- Department of Cardiovascular Medicine, Ningbo Medical Center Lihuili Hospital, Ningbo, China
Objective: Hypertension is the most challenging public health problem worldwide and seriously affects human health. To date, there are no epidemiological studies on the prevalence of and risk factors for hypertension among older people in mainland China.
Methods: We conducted a meta-analysis of the prevalence and risk factors of hypertension among the older population in mainland China. We searched Chinese and English databases for Chinese and English literature on hypertension epidemiology published between 2000 and 2022, and hypertension data among the older population were extracted from the included literature. A meta-analysis was performed using a random-effects model (I2 > 50%) with 95% confidence intervals for the forest plots. Data were processed using RevMan 5.3. Forty-nine publications (with data from 84,429 samples) met the evaluation criteria and were included in this study.
Results: We found that the total prevalence of hypertension was 47%. The total prevalence rate of the older population in China from 2000 to 2010 was 50%, and the prevalence rate from 2011 to 2021 was 45%, with no significant differences. The total prevalence in Central China was the highest (59%). There was no significant correlation between the prevalence rate of the older population, sex, and urban or rural areas.
Conclusion: Hypertension is common among the older population in China, and its control rate is low. Therefore, effective prevention and treatment measures, as well as education, should be formulated to improve the diagnosis and treatment of hypertension in the older population.
1 Introduction
Cardiovascular diseases are the number one disease threatening human life and the leading cause of global medical burden (1). Hypertension is considered a major risk factor for cardiovascular disease-related death and is the most challenging public health problem worldwide (2). Hypertension is a chronic disease with elevated systemic arterial blood pressure as its main clinical feature. Due to fewer early symptoms, it is difficult to detect, and it is easy to miss the best treatment opportunity. Once long-term unsatisfactory control of blood pressure is achieved, serious complications such as heart disease, stroke, kidney damage, and visual impairment may occur, eventually increasing the morbidity and mortality of diseases related to blood (3). In China, deaths due to hypertension account for a large proportion of all cardiovascular disease-related deaths. Statistics show that 1.27 million of the 2.33 million deaths from cardiovascular disease are due to hypertension (4). Since 1958, China has conducted four large-scale national surveys on the prevalence of hypertension in 1958, 1979, 1980, 1991, and 2000, with prevalence rates of 5.11, 7.7, 11, and 24.27%, respectively (5). However, with the rapid development of China’s economy and the acceleration of urbanization, the prevalence of hypertension continues to rise sharply. According to statistics, 325 million Chinese adults had hypertension in 2010 (approximately 29.6% of the adult population) (6).
Hypertension is a common chronic disease in clinical practice and a risk factor for cardiovascular and cerebrovascular diseases (2). The blood pressure of normal people can fluctuate with changes in the internal and external environment, with the increase of age, the rise of systolic blood pressure is more obvious, and the diastolic blood pressure shows a downward trend, so the pulse pressure gradually increases (3). The analysis of the epidemiology and risk factors of hypertension is the main basis for the treatment of hypertension. Controlling the blood pressure within a scientific and reasonable range according to the different conditions of patients can reduce the clinical symptoms of patients and prevent the occurrence of complications.
To date, most epidemiological studies on hypertension in China focus on the prevalence rate and related risk factors in the adult population and pay little attention to the prevalence and epidemiology of the older population. Older adults have a high incidence of cardiovascular and cerebrovascular diseases, and the aggravation of China’s aging population will inevitably make us invest more energy into the health problems of the older population. Reliable information on hypertension trends and prevalence is critical for developing effective prevention and control strategies. However, individual studies on the prevalence of hypertension in older adults nationwide are scarce. Although some studies have reported the prevalence of hypertension in older populations, they were limited to individual regions and years. Therefore, it is necessary to perform a comprehensive assessment of the prevalence of hypertension among the older population in China.
China has a vast territory and is divided into seven administrative regions. Affected by the natural environment, there are great differences in the production and life style, cultural customs and other aspects of people in different regions, which has an important impact on the distribution of diseases. Studies have shown that the prevalence of hypertension is higher in northern China than in southern China (5). The prevalence is higher in large and medium-sized cities than in smaller cities (6). Rural residents have a lower prevalence than urban residents, but the prevalence is growing faster in rural areas than in cities, and the difference is changing (7). The regional differences of hypertension prevalence in China may be affected by regional economic development level, natural environment, special regional climate and other factors. However, there are still few reports on the regional differences in the prevalence of hypertension and the comprehensive analysis of risk factors in the older adult/adults population in China.
This study conducted a meta-analysis of the prevalence of hypertension in the older population in China and systematically evaluated the data obtained from the collected studies to clarify the trend of hypertension prevalence in the older population in China. The study also systematically assessed risk factors (age, geographical location, sex, and urban or rural residence) in the older age groups. The aim of this study was to clarify the epidemiological characteristics of hypertension in the Chinese mainland older adult/adults population and to provide additional data for the global epidemiological study of hypertension.
2 Materials and methods
2.1 Literature search strategy
This systematic review was conducted according to the methods and recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension statement. The inclusion criteria were retrospective cohort studies in Chinese and English. We searched English language databases (PubMed, Google Scholar, Cochrane Library, and Clinical Trials) and Chinese language databases (CNKI, Cqvip, WANFANG data, and Baidu Scholar) to retrieve articles on the prevalence and epidemiology of hypertension in China that had been published between January 1, 2020, and December 31, 2022. The search method adopted a combination of subject words and free words, and the search terms included “hypertens,” “hypertension,” “epidemiology,” “incidence,” “prevalence,” “China,” “Chinese,” or variants and combinations of these keywords. Take “China” or “Chinese” as crowd qualifiers. The literature found in the term search is reviewed to determine other qualifications.
2.2 Inclusion and exclusion criteria for articles
The inclusion criteria were as follows: (1) the publications collected in this study were cross-sectional studies on the prevalence and epidemiology of hypertension published between 2000 and 2022; (2) the study samples for these publications were age-specific and included people aged >60 years; (3) the studies included in these publications were conducted on mainland Chinese populations; (4) all patients were diagnosed with hypertension. Exclusion criteria were as follows: occupational groups; ethnic minorities; pregnant women; specific sex; non-research-based publications, such as reviews, press releases, newsletters, and forums; study population size of fewer than 30 cases; and sample time, sample size, and prevalence not specified in the study.
2.3 Data extraction and quality assessment
The corresponding data from the studies that met the inclusion criteria were extracted by two reviewers. Start with a quick review of the title and abstract, excluding irrelevant studies. The remaining studies were evaluated and screened for readability. In cases of disagreement, the study was evaluated by a third reviewer until an interactive consensus was reached on the inclusion criteria. The quality of the selected publications was estimated using the Newcastle-Ottawa Scale (NOS) (7). The full score is 10 points; studies with ≥5 points can be included in the meta-analysis. Microsoft Office Excel was used to create the data extraction tables. The information extracted from the included studies included the number of patients, aged >60 years, geographical location, sex, urban and rural areas, study design, sample size, author, and year of publication.
2.4 Statistical analysis
A random-effects model was used for eligible studies. Meta-analysis was performed using Review Manager 5.3 (Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014). Forest plots were used to summarize the estimates with 95% confidence intervals (CIs). An I2 was used to evaluate heterogeneity. If the heterogeneity test showed p ≥ 0.1 and I2 ≤ 50%, this indicates homogeneity between studies, and the fixed-effects model can be used for combined analysis. p < 0.1 and I2 > 50% indicated heterogeneity between studies; sensitivity analysis or subgroup analysis was then used to determine the source of heterogeneity. If heterogeneity remained large, a random-effects model or descriptive analysis was used. Statistical significance was set at p < 0.05, and 95% CIs were reported.
3 Results
3.1 Description of studies
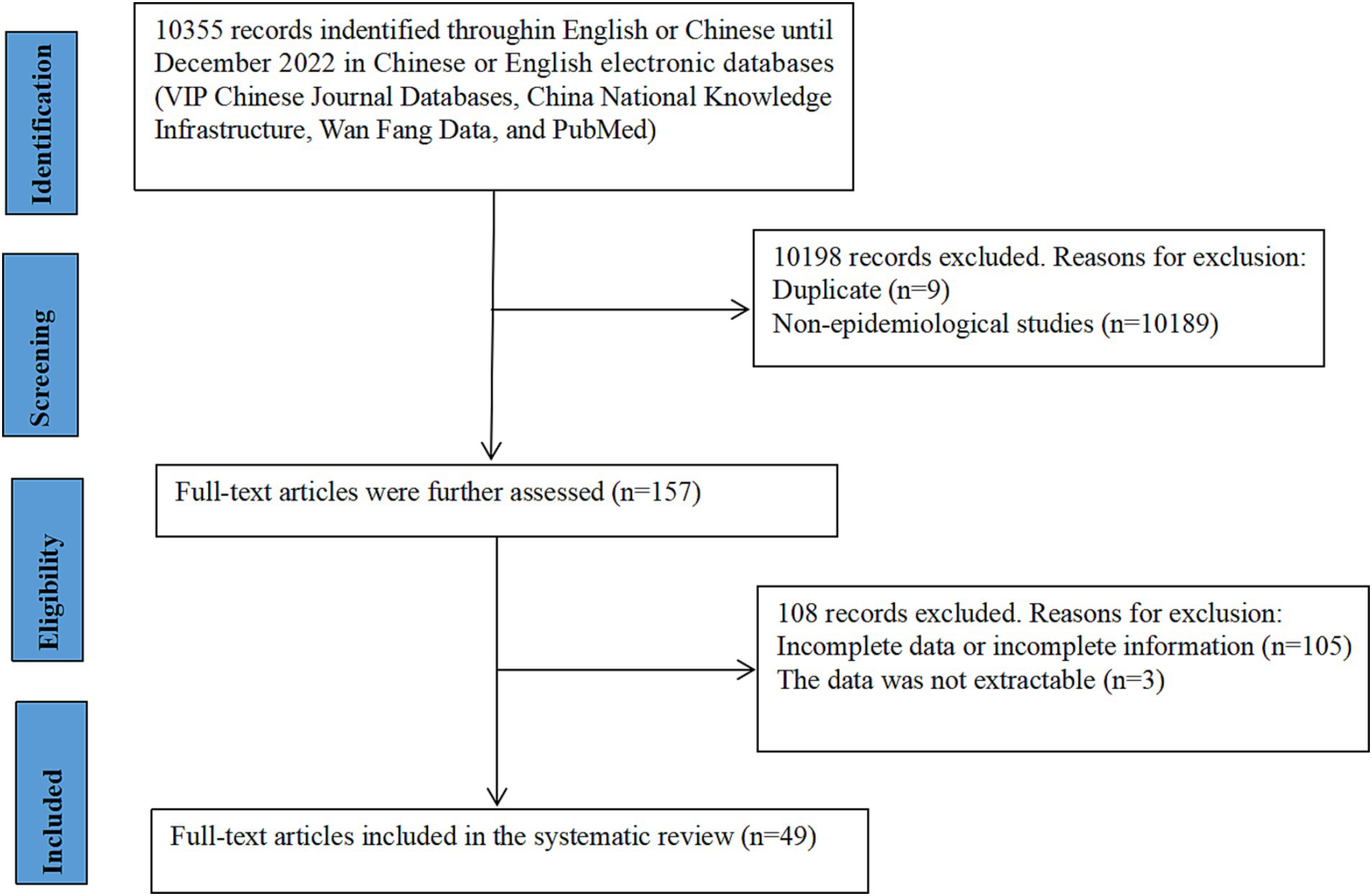
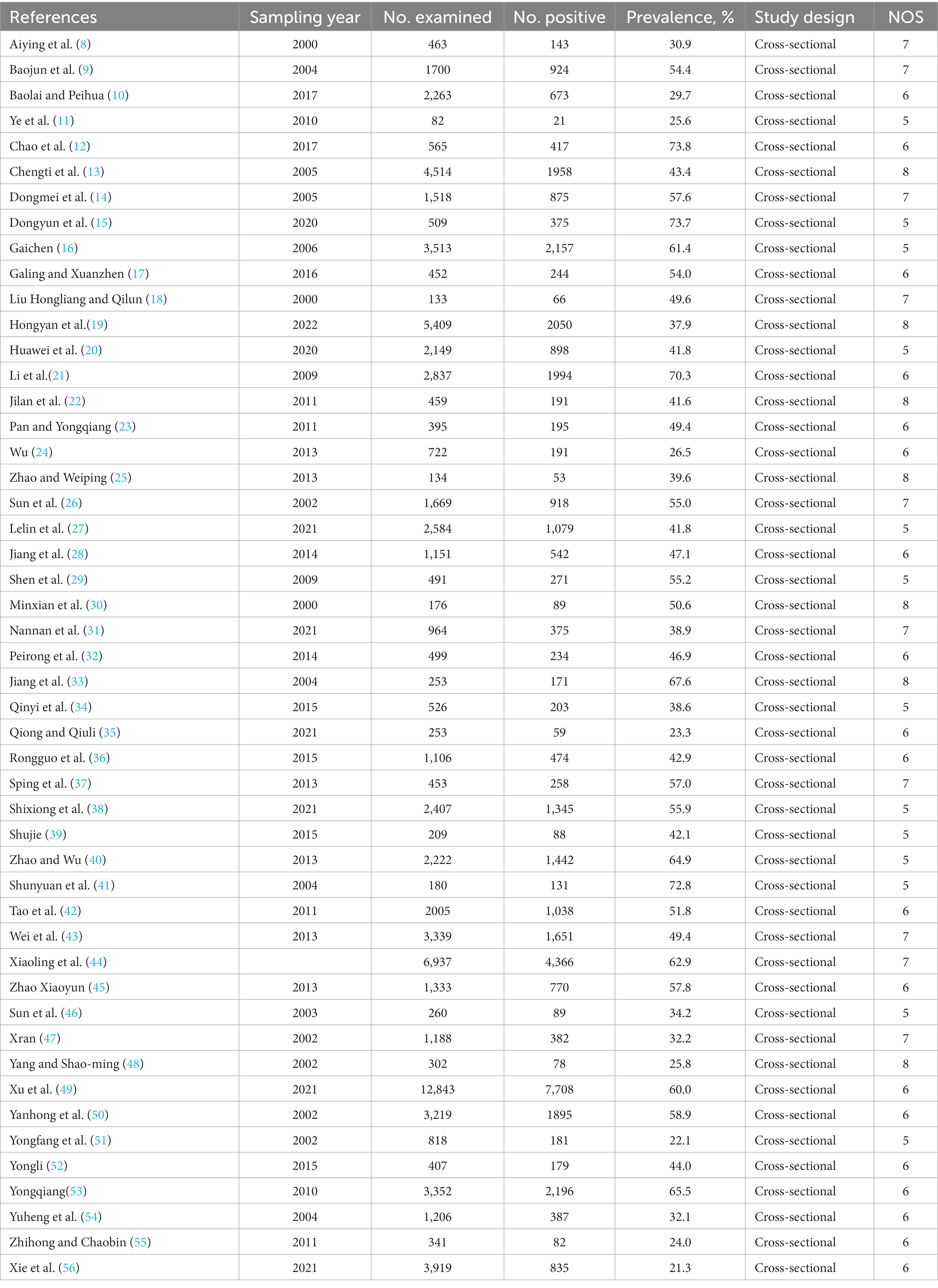
A total of 10,335 Chinese and English articles were identified based on the database search strategies. After scanning the titles and abstracts, 157 articles were considered for full-text evaluation. After excluding 108 articles with incomplete data, 49 articles were included in the meta-analysis and data extraction (Figure 1). All included studies were single cross-sectional studies conducted from 2000 to 2022, with sample sizes ranging from 82 to 12,843. The included studies were from seven administrative regions of China: 14 from East China, 11 from North China, six from South China, six from Southwest China, five from Northwest China, four from Northeast China, and three from Central China. Among the 49 studies, four described the rural–urban difference in the prevalence of older adults, nine did not classify the rural–urban difference in the prevalence of older patients, 27 were from urban prevalence studies, and nine were from rural prevalence studies. According to our criteria, zero publications were of high quality (4–5 points), 43 were of moderate quality (2–3 points), and six were of low quality (1 point). A cross-sectional review of all articles was performed (Table 1).
3.2 Prevalence of hypertension in China
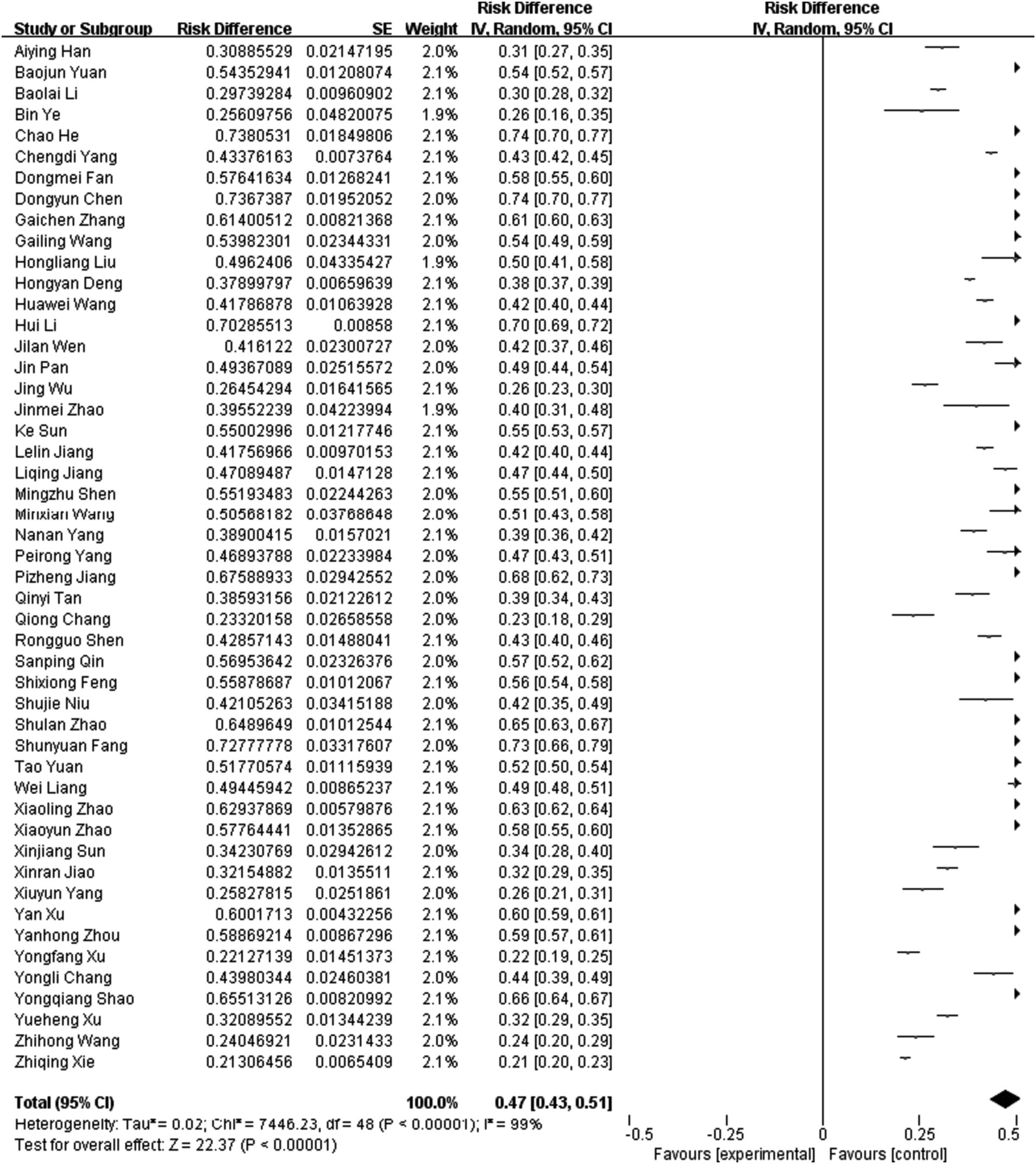
The 49 articles included in this study had a total sample size of 84,429 cases, of which 42,941 were positive. The pooled prevalence of hypertension in the older population in mainland China was 47% (95% CI, 43–51) (Figure 2). Among the 49 studies, there were 20 studies from 2000 to 2010, and the estimated prevalence was 50% (95% CI, 44–56). There were 29 studies from 2011 to 2022, and the estimated prevalence was 45% (95% CI, 39–50). The results showed that the total prevalence rate in the older population in China during 2011–2022 was slightly lower than that in 2010–2011, but the difference was not statistically significant (p > 0.05) (Table 2).
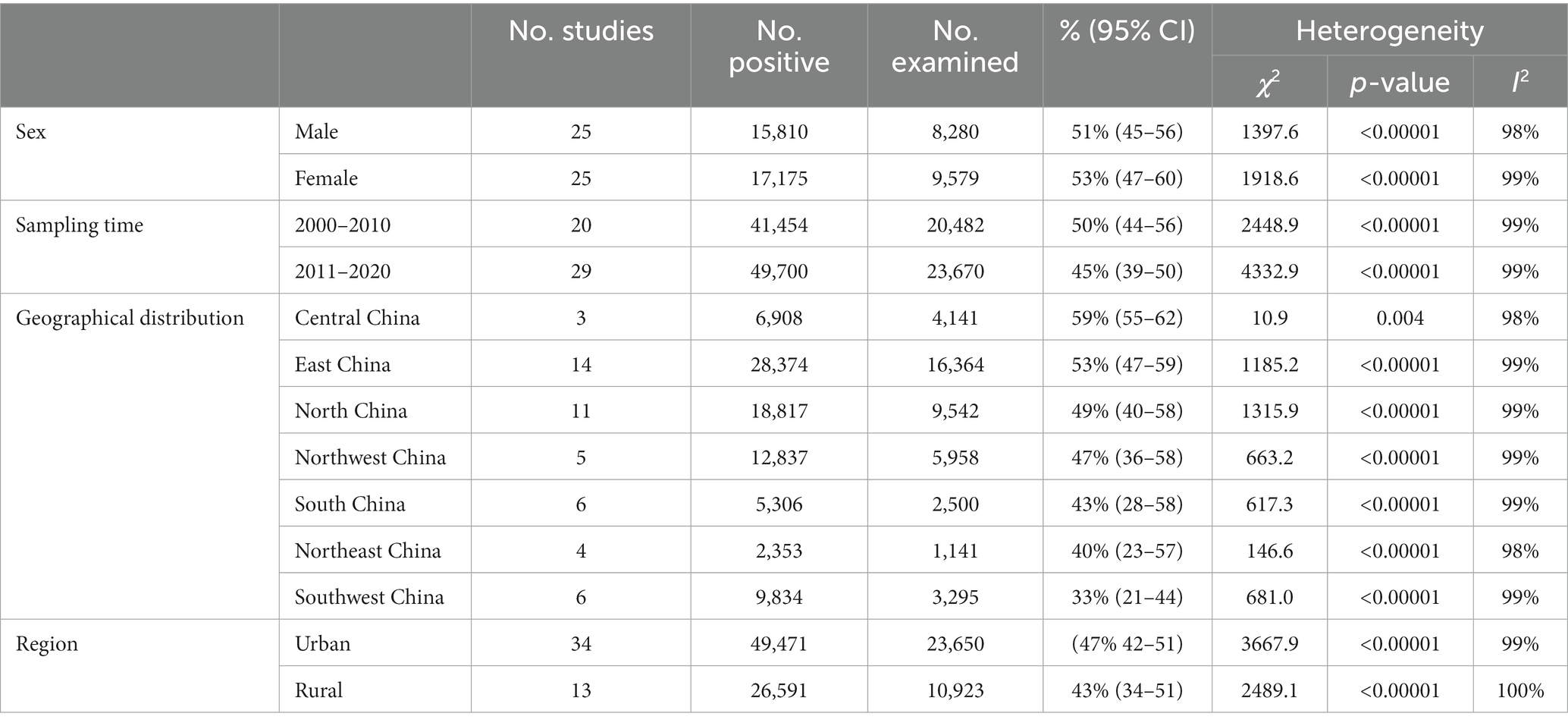
3.3 Analysis of epidemic factors of hypertension
A total of 25 included studies examined the relationship between sex and the prevalence of hypertension in the older population. The results showed that the prevalence rate in males was 51% (95% CI, 45–56) and that in females was 53% (95% CI, 47–60), with no statistical difference (p > 0.05) (Table 2). In addition, the results showed that the prevalence was 47% (95% CI, 42–51) in urban and 43% (95% CI, 34–51) in rural, with no significant difference (p > 0.05) (Table 2). Furthermore, the results of the regional distribution analysis showed that the total prevalence in Central China was the highest (59%). The prevalence rates in the other regions were 53% in East China, 49% in North China, 47% in Northwest China, 43% in South China, 40% in Northeast China, and 33% in Southwest China (Figure 3, Table 2).
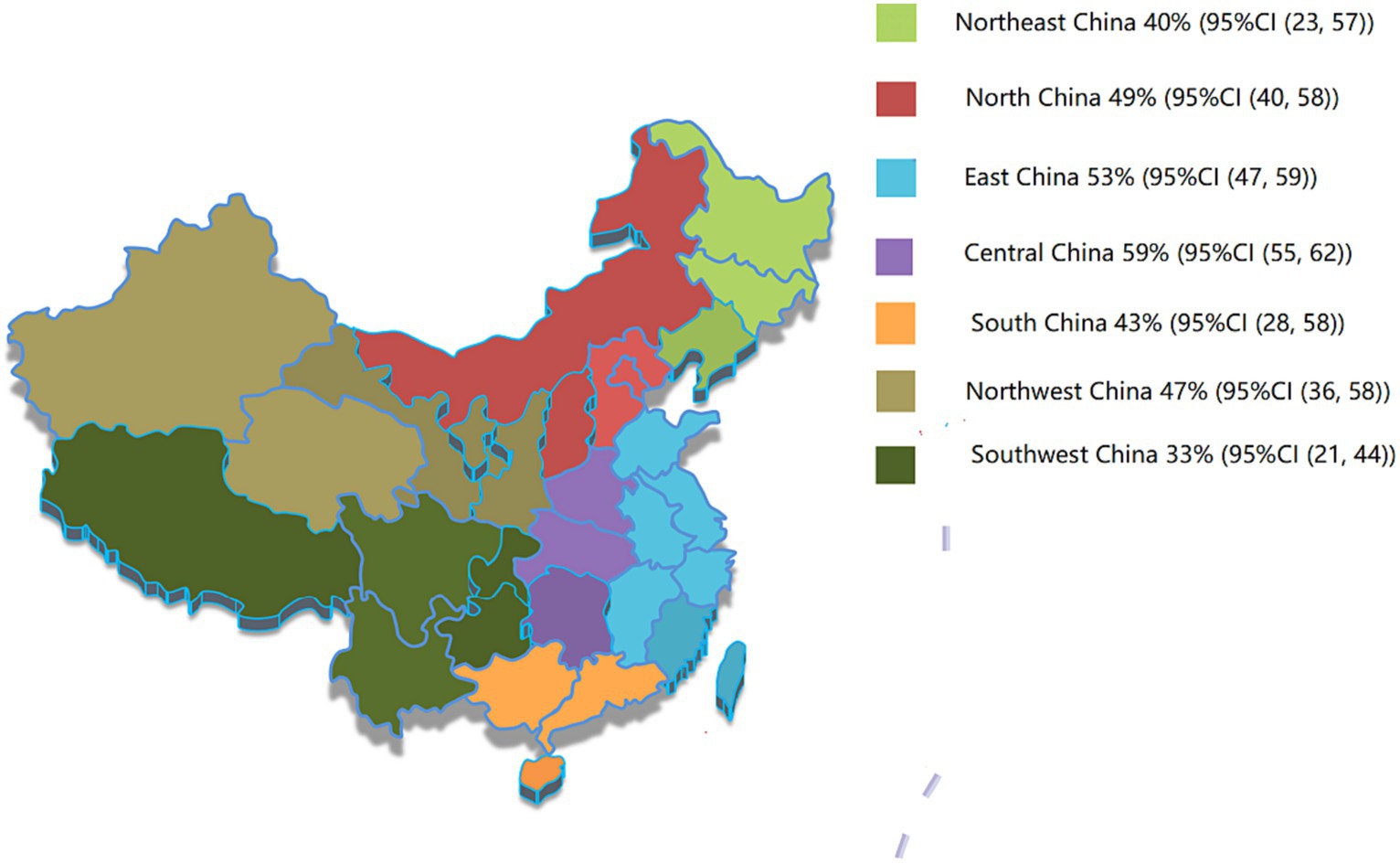
Figure 3. Prevalence of hypertension in seven administrative regions of China. Northeast China includes Liaoning, Jilin, and Heilongjiang provinces; North China includes Beijing, Tianjin, Hebei, and Shanxi provinces and Inner Mongolia; Central China includes Henan, Hubei, and Hunan provinces; East China includes Shanghai, Shandong, Jiangsu, Anhui, Jiangxi, Zhejiang, Fujian, and Taiwan provinces; South China includes Guangdong province, Guangxi province, Hainan province, Hong Kong Special Administrative Region, and Macao Special Administrative Region; Northwest China includes Shaanxi, Gansu, Qinghai, Ningxia, and Xinjiang province. The Southwest China includes Sichuan province, Guizhou province, Yunnan province, Tibet, and Chongqing.
4 Discussion
Studies have shown that the prevalence of hypertension in Chinese adults ranges from 13.6 to 27.2% (57). Furthermore, the prevalence of hypertension increases with age, with the highest prevalence in older adults compared to those of adults or young adults. This study showed that the total prevalence rate of hypertension in the older population in China was 47%, significantly higher than the reported prevalence rate in the adult population in China. These results indicate that with the development of China’s aging population, the prevention and control of hypertension in older adults is more demanding. In addition, it has been reported that in the past 20 years, there has been a high prevalence of hypertension in older adults in China (58). The comparative analysis of the prevalence between 2000 and 2010 and 2011 and 2022 in this study shows that there is no significant difference in the prevalence between the two periods and that both present a high prevalence, which proves that hypertension remains a potential threat to the older population. The older population has a high incidence of cardiovascular and cerebrovascular diseases, and hypertension results from multi-factor interactions such as poor lifestyle and psychological impact. Community health service centers must conduct various forms of health education and behavioral guidance to improve the awareness rate, control rate, and treatment compliance of patients with hypertension. A survey of 142,042 participants from countries with different income levels showed that 26,877 (46.5%) were aware of their hypertension status. However, statistics indicate a gradual decline in awareness rates from high to low-income countries. Of these, only 17% are in Brazil, and 88% are in the United States (59). Differences in awareness rates between countries may depend on a country’s education level, economic level, health status, and health awareness. The main measures of hypertension control are drug and non-drug intervention (60). Once the awareness and cure rates of hypertension are higher than the control rate, non-drug interventions need to be strengthened, especially control of smoking and alcohol abuse, regular exercise, and weight control (61). Older Chinese individuals generally have low levels of education and income. Therefore, the high prevalence of hypertension in the older population in this study suggests that there is still a long way to go before health education for hypertension can be implemented. We should strengthen health education for the older adult/adults. We should encourage the older adult/adults to have civilized and healthy living habits and behaviors. Older people should be encouraged to monitor their blood pressure regularly and to be active in physical activity. We should instruct the older adult/adults to eat a balanced diet, which should be light and vegetarian.
In epidemiological studies of hypertension, regional differences cannot be ignored (5). In this study, 49 included studies were conducted according to the statistics of seven administrative regions, and the results showed the prevalence rate in densely urbanized areas such as Central China, East China, and North China was higher than that in other regions, indicating that with the progress of economic development and urbanization, the hidden danger of hypertension in older adults will become increasingly prominent. In addition, the prevalence of hypertension in the adult population has been reported to be higher in males than in females. Possible explanations include differences in physical structure or undesirable habits, such as smoking and drinking, which are higher in males than in females (62). However, these results are based only on young adults. The results of this study did not show a statistically significant difference between the prevalence of hypertension and sex in the older population in China. Estrogen has a protective effect on the function of female cardiovascular system. However, the protective effect of estrogen gradually declines with age, which may be the reason for the increased prevalence of hypertension in older women. This suggests that sex differences in the prevalence of hypertension in the older population have been blurred, and more attention should be paid to prevention and control.
This study showed that there was no significant difference in the prevalence of hypertension in the older adult/adults between urban and rural areas, which further supports the fact that hypertension is more harmful to the older population and has a high prevalence rate between urban and rural areas. In contrast to developed countries, the gap between urban and rural areas, social and economic levels, and the way of life of Chinese people have all undergone great changes in the last decade. The urban population is dense, and the older adult/adults have less space for activities, so they lack exercise. Urbanization also brings dietary bias, with the older adult/adults consuming sugar and salt for a long time. All of which increase the risk of hypertension. In addition, due to poor health and medical conditions in rural areas, as well as insufficient awareness of the importance of grassroots health workers to prevent hypertension, some older adult/adults people in rural China have long had a bad habit of smoking. This is also one of the reasons for the high prevalence of hypertension. Studies have shown that the cure, control, and control rates of rural low-income individuals were lower. Healthcare, information, and education for low-income groups should be strengthened. It is necessary to increase investment in the improvement of rural medical and health conditions, establish relevant policies to strengthen rural construction, consolidate the economic foundation of rural residents from various aspects, better improve their living standards, fundamentally eliminate the problem of looking down on diseases due to poor economy, and strengthen the health management of older adult/adults patients with hypertension to reduce the prevalence rate.
Limitations of this study include: First, although several MeSH terms were used, it is possible that not all publications related to hypertension in the mainland Chinese population were covered in the selected database. Second, most of the included studies were published in Chinese. While these publications meet the inclusion criteria, we hope to have easy access to more English-language publications in the future.
4.1 Conclusion
The results of this study can be used as auxiliary data for hypertension prevention and control planning in older populations. To our knowledge, this is the first study to analyze the epidemiology of hypertension in the older Chinese population. The results showed that the prevalence rate of hypertension was high in the older population in China. The prevalence rate of hypertension presented regional distribution characteristics, and the differences between urban and rural areas and sex were not significant, suggesting that we need to formulate and develop hypertension prevention and control strategies and health education programs in the older population to strengthen the detection, prevention, and treatment of hypertension in the older population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Author contributions
ZW: Data curation, Methodology, Writing – original draft, Writing – review & editing. SW: Investigation, Methodology, Software, Writing – original draft. HL: Investigation, Methodology, Software, Writing – original draft. CW: Data curation, Methodology, Software, Writing – original draft. DG: Conceptualization, Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (2023KY1037).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ezzati, M, Lopez, AD, Rodgers, A, Vander Hoorn, S, and Murray, CJL. Selected major risk factors and global and regional burden of disease. Lancet. (2002) 360:1347–60. doi: 10.1016/S0140-6736(02)11403-6
2. He, J, Gu, D, Chen, J, Wu, X, Kelly, TN, and Huang, JF. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet. (2016) 374:1765–72.
3. Zhang, M, Shi, Y, Zhou, B, et al. Prevalence, awareness, treatment, and control of hypertension in China. Hypertension, (2002) 380:e071952. doi: 10.1136/bmj-2022-071952
4. Bromfield, S, and Muntner, P. Hypertension: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep. (2013) 15:134–6. doi: 10.1007/s11906-013-0340-9
5. Fang, L, Song, J, Ma, Z, Zhang, L, Jing, C, and Chen, D. Prevalence and characteristics of hypertension in mainland Chinese adults over decades: a systematic review. J Hum Hypertens. (2014) 28:649–56. doi: 10.1038/jhh.2014.5
6. Meng, XJ, Dong, GH, Wang, D, Liu, MM, Lin, Q, Tian, S, et al. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J Hypertens. (2011) 29:1303–10. doi: 10.1097/HJH.0b013e328347f79e
7. Lo, CK, Mertz, D, and Loeb, M. Newcastle-Ottawa scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. (2014) 14:45. doi: 10.1186/1471-2288-14-45
8. Aiying, H, Wu, G, and Guo, YG. Epidemiological investigation and analysis of hypertension in urban residents of Linhe City. Inner Mongol Prevent Med. (2022) 2:66–7. doi: 10.1177/20503121211024519
9. Bajun, Y, Xiaoqun, P, Zumin, S, and Yue, D. Epidemiologic study on prevalence of hypertension and related factors in Jiangsu Province. Jiangsu Prevent Med. (2004) 3:5–7. doi: 10.1136/bmjopen-2018-027215
10. Baolai, L, and Peihua, J. Epidemiological investigation and analysis of hypertension in rural adult residents in Longxi County from 2015 to 2016. Primary Health Care. (2017) 31:49–51. doi: 10.1097/MD.0000000000034402
11. Ye, B, Huang, X, and Wang, J. Epidemiological analysis of hypertension in residents of Lianhua street. Shenzhen Pract Prevent Med. (2010) 17:1882–3. doi: 10.1038/sj.jhh.1000511
12. Chao, H, Sun Xin, Z, Yan-Yan, ZY-Y, Yang Shuai-Shuai, Z, Xu-xi, LZ, Ru-Bing, B, et al. Epidemiological investigation of hypertension and its risk factors in Shunyi District, Beijing. China. Health Educ. (2017) 33:59–63.
13. Chengti, Y, Xiaoping, L, Li Xixi, Y, Jing, JW, and Chao, Y. An epidemiological survey of hypertension in Qilihe district of Lanzhou city. Chin J Cardiol. (2005) 7:658–9.
14. Dongmei, F, Hongjian, L, and Ling, H. An epidemiological survey on the prevalence of hypertension in Taixing City. Occup Health. (2005) 8:1211.
15. Dongyun, C, Xiuyou, C, and Yuting, H. Epidemiologic investigation of hypertension and its risk factors in Dongguan City. Jiangxi Med. (2019) 55:50–3.
16. Gaichen, Z . Epidemiological study on hypertension in the middle-aged and elderly population in Anyang city. Disease Surveill. (2006) 9:487–9.
17. Galing, W, and Xuanzhen, C. Epidemiologic investigation and analysis of hypertension in elderly population in urban area of Xinzhou city, Shanxi Province. J Integr Tradition Chin West Med Card Cerebrovasc Dis. (2016) 14:997–000.
18. Liu Hongliang, D, and Qilun, ZS. Epidemiologic survey of hypertension in southern Shandong Province. China Primary Health Care. (2000) 2:32.
19. Hongyan, D, Moxuan, Z, Fen, L, et al. Investigation of hypertension risk factors in Qinglongqiao community, Beijing. Cont Med Educ. (2022) 36:141–4.
20. Huawei, W, Meng Zhaohui, L, Yanan, HZ, Jun, X, and Lixing, C. The prevalence of hypertension and its related risk factors in rural residents of Dai nationality in Xishuangbanna, Yunnan Province. J Kunming Med Univ. (2019) 41:42–7. doi: 10.21203/rs.2.13850/v1
21. Li, H, Meng, Q, Sun, X, Salter, A, Briggs, NE, and Hiller, JE. Prevalence, awareness, treatment, and control of hypertension in rural China: results from Shandong Province. J Hypertens. (2010) 28:432–8. doi: 10.1097/HJH.0b013e328334b39e
22. Jilan, W, Rongshan, L, Yuanyuan, S, and Suping, W. An epidemiological survey of hypertension among community residents in Youyu County Shanxi Province. Chin J Public Health. (2011) 27:734–6.
23. Jin, P, and Yongqiang, S. Epidemiological investigation of hypertension in Wenzhou city. Mod Pract Med. (2011) 23:1005–7.
24. Wu, J . Epidemiological survey of hypertension in community residents of Shizhong District, Zaozhuang City from 2011 to 2012. Prevent Med Forum. (2013) 19:848–9.
25. Zhao, JM, and Weiping, Y. Epidemiologic investigation of hypertension and diabetes mellitus in adults in Erdao district of Changchun City. Chin J Health Eng. (2013) 12:253–254+256.
26. Ke, S, Dan, L, Xiu-fen, Z, Limei, Z, Wei, P, Qin, W, et al. Epidemiological survey of hypertension prevalence in Dalian City. China Chron Dis Prevent Contr. (2002) 4:186–7.
27. Lelin, J, Fanhao, Y, Sisi, H, et al. Investigation on hypertension prevalence and knowledge level of community residents in Wenzhou area. ECG Circ. (2011) 40:179–82.
28. Jiang, LQ, Liang, YM, Liu, YS, and Meng, JJ. Epidemiologic investigation and risk factors analysis of hypertension in rural areas of Cangzhou. Chin J Gerontol. (2014) 34:1903–4.
29. Shen, MJ, Wang Dongyue, W, and Ye, WW. Epidemiologic analysis of hypertension prevalence rate and related factors in Changshu City Jiangsu. Prev Med. (2009) 20:30–2.
30. Minxian, W, Xiaoyan, H, Bin, H, Linan, L, Yinshan, L, Renyu, L, et al. Epidemiological investigation and analysis of hypertension in enterprise community population in Anyang city. Disease Surveillance. (2000) 9:346–8.
31. Nannan, Y, Zhiqin, M, and Xiaoyan, C. Prevalence and epidemiology of hypertension in a community in Longgang District, Shenzhen in 2019. Chin Med Innov. (2019) 18:122–6. doi: 10.1136/bmjopen-2022-061606
32. Peirong, Y, Rui, L, Deng Feng, Q, Meng, WH, and Biao, Y. Epidemiological investigation and analysis of hypertension among residents in Baoji City. Med Animal Control. (2014) 30:379–82. doi: 10.1038/sj.jhh.1000979
33. Jiang, PZ, Jiang, YM, and Hu, YG. Epidemiologic survey of hypertension in Quzhou city in 2003. Prevent Treat Cardiovasc Cerebrovasc Dis. (2004) 6:50–1.
34. Qinyi, T, Weihong, M, Qi, L, Lingxiang, P, Jiaji, T, Xiaoling, Y, et al. Epidemiological investigation and analysis of elderly hypertension in Lidong community. Intern Med. (2015) 10:363–364+362. doi: 10.2174/1871525713666150310112350
35. Qiong, C, and Qiuli, H. Investigation on hypertension occurrence, epidemiological characteristics and health management needs of middle-aged and elderly residents in Chongqing. J Pract Cardio-cerebral Pulmon Vasc Dis. (2021) 29:21–8.
36. Rongguo, S, Xia Wei, L, Chongbai, LX, and Pingli, ZY. Epidemiological survey of hypertension among the elderly aged over 65 years in Moling community of Jiangning City, Nanjing. J Liaoning Med Coll. (2015) 36:95–7.
37. Sping, Q, Yangjie, W, Xia, H, Lian-Ying, D, Jin-xia, G, Chun-feng, L, et al. An epidemiological survey of hypertension in Hohhot residents. J CJ. (2013) 14:665–7.
38. Shixiong, F, Zewen, Z, Yingchun, L, Qiuping, W, Min, H, Xiaoyun, Z, et al. Study on the prevalence and influencing factors of hypertension in 35 ~ 74 years old Zhuang people in Guangxi. J Guangxi Med Univ. (2005) 38:591–8.
39. Shujie, N . Epidemiologic investigation and risk factors analysis of hypertension in Baicheng City residents. J Integr Chin West Med Cardiovasc Dis. (2015) 3:185–6.
40. Zhao, SL, and Wu, YJ. Epidemiology of hypertension in middle-aged and elderly people in Honggu area of Gansu Province. Chin J Gerontol. (2013) 33:3954–5. doi: 10.1155/2019/4634823
41. Shunyuan, F, Xiaoxia, Z, Dafeng, J, Qing-min, L, Hui-ren, J, Shen Gen-Hui, F, et al. An epidemiological survey of hypertension in Hangzhou in 2003. Prevent Treat Cardiovasc Cerebrovasc Dis. (2004) 6:40–2.
42. Tao, Y, Meng, X, Xiaobo, H, Wei, Z, Ya, L, Yanjing, Y, et al. Epidemiologic survey of hypertension in elderly population in Chengdu area. Sichuan Med. (2011) 32:460–3.
43. Wei, L, Xiaowei, Z, Wang Qiongying, Y, Heng, ZT, Yang, Z, et al. An epidemiological survey of hypertension in middle-aged and elderly residents in Gansu Province. Chin J Gerontol. (2017) 37:4103–5.
44. Xiaoling, Z, Lina, M, Zhe, T, Shaochen, G, Fei, S, Liu Hongjun, W, et al. Epidemiologic changes of hypertension in the elderly in Beijing. Chin J Prevent Med. (2010) 11:566–8. doi: 10.1371/journal.pone.0135480
45. Zhao Xiaoyun, L, Yonggang, ZH, Junming, W, and Guangyao, S. Epidemiologic analysis of hypertension in 51239 health checkup population in Hebei province. Chin J Gerontol. (2013) 33:4818–20.
46. Sun, XJ, Yue Aiping, Y, and Shuhua,. Epidemiological investigation and analysis of hypertension in community residents. Occup Health. (2003) 11:81–2. (in Chinese)
47. Xran, J . An epidemiological survey of hypertension in Miyun district of Beijing. Chin J Public Health. (2002) 9:12–3.
48. Yang, X-Y, and Shao-ming, Z. Epidemiologic survey of hypertension in Jinniu District of Chengdu. J Sichuan Provin Health Manag Insti. (2002) 4:253–4.
49. Xu, Y, Zhu, P, Liu, J, Chen, YY, Xu, LP, Na, CX, et al. Epidemiologic characteristics of hypertension in 94591 residents of Jiangxi Province. China Health Statis. (2019) 38:222–5.
50. Yanhong, Z, Yang Fengdong, X, Hongwei, LY, Yiqun, X, and Le, Z. An epidemiological study of hypertension in the middle-aged and elderly population in Changsha city. Chin J Hyperten. (2002) 3:85–7. doi: 10.3784/j.issn.1003-9961.2006.9.487
51. Yongfang, X, Yuqiao, Q, Linfang, G, Naying, C, Xiaoyu, M, and Guimin, L. An epidemiological survey of hypertension in residents of Nanning city. J Guangxi Med Univ. (2002) 6:912–3.
52. Yongli, C . Epidemiological investigation on the prevalence of hypertension and its influencing factors in urban and rural residents in Xingtai City. Hebei Prov Pract Cardio-Cerebropulm Vasc Dis. (2015) 23:37–40.
53. Yongqiang, S, Jian, W, Yi, C, Jianyong, Z, and Xiaowei, L. Epidemiological investigation on the status quo and risk factors of hypertension in 10 communities in Wenzhou. Chinese Journal of Preventive Medicine. (2010) 11:1270–3.
54. Yuheng, X, Jun, M, Xie, Z, and Tang, F. An epidemiological survey of hypertension among community residents in Dongchuan district. Occup Health. (2004) 12:120–2.
55. Zhihong, W, and Chaobin, Z. Epidemiologic analysis of hypertension in Shuangyang District of Changchun City. Jilin Provin Chin Commun Phys. (2011) 13:313–4.
56. Xie Zhiqing, L, Yulong, LL, Hua, L, Xiuke, Y, Mi, L, Fanyong, Z, et al. Analysis of epidemiological characteristics of chronic kidney disease in patients with hypertension and diabetes aged 30 years and above in rural Qiannan prefecture. Modern Prev Med. (2019) 48:586–589+593.
57. Tong Mingkun, M, Sailimai, JC, Jing, W, Ruiqi, S, Yongxiang, G, Bo, W, et al. Investigation on prevalence rate, awareness rate, treatment rate and control rate of hypertension in tens of thousands of patients. Chin J Circ. (2019) 35:866–72.
58. Dong-Feng, GU, Jiang, HE, and Xi-Gui, WU. Main causes and its modifiable risks of death among men and women in China. Chin J Prevent Control Chron Non Commun Dis. (2006)
59. Wu, X, Duan, X, Gu, D, Hao, J, Tao, S, and Fan, D. Prevalence of hypertension and its trends in Chinese population. Int J Cardiol. (1995) 52:39–44. doi: 10.1016/0167-5273(95)02443-Z
60. Wu, J, Li, T, Song, X, Sun, W, Zhang, Y, Liu, Y, et al. Prevalence and distribution of hypertension and related risk factors in Jilin Province, China 2015: a cross-sectional study. BMJ Open. (2018) 8:e020126. doi: 10.1136/bmjopen-2017-020126
61. Ke, L, Ho, J, Feng, J, Mpofu, E, Dibley, MJ, Feng, X, et al. Modifiable risk factors including sunlight exposure and fish consumption are associated with risk of hypertension in a large representative population from Macau. J Steroid Biochem Mol Biol. (2014) 144:152–5. doi: 10.1016/j.jsbmb.2013.10.019
Keywords: older population, hypertension, prevalence, meta-analysis, systematic review
Citation: Wang Z, Wang S, Lin H, Wang C and Gao D (2024) Prevalence of hypertension and related risk factors in older Chinese population: a meta-analysis. Front. Public Health. 12:1320295. doi: 10.3389/fpubh.2024.1320295
Edited by:
Jiandong Zhou, University of Warwick, United KingdomReviewed by:
Xiang Xiang, First Affiliated Hospital of Xinjiang Medical University, ChinaHeba Abdeen, Cairo University, Egypt
Haiping Duan, Qingdao Municipal Center for Disease Control and Prevention, China
Copyright © 2024 Wang, Wang, Lin, Wang and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Da Gao, Z2FvZGFfNzg5MEAxNjMuY29t
 Zicheng Wang
Zicheng Wang Da Gao
Da Gao