- 1Department of Orthopedics, Zhejiang Hospital, Hangzhou, China
- 2Department of Neurosurgery, Zhejiang Hospital, Hangzhou, China
- 3Department of Radiology, Zhejiang Hospital, Hangzhou, China
Introduction: Mild traumatic brain injury (mTBI) is a prevalent health issue with significant effects on patients' lives. Understanding and attitudes toward mTBI among patients and their families can influence management and outcomes. This study aimed to assess knowledge and attitudes toward mTBI in these groups.
Methods: A cross-sectional study was conducted at Zhejiang Hospital from July 1, 2023, to September 30, 2023. Patients with mTBI and their family members participated. Data were collected via an online questionnaire covering demographic information and mTBI knowledge and attitudes. Knowledge scores ranged from 0 to 20 and attitude scores from 8 to 40. Multivariate logistic regression identified factors influencing these scores.
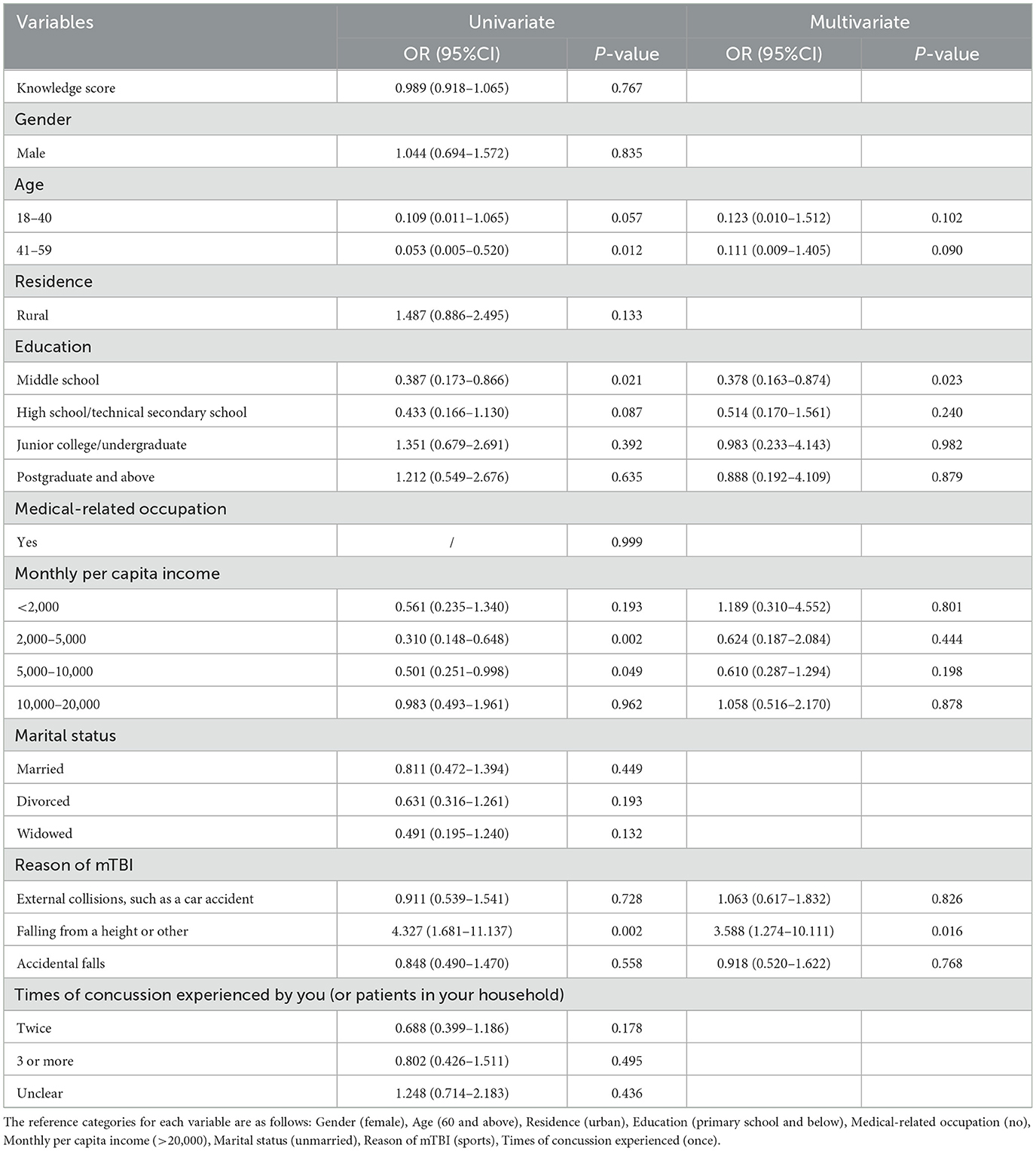
Results: A total of 573 valid questionnaires were analyzed (289 males, 50.44%; 284 females, 49.56%). Among respondents, 258 (45.03%) had experienced a concussion. Mean knowledge and attitude scores were 11.00 ± 2.75 and 27.78 ± 4.07, respectively. Monthly per capita income of 5,000–10,000 RMB was negatively associated with knowledge and attitude scores (β = 0.160, 95% CI: [3.245 to 0.210], P = 0.026). Middle school education decreased the likelihood of positive attitudes toward mTBI (OR = 0.378, 95% CI: [0.1630.874], P = 0.023). mTBI due to falls was associated with increased likelihood of positive attitudes (OR = 3.588, 95% CI: [1.274–10.111], P = 0.016).
Discussion: Significant gaps in knowledge and attitudes toward mTBI exist among patients and their families, influenced by income and education levels. Personal experience with mTBI from falls correlates with more positive attitudes. These findings highlight the need for targeted educational interventions to improve understanding and attitudes, ultimately enhancing patient care and management. Comprehensive, accessible mTBI education is crucial for fostering positive attitudes and better knowledge among patients and their families.
1 Background
Traumatic brain injury (TBI) encompasses a spectrum of severity, with mild traumatic brain injury (mTBI) or concussion being the most common subtype, constituting over 80% of TBI cases (1–3). The disruption of extensive brain networks by TBI, particularly in cases of mTBI, underscores the significant neurological effects even seemingly minor physiological disturbances can induce (4, 5). The clinical significance and long-term implications of mTBI are profound, with affected individuals potentially experiencing a wide array of consequences, including but not limited to headaches, dizziness, neck pain, drowsiness, issues with balance and vision, memory impairment, emotional and mood disturbances, fatigue, and sleep disruptions (6). As a significant global health concern, TBI is associated with elevated mortality rates, disability, and reduced health-related quality of life (7). This condition poses a serious threat to individuals' lives and has a profound effect on their overall wellbeing. Annually, over 27 million people worldwide experience TBI (8), frequently resulting in cognitive and functional deficits, impeding daily life activities, and diminishing overall quality of life (9–11). Therefore, a comprehensive approach is essential to address TBI, with a specific focus on mTBI, as it is a common contributor to neurological morbidity and a leading cause of disability, adversely affecting patient function and quality of life.
In accordance with the Knowledge, Attitude, and Practice (KAP) model, individual behaviors are influenced by their knowledge and attitude (12). Knowledge can be considered as a distal determinant of behavior, which is mediated by attitude. Knowledge holds particular significance in shaping attitudes toward health-related behaviors within the framework of the knowledge-attitude-behavior model (13). Given that patients and their family members are either directly affected by or closely connected to individuals with mTBI, their levels of knowledge and attitudes assume a pivotal role in the processes of rehabilitation and management. Gaining insights into their perspectives and needs can greatly aid healthcare professionals in better fulfilling their requirements and delivering more effective medical care. Currently, there is a notable absence of pertinent research within this specific domain, underscoring an existing gap in the academic literature.
Therefore, this study aimed to investigate the knowledge and attitudes toward mTBI among patients and their family members.
2 Methods
2.1 Study design and participants
This cross-sectional study was conducted between July 1, 2023 and September 30, 2023 at Zhejiang Hospital among patients and their family members of mTBI. This study received ethical approval from the Medical Ethics Committee of Zhejiang Hospital and obtained informed consent from all participants. Inclusion Criteria: (1) Patients with mild traumatic brain injury/Family members of patients with mild traumatic brain injury; (2) History of mild traumatic brain injury within the past year. Mild TBI (mTBI) is defined as the initial Glasgow coma score (GCS) of 13–15, loss of consciousness (LOC) of <30 min, duration of change in mental state (AOC), and posttraumatic amnesia (PTA) of <24 h after external violence on the patient's head, with a negative head CT scan result (14). Exclusion criteria included: (1) Questionnaire completion time of <90 s, suggesting insufficient engagement; (2) Participants expressing disagreement in their responses, indicating potential misunderstandings; (3) Incorrect answers to trap questions designed to test the accuracy of knowledge. Informed consent was obtained from all participants.
2.2 Questionnaire and quality control
The questionnaire was developed based on the 2022 Neurosurgery Guidelines for Diagnosis and Treatment of Cranial Injuries and previous literatures (15–17). A pilot test was conducted involving a small sample of 22 respondents. Participants were recruited through a randomized questionnaire survey administered by neurosurgeons, targeting patients with mild brain injuries and their families at neurosurgery outpatient and inpatient clinics. The internal consistency of the questionnaire was assessed using Cronbach's α coefficient, which yielded a value of 0.856, indicating satisfactory internal reliability. The final questionnaire comprised four sections: demographic information (covering gender, age, education, and professional title), a knowledge section, and an attitude section. The knowledge segment encompassed 13 questions, with the 9th and 10th questions each containing 6 and 3 sub-questions, respectively. Respondents received 1 point for correct answers and 0 points for incorrect or unclear responses, resulting in a knowledge score range of 0–20 points. The attitude section consisted of eight questions, employing a five-point Likert scale ranging from very positive (five points) to very negative (one point), with a total score range of 8–40 points. Positive attitude was defined as achieving scores surpassing 70% of the maximum possible score in each respective section (18–20).
Online e-questionnaires were created using the Wen-Juan-Xing online platform in China (https://www.wjx.cn/app/survey.aspx), and QR codes were provided for access to the electronic version. The distribution of questionnaires occurred in emergency surgery, neurosurgery, and orthopedic consultation rooms, as well as during follow-up visits and appointments with patients recovering from cerebral concussion, facilitated by psychiatrists and orthopedic doctors. To ensure the quality and completeness of the questionnaire results, each IP address could only be used once for submission, and every question was mandatory. The research team meticulously checked all questionnaires for completeness, consistency, and validity.
2.3 Statistical analysis
Data analysis was conducted using SPSS 26.0 (IBM, Armonk, NY, USA). Continuous data are presented as means and standard deviations (SD), while categorical data are expressed as n (%). Continuous variables underwent a normality test, with the t-test for normally distributed data and the Wilcoxon Mann–Whitney test for non-normally distributed data when comparing two groups. For three or more groups with normally distributed continuous variables and uniform variance, ANOVA was used for comparisons, while the Kruskal–Wallis test was employed for non-normally distributed data. Multivariate analysis was used to explore the factors influencing knowledge and attitudes score and positive attitudes. A two-sided P-value <0.05 was considered statistically significant.
3 Results
Initially, a total of 950 questionnaires were collected in the study, excluding 12 cases of questionnaires with too short response time (<90 s); two cases of disagreement with participation; and 363 cases of wrong answers to the trap questions of the knowledge dimensions, leaving 573 valid questionnaires with an effective rate of 60.25%. One of the questionnaires was not filled in for age, which was supplemented by using the mean value. Among them, 289 (50.44%) were males, 312 (54.45%) were aged 18–40 years, 203 (35.43%) had junior college or undergraduate education. Two hundred-eighteen (38.05%) suffered from mTBI due to external collision such as a car accident, and 258 (45.03%) experienced once of concussion.
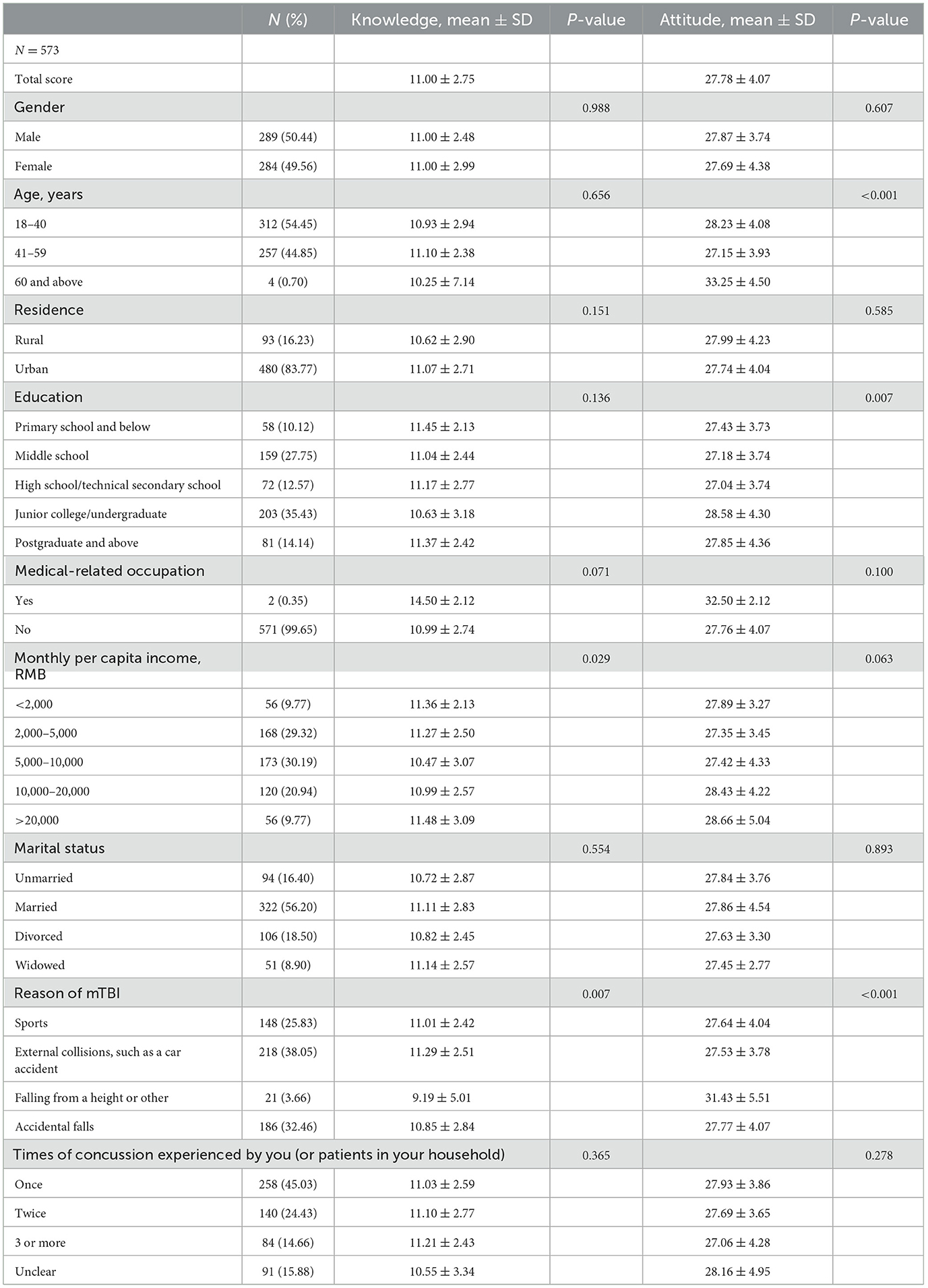
The mean knowledge and attitude scores were 11.00 ± 2.75 (possible range: 0–20) and 27.78 ± 4.07 (possible range: 8–40), respectively. The knowledge score varied from patients with different monthly per capita income (P = 0.029) and the reasons they suffered a mTBI (P = 0.007). As for the attitude score, there were difference among patients with different age (P < 0.001), education (P = 0.007), and the reasons they suffered a mTBI (P < 0.001; Table 1).
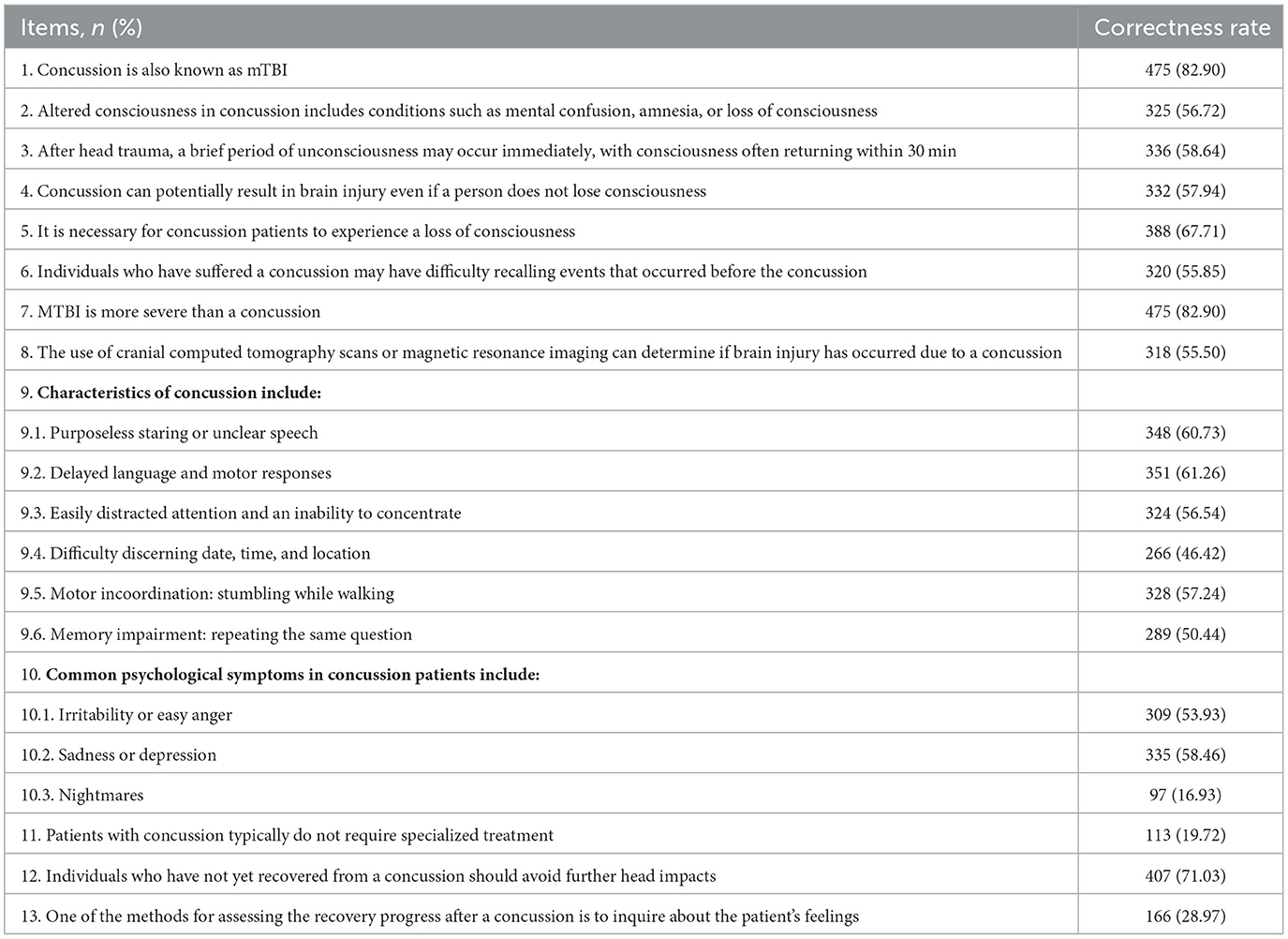
The distribution of knowledge dimensions revealed that the three knowledge items with the highest correctness rates were as follows: “Concussion is also known as mTBI.” (K1) with 82.90%, “mTBI is more severe than a concussion.” (K7) with 82.90%, and “Individuals who have not yet recovered from a concussion should avoid further head impacts.” (K12) with 71.03%. Contrarily, the three items with the lowest correctness rates were “Common psychological symptoms in concussion patients include nightmares.” (K10.3) with 16.93%, “Patients with concussion typically do not require specialized treatment.” (K11) with 19.72%, and “One of the methods for assessing the recovery progress after a concussion is to inquire about the patient's feelings.” (K13) with 28.97% (Table 2).
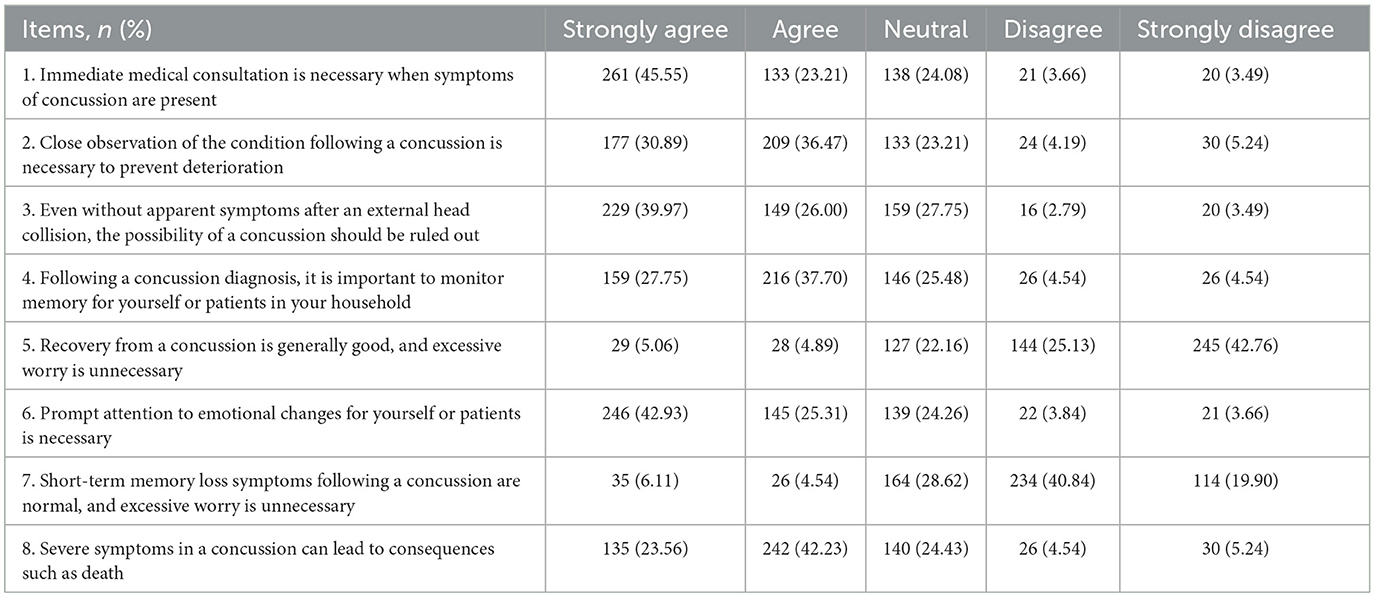
Participants' attitudes toward mTBI (concussion) varied considerably, 68.76% of respondents recognized the necessity of seeking immediate medical consultation when symptoms of a concussion are present (A1). Additionally, 67.36% stressed the importance of closely monitoring the condition following a concussion to prevent deterioration (A2). 66.97% believed that even in the absence of apparent symptoms after an external head collision, it is essential to rule out the possibility of a concussion (A3). Moreover, 65.45% acknowledged the importance of monitoring memory, either for themselves or patients in their household, following a concussion diagnosis (A4). When it came to concerns about concussion recovery (A5), 67.89% expressed varying degrees of concern, while 9.95% believed in generally good recovery and considered excessive worry unnecessary. Regarding emotional changes and attention, 68.24% agreed on the need to promptly address emotional changes for oneself or patients (A6). Conversely, only 10.65% believed that short-term memory loss symptoms following a concussion are normal, while 60.74% expressed some level of concern (A7). Furthermore, 65.79% recognized that severe symptoms resulting from a concussion could lead to consequences such as death (A8; Table 3).
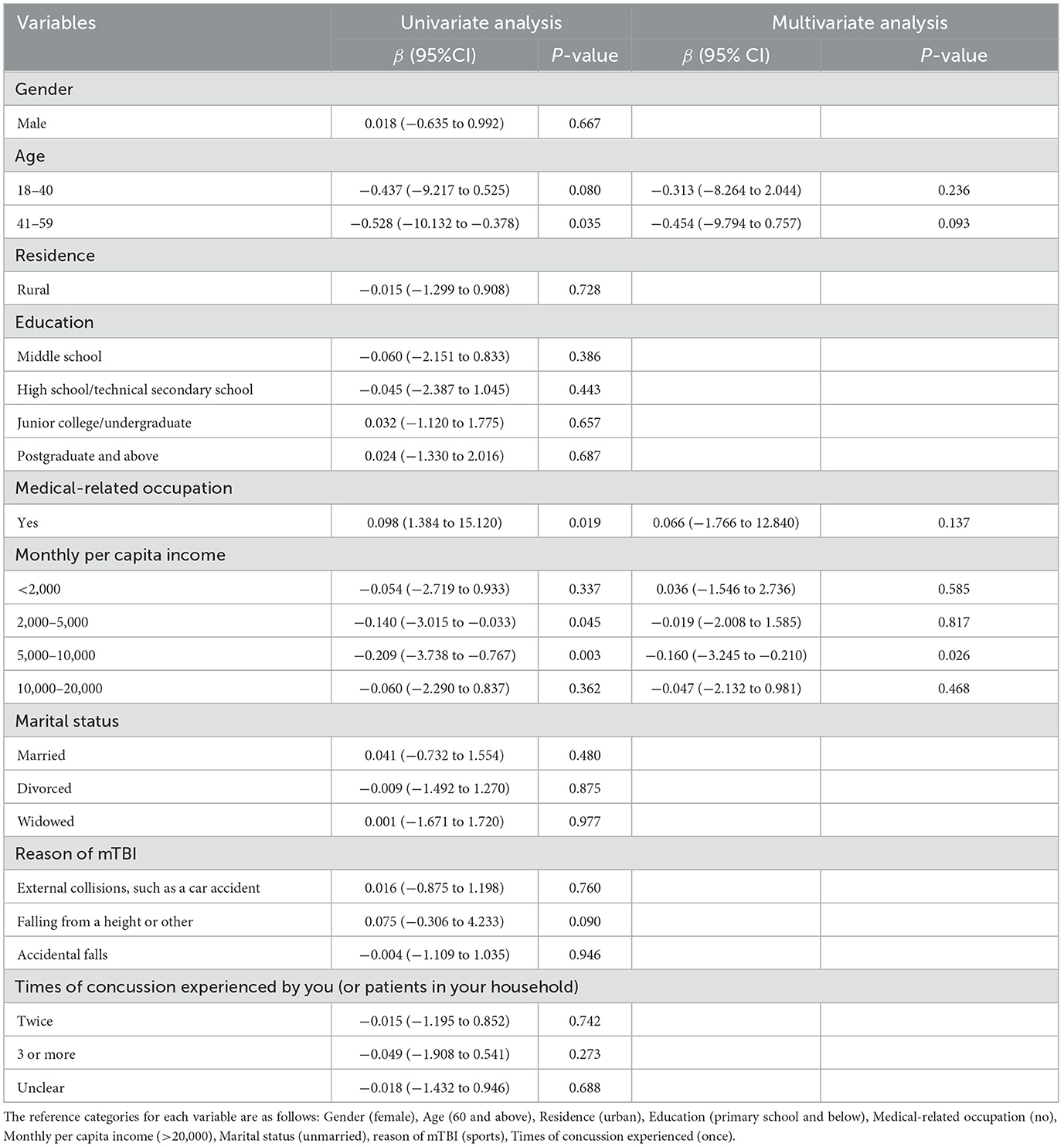
Multivariate analysis showed that monthly per capita income between 5,000 and 10,000 RMB was independently associated with knowledge and attitude score [β = −0.160, 95% CI: (−3.245 to 0.210), P = 0.026; Table 4]. Moreover, middle school education [OR = 0.378 95% CI: (0.163–0.874), P = 0.023] and suffering a mTBI due to falling from a height or other [OR = 3.588, 95% CI: (1.274–10.111), P = 0.016] were independently associated with positive attitude (Table 5).
4 Discussion
As evidenced by our findings, patients and family members exhibit inadequate knowledge and suboptimal attitudes toward mTBI, underscoring the critical need for healthcare professionals across various settings—from emergency surgery units to outpatient psychiatric clinics—to enhance clinical practices. This enhancement should particularly focus on patient and carer education, adapted to the specific contexts of different healthcare environments. Given the varied causes of mTBI, from sports-related concussion (SRC) to falls from a height, our study advocates for personalized support that addresses the unique challenges and needs associated with each type of injury. This approach is grounded in emerging research that supports tailored interventions based on the underlying cause of mTBI to improve patient outcomes. Beyond merely listing examples, our findings illuminate the profound implications of enhancing mTBI awareness and management. Specifically, by addressing the knowledge and attitude gaps identified, healthcare practices can evolve to more effectively educate patients and their families—especially those from lower-income backgrounds—about mTBI. Such informed engagement is crucial for improving mTBI outcomes and patient adherence to recommended care plans, thereby facilitating more effective management of mTBI.
The study findings indicate that patients and their family members exhibit inadequate knowledge and less favorable attitudes toward mTBI. These results are in line with previous studies, which has consistently highlighted a general lack of awareness and suboptimal attitudes toward TBI in healthcare settings (21, 22). The study also identifies several influencing factors, such as income, education, and the causes of TBI, which should be considered in clinical practice. For instance, socioeconomic status, as indicated by monthly per capita income, plays a significant role in knowledge and attitude scores, suggesting that tailored interventions may be necessary for individuals with lower incomes, echoing findings from studies in other health domains (23). Furthermore, education level demonstrated a significant association with attitudes toward mTBI, where individuals with higher educational backgrounds, particularly those with junior college/undergraduate degrees, exhibited more positive attitudes. This finding underscore that education not only enhances knowledge but also positively influences health-related attitudes, potentially leading to more effective coping strategies and adherence to treatment protocols in the face of health challenges. The reasons behind TBI occurrences, such as falls from heights, are associated with more positive attitudes, emphasizing the need for personalized support based on the circumstances of the injury. Additionally, variations in attitude scores among patients of different age groups and educational backgrounds highlight the importance of targeted educational initiatives. In light of these findings, healthcare professionals should prioritize patient and family education, particularly for those from diverse demographic backgrounds, to enhance clinical management and outcomes related to mTBI (24, 25).
The findings from the knowledge dimension of this study provide insight into the existing deficiencies in understanding mTBI and concussion among patients and their family members. While some respondents exhibited a relatively accurate understanding of certain aspects, such as the definition of concussion and its potential consequences, a significant proportion displayed gaps in knowledge. For instance, misconceptions regarding the necessity of experiencing loss of consciousness or the severity of mTBI compared to a concussion were prevalent. The assessment of recovery progress after a concussion was also found to be poorly understood, as a relatively low percentage of respondents recognized the importance of assessing patients' feelings. Such knowledge gaps underline the critical need for targeted education and awareness campaigns. To improve clinical practice, initiatives should focus on disseminating accurate information about the nature of mTBI, the importance of assessing recovery, and the potential psychological symptoms (26, 27). Additionally, promoting the understanding that individuals with concussion should avoid further head impacts and that specialized treatment might be necessary for some patients is essential for enhancing the management and outcomes of mTBI cases (28, 29). For clinicians in emergency settings, this might mean emphasizing the seriousness of any head injury, regardless of immediate symptoms. In contrast, those in rehabilitation or psychiatric settings might focus on educating patients about the recovery timeline and potential psychological symptoms.
The results from the attitude dimension of this study reveal a spectrum of attitudes held by patients and their family members toward mTBI and concussion. While a notable proportion of respondents demonstrated a positive attitude by recognizing the importance of immediate medical consultation when TBI symptoms are present, and the need for close observation following a concussion, there were also prevalent neutral and negative attitudes in certain aspects. Notably, a substantial number of respondents held neutral or negative attitudes regarding the necessity of excessive worry and emotional changes following a concussion, and the potential severity of symptoms, including the possibility of death. These findings are consistent with previous studies indicating variations in attitudes toward TBI and the associated emotional and cognitive aspects (30). To address these deficiencies in attitudes, initiatives to improve clinical practice should aim at fostering a more informed and empathetic perspective. Education and counseling should be directed toward emphasizing the importance of timely medical attention, vigilant observation, and supportive emotional care following a concussion (31, 32). Initiatives should also work to dispel misconceptions regarding symptom severity and emphasize the potential consequences of severe TBI (33, 34). Ultimately, by addressing the specific knowledge gaps and misconceptions identified in our study, these efforts are expected to foster a more positive and well-informed attitude among patients and their families. This direct targeting of educational content, informed by our findings, is anticipated to lead to better clinical management and outcomes for mTBI cases (35, 36).
This study has several limitations. First, data were collected through online questionnaires, which may introduce selection bias, as it excludes individuals without internet access or those who choose not to participate. Second, the study relies on self-reported information, which can be subject to recall bias and social desirability bias, potentially affecting the accuracy of the responses. Additionally, the study's cross-sectional design limits the ability to establish causality or assess changes in knowledge and attitudes over time. Furthermore, the study was conducted in a specific geographic area, which may limit the generalizability of the findings to other regions or populations with different socio-cultural backgrounds. The recruitment strategy utilized in this study, spanning diverse healthcare settings and periods, enriches the applicability of our findings. However, it also introduces considerations for future research, particularly in examining how seasonal variations and different healthcare environments may impact the prevalence and understanding of mTBI. Such insights could inform more nuanced approaches to patient education and care, potentially tailoring strategies to specific times of the year or patient populations.
In conclusion, patients and family members had inadequate knowledge and suboptimal attitude toward mTBI. Special attention should be given to individuals with lower monthly per capita incomes, as they exhibited less knowledge and less favorable attitudes. Tailored interventions and support programs should be developed to address the specific needs of this demographic. Additionally, recognizing the influence of injury causes on attitudes, such as falling from a height, can guide clinicians in providing personalized counseling and support.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Review Committee of Zhejiang Hospital [2022-139K]. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
JH: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. ZC: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. JZ: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. XL: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Exploration and Prognostic Analysis of Enhanced 3D Volume Liquid Attenuation Inversion Recovery (3D-T2-FLAIR+C) Sequence in Mild Traumatic Brain Injury (2022KY474).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1349169/full#supplementary-material
References
1. Desai A, Chen H, Kevala K, Kim HY. Higher n-3 polyunsaturated fatty acid diet improves long-term neuropathological and functional outcome after repeated mild traumatic brain injury. J Neurotrauma. (2021) 38:2622–32. doi: 10.1089/neu.2021.0096
2. Liu Y, Wu W, Chen X, Wu M, Hu G, Zhou G, et al. Aberrant correlation between the default mode and salience networks in mild traumatic brain injury. Front Comput Neurosci. (2020) 14:68. doi: 10.3389/fncom.2020.00068
3. Shi J, Li X, Cavagnaro MJ, Cai J, Zhang C, Li N, et al. Versatile pep-CPDs nanoprobe for rapid detection of mTBI biomarker in clinical instances and safe fluorescence imaging in vivo for improved weight-drop mouse model. Front Bioeng Biotechnol. (2022) 10:807486. doi: 10.3389/fbioe.2022.807486
4. Cook NE, Iverson GL, Maxwell B, Zafonte R, Berkner PD. Adolescents with ADHD Do not take longer to recover from concussion. Front Pediatr. (2020) 8:606879. doi: 10.3389/fped.2020.606879
5. Raizman R, Tavor I, Biegon A, Harnof S, Hoffmann C, Tsarfaty G, et al. Traumatic brain injury severity in a network perspective: a diffusion MRI based connectome study. Sci Rep. (2020) 10:9121. doi: 10.1038/s41598-020-65948-4
6. Dean PJ, Sterr A. Long-term effects of mild traumatic brain injury on cognitive performance. Front Hum Neurosci. (2013) 7:30. doi: 10.3389/fnhum.2013.00030
7. Parmontree P, Tunthanathip T, Doungngern T, Rojpitbulstit M, Kulviwat W, Ratanalert S. Predictive risk factors for early seizures in traumatic brain injury. J Neurosci Rural Pract. (2019) 10:582–7. doi: 10.1055/s-0039-1700791
8. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2019) 18:56–87. doi: 10.1016/S1474-4422(18)30415-0
9. Gao X, Wang H, Gao YY, Zhou XM, Tao T, Liu GJ, et al. Elevated hippocampal CD24 in astrocytes participates in neural regeneration possibly via activating SHP2/ERK pathway after experimental traumatic brain injury in mice. Am J Transl Res. (2020) 12:6395–408.
10. Latini F, Fahlström M, Vedung F, Stensson S, Larsson EM, Lubberink M, et al. Refined analysis of chronic white matter changes after traumatic brain injury and repeated sports-related concussion: of use in targeted rehabilitative approaches? J Clin Med. (2022) 11:358. doi: 10.3390/jcm11020358
11. Lv K, Yuan Q, Fu P, Wu G, Wu X, Du Z, et al. Impact of fibrinogen level on the prognosis of patients with traumatic brain injury: a single-center analysis of 2570 patients. World J Emerg Surg. (2020) 15:54. doi: 10.1186/s13017-020-00332-1
12. World Health Organization. Advocacy, Communication and Social Mobilization for TB Control: A Guide to Developing Knowledge, Attitude and Practice Surveys. Geneva: World Health Organization (2008).
13. Ng TKC, Lo MF, Fong BYF, Yee HHL. Predictors of the intention to use traditional Chinese medicine (TCM) using extended theory of planned behavior: a cross-sectional study among TCM users in Hong Kong. BMC Complement Med Ther. (2022) 22:113. doi: 10.1186/s12906-022-03598-x
14. Levin HS, Diaz-Arrastia RR. Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol. (2015) 14:506–17. doi: 10.1016/S1474-4422(15)00002-2
15. Hawryluk GWJ, Rubiano AM, Totten AM, O'Reilly C, Ullman JS, Bratton SL, et al. Guidelines for the management of severe traumatic brain injury: 2020 update of the decompressive craniectomy recommendations. Neurosurgery. (2020) 87:427–34. doi: 10.1093/neuros/nyaa278
16. Lee SY, Amatya B, Judson R, Truesdale M, Reinhardt JD, Uddin T, et al. Clinical practice guidelines for rehabilitation in traumatic brain injury: a critical appraisal. Brain Inj. (2019) 33:1263–71. doi: 10.1080/02699052.2019.1641747
17. Silverberg ND, Iaccarino MA, Panenka WJ, Iverson GL, McCulloch KL, Dams-O'Connor K, et al. Management of concussion and mild traumatic brain injury: a synthesis of practice guidelines. Arch Phys Med Rehabil. (2020) 101:382–93. doi: 10.1016/j.apmr.2019.10.179
18. Lee F, Suryohusodo AA. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: a cross-sectional study. Front Public Health. (2022) 10:957630. doi: 10.3389/fpubh.2022.957630
19. Salman M, Mustafa ZU, Rao AZ, Khan QU, Asif N, Hussain K, et al. Serious inadequacies in high alert medication-related knowledge among pakistani nurses: findings of a large, multicenter, cross-sectional survey. Front Pharmacol. (2020) 11:1026. doi: 10.3389/fphar.2020.01026
20. Hebo HJ, Gemeda DH, Abdusemed KA. Hepatitis B and C viral infection: prevalence, knowledge, attitude, practice, and occupational exposure among healthcare workers of Jimma University Medical Center, Southwest Ethiopia. ScientificWorldJournal. (2019) 2019:9482607. doi: 10.1155/2019/9482607
21. Stead TS, Daneshvar Y, Ayala S, Ganti L. Knowledge, awareness, and attitudes regarding concussion among middle schoolers. Cureus. (2019) 11:e4863. doi: 10.7759/cureus.4863
22. Tahara S, Otsuka F, Endo T. Recognition and practice of hypopituitarism after traumatic brain injury and subarachnoid hemorrhage in Japan: a survey. Neurol Ther. (2023) 13:39–51. doi: 10.1007/s40120-023-00553-x
23. Zheng X, Xue Y, Dong F, Shi L, Xiao S, Zhang J, et al. The association between health-promoting-lifestyles, and socioeconomic, family relationships, social support, health-related quality of life among older adults in china: a cross sectional study. Health Qual Life Outcomes. (2022) 20:64. doi: 10.1186/s12955-022-01968-0
24. Frías CE, Casafont C, Cabrera E, Zabalegui A. Validation of the Spanish version of the double knowledge expectations and received knowledge significant other scale for informal caregivers of people with dementia (KESO-DEM/RKSO-DEM). Int J Environ Res Public Health. (2022) 19:5314. doi: 10.3390/ijerph19095314
25. Nam K, Kim DU, Lee TH, Iwashita T, Nakai Y, Bolkhir A, et al. Patient perception and preference of EUS-guided drainage over percutaneous drainage when endoscopic transpapillary biliary drainage fails: an international multicenter survey. Endosc Ultrasound. (2018) 7:48–55. doi: 10.4103/eus.eus_100_17
26. Reichert MC, Kupcinskas J, Schulz A, Schramm C, Weber SN, Krawczyk M, et al. Common variation in FAM155A is associated with diverticulitis but not diverticulosis. Sci Rep. (2020) 10:1658. doi: 10.1038/s41598-020-58437-1
27. Wang Y, Guo S, Xiao ML, Zhang H. Efficacy and safety of acupuncture combined with Chinese herbal medicine traditional Chinese medicine for poststroke cognitive impairment: a protocol for a systematic review and meta-analysis. Medicine. (2022) 101:e29019. doi: 10.1097/MD.0000000000029019
28. Miller LE, Urban JE, Whelan VM, Baxter WW, Tatter SB, Stitzel JD. An envelope of linear and rotational head motion during everyday activities. Biomech Model Mechanobiol. (2020) 19:1003–14. doi: 10.1007/s10237-019-01267-6
29. Wilde EA, Ware AL, Li X, Wu TC, McCauley SR, Barnes A, et al. Orthopedic injured versus uninjured comparison groups for neuroimaging research in mild traumatic brain injury. J Neurotrauma. (2019) 36:239–49. doi: 10.1089/neu.2017.5513
30. Howlett JR, Nelson LD, Stein MB. Mental health consequences of traumatic brain injury. Biol Psychiatry. (2022) 91:413–20. doi: 10.1016/j.biopsych.2021.09.024
31. Pepin ME, Webb WM, Boppana S, Weaver AN, Seay RL, Dempsey DM, et al. Gamification: an innovative approach to reinforce clinical knowledge for MD-PhD students during their PhD research years. Med Sci Educ. (2019) 29:739–47. doi: 10.1007/s40670-019-00725-1
32. Wang Y, Dai Y, Li H, Song L. Social media and attitude change: information booming promote or resist persuasion? Front Psychol. (2021) 12:596071. doi: 10.3389/fpsyg.2021.596071
33. Bayly PV, Alshareef A, Knutsen AK, Upadhyay K, Okamoto RJ, Carass A, et al. MR imaging of human brain mechanics in vivo: new measurements to facilitate the development of computational models of brain injury. Ann Biomed Eng. (2021) 49:2677–92. doi: 10.1007/s10439-021-02820-0
34. Li YF, Ren X, Zhang L, Wang YH, Chen T. Microglial polarization in TBI: signaling pathways and influencing pharmaceuticals. Front Aging Neurosci. (2022) 14:901117. doi: 10.3389/fnagi.2022.901117
35. Gaiger A, Lubowitzki S, Krammer K, Zeilinger EL, Acel A, Cenic O, et al. The cancer survival index-A prognostic score integrating psychosocial and biological factors in patients diagnosed with cancer or haematologic malignancies. Cancer Med. (2022) 11:3387–96. doi: 10.1002/cam4.4697
Keywords: knowledge, attitude, traumatic brain injury, patients, cross-sectional study
Citation: He J, Chen Z, Zhang J and Liu X (2024) Knowledge and attitudes toward mild traumatic brain injury among patients and family members. Front. Public Health 12:1349169. doi: 10.3389/fpubh.2024.1349169
Received: 08 December 2023; Accepted: 13 May 2024;
Published: 24 May 2024.
Edited by:
Sarah C. Hellewell, Curtin University, AustraliaReviewed by:
Ricardo Jesus Martinez-Tapia, National Autonomous University of Mexico, MexicoGill Cowen, Curtin University, Australia
Copyright © 2024 He, Chen, Zhang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao Liu, Y2FubmVseWVzQDE2My5jb20=; Jianjun Zhang, emhhbmd5cDMxMTEzQDE2My5jb20=
†These authors have contributed equally to this work
 Jian He1†
Jian He1† Xiao Liu
Xiao Liu