- 1Mt. Hope Family Center, University of Rochester, Rochester, NY, United States
- 2Department of Pediatrics, University of Minnesota Twin Cities, Minneapolis, MN, United States
- 3Great Lakes Neurobehavioral Center, Edina, MN, United States
- 4International Adult Leadership Collaborative of FASD Changemakers
Fetal alcohol spectrum disorders (FASD) are among the most common neurodevelopmental disorders and substantially impact public health. FASD can affect people of all races and ethnicities; however, there are important racial and ethnic disparities in alcohol-exposed pregnancy prevention, assessment and diagnosis of FASD, and interventions to support individuals with FASD and their families. In this article we use the Dis/Ability Studies and Critical Race Theory (Dis/Crit) framework to structure the exploration of disparities and possible solutions within these three areas (prevention, diagnosis, intervention). Dis/Crit provides a guide to understanding the intersection of dis/ability and race, while framing both as social constructs. Following the Dis/Crit framework, the systemic, historical, and contemporary racism and ableism present in psychological care is further discussed. We aim to elucidate these racial and ethnic disparities within the fields of psychology and neuropsychology through the Dis/Crit framework and provide potential points of action to reduce these disparities.
Introduction
Fetal alcohol spectrum disorders (FASD) are neurodevelopmental conditions associated with prenatal alcohol exposure (PAE). In the United States, FASD affect approximately 1.1–5% of school-aged children (1), making them among the most common neurodevelopmental disorders. Diagnostic criteria for FASD include neurobehavioral differences in the presence of PAE and may include subtle facial features and smaller growth in body and brain size in some individuals (2, 3). Outcomes are variable in FASD; many risk and protective factors can influence functioning such as genetics, nutrition, receipt of services, and trauma/life stressors. Without adequate understanding and support, people with FASD are at higher risk for academic challenges (4), mental health conditions (5), housing and independent living issues, and trouble with the law (6, 7). FASD has a considerable public health impact (8) representing substantial societal and economic costs (9). Additionally, FASD are under-recognized and commonly misdiagnosed (10, 11).
Importantly, although FASD can affect people regardless of race, ethnicity, and socioeconomic status (SES), FASD is identified at higher rates in Native American, Black, and low-SES communities compared to White and middle/upper class communities (12). This pattern is the opposite in other neurodevelopmental disabilities such as attention-deficit/hyperactivity disorder (13, 14) and autism spectrum disorder (15, 16), with both diagnoses given to White individuals more frequently than Black, Indigenous, and People of Color (BIPOC) (13, 17). Greater attention to these disparities is needed within FASD and is relative to other neurodevelopmental disorders.
Dis/ability Studies and Critical Race Theory (Dis/Crit) provides a framework for understanding the intersections of race and dis/ability. We use the dis/ability notation instead of “disability” to disrupt the potentially harmful idea that some people cannot be successful within society’s view of appropriate functioning due to not being “able” (18, 19). Dis/Crit frames racial and dis/ability identities as social constructs. This means there are no clear biological indicators distinguishing unique races or dis/abilities. Society defines the boundaries of what constitutes different race and dis/ability groups, which change over time and are shaped by current and historical power structures and values. Critical to Dis/Crit is an appreciation of the influence of intersecting identities and how societal responses to individual differences result in multiple marginalization (20). Further, Dis/Crit acknowledges how this double marginalization is maintained by systems of oppression in ways that exacerbate inequality and injustice for BIPOC communities (21). For example, Black and Native American children, while overrepresented in special education (22), experience significant delays in diagnosis (and underdiagnosis) of neurodevelopmental conditions (17, 23).
Neurodevelopmental conditions result from a complex interplay of biological risks, social-historical influences, and environmental factors (24, 25). Dis/Crit provides a framework for understanding how racial/ethnic disparities in prevention, assessment/diagnosis, and intervention for individuals with FASD stem from complex interactions between social determinants of health and structural racism disproportionately affecting BIPOC (26). These issues represent an urgent public health crisis. Here, we provide examples of such disparities, perspectives regarding their potential causes and conditions, and solutions to advance equitable, culturally-responsive, and evidence-based psychological and neuropsychological care of individuals with FASD (Figure 1).
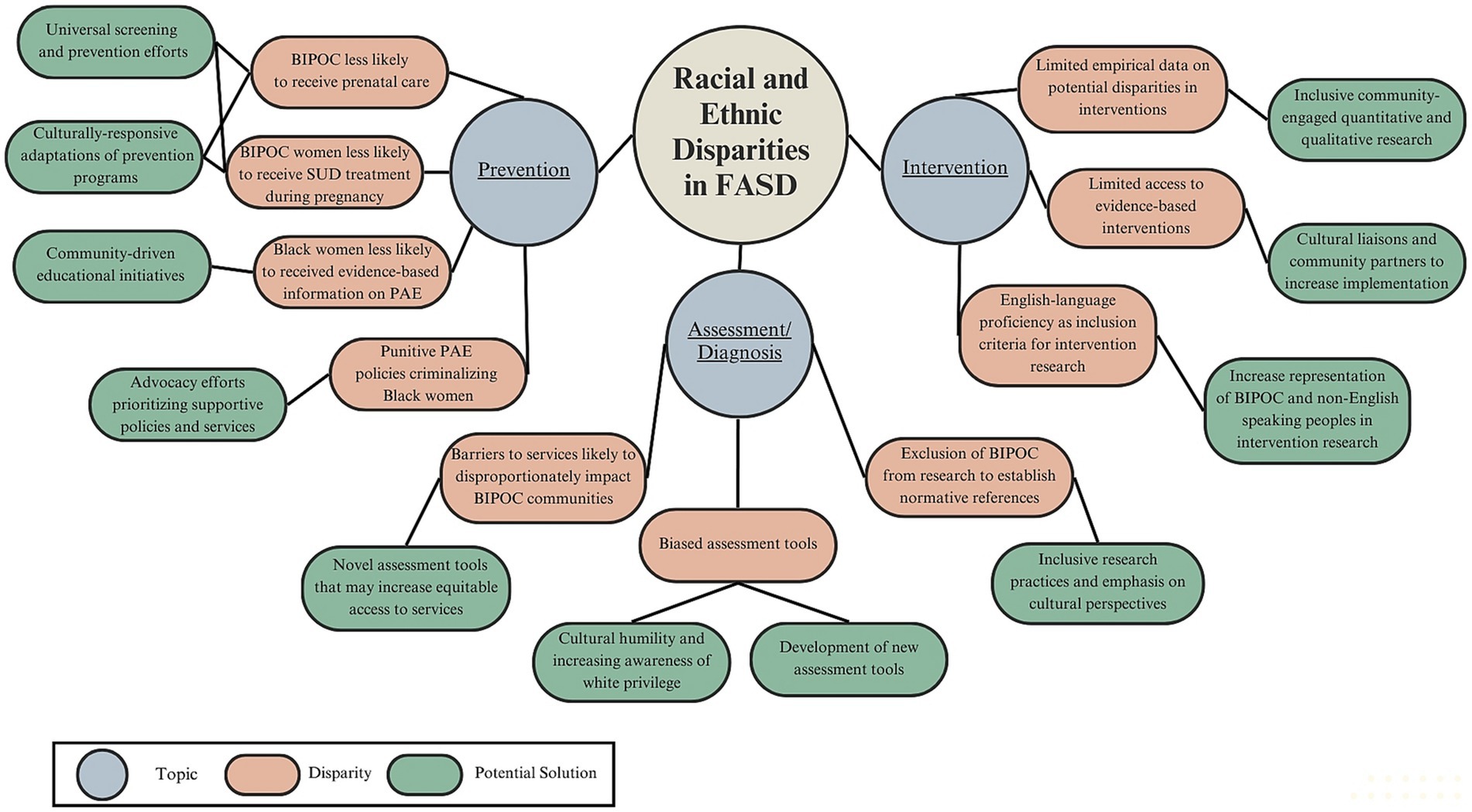
Figure 1. Graphical overview of racial and ethnic disparities in FASD within prevention, assessment/diagnosis, and interventions domains, and potential solutions.
Our authorship team recognizes the importance of acknowledging our positionality. Our racial/ethnic backgrounds consist of individuals who are White, Black, Native American, and non-Hispanic. Multiple authors are also individuals with FASD. We acknowledge the power dynamics inherent in research, particularly within marginalized communities, and aim to approach this topic with cultural humility.
Racial and ethnic disparities in prenatal care, substance use disorder treatment, and evidence-based information
Mitigating racial/ethnic disparities in FASD necessitates an initial focus on the prevention of alcohol-exposed pregnancies (AEPs). Racial/ethnic differences in AEP are understudied and findings have been equivocal. Several studies suggest an increased risk of AEPs in racial/ethnic minorities (27–30) whereas others suggest White individuals are more likely to have an AEP (31, 32).
Aligning with the Dis/Crit framework, it is imperative to recognize and address historical and ongoing racially-biased practices contributing to a disproportionate incidence of AEPs among BIPOC communities on a global scale. Examples of this include intergenerational trauma in Indigenous communities (33–35) and practices such as the “dop system” in South Africa, originating during apartheid, whereby White farm owners used alcohol as a form of labor payment and social control of marginalized racial groups (36–38).
Significant racial/ethnic disparities are evident in prenatal care, receipt of evidence-based AEP information, and interventions for substance and alcohol use disorders (SUDs and AUDs). Importantly, historical and ongoing race-based and intergenerational trauma impacts multiple non-White and BIPOC communities including Black/African Americans, American Indians and Alaska Natives, and people of Jewish and Asian ancestry (39). This historical context contributes higher rates of stress and disproportionate access to resources for marginalized groups (40). The prenatal period is a pivotal juncture for preventing AEPs (41). BIPOC women are less likely than White women to receive prenatal care (42) and experience disparities in respect and autonomy within healthcare settings (43) potentially contributing to underutilization of services (44). Regarding receipt of evidence-based prenatal education, the literature is mixed. Some research has suggested Black women are less likely to receive evidence-based information regarding the negative impacts of AEPs compared to White women (45). However, recent data indicate BIPOC and low-SES women are more likely to receive comprehensive prenatal health education (including AEP information) than White and economically advantaged counterparts despite experiencing greater risks for adverse birth outcomes suggesting such prenatal health education is inadequately addressing these disparities (46). Moreover, significant gaps in receipt of mental health treatment exist for Black and Hispanic pregnant women with SUDs when compared to White women, even after controlling for education level, income, age, health insurance, and urbanicity (47). Pregnant BIPOC with AUDs are less likely to seek treatment, partially due to risk of victimization stemming from policies pertaining to AEPs (48–50). These policies may heighten the risk of criminalization among BIPOC women and reduce reporting for fear of losing their children or other punitive measures (50).
Potential solutions
To reduce disparities in the receipt of evidence-based prenatal information and SUDs care, mental health providers can incorporate universal screening techniques, following the Screening, Brief Intervention, and Referral to Treatment (SBIRT) model (51). These efforts should include reflective and supervisory practice regarding racial/ethnic stereotyping potentially influencing disparities. Moreover, mental health practitioners can support open discussions about PAE by utilizing SAMHSA’s guidelines to reduce stigmatizing language (52) while being mindful of their respective state’s policies on AEPs and mandated child welfare reporting. Advocacy efforts should support policies prioritizing supportive over punitive actions for pregnant individuals who report an AEP. Efforts to reduce racial/ethnic disparities in AEPs should also involve tailored, culturally-responsive adaptations of prevention programs. Emphasis should be placed on collaboration with individuals with living experience (i.e., those with AEPs and BIPOC) as well as qualitative research methodology to understand experiences of intersectionality within systems of care. For example, Gonzales et al., emphasizes the importance of community-level healing practices (i.e., drumming, talking circles, and sharing practices related to pregnancy and parenting) to address racialized trauma as a key factor in contributing to AEPs in a Native American community (53). This underscores the need for culturally-informed, trauma-responsive training for mental health practitioners and those providing prenatal care. Finally, community-driven initiatives such as Proof Alliance’s program “Our Children Are Sacred” (54), which disseminates information on AEPs while addressing the historical trauma and racism experienced by Indigenous communities, will be important.
Racial and ethnic disparities in assessment and diagnosis of FASD
The diagnostic process of FASD considers what is known about PAE; brain differences; smaller growth in height, weight, and head circumference; distinctive facial features (thin upper lip, smooth philtrum, short eye openings); and below average performance (i.e., 1.5–2 standard deviations below the mean depending on the diagnostic system) on norm-referenced neurocognitive and neurobehavioral measures (2, 55). Early diagnosis and intervention are crucial in supporting long-term functional outcomes (56, 57) and preventing adverse outcomes such as school disruption, mental health challenges, and trouble with the law, which have disproportionate consequences for BIPOC individuals. However, numerous barriers make early and accurate diagnosis a substantial hurdle for many individuals (58, 59). These barriers include a high cost of services, lack of healthcare access, lack of trained clinicians, the “hidden” nature of the condition for individuals who do not have facial and growth differences (25, 60), and stigma regarding AEPs (61–63). Such healthcare disparities disproportionately affect BIPOC, low-SES, and rural communities (64–66)—communities already at high risk for unequal access to prevention and early intervention. To our knowledge there are no empirical studies addressing potential ways in which race, dis/ability status, and other factors may contribute to healthcare inequalities for people with FASD and their families.
Psychologists and neuropsychologists play an important role in FASD diagnosis by collecting developmental histories, performing and interpreting neuropsychological assessments, and providing recommendations for services (67). The fields of psychology and neuropsychology have deep roots in structural racism. For example, many current cognitive performance assessments have been criticized for contributing to racially-biased educational placement of BIPOC and low-SES students in special education (68, 69).
Importantly, BIPOC have been systematically excluded from research aimed at determining normative references of typical development, which likely contributes to inequality in rates of FASD diagnosis (12). Normative references for lip/philtrum ratings are available only for children of European, Black/African American, and South African mixed-race heritage (70, 71). Although the three cardinal facial features associated with PAE are present across racial/ethnic groups, threshold cutoffs for diagnosis vary by race/ethnicity (71–73). Clinicians often have to use their judgment to decide which racial guide to use for individuals whose race is not represented in existing guides. Similarly, available normative data for head circumference and palpebral fissure length (eye openings) is based on smaller samples predominantly composed of individuals of European heritage (74, 75). Moreover, factors such as stereotype threat can lead to underestimation of cognitive abilities in BIPOC (76, 77) suggesting they may be more likely to meet cutoffs used to quantify below average performance in FASD diagnostic systems.
Potential solutions
First, it is imperative that we strive to improve representation and normative data for the tools we use to inform assessment and diagnosis of individuals of diverse racial/ethnic backgrounds (25, 73). Moreover, factors such as cultural, linguistic, and SES background; quality of and access to educational opportunities; test familiarity; stereotype threat; and appropriateness of test norms should be thoughtfully considered as potential contributors to observed performance on neuropsychological assessment (78). Use of technologies such as digital and mobile health could also increase access to assessment and diagnosis for families in rural and under-resourced communities (79), although similar attention is needed to possible normative limitations and content biases. Efforts to reduce racial/ethnic disparities in assessment and diagnosis of FASD must also include a concerted effort to address the systemic racism and White privilege ingrained in medicine (80, 81). White psychologists/neuropsychologists must acknowledge the “invisible knapsack” of White privilege (82) and its potential role in engendering a rational mistrust of medical providers for BIPOC. Aligned with the Dis/Crit framework, researchers and clinicians should also consider how ableist language (e.g., “impairment,” “deficit”) as used in current FASD diagnostic systems may contribute to stigmatization as well as the intersectionality of receiving an FASD diagnosis and identifying as BIPOC (18). Additionally, centering research efforts on understanding cultural perspectives of FASD (83), perspectives of individuals with living experiences (84), and how the intersection of race and dis/ability may further affect access to systems of care will be crucial to ensuring research outcomes are valuable to and address the priorities of the FASD community.
Disparities in neurodevelopmental and behavioral interventions for people with FASD
Despite a considerably high prevalence, few interventions have been developed to support symptoms of FASD, and a majority of existing interventions have not yet progressed to active community implementation. A comprehensive review of the literature on interventions for FASD is beyond the scope of this paper (85, 86). To our knowledge, empirical studies on potential racial and ethnic disparities in interventions for FASD have not been published despite clear evidence for such disparities in neurodevelopmental disability literature more broadly (87–89). However, it is critical to acknowledge FASD intervention research and clinical services are rooted in the tradition of Western medicine, with limited access to services globally (85). Furthermore, numerous barriers impede evidence-based intervention for FASD across diverse cultures, including absence of local programs, housing of interventions in universities/medical centers who historically mistreated and oppressed BIPOC individuals, and failure of existing interventions to address individual differences at the intersection of dis/ability and culture (90).
A majority of interventions for FASD have been developed in North America (86) and many require English language proficiency as an inclusion criterion. While not specific to FASD intervention research, others have noted an increasing trend of English language requirements in behavioral clinical trials broadly (91). This constitutes a major limitation of current intervention research in the field of FASD likely to disproportionately affect BIPOC, non-English speaking, and bi/multilingual individuals and is likely to reduce the generalizability of intervention research. Many existing interventions are also caregiver-driven, which may hinder access for single-parent households or parents with multiple jobs.
Potential solutions
The inclusion of BIPOC and those with living experiences of FASD is crucial to community-engaged and inclusive intervention research (92). The use of qualitative methodologies to understand intersecting experiences of race and dis/ability in their entirety should be a first step in addressing disparities. Consistent with the Dis/Crit framework, it is imperative to include perspectives of individuals at the intersection of dis/ability and BIPOC identities as there are increased health disparities and unique experiences within systems for those holding such intersecting identities (93). Research advisory boards and community-based participatory research can be invaluable in ensuring the voices of community members are incorporated into ongoing research efforts (94–96). To highlight the need for community-engaged research, the annual meeting of the Fetal Alcohol Spectrum Disorder Study Group in 2022 featured a panel discussion including two adults with living experiences of FASD (“Nothing about us without us”) (97). A detailed qualitative analysis of best practices for community-engaged research with adults with FASD is currently under development (98).
Researchers should consider ways in which new interventions can be developed and implemented in partnership with communities to be person-centered, culturally-appropriate, and accessible in a variety of languages (85). Diverse and representative research teams that include BIPOC, individuals with FASD, and BIPOC individuals with FASD may also bridge these partnerships and provide valuable perspectives. Beyond community partnership, researchers should focus intervention outcomes on community members’ specific priorities and consider the complex ways race and cultural identities may intersect with such priorities. Cultural liaisons (e.g., trained interventionists/providers who are culturally-affiliated) may also be consulted to assist with implementing interventions and addressing cultural differences (90). Additionally, mobile health initiatives such as the Families Moving Forward Connect app and the My Health Coach app for adults with FASD (99–101), which focus on supporting parents and adults in managing health needs for individuals with FASD, may increase access to evidence-based information and facilitate community support networks. Careful research is planned to determine whether cultural adaptations would be beneficial. Lastly, strategies to increase BIPOC representation in research such as building community trust, employing equitable recruiting methods, and offering information in multiple languages (102, 103) will help address racial/ethnic disparities in FASD intervention work. Implementation science guidelines addressing structural racism and health disparities can also guide scientifically sound intervention work (104, 105).
Discussion
A number of important factors have contributed to emerging evidence for racial/ethnic disparities in psychological care for individuals with FASD. While our understanding is far from complete, Dis/Crit provides a useful framework for conceptualizing the causes and conditions of such disparities and informing a path forward (21). In addition to the specific recommendations for potential solutions outlined above, several broad approaches will support systems-level changes coordinated across disciplines and settings.
It is of utmost importance to include individuals with living experiences of dis/ability (including FASD) and BIPOC at all levels of research aimed at understanding and supporting individuals with FASD. Community-engaged research practices are needed to foster collaborative dialogues with community members and highlight their cultural knowledge and living-experiences to better understand disparities within these communities. Moreover, community-engagement would support equitable research processes that empower individuals with FASD rather than further stigmatize/marginalize them. For example, adults with FASD who are authors on the current paper suggest a future aim of understanding how religion ties into cultural differences for people with FASD and how this may impact the diagnosis and intervention. Researchers and clinicians must strive for inclusivity, cultural humility, and equitable access to resources so individuals with FASD and their communities are supported in navigating each stage from prevention to intervention regardless of race/ethnicity. Equally important is diversification of the (predominantly White) psychology workforce in the United States (106, 107), which will allow for individuals seeking clinical services to feel represented and understood, help in reducing language barriers, and potentially lead to increased services globally. Importantly, communication and collaboration across systems of care (i.e., medical professionals and educators) is crucial in reducing disparities and promoting early and accurate identification of FASD. As primary care providers and other professionals (e.g., educators) are often at the forefront of care, psychologists and mental health professionals could offer support on early detection of AEP and FASD, provide referral resources, and intervention. Lastly, further research is needed to understand cultural perceptions and understanding of FASD (108), which could potentially increase stigmatization and create additional barriers to care for individuals with FASD (109–111). In addition to understanding cultural perceptions of the challenges of individuals with living experience of FASD and their families/caregivers, it will be important to focus on the strengths and resilience of the FASD community (112, 113).
Conclusion
In sum, racial/ethnic disparities in psychological care for individuals with FASD represent important challenges to the field and will require coordinated, collaborative, and inclusive efforts to overcome. We hope that increased awareness will foster discussion and stimulate creative solutions to improve equitable, culturally-responsive, and evidence-based psychological services and support for individuals with FASD and their families.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MR: Conceptualization, Visualization, Writing – original draft, Writing – review & editing. BG: Visualization, Writing – original draft, Writing – review & editing. AR: Writing – original draft, Writing – review & editing. CK-T: Writing – original draft, Writing – review & editing. ES: Writing – original draft, Writing – review & editing. EW: Writing – original draft, Writing – review & editing. JM: Writing – original draft, Writing – review & editing. EH: Writing – original draft, Writing – review & editing. MM: Writing – original draft, Writing – review & editing. SA: Writing – original draft, Writing – review & editing. CP: Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This article was made possible by a private donation to CP.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
FASD, fetal alcohol spectrum disorder; PAE, prenatal alcohol exposure; Dis/Crit, Dis/ability Studies and Critical Race Theory; BIPOC, Black, Indigenous and People of Color; SES, Socio-economic Status; AEPs, alcohol-exposed pregnancies; AUD, alcohol use disorder; SUD, substance use disorder.
References
1. May, PA, Chambers, CD, Kalberg, WO, Zellner, J, Feldman, H, Buckley, D, et al. Prevalence of fetal alcohol Spectrum disorders in 4 US communities. JAMA. (2018) 319:474–82. doi: 10.1001/jama.2017.21896
2. Hoyme, HE, Kalberg, WO, Elliott, AJ, Blankenship, J, Buckley, D, Marais, AS, et al. Updated clinical guidelines for diagnosing fetal alcohol Spectrum disorders. Pediatr Int. (2016) 138:e20154256. doi: 10.1542/peds.2015-4256
3. Wozniak, JR, Riley, EP, and Charness, ME. Clinical presentation, diagnosis, and management of fetal alcohol spectrum disorder. Lancet Neurol. (2019) 18:760–70. doi: 10.1016/S1474-4422(19)30150-4
4. Mattson, SN, Bernes, GA, and Doyle, LR. Fetal alcohol Spectrum disorders: a review of the neurobehavioral deficits associated with prenatal alcohol exposure. Alcohol Clin Exp Res. (2019) 43:1046–62. doi: 10.1111/acer.14040
5. Coles, CD, Grant, TM, Kable, JA, Stoner, SA, and Perez, ACollaborative Initiative on Fetal Alcohol Spectrum Disorders. Prenatal alcohol exposure and mental health at midlife: a preliminary report on two longitudinal cohorts. Alcohol Clin Exp Res. (2022) 46:232–42. doi: 10.1111/acer.14761
6. McLachlan, K, Flannigan, K, Temple, V, Unsworth, K, and Cook, JL. Difficulties in daily living experienced by adolescents, transition-aged youth, and adults with fetal alcohol Spectrum disorder. Alcohol Clin Exp Res. (2020) 44:1609–24. doi: 10.1111/acer.14385
7. Moore, EM, and Riley, EP. What happens when children with fetal alcohol Spectrum disorders become adults? Curr Dev Disord Rep. (2015) 2:219–27. doi: 10.1007/s40474-015-0053-7
8. Popova, S, Stade, B, Bekmuradov, D, Lange, S, and Rehm, J. What do we know about the economic impact of fetal alcohol spectrum disorder? A systematic literature review. Alcohol Alcohol. (2011) 46:490–7. doi: 10.1093/alcalc/agr029
9. Popova, S, Lange, S, Burd, L, and Rehm, J. The economic burden of fetal alcohol Spectrum disorder in Canada in 2013. Alcohol Alcohol. (2016) 51:367–75. doi: 10.1093/alcalc/agv117
10. Chasnoff, IJ, Wells, AM, and King, L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. (2015) 135:264–70. doi: 10.1542/peds.2014-2171
11. McLennan, JD . Misattributions and potential consequences: the case of child mental health problems and fetal alcohol Spectrum disorders. Can J Psychiatr. (2015) 60:587–90. doi: 10.1177/070674371506001210
12. Abel, E . An update on incidence of FAS: FAS is not an equal opportunity birth defect. Neurotoxicol Teratol. (1995) 17:437–43. doi: 10.1016/0892-0362(95)00005-C
13. Morgan, PL, Staff JHillemeier, MM, Farkas, G, and Maczuga, S. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics. (2013) 132:85–93. doi: 10.1542/peds.2012-2390
14. Shi, Y, Hunter Guevara, LR, Dykhoff, HJ, Sangaralingham, LR, Phelan, S, Zaccariello, MJ, et al. Racial disparities in diagnosis of attention-deficit/hyperactivity disorder in a US National Birth Cohort. JAMA Netw Open. (2021) 4:e210321. doi: 10.1001/jamanetworkopen.2021.0321
15. Liu, BM, Paskov, K, Kent, J, McNealis, M, Sutaria, S, Dods, O, et al. Racial and ethnic disparities in geographic access to autism resources across the US. JAMA Netw Open. (2023) 6:e2251182. doi: 10.1001/jamanetworkopen.2022.51182
16. Durkin, MS, Maenner, MJ, Baio, J, Christensen, D, Daniels, J, Fitzgerald, R, et al. Autism Spectrum disorder among US children (2002–2010): socioeconomic, racial, and ethnic disparities. Am J Public Health. (2017) 107:1818–26. doi: 10.2105/AJPH.2017.304032
17. Mandell, DS, Wiggins, LD, Carpenter, LA, Daniels, J, DiGuiseppi, C, Durkin, MS, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. Am J Public Health. (2009) 99:493–8. doi: 10.2105/AJPH.2007.131243
18. Annamma, SA, Connor, D, and Ferri, B. Dis/ability critical race studies (DisCrit): theorizing at the intersections of race and dis/ability In: Edward, T, David, G, and Gloria, L-B editors. Foundations of critical race theory in education. 3rd ed. New York, New York USA: Routledge (2023)
19. Goodley, D . The dis/ability complex. DiGeSt J Divers Gender Stud. (2018) 5:5–22. doi: 10.11116/digest.5.1.1
20. Crenshaw, K . Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. (1991) 43:1241–99. doi: 10.2307/1229039
21. Annamma, SA, Connor, D, and Ferri, B. Dis/ability critical race studies (DisCrit): theorizing at the intersections of race and dis/ability. Race Ethn Educ. (2013) 16:1–31. doi: 10.1080/13613324.2012.730511
22. Morgan, H . Misunderstood and mistreated: students of color in special education. VoR. (2020) 3:71–81. doi: 10.32623/3.10005
23. Constantino, JN, Abbacchi, AM, Saulnier, C, Klaiman, C, Mandell, DS, Zhang, Y, et al. Timing of the diagnosis of autism in African American children. Pediatrics. (2020) 146:e20193629. doi: 10.1542/peds.2019-3629
24. Boivin, MJ, Kakooza, AM, Warf, BC, Davidson, LL, and Grigorenko, EL. Reducing neurodevelopmental disorders and disability through research and interventions. Nature. (2015) 527:S155–60. doi: 10.1038/nature16029
25. Popova, S, Charness, ME, Burd, L, Crawford, A, Hoyme, HE, Mukherjee, RAS, et al. Fetal alcohol spectrum disorders. Nat Rev Dis Primers. (2023) 9:1–21. doi: 10.1038/s41572-023-00420-x
26. Krieger, N . Discrimination and health inequities. Int J Health Serv. (2014) 44:643–710. doi: 10.2190/HS.44.4.b
27. Morris, DS, Tenkku, LE, Salas, J, Xaverius, PK, and Mengel, MB. Exploring pregnancy-related changes in alcohol consumption between black and white women. Alcohol Clin Exp Res. (2008) 32:505–12. doi: 10.1111/j.1530-0277.2007.00594.x
28. Oh, SS, Kang, B, Park, J, Kim, S, Park, EC, Lee, SH, et al. Racial/ethnic disparity in association between fetal alcohol syndrome and alcohol intake during pregnancy: multisite retrospective cohort study. JMIR Public Health Surveill. (2023) 9:e45358. doi: 10.2196/45358
29. Rockhold, MN, Kautz-Turnbull, C, Smith, A, Shimp, R, Handley, E, Cerulli, C, et al. The role of maternal child maltreatment, intimate partner violence, social support, and race on prenatal subtance exposure. Under review.
30. Russo, D, Purohit, V, Foudin, L, and Salin, M. Workshop on alcohol use and health disparities 2002: a call to arms. Alcohol. (2004) 32:37–43. doi: 10.1016/j.alcohol.2004.01.003
31. Ethen, MK, Ramadhani, TA, Scheuerle, AE, Canfield, MA, Wyszynski, DF, Druschel, CM, et al. Alcohol consumption by women before and during pregnancy. Matern Child Health J. (2009) 13:274–85. doi: 10.1007/s10995-008-0328-2
32. O’Keeffe, LM, Kearney, PM, McCarthy, FP, Khashan, AS, Greene, RA, North, RA, et al. Prevalence and predictors of alcohol use during pregnancy: findings from international multicentre cohort studies. BMJ Open. (2015) 5:e006323. doi: 10.1136/bmjopen-2014-006323
33. Popova, S, Lange, S, Poznyak, V, Chudley, AE, Shield, KD, Reynolds, JN, et al. Population-based prevalence of fetal alcohol spectrum disorder in Canada. BMC Public Health. (2019) 19:845. doi: 10.1186/s12889-019-7213-3
34. Wolfson, L, Poole, N, Morton Ninomiya, M, Rutman, D, Letendre, S, Winterhoff, T, et al. Collaborative action on fetal alcohol Spectrum disorder prevention: principles for enacting the truth and reconciliation commission call to action #33. Int J Environ Res Public Health. (2019) 16:1589. doi: 10.3390/ijerph16091589
35. Yousefi, N, and Chaufan, C. ‘Think before you drink’: challenging narratives on foetal alcohol spectrum disorder and indigeneity in Canada. Health. (2022) 26:622–42. doi: 10.1177/13634593211038527
36. Goliath, V . Narratives of a historically marginalized south African community and its implications for drug abuse prevention In: Annaline, K, Nevashnee, P, and Veonna, G editors. Critical social work studies in South Africa; prospects and challenges. Stellenbosch South Africa: African Sun Media (2022). 233–57.
37. London, L . The `dop’ system, alcohol abuse and social control amongst farm workers in South Africa: a public health challenge. Soc Sci Med. (1999) 48:1407–14. doi: 10.1016/S0277-9536(98)00445-6
38. May, PA, Marais, AS, De Vries, M, Hasken, JM, Stegall, JM, Hedrick, DM, et al. The Dop system of alcohol distribution is dead, but It’s legacy lives on…. Int J Environ Res Public Health. (2019) 16:3701. doi: 10.3390/ijerph16193701
39. Fitzgerald, H, Johnson, D, Allen, J, Villarruel, F, and Qin, D. Historical and race-based trauma: resilience through family and community. Adv. Resil. Sci. (2021) 2:215–23. doi: 10.1007/s42844-021-00048-4
40. Salihu, HM, Salinas-Miranda, AA, King, LM, Dongarwar, D, Yusuf, KK, Ibrahimi, S, et al. Racism, psycho-social stress, and health-related quality of life. Int J MCH AIDS. (2020) 9:73–6. doi: 10.21106/ijma.339
41. Chang, G . Screening and brief intervention in prenatal care settings. Alcohol Res Health. (2004) 28:80–4.
42. Bryant, A, Worjoloh, A, Caughey, AB, and Washington, AE. Racial ethnic disparities in obstetric outcomes and care prevalence and determinants. Am J Obstet Gynecol. (2010) 202:335–43. doi: 10.1016/j.ajog.2009.10.864
43. Ibrahim, BB, Vedam, S, Illuzzi, J, Cheyney, M, and Kennedy, HP. Inequities in quality perinatal care in the United States during pregnancy and birth after cesarean. PLoS One. (2022) 17:e0274790. doi: 10.1371/journal.pone.0274790
44. Gadson, A, Akpovi, E, and Mehta, PK. Exploring the social determinants of racial/ethnic disparities in prenatal care utilization and maternal outcome. Semin Perinatol. (2017) 41:308–17. doi: 10.1053/j.semperi.2017.04.008
45. Kogan, MD, Kotelchuck, M, Alexander, GR, and Johnson, WE. Racial disparities in reported prenatal care advice from health care providers. Am J Public Health. (1994) 84:82–8. doi: 10.2105/AJPH.84.1.82
46. Nguyen, MN, Siahpush, M, Grimm, BL, Singh, GK, and Tibbits, MK. Women from racial or ethnic minority and low socioeconomic backgrounds receive more prenatal education: results from the 2012 to 2014 pregnancy risk assessment monitoring system. Birth. (2019) 46:157–65. doi: 10.1111/birt.12394
47. Salameh, TN, Hall, LA, Crawford, TN, Staten, RR, and Hall, MT. Racial/ethnic differences in mental health treatment among a national sample of pregnant women with mental health and/or substance use disorders in the United States. J Psychosom Res. (2019) 121:74–80. doi: 10.1016/j.jpsychores.2019.03.015
48. Paltrow, LM, and Flavin, J. Arrests of and forced interventions on pregnant women in the United States, 1973–2005: implications for Women’s legal status and public health. J Health Polit Policy Law. (2013) 38:299–343. doi: 10.1215/03616878-1966324
49. Roberts, SCM, Zahnd, E, Sufrin, C, and Armstrong, MA. Does adopting a prenatal substance use protocol reduce racial disparities in CPS reporting related to maternal drug use? A California case study. J Perinatol. (2015) 35:146–50. doi: 10.1038/jp.2014.168
50. Roberts, SCM, Mericle, AA, Subbaraman, MS, Thomas, S, Treffers, RD, Delucchi, KL, et al. Differential effects of pregnancy-specific alcohol policies on drinking among pregnant women by race/ethnicity. Health Equity. (2018) 2:356–65. doi: 10.1089/heq.2018.0059
51. Agerwala, SM, and McCance-Katz, EF. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: a brief review. J Psychoactive Drugs. (2012) 44:307–17. doi: 10.1080/02791072.2012.720169
52. Substance Abuse and Mental Health Services Administration (SAMHSA). TIP 58: addressing fetal alcohol spectrum disorders (FASD). (2021) Available at: https://www.samhsa.gov/resource/ebp/tip-58-addressing-fetal-alcohol-spectrum-disorders-fasd
53. Gonzales, KL, Jacob, MM, Mercier, A, Heater, H, Nall Goes Behind, L, Joseph, J, et al. An indigenous framework of the cycle of fetal alcohol spectrum disorder risk and prevention across the generations: historical trauma, harm and healing. Ethn Health. (2021) 26:280–98. doi: 10.1080/13557858.2018.1495320
54. Proof Alliance. Our children are sacred. (2023). Available at: https://www.proofalliance.org/support/native-communities/
55. Coles, CD, Gailey, AR, Mulle, JG, Kable, JA, Lynch, ME, and Jones, KL. A comparison among 5 methods for the clinical diagnosis of fetal alcohol Spectrum disorders. Alcohol Clin Exp Res. (2016) 40:1000–9. doi: 10.1111/acer.13032
56. Popova, S, Dozet, D, and Burd, L. Fetal alcohol Spectrum disorder: can we change the future? Alcohol Clin Exp Res. (2020) 44:815–9. doi: 10.1111/acer.14317
57. Reid, N, Dawe, S, Shelton, D, Harnett, P, Warner, J, Armstrong, E, et al. Systematic review of fetal alcohol Spectrum disorder interventions across the life span. Alcohol Clin Exp Res. (2015) 39:2283–95. doi: 10.1111/acer.12903
58. Coles, CD, Bandoli, G, Kable, JA, Del Campo, M, Suttie, M, and Chambers, CD. Comparison of three systems for the diagnosis of fetal alcohol spectrum disorders in a community sample. Alcohol Clin Exp Res. (2023) 47:370–81. doi: 10.1111/acer.14999
59. Grubb, M, Golden, A, Withers, A, Vellone, D, Young, A, and McLachlan, K. Screening approaches for identifying fetal alcohol spectrum disorder in children, adolescents, and adults: a systematic review. Alcohol Clin Exp Res. (2021) 45:1527–47. doi: 10.1111/acer.14657
60. Mather, M . The invisible disability. Adopt Foster. (2015) 39:197–200. doi: 10.1177/0308575915594983
61. Corrigan, PW, Lara, JL, Shah, BB, Mitchell, KT, Simmes, D, and Jones, KL. The public stigma of birth mothers of children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. (2017) 41:1166–73. doi: 10.1111/acer.13381
62. Corrigan, PW, Shah, BB, Lara, JL, Mitchell, KT, Combs-Way, P, Simmes, D, et al. Stakeholder perspectives on the stigma of fetal alcohol spectrum disorder. Addict Res Theory. (2019) 27:170–7. doi: 10.1080/16066359.2018.1478413
63. Roozen, S, Stutterheim, SE, Bos, AER, Kok, G, and Curfs, LMG. Understanding the social stigma of fetal alcohol Spectrum disorders: from theory to interventions. Found Sci. (2022) 27:753–71. doi: 10.1007/s10699-020-09676-y
64. Dubay, LC, and Lebrun, LA. Health, behavior, and health care disparities: disentangling the effects of income and race in the United States. Int J Health Serv. (2012) 42:607–25. doi: 10.2190/HS.42.4.c
65. Hartley, D . Rural health disparities, population health, and rural culture. Am J Public Health. (2004) 94:1675–8. doi: 10.2105/AJPH.94.10.1675
66. Nelson, A . Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. (2002) 94:666–8.
67. Barnes, G, Moore, E, Vaurio, L, and Mattson, S. Fetal alcohol spectrum disorders In: Miriam, HB, Robin, LP, Douglas Ris, M, Gerry Taylor, H, and Keith Owen Yeates, KO editors. Pediatric neuropsychology: research, theory, and practice. 3rd ed. New York, New York USA: Guilford Publications (2022). 179–205.
68. Holden, LR, and Hart, SA. Intelligence can be used to make a more equitable society but only when properly defined and applied. J Intelligence. (2021) 9:57. doi: 10.3390/jintelligence9040057
69. Holden, LR, and Tanenbaum, GJ. Modern assessments of intelligence must be fair and equitable. J Intelligence. (2023) 11:126. doi: 10.3390/jintelligence11060126
70. Astley, SJ . Validation of the fetal alcohol spectrum disorder (FASD) 4-digit diagnostic code. J Popl Ther Clin Pharmacol. (2013) 20 Available at: https://jptcp.com
71. Hoyme, HE, Hoyme, DB, Elliott, AJ, Blankenship, J, Kalberg, WO, Buckley, D, et al. A south African mixed race lip/philtrum guide for diagnosis of fetal alcohol spectrum disorders. Am J Med Genet A. (2015) 167:752–5. doi: 10.1002/ajmg.a.37023
72. May, PA, Gossage, JP, Smith, M, Tabachnick, BG, Robinson, LK, Manning, M, et al. Population differences in dysmorphic features among children with fetal alcohol spectrum disorders. J Dev Behav Pediatr. (2010) 31:304–16. doi: 10.1097/DBP.0b013e3181dae243
73. Tsang, TW, Laing-Aiken, Z, Latimer, J, Fitzpatrick, J, Oscar, J, Carter, M, et al. Digital assessment of the fetal alcohol syndrome facial phenotype: reliability and agreement study. BMJ Paediatr Open. (2017) 1:e000137. doi: 10.1136/bmjpo-2017-000137
74. Nellhaus, G . Head circumference from birth to eighteen years. Practical composite international and interracial graphs. Pediatrics. (1968) 41:106–14. doi: 10.1542/peds.41.1.106
75. Stromland, K, Chen, Y, Norberg, T, and Michael, G. Reference values of facial features in Scandinavian children measured with a range-camera technique (1998) 33:59–65. doi: 10.1080/02844319950159631,
76. Byrd, D, Arentoft, A, Scheiner, D, Westerveld, M, and Baron, IS. State of multicultural neuropsychological assessment in children: current research issues. Neuropsychol Rev. (2008) 18:214–22. doi: 10.1007/s11065-008-9065-y
77. VanLandingham, H, Ellison, RL, Laique, A, Cladek, A, Khan, H, Gonzalez, C, et al. A scoping review of stereotype threat for BIPOC: cognitive effects and intervention strategies for the field of neuropsychology. Clin Neuropsychol. (2022) 36:503–22. doi: 10.1080/13854046.2021.1947388
78. Olson, K, and Jacobson, K. Cross-cultural considerations in pediatric neuropsychology: a review and call to attention. Appl Neuropsychol Child. (2015) 4:166–77. doi: 10.1080/21622965.2013.830258
79. Suttie, M . Image analysis of neurofacial effects of prenatal alcohol exposure In: Alcohol and alcohol-related diseases. Cham: Springer International Publishing (2023)
80. Bailey, ZD, Feldman, JM, and Bassett, MT. How structural racism works—racist policies as a root cause of U.S. racial health inequities. N Engl J Med. (2021) 384:768–73. doi: 10.1056/NEJMms2025396
81. Elias, A, and Paradies, Y. The costs of institutional racism and its ethical implications for healthcare. Bioeth Inq. (2021) 18:45–58. doi: 10.1007/s11673-020-10073-0
82. Cory, JM . White privilege in neuropsychology: an ‘invisible knapsack’ in need of unpacking? Clin Neuropsychol. (2020) 35:206–18. doi: 10.1080/13854046.2020.1801845
83. Reid, N, Crawford, A, Petrenko, C, Kable, J, and Olson, HC. A family-directed approach for supporting individuals with fetal alcohol Spectrum disorders. Curr Dev Disord Rep. (2022) 9:9–18. doi: 10.1007/s40474-021-00241-1
84. Himmelreich, M, Lutke, C, and Hargrove, E. The lay of the land: fetal alcohol spectrum disorder (FASD) as a whole-body diagnosis In: Audrey, LB, and Margaret, MM editors. The Routledge handbook of social work and addictive behaviors. New York, New York, USA. (2020). 191–215.
85. Carmichael Olson, H, Pruner, M, Byington, N, and Jirikowic, T. FASD-informed care and the future of intervention In: Omar, AA-R, and Christie, LMP editors. Fetal alcohol spectrum disorders: a multidisciplinary approach Cham, Switzerland (2023) 269–362.
86. Ordenewitz, LK, Weinmann, T, Schlüter, JA, Moder, JE, Jung, J, Kerber, K, et al. Evidence-based interventions for children and adolescents with fetal alcohol spectrum disorders – a systematic review. Eur J Paediatr Neurol. (2021) 33:50–60. doi: 10.1016/j.ejpn.2021.02.001
87. Carr, T, and Lord, C. Longitudinal study of perceived negative impact in African American and Caucasian mothers of children with autism spectrum disorder. Autism. (2013) 17:405–17. doi: 10.1177/1362361311435155
88. Locke, J, Kang-Yi, CD, Pellecchia, M, Marcus, S, Hadley, T, and Mandell, DS. Ethnic disparities in school-based behavioral health service use for children with psychiatric disorders. J Sch Health. (2017) 87:47–54. doi: 10.1111/josh.12469
89. Pope, L, Light, J, and Franklin, A. Black children with developmental disabilities receive less AAC intervention than their white peers: preliminary evidence of racial disparities from a secondary data analysis. Am J Speech Lang Pathol. (2022) 31:2159–74. doi: 10.1044/2022_AJSLP-22-00079
90. Petrenko, CLM, and Alto, ME. Interventions in fetal alcohol spectrum disorders: an international perspective. Eur J Med Genet. (2017) 60:79–91. doi: 10.1016/j.ejmg.2016.10.005
91. Egleston, BL, Pedraza, O, Wong, YN, Dunbrack, RL, Griffin, CL, Ross, EA, et al. Characteristics of clinical trials that require participants to be fluent in English. Clin Trials. (2015) 12, 12:618–26. doi: 10.1177/1740774515592881
92. Fletcher-Watson, S, Brook, K, Hallett, S, Murray, F, and Crompton, CJ. Inclusive practices for neurodevelopmental research. Curr Dev Disord Rep. (2021) 8:88–97. doi: 10.1007/s40474-021-00227-z
93. Dorsey Holliman, B, Stransky, M, Dieujuste, N, and Morris, M. Disability doesn’t discriminate: health inequities at the intersection of race and disability. Front Rehabil Sci. (2023) 4:1075775. doi: 10.3389/fresc.2023.1075775
94. Adhikari, B, Pell, C, and Cheah, PY. Community engagement and ethical global health research. Global Bioethics. (2020) 31:1–12. doi: 10.1080/11287462.2019.1703504
95. Brockman, TA, Balls-Berry, JE, West, IW, Valdez-Soto, M, Albertie, ML, Stephenson, NA, et al. Researchers’ experiences working with community advisory boards: how community member feedback impacted the research. J Clin Transl Sci. (2021) 5:e117. doi: 10.1017/cts.2021.22
96. Matthews, AK, Anderson, EE, Willis, M, Castillo, A, and Choure, W. A community engagement advisory board as a strategy to improve research engagement and build institutional capacity for community-engaged research. J Clin Transl Sci. (2018) 2:66–72. doi: 10.1017/cts.2018.14
97. Petrenko, CLM, Hamre, KM, Brigman, JL, and Parnell, S. Proceedings of the 2022 annual meeting of the fetal alcohol Spectrum disorders study group. Alcohol. (2023) 113:11–20. doi: 10.1016/j.alcohol.2023.08.002
98. Speybroeck, E, Cerulli, C, Foss, J, Rio, E, Dhilla, R, Lutke, C, et al. Partnering with people with fetal alcohol spectrum disorders in research: community advisory board best practices and recommendations. Manuscript in preparation.
99. Petrenko, CL, Parr, J, Kautz, C, Tapparello, C, and Olson, HC. A Mobile health intervention for fetal alcohol Spectrum disorders (families moving forward connect): development and qualitative evaluation of design and functionalities. JMIR Mhealth Uhealth. (2020) 8:e14721. doi: 10.2196/14721
100. Petrenko, CLM, Kautz-Turnbull, CC, Roth, AR, Parr, JE, Tapparello, C, Demir, U, et al. Initial feasibility of the “families moving forward connect” Mobile health intervention for caregivers of children with fetal alcohol Spectrum disorders: mixed method evaluation within a systematic user-centered design approach. JMIR Form Res. (2021) 5:e29687. doi: 10.2196/29687
101. Speybroeck, E, Petrenko, CLM, Tapparello, C, Zhang, S, Looney, J, Lutke, C, et al. My health coach mobile health app for adults with fetal alcohol spectrum disorders: qualitative evaluation of design from key stakeholders. Manuscript under review.
102. Garnett, A, and Northwood, M. Recruitment of community-based samples: experiences and recommendations for optimizing success. Can J Nurs Res. (2022) 54:101–11. doi: 10.1177/08445621211060935
103. Shea, L, Pesa, J, Geonnotti, G, Powell, V, Kahn, C, and Peters, W. Improving diversity in study participation: patient perspectives on barriers, racial differences and the role of communities. Health Expect. (2022) 25:1979–87. doi: 10.1111/hex.13554
104. Kerkhoff, AD, Farrand, E, Marquez, C, Cattamanchi, A, and Handley, MA. Addressing health disparities through implementation science—a need to integrate an equity lens from the outset. Implement Sci. (2022) 17:13. doi: 10.1186/s13012-022-01189-5
105. Shelton, RC, Adsul, P, and Oh, A. Recommendations for addressing structural racism in implementation science: a call to the field. Ethn Dis. (2021) 31:357–64. doi: 10.18865/ed.31.S1.357
106. American Psychological Association. (2021). CWS data tool: demographics of the U.S. psychology workforce. Available at: https://www.apa.org/workforce/data-tools/demographics; https://www.apa.org
107. Grapin, SL, Bocanegra, JO, Green, TD, Lee, ET, and Jaafar, D. Increasing diversity in school psychology: uniting the efforts of institutions, faculty, students, and practitioners. Contemp Sch Psychol. (2016) 20:345–55. doi: 10.1007/s40688-016-0092-z
108. Reid, N, Hawkins, E, Liu, W, Page, M, Webster, H, Katsikitis, M, et al. Yarning about fetal alcohol spectrum disorder: outcomes of a community-based workshop. Res Dev Disabil. (2021) 108:103810. doi: 10.1016/j.ridd.2020.103810
109. Grinker, RR, Kang-Yi, CD, Ahmann, C, Beidas, RS, Lagman, A, and Mandell, DS. Cultural adaptation and translation of outreach materials on autism Spectrum disorder. J Autism Dev Disord. (2015) 45:2329–36. doi: 10.1007/s10803-015-2397-6
110. Lovelace, TS, Robertson, RE, and Tamayo, S. Experiences of African American mothers of sons with autism spectrum disorder: lessons for improving service delivery. Educ Train Aut Dev Disabil. (2018) 53:3–16. Available at: https://www.researchgate.net/publication/320426780_Experiences_of_African_American_mothers_of_sons_with_autism_spectrum_disorder_Lessons_for_improving_service_delivery#fullTextFileContent
111. Zuckerman, KE, Sinche, B, Cobian, M, Cervantes, M, Mejia, A, Becker, T, et al. Conceptualization of autism in the Latino community and its relationship with early diagnosis. J Dev Behav Pediatr. (2014) 35:522–32. doi: 10.1097/DBP.0000000000000091
112. Flannigan, K, Wrath, A, Ritter, C, McLachlan, K, Harding, KD, Campbell, A, et al. Balancing the story of fetal alcohol spectrum disorder: a narrative review of the literature on strengths. Alcoholism. (2021) 45:2448–64. doi: 10.1111/acer.14733
113. Petrenko, C, and Kautz-Turnbull, C. From surviving to thriving: a new conceptual model to advance interventions to support people with FASD across the lifespan In: Deborah, JF, and Silvia, L editors. International review of research in developmental disabilities. Amsterdam, Netherlands. (2021). 39–75.
Keywords: fetal alcohol spectrum disorder, FASD, prenatal alcohol exposure, Dis/Crit, disparities, race, ethnicity
Citation: Rockhold MN, Gimbel BA, Richardson AA, Kautz-Turnbull C, Speybroeck EL, de Water E, Myers J, Hargrove E, May M, Abdi SS and Petrenko CLM (2024) Racial and ethnic disparities in psychological care for individuals with FASD: a dis/ability studies and critical race theory perspective toward improving prevention, assessment/diagnosis, and intervention. Front. Public Health. 12:1355802. doi: 10.3389/fpubh.2024.1355802
Edited by:
Kaston D. Anderson Jr., Michigan State University, United StatesReviewed by:
Mary Lehman Held, The University of Tennessee, Knoxville, United StatesCopyright © 2024 Rockhold, Gimbel, Richardson, Kautz-Turnbull, Speybroeck, de Water, Myers, Hargrove, May, Abdi and Petrenko. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christie L. M. Petrenko, Q2hyaXN0aWVfUGV0cmVua29AdXJtYy5yb2NoZXN0ZXIuZWR1
†These authors have contributed equally to this work and share first authorship
 Madeline N. Rockhold
Madeline N. Rockhold Blake A. Gimbel
Blake A. Gimbel Alesia A. Richardson1
Alesia A. Richardson1 Carson Kautz-Turnbull
Carson Kautz-Turnbull Erik de Water
Erik de Water Julianne Myers
Julianne Myers Christie L. M. Petrenko
Christie L. M. Petrenko