects of different exercise therapies on chronic low back pain and provide a reference for exercise regimens in CLBP patients.
Methods: We searched PubMed, EMBASE, Cochrane Library, and Web of Science from inception to 10 May 2022. Inclusion and exclusion criteria were used for selection. We collected information from studies to compare the effects of 20 exercise interventions on patients with chronic low back pain.
Results: This study included 75 randomized controlled trials (RCTs) with 5,254 participants. Network meta-analysis results showed that tai chi [standardized mean difference (SMD), −2.11; 95% CI, −3.62 to −0.61], yoga (SMD, −1.76; 95% CI −2.72 to −0.81), Pilates exercise (SMD, −1.52; 95% CI, −2.68, to −0.36), and sling exercise (SMD, −1.19; 95% CI, −2.07 to −0.30) showed a better pain improvement than conventional rehabilitation. Tai chi (SMD, −2.42; 95% CI, −3.81 to −1.03) and yoga (SMD, −2.07; 95% CI, −2.80 to −1.34) showed a better pain improvement than no intervention provided. Yoga (SMD, −1.72; 95% CI, −2.91 to −0.53) and core or stabilization exercises (SMD, −1.04; 95% CI, −1.80 to −0.28) showed a better physical function improvement than conventional rehabilitation. Yoga (SMD, −1.81; 95% CI, −2.78 to −0.83) and core or stabilization exercises (SMD, −1.13; 95% CI, −1.66 to −0.59) showed a better physical function improvement than no intervention provided.
Conclusion: Compared with conventional rehabilitation and no intervention provided, tai chi, toga, Pilates exercise, sling exercise, motor control exercise, and core or stabilization exercises significantly improved CLBP in patients. Compared with conventional rehabilitation and no intervention provided, yoga and core or stabilization exercises were statistically significant in improving physical function in patients with CLBP. Due to the limitations of the quality and quantity of the included studies, it is difficult to make a definitive recommendation before more large-scale and high-quality RCTs are conducted.
Introduction
Low back pain is a more severe low back pain syndrome that can be classified by duration as acute (pain lasting for less than 6 weeks), subchronic (6–12 weeks), or chronic (more than 12 weeks) (1, 2). Only 39–76% of patients fully recover after an acute pain episode, suggesting that a significant proportion suffer from chronic low back pain (CLBP) (3). CLBP is a common and effective public health problem worldwide and is the second most common reason for medical visits in people aged 65 years or older (4, 5). Studies have found that the incidence and prevalence of CLBP increase with age (6–8). CLBP imposes an enormous economic and social burden, which will become even more onerous in the coming decades as the number of patients with CLBP is expected to increase significantly (9). In addition, a study of nearly 200,000 people in 43 countries found that those with CLBP were twice as likely to suffer from depression, anxiety, psychosis, or sleep deprivation (10, 11).
CLBP can lead to disability, high treatment costs, absenteeism, and sick leave (10). Exercise therapy is based on kinematics, biomechanics, physiology, and pathology to improve body function, regulate physiological state, improve mental quality, and eliminate mental disorders. Exercise therapy is characterized by low harm, low cost, and easy implementation and has become the first choice in the clinical treatment of CLBP (12). There are many kinds of exercise therapy (12), and it is unclear which exercise therapy is the best. Direct comparative evidence of exercise therapy suggests that core stability training is more effective than aerobic and stretching exercises in treating CLBP (13).
A review by Hayden reported that exercise therapy might be more effective than education and non-exercise physiotherapy alone in improving pain and function (14). However, Pilates remains controversial for CLBP pain, as reported in paired meta-analyses (15). In a previous net meta-analysis, studies found that exercise and heat were the best modalities for relieving CLBP pain (16). However, we found that the current study needs a detailed breakdown of exercise modalities (16) as it does not describe the effects of all current exercise modalities, such as tai chi and water sports, on the effects of CLBP (17, 18). We wanted to better explore the effects of other exercises on CLBP patients. We performed a complex variety of exercise therapies, included more exercise modalities in our network meta-analysis, and analyzed RCTs on the effects of different exercise therapies on patients with CLBP to evaluate their therapeutic effects comprehensively and suggest the best exercise therapy for selecting exercise programs.
Materials and methods
This network meta-analysis was designed according to the guidelines for Preferred Reporting Items of Systems Review and Network Meta-Analysis (PRISMA-NMA) (19), registered in the PROSPERO database (CRD42023388526).
Search strategy
PubMed, Web of Science, Embase, and Cochrane Library were searched to identify studies published as of 10 May 2022 associated with RCT of exercise therapy for CLBP. The search takes a combination of subject words and free words. The search strategy is shown in Supplementary Appendix 1.
Study selection
Two independent reviewers (Chengkun Yan and Xian Huang Li) screened the titles and abstracts of publications retrieved by the search strategy to identify those eligible for inclusion. The full text of potentially eligible studies was evaluated according to the inclusion and exclusion criteria. The disagreements between reviewers were resolved through discussion. The NoteExpress software is used to manage this phase.
Inclusion criteria
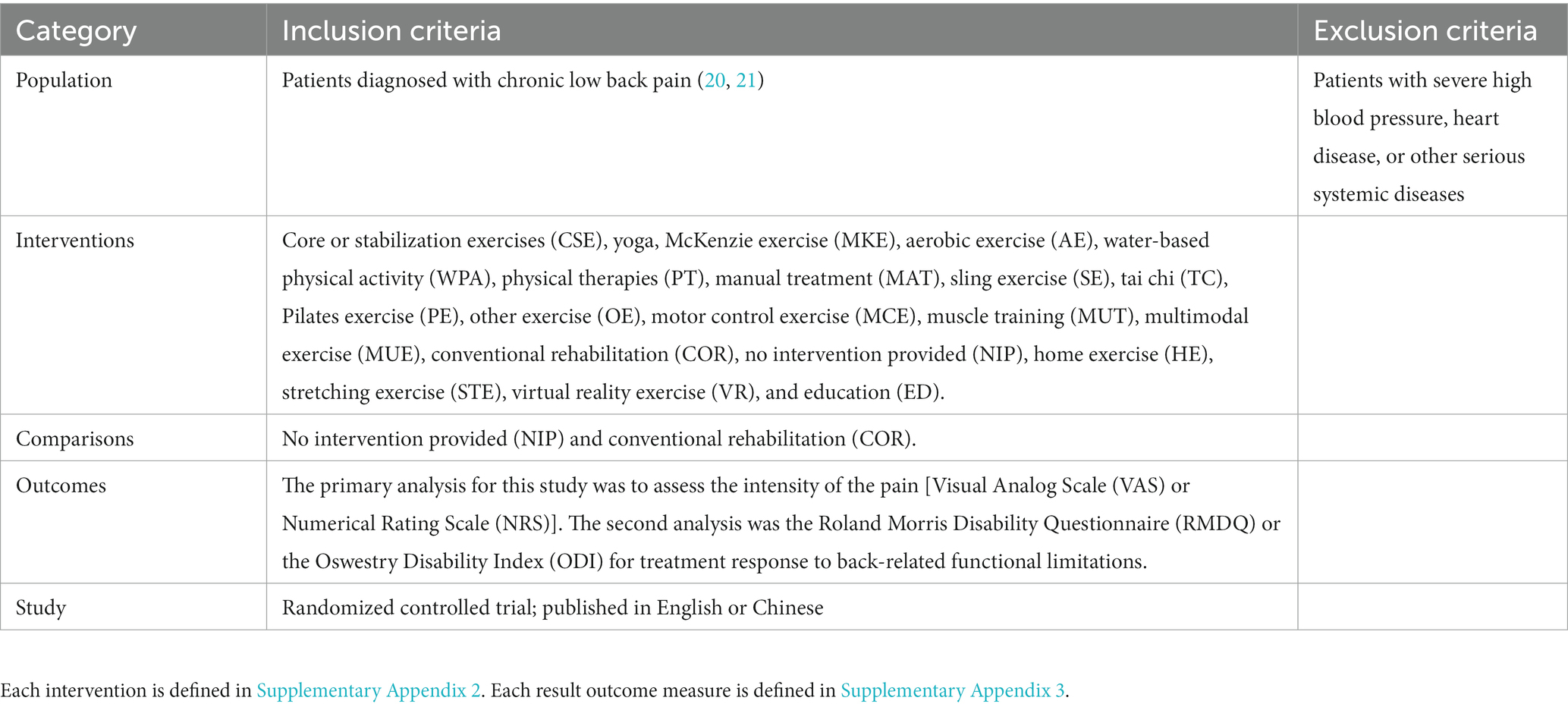
Inclusion and exclusion criteria are based on PICOS standards, see Table 1 for specific inclusion and exclusion criteria.
Data extraction
Data extraction pairs of reviewers independently extracted the following data: first author, year of publication, country, sample size, CLBP time, age, weight, height, intervention, and intervention time. Data were expressed as mean ± standard deviation (SD). If outcome measures report multiple time points, we extract the data for the latest time point.
Risk of bias assessment
The risk of bias was assessed independently by two reviewers and adjudicated by a third reviewer using the Cochrane Collaboration’s tools (22), which include sequence generation, assignment hiding, blinding, incomplete results data, non-selective results reporting, and other sources of bias. Each criterion was judged to have a low, unclear, or high risk of bias.
Data analysis
We used the “netmeta” package of R-4.2.1 software to conduct a network meta-analysis. The STATA 15.1 “networkplot” function is used to draw and generate network diagrams to describe and present different forms of exercise. We used nodes to represent various interventions and edges to represent head-to-head comparisons between interventions. The node split method was used to assess inconsistency between direct and indirect comparisons (23). The pooled estimates and 95% confidence intervals (95% CI) were calculated using random effects network element analysis. When we are interested in outcomes that use the same unit of measurement in the study, consider mean difference (MD) as a therapeutic effect to analyze the results or evaluate standardized mean difference (SMD). A pairwise random-effects meta-analysis was performed to compare various exercise treatments. Heterogeneity was assessed for all pairwise comparisons using the I2 statistic and publication bias using the value of p of Egger’s test. Funnel plots were conducted to determine publication bias and minor study effects measured by results reported in more than 10 studies.
Results
Literature selection
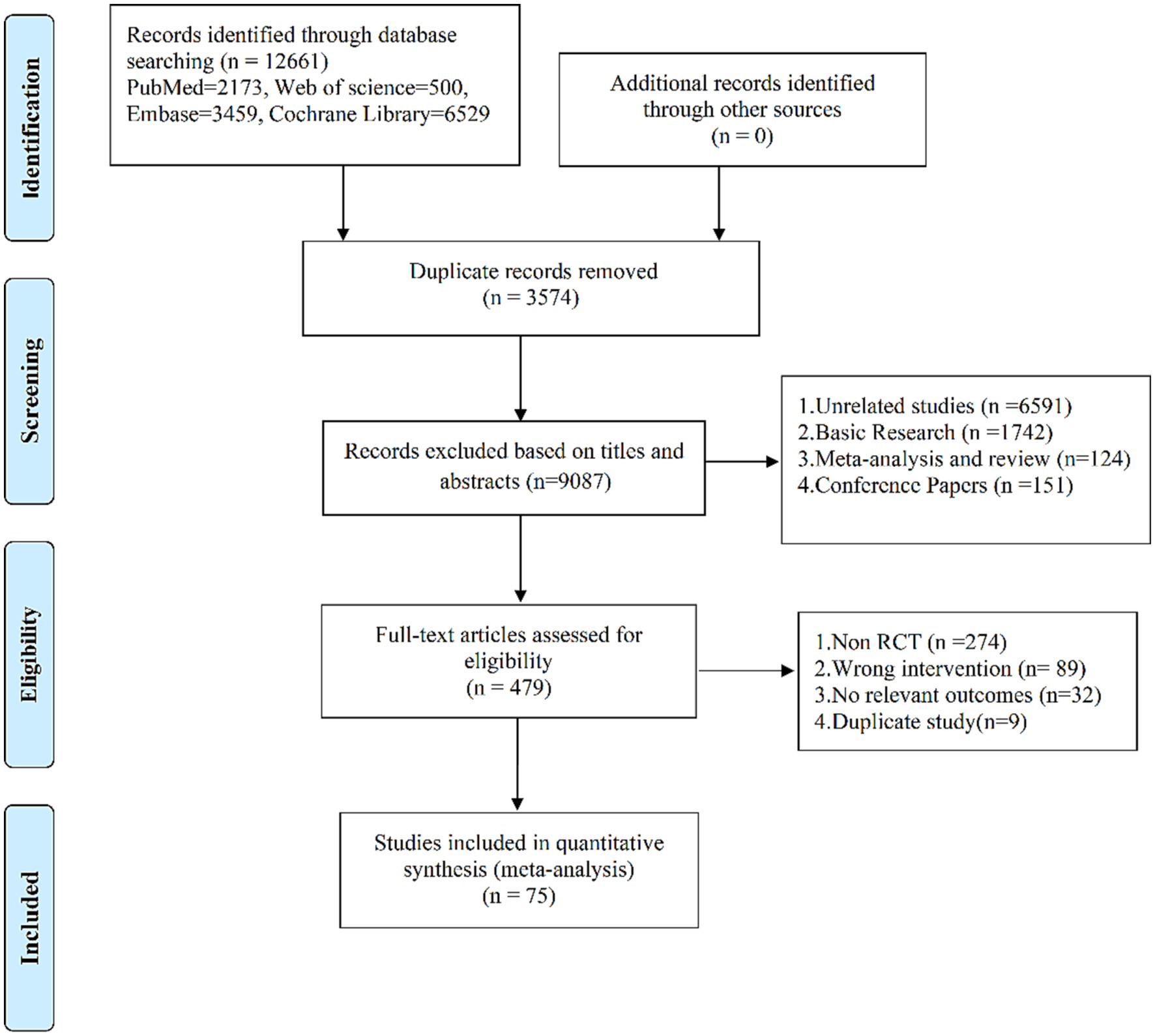
After deleting duplicates, 9,087 records were retrieved, and 8,608 studies were discarded. The full text of the remaining 479 records was examined, and 404 records did not meet the inclusion criteria: 274 were non-RCTs, 89 were wrong interventions, 32 were no relevant outcomes, and 9 were duplicate studies. In the end, 75 studies (24–98) were included. The research flow chart is shown in Figure 1.
Study and participant characteristics
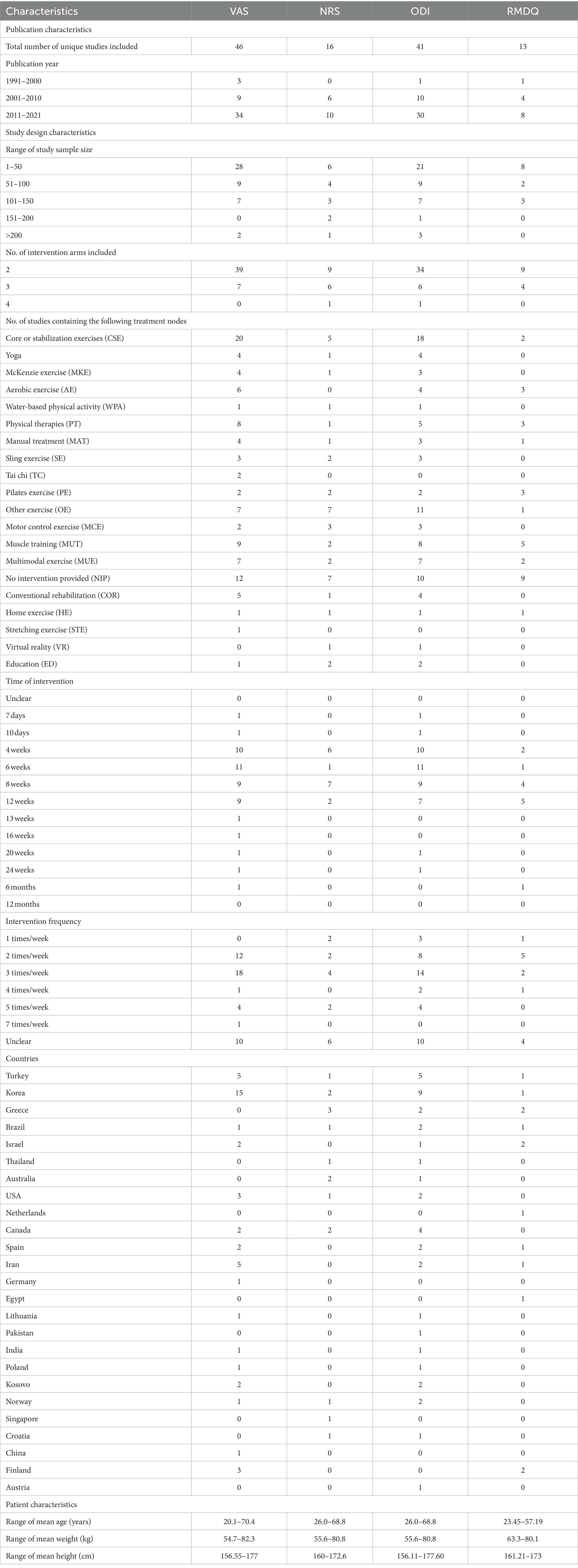
The included studies, published between 1998 and 2021, compared the effects of 20 different therapies on CLBP. The intervention lasted from 7 days to 24 weeks. A total of 5,254 patients were reported in the included studies. Of all the included studies, 46 reported VAS, 16 reported NRS, 41 reported ODI, and 13 reported RMDQ. The average age ranged from 20.1 ± 0.7 to 70.4 ± 3.2 years, the average weight ranged from 54.7 ± 7.6 kg to 81 ± 18.6 kg, and the average height ranged from 156.11 ± 9.44 cm to 177.60 ± 9.98 cm. The characteristics of the studies and the participants are shown in Table 2 and Supplementary Appendix 4. The risk of bias assessment for each individual study is presented in Supplementary Appendix 5 and summary data in Figure 2. In addition, we conducted regression analyses of age and gender, as shown in Supplementary Appendix 9.
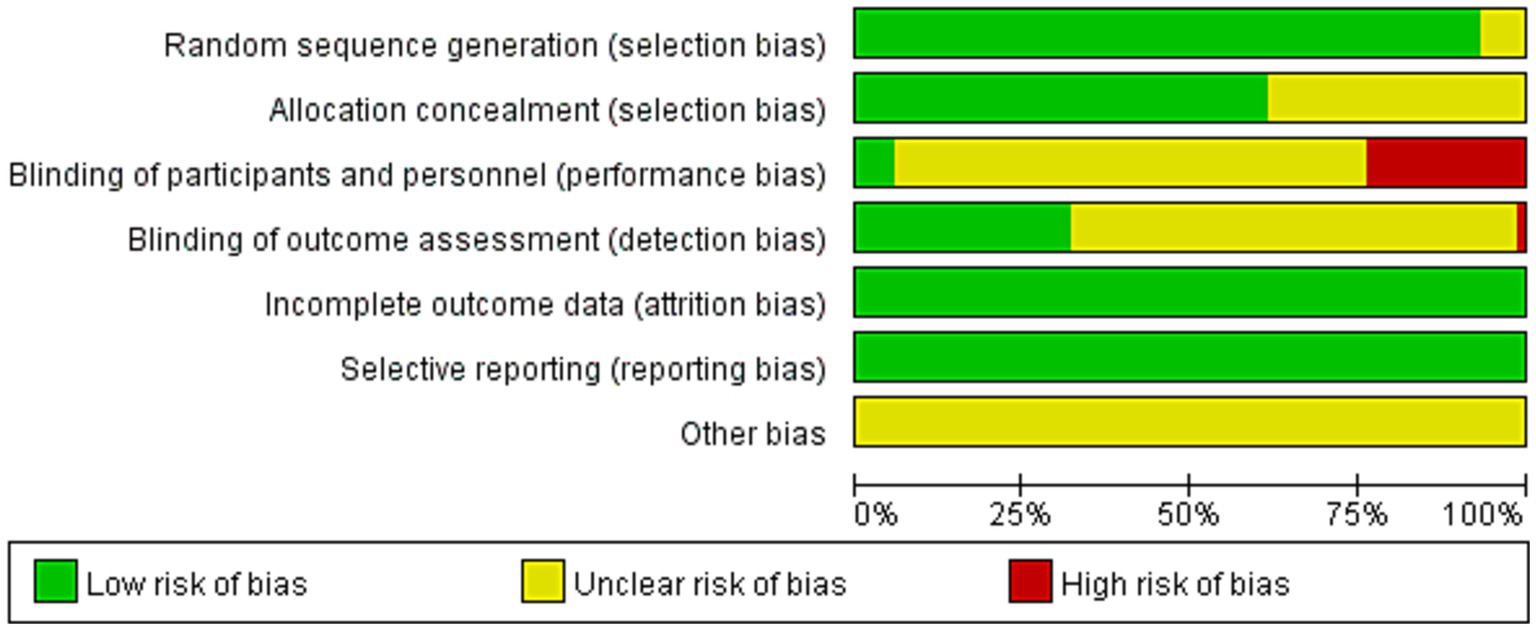
Figure 2. Percentage of studies examining the efficacy of exercise training in patients with non-specific chronic low back pain with low, unclear, and high risk of bias for each feature of the Cochrane Risk of Bias Tool.
Outcomes
Pain
In total, 62 studies (24–30, 33, 35–50, 52–56, 58, 60, 61, 63–65, 67–71, 73–79, 82–84, 86–92, 94–98) assessed pain, involving a total of 3,123 participants. We included the following 20 interventions in our network meta-analysis (Figure 2): TC, yoga, PE, SE, MCE, WPA, CSE, MUE, MKE, HE, MAT, MUT, STE, ED, OE, AE, PT, VR, COR, and NIP. TC (SMD, −2.11; 95% CI, −3.62 to −0.61), yoga (SMD, −1.76; 95% CI, −2.72 to −0.81), PE (SMD, −1.52; 95% CI, −2.68, to −0.36), SE (SMD, −1.19; 95% CI, −2.07 to −0.30), MCE (SMD, −1.02; 95% CI, −1.86 to −0.18), CSE (SMD, −0.95; 95% CI, −1.56 to −0.33), MUE (SMD, −0.94; 95% CI, −1.71 to −0.18), and MKE (SMD, −0.91; 95% CI, −1.81 to −0.01) showed a better pain improvement than COR. TC (SMD, −2.42; 95% CI, −3.81 to −1.03), yoga (SMD, −2.07; 95% CI, −2.80 to −1.34), PE (SMD, −1.83; 95% CI, −2.72 to −0.93), SE (SMD, −1.49; 95% CI, −2.20 to −0.79), MCE (SMD, −1.33; 95% CI, −2.12 to −0.54), WPA (SMD, −1.36; 95% CI, −2.59 to −0.14), CSE (SMD, −1.25; 95% CI, −1.71 to −0.79), MUE (SMD, −1.25; 95% CI, −1.84 to −0.65), MKE (SMD, −1.22; 95% CI, −1.98 to −0.45), HE (SMD, −1.20; 95% CI, −2.19 to −0.22), MAT (SMD, −1.16; 95% CI, −1.89 to −0.42), MUT (SMD, −1.08; 95% CI, −1.67 to −0.49), STE (SMD, −1.02; 95% CI, −3.07 to −1.03), ED (SMD, −0.93; 95% CI, −1.84 to −0.01), OE (SMD, −0.97; 95% CI, −1.52 to −0.43), and AE (SMD, −0.82; 95% CI, −1.54 to −0.10) showed a better pain improvement than NIP (Figure 3A). The comparison adjusted funnel plot did not provide evidence for apparent publication bias and Egger’s test (p = 0.601) (Supplementary Appendix 6.1). Heterogeneity, intransitivity, and inconsistency of the network meta-analysis were also evaluated (Supplementary Appendix 7). Direct pain was also evaluated (Supplementary Appendix 8.1).
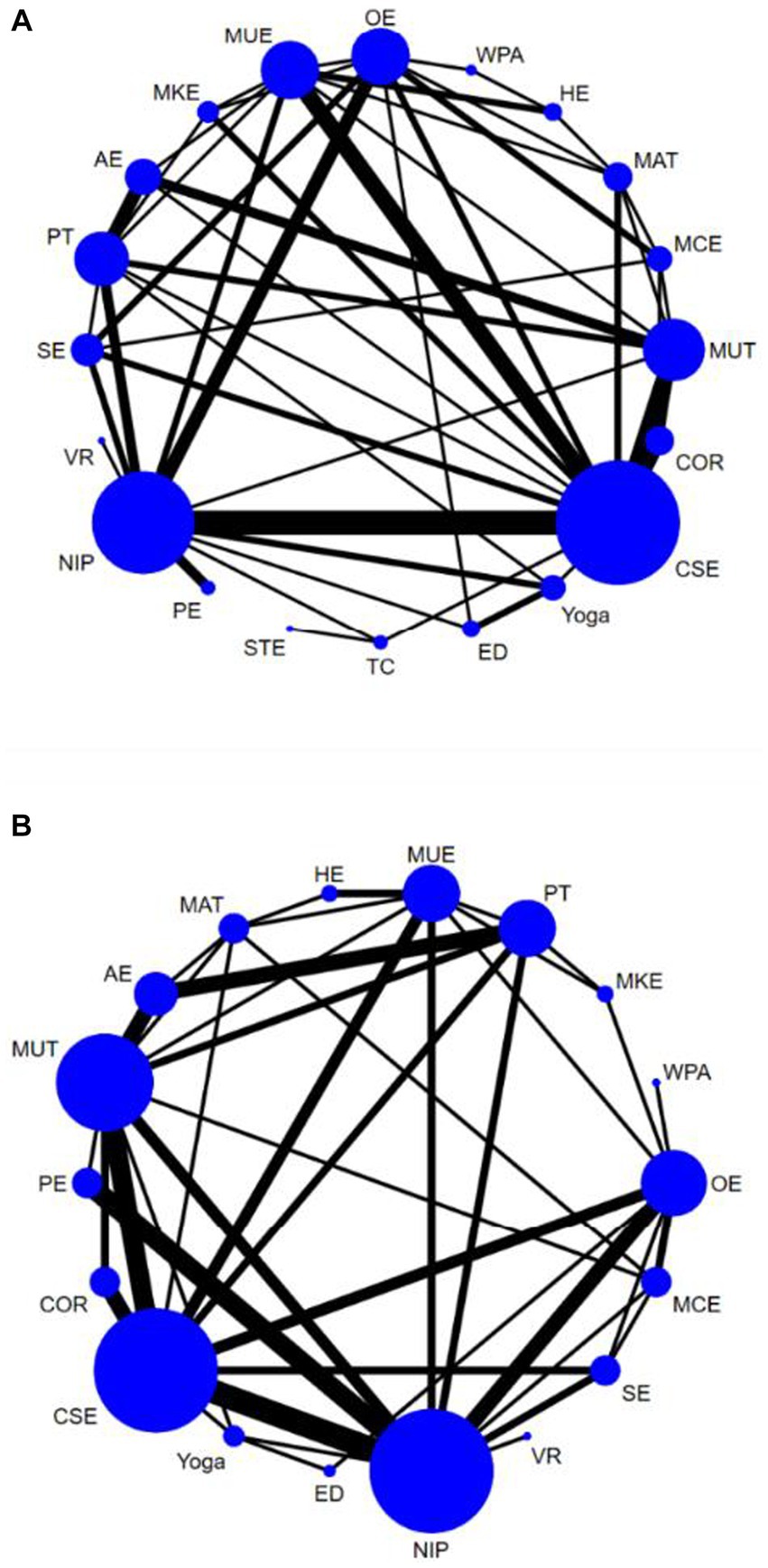
Figure 3. Network plots of pain and Physical function. The size of the nodes represents how many times the exercise appears in any comparison aboutthat treatment and the width of the edges represents the total sample size in the comparisons it connects. Core or stabilization exercises (CSE), Yoga, McKenzie exercise (MKE), Aerobic exercise (AE), Water-based physical activity (WPA), Physical therapies (PT), Manual treatment (MAT), Sling exercise (SE), Tai chi (TC), Pilates exercise (PE), Other exercise (OE), Motor control exercise (MCE), Muscle training (MUT), Multimodal exercise (MUE), Conventional rehabilitation (COR), No intervention provided (NIP), Home exercise (HE), Stretching exercise (STE).Virtual Reality exercise (VR), Education (ED).
Physical function
In total, 54 studies (28, 30–35, 38, 39, 41, 44–55, 57–64, 66, 67, 72, 74, 76–82, 85–88, 90–98) assessed physical function, involving a total of 4,355 participants. We included the following 18 interventions in our network meta-analysis (Figure 2), including the NIP, VR, SE, MCE, OE, WAP, MKE, PT, MUE, HE, MAT, AE, MUT, PE, COR, CSE, yoga, and ED. Yoga (SMD, −1.72; 95% CI, −2.91 to −0.53), CSE (SMD, −1.04; 95% CI, −1.80 to −0.28) showed a better physical function improvement than COR. Yoga (SMD, −1.81; 95% CI, −2.78 to −0.83), CSE (SMD, −1.13; 95% CI, −1.66 to −0.59), SE (SMD, −1.10; 95% CI, −2.06 to −0.15), OE (SMD, −1.05; 95% CI, −1.66 to −0.43), PE (SMD; −1.08, 95% CI, −1.85 to −0.31), and MCE (SMD, −0.90; 95% CI, −1.76 to −0.04) showed a better physical function improvement than NIP (Figure 3B). The comparison-adjusted funnel plot did not provide evidence for apparent publication bias and Egger’s test (p = 0.616) (Supplementary Appendix 6.2). Heterogeneity, intransitivity, and inconsistency of the network meta-analysis (NMA) were evaluated (Supplementary Appendix 7). Direct comparisons of physical function were also evaluated (Supplementary Appendix 8.2 and Figure 4).
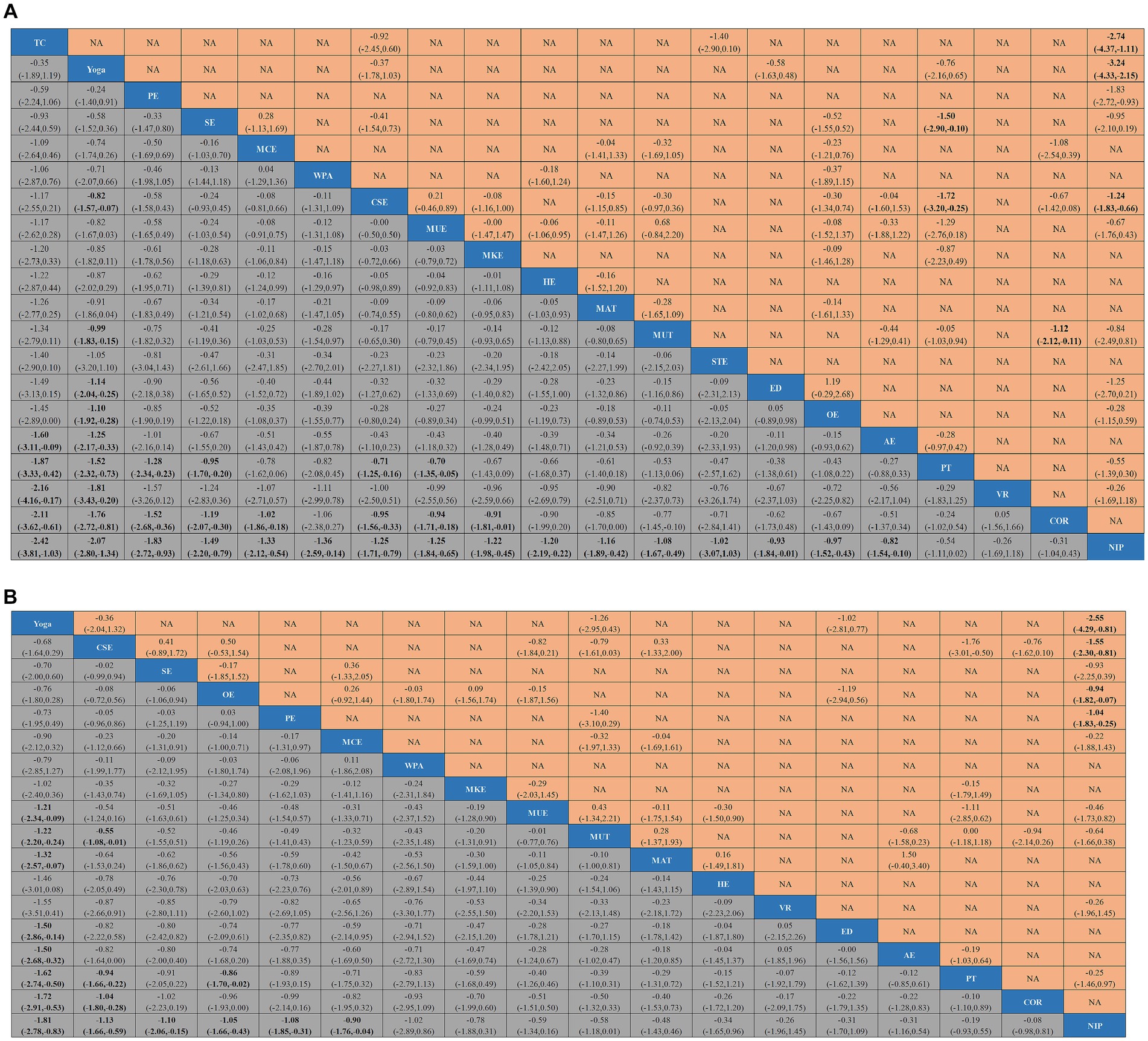
Figure 4. League tables of outcome analyses. Data are mean differences and 95% credibility intervals for continuous data. Core or stabilization exercises (CSE), Yoga, McKenzie exercise (MKE), Aerobic exercise (AE), Water-based physical activity (WPA), Physical therapies (PT), Manual treatment (MAT), Sling exercise (SE), Tai chi (TC), Pilates exercise (PE), Other exercise (OE), Motor control exercise (MCE), Muscle training (MUT), Multimodal exercise (MUE), Conventional rehabilitation (COR), No intervention provided (NIP), Home exercise (HE), Stretching exercise (STE).Virtual Reality exercise (VR), Education (ED).
Discussion
CLBP is a global aging and public health problem. The global 1-year prevalence of CLBP in older adults is 13–50% (99, 100). The medical burden associated with CLBP is high, not only due to direct costs (medical appointments, tests, medications, and hospitalizations) but also due to loss of work productivity (101, 102). Exercise therapy can relieve pain and improve dysfunction in CLBP. Nevertheless, there are many types of exercise therapy, and it needs to be clarified which exercise is the best training method. In this study, we assessed the relative effects of 20 different interventions on pain and physical function in patients with CLBP. Regression analyses showed no correlation between patient age and patients’ pain scores and physical functioning scores. In addition, regression analyses also showed no correlation between patients’ gender and patients’ pain scores and physical function scores. Tai chi, yoga, Pilates exercise, sling exercise, motor control exercise, core or stabilization exercises, multimodal exercise, and McKenzie exercise are more beneficial for pain relief than conventional rehabilitation, and no intervention is provided. Water-based physical activity, home exercise, manual treatment, muscle training, stretching exercise, education, other exercise, and aerobic exercise are more useful for pain relief than no intervention provided. Yoga and core or stabilization exercises showed better physical function improvement than conventional rehabilitation, and no intervention was provided. Sling exercise, Pilates exercise, and motor control exercise, other exercises, showed better physical function improvement than no intervention provided.
In our study, we found that tai chi can reduce pain in patients with chronic low back pain. The results of this study are the same as those of Lauche et al. (103). Compared with other forms of exercise, tai chi can increase structural flexibility and mobility, improve muscle strength and endurance, increase the tensile strength of ligaments and bursae, enhance cardiopulmonary function, and reduce stress, anxiety, and depression (104). Tai chi can significantly increase bone density value, improve limb motor and balance function, and effectively improve the symptoms of low back pain (103, 105). In addition, CLBP trunk proprioception is diminished, resulting in deficits in the control of ankle and hip strategies during balance control, a phenomenon that exacerbates the decreased trunk proprioception in CLBP (106). Tai chi can alter brain waves in the brain’s perception of pain areas (parietal and prefrontal lobes), and the brain processes relevant information more efficiently, improving proprioception in the brain centers (107). Some studies have reported that tai chi can reduce serum B-type linalool peptide levels, increase per-pulse output, improve blood circulation throughout the body, and improved blood circulation can transport blood calcium and other nutrients to the lumbar region, increase the metabolism of the lumbar bones, improve the absorption of calcium and other minerals by bone cells, and improve bone density in the lumbar region (108). The 2017 American Medical Association’s Authoritative Guidelines for the treatment of low back pain recommend tai chi for the treatment of chronic low back pain (109). Our study further supports this result.
Physical therapies involve whole-body movement that emphasizes the body posture of the human body standing and enhances the body control and balance ability through the brain consciousness to control smooth body movements and correct breathing (110, 111). In addition to core strengthening, physical therapies emphasize the coordination of breathing and movement posture, which can reduce joint contraction and fatigue of trunk muscles, effectively reduce pain, and improve body function, and are widely used in treating CLBP.
One study reported that in patients with low back pain, the height of the intervertebral disc and the length and load of the paravertebral ligament changed, and the adaptability of the proprioceptive receptor decreased, thus reducing the proprioceptive input and weakening the neuromuscular reflex of the paravertebral muscle, resulting in lumbar instability and decreased postural control (112). Sling exercise activates the core muscle group by suspending part of the body and placing the body in an unstable state, improving muscle imbalance, improving the control ability of the neuromuscular system, enhancing the stability of the lumbar spine, and improving physical function. In our study, core stabilization training was found to be effective in reducing pain. Changes in plasma β-endorphin levels can indicate efficacy response in chronic lower back pain (113). Cortisol is a type of glucocorticoid produced by the hypothalamic–pituitary–adrenal axis activity. Uncomfortable physical pain in CLBP can trigger anxiety in patients. Pain and anxiety lead to increased hypothalamic-pituitary-adrenal axis activation, leading to elevated cortisol levels in patients (114). In addition, pain neuronal excitability releases transmitters (115). In addition, interleukin 4 (IL-4), an anti-inflammatory cytokine produced by macrophages and monocytes, inhibits the synthesis of pro-inflammatory cytokines. It has been found (114, 116–118) that the mechanism of action of core stabilization training for CLBP is mainly through altering the neurotransmitters β-endorphin, cortisol, and IL-4 levels. Ko et al. (74) proved that both suspension and stability training could effectively relieve pain and enhance lumbar muscle strength and flexibility in CLBP patients.
In our study, we found that Yoga can reduce pain in patients with chronic low back pain. The results of this study are the same as those of Zhu et al. (119). Yoga originated in India and has a history of more than 4,000 years. While promoting spinal tissue stretching, flexibility, and balance training, yoga can also strengthen back muscles, relieve pain, and improve patients with functional impairment (56). In addition, yoga can effectively improve the lumbar pain and spinal flexibility of CLBP patients by stretching the spine vertebra and making the lumbar spine get strength training. More than half of CLBP patients in the United States choose yoga as an adjunct therapy (120). Guidelines developed by the American Pain Society suggest that for CLBP not alleviated by medication and self-management, consider recommending yoga as adjunctive therapy to help patients relieve pain (121).
Fernández-Rodríguez et al. conducted a network meta-analysis of nine exercises. They found that Pilates was the most effective intervention for reducing pain (114). Unlike our study, tai chi and yoga were more effective than Pilates exercises in reducing pain. In Gianola et al. (16) and Owen et al. (18) network meta-analysis, Tai chi was not treated as a separate intervention, and conventional rehabilitation and no intervention provided were not treated as control groups. However, we have classified, in detail, the different exercises into 20 other activities, including tai chi, virtual reality exercises, and conventional rehabilitation, for a more comprehensive NMA. Our study provides evidence that “active therapies” such as tai chi, yoga, sling exercise, and core or stabilization exercises, in which patients are guided and actively encouraged to move and exercise in a gradual manner, are most effective. In our study, we did not recommend virtual reality exercise, conventional rehabilitation, and no intervention provided for CLBP patients. They are less effective in pain in patients with CLBP.
Strengths and limitations
Our review has several strengths. First, we used the network meta-analysis design to synthesize direct and indirect evidence from various exercise interventions that can be used to treat CLBP. Importantly, we used a nuanced approach to categorize exercise interventions. Previous reviews have often grouped different exercise interventions, potentially leading to heterogeneous comparisons and inaccurate estimates of therapeutic effectiveness in a single comparison. Interventions were divided into 20 types, and various interventions were defined. However, we also have certain limitations. First, we did not take the intervention period, intensity, and frequency into consideration. Second, the implementation quality of the blind method included in the literature is not high, and pain and functional improvement are subjective indicators, which may lead to the bias of the results due to the different focus of researchers. Third, we only included English literature, which may lead to heterogeneity. Fourth, the study did not analyze differences by initial categories that are important for both VAS and physical function. Fifth, CLBP was not considered in terms of the presence of a neuropathic or nocioplastic component. Sixth, biomarkers showing the effects of different exercise interventions were unavailable in the study. Finally, gender considerations were missing from the study reports. There are some gender differences in abdominal and lumbar muscle characteristics between female and male subjects (122), which can lead to differences in response to post-exercise emerging in gender-specific CLBP patients.
Conclusion
This systematic review examined pain reduction and physical function improvement in patients with CLBP treated with exercise. Compared to COR and NIP, exercise is effective in relieving pain and improving physical function. In conclusion, understanding the benefits of exercise versus non-exercise therapy is essential to better serve patients with CLBP.
Author contributions
YuL and LH designed the study. CY and XL acquired, analyzed, and interpreted the data. XD, YiL, YH, and YuL revised the manuscript. XZ and XC contributed to the revision of the article. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Sanming Project of Medicine in Shenzhen (no. SZSM202111013).
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1155225/full#supplementary-material
References
1. Indahl, A. Low back pain: diagnosis, treatment, and prognosis. Scand J Rheumatol. (2004) 33:199–209. doi: 10.1080/03009740410006916
2. Van Zundert, J, Van Boxem, K, Vanelderen, P, Puylaert, M, De Vooght, P, Mestrum, R, et al. Establishing the diagnosis of low back pain: patient selection for interventional pain medicine. Pain Manag. (2013) 3:129–36. doi: 10.2217/pmt.13.3
3. Menezes Costa, L d C, Maher, CG, Hancock, MJ, McAuley, JH, Herbert, RD, and Costa, LOP. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. (2012) 184:E613–24. doi: 10.1503/cmaj.111271
4. Cypress, BK. Characteristics of physician visits for back symptoms: a national perspective. Am J Public Health. (1983) 73:389–95. doi: 10.2105/AJPH.73.4.389
5. Deyo, RA, and Weinstein, JN. Low back pain. N Engl J Med. (2001) 344:363–70. doi: 10.1056/NEJM200102013440508
6. Thomas, E, Peat, G, Harris, L, Wilkie, R, and Croft, PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the north Staffordshire osteoarthritis project (NorStOP). Pain. (2004) 110:361–8. doi: 10.1016/j.pain.2004.04.017
7. Cassidy, JD, Carroll, LJ, and Côté, P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). (1998) 23:1860–6; discussion 1867. doi: 10.1097/00007632-199809010-00012
8. Dionne, CE, Dunn, KM, and Croft, PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing. (2006) 35:229–34. doi: 10.1093/ageing/afj055
9. Wewege, MA, Booth, J, and Parmenter, BJ. Aerobic vs. resistance exercise for chronic non-specific low back pain: a systematic review and meta-analysis. J Back Musculoskelet Rehabil. (2018) 31:889–99. doi: 10.3233/BMR-170920
10. Melloh, M, Röder, C, Elfering, A, Theis, JC, Müller, U, Staub, LP, et al. Differences across health care systems in outcome and cost-utility of surgical and conservative treatment of chronic low back pain: a study protocol. BMC Musculoskelet Disord. (2008) 9:81. doi: 10.1186/1471-2474-9-81
11. Stubbs, B, Koyanagi, A, Thompson, T, Veronese, N, Carvalho, AF, Solomi, M, et al. The epidemiology of back pain and its relationship with depression, psychosis, anxiety, sleep disturbances, and stress sensitivity: data from 43 low- and middle-income countries. Gen Hosp Psychiatry. (2016) 43:63–70. doi: 10.1016/j.genhosppsych.2016.09.008
12. O'Connell, NE, Cook, CE, Wand, BM, and Ward, SP. Clinical guidelines for low back pain: a critical review of consensus and inconsistencies across three major guidelines. Best Pract Res Clin Rheumatol. (2016) 30:968–80. doi: 10.1016/j.berh.2017.05.001
13. Wang, XQ, Zheng, JJ, Yu, ZW, Bi, X, Lou, SJ, Liu, J, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS One. (2012) 7:e52082. doi: 10.1371/journal.pone.0052082
14. Hayden, JA, Ellis, J, Ogilvie, R, Malmivaara, A, and van Tulder, MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. (2021) 2021:CD009790. doi: 10.1002/14651858.CD009790.pub2
15. Miyamoto, GC, Costa, LO, and Cabral, CM. Efficacy of the Pilates method for pain and disability in patients with chronic nonspecific low back pain: a systematic review with meta-analysis. Braz J Phys Ther. (2013) 17:517–32. doi: 10.1590/S1413-35552012005000127
16. Gianola, S, Bargeri, S, Del Castillo, G, Corbetta, D, Turolla, A, Andreano, A, et al. Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: a systematic review with network meta-analysis. Br J Sports Med. (2022) 56:41–50. doi: 10.1136/bjsports-2020-103596
17. Hayden, JA, Ellis, J, Ogilvie, R, Stewart, SA, Bagg, MK, Stanojevic, S, et al. Some types of exercise are more effective than others in people with chronic low back pain: a network meta-analysis. J Physiother. (2021) 67:252–62. doi: 10.1016/j.jphys.2021.09.004
18. Owen, PJ, Miller, CT, Mundell, NL, Verswijveren, SJJM, Tagliaferri, SD, Brisby, H, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. (2020) 54:1279–87. doi: 10.1136/bjsports-2019-100886
19. Hutton, B, Salanti, G, Caldwell, DM, Chaimani, A, Schmid, CH, Cameron, C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
20. Koes, BW, van Tulder, M, Lin, CW, Macedo, LG, McAuley, J, and Maher, C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. (2010) 19:2075–94. doi: 10.1007/s00586-010-1502-y
21. van Tulder, M, Becker, A, Bekkering, T, Breen, A, del Real, MT, Hutchinson, A, et al. COST B13 working group on guidelines for the management of acute low back pain in primary care. Eur Spine J. (2006). Suppl 2:S169–91. doi: 10.1007/s00586-006-1071-2.
22. Higgins, JP, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
23. Rücker, G, and Schwarzer, G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. (2015) 15:58. doi: 10.1186/s12874-015-0060-8
24. Hosseinifar, M, Akbari, M, Behtash, H, Amiri, M, and Sarrafzadeh, J. The effects of stabilization and Mckenzie exercises on transverse abdominis and multifidus muscle thickness, pain, and disability: a randomized controlled trial in NonSpecific chronic low Back pain. J Phys Ther Sci. (2013) 25:1541–5. doi: 10.1589/jpts.25.1541
25. Liu, J, Yeung, A, Xiao, T, Tian, X, Kong, Z, Zou, L, et al. Chen-style tai chi for individuals (aged 50 years old or above) with chronic non-specific low Back pain: a randomized controlled trial. Int J Environ Res Public Health. (2019) 16:517. doi: 10.3390/ijerph16030517
26. Suh, JH, Kim, H, Jung, GP, Ko, JY, and Ryu, JS. The effect of lumbar stabilization and walking exercises on chronic low back pain: a randomized controlled trial. Medicine. (2019) 98:e16173. doi: 10.1097/MD.0000000000016173
27. Cho, HY, Kim, EH, and Kim, J. Effects of the CORE exercise program on pain and active range of motion in patients with chronic low Back pain. J Phys Ther Sci. (2014) 26:1237–40. doi: 10.1589/jpts.26.1237
28. Kim, SS, Min, WK, Kim, JH, and Lee, BH. The effects of VR-based Wii fit yoga on physical function in middle-aged female LBP patients. J Phys Ther Sci. (2014) 26:549–52. doi: 10.1589/jpts.26.549
29. Kankaanpää, M, Taimela, S, Airaksinen, O, and Hänninen, O. The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self-experienced disability, and lumbar fatigability. Spine. (1999) 24:1034–42. doi: 10.1097/00007632-199905150-00019
30. Kuvačić, G, Fratini, P, Padulo, J, Antonio, DI, and De Giorgio, A. Effectiveness of yoga and educational intervention on disability, anxiety, depression, and pain in people with CLBP: a randomized controlled trial. Complement Ther Clin Pract. (2018) 31:262–7. doi: 10.1016/j.ctcp.2018.03.008
31. Koldaş Doğan, S, Sonel Tur, B, Kurtaiş, Y, and Atay, MB. Comparison of three different approaches in the treatment of chronic low back pain. Clin Rheumatol. (2008) 27:873–81. doi: 10.1007/s10067-007-0815-7
32. Cho, I, Jeon, C, Lee, S, Lee, D, and Hwangbo, G. Effects of lumbar stabilization exercise on functional disability and lumbar lordosis angle in patients with chronic low back pain. J Phys Ther Sci. (2015) 27:1983–5. doi: 10.1589/jpts.27.1983
33. Oh, BH, Kim, HH, Kim, CY, and Nam, CW. Comparison of physical function according to the lumbar movement method of stabilizing a patient with chronic low back pain. J Phys Ther Sci. (2015) 27:3655–8. doi: 10.1589/jpts.27.3655
34. Kang, JI, Jeong, DK, and Choi, H. Effect of exhalation exercise on trunk muscle activity and oswestry disability index of patients with chronic low back pain. J Phys Ther Sci. (2016) 28:1738–42. doi: 10.1589/jpts.28.1738
35. Mannion, AF, Müntener, M, Taimela, S, and Dvorak, J. Comparison of three active therapies for chronic low back pain: results of a randomized clinical trial with one-year follow-up. Rheumatology. (2001) 40:772–8. doi: 10.1093/rheumatology/40.7.772
36. Miller, ER, Schenk, RJ, Karnes, JL, and Rousselle, JG. A comparison of the McKenzie approach to a specific spine stabilization program for chronic low back pain. J Man Manip Ther. (2005) 13:103–12. doi: 10.1179/106698105790824996
37. Akbari, A, Khorashadizadeh, S, and Abdi, G. The effect of motor control exercise versus general exercise on lumbar local stabilizing muscles thickness: randomized controlled trial of patients with chronic low back pain. J Back Musculoskelet Rehabil. (2008) 21:105–12. doi: 10.3233/BMR-2008-21206
38. Moon, HJ, Choi, KH, Kim, DH, Kim, HJ, Cho, YK, Lee, KH, et al. Effect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back pain. Ann Rehabil Med. (2013) 37:110–7. doi: 10.5535/arm.2013.37.1.110
39. Bronfort, G, Maiers, MJ, Evans, RL, Schulz, CA, Bracha, Y, Svendsen, KH, et al. Supervised exercise, spinal manipulation, and home exercise for chronic low back pain: a randomized clinical trial. Spine J. (2011) 11:585–98. doi: 10.1016/j.spinee.2011.01.036
40. Cai, C, Yang, Y, and Kong, PW. Comparison of lower limb and Back exercises for runners with chronic low Back pain. Med Sci Sports Exerc. (2017) 49:2374–84. doi: 10.1249/MSS.0000000000001396
41. Demirel, A, Oz, M, Ozel, YA, Cetin, H, and Ulger, O. Stabilization exercise versus yoga exercise in non-specific low back pain: pain, disability, quality of life, performance: a randomized controlled trial. Complement Ther Clin Pract. (2019) 35:102–8. doi: 10.1016/j.ctcp.2019.02.004
42. Dundar, U, Solak, O, Yigit, I, Evcik, D, and Kavuncu, V. Clinical effectiveness of aquatic exercise to treat chronic low back pain: a randomized controlled trial. Spine. (2009) 34:1436–40. doi: 10.1097/BRS.0b013e3181a79618
43. Roh, HS, Cho, WJ, Ryu, WJ, Park, SJ, and An, CS. The change of pain and lumbosacral sagittal alignment after sling exercise therapy for patients with chronic low back pain. J Phys Ther Sci. (2016) 28:2789–92. doi: 10.1589/jpts.28.2789
44. Rydeard, R, Leger, A, and Smith, D. Pilates-based therapeutic exercise: effect on subjects with nonspecific chronic low back pain and functional disability: a randomized controlled trial. J Orthop Sports Phys Ther. (2006) 36:472–84. doi: 10.2519/jospt.2006.2144
45. Garcia, AN, Costa Lda, C, da Silva, TM, Gondo, FL, Cyrillo, FN, Costa, RA, et al. Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther. (2013) 93:729. doi: 10.2522/ptj.20120414
46. Torstensen, TA, Ljunggren, AE, Meen, HD, Odland, E, Mowinckel, P, and Geijerstam, S. Efficiency and costs of medical exercise therapy, conventional physiotherapy, and self-exercise in patients with chronic low back pain. A pragmatic, randomized, single-blinded, controlled trial with 1-year follow-up. Spine. (1998) 23:2616–24. doi: 10.1097/00007632-199812010-00017
47. Mannion, AF, Müntener, M, Taimela, S, and Dvorak, J. A randomized clinical trial of three active therapies for chronic low back pain. Spine. (1999) 24:2435–48. doi: 10.1097/00007632-199912010-00004
48. Macedo, LG, Latimer, J, Maher, CG, Hodges, PW, McAuley, JH, Nicholas, MK, et al. Effect of motor control exercises versus graded activity in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther. (2012) 92:363–77. doi: 10.2522/ptj.20110290
49. Lee, JS, and Kang, SJ. The effects of strength exercise and walking on lumbar function, pain level, and body composition in chronic back pain patients. J Exerc Rehabil. (2016) 12:463–70. doi: 10.12965/jer.1632650.325
50. Kell, RT, and Asmundson, GJG. A comparison of two forms of periodized exercise rehabilitation programs in the management of chronic nonspecific low-back pain. J Strength Cond Res. (2009) 23:513–23. doi: 10.1519/JSC.0b013e3181918a6e
51. Chatzitheodorou, D, Kabitsis, C, Malliou, P, and Mougios, V. A pilot study of the effects of high-intensity aerobic exercise versus passive interventions on pain, disability, psychological strain, and serum cortisol concentrations in people with chronic low back pain. Phys Ther. (2007) 87:304–12. doi: 10.2522/ptj.20060080
52. Murtezani, A, Govori, V, Meka, VS, Ibraimi, Z, Rrecaj, S, and Gashi, S. A comparison of Mckenzie therapy with electrophysical agents for the treatment of work related low back pain: a randomized controlled trial. J Back Musculoskelet Rehabil. (2015) 28:247–53. doi: 10.3233/BMR-140511
53. Unsgaard-Tøndel, M, Fladmark, AM, Salvesen, Ø, and Vasseljen, O. Motor control exercises, sling exercises, and general exercises for patients with chronic low back pain: a randomized controlled trial with 1-year follow-up. Phys Ther. (2010) 90:1426–40. doi: 10.2522/ptj.20090421
54. Murtezani, A, Hundozi, H, Orovcanec, N, Sllamniku, S, and Osmani, T. A comparison of high intensity aerobic exercise and passive modalities for the treatment of workers with chronic low back pain: a randomized, controlled trial. Eur J Phys Rehabil Med. (2011) 47:359–66.
55. Szulc, P, Wendt, M, Waszak, M, Tomczak, M, Cieślik, K, and Trzaska, T. Impact of McKenzie method therapy enriched by muscular energy techniques on subjective and objective parameters related to spine function in patients with chronic low Back pain. Med Sci Monit. (2015) 21:2918–32. doi: 10.12659/MSM.894261
56. Tekur, P, Nagarathna, R, Chametcha, S, Hankey, A, and Nagendra, HR. A comprehensive yoga programs improves pain, anxiety and depression in chronic low back pain patients more than exercise: an RCT. Complement Ther Med. (2012) 20:107–18. doi: 10.1016/j.ctim.2011.12.009
57. Tekur, P, Singphow, C, Nagendra, HR, and Raghuram, N. Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: a randomized control study. J Altern Complement Med. (2008) 14:637–44. doi: 10.1089/acm.2007.0815
58. Sipaviciene, S, and Kliziene, I. Effect of different exercise programs on non-specific chronic low back pain and disability in people who perform sedentary work. Clin Biomech (Bristol, Avon). (2020) 73:17–27. doi: 10.1016/j.clinbiomech.2019.12.028
59. Shnayderman, I, and Katz-Leurer, M. An aerobic walking programme versus muscle strengthening programme for chronic low back pain: a randomized controlled trial. Clin Rehabil. (2013) 27:207–14. doi: 10.1177/0269215512453353
60. Shamsi, MB, Rezaei, M, Zamanlou, M, Sadeghi, M, and Pourahmadi, MR. Does core stability exercise improve lumbopelvic stability (through endurance tests) more than general exercise in chronic low back pain? A quasi-randomized controlled trial. Physiother Theory Pract. (2016) 32:171–8. doi: 10.3109/09593985.2015.1117550
61. Shamsi, MB, Sarrafzadeh, J, and Jamshidi, A. Comparing core stability and traditional trunk exercise on chronic low back pain patients using three functional lumbopelvic stability tests. Physiother Theory Pract. (2015) 31:89–98. doi: 10.3109/09593985.2014.959144
62. Waseem, M, Karimi, H, Gilani, SA, and Hassan, D. Treatment of disability associated with chronic non-specific low back pain using core stabilization exercises in Pakistani population. J Back Musculoskelet Rehabil. (2019) 32:149–54. doi: 10.3233/BMR-171114
63. Valenza, MC, Rodríguez-Torres, J, Cabrera-Martos, I, Díaz-Pelegrina, A, Aguilar-Ferrándiz, ME, and Castellote-Caballero, Y. Results of a Pilates exercise program in patients with chronic non-specific low back pain: a randomized controlled trial. Clin Rehabil. (2017) 31:753–60. doi: 10.1177/0269215516651978
64. Yozbatiran, N, Yildirim, Y, and Parlak, B. Effects of fitness and aquafitness exercises on physical fitness in patients with chronic low back pain. Pain Clin. (2004) 16:35–42. doi: 10.1163/156856904322858684
65. Williams, KA, Petronis, J, Smith, D, Goodrich, D, Wu, J, Ravi, N, et al. Effect of Iyengar yoga therapy for chronic low back pain. Pain. (2005) 115:107–17. doi: 10.1016/j.pain.2005.02.016
66. Zeada, MA. Effects of Pilates on low back pain and urine catecholamine. Ovidus Univ Ann Ser Phys Edu Sport Sci Move Health. (2012) 12:41–7.
67. Cruz-Díaz, D, Bergamin, M, Gobbo, S, Martínez-Amat, A, and Hita-Contreras, F. Comparative effects of 12 weeks of equipment based and mat Pilates in patients with chronic low Back pain on pain, function and transversus abdominis activation. A randomized controlled trial. Complement Ther Med. (2017) 33:72–7. doi: 10.1016/j.ctim.2017.06.004
68. Yoo, YD, and Lee, YS. The effect of core stabilization exercises using a sling on pain and muscle strength of patientswith chronic low back pain. J Phys Ther Sci. (2012) 24:671–4. doi: 10.1589/jpts.24.671
69. Cho, Y. Effects of tai chi on pain and muscle activity in young males with acute low back pain. J Phys Ther Sci. (2014) 26:679–81. doi: 10.1589/jpts.26.679
70. Hwangbo, G, Lee, CW, Kim, SG, and Kim, HS. The effects of trunk stability exercise and a combined exercise program on pain, flexibility, and static balance in chronic low back pain patients. J Phys Ther Sci. (2015) 27:1153–5. doi: 10.1589/jpts.27.1153
71. Young, KJ, Je, CW, and Hwa, ST. Effect of proprioceptive neuromuscular facilitation integration pattern and swiss ball training on pain and balance in elderly patients with chronic back pain. J Phys Ther Sci. (2015) 27:3237–40. doi: 10.1589/jpts.27.3237
72. Jeong, UC, Sim, JH, Kim, CY, Hwang-Bo, G, and Nam, CW. The effects of gluteus muscle strengthening exercise and lumbar stabilization exercise on lumbar muscle strength and balance in chronic low back pain patients. J Phys Ther Sci. (2015) 27:3813–6. doi: 10.1589/jpts.27.3813
73. Yu, SH, Sim, YH, Kim, MH, Bang, JH, Son, KH, Kim, JW, et al. The effect of abdominal drawing-in exercise and myofascial release on pain, flexibility, and balance of elderly females. J Phys Ther Sci. (2016) 28:2812–5. doi: 10.1589/jpts.28.2812
74. Ko, KJ, Ha, GC, Yook, YS, and Kang, SJ. Effects of 12-week lumbar stabilization exercise and sling exercise on lumbosacral region angle, lumbar muscle strength, and pain scale of patients with chronic low back pain. J Phys Ther Sci. (2018) 30:18–22. doi: 10.1589/jpts.30.18
75. Arampatzis, A, Schroll, A, Catalá, MM, Laube, G, Schüler, S, and Dreinhofer, K. A random-perturbation therapy in chronic non-specific low-back pain patients: a randomised controlled trial. Eur J Appl Physiol. (2017) 117:2547–60. doi: 10.1007/s00421-017-3742-6
76. Noormohammadpour, P, Kordi, M, Mansournia, MA, Akbari-Fakhrabadi, M, and Kordi, R. The role of a multi-step Core stability exercise program in the treatment of nurses with chronic low Back pain: a single-blinded randomized controlled trial. Asian Spine J. (2018) 12:490–502. doi: 10.4184/asj.2018.12.3.490
77. Bae, CR, Jin, Y, Yoon, BC, Kim, NH, Park, KW, and Lee, SH. Effects of assisted sit-up exercise compared to core stabilization exercise on patients with non-specific low back pain: a randomized controlled trial. J Back Musculoskelet Rehabil. (2018) 31:871–80. doi: 10.3233/BMR-170997
78. Segal-Snir, Y, Lubetzky, VA, and Masharawi, Y. Rotation exercise classes did not improve function in women with non-specific chronic low back pain: a randomized single blind controlled study. J Back Musculoskelet Rehabil. (2016) 29:467–75. doi: 10.3233/BMR-150642
79. Ulger, O, Demirel, A, Oz, M, and Tamer, S. The effect of manual therapy and exercise in patients with chronic low back pain: double blind randomized controlled trial. J Back Musculoskelet Rehabil. (2017) 30:1303–9. doi: 10.3233/BMR-169673
80. Schinhan, M, Neubauer, B, Pieber, K, Gruber, M, Kainberger, F, Castellucci, C, et al. Climbing has a positive impact on low Back pain: a prospective randomized controlled trial. Clin J Sport Med. (2016) 26:199–205. doi: 10.1097/JSM.0000000000000238
81. del Pozo-Cruz, B, Hernández Mocholí, MA, Adsuar, JC, Parraca, JA, Muro, I, and Gusi, N. Effects of whole body vibration therapy on main outcome measures for chronic non-specific low back pain: a single-blind randomized controlled trial. J Rehabil Med. (2011) 43:689–94. doi: 10.2340/16501977-0830
82. Kell, RT, Risi, AD, and Barden, JM. The response of persons with chronic nonspecific low back pain to three different volumes of periodized musculoskeletal rehabilitation. J Strength Cond Res. (2011) 25:1052–64. doi: 10.1519/JSC.0b013e3181d09df7
83. Yoo, JH, Kim, SE, Lee, MG, Jin, JJ, Hong, J, Choi, YT, et al. The effect of horse simulator riding on visual analogue scale, body composition and trunk strength in the patients with chronic low back pain. Int J Clin Pract. (2014) 68:941–9. doi: 10.1111/ijcp.12414
84. Oh, HW, Lee, MG, Jang, JY, Jin, JJ, Cha, JY, Jin, YY, et al. Time-effects of horse simulator exercise on psychophysiological responses in men with chronic low back pain. Isokinet Exerc Sci. (2014) 22:153–63. doi: 10.3233/IES-140533
85. Harts, CC, Helmhout, PH, de Bie, RA, and Staal, JB. A high-intensity lumbar extensor strengthening program is little better than a low-intensity program or a waiting list control group for chronic low back pain: a randomised clinical trial. Aust J Physiother. (2008) 54:23–31. doi: 10.1016/S0004-9514(08)70062-X
86. Gur, A, Karakoc, M, Cevik, R, Nas, K, Sarac, AJ, and Karakoc, M. Efficacy of low power laser therapy and exercise on pain and functions in chronic low back pain. Lasers Surg Med. (2003) 32:233–8. doi: 10.1002/lsm.10134
87. Zadro, JR, Shirley, D, Simic, M, Mousavi, SJ, Ceprnja, D, Maka, K, et al. Video-game-based exercises for older people with chronic low Back pain: a randomized Controlledtable trial (GAMEBACK). Phys Ther. (2019) 99:14–27. doi: 10.1093/ptj/pzy112
88. Williams, K, Abildso, C, Steinberg, L, Doyle, E, Epstein, B, Smith, D, et al. Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine. (2009) 34:2066–76. doi: 10.1097/BRS.0b013e3181b315cc
89. Costa, LO, Maher, CG, Latimer, J, Hodges, PW, Herbert, RD, Refshauge, KM, et al. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther. (2009) 89:1275–86. doi: 10.2522/ptj.20090218
90. Kofotolis, N, and Kellis, E. Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional performance in women with chronic low back pain. Phys Ther. (2006) 86:1001–12.16813479. doi: 10.1093/ptj/86.7.1001
91. Areeudomwong, P, Wongrat, W, Neammesri, N, and Thongsakul, T. A randomized controlled trial on the long-term effects of proprioceptive neuromuscular facilitation training, on pain-related outcomes and back muscle activity, in patients with chronic low back pain. Musculoskeletal Care. (2017) 15:218–29. doi: 10.1002/msc.1165
92. Masharawi, Y, and Nadaf, N. The effect of non-weight bearing group-exercising on females with non-specific chronic low back pain: a randomized single blind controlled pilot study. J Back Musculoskelet Rehabil. (2013) 26:353–9. doi: 10.3233/BMR-130391
93. Lawand, P, Lombardi Júnior, I, Jones, A, Sardim, C, Ribeiro, LH, and Natour, J. Effect of a muscle stretching program using the global postural reeducation method for patients with chronic low back pain: a randomized controlled trial. Joint Bone Spine. (2015) 82:272–7. doi: 10.1016/j.jbspin.2015.01.015
94. Kofotolis, N, Kellis, E, Vlachopoulos, SP, Gouitas, I, and Theodorakis, Y. Effects of Pilates and trunk strengthening exercises on health-related quality of life in women with chronic low back pain. J Back Musculoskelet Rehabil. (2016) 29:649–59. doi: 10.3233/BMR-160665
95. Kofotolis, ND, Vlachopoulos, SP, and Kellis, E. Sequentially allocated clinical trial of rhythmic stabilization exercises and TENS in women with chronic low back pain. Clin Rehabil. (2008) 22:99–111. doi: 10.1177/0269215507080122
96. Kim, T, Lee, J, Oh, S, Kim, S, and Yoon, B. Effectiveness of simulated horseback riding for patients with chronic low Back pain: a randomized controlled trial. J Sport Rehabil. (2020) 29:179–85. doi: 10.1123/jsr.2018-0252
97. Salik Sengul, Y, Yilmaz, A, Kirmizi, M, Kahraman, T, and Kalemci, O. Effects of stabilization exercises on disability, pain, and core stability in patients with non-specific low back pain: a randomized controlled trial. Work. (2021) 70:99–107. doi: 10.3233/WOR-213557
98. Ferreira, ML, Ferreira, PH, Latimer, J, Herbert, RD, Hodges, PW, Jennings, MD, et al. Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: a randomized trial. Pain. (2007) 131:31–7. doi: 10.1016/j.pain.2006.12.008
99. Leopoldino, AA, Diz, JB, Martins, VT, Henschke, N, Pereira, LS, Dias, RC, et al. Prevalence of low back pain in older Brazilians: a systematic review with meta-analysis. Rev Bras Reumatol Engl Ed. (2016) 56:258–69. doi: 10.1016/j.rbre.2016.03.011
100. Patel, KV, Guralnik, JM, Dansie, EJ, and Turk, DC. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and aging trends study. Pain. (2013) 154:2649–57. doi: 10.1016/j.pain.2013.07.029
101. Maher, C, Underwood, M, and Buchbinder, R. Non-specific low back pain. Lancet. (2017) 389:736–47. doi: 10.1016/S0140-6736(16)30970-9
102. Dieleman, JL, Baral, R, Birger, M, Bui, AL, Bulchis, A, Chapin, A, et al. US spending on personal health care and public health, 1996–2013. JAMA. (2016) 316:2627–46. doi: 10.1001/jama.2016.16885
103. Lauche, R, Stumpe, C, Fehr, J, Cramer, H, Cheng, YW, Wayne, PM, et al. The effects of tai chi and Neck exercises in the treatment of chronic nonspecific neck pain: a randomized controlled trial. J Pain. (2016) 17:1013–27. doi: 10.1016/j.jpain.2016.06.004
104. Kong, LJ, Lauche, R, Klose, P, Bu, JH, Yang, XC, Guo, CQ, et al. Tai chi for chronic pain conditions: a systematic review and Meta-analysis of randomized controlled trials. Sci Rep. (2016) 6:25325. doi: 10.1038/srep25325
105. Hall, AM, Kamper, SJ, Emsley, R, and Maher, CG. Does pain-catastrophising mediate the effect of tai chi on treatment outcomes for people with low back pain? Complement Ther Med. (2016) 25:61–6. doi: 10.1016/j.ctim.2015.12.013
106. Ito, T, Sakai, Y, Morita, Y, Yamazaki, K, Igarashi, K, Nishio, R, et al. Proprioceptive weighting ratio for balance control in static standing is reduced in elderly patients with non-specific low Back pain. Spine. (2018) 43:1704–9. doi: 10.1097/BRS.0000000000002817
107. Wennan, Z. Experimental study on the effect of tai chi exercise on event-related potentials in patients with chronic lower back pain[D] Shanghai Institute of Physical Education (2013).
108. Yeh, GY, Wood, MJ, Lorell, BH, Stevenson, LW, Eisenberg, DM, Wayne, PM, et al. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. (2004) 117:541–8. doi: 10.1016/j.amjmed.2004.04.016
109. Qaseem, A, Wilt, TJ, RM, ML, Forciea, MA, Clinical Guidelines Committee of the American College of Physicians, Denberg, TD, et al. Noninvasive treatments for acute, subacute, and chronic low Back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. (2017) 166:514–30. doi: 10.7326/M16-2367
110. Byrnes, K, Wu, PJ, and Whillier, S. Is Pilates an effective rehabilitation tool? A systematic review. J Bodyw Mov Ther. (2018) 22:192–202. doi: 10.1016/j.jbmt.2017.04.008
111. Miranda, S, and Marques, A. Pilates in noncommunicable diseases: a systematic review of its effects. Complement Ther Med. (2018) 39:114–30. doi: 10.1016/j.ctim.2018.05.018
112. Kaigle, AM, Holm, SH, and Hansson, TH. Experimental instability in the lumbar spine. Spine. (1995) 20:421–30. doi: 10.1097/00007632-199502001-00004
113. Choi, HY, and Lee, CH. Can Beta-endorphin be used as a biomarker for chronic low Back pain? A Meta-analysis of randomized controlled trials. Pain Med. (2019) 20:28–36. doi: 10.1093/pm/pny186
114. Paungmali, A, Joseph, LH, Punturee, K, Sitilertpisan, P, Pirunsan, U, and Uthaikhup, S. Immediate effects of Core stabilization exercise on β -endorphin and cortisol levels among patients with chronic nonspecific low Back pain: a randomized crossover design. J Manip Physiol Ther. (2018) 41:181–8. doi: 10.1016/j.jmpt.2018.01.002
115. Barros Dos Santos, AO, Pinto de Castro, JB, Lima, VP, da Silva, EB, and de Souza Vale, RG. Effects of physical exercise on low back pain and cortisol levels: a sys-tematic review with meta-analysis of randomized controlled trials. Pain Manag. (2021) 11:49–57. doi: 10.2217/pmt-2020-0020
116. Zhai, YY, Cui, YH, and Xu, HK. Effects of core stabilization exercise on β-endorphin and cortisol levels in patients with nonspecific low back pain. J Neck Low Back Pain. (2021) 42:100–2.
117. Wang, K, Bao, JP, Yang, S, Hong, X, Liu, L, Xie, XH, et al. A cohort study comparing the se- rum levels of pro- or anti-inflammatory cytokines in patients with lumbar radicular pain and healthy subjects. Eur Spine J. (2016) 25:1428–34. doi: 10.1007/s00586-015-4349-4
118. Nambi, G, Abdelbasset, WK, Alsubaie, SF, Moawd, SA, Verma, A, Saleh, AK, et al. Isokinetic training - its radiographic and inflammatory effects on chronic low back pain: a randomized controlled trial. Medicine. (2020) 99:e23555. doi: 10.1097/MD.0000000000023555
119. Zhu, F, Zhang, M, Wang, D, Hong, Q, Zeng, C, and Chen, W. Yoga compared to non-exercise or physical therapy exercise on pain, disability, and quality of life for patients with chronic low back pain: a systematic review and meta-analysis of randomized controlled trials. PLoS One. (2020) 15:e0238544. doi: 10.1371/journal.pone.0238544
120. Carneiro, KA, and Rittenberg, JD. The role of exercise and alternative treatments for low back pain. Phys Med Rehabil Clin. (2010) 21:777–92. doi: 10.1016/j.pmr.2010.06.006
121. Wolsko, PM, Eisenberg, DM, Davis, RB, Kessler, R, and Phillips, RS. Patterns and perceptions of care for treatment of back and neck pain: results of a national survey. Spine. (2003) 28:292–7. discussion: 298. doi: 10.1097/01.BRS.0000042225.88095.7C
122. Deodato, M, Saponaro, S, Šimunič, B, Martini, M, Galmonte, A, Murena, L, et al. Sex-based comparison of trunk flexors and extensors functional and contractile characteristics in young gymnasts. Sport Sci Health. (2023) 1–9. doi: 10.1007/s11332-023-01083-7
123. Fernández-Rodríguez, R, Álvarez-Bueno, C, Cavero-Redondo, I, Torres-Costoso, A, Pozuelo-Carrascosa, DP, Reina-Gutiérrez, S, et al. Best exercise options for reducing pain and disability in adults with chronic low back pain: pilates, strength, core-based, and mind-body. A network Meta-analysis. J Orthop Sports Phys Ther. (2022) 52:505–21. doi: 10.2519/jospt.2022.10671
Keywords: exercise therapy, chronic low back pain, network meta-analysis, CLBP, aging and public health
Citation: Li Y, Yan L, Hou L, Zhang X, Zhao H, Yan C, Li X, Li Y, Chen X and Ding X (2023) Exercise intervention for patients with chronic low back pain: a systematic review and network meta-analysis. Front. Public Health. 11:1155225. doi: 10.3389/fpubh.2023.1155225
Edited by:
Jun Zou, Shanghai University of Sport, ChinaReviewed by:
Manuela Deodato, University of Trieste, ItalyLjubica Konstantinovic, University of Belgrade, Serbia
Indrani Poddar, University of Minnesota Twin Cities, United States
Copyright © 2023 Li, Yan, Hou, Zhang, Zhao, Yan, Li, Li, Chen and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaorong Ding, MTQ0MjkzNTE5M0BxcS5jb20=; Xiaoan Chen, ODEyNTU3NDUzQHFxLmNvbQ==
†These authors have contributed equally to this work
 Ying Li
Ying Li Lei Yan2,3†
Lei Yan2,3†