- 1Department of Medical Humanities and Social Sciences, College of Medicine, Yonsei University, Seoul, Republic of Korea
- 2Center for Global Development, Yonsei lnstituite for Global Health, Yonsei University Health System, Seoul, Republic of Korea
- 3School of Social Work, The University of Memphis, Memphis, TN, United States
- 4Institute of Media Arts, Yonsei University, Seoul, Republic of Korea
Background: Human papillomavirus (HPV) can cause cancers in men and women. Despite the availability of an effective vaccine, HPV vaccination coverage remains suboptimal among college students. Literature showed that hesitancy for HPV vaccination is a leading barrier to the uptake in this group. However, prior interventions have shown limitations in reducing HPV vaccine hesitancy in college students. Thus, this study examined a conventional educational approach using a vaccine information statement (VIS), and subsequently explored college students’ HPV vaccine hesitancy and the potential of virtual reality (VR) technology to overcoming the limitations of interventional efforts.
Methods: We employed a mixed-methods design along with convenience sampling, constituting a one-way pre- and post-intervention (HPV VIS) survey (Study A) and individual interviews (Study B). All data collections occurred with 44 college students at an urban public university at the mid-south region of the U.S. between October 2022 and April 2023. Study A assessed changes in HPV vaccination outcomes including knowledge, beliefs/attitudes, vaccine hesitancy, and intentions. Study B measured college students’ primary reasons for HPV vaccine hesitancy and preferred strategies for the vaccination promotion including VR-based education. We conducted paired t-test and Wilcoxon signed ranks test for quantitative data and framework analysis for qualitative data.
Results: Participants reported significant improvements in knowledge [t(43) = 6.68, p < 0.001] regarding HPV vaccination between before and after reading the HPV VIS. No change was observed in beliefs/attitudes, vaccine hesitancy, and intentions. The framework analysis revealed college students’ reasons for HPV vaccine hesitancy, needed information, and preferred strategies along with the potential of VR technology for future HPV vaccination education.
Conclusion: The findings provided essential information on designing HPV vaccination information focused on vaccine hesitancy among college students. Future research should consider these findings in developing interventions including VR to increasing HPV vaccine acceptance among college students.
1 Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States (U.S.) (1). Among over 200 varieties of this virus, long-lasting infections with high-risk HPVs (e.g., HPV16 and HPV18) can lead to cancers for both women and men (2). HPV accounts for the majority of cervical cancers, above 90% of anal cancers, 75% of vaginal cancers, 70% of oropharyngeal and vulvar cancers, and over 60% of penile cancers in the U.S. (2). It is estimated that there were approximately 47,199 new cases of HPV-associated cancer in the U.S. each year, with 26,177 cases in women and 21,022 cases in men (3).
The HPV vaccine is highly effective in protecting against the types of HPV which lead to cancer (4). The Advisory Committee on Immunization Practices (ACIP) recommends initiating HPV vaccination as early as age 9, and receiving routine vaccination at age 11 or 12, or catch-up vaccination for adults up to the age of 26 who have not yet received their recommended vaccinations (5). Although safe, efficacious vaccines against HPV have been available since 2006 for women and 2009 for men (6, 7), many eligible young adults have chosen to delay or refuse HPV vaccination (8–10). Across all age-based populations in the U.S., college students have reported high rates of HPV prevalence along with low rates of HPV vaccination (11–13). The 2022 National College Health Assessment survey demonstrated that only 41% of male college students and 57% of female college students were up to date with recommended HPV vaccine series (14). This lags behind 60 and 64% of HPV vaccination coverage for male and female adolescents, respectively, aged 13 through 17 years (15), and falls far short below the 80% benchmark of the national goal set by Healthy People 2030 (8–10).
Existing literature has shown that the suboptimal HPV vaccination coverage in U.S. college students was associated with multi-level factors: individual characteristics, interpersonal influences, and social and structural factors. Individual characteristics include a lack of awareness and knowledge of HPV and the vaccination (16) and HPV vaccine-related misperceptions, misbeliefs, and negative attitudes (17, 18). Interpersonal influences include parent’s or peer’s negative attitudes toward the vaccination or vaccine endorsement (19, 20), and lack of recommendations from healthcare providers (17). Social and structural factors include social/religious norms or stigma (11, 19, 21, 22), the spread of misinformation (19, 23), costs and insufficient insurance coverage (20, 21, 24), complex vaccination schedules (24), limited campus vaccine availability, and the absence of policies or programs for HPV vaccination (22).
Research also has indicated that vaccine hesitancy is a leading barrier to HPV vaccination among college students (25, 26). Further, over the past few years the COVID-19 pandemic has elevated levels of vaccine hesitancy both nationally and globally (27). The Strategic Advisory Group of Experts on Immunization Working Group (hereafter, Sage Working Group), established by the World Health Organization (WHO), defined vaccine hesitancy as a “delay in acceptance or refusal of vaccination despite availability of vaccine services” (28). Vaccine hesitancy is characterized by its complexity, context specificity, and variabilities based on time, place, and types of vaccines, existing on a continuum between full acceptance and outright refusal of vaccination (29).
To increase HPV vaccination among college students, previous interventions have employed health education and communication strategies. These strategies involve one or a combination of: (a) delivery of HPV vaccination information or messages by peers and/or health experts (30, 31) via leaflets (32), videos (33), websites (34, 35), text/email (36), social media (37), or campaigns (38, 39) and (b) reminders of vaccine appointments using letters (40) or electronic messaging (36, 41). These interventional efforts yielded some positive vaccination outcomes, with improvements mostly observed in knowledge of HPV and the vaccination (23, 36), some in HPV vaccination-related perceptions, beliefs, attitudes, and/or intentions (23, 24, 42), but only limited increases in the uptake (20, 42). To date, few interventions have demonstrated rigorous evidence on their effectiveness in increasing actual uptake of HPV vaccination among college students. According to literature, one reason for this is because the majority of the interventions focused predominantly on increasing knowledge of HPV and the vaccination, but increased knowledge alone was insufficient to close the knowledge-vaccine adoption gap (24). Another reason is that the interventions addressed college students’ hesitancy for HPV vaccination only for certain dimensions of the hesitancy (43–45), while the vaccine hesitancy constitutes complex, multi-dimensional constructs (26). According to the SAGE Working Group (29), vaccine hesitancy comprises three psychological dimensions: confidence (trust in the effectiveness of a vaccine), complacency (perceptions of the need to vaccinate and risk), and convenience (accessibility, self-efficacy), categorized at multiple levels (including contextual influences, individual/group influences, and vaccine/vaccination-specific issues). Also, a recent systematic review conceptualized vaccine hesitancy as a state of indecisiveness regarding a vaccination decision, determined by two psychological factors: cognitive factors (knowledge, beliefs, self-efficacy) and affective factors (emotion, attitudes) (46). Therefore, there is a need for developing an innovative, effective intervention that overcomes the limitations of prior efforts to close the knowledge–behavior gap in HPV vaccine practice by reducing the vaccine hesitancy among college students through addressing multi-dimensions of the vaccine hesitancy.
An increasing body of research has attended to virtual reality (VR) to facilitate vaccination, widely employing it in the sectors ranging from health communication to medical training (47). VR is an interactive three-dimensional simulation which permits a person to experience real-world environments and learn new behaviors and skills through avoiding obstacles to targeted outcomes (48). Emerging evidence has demonstrated the potential of VR as an effective health education tool for addressing vaccine hesitancy and positively influencing a person’s vaccine-related decision-making (43). However, no study has examined the role of VR in lowering hesitancy for HPV vaccination especially for college students to advance their vaccination outcomes.
To develop a VR-based approach to alleviating hesitancy for HPV vaccination among college students and increasing their vaccination coverage, it is essential to understand why college students are hesitant to receive an HPV vaccine and what information they need to address the hesitancy. It is also important to obtain data on how college students view VR as a health education platform to deliver the vaccination information. Moreover, although HPV vaccine information statements (VIS) have been widely used in health education campaigns for the public. The functioning of the HPV VISs concerning HPV vaccination outcomes, including knowledge, beliefs, attitudes, intentions, and vaccine hesitancy among college students, remains unknown. Thus, this study employed a mixed methods design consisting of quantitative pre- and post-intervention survey (Study A) and qualitative interviews (Study B). Study A aimed to evaluate whether a conventional HPV vaccination education using an existing HPV vaccine information statement (HPV VIS, provided by the Centers for Disease Control and Prevention [CDC]) (49) can improve HPV vaccination outcomes including knowledge, beliefs/attitudes, vaccine hesitancy, and intentions among college students. Study A hypothesized that after reading the HPV VIS, college students would report significant changes in knowledge, beliefs/attitudes, vaccine hesitancy, and intentions compared to their status before reading the HPV VIS. The findings would inform the design and development of educational content aimed at reducing HPV vaccine hesitancy and facilitating the uptake among college students.
Additionally, Study B aimed to explore college students’ reasons for HPV vaccine hesitancy, needed information directed toward HPV vaccine hesitancy and the vaccination promotion, and preferred strategies and the potential of VR for improving HPV vaccination acceptance. The research questions of Study B include:
Research question 1: What are primary reasons for HPV vaccine hesitancy among college students?
Research question 2: What specific information do college students need to reduce HPV vaccine hesitancy and make an informed decision about HPV vaccination?
Research question 3: What are college students’ preferred strategies for HPV vaccination promotion and views of the potential of VR for the vaccination education?
2 Materials and methods
2.1 Study design and procedure
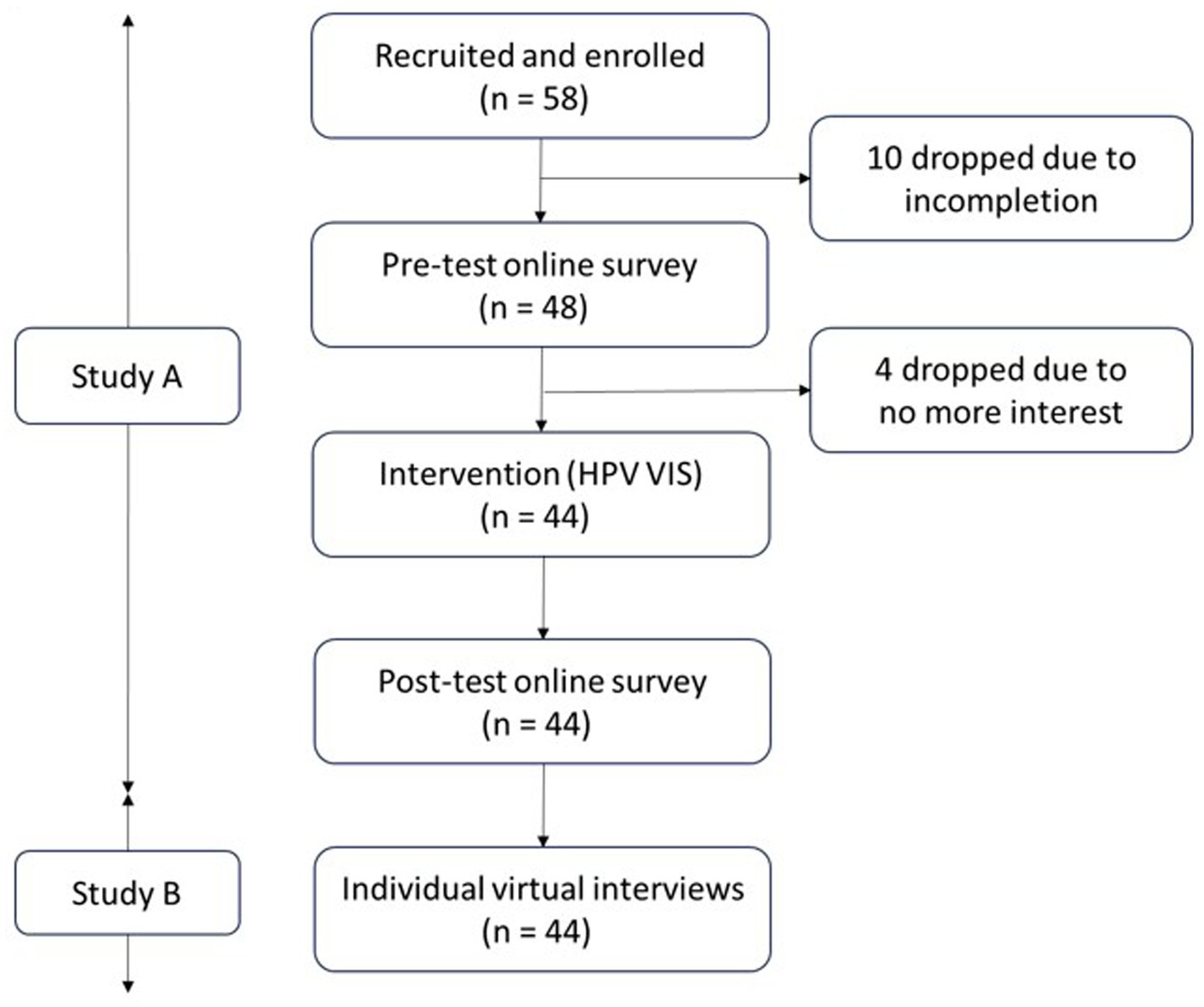
As shown in Figure 1, we employed a sequential quantitative-qualitative mixed method study with an emphasis on qualitative research—i.e., a quan-QUAL design (50–52). The study constituted two parts: a one-way pre- and post-intervention (i.e., HPV VIS education) survey (Study A) and subsequent qualitative individual interviews (Study B). For Study A, we provided the two-page-long HPV VIS for participants individually to read on a shared screen through a university virtual conference platform (i.e., Zoom). We administered online survey using Qualtrics before and after the intervention. For Study B, we performed an individual interview with the participants who had completed Study A using the same virtual conference platform. The university’s institutional review board approved this study (IRB ID#: PRO-FY2023-57).
2.2 Study setting
This study took place at an urban public university in the mid-south region of the U.S. The university was situated in a metropolitan area in the western region of Tennessee. The university had an enrollment of over 21,000 students at the time of the study, offering degrees from baccalaureates to doctoral levels. For characteristics of the enrolled students, approximately 60% were female, with more than half falling between the ages of 18 and 26 years old. White students accounted for about 41%, followed by African American students at 34%, Hispanic students at 8%, and Asian students at 5%. Furthermore, first-generation students constituted about 31% of the degree-seeking undergraduates. Lastly, about two thirds of the students came from in-state, while 46% were Pell grant recipients.
2.3 Study A
2.3.1 Sampling and data collection
We performed convenience sampling to recruit study participants at the university between October 2022 and April 2023. Eligible participants should be undergraduates who were currently enrolled for the university and aged between 18 and 26 years old. For recruitment, we used advertisements of referrals, flyers, and emails. A total of 58 students participated in this study, and we sent the participants a link to an online survey that included a brief study description, a consent form, screening questions, and a baseline survey questionnaire. Among the 58 participants, 48 students were eligible and completed both the consent form and the baseline survey. We contacted these students via email to set up a Zoom-based individual virtual conference for the intervention and the post-intervention survey (as well as an individual interview) at the participants’ preferred date and time. Out of the 48 participants, 44 students were scheduled for an individual virtual conference because four students dropped out of the study due to their no more interest in the study. At the beginning of the virtual conference, we asked a participant to read the HPV VIS, which took about 5 min on average. Upon the completion of the reading, we emailed another link to the post-intervention survey for the participant to complete. Once the participant completed the post survey, we transited to an individual interview. The intervention, post-test, and interview were conducted orderly on the same day. The pre- and post-intervention surveys took approximately 15 min and 6 min, respectively, while the individual interview took about 25 min on average.
2.3.2 Measures
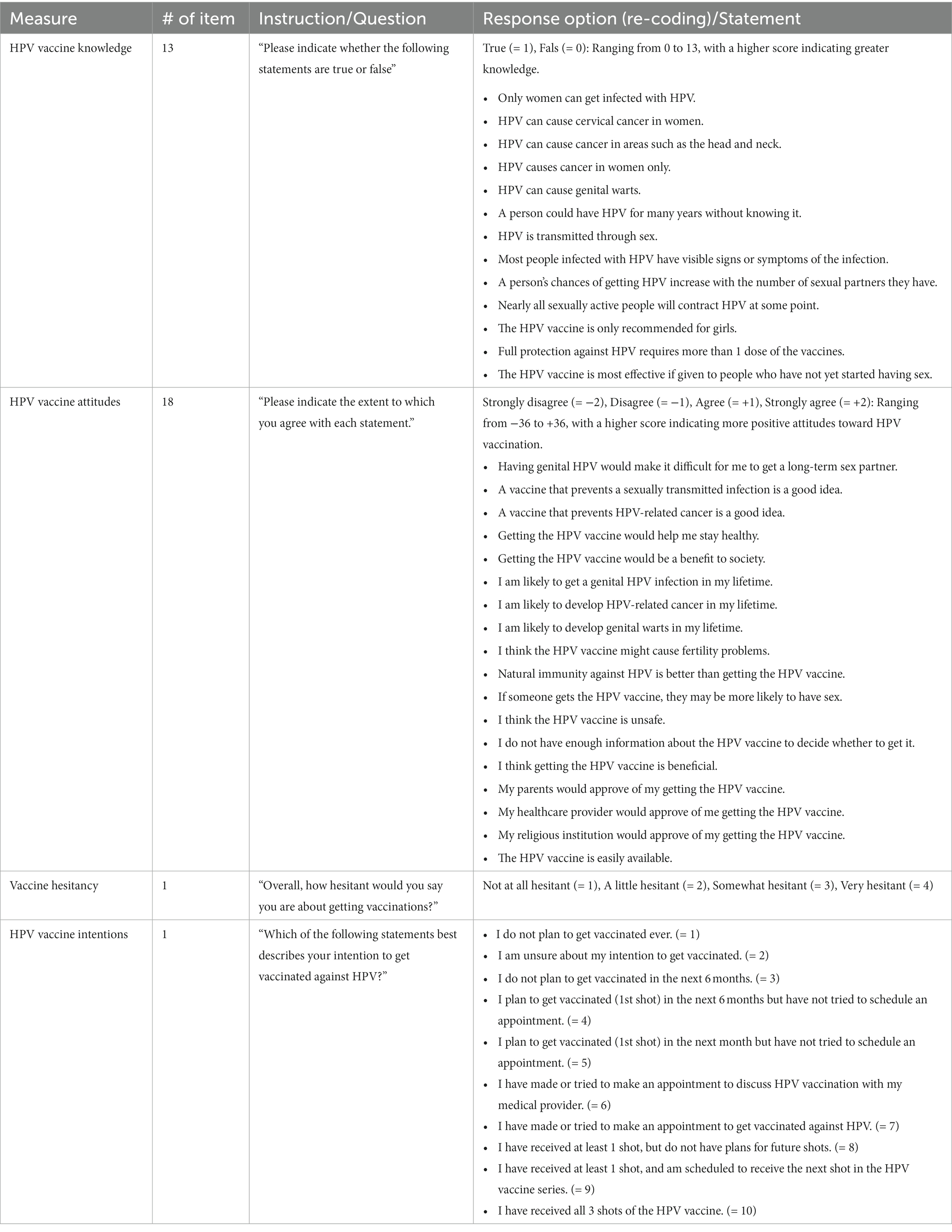
For survey, we carefully reviewed existing literature and adopted valid measures regarding HPV vaccination for college students to collect quantitative information on knowledge, beliefs/attitudes, vaccine hesitancy, intentions, and sociodemographics (see Table 1) for comparisons in changes of the measures of interest between pre- and post-education. We excluded sociodemographic measures only from the post-intervention survey.
2.3.2.1 Vaccine knowledge
We measured HPV vaccine knowledge through adopting Harrison et al.’s 13-item true/false HPV Knowledge Questionnaire (HPV-KQ) (53).
2.3.2.2 Vaccine beliefs/attitudes
To assess HPV vaccine beliefs/attitudes, we used Patel et al.’s 18-item HPV-related Beliefs/Attitudes on a four-point Likert scale (“strongly disagree,” “disagree,” “agree,” and “strongly agree”) (54).
2.3.2.3 Vaccine hesitancy
We assessed the degree of vaccine hesitancy with a question (“How hesitant would you say you are about getting vaccinations?”) on a four-point Likert scale (“not at all hesitant,” “a little hesitant,” “somewhat hesitant,” or “very hesitant”).
2.3.2.4 Vaccine intentions
We measured HPV vaccination intentions with one item of the HPV Vaccination Stage of Change Scale with 10 options: e.g., “I am unsure about my intention to get vaccinated,” “I do not plan to get vaccinated in the next six months,” “I plan to get vaccinated (1st shot) in the next month but have not tried to schedule an appointment,” “I have made or tried to make an appointment to get vaccinated against HPV” (54).
2.3.2.5 Sociodemographic information
We measured sociodemographic characteristics, including age (year), sex (female vs. male), sexual orientation (heterosexual, bisexual, lesbian, not listed, prefer not to reply), race (Black/African American, white, Asian, Native American/American Indian), Hispanic/Latino, school year, living arrangement, marital status, employment, health insurance, HPV vaccination status (never received, unsure/do not know, and received—all recommended shots, at least 1 shot and scheduled for the next shot, or at least 1 shot but no plan), self-rate health status, and religiosity.
2.3.3 Data analysis
We performed descriptive statistics to describe sociodemographic characteristics of the participants. We performed a paired t-test to assess within-group mean differences for continuous variables (i.e., knowledge and beliefs/attitudes) and Wilcoxon signed ranks test for ordinal variables (i.e., vaccine hesitancy and intentions). We conducted all statistical analyses with a 5% statistical significance level using IBM SPSS Statistics software version 29.0.1.
2.4 Study B
2.4.1 Data collection
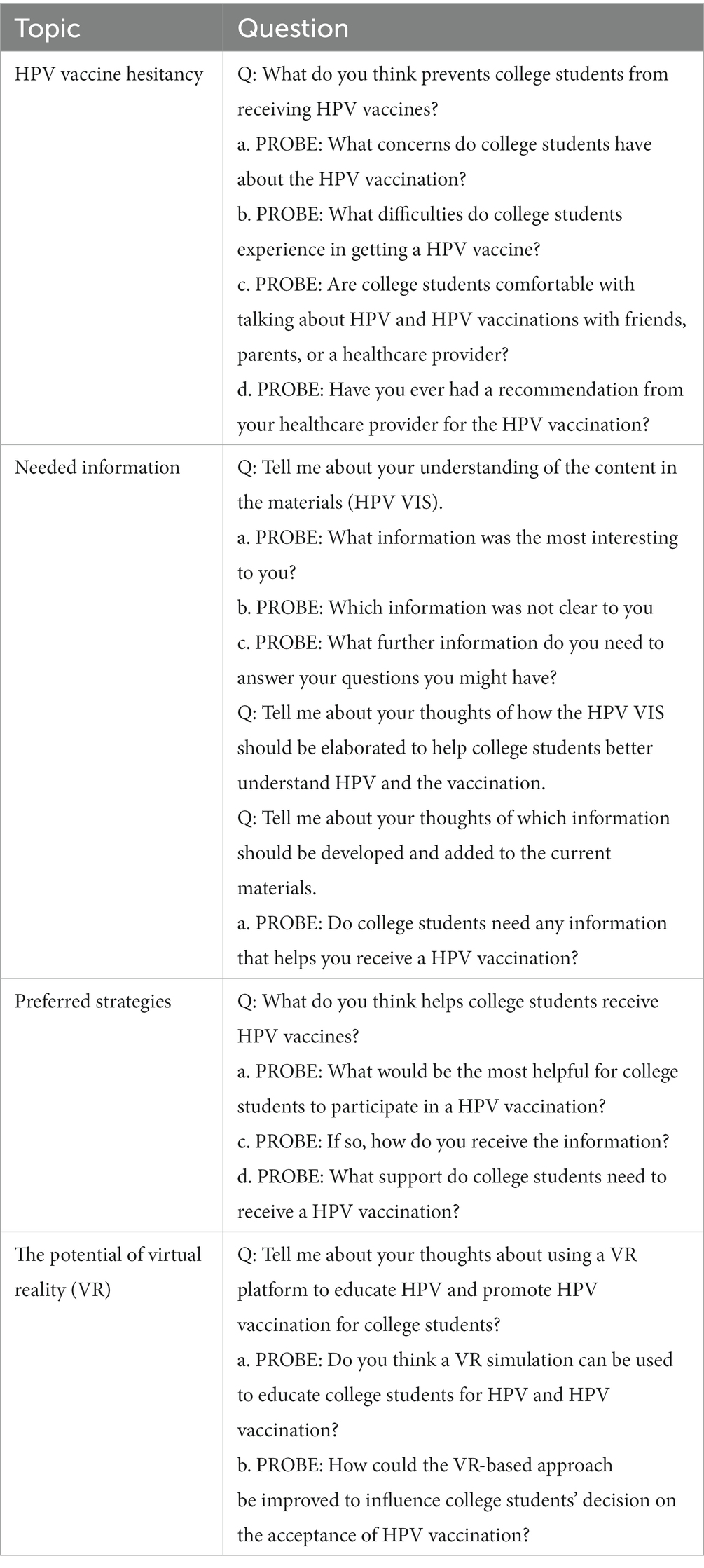
We developed semi-structured open-ended questions regarding HPV vaccine hesitancy, needed information for vaccine hesitancy and vaccination promotion, and preferred strategies and the potential of VR for HPV vaccination education (see Table 2). We conducted qualitative individual interviews using a Zoom-based virtual conference with 44 participants who had completed Study A. We digitally recorded all interviews via Zoom. All participants received a $40-worth electronic gift card as an honorarium after completing the interview.
2.4.2 Data analysis
We analyzed the interview data transcribed verbatim using framework analysis. The framework analysis follows six phases: Familiarization with the interview data, coding, developing a working analytical framework, applying the analytical framework, charting data into the framework matrix, and interpreting the data (55). In the initial phase, three authors individually reviewed the interview data multiple times to gain familiarity. Prior to coding, the authors identified themes and sub-themes based on the interview topics. In the coding phase, the authors independently coded two interview data sets and met online to reconcile any discrepancies and finalize the codes. This coding process was then repeated for an additional three interview data sets. For coding of the reasons for HPV vaccine hesitancy, particularly, we adopted the Vaccine Hesitancy Determinants Matrix developed by WHO’s Sage Working Group that classifies factors contributing to vaccine hesitancy into individual/group influences, contextual influences, and vaccine/vaccination-specific issues (56). Subsequently, the authors developed a working analytical framework using a spreadsheet to encompass themes, sub-themes, codes, and associated quotes. Utilizing this framework, the authors independently coded the remaining interview data, cross-referencing and finalizing the matrix collectively. The interview data were then organized into the framework matrix. In the final phase, the three authors interpreted the data.
3 Results
3.1 Study A
3.1.1 Sociodemographic characteristics
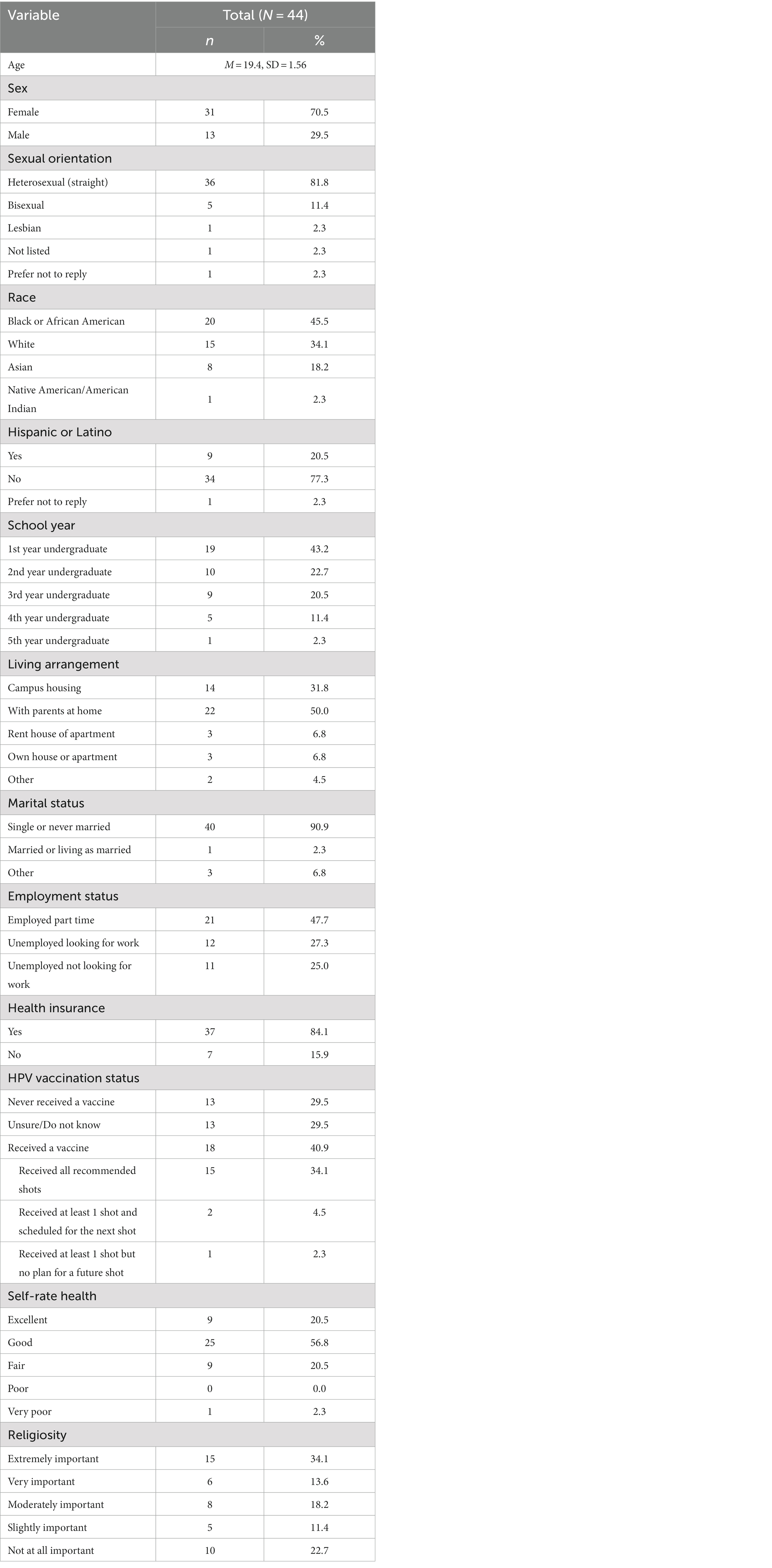
Table 3 presents sociodemographic characteristics of the participants. The mean age was 19 years old (SD = 1.56). Compared to the student body of the university, the participants were higher in the rates of females (71% vs. 60%), African Americans (46% vs. 34%), Hispanic/Latino (21% vs. 8%). More than two thirds were in the 1st or 2nd school years (43 and 23%). Half (50%) of the participants reported living with a parent at home. The majority (91%) were single or never married. Almost half of the participants (48%) were part-time employees. About 84% were covered by a health insurance, and 41% reported the receipt of at least shot of a HPV vaccine. Finally, two thirds (66%) reported religion as moderately to extremely important.
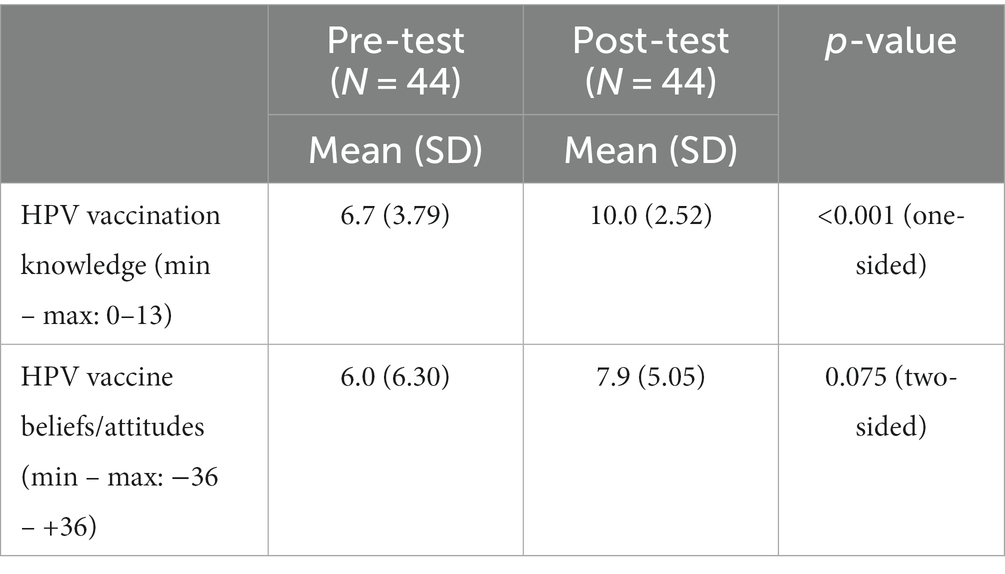
3.1.2 Knowledge, beliefs/attitudes, vaccine hesitancy, and intentions
Table 4 shows the results from the paired t-test for the continuous variables of knowledge and beliefs/attitudes. The HPV vaccine knowledge was found to have a mean of 6.7 (n = 44, SD = 3.79) at pre-intervention, and a mean of 10.0 (n = 44, SD = 2.52) at post-intervention. The vaccine beliefs/attitudes was found to have a mean of 6.0 (n = 44, SD = 6.30) at pre-intervention, and a mean of 7.9 (n = 44, SD = 5.05) at post-intervention. The results indicated a significant improvement in knowledge [t(43) = 6.68, p < 0.001] and a marginal improvement in beliefs/attitudes [t(43) = 1.82, p = 0.075] regarding HPV vaccination between before and after reading the HPV VIS. Also, we performed the Wilcoxon signed ranks test for the ordinal variables of vaccine hesitancy and intentions. The vaccine hesitancy was found to have a mean rank of 6.9 at pre-intervention, and a mean rank of 6.0 at post-intervention. The vaccine intentions was found to have a mean rank of 6.8 at pre-intervention, and a mean rank of 7.3 at post-intervention. The analysis showed no significant change in vaccine hesitancy (Z = −0.78, p < 0.44) or vaccine intentions (Z = −0.14, p < 0.89) before and after the intervention.
3.2 Study B
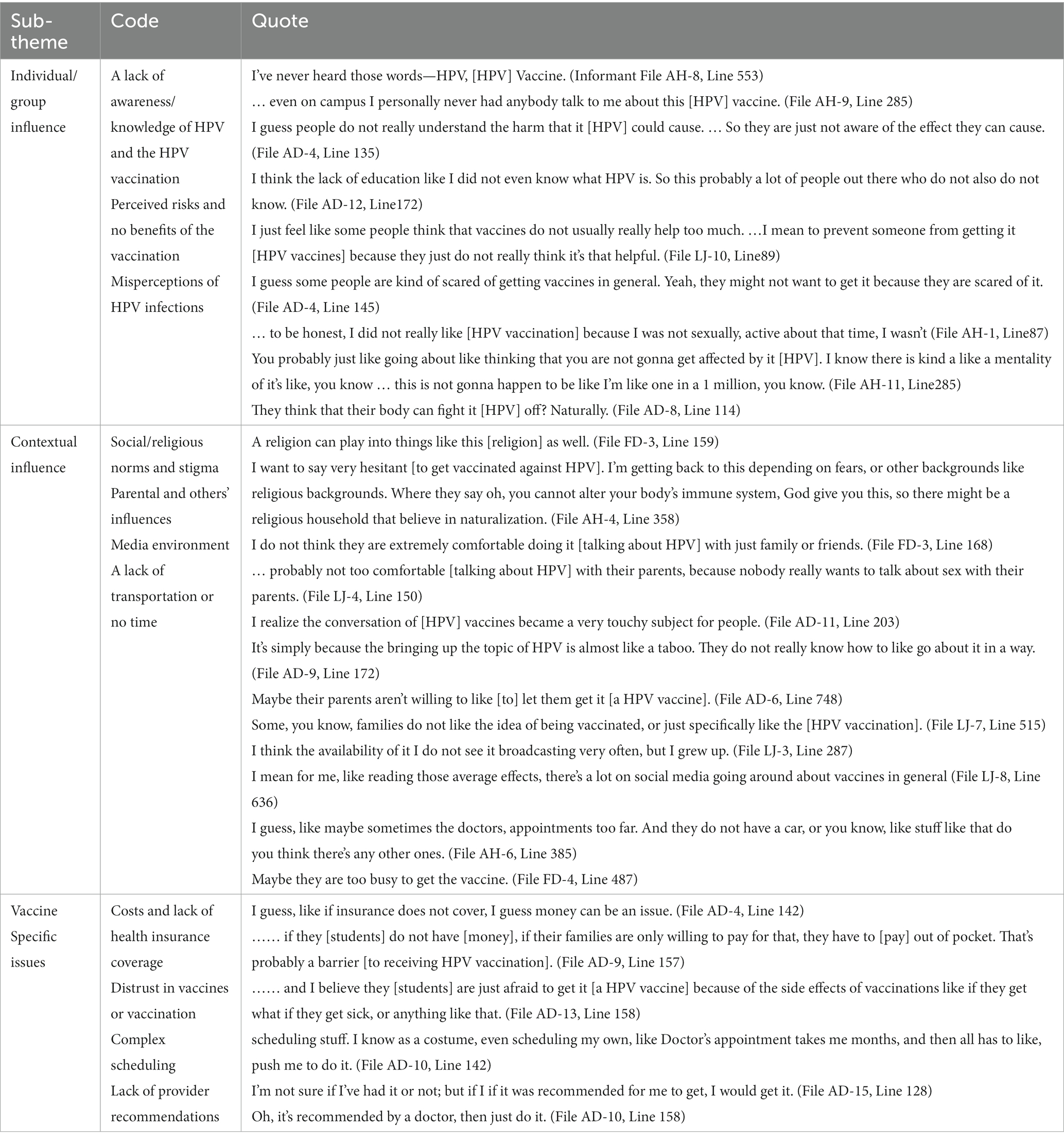
3.2.1 Reasons for HPV vaccine hesitancy (theme 1, research question 1)
The qualitative analysis revealed several reasons for HPV vaccine hesitancy among college students. This included individual/group influences, contextual influences, and vaccine/vaccination-specific issues (Table 5).
For the individual/group influences on HPV vaccine hesitancy, students were hesitant to receive a HPV vaccine due to a lack of awareness or knowledge of HPV and the HPV vaccination ([Informant] AH-8, [Transcript line] #553; AH-9, #285; AD-4, #135; “I’ve never heard those words—HPV, [HPV] Vaccine.”), perceived risks and no benefits of the vaccination (LJ-10, #89; AD-4, #145; “I just feel like some people think that vaccines do not usually really help too much. …I mean to prevent someone from getting it [HPV vaccines] because they just do not really think it’s that helpful.”), and misperceptions of HPV infections (AH-1, #87; AH-11, #285; AD-8, #114; “You probably just like going about like thinking that you are not gonna get affected by it [HPV]. I know there is kind a like a mentality of it’s like, you know … this is not gonna happen to be like I’m like one in a 1 million, you know.”).
For the contextual influences on the vaccine hesitancy, students stated social/religious norms and stigma (FD-3, #159; AH-4, #358; “I want to say very hesitant [to get vaccinated against HPV]. I’m getting back to this depending on fears, or other backgrounds like religious backgrounds. Where they say oh, you cannot alter your body’s immune system, God give you this, so there might be a religious household that believe in naturalization.”), parental and others’ influences (FD-3, #168; LJ-4, #150; AD-11, #203; AD-9, #172; AD-6, #748, LJ-7, #515; “Some, you know, families do not like the idea of being vaccinated, or just specifically like the [HPV vaccination]”), media environment (LJ-3, #287; LJ-8, #636; “I mean for me, like reading those average effects, there’s a lot on social media going around about vaccines in general.”), and a lack of transportation or no time (AH-6, #385; FD-4, #487; “I guess, like maybe sometimes the doctors, appointments too far. And they do not have a car, or you know, like stuff like that do you think there’s any other ones.” (File AH-6, Line 385) “Maybe they are too busy to get the vaccine.”).
Lastly, college students were hesitant for HPV vaccination due to the vaccine/vaccination-specific issues, including costs and lack of health insurance coverage (AD-4, #142; AD-9, #157; “I guess, like if insurance does not cover, I guess money can be an issue.”), distrust in vaccines or vaccination (i.e., concerns over side effects) (AD-13, #158; “…… and I believe they [students] are just afraid to get it [a HPV vaccine] because of the side effects of vaccinations like if they get what if they get sick, or anything like that.”), complex scheduling (AD-10, #142; “I know as a costume, even scheduling my own, like Doctor’s appointment takes me months, and then all has to like, push me to do it.”), and a lack of provider recommendations (AD-15, #128; AD-10, #158; “I’m not sure if I’ve had it or not; but if I if it was recommended for me to get, I would get it.”).
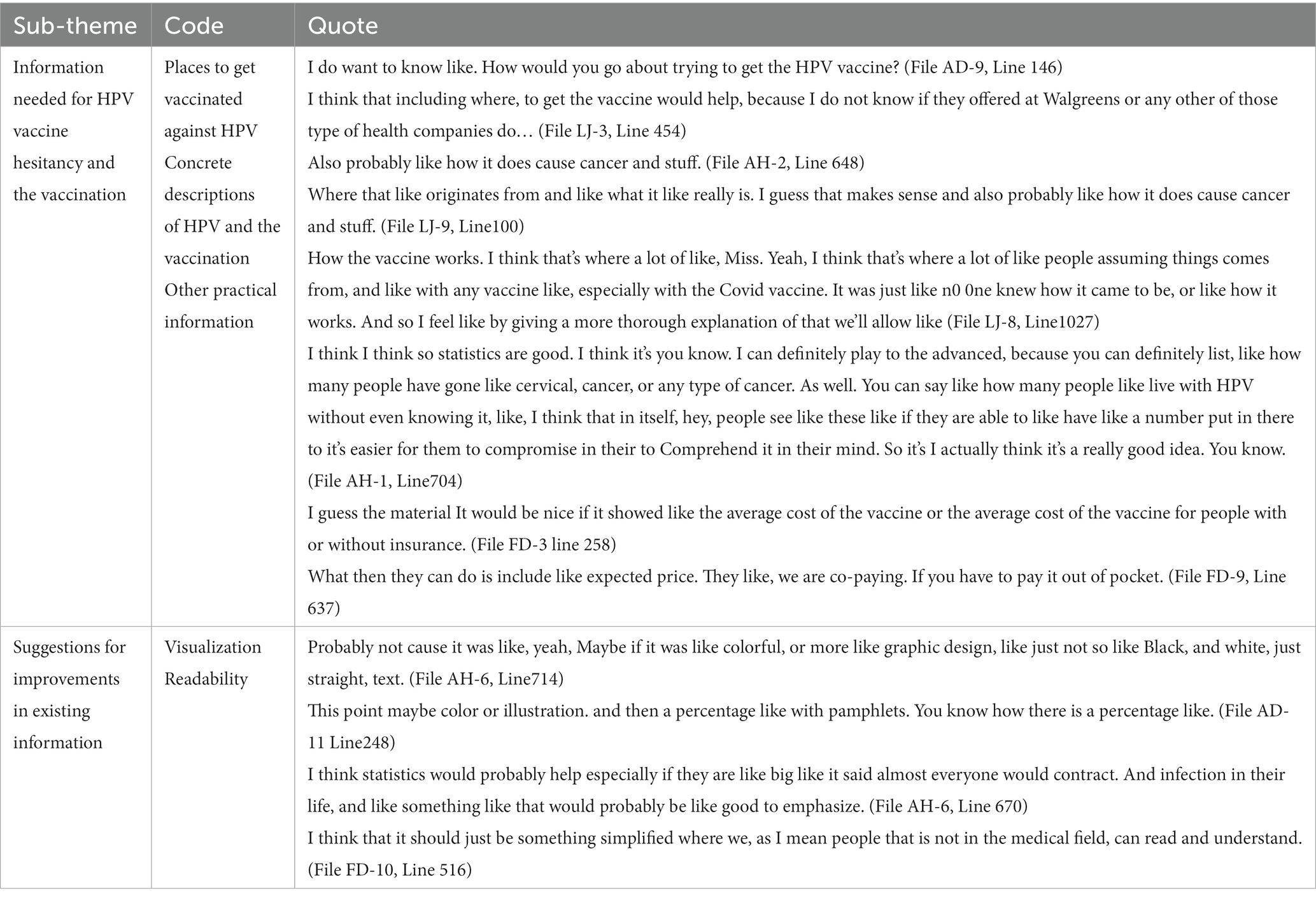
3.2.2 Needed information for HPV vaccination (theme 2, research question 2)
The analysis also revealed college students’ needed information for reducing HPV vaccine hesitancy and facilitating the uptake (Table 6). This information included places for HPV vaccination, concrete descriptions of the virus and the vaccination, and other practical information.
More specifically, students stated that they sought to receive information on where to get vaccinated (AD-9, #146; LJ-3, #454; “I think that including where, to get the vaccine would help, because I do not know if they offered at Walgreens or any other of those type of health companies do……”). Students also mentioned that the information should include the process of HPV infection and its consequences, a mechanism in which a vaccine prevents against HPV and relevant cancers, and costs related to the vaccination (AH-2, #648; LJ-8, #1027; AH-1, #704; FD-3 #258; FD-9, #637; “How the vaccine works. I think that’s where a lot of like, Miss. Yeah, I think that’s where a lot of like people assuming things comes from, and like with any vaccine like, especially with the Covid vaccine.”). Additionally, students offered suggestions for improving the existing HPV VIS. Students indicated that the HPV VIS should include more visuals (e.g., statistics, graphics, illustrations), and its content should be simple to enhance readability (e.g., plain language avoiding medical jargons) (AH-6, #714; AD-11, #248; FD-10, #516; AH-6, #670; “Probably not cause it was like, yeah, Maybe if it was like colorful, or more like graphic design, like just not so like Black, and white, just straight, text.”).
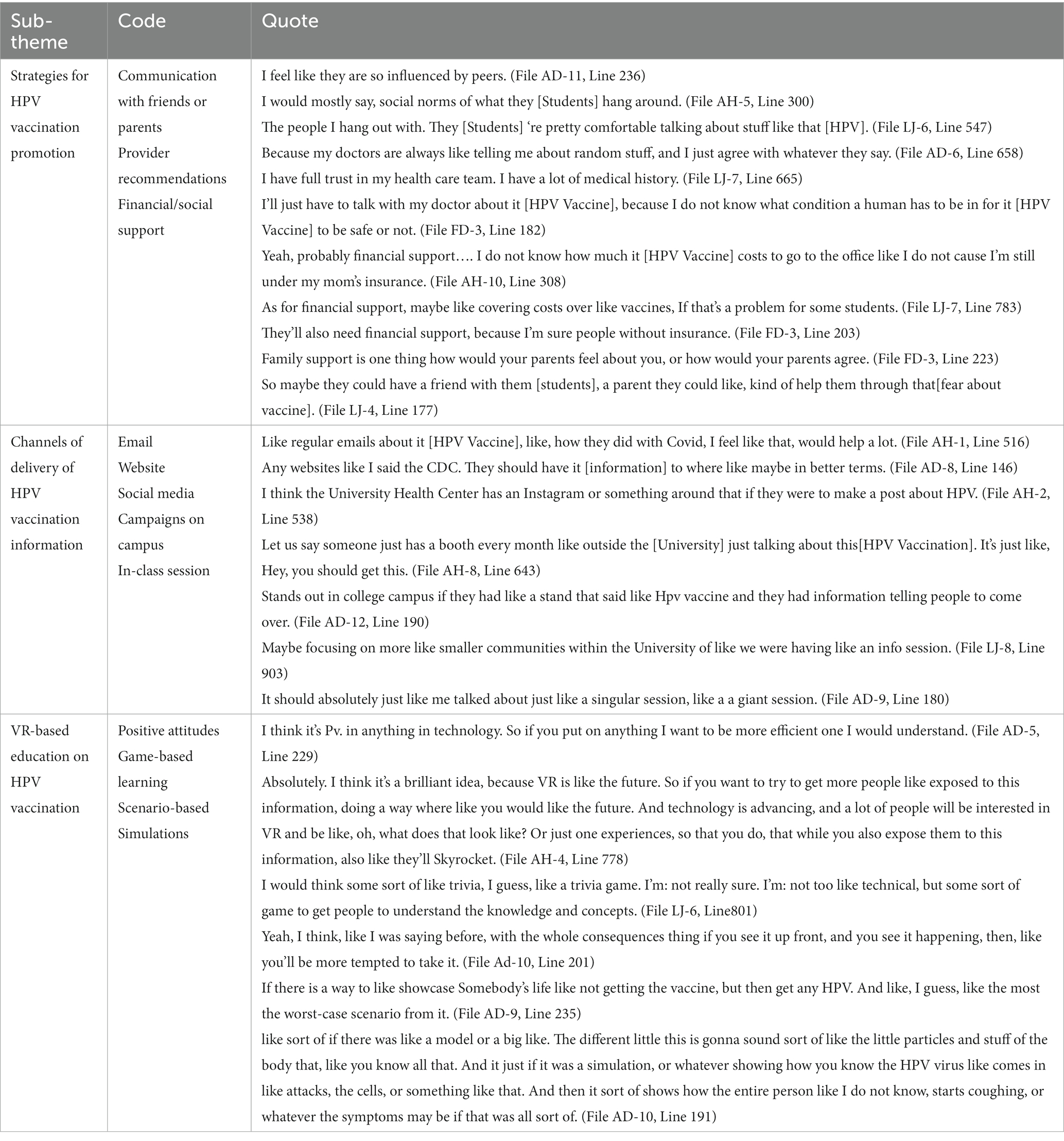
3.2.3 Preferred strategies and the potential of VR for the vaccination promotion (theme 3, research question 3)
Students suggested several strategies for facilitating HPV vaccination among college students (Table 7).
These strategies included communications with a friend or parent (AD-11, #236; AH-5, #300; LJ-6, #547; “I would mostly say, social norms of what they [Students] hang around.”), provider recommendations (AD-6, #658; LJ-7, #665; FD-3, #182; “I’ll just have to talk with my doctor about it [HPV Vaccine], because I do not know what condition a human has to be in for it [HPV Vaccine] to be safe or not.”), and financial or social support (AH-10, #308; LJ-7, #783; FD-3, #203; FD-3, #223; LJ-4, #177; “They’ll also need financial support, because I’m sure people without insurance.”). Students also stated that their preferred channels of delivery of HPV vaccination information included email, website, or social media (AH-1, #516; AD-8, #146; AH-2, #538; “Like regular emails about it [HPV Vaccine], like, how they did with Covid, I feel like that, would help a lot.”), campus-wide campaign, and in-class session (AH-8, #643; AD-12, #190; LJ-8, #903; AD-9, #180; “Let us say someone just has a booth every month like outside the [University] just talking about this [HPV Vaccination]. It’s just like, Hey, you should get this.”).
Lastly, students mentioned their thoughts and opinions of using VR as an education platform for reducing HPV vaccination hesitancy and increasing the uptake (Table 7). Most of the students revealed the positive attitudes toward the use of VR, stating that VR would be an attractive (“cool”), effective platform for HPV vaccination education among college students (AD-5, #229; AH-4, #778; “I think it’s a brilliant idea, because VR is like the future. So if you want to try to get more people like exposed to this information, doing a way where like you would like the future. And technology is advancing, and a lot of people will be interested in VR and be like, oh, what does that look like? Or just one experiences, so that you do, that while you also expose them to this information, also like they’ll Skyrocket.”). To maximize the education outcomes, students added that the VR-based vaccination education should involve game-based learning (LJ-6, #801) and scenario-based simulations guiding a vaccination procedure (AD-10, #201; AD-9, #235; AD-10, #191; “I think, like I was saying before, with the whole consequences thing if you see it up front, and you see it happening, then, like you’ll be more tempted to take it.”).
4 Discussion
Using a mixed-methods approach, we examined the effects of a conventional HPV vaccination education approach using the HPV VIS in advancing HPV vaccination outcomes including knowledge, beliefs/attitudes, vaccine hesitancy, and intentions among college students. We also assessed college students’ perceived reasons for HPV vaccine hesitancy, needed information, and preferred strategies including VR technology for HPV vaccination education. The findings provided essential information on designing HPV vaccination information or messaging focused on college students’ vaccine hesitancy. Also, the findings offered several implications for future research on interventional strategies for increasing HPV vaccine acceptance among college students.
Firstly, we found that the exposure to the HPV VIS among college students was effective in improving their knowledge regarding HPV vaccination, but no effect was observed in beliefs/attitudes, vaccine hesitancy, and intentions. This finding supports the fundamental role that conventional vaccination education including the VIS plays in increasing knowledge of HPV vaccination among college students (36). As consistent with the existing literature, however, this finding also implies that the conventional educational approach may have a limited influence on other HPV vaccination outcomes (i.e., beliefs/attitudes, vaccine hesitancy, and intentions) in this group which mediate the link between knowledge and uptake (23). According to theoretical frameworks of health behavior change (including health belief model and theory of planned behavior), an intention to engage in vaccination is determined by a person’s beliefs, attitudes, and subjective norms at a specific context and time (43, 57). Accordingly, it is critical for HPV vaccination education for college students to employ multi-interventional components that address their vaccine-related beliefs and attitudes associated particularly with their social norms. Future research should examine an optimized, theory-informed combination of these interventional components. These findings can help public health researchers and practitioners better understand the paths from the beliefs or attitudes to intentions, resulting eventually in the uptake among college students. In the paths, it is also important to first investigate college students’ information needs and specific reasons for the vaccine hesitancy and then design content and messaging tailored to effectively mitigate their vaccine hesitancy (58).
Secondly, we identified primary reasons for HPV vaccine hesitancy that college students perceived. While these reasons mostly are consistent with the existing literature, particularly, our findings underscore the context specificity of HPV vaccine hesitancy (i.e., social/religious norms and stigma and parental and others’ influences) in this group. Many students in our study mentioned that they felt embarrassment or difficulties of openly discussing HPV-related topics with parents and others in milieu of the mid-south region of the U.S. Particularly, this region has been widely affected by religious and political norms in which HPV is perceived as a taboo. In this study nearly two thirds reported that religion is moderately to extremely important. Vaccine hesitancy related to social/religious norms might contribute to consistently reported lower rates of HPV vaccination, compared to different U.S. regions (59), along with high rates of HPV prevalence, HPV-associated cancers, and cervical cancer mortality (60) in this region. While researchers and practitioners need to consider the identified reasons for HPV vaccine hesitancy in developing interventions, the interventional efforts should address the context-specific reasons for HPV vaccine hesitancy in college students.
Next, we identified college students’ needed information and preferred strategies for HPV vaccination promotion including channels of vaccination information delivery. The findings highlight the urgent need of developing specific and practical information for college students’ HPV vaccination promotion such as places for vaccination and vaccination procedure. In particular, as a HPV vaccine was not available to students on campus at the time of this research, interventional efforts should involve stakeholders on HPV vaccination at the university including a health student center in the initial stage of research. The findings also imply the importance of influences by peers, parents, and healthcare providers on vaccination-related decision making. This suggests that interventional components should leverage these influences when they design content and messaging related to the vaccination for college students. These efforts will enhance the vaccine accessibility in terms of locations, costs, and health insurance as well as the acceptability of the targeted or tailored information on HPV vaccination.
Finally, we found that college students viewed VR as a valuable technology for HPV vaccination education. Prior studies also showed that VR-based vaccination education had a positive impact on improving vaccination attitudes and intentions among the adult populations. For example, Vandeweerdt et al. found that VR was more effective in increasing COVID-19 vaccination intentions among adults, compared to texts and images (61). Nowak et al. also used a VIS paired with a VR-based simulation improved influenza vaccine-related attitudes and intentions among vaccine-avoidant adults aged 18 to 49 years (62). Furthermore, a recent study found that VR simulations significantly increased perceived efficacy to influenza vaccination and vaccination intention for both protecting the self and others in the community among college students in Taiwan (63). In these studies, VR played a significant role in making participants’ vaccination experience more immediate, engaging, and informative within mediated immersive environments than did the conventional approaches (61, 62, 64). A systematic review indicated that VR’s unique features, such as embodiment, realism, and interactivity, enable users to overcome their psychological barriers to a target behavior, leading to an increased likelihood of behavior change (48). Similarly, because vaccine hesitancy poses a wide array of psychological barriers (e.g., social/religious norms and stigma) to HPV vaccination, these findings imply the potential of VR to mitigate hesitancy for HPV vaccination, serving as an effective educational platform for improving HPV vaccination outcomes. Next studies should examine the acceptability and feasibility for the use of VR in the context of HPV vaccination among college students. As the distinct gap in HPV vaccine coverage by gender has persisted, future research should also examine VR-based educational interventions for addressing gender-specific hesitancy for HPV vaccination.
4.1 Limitations
We conducted a mixed-methods study to obtain comprehensive data, but the findings of this study might include some limitations. As the study employed non-probability sampling and a one-way study design, the findings may not be generalizable to other populations or settings. Additionally, the data was based on self-report which could introduce some recall bias. While individual interviews with a sample size of 44 achieved saturation to enhance the trustworthiness of the findings, the pre- and post-intervention survey with this sample size might not fully capture the effect of the HPV VIS in the changes in the beliefs/attitudes, vaccine hesitancy and intentions. Future studies using probability sampling along with a comparison group can offer a better understanding of the role of conventional vaccination education in college students (e.g., unvaccinated vs. vaccinated participants). Finally, this study explored HPV vaccine hesitancy in college students employing a framework analysis approach. Different qualitative analytic approaches (e.g., content analysis, thematic analysis) may reveal different themes and codes.
5 Conclusion
This mixed methods research informed effective educational approaches to HPV vaccination promotion targeted toward college students. The pre- and post-intervention survey found positive effects of a conventional vaccination education using the HPV VIS in increasing knowledge for college students. However conventional vaccination education also showed limitations in influencing beliefs/attitudes, vaccine hesitancy and intentions in this group. Also, the qualitative individual interviews identified primary reasons for HPV vaccine hesitancy among college students and needed information, for HPV vaccination education which can guide future interventions. These findings offer useful implications for generating strategies for educating and facilitating college students to increase HPV vaccination acceptance particularly through addressing their reasons for vaccine hesitancy. Also, the findings provide essential insight for future interventions using the potential of a VR-based HPV education for improving the vaccination outcomes in college students.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of the University of Memphis. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SY: Formal analysis, Writing – original draft. HK: Formal analysis, Writing – original draft. JA: Formal analysis, Writing – original draft. SJ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was funded by the West Cancer Foundation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Centers for Disease Control and Prevention. (2023). [cited 2023 Oct 28]. Available at: https://www.cdc.gov/vaccines/vpd/hpv/index.html.
2. National Cancer Institute. (2019). [cited 2023 Jul 21]. Available at: https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer.
3. Centers for Disease Control and Prevention. (2022). [cited 2023 Jul 21]. Available at: https://www.cdc.gov/cancer/hpv/statistics/index.htm.
4. National Cancer Institute. (2021). [cited 2023 Jul 22]. Available at: https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet.
5. Meites, E. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb mortal Wkly rep [internet]. (2019). [cited 2022]; 68. Available at: https://www.cdc.gov/mmwr/volumes/68/wr/mm6832a3.htm.
6. Centers for Disease Control and Prevention. (2023). [cited 2023 Jul 27]. Available at: https://www.cdc.gov/vaccines/acip/recs/grade/HPV-adults-etr.html.
7. Quinn, S, and Goldman, RD. Human papillomavirus vaccination for boys. Can Fam Physician. (2015) 61:43–6.
8. Chen, MM, Mott, N, Clark, SJ, Harper, DM, Shuman, AG, Prince, MEP, et al. HPV vaccination among Young adults in the US. JAMA. (2021) 325:1673–4. doi: 10.1001/jama.2021.0725
9. Lu, P-J, Hung, M-C, Srivastav, A, Grohskopf, LA, Kobayashi, M, Harris, AM, et al. Surveillance of vaccination coverage among adult populations -United States, 2018. Morb Mortal Wkly Rep Surveill Summ Wash DC. (2002) 2021:1–26.
10. National Vaccine Advisory Committee. Overcoming barriers to low HPV vaccine uptake in the United States: recommendations from the National Vaccine Advisory Committee: approved by the National Vaccine Advisory Committee on June 9, 2015. DHHS publication (2016). 131: 17–25, doi: 10.1177/003335491613100106
11. Goldfarb, JA, and Comber, JD. Human papillomavirus (HPV) infection and vaccination: a cross-sectional study of college students’ knowledge, awareness, and attitudes in Villanova. PA Vaccine X. (2022) 10:100141. doi: 10.1016/j.jvacx.2022.100141
12. Koskan, A, Cantley, A, Li, R, Silvestro, K, and Helitzer, D. College students’ digital media preferences for future HPV vaccine campaigns. J Cancer Educ. (2022) 37:1743–51. doi: 10.1007/s13187-021-02022-1
13. Mavundza, EJ, Iwu-Jaja, CJ, Wiyeh, AB, Gausi, B, Abdullahi, LH, Halle-Ekane, G, et al. A systematic review of interventions to improve HPV vaccination coverage. Vaccine. (2021) 9:687. doi: 10.3390/vaccines9070687
14. American College Health Association. (2023). Available at: https://www.acha.org/ACHA/Resources/Survey_Data/ACHA/Resources/Survey_Data.aspx.
15. Pingali, C. National Vaccination Coverage among Adolescents Aged 13–17 years — National Immunization Survey-Teen, United States, 2021. MMWR Morb mortal Wkly rep [internet]. (2022). [cited 2023 Apr 11]; 71. Available at: https://www.cdc.gov/mmwr/volumes/71/wr/mm7135a1.htm.
16. Kitur, H, Horowitz, AM, Beck, K, and Wang, MQ. HPV knowledge, vaccine status, and health literacy among university students. J Cancer Educ. (2022) 37:1606–13. doi: 10.1007/s13187-021-01997-1
17. D’Errico, MP, Tung, W-C, Lu, M, and D’Errico, R. Barriers and recommendations associated with human papillomavirus vaccination among college students. J Nurse Pract. (2020) 16:533–7. doi: 10.1016/j.nurpra.2020.04.011
18. Gönenç, İM, Abbas, MN, Çalbayram, N, and Ylmaz, S. A review of knowledge and attitudes of young people on cervical cancer and HPV vaccination. J Public Health. (2020) 28:97–03.
19. Kellogg, C, Shu, J, Arroyo, A, Dinh, NT, Wade, N, Sanchez, E, et al. A significant portion of college students are not aware of HPV disease and HPV vaccine recommendations. Hum Vaccin Immunother. (2019) 15:1760–6. doi: 10.1080/21645515.2019.1627819
20. Kessler, R, and Auwaerter, P. Strategies to improve human papillomavirus (HPV) vaccination rates among college students. J Am Coll Heal. (2021) 10:1–8.
21. McLendon, L, Puckett, J, Green, C, James, J, Head, KJ, Yun Lee, H, et al. Factors associated with HPV vaccination initiation among United States college students. Hum Vaccin Immunother. (2021) 17:1033–43. doi: 10.1080/21645515.2020.1847583
22. Kasymova, S, Harrison, SE, and Pascal, C. Knowledge and awareness of human papillomavirus among college students in South Carolina. Infect Dis Res Treat. (2019) 12:1882507. doi: 10.1177/1178633718825077
23. Ou, L, and Youngstedt, SD. The role of vaccination interventions to promote HPV vaccine uptake rates in a college-aged population: a systematic review. J Cancer Educ. (2022) 37:244–50. doi: 10.1007/s13187-020-01806-1
24. Barnard, M, Cole, AC, Ward, L, Gravlee, E, Cole, ML, and Compretta, C. Interventions to increase uptake of the human papillomavirus vaccine in unvaccinated college students: a systematic literature review. Prev Med Rep. (2019) 14:100884. doi: 10.1016/j.pmedr.2019.100884
25. Sonawane, K, Lin, Y-Y, Damgacioglu, H, Zhu, Y, Fernandez, ME, Montealegre, JR, et al. Trends in human papillomavirus vaccine safety concerns and adverse event reporting in the United States. JAMA Netw Open. (2021) 4:e2124502. doi: 10.1001/jamanetworkopen.2021.24502
26. World Health Organization. (2015). Available at: https://www.who.int/groups/strategic-advisory-group-of-experts-on-immunization.
27. National Foundation for Infectious Diseases. Natl. Found. Infect. Dis. (2020). [cited 2021 Apr 25]. Available at: https://www.nfid.org/keep-up-the-rates/issue-brief-the-impact-of-covid-19-on-us-vaccination-rates/.
28. World Health Organization. (2019). Available at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
29. Mac Donald NE, SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
30. Hopfer, S. Effects of a narrative HPV vaccination intervention aimed at reaching college women: a randomized controlled trial. Prev Sci Off J Soc Prev Res. (2012) 13:173–82. doi: 10.1007/s11121-011-0254-1
31. Long, AG, Roberts, CM, and Hayney, MS. Pharmacy student involvement with increasing human papillomavirus (HPV) vaccination among international college students. J Am Pharm Assoc. (2017) 57:127–8. doi: 10.1016/j.japh.2016.11.009
32. Juraskova, I, Bari, RA, O’Brien, MT, and McCaffery, KJ. HPV vaccine promotion: does referring to both cervical Cancer and genital warts affect intended and actual vaccination behavior? Womens Health Issues. (2011) 21:71–9. doi: 10.1016/j.whi.2010.08.004
33. Gerend, MA, and Shepherd, JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med Publ Soc Behav Med. (2012) 44:171–80. doi: 10.1007/s12160-012-9366-5
34. Dempsey, AF, Maertens, J, Sevick, C, Jimenez-Zambrano, A, and Juarez-Colunga, E. A randomized, controlled, pragmatic trial of an iPad-based, tailored messaging intervention to increase human papillomavirus vaccination among Latinos. Hum Vaccin Immunother. (2019) 15:1577–84. doi: 10.1080/21645515.2018.1559685
35. Bennett, AT, Patel, DA, Carlos, RC, Zochowski, MK, Pennewell, SM, Chi, AM, et al. Human papillomavirus vaccine uptake after a tailored, online educational intervention for female university students: a randomized controlled trial. J Women's Health. (2015) 24:950–7. doi: 10.1089/jwh.2015.5251
36. Richman, AR, Maddy, L, Torres, E, and Goldberg, EJ. A randomized intervention study to evaluate whether electronic messaging can increase human papillomavirus vaccine completion and knowledge among college students. J Am Coll Health J ACH. (2016) 64:269–78. doi: 10.1080/07448481.2015.1117466
37. Lee, MJ, and Cho, J. Promoting HPV vaccination online: message design and media choice. Health Promot Pract. (2017) 18:645–53. doi: 10.1177/1524839916688229
38. Gerend, MA, Murdock, C, and Grove, K. An intervention for increasing HPV vaccination on a university campus. Vaccine. (2020) 38:725–9. doi: 10.1016/j.vaccine.2019.11.028
39. Sundstrom, B, Brandt, HM, Gray, L, and Young Pierce, J. It’s my time: applying the health belief model to prevent cervical cancer among college-age women. J Commun Manag. (2018) 22:161–78. doi: 10.1108/JCOM-06-2016-0044
40. Patel, DA, Zochowski, M, Peterman, S, Dempsey, AF, Ernst, S, and Dalton, VK. Human papillomavirus vaccine intent and uptake among female college students. J Am Coll Heal. (2012) 60:151–61. doi: 10.1080/07448481.2011.580028
41. Stephens, AB, Wynn, CS, and Stockwell, MS. Understanding the use of digital technology to promote human papillomavirus vaccination – a RE-AIM framework approach. Hum Vaccin Immunother. (2019) 15:1549–61. doi: 10.1080/21645515.2019.1611158
42. Piedimonte, S, Leung, A, Zakhari, A, Giordano, C, Tellier, PP, and Lau, S. Impact of an HPV education and vaccination campaign among Canadian university students. J Obstet Gynaecol. (2018) 40:440–6. doi: 10.1016/j.jogc.2017.07.028
43. Li, L, Wood, CE, and Kostkova, P. Vaccine hesitancy and behavior change theory-based social media interventions: a systematic review. Transl Behav Med. (2022) 12:243–72. doi: 10.1093/tbm/ibab148
44. Hayes, KN, Pan, I, Kunkel, A, McGivney, MS, and Thorpe, CT. Evaluation of targeted human papillomavirus vaccination education among undergraduate college students. J Am Coll Heal. (2019) 67:781–9. doi: 10.1080/07448481.2018.1515742
45. Krawczyk, A, Lau, E, Perez, S, Delisle, V, Amsel, R, and Rosberger, Z. How to inform: comparing written and video education interventions to increase human papillomavirus knowledge and vaccination intentions in Young adults. J Am Coll Heal. (2012) 60:316–22. doi: 10.1080/07448481.2011.615355
46. Bussink-Voorend, D, Hautvast, JLA, Vandeberg, L, Visser, O, and Hulscher, MEJL. A systematic literature review to clarify the concept of vaccine hesitancy. Nat. Nat Hum Behav. (2022) 6:1634–48. doi: 10.1038/s41562-022-01431-6
47. Aliwi, I, Schot, V, Carrabba, M, Duong, P, Shievano, S, Caputo, M, et al. The role of immersive virtual reality and augmented reality in medical communication: a scoping review. J Patient Exp. (2023) 10:1171562. doi: 10.1177/23743735231171562
48. Wienrich, C, Döllinger, N, and Hein, R. Behavioral framework of immersive technologies (behave FIT): how and why virtual reality can support behavioral change processes. Front Virtual Real. (2021) 2:194. doi: 10.3389/frvir.2021.627194
49. Centers for Disease Control and Prevention. (2023). [cited 2023 Aug 4]. Available at: https://www.cdc.gov/vaccines/hcp/vis/vis-statements/hpv.html.
50. Tashakkori, A, and Teddlie, C. SAGE handbook of mixed methods in social & behavioral research. CA, U.S.A: SAGE Publications (2021).
51. Castro, FG, Kellison, JG, Boyd, SJ, and Kopak, A. A methodology for conducting integrative mixed methods research and data analyses. J Mix Methods Res. (2010) 4:342–60. doi: 10.1177/1558689810382916
52. Morse, JM. Approaches to qualitative-quantitative methodological triangulation. Nurs Res. (1991) 40:120–3. doi: 10.1097/00006199-199103000-00014
53. Harrison, SE, Yelverton, V, Wang, Y, Ostermann, J, Fish, LJ, Williams, CL, et al. Examining associations between knowledge and vaccine uptake using the human papillomavirus knowledge questionnaire (HPV-KQ). Am J Health Behav. (2021) 45:810–27. doi: 10.5993/AJHB.45.5.2
54. Patel, DA, Grunzweig, KA, Zochowski, MK, Dempsey, AF, Carlos, RC, and Dalton, VK. Human papillomavirus vaccine stages of change among male and female university students: ready or not? J Am Coll Health J ACH. (2013) 61:336–46. doi: 10.1080/07448481.2013.811244
55. Gale, NK, Heath, G, Cameron, E, Rashid, S, and Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13:117. doi: 10.1186/1471-2288-13-117
56. Kulkarni, S, Harvey, B, Prybylski, D, and Jalloh, MF. Trends in classifying vaccine hesitancy reasons reported in the WHO/UNICEF joint reporting form, 2014–2017: use and comparability of the vaccine hesitancy matrix. Hum Vaccin Immunother. (2021) 17:2001–7. doi: 10.1080/21645515.2020.1859319
57. Fallucca, A, Immordino, P, Riggio, L, Casuccio, A, Vitale, F, and Restivo, V. Acceptability of HPV vaccination in Young students by exploring health belief model and health literacy. Vaccine. (2022) 10:998. doi: 10.3390/vaccines10070998
58. Dubé, E, Gagnon, D, and Mac Donald, NE. Strategies intended to address vaccine hesitancy: review of published reviews. Vaccine. (2015) 33:4191–03. doi: 10.1016/j.vaccine.2015.04.041
59. Centers for Disease Control and Prevention. (2022). Available at: https://stacks.cdc.gov/view/cdc/120475.
60. Dyne EAV. Trends in human papillomavirus–associated cancers — United States, 1999–2015. MMWR Morb mortal Wkly rep [internet]. (2018).[cited 2020 Oct 23]; 67. Available from: https://www.cdc.gov/mmwr/volumes/67/wr/mm6733a2.htm.
61. Vandeweerdt, C, Luong, T, Atchapero, M, Mottelson, A, Holz, C, Makransky, G, et al. Virtual reality reduces COVID-19 vaccine hesitancy in the wild [internet]. PsyArXiv (2021). [cited 2022 Feb 6]. Available at: https://psyarxiv.com/sq9yc/.
62. Nowak, GJ, Evans, NJ, Wojdynski, BW, Ahn, SJ, Len-Rios, ME, Carera, K, et al. Using immersive virtual reality to improve the beliefs and intentions of influenza vaccine avoidant 18-to-49-year-olds: considerations, effects, and lessons learned. Vaccine. (2020) 38:1225–33. doi: 10.1016/j.vaccine.2019.11.009
63. Lee, J, Wu, D-Y, Lin, J-H, Kim, J, and Ahn, SJ. Using time travel in virtual reality (VR) to increase efficacy perceptions of influenza vaccination. J Comput-Mediat Commun. (2023) 28:zmad 010. doi: 10.1093/jcmc/zmad010
Keywords: college students, HPV vaccination, human papillomavirus, mixed-methods study, vaccine hesitancy, virtual reality
Citation: Yoon S, Kim H, An J and Jin SW (2024) Exploring human papillomavirus vaccine hesitancy among college students and the potential of virtual reality technology to increase vaccine acceptance: a mixed-methods study. Front. Public Health. 12:1331379. doi: 10.3389/fpubh.2024.1331379
Edited by:
Mwansa Ketty Lubeya, University of Zambia, ZambiaReviewed by:
Masangu Mulongo, Wits Health Consortium (WHC), South AfricaAaliyah Gray, Florida International University, United States
Copyright © 2024 Yoon, Kim, An and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seok Won Jin, c2ppbjFAbWVtcGhpcy5lZHU=
†These authors have contributed equally to this work and share first authorship
 Sangchul Yoon
Sangchul Yoon Heeyeon Kim2†
Heeyeon Kim2† Seok Won Jin
Seok Won Jin