- 1Department of Public Health, Sarab Faculty of Medical Sciences, Sarab, Iran
- 2Research Center of Psychiatry and Behavioral Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
- 3Department of Public Health, School of Public Health, Research Center for Evidence-Based Health Management, Maragheh University of Medical Sciences, Maragheh, Iran
- 4Department of Nursing, Sarab Faculty of Medical Sciences, Sarab, Iran
Background: Adherence to medication is an essential factor in controlling and reducing the side effects of non-communicable diseases, particularly hypertension. Medication adherence varies in older adults due to the effects of various factors. The research aimed to examine the determinants of medication adherence among older adults with hypertension.
Methods: This cross-sectional study was performed among 300 people aged 60 years or older referring to health centers in Sarab, Iran, between February and May 2023. To collect data, valid and reliable tools were applied.
Results: There was a significant association between age groups, level of education, and monthly income status with adherence to medication (p-value <0.05). According to the results of hierarchical regression, demographic variables collectively explained 3.2% of the variance in adherence to therapeutic regimens (p-value = 0.143). The inclusion of illness perception at step 2, along with demographic variables, led to a further significant increase in 9.6% of the variance (p-value <0.001). In the final step, health literacy dimensions were added, which explained an additional 8.7% of the variance (p-value <0.001). In total, demographic variables, illness perception, and HL dimensions explained 21.5% of the variance in adherence to therapeutic regimens.
Conclusion: According to the results, demographic variables, illness perception, and HL dimensions were the main determinants of medication adherence among older adults. Health educators should focus on creating interventions that improve medication adherence by addressing illness perception and health literacy dimensions in this particular population.
1 Introduction
Hypertension, also known as high blood pressure, is a chronic disease that contributes significantly to the burden of cardiovascular diseases (1). The prevalence of hypertension is increasing worldwide due to an aging population and increased exposure to lifestyle risk factors (1–3). According to the reported statistics by the Centers for Disease Control and Prevention (2015–2018), 66.7% of men aged 65–74 and 81.5% of men aged above 75, as well as 74.3% of women aged 65–74 and 86% of women aged above 75, suffer from high blood pressure (4).
Although hypertension often has no symptoms, the complications caused by it, such as stroke, cerebral infarction and cerebral hemorrhage, kidney failure, heart problems, and death, have caused this disease to be called the “silent killer” (2, 3, 5). Hypertension has some modifiable risk factors, such as smoking, inactivity, and obesity (1, 3). Reducing the risk of complications from hypertension could be achieved through drug therapy (3). Although the treatment of hypertension is a lifelong process, the continuation of treatment and its adherence can play a crucial role in controlling the disease (1) and preventing disability in people aged 65 and older (5).
Medication adherence is one of the health-related coping strategies that refers to the extent to which people’s behavior matches the health or treatment recommendations provided by healthcare providers (6). According to the literature, medication adherence can affect the therapeutic and clinical outcome, as well as health-related quality of life (3, 7, 8). Medication non-adherence is a major global health problem with significant consequences in older adults due to their chronic and multiple diseases and polypharmacy (9, 10). Patients with high blood pressure are unaware of the progress of the disease and its potential damage to various organs of the body if they do not adhere to the treatment (5, 11, 12). Demographic, medical, pharmaceutical, behavioral, and economic factors (1, 5, 13) can disrupt a person’s efforts to adherence treatment, some of which occur intentionally and some unintentionally (13). Low-income populations afflicted with chronic conditions represent a susceptible demographic when it comes to adherence to treatment, as their access to adequate pharmacological therapy may be impeded by restricted resources, thereby hindering their ability to receive the necessary ongoing medical care often necessary for the management of chronic ailments (14).
Illness perception is one of the most important factors in this regard (15). People adhere to the prescribed treatment depending on whether they correctly understand their disease or not and the relevance of the recommended treatment with the effective management of the disease (13). In other words, the way a patient perceives the illness and the benefits of prescribed medications can affect their willingness to adhere to medication regimens (15, 16). According to the literature, illness perception and positive beliefs about treatment in older adults with hypertension are associated with medication adherence (13, 15, 16).
Another important effective factor in the management of hypertension and medication adherence is health literacy (5, 17). Health literacy is the ability of an individual to obtain, interpret, understand, and translate knowledge and health information to make appropriate health decisions and improve health (18–20). It includes using the skills of reading, writing, listening, calculating, speaking, analyzing, and making decisions in a healthy situation; it is not necessarily related to years of education or general reading ability (19). Health literacy significantly affects the ability to take medication and disease knowledge in older adults (18).
Many seniors suffer from poor health literacy, with three out of four having difficulty interpreting the printed health information and more than 75% of them having difficulty with math calculations and understanding numbers, which are important for adherence to medical orders (5). Health literacy has a positive and strong relationship with medication adherence (18). Despite decades of research in medication adherence, non-adherence to treatment in patients aged over 65 years with blood pressure is still controversial (9). Considering the importance of medication adherence in older adults’ health, the present study aimed to identify the determinants of medication adherence among older patients with hypertension.
2 Methods
2.1 Participants and sampling
This cross-sectional study took place in Sarab, Iran, between February to May 2023. The participants were people aged 60 years or older referring to Sarab health centers. The sample size was calculated as 300 people based on the formula and the information derived from a similar study (21) and a confidence level of %95, Z = 1.96, SD = 2.27, and mean = 5.21. The inclusion criteria for this study were individuals aged 60 years or older, diagnosed with hypertension, free from psychiatric disorders, and willing to sign a consent form to participate. The only exclusion criterion was unwillingness to take part in the study.
For sampling, a multi-state cluster random method was used. The city of Sarab comprised four health centers, each considered as a cluster. Eligible participants were randomly chosen from these centers using health records. Following an explanation of the study’s objectives, informed consent was obtained from the participants. First author, second and corresponding author were conducted face-to-face interviews to collect data through questionnaires. The interviews took place at the participants’ doorsteps and lasted approximately 20–25 min.
2.2 Measuring
2.2.1 Demographic information form
Demographic information included age, gender, marital status, occupation, education level, and monthly income status.
2.3 Health literacy scale
To collect data, the researchers utilized the validated Health Literacy for Iranian Adults (HELIA) questionnaire (22). The scale included 47 items and five subscales as follows: reading health information (4 items; α = 0.72); understanding health information (7 items; α = 0.86) using a five-point Likert scale ranging from completely difficult (1) to completely easy (5); appraisal of health information (4 items; α = 0.77); ability to access health information (6 items; α = 0.86); and decision making (12 items; α = 0.89) based on five-point Likert scale (always = 5, most of the time = 4, sometimes = 3, seldom = 2 and never = 1).
2.4 Morisky medication adherence scale (MMAS-8)
The Persian version of the MMAS-8 scale was used to measure treatment adherence (23). For each item, the response categories were yes/no, with a dichotomous response and a five-point Likert response for the final item. The total score ranges from 0 to 8. Scores of less than 6 indicate low adherence, scores of 6 to <8 indicate moderate adherence, and score = 8 indicates high adherence.
2.5 Illness perception scale
To measure illness perception, the Brief Illness Perception Questionnaire (BIPQ-R) was employed (24). This measurement tool includes eight items that are rated on a 0–10 scale. The following five items assess cognitive illness representations: consequences (degree of impact on life), timeline (perceived timeline of illness), personal control (perceived control of illness), treatment control (perceived benefit from treatment), and identity (grade of symptoms associated with the illness). Concern (level of concern about the disease) and emotional affect (level of affect) are two questions that assess emotional illness representations. The last item assesses the comprehensibility/coherence of illness.
2.6 Data analysis
Depending on the data distribution type, percentages and frequencies were applied for categorical variables, while mean, standard deviation, median, and quartile deviation were used for continuous variables. The independent samples t-test and one-way ANOVA were used for bivariate comparisons of quantitative variables. The link between HL dimensions and illness perception with treatment adherence was measured using the Pearson correlation.
Three different blocks of independent variables were used to do a hierarchical regression analysis on treatment adherence. Demographic variables made up Block 1. Block 2 came with demographic characteristics and illness perception. The scores from HL dimensions, illness perception, and demographic variables of block three made up this block. To determine the percentage of variance characterized by treatment adherence, we evaluated the adjusted R2 change after inserting each block. The assumptions behind regressions were confirmed by tests for multi-collinearity, normalcy, and significant data points. The threshold for significance was fixed at = 0.05, and the significance level was set to α = 0.05. All analyses were conducted using the SPSS 21 software.
3 Results
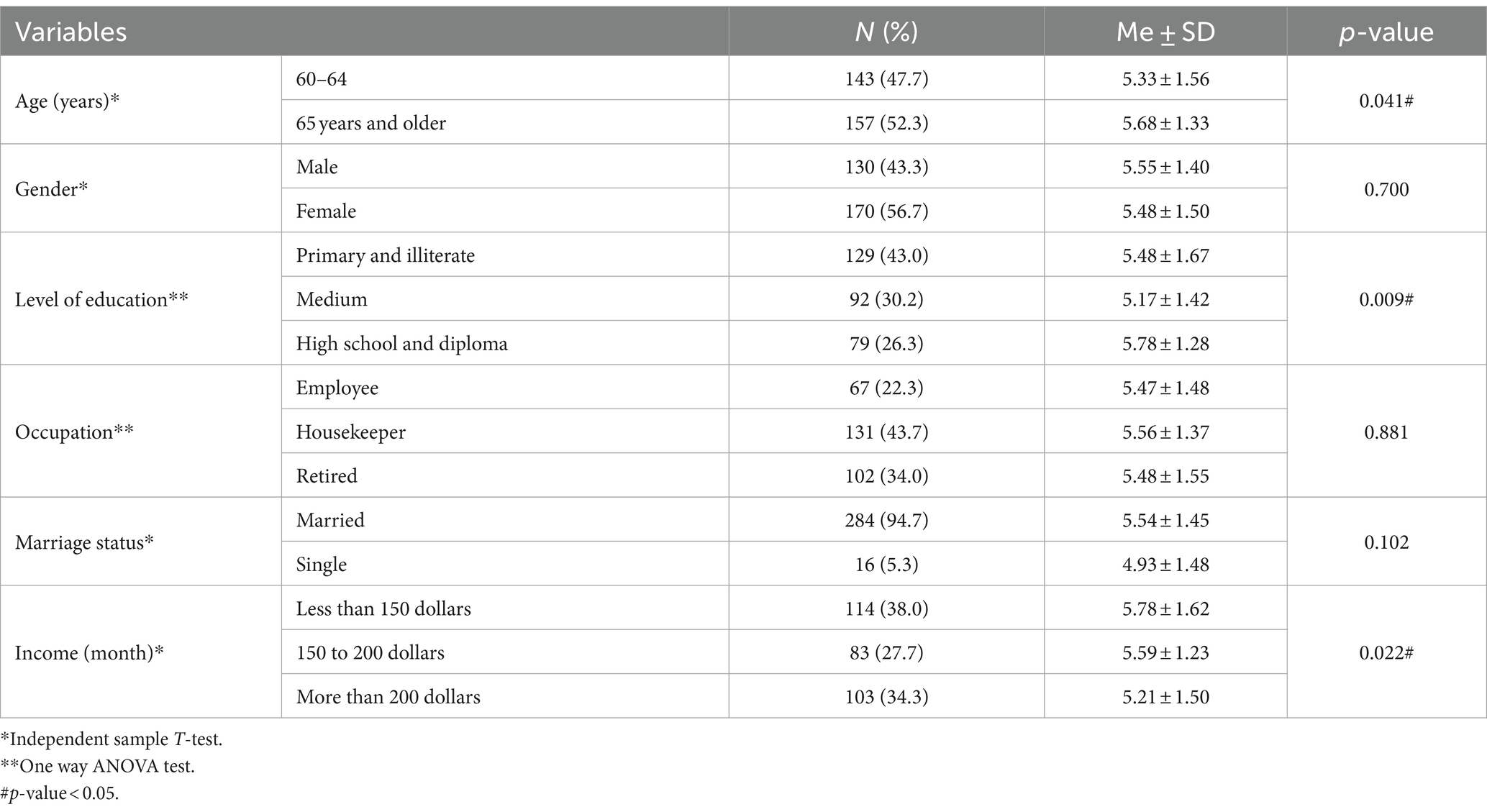
A total of 300 individuals agreed to participate in the study. The median of systolic hypertension was found to be 148.97 mmHg (SD = ±21.20), while the median diastolic hypertension was measured at 103.10 mmHg (SD = ±21.98). Among the participants, 43.3% were male, and most of them were illiterate or had primary education (43.0%). Based on the findings, there was a statistically significant association between age groups, education level, and monthly income status with adherence to therapeutic regimens. Table 1 shows the demographic characteristics and their relationship to adherence to therapeutic regimens.
The bivariate associations for HL dimensions and illness perception with adherence to therapeutic regimens are displayed in Table 2. Using the Pearson correlation coefficient test, we observed that adherence to therapeutic regimens had statistically significant relationships with illness perception and all HL dimensions (p-value <0.05).
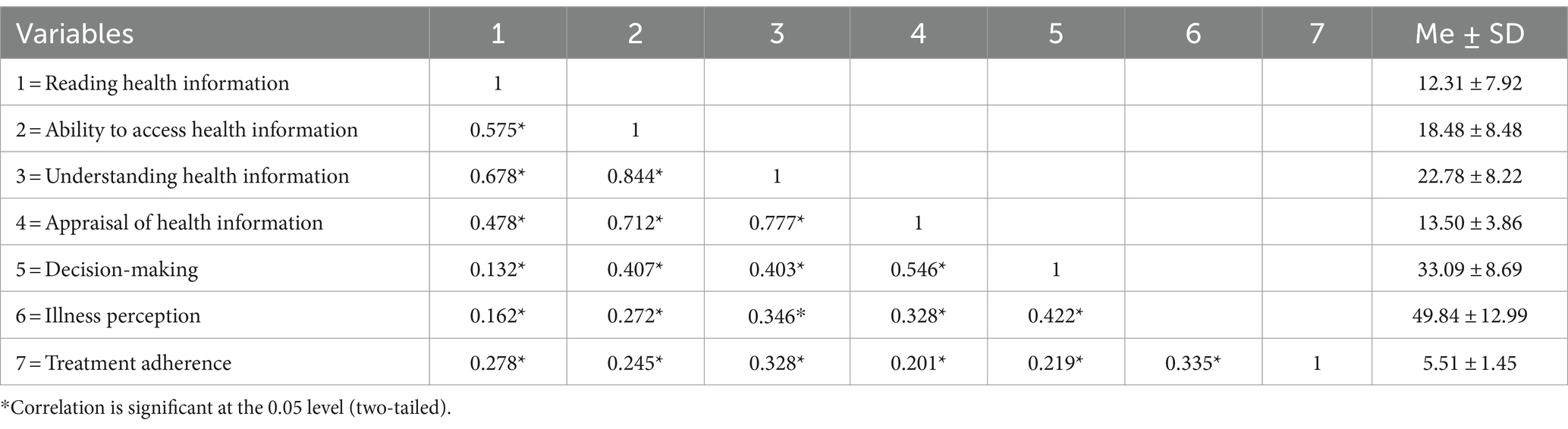
Table 2. Bivariate correlation matrix of the relationship between HL dimension, illness perception, and adherence to medication.
In Table 3, hierarchical regression was used to assess the predictive validity of demographic variables, illness perception, and HL dimensions over adherence to therapeutic regimens. The results revealed that, in step 1, demographic variables were collectively able to explain 3.2% of the variance in adherence to therapeutic regimens (p-value = 0.143). Inclusion of illness perception at step 2 significantly increased 9.6% of the variance explained in hypertension (p-value <0.001). In the final step, reading health information, ability to access health information, understanding health information, appraisal of health information, and decision-making were added, which explained an additional 8.7% of the variance (p-value <0.001). In total, demographic variables, illness perception, and HL dimensions explained 21.5% of the variance related to adherence to therapeutic regimens.
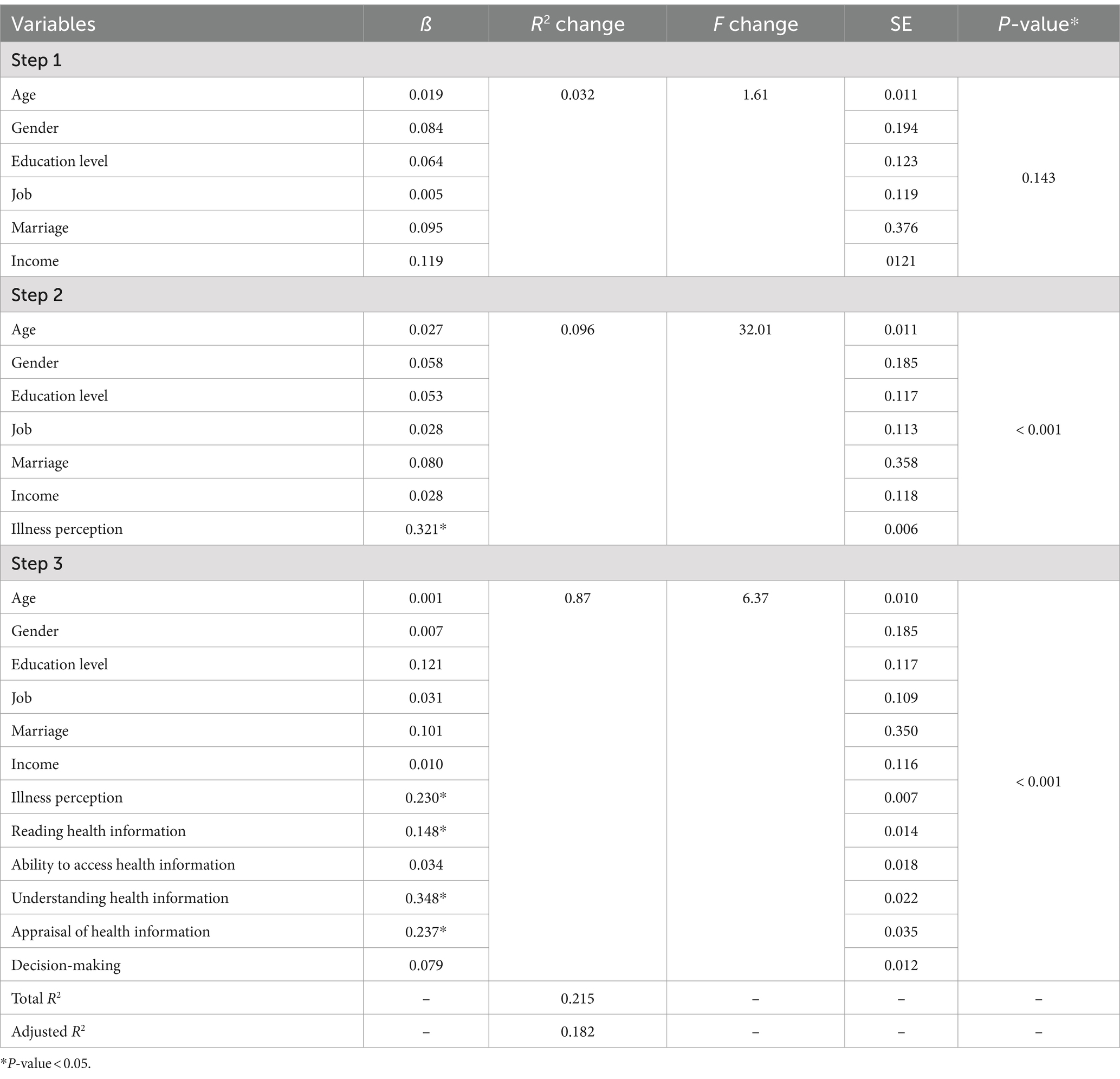
Table 3. Hierarchical linear regression for adherence to medication through demographic characteristics, HL dimensions, and illness perception.
4 Discussion
Adherence to medication is an important factor in controlling and reducing the side effects of diseases, particularly in the older population. Medication adherence varies in older adults due to the effects of various factors. In this study, we examined the determinants of medication adherence among older adults with hypertension.
Based on the findings, there was a statistically significant association between age groups, education level, and monthly income status with adherence to medication. Better medication adherence is affected by aging, high incomes, and high education levels. Previous studies showed that drug adherence was better in patients aged 65–80 years compared to younger hypertensive patients, and age was a significant factor (2, 25, 26). The results revealed that counties with low income were associated with poor medication adherence (27–29). In Iran, health costs increased in the past years and on the other hand, limited resources are concerns in the health system (30). A Scoping Review in Iran demonstrated health costs and amount of out-of-pocket payment are high (31).
Also, employment in informal and formal occupations was considered a significant predictor of medication adherence among people with hypertension (32). In several other studies, educational level was a determinant of medication adherence in hypertensive individuals (1, 25, 33). The main reason for the higher medication adherence among people with higher education can be attributed to their adequate knowledge. It has been reported that both medication adherence and blood pressure control rates were significantly related to hypertension knowledge (34). Medication literacy is an influencing factor for blood pressure control among patients with hypertension (35). These subgroups of demographical variables should be prioritized for interventional programs by health care providers in these patients.
The results of this study demonstrated that adherence to medication had a significant relationship with illness perception and all HL dimensions. This result is in line with previous studies which reported the strong association between medication adherence and health literacy among older adults hypertensive patients (36) and people with hypertension (25, 37). Baharvand et al. (38) found that perceptions of illness consequences could significantly predict treatment adherence. Accordance their results, treatment adherence of hypertensive patients in western Iran is at low level, but their perception of hypertension is at moderate level. A systematic review by Hyvert et al. (29) confirmed an unclear relationship between health literacy and medication adherence, in which 14 studies reported a positive relationship. Lower HL in patients with hypertension made them unable to read or understand the instructions of the prescription drugs; they also failed to communicate effectively with doctors. In addition, hypertensive patients with better HL had better control of their diseases (39). The low level of health literacy caused a 10-year increased risk of cardiovascular disease (40). The higher HL is usually related to better blood pressure control, better hypertension knowledge, better medication adherence, and higher levels of health-related quality of life of the patients; also, health literacy levels affected the outcomes of hypertension health (41).
The results indicated that demographic variables were collectively able to explain 3.2% of the variance in adherence to medication adherence, but this relationship was not significant. The inclusion of illness perception at step 2 significantly increased 9.6% of the variance explained in hypertension. In the final step, reading health information, ability to access health information, understanding health information, appraisal of health information, and decision-making explained an additional 8.7% of the variance. In total, demographic variables, illness perception, and HL dimensions explained 21.5% of the variance in adherence to medication. This finding reinforced the previous report that the complexity of the regimen, health literacy, patient-doctor relationship, family support, and duration of antihypertensive drug use explained 36.1% of the variance in adherence to medication (42). A previous study highlighted that self-efficacy, health belief, patient-provider communication, and medication regimen complexity significantly determined 39.9% of the variation in medication adherence (43). Also, the results of another study revealed that age, sex, education level, anxiety, depression, sleep disturbances, and health literacy accounted for 13.6% of the variance in medication adherence (17). Hence, it is essential to address these predictors in designing patient-centered programs to improve antihypertensive medication adherence in these patients. The current research highlights the need for more specific interventions aiming at promoting HL in hypertension health outcomes and its determinants.
This study had some limitations. First, the participants in this research were selected from a limited area in Iran; therefore, the result cannot be generalized. Second, the measurement of medication adherence was based on self-reported questionnaires, which may introduce recall bias. Third, the sample size was small; studies with larger samples are suggested to be conducted in the future. Fourth, we used Morisky questionnaire. However, after the implementation of the study (between February and May 2023), some concerns have been raised regarding the questionnaire’s statistical analysis in September 2023. Therefore, future studies should use this questionnaire more cautiously.
5 Conclusion
According to the results, adherence to medication had a significant relationship with illness perception and all HL dimensions. Overall, demographic variables, illness perception, and HL dimensions explained 21.5% of the variance related to medication adherence. Policymakers, pharmacists and health educators should develop interventions to enhance medication adherence by improving illness perception and HL dimensions among patients. It is also important to address demographic variables in designing patient-centered programs.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Faculty of Ethics Committee in Sarab Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TB: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing, Resources. SR: Writing – original draft, Writing – review & editing. SP: Data curation, Writing – original draft, Writing – review & editing. AL: Writing – original draft, Writing – review & editing. KM: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the Clinical Research Development Unit of Zahra Mardani Azari children’s hospital, Tabriz University of Medical Sciences, Tabriz, Iran, for the assistance. Also, this research was approved by the Sarab Faculty of Medical Sciences.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nagamine, Y, Shobugawa, Y, Sasaki, Y, Takagi, D, Fujiwara, T, Khin, YP, et al. Associations between socioeconomic status and adherence to hypertension treatment among older adults in urban and rural areas in Myanmar: a cross-sectional study using baseline data from the JAGES in Myanmar prospective cohort study. BMJ Open. (2023) 13:e065370. doi: 10.1136/bmjopen-2022-065370
2. Burnier, M, Polychronopoulou, E, and Wuerzner, G. Hypertension and drug adherence in the elderly. Front Cardiovasc Med. (2020) 7:49. doi: 10.3389/fcvm.2020.00049
3. Lee, S, Jeong, K-H, Lee, S, and Park, H. A study on types of medication adherence in hypertension among older patients and influencing factors. Healthcare. (2022) 10:1–9. doi: 10.3390/healthcare10112322
4. CDC. Older Persons’ Health United State: National Center for Health Statistics; (2019). Available at: https://www.cdc.gov/nchs/data/hus/2019/022-508.pdf
5. Hall-McArthur, C. A quality improvement project: Evaluation of teach-back training on medication adherence in hypertensive older veterans. Florida: Jacksonville University (2021).
6. Sabaté, E. Adherence to long-term therapies: Evidence for action. World Health Organization (2003).
7. Moradkhani, B, Mollazadeh, S, Niloofar, P, Bashiri, A, and Oghazian, MB. Association between medication adherence and health-related quality of life in patients with chronic obstructive pulmonary disease. J Pharm Health Care Sci. (2021) 7:40. doi: 10.1186/s40780-021-00222-x
8. Khayyat, SM, Mohamed, MMA, Khayyat, SMS, Hyat Alhazmi, RS, Korani, MF, Allugmani, EB, et al. Association between medication adherence and quality of life of patients with diabetes and hypertension attending primary care clinics: a cross-sectional survey. Qual Life Res. (2019) 28:1053–61. doi: 10.1007/s11136-018-2060-8
9. Pobrotyn, P, Chudiak, A, Uchmanowicz, B, Drobnik, J, and Gajda, R. Adherence problems in elderly patients with hypertension. Med Res J. (2023) 1:34–42. doi: 10.5603/MRJ.a2023.0004
10. Ranjbaran, S, Shojaeizadeh, D, Dehdari, T, Yaseri, M, and Shakibazadeh, E. Determinants of medication adherence among Iranian patients with type 2 diabetes: an application of health action process approach. Heliyon. (2020) 6:e04442. doi: 10.1016/j.heliyon.2020.e04442
11. Carey, RM, Muntner, P, Bosworth, HB, and Whelton, PK. Prevention and control of hypertension: JACC health promotion series. J Am Coll Cardiol. (2018) 72:1278–93. doi: 10.1016/j.jacc.2018.07.008
12. Brouwers, S, Sudano, I, Kokubo, Y, and Sulaica, EM. Arterial hypertension. Lancet. (2021) 398:249–61. doi: 10.1016/S0140-6736(21)00221-X
13. Lo, SH, Chau, JP, Woo, J, Thompson, DR, and Choi, KC. Adherence to antihypertensive medication in older adults with hypertension. J Cardiovasc Nurs. (2016) 31:296–303. doi: 10.1097/JCN.0000000000000251
14. Fernandez-Lazaro, CI, Adams, DP, Fernandez-Lazaro, D, Garcia-González, JM, Caballero-Garcia, A, JAJRiS, M-C, et al. Medication adherence and barriers among low-income, uninsured patients with multiple chronic conditions. Res Soci Admin Pharm. (2019) 15:744–53. doi: 10.1016/j.sapharm.2018.09.006
15. Bilondi, SS, Noghabi, AD, and Aalami, H. The relationship between illness perception and medication adherence in patients with diabetes mellitus type II: illness perception and medication adherence. J Prev Med Hyg. (2021) 62:E966–71. doi: 10.15167/2421-4248/jpmh2021.62.4.2277
16. Rajpura, J, and Nayak, R. Medication adherence in a sample of elderly suffering from hypertension: evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J Manag Care Pharm. (2014) 20:58–65. doi: 10.18553/jmcp.2014.20.1.58
17. Lor, M, Koleck, TA, Bakken, S, Yoon, S, and Dunn Navarra, A-M. Association between health literacy and medication adherence among Hispanics with hypertension: correction. J Racial Ethn Health Disparities (2019). 6:517–24.
18. Saqlain, M, Riaz, A, Malik, MN, Khan, S, Ahmed, A, Kamran, S, et al. Medication adherence and its association with health literacy and performance in activities of daily livings among elderly hypertensive patients in Islamabad, Pakistan. Medicina. (2019) 55:163. doi: 10.3390/medicina55050163
19. Liu, C, Wang, D, Liu, C, Jiang, J, Wang, X, Chen, H, et al. What is the meaning of health literacy? A systematic review and qualitative synthesis. Family Med Comm Health. (2020) 8:e000351. doi: 10.1136/fmch-2020-000351
20. Ranjbaran, S, Chollou, KM, and Babazadeh, T. Assessment of health literacy and health promoting behaviors among the urban adult population. Ethiop J Health Sci. (2022) 32:985–92. doi: 10.4314/ejhs.v32i5.14
21. Mohammadi, SDNK, Dalvandi, A, and Norouzi, M. The level of illness perception and its relationship with adherence to the medical regimen in the elderly with hypertension. IJRN. (2018) 4:40–6.
22. Montazeri, A, Tavousi, M, Rakhshani, F, Azin, SA, Jahangiri, K, Ebadi, M, et al. Health Literacy for Iranian Adults (HELIA): development and psychometric properties. PAYESH (2014) 13:589–99.
23. Moharamzad, YSH, Shahraki, BN, Rai, A, Saadat, Z, Aerab-Sheibani, H, Naghizadeh, MM, et al. Validation of the Persian version of the 8-item Morisky medication adherence scale (MMAS-8) in Iranian hypertensive patients. Global J Health Sci. (2015) 7:173. doi: 10.5539/gjhs.v7n4p173
24. Karimi-Ghasemabad, SAB, Saeedi, A, Talebian Moghaddam, S, and Nakhostin, AN. The Persian brief illness perception questionnaire: validation in patients with chronic nonspecific low Back pain. Sci World J. (2021) 2021:1–7. doi: 10.1155/2021/3348011
25. Lor, M, Koleck, T, Bakken, S, Yoon, S, and Dunn, NA-M. Association between health literacy and medication adherence among hispanics with hypertension. J Racial Ethn Health Disparities. (2019) 6:517–24. doi: 10.1007/s40615-018-00550-z
26. Uchmanowicz, B, Jankowska, E, Uchmanowicz, I, and Morisky, D. Self-reported medication adherence measured with morisky medication adherence scales and its determinants in hypertensive patients aged≥ 60 years: a systematic review and meta-analysis. Front Pharmacol. (2019) 10:168. doi: 10.3389/fphar.2019.00168
27. Affusim, C, and Salam, T. Factors Affecting Medication Adherence in Patients with Hypertension Attending a Tertiary Hospital in Southern Nigeria. NJFP. (2021) 12:53–63.
28. Han, Y, Saran, R, Erickson, SR, Hirth, RA, He, K, and Balkrishnan, R. Environmental and individual predictors of medication adherence among elderly patients with hypertension and chronic kidney disease: a geospatial approach. Res Social Adm Pharm. (2020) 16:422–30. doi: 10.1016/j.sapharm.2019.06.011
29. Hyvert, S, Yailian, A-L, Haesebaert, J, Vignot, E, Chapurlat, R, Dussart, C, et al. Association between health literacy and medication adherence in chronic diseases: a recent systematic review. Int J Clin Pharm. (2023) 45:38–51. doi: 10.1007/s11096-022-01470-z
30. Masoudi Asl, I, Bakhtiari Aliabad, M, Akhavan Behbahani, A, and Rahbari, BM. Health system costs in Iran, how to manage it. Iran J Health Insurance. (2019) 1:117–27.
31. Negarandeh, R, Kamran, A, and Heydari, H. Iran’s health system performance in achieving goals based on the World Health Organization’s framework. A Scoping Rev J Res Health. (2023) 12:65–74. doi: 10.32598/JRH.12.2.1932.1
32. Ipinnimo, T, Abodunrin, O, and Durowade, K. Relationship between cost of care and medication adherence among hypertensive patients attending a Tertiary health Facility in Ekiti State, Nigeria. J Comm Med Primary Health Care. (2022) 34:38–57. doi: 10.4314/jcmphc.v34i1.3
33. Guerra, C, Conte, E, Del Rio, AI, Motta, J, Moreno Velásquez, I, and Quintana, HK, editors. Medication adherence in hypertensive individuals in Panama 2019: a national cross-sectional study. Healthcar (2022). 10:1–13. doi: 10.3390/healthcare10112244
34. Malik, A, Yoshida, Y, Erkin, T, Salim, D, and Hamajima, N. Hypertension-related knowledge, practice and drug adherence among inpatients of a hospital in Samarkand, Uzbekistan. Nagoya J Med Sci. (2014) 76:255–63.
35. Qin, N, Yao, Z, Shi, S, Duan, Y, Li, X, Liu, H, et al. Association between medication literacy and blood pressure control among hypertensive patients. Int J Nurs Pract. (2023):e13153. doi: 10.1111/ijn.13153
36. Maleki, G, Norian, R, Moeini, B, Barati, M, Maleki, S, and Afshari, M. Factors related to medication adherence in patients with hypertension in Iran: a systematic review study. Blood Press Monit. (2023) 28:221–35. doi: 10.1097/MBP.0000000000000665
37. Silva, IC, Nogueira, MRN, Cavalcante, TF, Felipe, GF, Morais, HCC, Moreira, RP, et al. Health literacy and adherence to the pharmacological treatment by people with arterial hypertension. Rev Bras Enferm. (2022) 75:75. doi: 10.1590/0034-7167-2022-0008pt
38. Baharvand, P, Malekshahi, F, and Babakhani, A. Perception of hypertension and adherence to hypertension treatment among patients attending a hospital in western Iran: a cross-sectional study. Health Sci Rep. (2023) 6:e1501. doi: 10.1002/hsr2.1501
39. Zhang, Q, Huang, F, Zhang, L, Li, S, and Zhang, J. The effect of high blood pressure-health literacy, self-management behavior, self-efficacy and social support on the health-related quality of life of Kazakh hypertension patients in a low-income rural area of China: a structural equation model. BMC Public Health. (2021) 21:1–10. doi: 10.1186/s12889-021-11129-5
40. Halladay, JR, Donahue, KE, Cené, CW, Li, Q, Cummings, DM, Hinderliter, AL, et al. The association of health literacy and blood pressure reduction in a cohort of patients with hypertension: the heart healthy Lenoir trial. Patient Educ Couns. (2017) 100:542–9. doi: 10.1016/j.pec.2016.10.015
41. Mourouti, N, Michou, M, and Costarelli, V. Health literacy in relation to health outcomes in hypertension: A systematic review. J Atherosclerosis prev Treat. (2022). 13:1–10. doi: 10.53590/japt.02.1034
42. Hassan, H, Wattanakitkraileart, D, and Pongthavornkamol, K. Factors predicting medication adherence in patients with essential hypertension in Malé. Maldives Nur Sci J Thailand. (2023) 41:100–13.
Keywords: adherence, medication, hypertension, older adults, Iran
Citation: Babazadeh T, Ranjbaran S, Pourrazavi S, Latifi A and Maleki Chollou K (2024) Impact of health literacy and illness perception on medication adherence among older adults with hypertension in Iran: a cross-sectional study. Front. Public Health. 12:1347180. doi: 10.3389/fpubh.2024.1347180
Edited by:
Maria Lorenza Muiesan, University of Brescia, ItalyReviewed by:
Alberto Zucchelli, University of Brescia, ItalyMichel Burnier, Université de Lausanne, Switzerland
Brian Godman, University of Strathclyde, United Kingdom
Copyright © 2024 Babazadeh, Ranjbaran, Pourrazavi, Latifi and Maleki Chollou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Khalil Maleki Chollou, a2htYWxla2k0NDRAZ21haWwuY29t
 Towhid Babazadeh
Towhid Babazadeh Soheila Ranjbaran
Soheila Ranjbaran Sara Pourrazavi
Sara Pourrazavi Arman Latifi3
Arman Latifi3 Khalil Maleki Chollou
Khalil Maleki Chollou