- School of Nursing and Health, Zhengzhou University, Zhengzhou, Henan, China
Objectives: Sarcopenia and disability represent significant concerns impacting the health of older people. This study aimed to explore the bidirectional relationship between sarcopenia and disability in Chinese older people.
Methods: This study recruited older people ≥60 years old from the China Health and Retirement Longitudinal Study. In phase I, the study analyzed the relation between disability and subsequent sarcopenia using multinomial logistic regression models. Conversely, in phase II, the study assessed whether sarcopenia was associated with future disability using binary logistic regression models.
Results: In phase I, 65 (16.80%) new cases of possible sarcopenia, 18 (4.65%) cases of sarcopenia, and 9 (2.33%) cases of severe sarcopenia were observed in the disabled older people and 282 (10.96%) new cases of possible sarcopenia, 97 (3.77%) cases of sarcopenia, 35 (1.36%) cases of severe sarcopenia were observed in the older people without disability. The OR (95% CI) for sarcopenia in older disabled individuals compared to those without disability was 1.61 (1.25–2.07). Adjusting for all covariates in 2011, the OR (95% CI) value for disabled individuals vs. those without disability was 1.35 (1.02–1.79). Subgroup analyses showed that disabled participants aged <80 years were more likely to have sarcopenia (OR = 1.42, 95% CI: 1.07–1.89), and the risk of sarcopenia did not differ significantly between sex subgroups. In phase II, 114 cases (33.83%) in the possible sarcopenia patients, 85 cases (28.91%) in the sarcopenia patients, 23 cases (35.94%) in the severe sarcopenia patients, and 501 cases (16.10%) in the individuals without sarcopenia showed symptoms of disability. The OR (95% CI) for disability was 2.66 (2.08–3.40) in the possible sarcopenia patients, 2.12 (1.62–2.77) in the sarcopenia patients, and 2.92 (1.74–4.91) in the severe sarcopenia patients compared with the no sarcopenia patients. After adjusting for all covariates in 2011, the OR (95% CI) values were 2.21 (1.70–2.85) in the possible sarcopenia patients, 1.58 (1.14–2.19) in the sarcopenia patients, and 1.99 (1.14–3.49) in the severe sarcopenia patients, as compared to the older people without sarcopenia. Subgroup analyses showed that compared with men, women with possible sarcopenia had a higher risk of disability (OR = 2.80, 95% CI: 1.98–3.97). In addition, participants aged <80 years with sarcopenia or severe sarcopenia s were more likely to have disability (OR = 2.13, 95% CI: 1.52–2.98; OR = 2.98, 95% CI: 1.60–5.54).
Conclusion: The occurrence of disability increase the risk of sarcopenia in the older people, and baseline sarcopenia predicts the future disability in older people.
Introduction
With the increasing aging of the population, the prevalence of sarcopenia is on the rise. Currently, ~50 million older persons worldwide suffer from sarcopenia, and this number is expected to reach 500 million by 2050 (1, 2). In Japan, the prevalence of sarcopenia among older individuals is 11.5–16.7% (3), while in China, it is 26.6% (4). Older people with sarcopenia experience significantly lower quality of life in terms of physical function, health status, and social function (5), and they are at a higher risk for falls, disability, death, cognitive impairment, and depression (6–12). Additionally, sarcopenia can either cause or exacerbate other conditions such as osteoporosis (13) and coronary heart disease (14). Therefore, it is crucial to identify the risk factors for sarcopenia in order to develop effective prevention programs. Furthermore, disability is also a significant issue in the aging population. In China, the number of disabled older people is projected to exceed 42 million in 2020 and reach 137 million by 2030 (15, 16). Disability negatively impacts the quality of life of the older people, and adds to the burden of care for their families and society (17). Therefore, it is important to study the factors influencing disability and work toward preventing disability in older people.
Several studies have analyzed the relationship between sarcopenia and disability, Xu et al. (7) found that sarcopenia was independently associated with disability in community-dwelling older people in China, with those suffering from sarcopenia being approximately twice as likely to be disabled in ADLs compared to those without sarcopenia. Kitamura et al. (3) demonstrated that older Japanese sarcopenia patients had an increased risk of disability, and there was no significant increase in disability risk for those with possible sarcopenia and those with only low muscle mass. However, no relevant studies have explored the interrelationship between the two. Considering the shared influencing factors and pathophysiological mechanisms between sarcopenia and disability, such as age, physical activity, inflammatory responses, and levels of oxidative stress, it is possible that they may interact with each other.
This study aims to analyze the relation between sarcopenia and disability based on the findings of the China Health and Retirement Longitudinal Study (CHARLS). In phase I, the study assessed disability and future sarcopenia's connection. In phase II, the study analyzed the relation between the presence of sarcopenia and disability.
Methods
Data sources
In this study, we utilized data from CHARLS (18). The data set is a longitudinal, nationally representative cohort survey with people in China aged 45 years and older, aiming at collecting information related to social, economic and health conditions. The national baseline assessment was conducted in 2011, involving ~17,000 participants, and follow-up assessments were carried out in 2013, 2015, and 2018, and there were studies described CHARLS in more detail (18, 19). The data of 2011 and 2015 were used for this study. In phase I, we focused on individuals without sarcopenia in 2011, dividing them into disability and no disability groups, and then followed up to 2015 to assess the development of possible sarcopenia, sarcopenia, and severe sarcopenia. In phase II, we studied individuals without disability in 2011, categorizing them into no sarcopenia, possible sarcopenia, sarcopenia, and severe sarcopenia groups, and followed them up to 2015 to assess disability status.
Participants
Phase I participants must meet the following requirements: (1) aged ≥60 years, (2) without possible sarcopenia and sarcopenia, (3) collected the information related to ADL, (4) successfully followed up in 2015. A total of 2,961 participants were included in the follow-up analysis (Figure 1). Phase II participants were required to (1) aged ≥60 years, (2) without disability, (3) collected the information related to sarcopenia, (4) successfully followed up in 2015. Ultimately, 3,806 participants were included in the follow-up analysis (Figure 1). Less than 5% of the data were missing covariable information, we imputed missing data based on mean imputation.
Sarcopenia
In this study, we adopted the AWGS 2019 standard to define and evaluate sarcopenia using three indexes: appendicular skeletal muscle mass (ASM), muscle strength and physical function (20). Sarcopenia is characterized by decreased muscle mass, accompanied by reduced physical function and/or muscle strength. In addition, the 2019 Asian Sarcopenia Working Group pointed out that if older people have normal muscle mass and decreased muscle strength, regardless of whether the physical function is decreased, they are called possible sarcopenia patients.
ASM is calculated using anthropometric equation developed and verified for China population (21). ASM = 0.193 * weight (kg) + 0.107 * height (cm) – 4.157 * sex (male = 1, female = 2) – 0.037 * age – 2.631. Studies have shown strong agreement between dual X-ray absorptiometry (DXA) and the ASM equation model (21, 22). The critical value of muscle mass reduction is determined according to the sex-specific lowest 20% of the height (Ht)-adjusted muscle mass [skeletal muscle mass index (SMI) = ASM/Ht2] within the study population (22–24). In this study, the SMI value of women is < 5.38 kg/m2, and that of men is < 7.08 kg/m2, which indicates that muscle mass is reduced. Muscle strength was measured using a grip strength meter, and values below 28 kg for males and below 18 kg for females indicate decreased muscle strength. Decline in physical function in this study was defined as a decline in lower limb mobility in the older person, which was assessed using the chair stand test, if an individual takes longer than 12 s to complete the task for five-times, it indicates a decline in physical function.
Disability
In this study, disability refers to the decreased ability of older people to perform activities of daily living assessed using the basic activities of daily living (BADL) and instrumental activities of daily living (IADL) scales (25). BADLs includes six questions: dressing, getting out of bed, eating, bathing, toileting and continence. IADLs includes five problems: doing housework, taking medication, shopping, cooking and handling finances. Each question includes four answer options: no difficulty; difficult but achievable; some difficulties and need help; unable to complete. The older people are considered to have a disability if they lack complete independence in any question (26, 27).
Covariates
Other covariates collected included sex (females and males), age, residence (rural and urban), marital status (married/cohabitated and separated/divorced/widowed/never married), educational level (illiterate/primary school, middle school, high school/vocational high school, and junior college or above), smoking status (still smoking, ever smoking, and never smoking), drinking status (drink more than once a month, drink but less than once a month, no drinking), body mass index (BMI < 18.5, 18.5 ≤ BMI < 24, BMI ≥ 24), and annual household expenditure level (in tertiles), whether accompanied by other chronic diseases [high blood sugar (HBS)/diabetes, lung disease, hypertension, heart disease, cancer, stroke, dyslipidemia, digestive disease, kidney disease, liver disease, emotional, nervous, or psychiatric problems, memory-related disease, arthritis or rheumatism and asthma].
Statistical analyses
We conducted statistical analyses to assess the normality of continuous variables using Skewness-Kurtosis tests. Since the age did not follow a normal distribution (P < 0.05), its description was based on the median (p25–p75), and the comparison of baseline characteristics between groups utilized the Wilcoxon rank sum test and Kruskal-Wallis rank sum test. Categorical variables were described with frequency (percentage), and the differences in baseline characteristics between groups were compared using the chi-square test. In phase I, we utilized binary logistic regression models to estimate the odds ratio (ORs) and confidence intervals (CIs) between baseline disability and subsequent sarcopenia. In phase II, binary logistic regression models were also used to investigate whether baseline sarcopenia was associated with an increased risk of disability in older people. Both models were adjusted for potential confounding factors (adjusted Model 1 adjusted for gender and age; adjusted model 2 adjusted all covariates in this study). Finally, sex and age (< 80, ≥80) were analyzed in subgroups. In order to explore whether other chronic diseases will affect the results, we conducted a sensitivity analysis. In addition, we performed additional post-hoc power analysis for each of the two phases. Statistical analyses were carried out using STATA version 17 software, with the significance level set at 0.05.
Results
Baseline characteristics of the participants
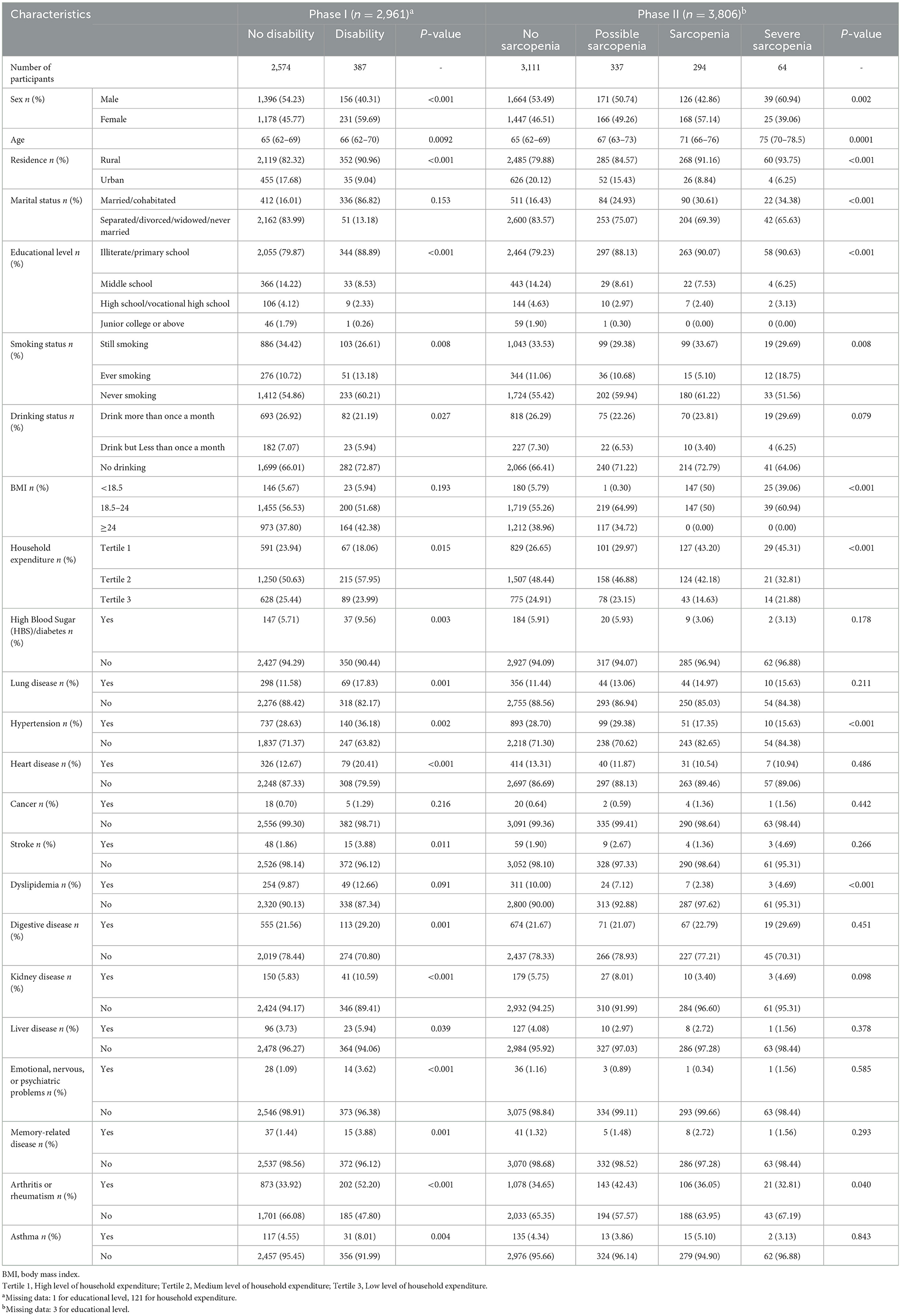
The results showed that in phase I, out of 2,961 participants, 387 (13.07%) had disability, while in phase II, out of 3,806 older persons, 337 (8.85%) participants had possible sarcopenia, 294 (7.72%) had sarcopenia, and 64 (1.68%) had severe sarcopenia. Table 1 presents the baseline characteristics of the two phases.
Phase I: the relationship between baseline disability and follow-up sarcopenia
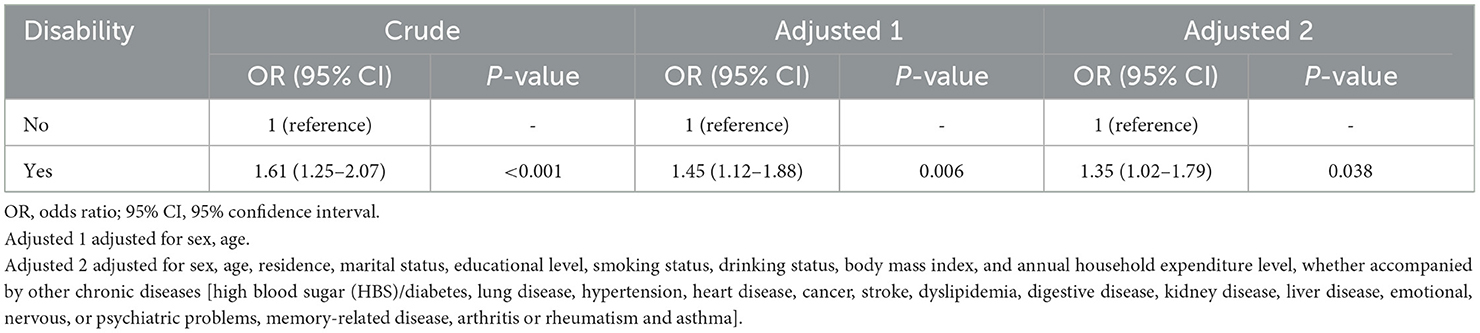
During the 4-year follow-up, 65 (16.8%) new cases of possible sarcopenia, 18 (4.7%) new cases of sarcopenia, and 9 (2.3%) new cases of severe sarcopenia were reported in disabled patients, additional information is shown in Table 2. Those considered disabled had a higher risk of subsequent sarcopenia (crude OR = 1.61; 95% CI = 1.25–2.07). After adjusting for all covariates in 2011, the OR (95% CI) values for older people with disability was 1.35 (1.02–1.79) compared with individuals without disability (Table 3). Subgroup analyses showed that participants with disability aged < 80 years had a higher risk of sarcopenia (OR = 1.42, 95% CI: 1.07–1.89), but the risk of sarcopenia did not differ significantly between sex subgroups (Supplementary Table 1). In addition, as a sensitivity analyses, we excluded patients with concomitant comorbidities of other chronic diseases, and the results did not change substantially, suggesting that the relationship between sarcopenia and disability is unlikely to be influenced by these diseases (Supplementary Table 2). After post-hoc power analysis, we found that with the group size, at alpha=0.5 the expected power to detect the difference seen is 96%. If we look for a detectable difference between no sarcopenia, sarcopenia and possible or severe sarcopenia, the power is 95%.
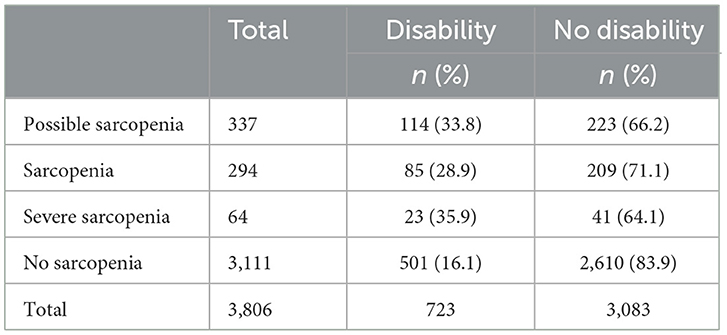
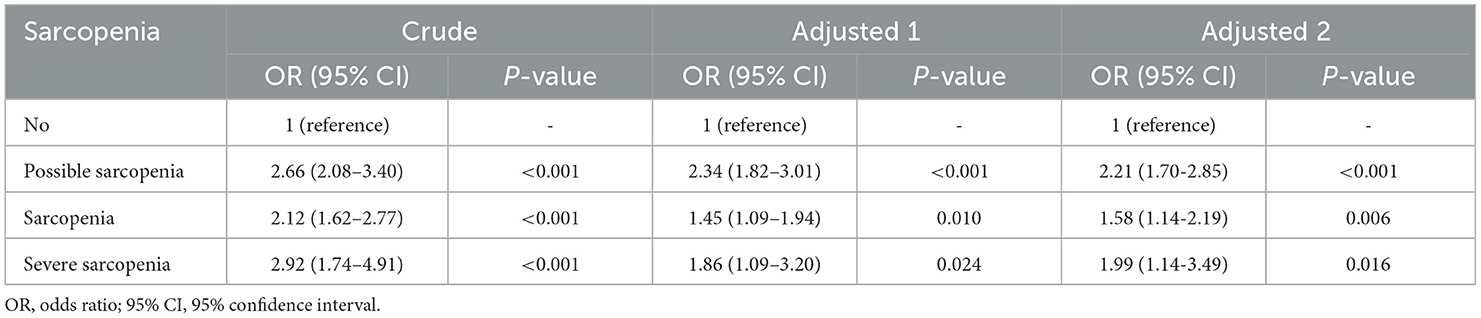
Phase II: association of baseline sarcopenia with follow-up disability
At this phase, 114 patients with possible sarcopenia, 85 patients with sarcopenia, 23 patients with severe sarcopenia, and 501 individuals with no sarcopenia showed symptoms of disability (Table 4). Compared to patients without sarcopenia, the OR (95% CI) for disability was 2.66 (2.08–3.40) for patients with possible sarcopenia, 2.12 (1.62–2.77) for patients with sarcopenia, and 2.92 (1.74–4.91) for patients with severe sarcopenia. After adjusting for all covariates at baseline, the OR (95% CI) in patients with possible sarcopenia compared with patients without sarcopenia was 2.21 (1.70–2.85), for patients with sarcopenia was 1.58 (1.14–2.19), and for patients with severe sarcopenia, the OR (95% CI) was 1.99 (1.14–3.49; Table 5). Subgroup analysis shows older female patients who may have sarcopenia are at higher risk of disability than men (OR = 2.80, 95% CI: 1.98–3.97), and patients with sarcopenia or severe sarcopenia aged < 80 years had a higher risk of disability (OR = 2.13, 95% CI: 1.52–2.98; OR = 2.98, 95% CI: 1.60–5.54; Supplementary Table 3). In addition, the results did not change after sensitivity analyses (Supplementary Table 4). Post-hoc power analysis shows that with the group size, at alpha = 0.05 the expected power to detect the difference seen is 100%.
Discussion
In our study, we observed a bidirectional relationship between disability and sarcopenia. Specifically, disability in older people increases the risk of developing sarcopenia, while possible sarcopenia, sarcopenia, and severe sarcopenia also increase the risk of subsequent disability. Even after adjusting for sex, age, or other confounders, the relation still existed. Furthermore, the connection between disability and sarcopenia exhibited some variation in subgroup analyses based on age and sex.
Several scholars in the field have analyzed the impact of sarcopenia on disability. For instance, Phillips et al. noted that sarcopenia results in higher disability scores in older people, and the 3-year incidence of disability was ~32.7% (28). Moreover, in a cross-sectional analyses of 27,924 participants in the Canadian Longitudinal Study (29), sarcopenia was associated with an increased risk of ADL disability. It is worth noting that studies have indicated that older individuals with sarcopenia exhibit lower levels of basic and instrumental activities of daily living compared to those without sarcopenia (30, 31), suggesting that both may be influenced by sarcopenia.
Sarcopenia as a risk factor for subsequent disability is confirmed by the fact that sarcopenia is associated with future disability, even after adjusting for sex, age, and other covariates. Proactively preventing and managing sarcopenia has been shown to effectively reduce the risk of disability (32, 33), therefore, it is recommended that sarcopenia should be included when screening for disability. Additionally, our study found that the ORs for increased risk of disability did not progressively increase by severity of sarcopenia. Patients with possible sarcopenia and severe sarcopenia displayed a higher risk of disability, while patients with sarcopenia had a relatively lower risk, it is an interesting phenomenon. This may because that a higher number of patients with possible sarcopenia had reduced physical function and therefore a higher risk of subsequent disability, whereas all patients with severe sarcopenia had reduced physical function. Therefore, patients with possible sarcopenia (especially with reduced physical function) need to be given equivalent attention as patients with severe sarcopenia when it comes to preventing disability in the older person. We are currently unaware of studies investigating the impact of disability on sarcopenia. In our study, disability remained positively associated with subsequent sarcopenia even after adjustment for covariables. Older people who are impaired in physical activity (34) and spend most of their time in a sedentary state (35) are at increased risk for sarcopenia, which may contribute to the results of the study.
Several explanations may elucidate the bidirectional relation between disability and sarcopenia. Firstly, sarcopenia may lead to an increased number of falls (6) and reduced exercise participation (36) in older people, consequently increasing the risk of disability. Similarly, decreased mobility (37) and heightened risk of malnutrition (38) in disabled older people may also contribute to the onset of sarcopenia. If the energy intake is low and cannot match the energy expenditure level, it will lead to weight loss and loss of muscle mass in the older people. In addition, as the amount of food consumed by the older people decreases, it may lead to difficulties in meeting nutritional needs, especially micronutrients, which will also increase the risk of sarcopenia in the older people (39). Secondly, aging will leads to heightened inflammation levels, which directly impacts the metabolism of muscle tissue and bone (40), ultimately causing declining physical function or disability. Elevated inflammation levels may play a role in the bidirectional correlation between sarcopenia and disability in the older people. One study has indicated (41) that increased levels of superoxide dismutase (SOD), the main antioxidant enzyme, reduce the risk of disability in older individuals. Moreover, higher levels of oxidative stress are associated with an increased risk of sarcopenia, indicating that oxidative stress levels may influence the relationship between sarcopenia and disability (42). Finally, it is important to note that older individuals with chronic diseases, such as diabetes (43) and COPD (44), are at an increased risk of developing sarcopenia. Similarly, diabetes (45) and COPD (46) can elevate the risk of disability.
In the subgroup analyses, we found a higher risk of subsequent sarcopenia in disabled persons aged < 80 years, as well as a higher prevalence of disability in individuals aged < 80 years with sarcopenia and severe sarcopenia. This could be attributed to the higher occurrence of malnutrition, reduced physical activity, and decreased physical function in older individuals aged ≥80 years, thereby weakening the relationship between the two conditions. Consequently, in the prevention of sarcopenia and disability, greater attention should be directed toward disabled or sarcopenia patients < 80 years of age, and all older people ≥80 years of age. Furthermore, in a subgroup analysis by sex, women with possible sarcopenia are more susceptible to disability than men. This may be due to women having less time for physical activity (47) and poorer health status (48) compared to men, and the allocation of social and family roles that negatively affects their access to healthcare and health protection based on traditional Chinese cultural beliefs. Additionally, previous studies have also indicated that older women are more severely disabled than men (49, 50), which could be related to the above reasons. Taken together, our study results advocate for the consideration of sex and age effects when formulating intervention strategies for sarcopenia or disability.
The study used a nationally representative cohort survey to reflect the general health status of Chinese older adults, it has large sample size and a long follow-up period. Second, it may be the first study to examine the bidirectional relationship between disability and sarcopenia using a single cohort. In addition, this study adjusted for confounding variables including gender, age, education level, and other baseline characteristics. However, we should also note the limitations of this study. First, some disease-related data were self-reported, and these diseases may generate measurement errors. In addition, there may be other unmeasured confounders influencing the association between disability and sarcopenia, but it is difficult to avoid this issue in most observational studies. Finally, the follow-up interval in this study was 4 years, and future studies need to conduct longer follow-ups to analyze whether the bidirectional association between disability and sarcopenia can be sustained over a longer period of time.
Conclusions
In conclusion, we found a bidirectional relation between disability and sarcopenia. Disability can influence subsequent sarcopenia, and sarcopenia can also predict the incidence of subsequent disability. Screening and timely management of sarcopenia should be enhanced to prevent disability in older people. Furthermore, when assessing the relationship between disability and sarcopenia, we should be mindful of the impact of gender and age to help clinical staff develop more targeted and applicable interventions to promote healthy aging.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Peking University Biomedical Ethics Review Committee (IRB00001052-11015). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
LL: Writing – review & editing, Writing – original draft, Conceptualization. YZ: Writing – review & editing, Writing – original draft, Validation. YS: Methodology, Software, Writing – original draft, Writing – review & editing. LW: Writing – original draft, Methodology. LM: Writing – review & editing, Software. TZ: Writing – review & editing, Investigation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the 2023 Henan Province Social Science Joint Committee Research Topic (Grant No. SKL-2023-569).
Acknowledgments
We are grateful to the CHARLS research team and every respondent.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1309673/full#supplementary-material
References
1. Cao L, Morley JE. Sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (ICD-10-CM) code. J Am Med Dir Assoc. (2016) 17:675–7. doi: 10.1016/j.jamda.2016.06.001
2. Morley JE. Frailty and sarcopenia in elderly. Wien Klin Wochenschr. (2016) 128:439–45. doi: 10.1007/s00508-016-1087-5
3. Kitamura A, Seino S, Abe T, Nofuji Y, Yokoyama Y, Amano H, et al. Sarcopenia: prevalence, associated factors, and the risk of mortality and disability in Japanese older adults. J Cachexia Sarcopenia Muscle. (2021) 12:30–8. doi: 10.1002/jcsm.12651
4. Wu X, Li X, Xu M, Zhang Z, He L, Li Y. Sarcopenia prevalence and associated factors among older Chinese population: findings from the China Health and Retirement Longitudinal Study. PLoS ONE. (2021) 16:e0247617. doi: 10.1371/journal.pone.0247617
5. Chagas CS, Ohara DG, Matos AP, Oliveira MSR. Association between sarcopenia and health-related quality of life in community-dwelling older adults. Acta Paulista De Enfermagem. (2021) 34:eAPE002125. doi: 10.37689/acta-ape/2021AO002125
6. Zhang X, Huang P, Dou Q, Wang C, Zhang W, Yang Y, et al. Falls among older adults with sarcopenia dwelling in nursing home or community: a meta-analysis. Clin Nutr. (2020) 39:33–9. doi: 10.1016/j.clnu.2019.01.002
7. Xu W, Chen T, Cai Y, Hu Y, Fan L, Wu C. Sarcopenia in community-dwelling oldest old is associated with disability and poor physical function. J Nutr Health Aging. (2020) 24:339–45. doi: 10.1007/s12603-020-1325-4
8. Xu J, Wan CS, Ktoris K, Reijnierse EM, Maier AB. Sarcopenia is associated with mortality in adults: a systematic review and meta-analysis. Gerontology. (2022) 68:361–76. doi: 10.1159/000517099
9. Brown JC, Harhay MO, Harhay MN. Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J Cachexia Sarcopenia Muscle. (2016) 7:290–8. doi: 10.1002/jcsm.12073
10. Bai A, Xu W, Sun J, Liu J, Deng X, Wu L, et al. Associations of sarcopenia and its defining components with cognitive function in community-dwelling oldest old. BMC Geriatr. (2021) 21:292. doi: 10.1186/s12877-021-02190-1
11. Peng TC, Chen WL, Wu LW, Chang YW, Kao TWet al. Sarcopenia and cognitive impairment: a systematic review and meta-analysis. Clin Nutr. (2020) 39:2695–701. doi: 10.1016/j.clnu.2019.12.014
12. Chen X, Guo J, Han P, Fu L, Jia L, Yu H, et al. Twelve-month incidence of depressive symptoms in suburb-dwelling Chinese older adults: role of sarcopenia. J Am Med Dir Assoc. (2019) 20:64–9. doi: 10.1016/j.jamda.2018.07.017
13. Kirk B, Phu S, Brennan-Olsen SL, Bani Hassan E, Duque G. Associations between osteoporosis, the severity of sarcopenia and fragility fractures in community-dwelling older adults. Eur Geriatr Med. (2020) 11:443–50. doi: 10.1007/s41999-020-00301-6
14. Chen YY, Chen WL, Peng TC, Liaw FY, Chao YP, Kao TW. Relationship between sarcopenia and cardiovascular disease risk among Taiwanese older adults. Public Health Nutr. (2022) 25:1–21. doi: 10.1017/S1368980022000684
15. Cao L, Zhou Y, Liu H, Shi M, Wei Y, Xia Y. Bidirectional longitudinal study of frailty and depressive symptoms among older Chinese adults. Front Aging Neurosci. (2022) 14:791971. doi: 10.3389/fnagi.2022.791971
16. Luo Y, Su B, Zheng X. Trend sand challenges for population and health during population aging-China,2015- 2050. China CDC Wkly. (2021) 28:593–8. doi: 10.46234/ccdcw2021.158
17. Chi W-C, Chang K-H, Escorpizo R, Yen C-F, Liao H-F, Chang F-H, et al. Measuring disability and its predicting factors in a large database in Taiwan using the World Health Organization Disability Assessment Schedule 20. Int J Environ Res Public Health. (2014) 11:12148–61. doi: 10.3390/ijerph111212148
18. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
19. Shen Y, Zhang Y, Xiong S, Zhu X, Ke C. High-sensitivity C-reactive protein and cystatin C independently and jointly predict all-cause mortality among the middle-aged and elderly Chinese population. Clin Biochem. (2019) 65:7–14. doi: 10.1016/j.clinbiochem.2018.12.012
20. Chen L-K, Woo J, Assantachai P, Auyeung T-W, Chou M-Y, Iijima K, et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. (2020) 21:300–7.e2. doi: 10.1016/j.jamda.2019.12.012
21. Wen X, Wang M, Jiang CM, Zhang YM. Anthropometric equation for estimation of appendicular skeletal muscle mass in Chinese adults. Asia Pac J Clin Nutr. (2011) 20:551–6. doi: 10.6133/APJCN.2011.20.4.08
22. Yang M, Hu X, Wang H, Zhang L, Hao Q, Dong B. Sarcopenia predicts readmission and mortality in elderly patients in acute care wards: a prospective study. J Cachexia Sarcopenia Muscle. (2017) 8:251–8. doi: 10.1002/jcsm.12163
23. Alexandre Td, Duarte YAd, Santos JLF, Wong R, Lebrão ML. Sarcopenia according to the European Working Group on Sarcopenia in Older People (EWGSOP) vs. dynapenia as a risk factor for mortality in the elderly. J Nutr Health Aging. (2014) 18:751–6. doi: 10.1007/s12603-014-0540-2
24. Delmonico MJ, Harris TB, Lee J-S, Visser M, Nevitt M, Kritchevsky SB, et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc. (2007) 55:769–74. doi: 10.1111/j.1532-5415.2007.01140.x
25. Jin X, He J, Liang Y, Sun X, Yan S, Wu Y, et al. Associations between household solid fuel use and activities of daily living trajectories: a nationwide longitudinal study of middle and older adults in China. Environ Int. (2022) 170:107605. doi: 10.1016/j.envint.2022.107605
26. Qiao Y, Liu S, Li G, Lu Y, Wu Y, Shen Y, et al. Longitudinal follow-up studies on the bidirectional association between ADL/IADL disability and multimorbidity: results from two national sample cohorts of middle-aged and elderly adults. Gerontology. (2021) 67:563–71. doi: 10.1159/000513930
27. Yuan M, Qin F, Zhou Z, Fang Y. Gender-specific effects of adverse childhood experiences on incidence of activities of daily life disability in middle-age and elderly Chinese population. Child Abuse Negl. (2021) 117:105079. doi: 10.1016/j.chiabu.2021.105079
28. Phillips A, Strobl R, Vogt S, Ladwig K-H, Thorand B, Grill E. Sarcopenia is associated with disability status-results from the KORA—age study. Osteoporos Int. (2017) 28:2069–79. doi: 10.1007/s00198-017-4027-y
29. Mayhew AJ, Sohel N, Beauchamp MK, Phillips S, Raina P. Sarcopenia definition and outcomes consortium 2020 definition: association and discriminatory accuracy of sarcopenia with disability in the Canadian Longitudinal Study on aging. J Gerontol A Biol Sci Med Sci. (2023) 78:1597–603. doi: 10.1093/gerona/glad131
30. Shiozu H, Higashijima M, Koga T. Association of sarcopenia with swallowing problems, related to nutrition and activities of daily living of elderly individuals. J Phys Ther Sci. (2015) 27:393–6. doi: 10.1589/jpts.27.393
31. Baumgartner RN, Wayne SJ, Waters DL, Janssen I, Gallagher D, Morley JE. Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly. Obes Res. (2004) 12:1995–2004. doi: 10.1038/oby.2004.250
32. Silva R, Pizato N, da Mata F, Figueiredo A, Ito M, Pereira MG. Mediterranean diet and musculoskeletal-functional outcomes in community-dwelling older people: a systematic review and meta-analysis. J Nutr Health Aging. (2018) 22:655–63. doi: 10.1007/s12603-017-0993-1
33. Chiba I, Lee S, Bae S, Makino K, Katayama O, Harada K, et al. Association of daily physical activity with disability in community-dwelling older adults with/without chronic kidney disease. J Nutr Health Aging. (2022) 26:521–8. doi: 10.1007/s12603-022-1790-z
34. Li P-S, Hsieh C-J, Shih Y-L, Lin Y-T, Liu C-Y. The effect of research on life satisfaction in middle-aged and older adults: physical disability and physical activity as a parallel and serial mediation analysis. BMC Geriatr. (2023) 23:176. doi: 10.1186/s12877-023-03873-7
35. Alfonso-Rosa RM, Álvarez-Barbosa F, Raimundo AM, Ferreira S, Cruz BDP, Pozo-Cruz JD. Can physical activity make up for the self-care disability effects of too much sitting? A moderation analysis in octogenarians residing in living care facilities. J Geriatr Phys Ther. (2022) 45:E155–60. doi: 10.1519/JPT.0000000000000338
36. Maruya K, Asakawa Y, Ishibashi H, Fujita H, Arai T, Yamaguchi H. Effect of a simple and adherent home exercise program on the physical function of community dwelling adults sixty years of age and older with pre-sarcopenia or sarcopenia. J Phys Ther Sci. (2016) 28:3183–8. doi: 10.1589/jpts.28.3183
37. Pan C, Kelifa MO, Liang J, Wang P. Joint trajectories of disability and related factors among older adults in China. Public Health. (2021) 199:96–102. doi: 10.1016/j.puhe.2021.08.018
38. Li X, Cao X, Ying Z, Zhang J, Sun X, Hoogendijk EO, et al. Associations of serum albumin with disability in activities of daily living, mobility and objective physical functioning regardless of vitamin D: cross-sectional findings from the chinese longitudinal healthy longevity survey. Front Nutr. (2022) 9:809499. doi: 10.3389/fnut.2022.809499
39. Robinson S, Cooper C, Aihie Sayer A. Nutrition and sarcopenia: a review of the evidence and implications for preventive strategies. J Aging Res. (2012) 2012:510801. doi: 10.1155/2012/510801
40. Pan L, Xie W, Fu X, Lu W, Jin H, Lai J, et al. Inflammation and sarcopenia: a focus on circulating inflammatory cytokines. Exp Gerontol. (2021) 154:111544. doi: 10.1016/j.exger.2021.111544
41. Li X, Cao X, Ying Z, Yang G, Hoogendijk EO, Liu Z. Plasma superoxide dismutase activity in relation to disability in activities of daily living and objective physical functioning among Chinese older adults. Maturitas. (2022) 161:12–7. doi: 10.1016/j.maturitas.2022.01.018
42. Bernabeu-Wittel M, Gómez-Díaz R, González-Molina Á, Vidal-Serrano S, Díez-Manglano J, Salgado F, et al. Oxidative stress, telomere shortening, and apoptosis associated to sarcopenia and frailty in patients with multimorbidity. J Clin Med. (2020) 9:2669. doi: 10.3390/jcm9082669
43. Kang S, Oh TJ, Cho BL, Park YS, Roh E, Kim HJ, et al. Sex differences in sarcopenia and frailty among community-dwelling Korean older adults with diabetes: the Korean Frailty and Aging Cohort Study. J Diabetes Investig. (2021) 12:155–64. doi: 10.1111/jdi.13348
44. Chen L-K, Lee W-J, Peng L-N, Liu L-K, Arai H, Akishita M, et al. Recent advances in sarcopenia research in Asia: 2016 update from the Asian working group for sarcopenia. J Am Med Dir Assoc. (2016) 17:767. doi: 10.1016/j.jamda.2016.05.016
45. Tomic D, Shaw JE, Magliano DJ. The burden and risks of emerging complications of diabetes mellitus. Nat Rev Endocrinol. (2022) 18:525–39. doi: 10.1038/s41574-022-00690-7
46. Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. (2022) 10:447–58. doi: 10.1016/S2213-2600(21)00511-7
47. Matud MP, Díaz A. Gender, exercise, and health: a life-course cross-sectional study. Nurs Health Sci. (2020) 22:812–21. doi: 10.1111/nhs.12736
48. Raczkiewicz D, Bejga P, Owoc J, Witczak M, Bojar I. Gender gap in health condition and quality of life at advanced age. Ann Agric Environ Med. (2020) 27:636–43. doi: 10.26444/aaem/125753
49. Kaneda T, Zimmer Z, Fang X, Tang Z. Gender differences in functional health and mortality among the Chinese elderly: testing an exposure versus vulnerability hypothesis. Res Aging. (2009) 31:361–88. doi: 10.1177/0164027508330725
Keywords: sarcopenia, disability, bidirectional relationship, CHARLS, older people
Citation: Liu L, Zhang Y, Shi Y, Wu L, Meng L and Zhao T (2024) The bidirectional relationship between sarcopenia and disability in China: a longitudinal study from CHARLS. Front. Public Health 12:1309673. doi: 10.3389/fpubh.2024.1309673
Received: 08 October 2023; Accepted: 10 April 2024;
Published: 07 May 2024.
Edited by:
Xiaolei Liu, Sichuan University, ChinaReviewed by:
Silvia Giovannini, Catholic University of the Sacred Heart, Rome, ItalyDulaney Wilson, Medical University of South Carolina, United States
Copyright © 2024 Liu, Zhang, Shi, Wu, Meng and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Zhang, emhhbmd5YW5teUAxMjYuY29t; Yan Shi, c2hpeWFuQHp6dS5lZHUuY24=
 Li Liu
Li Liu Yan Zhang*
Yan Zhang*