- 1Environment and Sustainability Research Initiative, Khulna, Bangladesh
- 2Environmental Science Discipline, Life Science School, Khulna University, Khulna, Bangladesh
- 3Department of Parks, Recreation, and Tourism Management, Clemson University, Clemson, SC, United States
- 4Department of Tourism Management, Faculty of Tourism, Ondokuz Mayıs University, Samsun, Türkiye
- 5Department of Environmental Science and Management, North South University, Dhaka, Bangladesh
- 6Psychology Department, College of Education, Sultan Qaboos University, Muscat, Oman
- 7Psychology Department, Faculty of Arts, Menoufia University, Shibin el Kom, Egypt
- 8Department of Hygiene, Faculty of Public Health, Medical University of Plovdiv, Plovdiv, Bulgaria
- 9Research Group “Health and Quality of Life in a Green and Sustainable Environment”, SRIPD, Medical University of Plovdiv, Plovdiv, Bulgaria
- 10Environmental Health Division, Research Institute at Medical University of Plovdiv, Medical University of Plovdiv, Plovdiv, Bulgaria
- 11Institute of Highway Engineering and Transport Planning, Graz University of Technology, Graz, Austria
- 12Swinburne University of Technology, Hawthorn, VIC, Australia
- 13Department of Computational Diagnostic Radiology and Preventive Medicine, The University of Tokyo Hospital, Tokyo, Japan
- 14Department of Civil Engineering, University of Ottawa, Ottawa, ON, Canada
- 15Institute of Disaster Management, Khulna University Engineering & Technology, Khulna, Bangladesh
- 16Remote Sensing, Center for Environmental and Geographic Information Services (CEGIS), Dhaka, Bangladesh
- 17Department of Geography and Environment, Jagannath University, Dhaka, Bangladesh
- 18Faculty of Medicine, Aleppo University, Aleppo, Syria
- 19Green City Hospital, Kathmandu, Nepal
- 20Department of Microbiology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Dr. D. Y. Patil Vidyapeeth, Pune, India
- 21Faculty of Health Sciences, Universidad Cientifica del Sur, Lima, Peru
- 22Infectious and Tropical Diseases Service, Hospital Nacional Dos de Mayo, Lima, Peru
- 23Research Unit, Universidad Continental, Huancayo, Peru
- 24Grupo de Investigación Biomedicina, Faculty of Medicine, Fundación Universitaria Autónoma de las Américas-Institución Universitaria Visión de las Américas, Pereira, Colombia
- 25Gilbert and Rose-Marie Chagoury School of Medicine, Lebanese American University, Beirut, Lebanon
Introduction: The COVID-19 pandemic has had a significant impact on mental health globally, with limited access to mental health care affecting low- and middle-income countries (LMICs) the most. In response, alternative strategies to support mental health have been necessary, with access to green spaces being a potential solution. While studies have highlighted the role of green spaces in promoting mental health during pandemic lockdowns, few studies have focused on the role of green spaces in mental health recovery after lockdowns. This study investigated changes in green space access and associations with mental health recovery in Bangladesh and Egypt across the pandemic.
Methods: An online survey was conducted between January and April 2021 after the first lockdown was lifted in Bangladesh (n = 556) and Egypt (n = 660). We evaluated indoor and outdoor greenery, including the number of household plants, window views, and duration of outdoor visits. The quantity of greenness was estimated using the normalized difference vegetation index (NDVI). This index was estimated using satellite images with a resolution of 10x10m during the survey period (January-April 2021) with Sentinel-2 satellite in the Google Earth Engine platform. We calculated averages within 250m, 300m, 500m and 1000m buffers of the survey check-in locations using ArcGIS 10.3. Multiple linear regression models were used to evaluate relationships between changes in natural exposure and changes in mental health.
Results: The results showed that mental health improved in both countries after the lockdown period. People in both countries increased their time spent outdoors in green spaces after the lockdown period, and these increases in time outdoors were associated with improved mental health. Unexpectedly, changes in the number of indoor plants after the lockdown period were associated with contrasting mental health outcomes; more plants translated to increased anxiety and decreased depression. Refocusing lives after the pandemic on areas other than maintaining indoor plants may assist with worrying and feeling panicked. Still, indoor plants may assist with depressive symptoms for people remaining isolated.
Conclusion: These findings have important implications for policymakers and urban planners in LMICs, highlighting the need to increase access to natural environments in urban areas to improve mental health and well-being in public health emergencies.
1 Introduction
The COVID-19 pandemic originated in Wuhan, China, in December 2019 and rapidly became a global crisis. On March 11, 2020, the World Health Organization declared it a pandemic due to its rapid transmission (1). By March 15, 2023, it had infected over 681 million people and resulted in 6.8 million deaths worldwide (2). To contain the viral spread, governments implemented various measures such as lockdowns, curfews, quarantines, and other non-pharmaceutical interventions (3). The Bangladesh government imposed a complete lockdown on March 26, 2020 and continued till May 31, 2020 (4), followed by zonal lockdowns from June 20, 2020 to July 9, 2020 (5). Similarly, Egypt implemented a nationwide lockdown from March 25 to June 27, 2020 (6). With no vaccine and limited understanding of the virus, these forms of social distancing were considered the most effective method of prevention and regulation during some periods of the pandemic (3, 7). However, such restrictions had profound consequences, affecting daily life, economies, and health, leaving many uncertain about the pandemic’s duration and the prospect of gaining control over it (8).
Correspondingly, the pandemic had substantial negative impacts on mental health worldwide, with numerous studies highlighting the harmful effects of social isolation and lockdowns on mental health (9–14). The pandemic led to increased symptoms of depression, anxiety, post-traumatic stress disorder (PTSD), distress, and insomnia (15). One review concluded that over 95% of people reported PTSD symptoms, 72% reported distress, 45% reported anxiety symptoms, and 34% reported insomnia during the pandemic (16). Such impacts were particularly acute in low- and middle-income countries (LMICs) due to their limited access to mental health care (17). A meta-analysis of 40 developing countries reported that distress (29%) and depression (27%) were the most prevalent mental health symptoms during COVID-19 (18).
Research on exposure to green spaces and benefits to mental health has gained attention from researchers and healthcare professionals in recent years. The stress reduction theory suggests that green spaces can induce a sense of emotional well-being and a calming effect on individuals (19). Thus, exposure to green spaces can promote relaxation and stress reduction. Further, attention restoration could be another established theory that suggests attention restoration in green space is associated with improved psychological well-being, including reduced symptoms of depression and anxiety (19). Earlier studies have shown that exposure to green spaces can have positive impacts on mental health, reducing symptoms of anxiety and depression, as well as promoting overall well-being (20–22). Green spaces have also played an essential role in alleviating the negative mental health burden during the COVID-19 lockdown (23, 24). A study in Spain reported individuals turned to green spaces as a source of comfort, both directly and indirectly, to alleviate the negative effects of the pandemic (25). A study in Bulgaria showed that visible access to the greenery around the home and neighborhood was associated with decreased symptoms of depression and anxiety during the pandemic (26). Window views of greenery have been found to provide micro-restorative episodes that aid in healing, psychological regeneration, and rehabilitation from traumatic events (27), including during lockdowns (26). A study from Italy reported greener views and access to private green spaces were associated with better mental health outcomes (28).
While the mental health benefits of urban green spaces are well understood in high-income countries (HICs) (29–31), the evidence does not represent the diversity of urban living conditions in rapidly urbanizing LMICs. The existing evidence largely excludes the types of urban environments where most of the world’s population lives (32). Consequently, researchers and policymakers should avoid assuming that findings from HICs can be automatically applied to LMICs, given the diverse urban conditions and environmental and cultural differences between these countries (33). Informal settlements and slums often characterize cities in LMICs, and people living in these areas may not have the same level of access to green space as those in more affluent areas (32). This lack of access to green space in low-income cities may have different impacts on mental health than in HIC cities, where the availability and quality of green space may differ. To date, few studies have focused on the association between green space exposure and mental health in LMICs (34). A spatial epidemiological study conducted in Bangladesh (a tropical climate) found a negative correlation between vegetation and psychological well-being (35). A study in India (a sub-tropical climate) found a positive association between lack of park access and depression (36).
Furthermore, a study in Egypt (a hot and dry climate) focused on the impact of the green space on people’s happiness (37). This existing literature shows contrasting findings before the pandemic and does not inform the role of green spaces in mental health during the pandemic. We know only one study that answers this literature gap: spending time in a home garden was associated with less anxiety and stress during the COVID-19 lockdown in India (38).
Further limiting our understanding of green space exposure and mental health during the pandemic is the limited research comparing associations during and after lockdowns. The importance of green spaces during lockdowns has been widely recognized (26–28). The green space’s role in mental health recovery after lockdowns may be equally important. As the world continues to navigate through the pandemic’s aftermath, policymakers and mental health professionals must focus on developing effective interventions and policies to support mental health recovery. The focus of the current study is to examine exposure to green spaces and mental health recovery following lockdowns in two LMICs. The two countries represent radically different climates, with Bangladesh being tropical and Egypt being deserts (39). This distinction allows for exploring how access to nature and its impact on mental health may differ in different climate zones, which is essential in developing targeted interventions for LMICs. Our primary research question (RQ) included: How were changes in nature access associated with recovery from poor mental health after lockdowns? By emphasizing the recovery phase of the pandemic, we sought to complement existing research, which primarily focused on the immediate effects of the pandemic (23, 40).
2 Materials and methods
2.1 Study design
A retrospective study design was adopted to conduct the study. Online surveys were administered between January and April 2021, when lockdowns were lifted and people were getting used to the ‘new normal’ of the pandemic in Bangladesh and Egypt. The survey used a free version of an online survey platform, KoBoToolbox,1 allowing the survey to be distributed and completed without face-to-face interaction. The target population was the general people aged 18 and above. We used a snowball sampling approach and distributed the invitations through email and various social media platforms (e.g., Facebook, WhatsApp, LinkedIn). Participants were informed about the study and allowed to withdraw at any time. A total of 1,216 respondents (556 from Bangladesh and 660 from Egypt) were included in the analysis.
The survey consisted of six sections. These included socio-demographic information, potential risk factors, potential mediators, perceived exposure to indoor and outdoor nature, and self-reported mental health. Respondents were asked to provide data for two time points: the period of lockdown during the pandemic and the post-lockdown period (the current time of the survey administration). The survey also collected the geolocation of the participants, which was used to calculate objective greenness levels at both periods. The survey form was written in English and translated into local languages. The research was approved by the ethics committee of the Institute of Disaster Management, Khulna University of Engineering and Technology, Khulna, Bangladesh and the Psychology Department, Faculty of Arts, Menoufia University, Egypt.
2.2 Nature exposure measures
2.2.1 Perceptions
We adopted two measures for perceived indoor nature exposure: the number of household plants and window views (41). The first was measured by asking, “How many indoor plants are in this home?” Respondents answered it numerically (i.e., 0, 1, or 2 plants). The second was measured by asking about the visibility of 13 built or natural spaces/elements through any of the windows of their residence. Respondents scored these as present or absent, providing binary measures for each type. The spaces/elements included industrial building(s), courtyard/housing block patio, urban area (houses and streets), road, park(s), river(s), lake(s), agricultural area(s), countryside, woodland(s)/forest, hill(s)/mountain(s), and little access to outdoor visual elements because of neighbor’s walls or no window views. Responses were categorized as natural (park, river, lake, agriculture, countryside, woodland/forest, hill/mountain), built (industrial buildings, houses and street, road, neighbors wall), or mixed (at least one item in the natural category and at least one in the built category). Respondents indicated their perceived indoor nature exposure during the lockdown and at the current time.
We measured perceived outdoor nature exposure with two items: spaces accessed outdoors and hours spent outdoors. Spaces accessed outdoors were asked first and included responses for during the lockdown (“Which outdoor spaces did you have physical access to during the COVID-19 lockdown?”) and current time (“Which outdoor green spaces have you visited in the last four weeks?”). Time spent outdoors was also asked for these two-time points and was measured by asking, ‘How many hours did you spend each day at the places you visited, on average?’ If participants spent time at two or more outdoor spaces, they were requested to provide the total average number of hours per day for all those spaces. Duration was scored on a 4-point scale: <1 h, 1–2 h, 3–5 h, and > 5 h, following a previous study (42). Because of slight differences in how the survey was administered between countries, we could not use the data from the spaces accessed outdoors in analyses. Our perceived outdoor nature exposure was limited to total time outdoors during the lockdown and current time.
2.2.2 Objective greenness
To measure the quantity of greenness, we initially considered three metrics: the normalized difference vegetation index (NDVI), enhanced vegetation index (EVI), and soil-adjusted vegetation index (SAVI). NDVI is a remote sensing index used to estimate vegetation cover and productivity. It is based on the difference in reflectance between the near-infrared (NIR) and red (RED) bands of electromagnetic radiation. The result of the NDVI calculation ranges from −1 to 1, with higher values indicating more excellent vegetation cover and productivity (43). EVI is similar to NDVI but was designed to reduce the influences of atmospheric and soil noise on the vegetation signal. We considered EVI since it can be an appropriate measure in regions with high atmospheric aerosol content, such as deserts, which may influence NDVI. SAVI corrects for the influence of soil brightness on the vegetation signal and is also particularly useful in regions with high soil brightness, such as deserts and semi-arid regions (44). These indices were estimated using satellite images with a resolution of 10 × 10m during the survey period (January–April 2021) with Sentinel-2 satellite in the Google Earth Engine platform. We calculated averages within 250 m, 300 m, 500 m and 1,000 m buffers of the survey check-in locations using ArcGIS 10.3 (Esri, Redlands, CA, United States). NDVI and EVI values were highly correlated, r = 0.68 to 1.0 (Supplementary Figure S1), and there were no changes between the lockdown and the current time in SAVI. For these reasons, NDVI was chosen for analysis. NDVI values across buffer sizes were also highly correlated r = 0.88 to 0.96 (Supplementary Figure S1), and 500 m was selected to correspond to the previous nature and health research (45).
2.3 Mental health measures
Several scales are generally accepted to measure mental health, including the 7-item Generalized Anxiety Disorder (GAD-7) scale, 9-item Patient Health Questionnaire (PHQ-9), and 4-item Patient Health Questionnaire (PHQ-4) to evaluate mental health (46–48). To keep the questionnaire brief, we used the 2-item Patient Health Questionnaire (PHQ-2) and 2-item General Anxiety Disorder (GAD-2) to measure depression and anxiety disorder, respectively. GAD-2 evaluated the frequency of participants feeling nervous, anxious, or on edge and unable to stop or control worrying over the last two weeks in lockdown and the current period (49). PHQ-2 rated the frequency of feeling down, depressed, or hopeless and having little interest or pleasure in doing things over the past two weeks for the same period (50). The response options were on 4-point Likert scales: 0 (not at all), 1 (several days), 2 (more than half of the day), and 3 (almost every day). The total score ranges from 0 to 6, with a cut-off value of ≥3 indicating a higher risk of anxiety and depression.
2.4 Covariates
We assessed socio-demographic variables, potential risk factors, and household characteristics that might affect mental health outcomes. Based on previous research (51, 52), we asked about gender, age, marital status, and family income in local currency (BDT and Egyptian pound) converted to USD (0–100, 101–200, 201–400, and > 400 USD). We also evaluated past COVID-19 diagnoses of respondents and their family members, providing four options: tested positive at least once, tested negative and never tested further positive, never tested, or at least one of the family members tested positive for COVID-19. We asked whether respondents had a chronic physical illness since these can influence mental health (53) and green space use (54). Two potential risk factors were also measured, including habit of smoking and body mass index (BMI). Smoking can have negative impacts on mental health (27), and BMI can influence quality of life (55).
2.5 Analysis
In this study, both the exposure and outcome variables were assessed at two-time points, allowing us to capture changes and developments over time in response to the intervention or exposure. In contrast, covariates, including socio-demographic and health-related variables, were collected at a single point in time. This design was chosen to examine how changes in exposure levels corresponded to changes in the outcome variables and whether socio-demographic characteristics influenced these changes. We compared the lockdown and current time values for all variables. These were tested with chi-square values of independence for count variables and paired sample t-tests for continuous variables. Next, we compared change scores for all variables between the countries using chi-squared tests and independent sample t-tests. Change scores were calculated as the current time value minus the lockdown period value.
Multiple linear regression models were used to assess associations between changes in mental health and changes in natural exposure. Separate models were run for anxiety and depression in each country. Bangladesh models included socio-demographic variables, potential risk factors, household characteristics, COVID-19 diagnosis, changes in the number of indoor plants, changes in window views of nature, changes in time spent outdoors, and greenness (NDVI-500). Models showed no evidence of multicollinearity, as demonstrated by variance inflation factor (VIF) values ≤2.5 and pairwise correlation values ≤0.7 (Supplementary Table S2). Normality tests on outcome variables were performed using Skewness and Kurtosis with a critical value of 3.0 and a visual inspection of histograms (Supplementary Table S3). The outcome values of depression and anxiety were distributed normally. All analyses were conducted with SPSS v21 (IBM, Armonk, New York) with an alpha set for significance at p < 0.05.
3 Results
3.1 Descriptive statistics
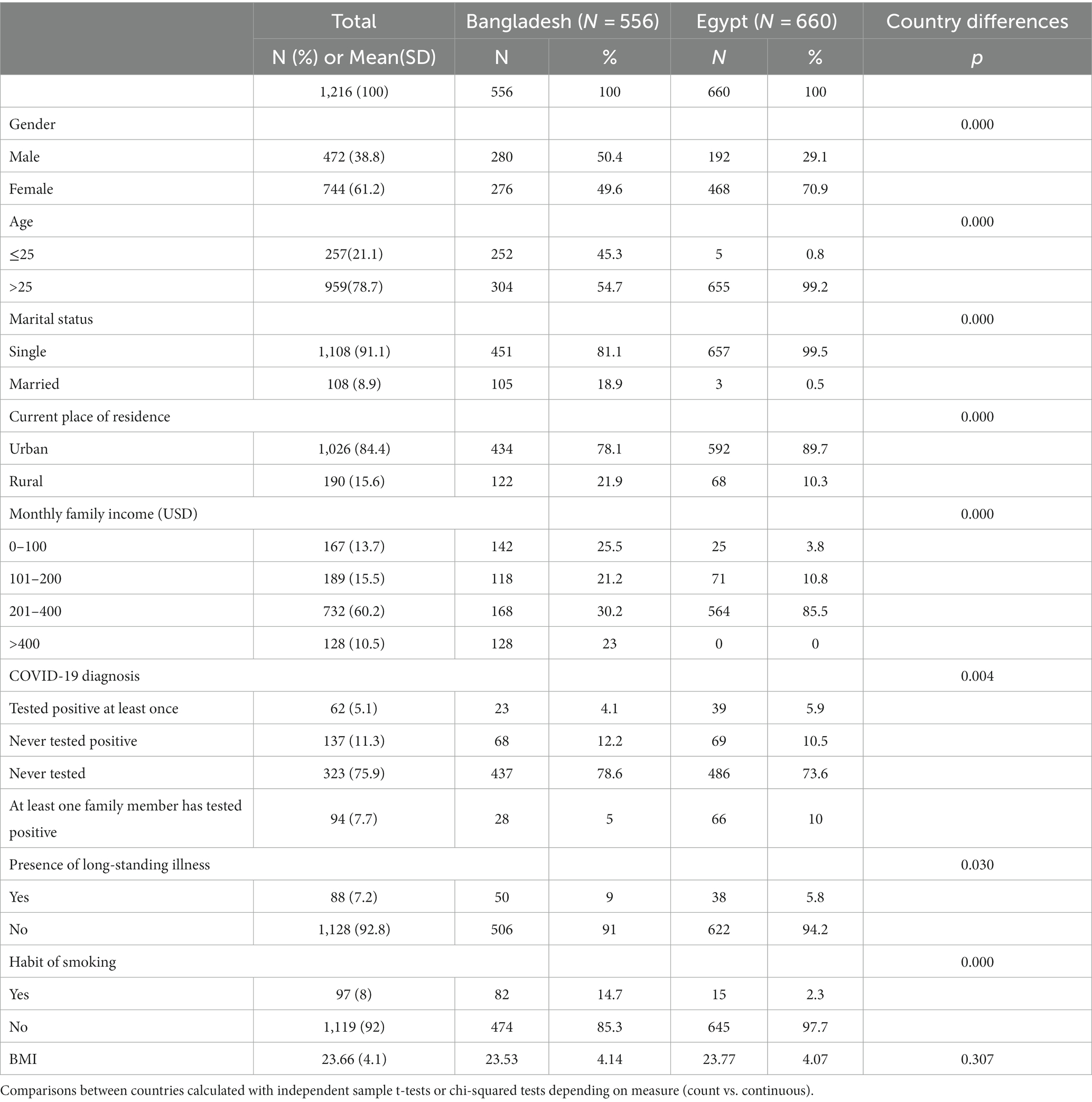
The characteristics of respondents are provided in Table 1. Most were female, aged >25 years, single, lived in an urban area, and reported a monthly family income between 201 and 400 USD. Most also reported they never tested for COVID-19 and did not have a long-standing illness or habit of smoking. Egypt respondents were more likely to be female, over 25, single, urban residents, and earning monthly incomes of 201–400 USD. The proportion of respondents who had never been tested for COVID-19 was higher in Bangladesh than in Egypt. In comparison, the proportion of respondents without a long-term illness or habit of smoking was higher in Egypt than in Bangladesh.
3.2 Changes in mental health and nature exposure
Anxiety and depression levels decreased in Bangladesh and Egypt from the lockdown to the current time (Figure 1, Supplementary Table S1). Bangladesh witnessed more substantial decreases in depression than Egypt. No between-country differences were seen for decreases in anxiety.
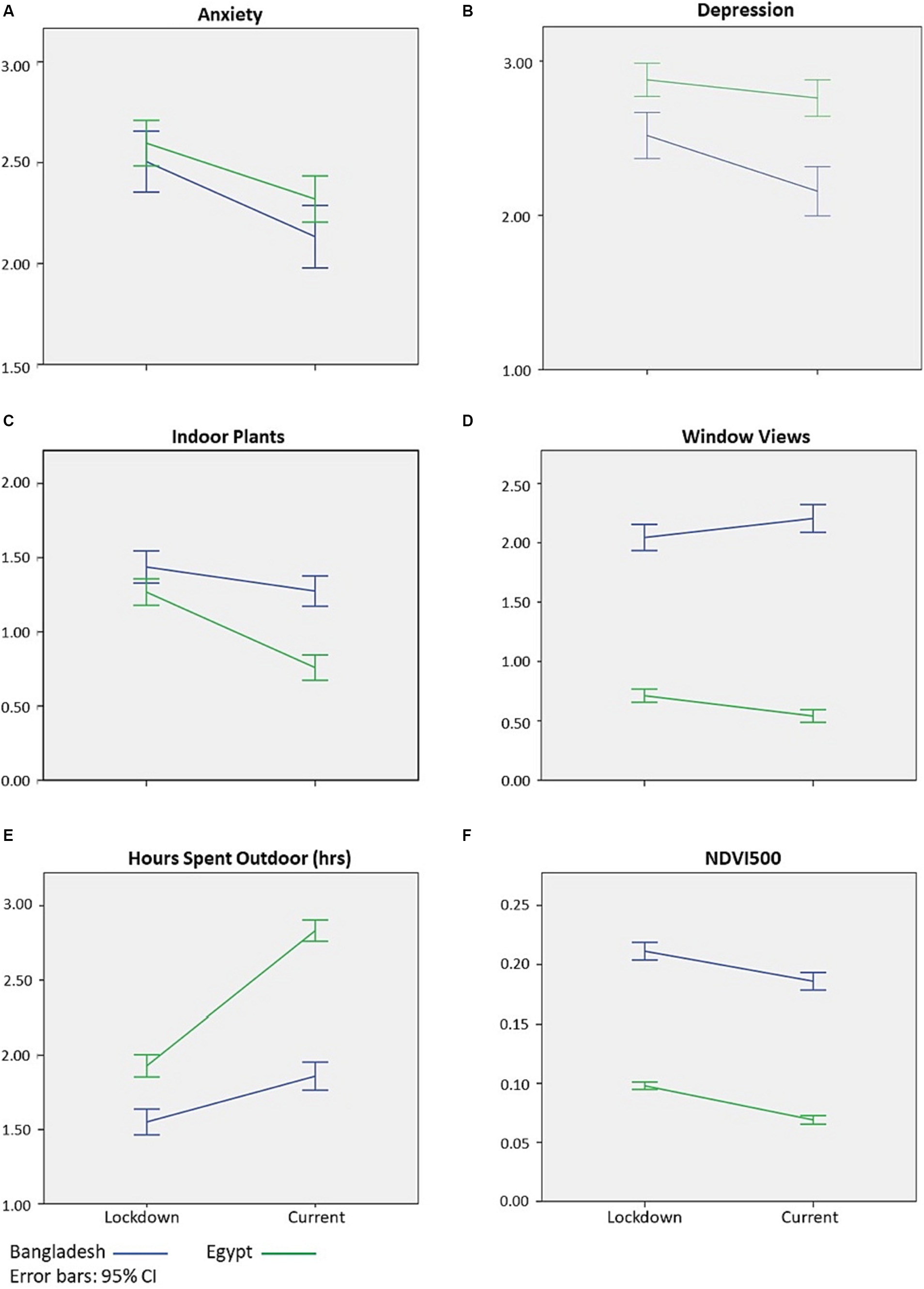
Figure 1. Changes in mental health (A,B), perceived nature exposure (C–E), and greenness (F) from the COVID-19 lockdown period to the current time in Bangladesh and Egypt (N = 1,216). CI, confidence intervals; NDVI500, normalized difference vegetation index within a 500 m buffer of survey respondent, hrs = hours.
Nature access changed from the lockdown to the current time with varying patterns. In both countries, hours spent outdoors increased while indoor plants decreased. Window views of nature increased in Bangladesh but decreased in Egypt. Greenness also increased in Bangladesh but decreased in Egypt.
3.3 Associations between changes in mental health and natural exposure
Changes in natural exposure partially corresponded with changes in mental health (Table 2, 3). In Bangladesh, increased outdoor time was associated with decreased anxiety and depression. In Egypt, a increase in the number of indoor plants was associated with increased anxiety but decreased depression. No other changes in natural exposure predicted changes in mental health. Overall, models of nature exposure, socio-demographic variables, potential risk factors, household characteristics, and COVID-19 diagnosis poorly explained changes in anxiety and depression. Variance explained ranged from 3% for depression to 5% for anxiety in Egypt models. The variance explained was greater in Bangladesh models, ranging from 7% for depression to 9% for anxiety.
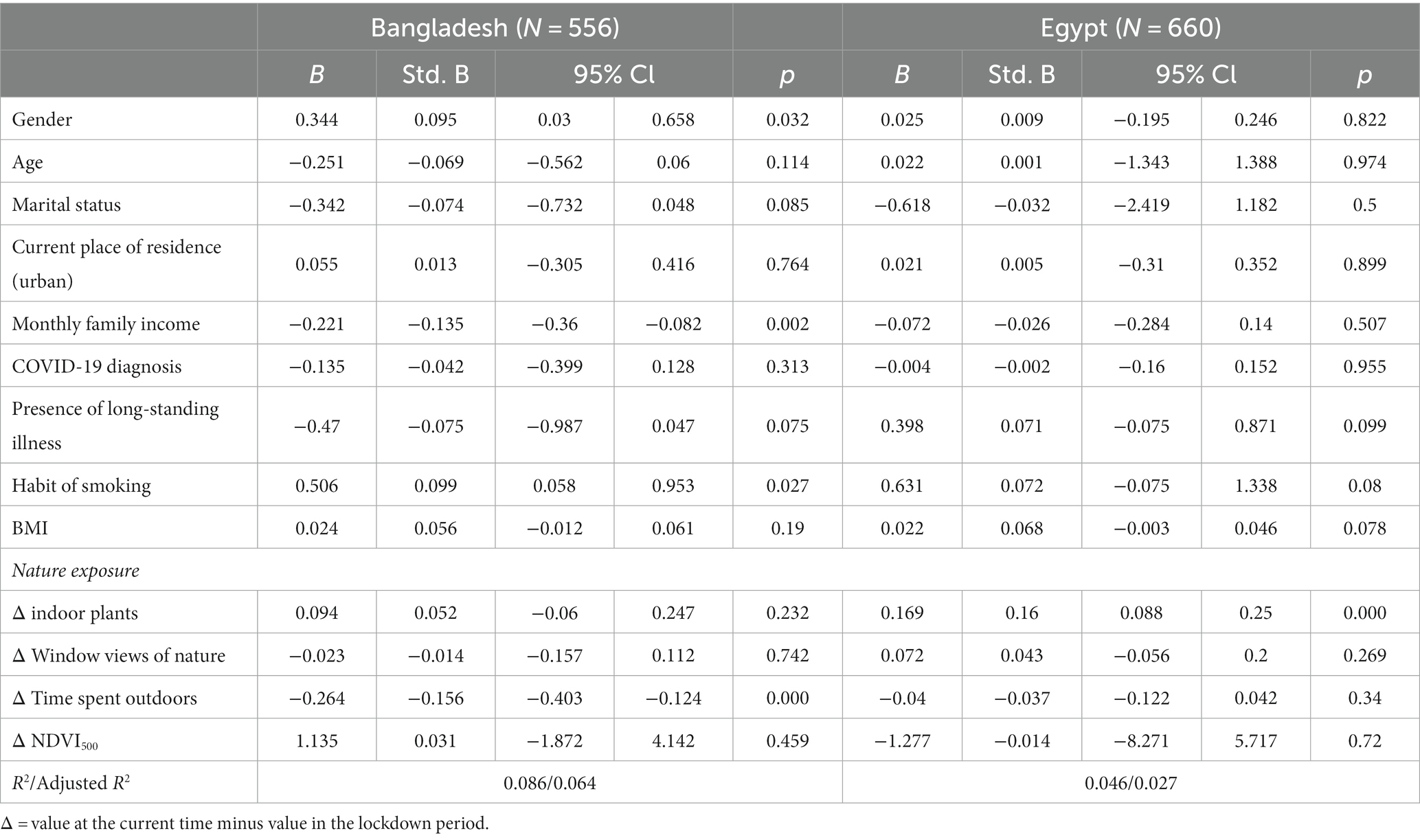
Table 2. Associations between changes in anxiety and nature exposure from the COVID-19 lockdown to the current time in Bangladesh and Egypt (N = 1,216).

Table 3. Associations between changes in depression and nature exposure from the COVID-19 lockdown to the current time in Bangladesh and Egypt (N = 1,216).
4 Discussion
4.1 Summary of main findings
The COVID-19 pandemic had a significant impact on people’s mental health. In LMICs, where access to mental health care is often limited, it is essential to identify alternative strategies to support mental health during these challenging times (17). One such strategy is access to nature, which has numerous mental health benefits (56, 57). However, the extent to which people in LMICs had access to nature and how such exposure influenced mental health recovery across the pandemic remains unclear.
This study investigated changes in nature exposure and associations with changes in mental health in two LMICs. Results showed that mental health improved in Egypt and Bangladesh after lockdowns. In addition, residents of both countries increased their time spent outdoors after lockdowns, and these changes were associated with reductions in anxiety and depression in Bangladesh. Changes in nature exposure were not associated with mental health recovery in Egypt, except that increase in the number of indoor plants were unexpectedly associated with increased anxiety but decreased depression. The study’s focus on mental health recovery aligns with the current global situation of most countries transitioning out of response to recovery. Therefore, the current study’s findings provide insights into how nature exposure might continue to support recovery from poor mental health during the pandemic in LMICs.
The observed decreases in anxiety and depression after lockdowns have been documented in other contexts. For instance, an Italian study showed relief from psychological distress and symptoms after the pandemic (58). The relaxation of lockdown measures may have reduced social isolation, increased social support, and more significant opportunities for engagement in recreational activities (59). Additionally, reducing COVID-19 cases and deaths may have reduced anxiety about the virus and its impact on health (60). While there is a lack of previous studies comparing green space use or access and associations with mental health in LMICs, findings from cross-country studies shed light on the observed differences between Egypt and Bangladesh. Ribeiro et al. (61)examined the relationship between nature exposure and mental health outcomes during the pandemic in Spain and Portugal. They are engaging with natural environments, whether in public or private green spaces, during lockdown periods positively reduced stress and improved mental well-being. Research before the pandemic identified differences between LMICs concerning perceived safety, preferred amenities, and the impact of climate on green space use (62). Considering this body of evidence, it is reasonable to attribute the differences in mental health recovery between Egypt and Bangladesh to various factors, such as variations in the study samples, severity of lockdown measures, cultural approaches to coping mechanisms, and mental health services.
We found that residents in both countries increased their time outdoors after lockdowns, likely due to lockdowns restricting people’s outdoor access. These changes may have led to a greater appreciation of the benefits of spending time in nature and motivated spending time outdoors (63). Similar findings have been seen in Scotland, where 80% of adults visited nature outdoors at least once a week after lockdowns, whereas 71% visited nature outdoors during the initial lockdown period (64). A study in Norway reported that there was a shift from residential and commercial zones toward city green spaces, including forests and protected areas after the lockdown was lifted, indicating a growing interest in nature access among the public during the post-lockdown time (65).
We also found that residents decreased the number of indoor plants after lockdowns, possibly due to shifts in focus from indoor to outdoor spaces. As lockdowns lifted, people may have experienced a greater appreciation for spending time outdoors in natural environments. The restricted mobility and confinement indoors during the lockdown period could have intensified people’s longing for open spaces and green surroundings. This newfound or reinvigorated appreciation for outdoor spaces might have led individuals to prioritize spending time outside rather than investing effort in maintaining indoor plants (66), which may have led to a decrease in their interest in keeping and maintaining indoor plants.
Increased time outdoors after lockdowns being associated with reduced anxiety and depression in Bangladesh aligns with earlier research. Spending time in green space can lead to numerous mental health benefits for mental health, including reduced symptoms of anxiety and depression before the pandemic (56, 57) and during it (38, 67). For instance, Beyer et al. (68) reported that time spent outdoors was negatively associated with depression (68), and Lesser and Nienhuis (69) found that inactive adults who spent more time outdoors during the pandemic experienced greater well-being (69). A study in Austria during the pandemic reported that spending time outdoors was associated with better mental health (70). Collectively, these findings can be explained by the biophilia hypothesis, which posits that humans have an innate connection to nature and that exposure to natural environments can positively impact mental health (71, 72). During lockdowns, people were restricted from going outdoors and connecting with nature. As restrictions lifted, people could spend more time outside and engage in outdoor activities (65). This increased exposure to nature may have contributed to the decrease in anxiety and depression.
Unexpectedly, our study found that increases in indoor plants were associated with increased anxiety and decreased depression in Egypt. Previous research suggests indoor plants positively affect mental health and well-being (28, 73). Residents who spent more time outdoors, engaging in recreational activities, and less time indoors after lockdowns may have felt less worried or panicked (66). In contrast, residents with more indoor plants could have continued indoor pursuits without these specific benefits derived from being outdoors but still felt less depressed while being isolated.
4.2 Study limitations
Several limitations to this study should be considered when interpreting the results. First, we used a retrospective study design with a single time point but repeated measures. Retrospective self-reported information on nature exposure and mental health during lockdowns may have been inaccurate. Participants may have underreported access and symptoms due to social desirability bias or other factors. This dataset also precluded us from establishing causal relationships between the variables. Second, we did not measure other potential factors that may have influenced the relationships between nature exposure and mental health. These factors include, but are not limited to, nature connection, types of recreational activities, quality of indoor living spaces, the therapeutic aspects of plant care, and the psychological impacts of isolation. Future studies should consider these elements for a more comprehensive understanding of the multifaceted relationship between nature exposure and mental well-being. Third, we did not explore the mechanisms underlying the relationships between nature access and mental health. Future research could examine the biological, psychological, and social pathways through which natural exposure may influence mental health recovery.
5 Conclusion
Residents in two LMICs increased their time outdoors in nature and saw improvements in their mental health after COVID-19 lockdowns. Increases in time outdoors were associated with mental health recovery in one country (Bangladesh). Decreases in the number of indoor plants were associated with contrasting mental health outcomes in the other country (Egypt). Access to outdoor nature exposure, but not necessarily having indoor plants and green window views, may assist with mental health recovery following public health crises. These findings can inform mental health interventions, especially in LMICs and during times of crisis like the COVID-19 pandemic. Encouraging individuals to spend more time outdoors in natural settings could be an effective and accessible strategy for promoting mental well-being. Further, this study underscores the need for further research into the relationship between nature exposure and mental health in LMICs, as well as the importance of incorporating these findings into educational programs for healthcare professionals, urban planners, and the general public.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by ethics committee of the Institute of Disaster Management, Khulna University of Engineering and Technology, Khulna, Bangladesh and Psychology Department, Faculty of Arts, Menoufia University, Egypt. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. MoB: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. Hİ: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. MaB: Conceptualization, Formal analysis, Investigation, Writing – review & editing. ASD: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. MHa: Formal analysis, Methodology, Writing – review & editing. MHe: Formal analysis, Methodology, Writing – review & editing. SA: Formal analysis, Investigation, Methodology, Writing – review & editing. AMD: Formal analysis, Investigation, Methodology, Writing – review & editing. FS: Formal analysis, Investigation, Methodology, Writing – review & editing. MAl: Formal analysis, Methodology, Writing – review & editing. SB: Formal analysis, Funding acquisition, Investigation, Methodology, Writing – review & editing. MK: Formal analysis, Funding acquisition, Investigation, Writing – review & editing. MHo: Data curation, Formal analysis, Investigation, Writing – review & editing. MAz: Formal analysis, Methodology, Writing – review & editing. MR: Data curation, Investigation, Methodology, Writing – review & editing. SS: Formal analysis, Methodology, Writing – review & editing. RS: Formal analysis, Methodology, Writing – review & editing. JM-I: Investigation, Methodology, Writing – review & editing. DB-A: Investigation, Methodology, Writing – review & editing. AR-M: Formal analysis, Investigation, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. AMD’s time on this publication is partially supported by the “Strategic Research and Innovation Program for the Development of Medical University – Plovdiv (SRIPD-MUP),” funded by the EU – NextGenerationEU, contract N° BG-RRP-2.004-0007-C01. The funding above source had no involvement in the study’s design, collection, analysis, interpretation of the data, writing of the report, nor in the decision to submit the manuscript for publication. Universidad Continental, Peru, covered the APC of this publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1334425/full#supplementary-material
Footnotes
References
1. Li, Q , Guan, X , Wu, P , Wang, X , Zhou, L , Tong, Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. (2020) 382:1199–07. doi: 10.1056/nejmoa2001316
2. Worldometer . Countries where coronavirus has spread - Worldometer. (2023). Available at: https://www.worldometers.info/coronavirus/countries-where-coronavirus-has-spread/ (Accessed March 15, 2023)
3. Haug, N , Geyrhofer, L , Londei, A , Dervic, E , Desvars-Larrive, A , Loreto, V, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. (2020) 4:1303–12. doi: 10.1038/s41562-020-01009-0
4. Mina, FB , Billah, M , Rahman, MS , Das, S , Karmakar, S , Hasan, MF, et al. COVID-19: transmission, diagnosis, policy intervention, and potential broader perspective on the rapidly evolving situation in Bangladesh. J Adv Biotechnol Exp Ther. (2020) 3:18–29. doi: 10.5455/JABET.2020.D152
5. Tabassum, T , Farzana, M , Nurun Nahar, A , Araf, Y , Ullah, A , Rahaman, TI, et al. COVID-19 in Bangladesh: wave-centric assessments and mitigation measures for future pandemics. Heliyon. (2023) 9:e20113. doi: 10.1016/j.heliyon.2023.e20113
6. Aly, M , AlMarzooqi, M , Mohamed, S , Alzahrani, TM , and Abdelkarim, O . Daily step counts before, during, and after COVID-19 pandemic: a smartphone-tracking study of university students in Egypt and Saudi Arabia. BMC Public Health. (2023) 23:1365. doi: 10.1186/s12889-023-16068-x
7. Alfano, V , and Ercolano, S . The efficacy of lockdown against COVID-19: A cross-country panel analysis. Appl Health Econ Health Policy. (2020) 18:509–17. doi: 10.1007/s40258-020-00596-3
8. Saladino, V , Algeri, D , and Auriemma, V . The psychological and social impact of Covid-19: new perspectives of well-being. Front Psychol. (2020) 11:684. doi: 10.3389/fpsyg.2020.577684
9. Singh, S , Roy, D , Sinha, K , Parveen, S , Sharma, G , and Joshi, G . Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
10. Patwary, MM , Bardhan, M , Disha, AS , Kabir, MP , Hossain, MR , Alam, MA, et al. Mental health status of university students and working professionals during the early stage of COVID-19 in Bangladesh. Int J Environ Res Public Health. (2022) 19:6834. doi: 10.3390/IJERPH19116834/S1
11. Cao, W , Fang, Z , Hou, G , Han, M , Xu, X , Dong, J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
12. Rossi, R , Socci, V , Talevi, D , Mensi, S , Niolu, C , Pacitti, F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psych. (2020) 11:790. doi: 10.3389/FPSYT.2020.00790/BIBTEX
13. Talevi, D , Socci, V , Carai, M , Carnaghi, G , Faleri, S , Trebbi, E, et al. Mental health outcomes of the covid-19 pandemic. Riv Psichiatr. (2020) 55:137–44. doi: 10.1708/3382.33569
14. Wang, C , Pan, R , Wan, X , Tan, Y , Xu, L , Ho, CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
15. Huang, Y , and Zhao, N . Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. (2020) 288:112954. doi: 10.1016/j.psychres.2020.112954
16. Vindegaard, N , and Benros, ME . COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
17. Kumar, M , and Kumar, P . Impact of pandemic on mental health in lower- and middle-income countries (LMICs). Glob Ment Heal. (2020) 7:e35. doi: 10.1017/gmh.2020.28
18. Chen, J , Zhang, SX , Yin, A , Yáñez, JA , and Wiener, N . Mental health symptoms during the COVID-19 pandemic in developing countries: a systematic review and meta-analysis (2022) 12:5011. doi: 10.7189/jogh.12.05011
19. Lei, L . The effect of neighborhood context on children’s academic achievement in China: exploring mediating mechanisms. Soc Sci Res. (2018) 72:240–57. doi: 10.1016/j.ssresearch.2018.03.002
20. Barnes, MR , Donahue, ML , Keeler, BL , Shorb, CM , Mohtadi, TZ , and Shelby, LJ . Characterizing nature and participant experience in studies of nature exposure for positive mental health an integrative review. Front Psychol. (2019) 9:617. doi: 10.3389/fpsyg.2018.02617
21. Liu, H , Nong, H , Ren, H , and Liu, K . The effect of nature exposure, nature connectedness on mental well-being and ill-being in a general Chinese population. Landsc Urban Plan. (2022) 222:104397. doi: 10.1016/j.landurbplan.2022.104397
22. Mizen, A , Song, J , Fry, R , Akbari, A , Berridge, D , Parker, SC, et al. Longitudinal access and exposure to green-blue spaces and individual-level mental health and well-being: protocol for a longitudinal, population-wide record-linked natural experiment. BMJ Open. (2019) 9:e027289. doi: 10.1136/bmjopen-2018-027289
23. Labib, SM , Browning, MHEM , Rigolon, A , Helbich, M , and James, P . Nature’s contributions in coping with a pandemic in the 21st century: a narrative review of evidence during COVID-19. Sci Total Environ. (2022) 833:155095. doi: 10.1016/J.SCITOTENV.2022.155095
24. Patwary, MM , Bardhan, M , Safia Disha, A , Dzhambov, AM , Parkinson, CEM , Browning, MH, et al. Nature exposure and mental health during the COVID-19 pandemic: a navigation guide systematic review with meta-analysis (2023). doi: 10.32942/X2588Z,
25. Pouso, S , Borja, Á , Fleming, LE , Gómez-Baggethun, E , White, MP , and Uyarra, MC . Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Sci Total Environ. (2021) 756:143984. doi: 10.1016/j.scitotenv.2020.143984
26. Dzhambov, AM , Lercher, P , Browning, MM , Stoyanov, D , Petrova, N , Novakov, S, et al. Does greenery experienced indoors and outdoors provide an escape and support mental health during the COVID-19 quarantine? Environ Res. (2021) 196:110420. doi: 10.1016/j.envres.2020.110420
27. Soga, M , Evans, MJ , Tsuchiya, K , Fukano, Y , Soga, M , Evans, MJ, et al. A room with a green view: the importance of nearby nature for mental health during the COVID-19 pandemic. Ecol Appl. (2020) 31:e2248. doi: 10.1002/eap.2248
28. Spano, G , D’Este, M , Giannico, V , Elia, M , Cassibba, R , Lafortezza, R, et al. Association between indoor-outdoor green features and psychological health during the COVID-19 lockdown in Italy: A cross-sectional nationwide study. Urban For Urban Green. (2021) 62:127156. doi: 10.1016/j.ufug.2021.127156
29. Li, A , Mansour, A , and Bentley, R . Green and blue spaces, COVID-19 lockdowns, and mental health: an Australian population-based longitudinal analysis. Heal Place. (2023) 83:103103. doi: 10.1016/j.healthplace.2023.103103
30. Lee, KO , Mai, KM , and Park, S . Green space accessibility helps buffer declined mental health during the COVID-19 pandemic: evidence from big data in the United Kingdom. Nat Ment Heal. (2023) 1:124–34. doi: 10.1038/s44220-023-00018-y
31. Maury-Mora, M , Gómez-Villarino, MT , and Varela-Martínez, C . Urban green spaces and stress during COVID-19 lockdown: A case study for the city of Madrid. Urban For Urban Green. (2022) 69. doi: 10.1016/j.ufug.2022.127492
32. United Nations . Slum Almanac 2015–2016. (2015). Available at: https://unhabitat.org/slum-almanac-2015-2016-0 (Accessed March 22, 2023).
33. Markevych, I , Schoierer, J , Hartig, T , Chudnovsky, A , Hystad, P , Dzhambov, AM, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. (2017) 158:301–17. doi: 10.1016/j.envres.2017.06.028
34. Nawrath, M , Guenat, S , Elsey, H , and Dallimer, M . Exploring uncharted territory: do urban greenspaces support mental health in low- and middle-income countries? Environ Res. (2021) 194:110625. doi: 10.1016/j.envres.2020.110625
35. Gruebner, O , Khan, MMH , Lautenbach, S , Müller, D , Kraemer, A , Lakes, T, et al. A spatial epidemiological analysis of self-rated mental health in the slums of Dhaka. Int J Health Geogr. (2011) 10:36. doi: 10.1186/1476-072X-10-36
36. Firdaus, G , and Ahmad, A . Temporal variation in risk factors and prevalence rate of depression in urban population: does the urban environment play a significant role? Int J Ment Health Promot. (2014) 16:279–88. doi: 10.1080/14623730.2014.931068
37. Kafafy, NA , and Fathy, HA . Assessing green spaces impact on people’s happiness in Cairo. Int J Dev Sustain. (2019) 8:30–47.
38. Basu, M , DasGupta, R , Kumar, P , and Dhyani, S . Home gardens moderate the relationship between Covid-19-induced stay-at-home orders and mental distress: a case study with urban residents of India. Environ Res Commun. (2021) 3:105002. doi: 10.1088/2515-7620/ac2ab2
39. WorldData . Climate comparison: Bangladesh/Egypt. (2023). Available at: https://www.worlddata.info/climate-comparison.php?r1=bangladesh&r2=egypt (Accessed March 21, 2023).
40. Zabini, F , Albanese, L , Becheri, FR , Gavazzi, G , Giganti, F , Giovanelli, F, et al. Comparative study of the restorative effects of Forest and urban videos during COVID-19 lockdown: intrinsic and benchmark values. Int J Environ Res Public Health. (2020) 17:8011. doi: 10.3390/ijerph17218011
41. Korpela, K , De Bloom, J , Sianoja, M , Pasanen, T , and Kinnunen, U . Nature at home and at work: naturally good? Links between window views, indoor plants, outdoor activities and employee well-being over one year. Landsc Urban Plan. (2017) 160:38–47. doi: 10.1016/j.landurbplan.2016.12.005
42. Van den Berg, M , Van Poppel, M , Van Kamp, I , Andrusaityte, S , Balseviciene, B , Cirach, M, et al. Visiting green space is associated with mental health and vitality: A cross-sectional study in four european cities. Heal Place. (2016) 38:8–15. doi: 10.1016/j.healthplace.2016.01.003
43. Leprieur, C , Kerr, YH , Mastorchio, S , and Meunier, JC . Monitoring vegetation cover across semi-arid regions: comparison of remote observations from various scales. Int J Remote Sens. (2000) 21:281–300. doi: 10.1080/014311600210830
44. Huete, AR . A soil-adjusted vegetation index (SAVI). Remote Sens Environ. (1988) 25:295–309. doi: 10.1016/0034-4257(88)90106-X
45. Labib, SM , Lindley, S , and Huck, JJ . Scale effects in remotely sensed greenspace metrics and how to mitigate them for environmental health exposure assessment. Comput Environ Urban Syst. (2020) 82:101501. doi: 10.1016/j.compenvurbsys.2020.101501
46. Kroenke, K , Spitzer, RL , and Williams, JBW . The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
47. Kroenke, K , Spitzer, RL , Williams, JBW , and Löwe, B . An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. (2009) 50:613–21. doi: 10.1016/S0033-3182(09)70864-3
48. Löwe, B , Decker, O , Müller, S , Brähler, E , Schellberg, D , Herzog, W, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
49. Kroenke, K , Spitzer, RL , Williams, JBW , Monahan, PO , and Lowe, B . Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
50. Kroenke, K , Spitzer, RL , and Williams, JBW . The patient health Questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
51. Zijlema, WL , Triguero-Mas, M , Smith, G , Cirach, M , Martinez, D , Dadvand, P, et al. The relationship between natural outdoor environments and cognitive functioning and its mediators. Environ Res. (2017) 155:268–75. doi: 10.1016/j.envres.2017.02.017
52. Wang, R , Yang, B , Yao, Y , Bloom, MS , Feng, Z , Yuan, Y, et al. Residential greenness, air pollution and psychological well-being among urban residents in Guangzhou, China. Sci Total Environ. (2020) 711:134843. doi: 10.1016/j.scitotenv.2019.134843
53. Moussavi, S , Chatterji, S , Verdes, E , Tandon, A , Patel, V , and Ustun, B . Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet. (2007) 370:851–8. doi: 10.1016/S0140-6736(07)61415-9
54. Labib, SM , Shuvo, FK , Browning, M , and Rigolon, A . Noncommunicable diseases, Park prescriptions, and urban green space use patterns in a global south context: the case of Dhaka, Bangladesh. Int J Environ Res Public Health. (2020) 17:3900. doi: 10.3390/ijerph17113900
55. Eddolls, WTB , McNarry, MA , Lester, L , Winn, CON , Stratton, G , and Mackintosh, KA . The association between physical activity, fitness and body mass index on mental well-being and quality of life in adolescents. Qual Life Res. (2018) 27:2313–20. doi: 10.1007/s11136-018-1915-3
56. White, MP , Alcock, I , Grellier, J , Wheeler, BW , Hartig, T , Warber, SL, et al. Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Sci Rep. (2019) 9:7730. doi: 10.1038/s41598-019-44097-3
57. Toda, MT , Riol, AA , Cirach, M , Estarlich, M , Fernández-Somoano, A , González-Safont, L, et al. Residential surrounding greenspaceand mental health in three Spanish areas. Int J Environ Res Public Health. (2020) 17:1–14. doi: 10.3390/ijerph17165670
58. Orfei, MD , Bossi, F , D’Arcangelo, S , Maggi, F , Lattanzi, N , Malizia, AP, et al. Mental health in the post-lockdown pandemic phase: relief or exacerbation of psychological distress? A cross-sectional study in the general population in Italy. Acta Psychol. (2022) 225:103555. doi: 10.1016/J.ACTPSY.2022.103555
59. Morse, KF , Fine, PA , and Friedlander, KJ . Creativity and leisure during COVID-19: examining the relationship between leisure activities, motivations, and psychological well-being. Front Psychol. (2021) 12:967. doi: 10.3389/fpsyg.2021.609967
60. Wang, C , Pan, R , Wan, X , Tan, Y , Xu, L , McIntyre, RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
61. Ribeiro, AI , Triguero-Mas, M , Santos, CJ , Gómez-Nieto, A , Cole, H , Anguelovski, I, et al. Exposure to nature and mental health outcomes during COVID-19 lockdown. A comparison between Portugal and Spain. Environ Int. (2021) 154:106664.
62. Rigolon, A , Browning, M , Lee, K , and Shin, S . Access to urban green space in cities of the global south: A systematic literature review. Urban Sci. (2018) 2:67. doi: 10.3390/urbansci2030067
63. Venter, ZS , Barton, DN , Gundersen, V , Figari, H , and Nowell, M . Urban nature in a time of crisis: recreational use of green space increases during the COVID-19 outbreak in Oslo, Norway. Environ Res Lett. (2020) 15:104075. doi: 10.1088/1748-9326/abb396
64. NatureScot . Outdoors and nature engagement sustained post-lockdown | NatureScot. (2020) https://www.nature.scot/outdoors-and-nature-engagement-sustained-post-lockdown (accessed March 16, 2023).
65. Venter, ZS , Barton, DN , Gundersen, V , Figari, H , and Nowell, MS . Back to nature: Norwegians sustain increased recreational use of urban green space months after the COVID-19 outbreak. Landsc Urban Plan. (2021) 214:104175. doi: 10.1016/j.landurbplan.2021.104175
66. Loebach, J , Rakow, DA , Meredith, G , and Shepley, MMC . Time outdoors in nature to improve staff well-being: examining changes in behaviors and motivations among university staff in the use of natural outdoor environments since the emergence of the COVID-19 pandemic. Front Psychol. (2022) 13:4109. doi: 10.3389/FPSYG.2022.869122/BIBTEX
67. Heo, S , Desai, MU , Lowe, SR , and Bell, ML . Impact of changed use of greenspace during covid-19 pandemic on depression and anxiety. Int J Environ Res Public Health. (2021) 18
68. Beyer, KMM , Szabo, A , and Nattinger, AB . Time spent outdoors, depressive symptoms, and variation by race and ethnicity. Am J Prev Med. (2016) 51:281–90. doi: 10.1016/j.amepre.2016.05.004
69. Lesser, IA , and Nienhuis, CP . The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health. (2020) 17:3899. doi: 10.3390/ijerph17113899
70. Haider, S , Smith, L , Markovic, L , Schuch, FB , Sadarangani, KP , Sanchez, GFL, et al. Associations between physical activity, sitting time, and time spent outdoors with mental health during the first COVID-19 lock down in Austria. Int J Environ Res Public Health. (2021) 18:9168. doi: 10.3390/ijerph18179168
71. Kellert, S , and Wilson, E . The biophilia hypothesis. (1995). Available at: https://books.google.com/books?hl=en&lr=&id=GAO8BwAAQBAJ&oi=fnd&pg=PP6&ots=pmuhKBHVv-&sig=_O2Le7GrwvaBJbuLS2HY4ix5060 (accessed March 21, 2023).
72. Ulrich, RS . Aesthetic and affective response to natural environment. Behav Nat Environ. (1983):85–25. doi: 10.1007/978-1-4613-3539-9_4
Keywords: green space exposure, NDVI, mental health, LMIC, COVID-19
Citation: Patwary MM, Bardhan M, İnan HE, Browning MHEM, Disha AS, Haque MZ, Helmy M, Ashraf S, Dzhambov AM, Shuvo FK, Alam MA, Billah SM, Kabir MP, Hossain MR, Azam MG, Rahman MM, Swed S, Sah R, Montenegro-Idrogo JJ, Bonilla-Aldana DK and Rodriguez-Morales AJ (2024) Exposure to urban green spaces and mental health during the COVID-19 pandemic: evidence from two low and lower-middle-income countries. Front. Public Health. 12:1334425. doi: 10.3389/fpubh.2024.1334425
Edited by:
Yuka Kotozaki, Iwate Medical University, JapanReviewed by:
Amir Raza, University of Arizona, United StatesAhmad Harakan, Muhammadiyah University of Makassar, Indonesia
Copyright © 2024 Patwary, Bardhan, İnan, Browning, Disha, Haque, Helmy, Ashraf, Dzhambov, Shuvo, Alam, Billah, Kabir, Hossain, Azam, Rahman, Swed, Sah, Montenegro-Idrogo, Bonilla-Aldana and Rodriguez-Morales. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: D. Katterine Bonilla-Aldana, ZGJvbmlsbGFAY29udGluZW50YWwuZWR1LnBl
 Muhammad Mainuddin Patwary
Muhammad Mainuddin Patwary Mondira Bardhan
Mondira Bardhan Hüseyin Ertan İnan
Hüseyin Ertan İnan Matthew H. E. M. Browning
Matthew H. E. M. Browning Asma Safia Disha
Asma Safia Disha Md. Zahidul Haque
Md. Zahidul Haque Mai Helmy
Mai Helmy Sadia Ashraf2
Sadia Ashraf2 Angel M. Dzhambov
Angel M. Dzhambov Faysal Kabir Shuvo
Faysal Kabir Shuvo Md. Ashraful Alam
Md. Ashraful Alam Sharif Mutasim Billah
Sharif Mutasim Billah Md. Pervez Kabir
Md. Pervez Kabir Md. Riad Hossain
Md. Riad Hossain Sarya Swed
Sarya Swed Ranjit Sah
Ranjit Sah D. Katterine Bonilla-Aldana
D. Katterine Bonilla-Aldana Alfonso J. Rodriguez-Morales
Alfonso J. Rodriguez-Morales