- 1Department of Midwifery, College of Health Science, Woldia University, Woldia, Ethiopia
- 2Department of Midwifery, College of Medicine and Health Science, Wollo University, Woldia, Ethiopia
Background: Effective breastfeeding techniques, which include proper attachment, positioning, and suckling, offer a range of benefits for both the mother and the infant. These techniques ensure efficient milk transfer, reduce the risk of infections, support optimal infant weight gain, enhance maternal comfort, and foster a strong emotional bond. This study aimed to identify the magnitude and factors associated with effective breastfeeding techniques among lactating women in the Legambo district of South Wollo, Ethiopia, in 2022.
Methods: A community-based cross-sectional study was conducted from September to November 2022. Samples were selected using a multi-stage sampling method from 18 wards (kebele). Data were collected using an interviewer-administered structured questionnaire and an observational checklist. The collected data were entered into Epi-Data and then exported to SPSS version 25.0 for analysis. Descriptive statistics and bivariate and multivariable logistic regression analyses were performed to identify the magnitude and associated factors. Variables with a p-value less than 0.05 on multivariable analysis were considered independent factors associated with the outcome variable.
Results: Six hundred and ten lactating women were included for observation and interviewed, resulting in a 96.2% response rate. The magnitude of effective breastfeeding technique practice was found to be 25.9% (95% CI: 22.47–29.57%). Factors associated with effective breastfeeding technique practice included being a working woman (AOR = 1.70; 95%CI: 1.07–2.72), age between 26 and 30 years (AOR = 0.37; 95%CI: 0.16–0.84), urban residence (AOR = 1.59; 95%CI: 1.06–2.39), initiating breastfeeding 1 to 2 h after birth (AOR = 0.27; 95%CI: 0.16–0.43), and initiating breastfeeding after 2 h of birth (AOR = 0.34; 95%CI: 0.17–0.67). Additionally, not receiving breastfeeding education (AOR = 0.46; 95%CI: 0.30–0.72) and experiencing current breast problems (AOR = 0.28; 95%CI: 0.28–0.75) were also found to have a significant association with effective breastfeeding technique practice.
Conclusion: Only one in four women demonstrated effective breastfeeding techniques, indicating that their practice was below the WHO’s recommendations. Therefore, it is crucial to consider the identified variables to improve the practice of effective breastfeeding techniques.
Introduction
Breastfeeding is the practice of feeding a child directly from the breast or through expressed milk by hand or with a pump (1, 2). It is a natural and essential practice that provides optimal nutrition and promotes the overall health and development of infants (1–3). The World Health Organization (WHO) and the Ethiopian Federal Ministry of Health recommend initiating breastfeeding within the first hour of a baby’s life and exclusively breastfeeding for the first 6 months. After 6 months, breastfeeding should be continued along with appropriate complementary feeding for up to 2 years and beyond (1, 2). Implementing these recommendations has the potential to prevent approximately 820,000 deaths of children under the age of 5 annually in low- and middle-income countries, where the burden of under-five mortality is high (4).
Breastfeeding has numerous short-term and long-term benefits for the mother and the child. It decreases the risk of infection, sudden infant death syndrome, asthma, food allergies, and diabetes for the baby while also improving cognitive development and decreasing the risk of obesity in adulthood (4–6). For the mother, breastfeeding offers benefits such as a decrease in postpartum hemorrhage, depression, and facilitation of involution. In the end, it also reduces the risk of breast cancer, cardiovascular disease, diabetes, metabolic syndrome, and rheumatoid arthritis (6–8).
Effective breastfeeding technique is a process of breastfeeding that occurs when the baby and mother show readiness for it, and the baby is appropriately positioned, has good attachment, and has good suckling (9, 10). Effective breastfeeding techniques are essential for women to feed their babies without pain, in a simple, safe, and time-saving manner (9). Proper attachment, positioning, and suckling during breastfeeding offer a range of benefits for both the mother and the infant. These components ensure efficient milk transfer, prevent nipple soreness and discomfort, reduce the risk of infections, support optimal infant weight gain, and enhance maternal comfort (10, 11).
Furthermore, practicing effective breastfeeding techniques fosters a strong emotional bond between the mother and the baby (9). Physical closeness, eye contact, and skin-to-skin contact during breastfeeding stimulate the release of oxytocin, a hormone that promotes feelings of love, nurturing, and attachment. This bonding experience contributes to the emotional wellbeing of both the mother and the infant (12). Emphasizing and supporting this aspect of breastfeeding is crucial to enhance successful breastfeeding outcomes and improve the overall health and wellbeing of both the mother and infant (10–12).
Promoting effective breastfeeding practices is of utmost importance in Ethiopia, where infant mortality rates remain a significant concern. However, there is a notable disparity in the prevalence and factors associated with effective breastfeeding techniques among different populations. Furthermore, most previous studies have been conducted in institutional settings. Therefore, this study aims to bridge these gaps by investigating the magnitude and factors associated with effective breastfeeding among lactating women in the Legambo district of South Wollo, Ethiopia, in 2022. The findings from this study will provide valuable insights to develop targeted interventions aimed at improving breastfeeding outcomes and enhancing the overall health and wellbeing of both mothers and infants, reducing healthcare costs, and fostering a sustainable environment in the region.
Materials and methods
Study setting
A community-based cross-sectional study was conducted in Legambo District, South Wollo Zone, from September to November 2022. The district is situated 450 km away from Bahir Dar, the capital city of the Amhara region, and 601 km from Addis Ababa, the capital city of Ethiopia. Legambo District comprises 41 wards, of which 38 are rural wards (kebeles) and three are urban wards. The district is equipped with 1 general hospital, 9 health centers, and 39 health posts (13).
Study population
The study included all lactating women who had given birth in the past 6 weeks and were living in selected wards of the district.
Eligibility criteria
All postnatal women who were breastfeeding during the study period were included. However, mothers of infants with serious illnesses that affect breastfeeding, such as inability to suck, lethargy, and unconsciousness, were excluded.
Sample size determination
The sample size was calculated using the single population proportion formula, assuming a 95% confidence interval, a 5% margin of error, and an estimated magnitude of effective breastfeeding of 48% based on a previous study in Gondar town (14). The margin of error was set at 1.5.
The formula used was: Sample size = [(Z1-α/2)2*P(1-P)]/d2.
where:
• (Z1-α/2) is the standard normal variation.
• P is the proportion in the population (48%).
• d is the margin of error (0.05).
The calculated sample size without considering design effect and non-respondents was 384. Taking into account a design effect of 1.5 and a 10% non-response rate, the final sample size was determined to be 634 postnatal mothers.
Sampling procedure
A multi-stage sampling method was employed. Initially, 18 wards (16 rural and 2 urban) were selected from the total using the lottery method. The target sample size was then proportionally allocated to each of the selected wards. Finally, study participants were recruited using a simple random sampling method, with the registration book at health posts serving as the sampling frame.
Operational definition
• Effective breastfeeding technique: The achievement of at least two criteria from positioning, three criteria from attachment, and two criteria from suckling while breastfeeding their infant (15).
• Breast problems: A woman who had one or more of the following six conditions: inverted nipple, flat nipples, cracked nipples, engorgement, mastitis, and breast abscess.
• Poor, average, and good positioning: Women who fulfill none or only one, any two, and all four/three out of four criteria were considered as poor, average, and good positioning, respectively (15). The criteria were as follows: the baby’s head and body are in line; the baby is held close to the body; the baby’s whole body is supported with the arm along their back; and the baby approaches breast nose to the nipple so that it comes to the breast from underneath the nipple (15).
• Poor, average, and good attachment: Women who fulfilled none or only one criterion, any two criteria, and all four/three criteria out of four criteria for infant attachment were considered as poor, average, and good attachment, respectively (15).
• Poor suckling: Women who do not achieve any or only one of the three criteria (slow and regular suckling, deep suckling, and sometimes pausing) (15).
• Deep suckling: A suckling demonstrated by visible or audible swallowing after every one or two sucks (14).
• Good knowledge about the benefits of breastfeeding: Women who correctly answered seven or more out of 13 questions were considered to have good knowledge about the benefits of breastfeeding (16).
Data collection tools and procedure
Data were collected using an interviewer-administered structured questionnaire and an observational checklist. The questionnaire included socio-demographic, obstetric, breastfeeding, and breast problem-related questions. The observational checklist was used to assess the woman’s and baby’s position, attachment, and suckling during breastfeeding, following the WHO’s breastfeeding checklist (14, 17). The data collection tools were developed after reviewing relevant literature to address important variables related to the main objective (12, 16, 18–22). Ten trained female bachelor (BSc.) degree midwives and two supervisors were employed as data collectors. They observed the breastfeeding practice of each mother for 4 min and recorded it on the observation checklist form. Written informed consent was obtained from all participants before the interview and observation, and confidentiality was assured throughout the study process.
Data quality control
To ensure data quality, both the data collectors and supervisors received 2 days of training before data collection. Language experts translated the English version of the questionnaire into the local language (Amharic). Additionally, a pre-test was conducted on 5% (32 mothers) of the sample size before the actual data collection. The tool was modified and corrected based on the pre-test results. Each questionnaire was checked for completeness before data entry, and the data were then edited, coded, and entered into Epi Data version 4.6.1. Double entry was performed, and entry errors were checked and corrected accordingly.
Data processing and analysis
The data were analyzed using SPSS version 25.0. Descriptive statistics such as frequency, percentage, mean, and standard deviation were calculated and presented in tables, figures, and text. Bivariate and multivariable logistic regression analyses were conducted to identify factors associated with effective breastfeeding. Variables with p-values less than 0.25 in the bivariate analysis were included in the multivariable logistic regression to examine the relative effect of confounding variables and variable interactions. Variables with p-values less than 0.05 in the multivariable analysis were considered independent factors associated with the outcome variable. The omnibus test of model coefficients and the Hosmer and Lemeshow goodness-of-fit test were used to assess model fitness, with p-values of 0.000 and 0.851, respectively. Variance inflation factor (VIF) and tolerance tests were also conducted to check for multicollinearity among the explanatory variables, with the highest VIF at 1.18 and the lowest tolerance test at 86.7%.
Results
Socio-demographic characteristics of study participants
Six hundred and ten lactating women were observed and interviewed for effective breastfeeding, with a response rate of 96.2%. The participants’ mean age (±SD) was 25.69 (±6.014) years. The majority of respondents, 471 (77.2%), were housewives, 327 (53.6%) were rural dwellers, and 545 (89.3%) were married. Only 115 (18.8%) had a secondary or higher degree of education (Table 1).
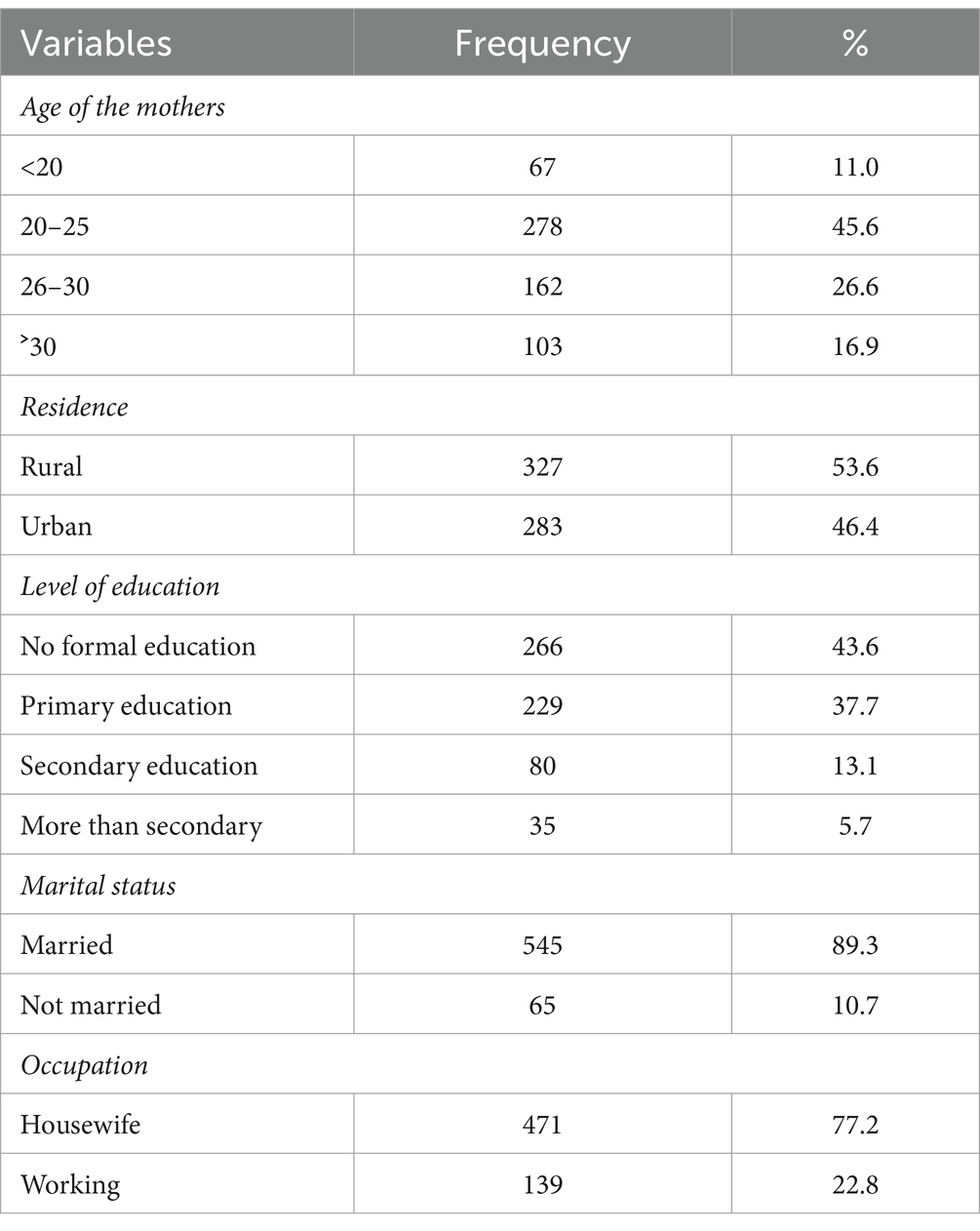
Table 1. Socio-demographic characteristics of study participants in Legambo District, North-East Ethiopia, 2022 (n = 610).
Obstetrics characteristics of the respondents
Three-hundred and eighty (62.3%) of the total participants were multipara, and 56 (9.2%) gave birth at home. Seventy-five percent (456%) of the study participants received prenatal care (ANC). In terms of mode of delivery, 517 (84.8%) were spontaneous vaginal deliveries. Infants were born at term in 534 (87.5%) of the cases, and 554 (90.8%) of postpartum women had no history of breast problems (Table 2).
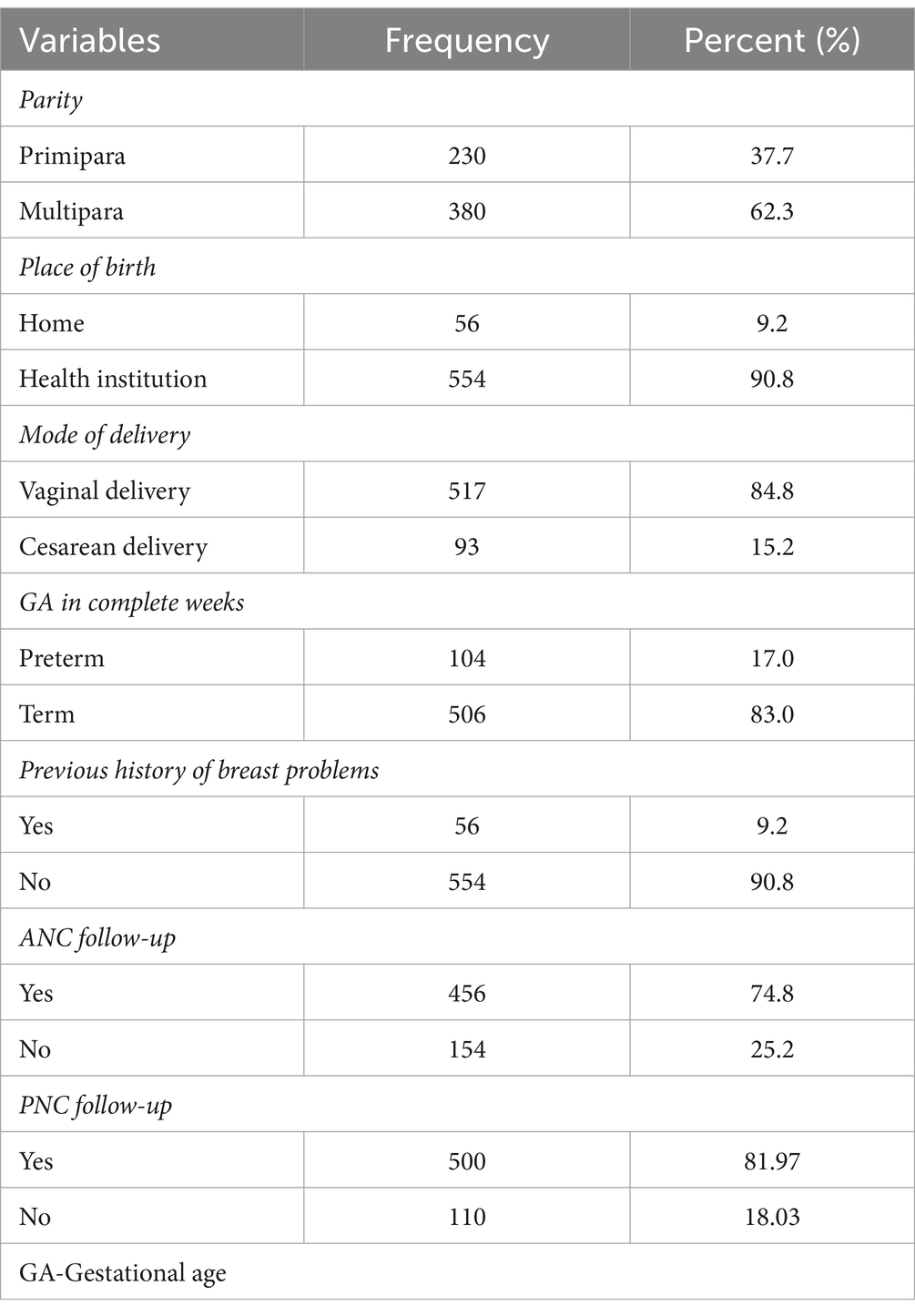
Table 2. Obstetrics characteristics of the participants for the study conducted in Legambo District, North East Ethiopia, 2022 (n = 610).
Breastfeeding characteristics of the study participants
Merely 74 (12.1%) of the total participants began breastfeeding within an hour after birth, whereas 236 (61.3%) of them got health education on the topic. Approximately 38.2% of the total participants were postpartum nursing mothers who mixed-fed their kids at the time of the interview with other foods and liquids in addition to breast milk (Table 3).
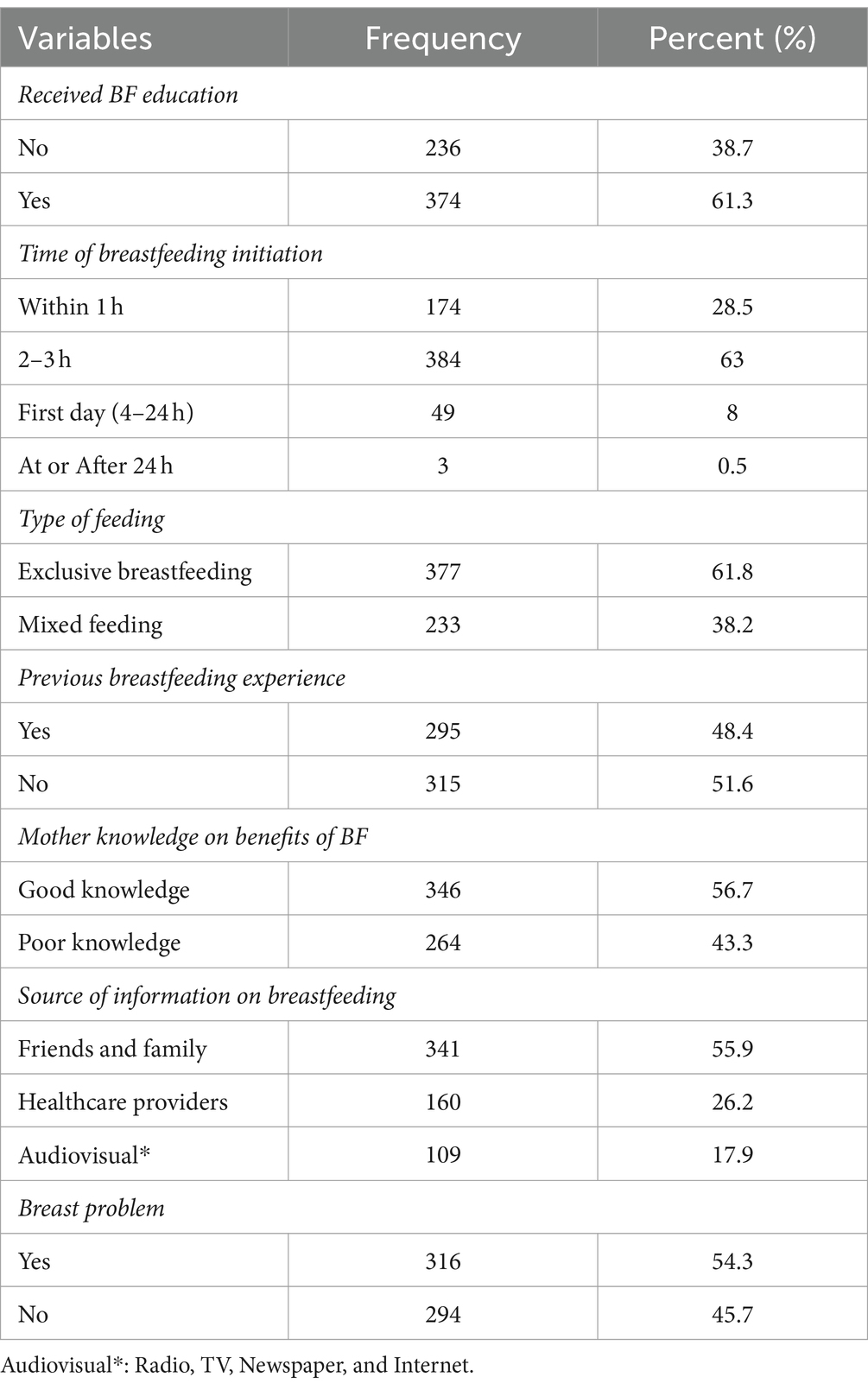
Table 3. Breastfeeding characteristics of the participants for the study conducted in Legambo District, North East Ethiopia, 2022 (n = 610).
Magnitude of effective breastfeeding
In this study, 358 (58.7%), 337 (55.2%), and 416 (68.2%) women demonstrated good positioning, attachment, and suckling, respectively. The practice of effective breastfeeding techniques was identified among 158 women, which accounts for a magnitude of 25.9% with a 95% confidence interval ranging from 22.47 to 29.57%. The remaining 452 (74.1%) women exhibited ineffective breastfeeding practices.
Factors associated with effective breastfeeding
Bi-variable and multivariable logistic regressions were performed. In the bi-variable analysis, 14 variables (occupation, age of mothers, residence, marital status, place of birth, parity, gestational age, mode of delivery, previous breast problem history, receiving BF education, breastfeeding experience, type of feeding, current breast problem, and BF initiation time) had p-values less than 0.25. These 14 variables were adjusted to each other on the multivariable logistic regression to identify the AOR with their 95% confidence interval. In the multivariable logistic regression analysis, age, residence, and occupation of the mothers, breastfeeding initiation time, receiving BF education, and current breast problem retained their association with effective breastfeeding at a p-value less than 0.05 (Table 4).
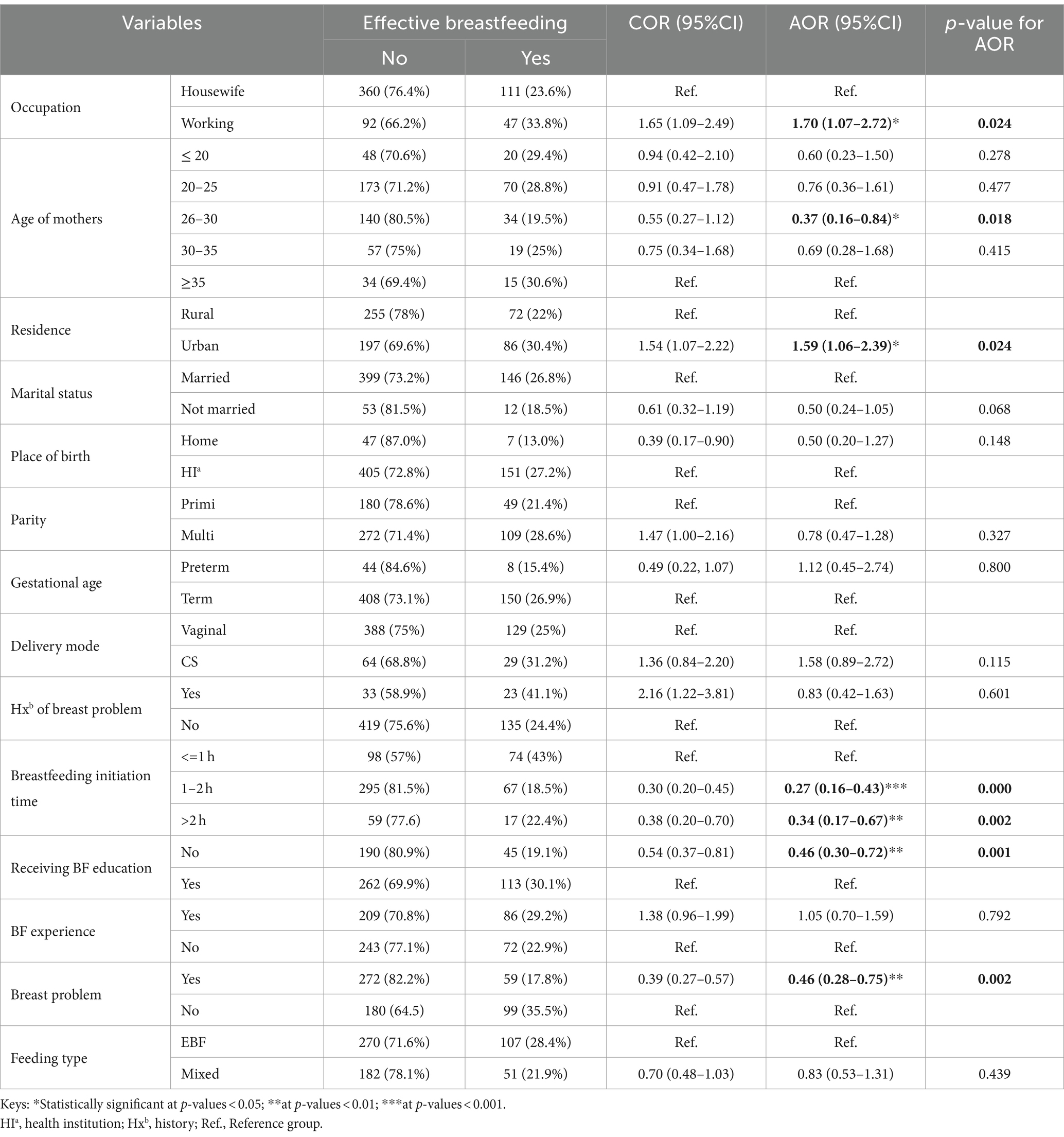
Table 4. Bi-variable and multivariable analysis of factors associated with effective breastfeeding techniques among postnatal lactating mothers in Legambo District, North East Ethiopia, 2022 (n = 610).
Discussion
The magnitude of effective breastfeeding among lactating women in the study area was 25.9% (95% CI: 22.47, 29.57). This result is consistent with a study conducted in Madhya Pradesh, India (31.4%) (23). However, it is lower than the findings of studies conducted in Southeast Nigeria (49%) (24), Gondar town health facilities (48%) (14), Harar city (43.4%) (25), South Ari district 36.5% (26), and Gidan district, Ethiopia (42.9%) (16). This difference could be attributed to the fact that the current study was community-based, and the district had a higher proportion of rural population than urban areas (27). Additionally, the educational levels of the participants in this study were generally lower, and a significant proportion of them were housewives. This factor might have affected the knowledge and practice of breastfeeding among the participants. Factors such as cultural beliefs, lack of awareness, and inadequate support systems could also contribute to the lower prevalence of effective breastfeeding observed in this study (28, 29).
In contrast, the magnitude of effective breastfeeding in this study is higher than that reported in a study conducted in a resettlement colony of Delhi (7.5%) (30). This difference might be attributed to several factors, including poor knowledge about the importance and benefits of effective breastfeeding, lack of breastfeeding-friendly workplaces, lack of support from family members, and harmful traditional practices. Additionally, limited access to healthcare, including comprehensive breastfeeding education and counseling programs, as well as inadequate postnatal and prenatal care for women living in resettlement areas, may contribute to this disparity (31, 32).
This study also found that working women had 1.7 times higher odds of practicing effective breastfeeding than housewives. Similar results were reported in studies conducted in Puducherry, India (33) and rural areas of Gandhinagar, India (34). This could be due to factors such as lower educational levels, reduced opportunities to attend breastfeeding-related health education sessions provided by healthcare providers, and vulnerability to traditional practices that discourage effective breastfeeding. Moreover, social isolation, lack of support from family members, lack of confidence in breastfeeding, and limited exposure to effective breastfeeding role models might result in lower effective breastfeeding practices among housewives.
Similarly, women residing in urban areas had 1.59 times higher odds of practicing effective breastfeeding techniques than those in rural areas. This could be attributed to higher educational levels, better access to breastfeeding advice, more exposure to breastfeeding role models, and access to healthcare services for any concern related to breastfeeding in urban areas.
Women aged between 26 and 30 years had 63% lower odds of practicing effective breastfeeding techniques than women aged 35 years and above. This finding is consistent with studies conducted in Southeast Nigeria (24), Puducherry, South India (33), and Gidan district, Ethiopia (16). The lower odds among younger women might be attributed to a lack of experience, lack of role models, lack of awareness about the benefit of effective breastfeeding, lack of time management due to multiple responsibilities, and their vulnerability to traditional practices.
The odds of practicing effective breastfeeding techniques were 54% lower among women who did not receive education on breastfeeding compared to those who did. This finding is also supported by studies conducted in Southeast Nigeria (24), Puducherry in South India (33), Vadodara in western India (35), and South Ari district (26), Harar city (25), Arbaminch Zuria (36), and Gondar town in Ethiopia (14). This might be because education creates awareness and promotes behavioral modifications, enabling women to understand the importance of proper breastfeeding techniques. Education also helps women anticipate challenges they may face during breastfeeding and equips them with strategies to overcome them. Moreover, it encourages women to seek support from family members, prioritize breastfeeding, and develop self-esteem, contributing to improved breastfeeding practices (18, 37, 38).
Women who initiated breastfeeding within 2 h had 73% lower odds of practicing effective breastfeeding than those who initiated breastfeeding within the first hour after giving birth. Similarly, women who breastfed after 2 h had 66% lower odds. The possible explanation for this might be that women who initiate breastfeeding later may have missed opportunities for guidance and support from healthcare professionals at the time of delivery, leading to a lack of knowledge about breastfeeding. Additional factors that can contribute to delayed initiation and lower rates of effective breastfeeding include breast problems, home deliveries, and complicated deliveries that require medical interventions. These factors can disrupt the natural process of early breastfeeding initiation and make it more challenging for women to establish effective breastfeeding practices (39–41).
Furthermore, women with current breast problems had 54% lower odds of practicing effective breastfeeding than women without breast problems. This finding is consistent with studies conducted in South Ari district (26), Harar city (25), and Gondar town (14) in Ethiopia. The possible reasons might be that women who do not practice effective breastfeeding may develop breast problems, or having breast problems may hinder their ability to practice effective breastfeeding (42).
Similar studies conducted in different parts of the world identified variables such as maternal level of education (24–26), parity (17, 26, 34, 35), antenatal care (16, 24), baby’s birth weight (34, 43), preterm birth (34, 43), early initiation of complementary feeding (36), poor knowledge on breastfeeding (36), postnatal visit (16, 25), previous breastfeeding experience (25), and place of delivery (16, 26) for having association with effective breastfeeding practice. However, these were not identified in the current study.
While interpreting the findings from this study, it is important to consider the limitations of the current study. These include the possibility that female participants may have behaved differently because they were aware of being observed despite attempts to conceal the checklists. Additionally, the outcome of effective breastfeeding practice in the neonate was not addressed in this study, such as weight gain, growth and development, malnutrition, respiratory and diarrheal diseases, and maternal–infant bonding.
Conclusion and recommendations
Only one in four women demonstrated effective breastfeeding techniques, indicating their practice was below the WHO’s recommendation. Maternal age, women’s occupation, lack of education about breastfeeding, and experiencing breast problems were found to be significantly associated with ineffective breastfeeding practice. Therefore, providing education on breastfeeding through promoting educational programs during the antenatal and postnatal periods and early management of breast problems will benefit women in practicing effective breastfeeding techniques. It is also better for future researchers to consider interventional studies by using breastfeeding counselors.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical review board of Wollo University College of medicine and Health Sciences (Ref. No CMHS/004/13). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EM: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. AS: Writing – original draft, Visualization, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis. HK: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. MA: Writing – original draft, Visualization, Validation, Supervision, Software, Project administration, Methodology, Investigation, Data curation. AA: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank all respondents and data collectors who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratios; COR, crude odd ratio; CI, confidence interval; WHO, World Health Organization; EBF, exclusive breastfeeding; PNC, postnatal care.
References
1. Moh, F . National guideline on adolescent, maternal, infant and young child nutrition. FMOH. (2016):1–70.
3. Tomori, C, Hernández-Cordero, S, Busath, N, Menon, P, and Pérez-Escamilla, R. What works to protect, promote and support breastfeeding on a large scale: a review of reviews. Matern Child Nutr. (2022) 18:e13344. doi: 10.1111/mcn.13344
4. Victora, CG, Bahl, R, Barros, AJ, França, GV, Horton, S, Krasevec, J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. (2016) 387:475–90. doi: 10.1016/S0140-6736(15)01024-7
5. Eidelman, AI, Schanler, RJ, Johnston, M, Landers, S, Noble, L, Szucs, K, et al. Breastfeeding and the use of human milk. Pediatrics. (2012) 129:e827–41. doi: 10.1542/peds.2011-3552
6. Organization WH . Global breastfeeding scorecard, 2019: Increasing commitment to breastfeeding through funding and improved policies and programmes. Geneva: World Health Organization (2019).
7. Rollins, NC, Bhandari, N, Hajeebhoy, N, Horton, S, Lutter, CK, Martines, JC, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. (2016) 387:491–04. doi: 10.1016/S0140-6736(15)01044-2
8. Labbok, MH . Effects of breastfeeding on the mother. Pediatr Clin N Am. (2001) 48:143–58. doi: 10.1016/S0031-3955(05)70290-X
9. Mulder, PJ . A concept analysis of effective breastfeeding. J Obstet Gynecol Neonatal Nurs. (2006) 35:332–9. doi: 10.1111/j.1552-6909.2006.00050.x
10. Organization WH . Guideline: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. Geneva: World Health Organization (2017).
11. Organization WH . Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. Geneva: World Health Organization (2009).
12. Organization WH . Implementation guidance: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative. Geneva: World Health Organization (2018).
13. office LDH . Legambo District health office 2020/21 report. Legambo, Ethiopia: Legambo District Health office (2021).
14. Safayi, BL, Assimamaw, NT, and Kassie, DG. Breastfeeding technique and associated factors among lactating mothers visiting Gondar town health facilities, Northwest Ethiopia: observational method. Ital J Pediatr. (2021) 47:1–10. doi: 10.1186/s13052-021-01158-6
15. Brugaletta, C, and Le Roch, K. Breastfeeding assessment tools for at-risk and malnourished infants aged under 6 months old: a systematic review. F1000Res. (2020) 9:1310. doi: 10.12688/f1000research.24516.1
16. Asmamaw, DB, Habitu, YA, Negash, WD, Desta, DZ, and Mekonnen, EG. Effective breastfeeding technique and associated factors among lactating mothers in Gidan District, north-east, Ethiopia: a community-based cross-sectional study. BMJ Open. (2022) 12:e059518. doi: 10.1136/bmjopen-2021-059518
17. Degefa, N, Tariku, B, Bancha, T, Amana, G, Hajo, A, Kusse, Y, et al. Breast feeding practice: positioning and attachment during breast feeding among lactating mothers visiting health facility in Areka town, southern Ethiopia. Int J Pediatr. (2019) 2019:1–6. doi: 10.1155/2019/8969432
18. Chipojola, R, Chiu, H-Y, Huda, MH, Lin, Y-M, and Kuo, S-Y. Effectiveness of theory-based educational interventions on breastfeeding self-efficacy and exclusive breastfeeding: a systematic review and meta-analysis. Int J Nurs Stud. (2020) 109:103675. doi: 10.1016/j.ijnurstu.2020.103675
19. Rodriguez-Gallego, I, Leon-Larios, F, Corrales-Gutierrez, I, and Gonzalez-Sanz, JD. Impact and effectiveness of group strategies for supporting breastfeeding after birth: a systematic review. Int J Environ Res Public Health. (2021) 18:2550. doi: 10.3390/ijerph18052550
20. Li, J, Nguyen, TT, Wang, X, Mathisen, R, and Fang, J. Breastfeeding practices and associated factors at the individual, family, health facility and environmental levels in China. Matern Child Nutr. (2020) 16:e13002. doi: 10.1111/mcn.13002
21. Organization WH . Guideline: Counselling of women to improve breastfeeding practices. Geneva: World Health Organization (2018).
22. Linde, K, Lehnig, F, Nagl, M, and Kersting, A. The association between breastfeeding and attachment: a systematic review. Midwifery. (2020) 81:102592. doi: 10.1016/j.midw.2019.102592
23. Rai, N, Tiwari, R, Soni, P, and Agrawal, R. A study of breast feeding practices and techniques among lactating mothers having infants less THAN six months of age in JABALPUR city of Madhya Pradesh, India. Euro J Mol Clin Med. (2022) 9:1–8.
24. Nduagubam, OC, Ndu, IK, Bisi-Onyemaechi, A, Onukwuli, VO, Amadi OFOkeke, IB, et al. Assessment of breastfeeding techniques in Enugu, south-East Nigeria. Ann Afr Med. (2021) 20:98–04. doi: 10.4103/aam.aam_22_20
25. Tiruye, G, Mesfin, F, Geda, B, and Shiferaw, K. Breastfeeding technique and associated factors among breastfeeding mothers in Harar city Eastern Ethiopia. Int Breastfeed J. (2018) 13:1–9. doi: 10.1186/s13006-018-0147-z
26. Yilak, G, Gebretsadik, W, Tadesse, H, Debalkie, M, and Bante, A. Prevalence of ineffective breastfeeding technique and associated factors among lactating mothers attending public health facilities of south Ari district, southern Ethiopia. PLoS One. (2020) 15:e0228863. doi: 10.1371/journal.pone.0228863
27. Cinar, N, Köse, D, and Altinkaynak, S. The relationship between maternal attachment, perceived social support and breast-feeding sufficiency. J Coll Physicians Surg Pak. (2015) 25:271–5.
28. Gutierrez-de-Terán-Moreno, G, Ruiz-Litago, F, Ariz, U, Fernández-Atutxa, A, Mulas-Martín, M-J, Benito-Fernández, E, et al. Successful breastfeeding among women with intention to breastfeed: from physiology to socio-cultural factors. Early Hum Dev. (2022) 164:105518. doi: 10.1016/j.earlhumdev.2021.105518
29. Ingram, J, Johnson, D, Copeland, M, Churchill, C, and Taylor, H. The development of a new breast feeding assessment tool and the relationship with breast feeding self-efficacy. Midwifery. (2015) 31:132–7. doi: 10.1016/j.midw.2014.07.001
30. Parashar, M, Singh, S, Kishore, J, and Patavegar, BN. Breastfeeding attachment and positioning technique, practices, and knowledge of related issues among mothers in a resettlement colony of Delhi. Infant Child Adolesc Nutr. (2015) 7:317–22. doi: 10.1177/1941406415602528
31. Uusimäki, K, Schneider, L, Lubeka, C, Kimiwye, J, and Mutanen, M. Mothers’ knowledge and practices on breastfeeding and complementary feeding in an urban slum area and rural area in Kenya: a cross-sectional interview study. J Child Health Care. (2022) 27:612–27. doi: 10.1177/13674935221083451
32. Guerra, JVV . Breast feeding in refugee context: a scoping review. J Food Sci Nutrition Disord. (2021) 1:1–7. doi: 10.55124/jfsn.v1i1.23
33. Nancy, S, Sindhuri, R, Arunagirinathan, A, and Dongre, AR. Breastfeeding positioning and attachment among postnatal mothers: a mixed methods study in a tertiary care hospital in Puducherry, South India. Ind J Commun Med Off Public Ind Assoc Prevent Soc Med. (2022) 47:120. doi: 10.4103/ijcm.ijcm_859_21
34. Prajapati, AC, Chandwani, H, Rana, B, and Sonaliya, KN. A community based assessment study of positioning, attachment and suckling during breastfeeding among 0-6 months aged infants in rural area of Gandhinagar district, Gujarat, India. Int J Commun Med Public Health. (2016) 3:1921–6. doi: 10.18203/2394-6040.ijcmph20162066
35. Davra, K, Chavda, P, Pandya, C, Dave, D, and Mehta, K. Breastfeeding position and attachment practices among lactating mothers: an urban community-based cross-sectional study from Vadodara city in western India. Clin Epidemiol Glob Health. (2022) 15:101009. doi: 10.1016/j.cegh.2022.101009
36. Tamiru, D, and Jisha, H. Breastfeeding skills in Arba Minch Zuria: the positioning and attachment initiatives. Int J Nurs Midwif. (2017) 9:46–52. doi: 10.5897/IJNM2016.0237
37. Kehinde, J, O'Donnell, C, and Grealish, A. The effectiveness of prenatal breastfeeding education on breastfeeding uptake postpartum: a systematic review. Midwifery. (2023) 118:103579. doi: 10.1016/j.midw.2022.103579
38. Wong, MS, Mou, H, and Chien, WT. Effectiveness of educational and supportive intervention for primiparous women on breastfeeding related outcomes and breastfeeding self-efficacy: a systematic review and meta-analysis. Int J Nurs Stud. (2021) 117:103874. doi: 10.1016/j.ijnurstu.2021.103874
39. Sharma, IK, and Byrne, A. Early initiation of breastfeeding: a systematic literature review of factors and barriers in South Asia. Int Breastfeed J. (2016) 11:1–12. doi: 10.1186/s13006-016-0076-7
40. Cohen, SS, Alexander, DD, Krebs, NF, Young, BE, Cabana, MD, Erdmann, P, et al. Factors associated with breastfeeding initiation and continuation: a meta-analysis. J Pediatr. (2018) 203:e21. doi: 10.1016/j.jpeds.2018.08.008
41. Takahashi, K, Ganchimeg, T, Ota, E, Vogel, JP, Souza, JP, Laopaiboon, M, et al. Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: secondary analysis of the WHO global survey. Sci Rep. (2017) 7:44868. doi: 10.1038/srep44868
42. Feenstra, MM, Kirkeby, MJ, Thygesen, M, Danbjørg, DB, and Kronborg, H. Early breastfeeding problems: a mixed method study of mothers’ experiences. Sex Reprod Healthc. (2018) 16:167–74. doi: 10.1016/j.srhc.2018.04.003
Keywords: effective breastfeeding techniques, good attachment, good positioning, good suckling, breastfeeding
Citation: Mislu E, Kumsa H, Arage MW, Shitie A and Adimasu A (2024) Effective breastfeeding techniques and associated factors among lactating women: a community-based study, north east Ethiopia. Front. Public Health. 12:1337822. doi: 10.3389/fpubh.2024.1337822
Edited by:
Karolina Krupa-Kotara, Medical University of Silesia, PolandReviewed by:
Sylvia Rao, National Institute of Nutrition (ICMR), IndiaAgata Wypych-Ślusarska, Medical University of Silesia, Poland
Dorota Szymańska, Silesian Higher Medical School, Katowice, Poland, in collaboration with reviewer AW-Ś
Copyright © 2024 Mislu, Kumsa, Arage, Shitie and Adimasu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Esuyawkal Mislu, ZXN1eWF3a2FsbWlzbHVAZ21haWwuY29t
 Esuyawkal Mislu
Esuyawkal Mislu Henok Kumsa1
Henok Kumsa1 Mulugeta Wodaje Arage
Mulugeta Wodaje Arage Anguach Shitie
Anguach Shitie