- 1School of Nursing, Johns Hopkins University, Baltimore, MD, United States
- 2Research, Development, and Innovation Center, Our Lady of Fatima University, Valenzuela, Philippines
- 3Sigma Theta Tau, International Honor Society in Nursing, Indianapolis, IN, United States
- 4School of Medicine, Johns Hopkins University, Baltimore, MD, United States
- 5Department of Computer Science, Johns Hopkins University, Baltimore, MD, United States
- 6Department of Pharmaceutical and Health Economics, University of Southern California School of Pharmacy, Los Angeles, CA, United States
- 7Office of the Vice Chancellor and President, University of Wollongong, Wollongong, NSW, Australia
Background: Physical inactivity and a sedentary lifestyle among community-dwelling older adults poses a greater risk for progressive physical and cognitive decline. Mixed reality technology-driven health enhancing physical activities such as the use of virtual coaches provide an emerging and promising solution to support healthy lifestyle, but the impact has not been clearly understood.
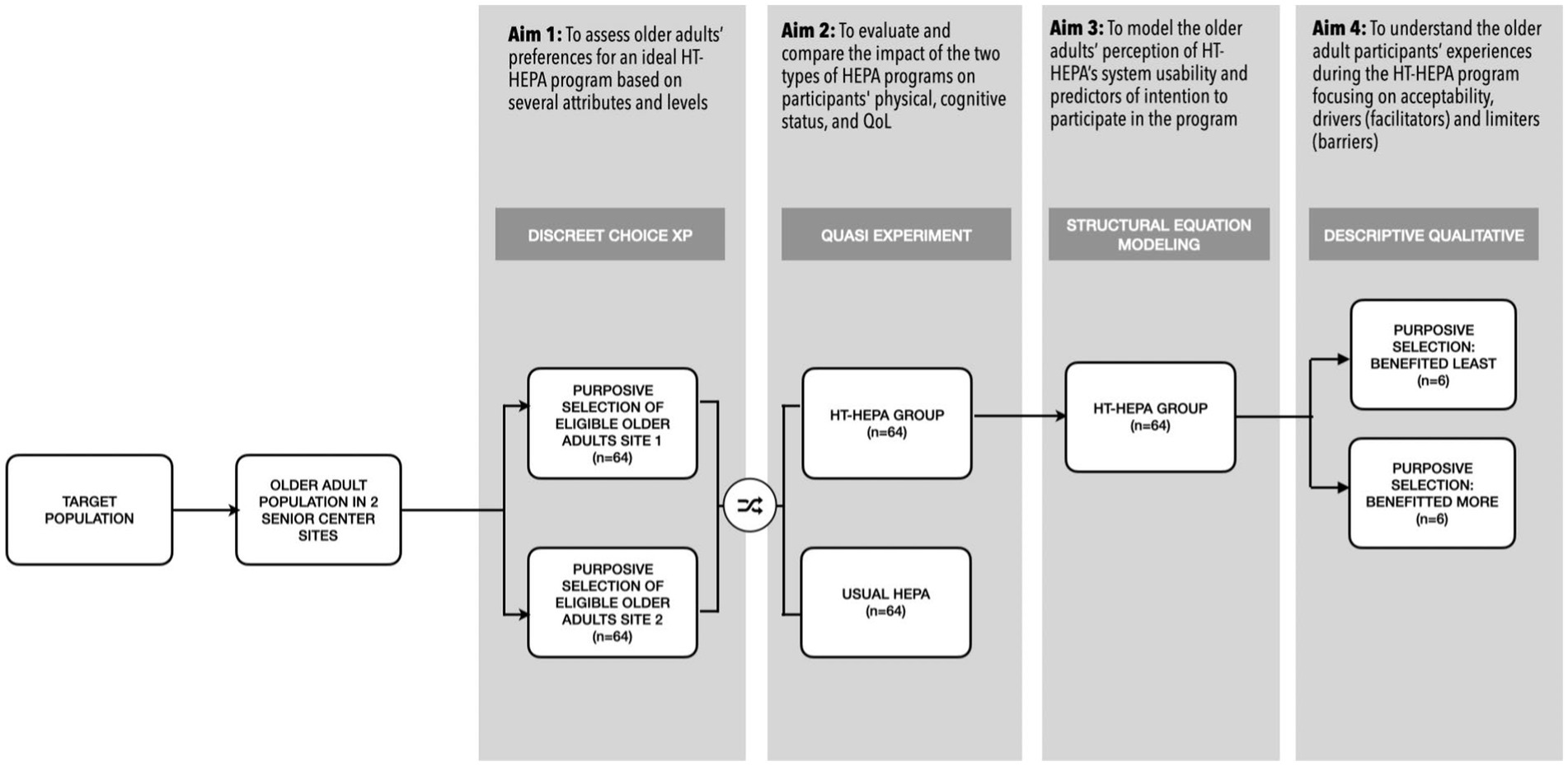
Methods and analysis: An observational explanatory sequential mixed-method research design was conceptualized to examine the potential impact of a user-preferred mixed reality technology-driven health enhancing physical activity program directed toward purposively selected community-dwelling older adults in two senior centers in the Philippines. Quantitative components of the study will be done through a discreet choice experiment and a quasi-experimental study. A total of 128, or 64 older adults in each center, will be recruited via posters at community senior centers who will undergo additional screening or health records review by a certified gerontologist to ensure safety and proper fit. Treatments (live coaching with video-based exercise and mixed reality technology-driven exercise) will be assigned to each of the two senior center sites for the quasi-experiment. The participants from the experimental group shall be involved in the discreet choice experiment, modeling, and usability evaluations. Finally, a qualitative sample of participants (n = 6) as key informants shall be obtained from the experimental group using purposive selection.
Discussion: This study protocol will examine the health impact of a promising mixed reality program in health promotion among older adults. The study utilizes a human-centered mixed method research design in technology development and evaluation in the context of developing nations.
Clinical trial registration: ClinicalTrials.gov, identifier NCT06136468.
Introduction
Physical inactivity, is common among older adults, affecting one-third of the global population (1, 2), and accounts for an estimated $53.8 billion global economic burden on the healthcare system (3, 4). It is also responsible for around 10% of global deaths annually (4). In the United States alone, almost 80% of older adults are considered inactive (5). Recent literature reviews reported a radical change in older adults’ lifestyles during the COVID-19 pandemic that further reduced physical activity (6, 7). In the Philippines, a survey reports that 67% percent of older adults are inactive, further exacerbated by the current pandemic (8, 9). The limitation on physical activity progresses physical deterioration and development of comorbidities and is considered a decisive risk factor for all-cause mortality (10). As an exemplar, the odds of COVID-19 death are 2.49 higher for inactive and sedentary patients (11). Therefore, there is a solid call to promote exercise programs that foster physical activity engagement and reduce sedentary lifestyle in older adults, most especially in the post-pandemic era (8, 12) since older adults are particularly susceptible of leading inactive lifestyles (13).
Forms of health-enhancing physical activity (HEPA) (14) like structured physical exercise are essential factors in maintaining normal body function, healthy aging, and promoting a longer life span (15). Regular exercise can help reduce frailty, fall risk, and premature morbidity. It is also relevant in preventing and managing health conditions common in the older adult population, such as hypertension, diabetes, obesity, insomnia, depression, and anxiety. Multinational campaigns and guidelines recommend the most beneficial multimodal exercise programs consisting of aerobic, resistance training, flexibility, and balance components (16). However, despite the tremendous benefits of HEPA, such as physical exercise, studies show that older adults are not actively engaged in such heath activities. In addition to the lack of a structured and enticing program, scholars reported several socio-cognitive processes that impact exercise behavior, adoption, and maintenance (17). In support, scientists have long established the critical role of culture, society, and environment in the success of HEPA programs (18). This outcome reinforces the development of location and culture-specific country programs based on the cohort preferences and national policy to support older adults’ HEPA (13), which are currently few and still underdeveloped (19).
As healthcare institutes recommend HEPA initiatives as essential components of health promotion for older adults, tools, and technologies supporting active lifestyles are increasing in parallel. Population aging and technological diffusion are two intersecting transitions currently experienced by the world. More than ever, the increased aging of the population requires technology-driven nursing services (20) to complement the demand for quality health services, especially for older adults with declining health and physical and mental challenges (21, 22). For instance, the introduction of Fourth Industrial Revolution technologies for health promotion for older people represents an emerging and promising intervention (23). Furthermore, numerous HEPA activities geared towards balance and muscle strength can be performed at home or on-site using technology tools such as health trackers and gadgets (24). In addition, multiple online resources that feature virtual guides are emerging and available.
Emerging electronic health (eHealth) interventions have centered on behavioral change relating to physical activity. They have shown effectiveness in many instances (25). The latest innovations in technology-driven HEPA are the utilization of humanoid (human-resembling) technologies (HTs) like physical humanoid robot coaches (HRCs) (22, 26). Due to the advent of virtual worlds and mixed reality applications, virtual digital assistants as embodied conversational agents are also emerging (25). Digital “coaches” in exercise projected through mixed reality displays are particularly useful in situations where social contact might be limited, such as during the pandemic through remote coaching (27). In addition, companies are now investing in developing technologies whose main structure is the fusion of the virtual and physical world in a “metaverse” (28). Health experts have arrived at a consensus that the emergence of metaverse applications will provide a promising future in delivering healthcare in all “spaces” and “dimensions” (29). The emergence of virtual coaches and metaverse studies in nursing is still novice but growing with increasing acknowledgment of opportunities and challenges surrounding its implementation (30–32).
While mixed reality technology-driven health enhancing physical activities has been previously shown to reduce the risk of diseases (33, 34), studies focusing on its impact on physical and mental functioning among older adults are still limited and scarce (35, 36). Scholars also reported a substantial divide among users and non-users of technologies for physical health (37). Furthermore, technology-lead interventions have been previously reported to be potentially susceptible to disregard due to usability issues and task quality. As a result, current studies are recommended to focus on the development and evaluation of user-preferred technologies via mixed-method inquiry (25, 38) to understand better how older adults interact with the technology and leverage the technology to meet their needs (22).
Objectives
In response to the current gray spots and gaps found in a recently published literature review (31), this study envisions to advance the science of mixed reality technology-driven health interventions in the field of nursing by examining its impact through an exercise program directed toward community-dwelling older adults. Specifically, it aims to:
Quantitative aim 1: to assess older adults’ preferences for an ideal mixed-reality-driven virtual coach program based on several attributes and levels. The subjects are hypothesized to select age and ability-specific choices based on previous exposure to technology and life experiences.
Quantitative aim 2: to evaluate the impact of the mixed-reality-driven virtual coach program on participants’ health. The causal relationship between the outcome variables will be obtained from valid and reliable tools. Older adults with active participation in the program groups are hypothesized to elicit comparable physical and cognitive performances.
Quantitative aim 3: to model the older adults’ perception of the mixed-reality-driven virtual coach program usability and predictors of intention to participate in the program. The subjects are postulated to show indications of higher behavioral intention to participate in the program as affected by various variables.
Qualitative aim 1: to understand the older adult participants’ experiences during the mixed-reality-driven virtual coach program. A narrative descriptive qualitative approach will be carried out to evaluate the challenges or difficulties and successes or benefits of the program among those who benefitted the least and most from the intervention. The older adult key informants are expected to story-tell their practices focusing on themes related to acceptability, barriers, and facilitators.
Overall, tt was hypothesized that: (a) the older adult participants will identify their technology preferences based on their previous experiences and combination of various attributes, and (b) the use of mixed reality technology in physical exercise program will produce comparable health assessments when compared with the traditional form of health enhancing physical activities.
Human-computer interaction (HCI) is core to ensuring the usability of technologies and their successful integration to practice (39–42). Previous literature (43, 44) highlighted that HCI directly impacts technology users’ behavioral intention and actual utilization (44). Therefore, the adapted HCI model (45) offers a robust framework for the study. This model highlights a multitude of essential factors that needs to be considered in technology adoption such as content (user-preference), computer (technology features) and context (individual experiences and client uniqueness) that serves as antecedents of successful technology use in healthcare.
Methods
Design
An explanatory sequential mixed-method research design will be used to understand the impact of the mixed-reality-driven virtual coach program community-dwelling Filipino older adults and compare its effects against the current exercise program (live coaching and video-based) on the participants’ health. The current study advances four (4) research phases that will make use of distinct research approaches. Phases 1–3 shall adopt a post-positivist approach (46) through discreet choice experiment (conjoint analysis), quasi experiment, and structural equation modeling. Phase 4 follows a qualitative-constructivist paradigm (47) using descriptive qualitative research.
Phase 1: older adults’ preference for an ideal mixed-reality-driven virtual coach program
Discrete choice experiment
Understanding how older adults value the essential components of healthcare interventions through the conjoint method is crucial to both the design and evaluation of the program (48). Discrete choice experiment (DCE) or conjoint analysis involves measuring psychological judgment between choices and alternatives. It is also powerful in understanding and predicting the technology users’ attribute tradeoffs, decisions, and preferences of technology features (49). DCE was initially introduced in psychology and marketing but has gained popularity in medicine and healthcare (50). The adaptive conjoint analysis method is the most appropriate for the current study due to its practical and respondent-friendly features (51). This study will follow the published standards in applying the conjoint analysis methods in healthcare (52). In addition, it will include essential steps in the development of the adaptive conjoint survey, as follows: (a) defining HT-HEPA attributes and levels based on literature evidence, and (b) designing the attributes and levels as components of the HT-HEPA program, and (c) designing the conjoint survey questionnaire. The computer-based survey questionnaire using the Sawtooth software will be distributed to participants.
Phase 2: impact of mixed-reality-driven virtual coach program on participants’ physical, cognitive status, and QoL
Quasi experiment
Quasi experimental research will be employed to estimate the effect and examine the causal relationship between the HT-HEPA intervention and the study respondents’ physical, cognitive status, and QoL. Quasi experiments are appropriate for practical situations and ethical compliance for studies involving vulnerable participants such as older adults (53), and allow scholars to conduct rigorous studies under certain limitations and non-control conditions (54).
Phase 3: mixed-reality-driven virtual coach program’s system usability and predictors of intention to program participation
Structural equation modeling (SEM)
The popularity of structural equation modeling (SEM) as a research approach is attributed to its capacity to concurrently evaluate the validity of the measurement (55) while testing the relationship between latent variables (56). Specifically, the variance-based partial least squares (PLS-SEM) technique shall be used in the current study to maximize statistical power and deliver better convergence behavior (57, 58). UTAUT, usability, and behavioral intention variables will be processed to create a parsimonious model. An independent usability testing (59) with descriptive analysis will also be carried out.
Phase 4: participants’ experiences: program acceptability, barriers, and facilitators
Descriptive qualitative
Descriptive qualitative research is mainstream in studies exploring human phenomena in nursing and healthcare practice (60). In capturing the participants’ lived experiences with the technology, a descriptive qualitative tradition with thematic analysis (61) shall be applied. A descriptive approach, based on Husserlian principles (62), is proven powerful in clarifying poorly understood concepts of experiences (63), such as the potential acceptance, barriers, and facilitators of mixed reality health enhancing physical activity participation.
Study setting, subject, and eligibility criteria
The study will be conducted at two senior centers in urban settings in the Philippines. The senior centers are served by a university-based medical facility located in the northern (Valenzuela City) and southern part (Quezon City) of Luzon Island in the Philippines, where the highest densities of older adults are found.
The eligible participants will be purposively selected from the regular attendees at the study sites using the inclusion criteria: (1) ambulatory, (2) can follow simple instructions, (3) normal eyes functioning without low vision (or at most with corrective lenses), and (4) willingness to participate in the program with signed informed consent. Older adults ages 60–75 regardless of the gender and who are considered fit to participate by the community physician will be targeted. A total of 128 or 64 older adults in each center, will be recruited via posters at community senior centers who will undergo additional screening or health records review by a certified gerontologist to ensure safety and proper fit. Afterward, the treatments will be assigned to each of the two senior center sites for the quasi-experimental study. Only the participants from the experimental group shall be involved in the usability evaluations and qualitative arm. The sampling plan is shown in Figure 1.
Informed consent and client involvement
Clients will be signing the printed informed consent and will be involved in the design and conduct of the study. An orientation will be conducted to communicate the research objectives, outcome measures, recruitment methods, and other relevant information. Client experience and preferences will be identified and incorporated.
Interventions
This study will involve the development of mixed reality technology-driven virtual coach exercise program. The program shall be called “Hataw at Sigla para kay Lolo and Lola” (Groove and Move for older Adults), and will consist of the following procedures:
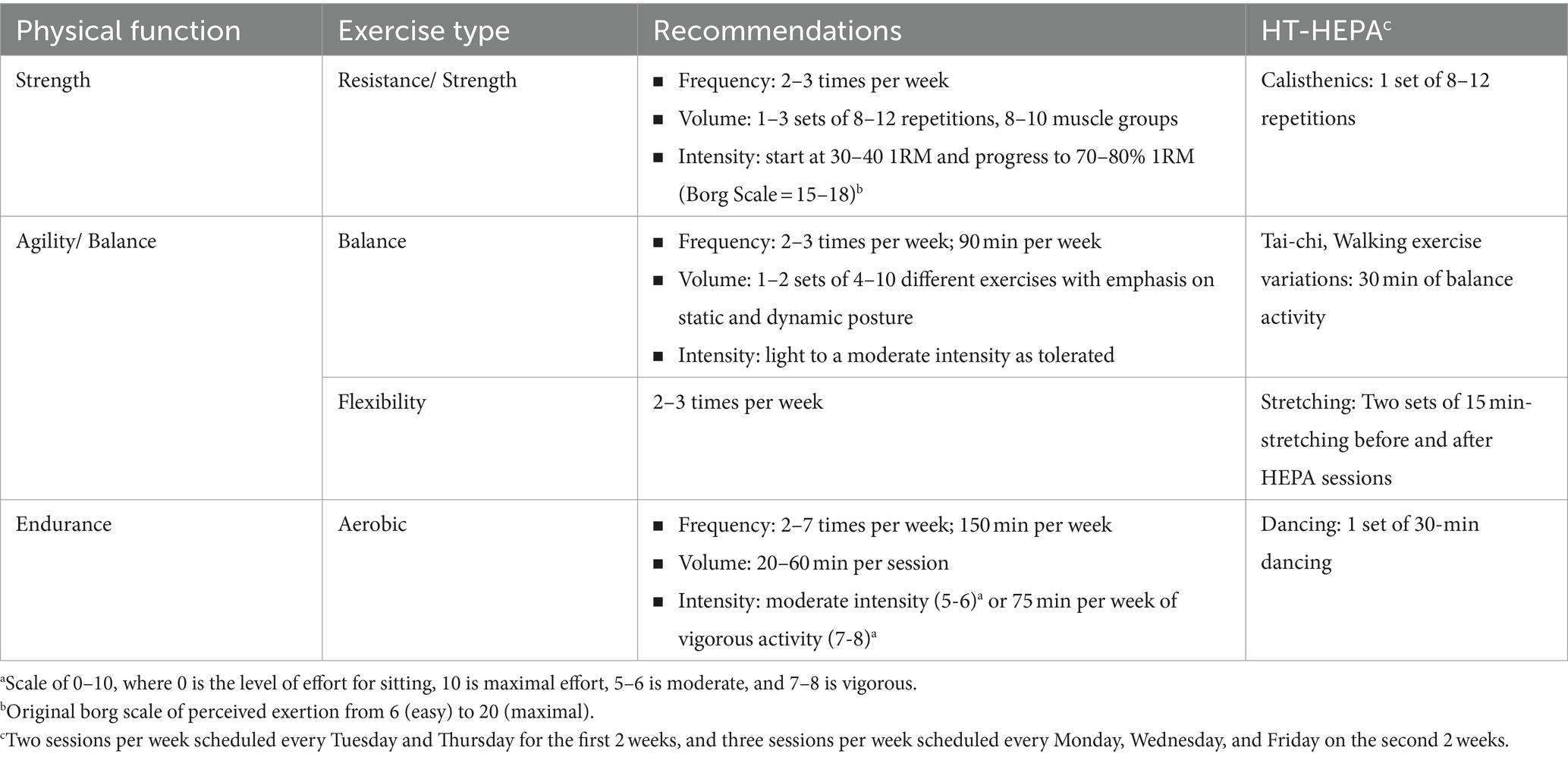
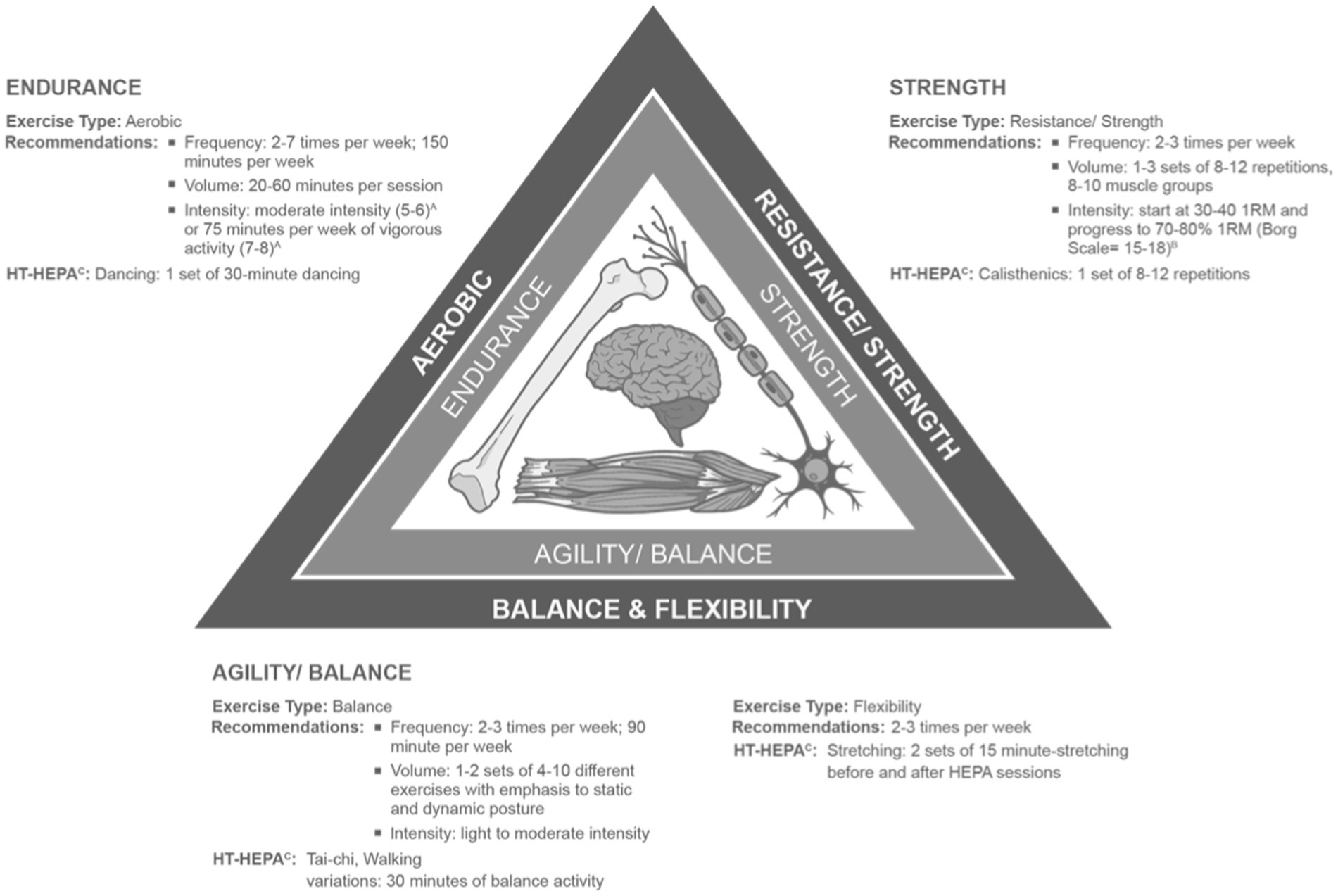
Identifying the standard exercise for Filipino older adults: the Philippines, similar to other territories, recommend a multimodal exercise as the most ideal program to support and improve the health of older adults (15, 64). This multimodal approach consists of aerobic, resistance, balance, and flexibility maneuvers (16). Developing the exercise program considers the uniqueness of the older adult cohorts with specific needs and requirements and compliance with recommended well-balanced exercise regimens (16). Results of systematic reviews (65, 66) and international expert consensus (64) shall serve as references for the age-appropriate program. The summary of the exercise components and recommendations are presented (Table 1; Figure 2). The ideal duration of the program is 1 h with 15 min of warming up and stretching before and after the session. This session length concurs with the current local recommendations (67, 68).
HT programming: this study will use a virtual humanoid “digital coach” to be projected using an optical see-through head-mounted-display (OST-HMD), Microsoft® Hololens (see Figure 3). The device has been the most dominant, popular, and fastest developing mixed reality display in healthcare research since its release in 2016 (52, 69) due to its commendable inbuilt processing units and more extensive network of developers in healthcare (70). The device has been used for health and education programs for older adults in previous studies. The Mixed Reality Toolkit version 2, Unity 2018.4.x, and Unreal Engine are the primary software to be used.
Improving client adherence and post-trial care
The participants (experimental and control) will receive an honorarium for their participation in the study. Other benefits include on-site snacks, free consultation from healthcare providers, and access to wellness facilities where the intervention will be conducted. In addition, participants who will be completing the whole program will receive wellness and exercise program paraphernalia.
Outcomes
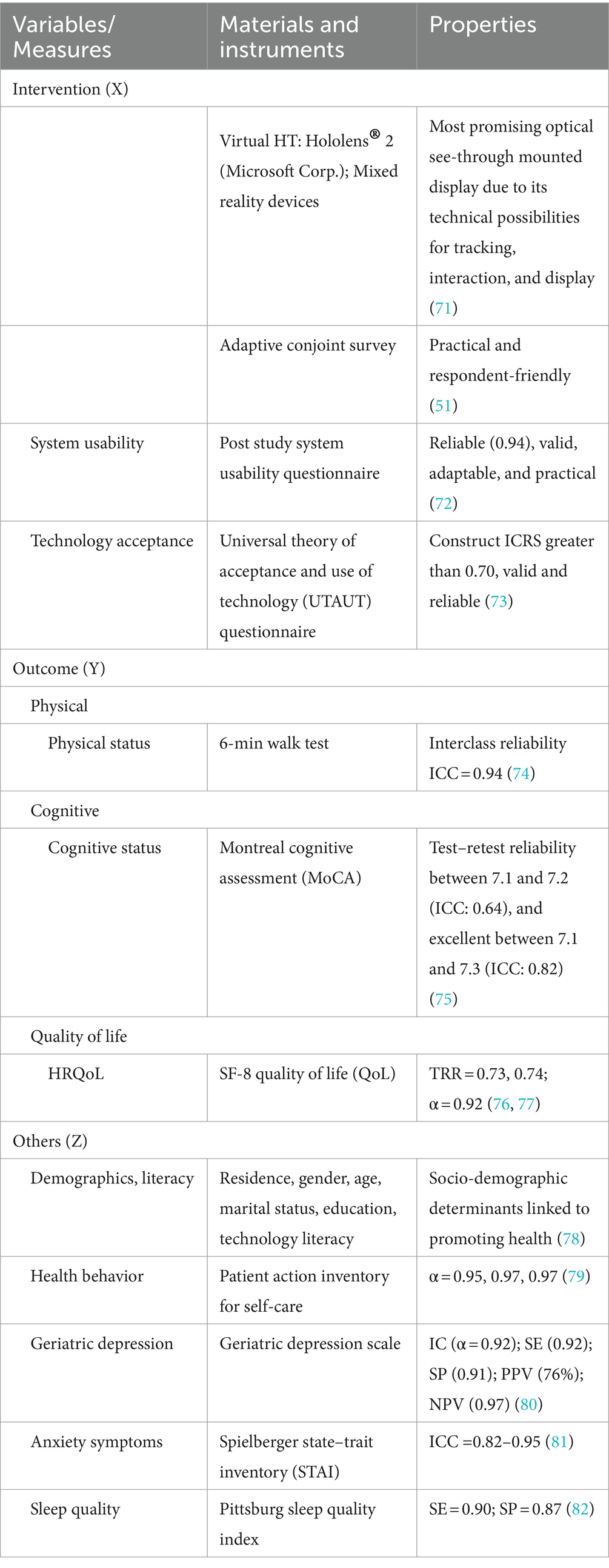
The predictor, outcome, and related variables will be assessed using appropriate, valid, and reliable measurement tools as shown in Table 2.
Data collection and timeline
This study is composed of three data collection steps:
Step 1: preparatory: this phase includes the necessary preparation to enrich the effectiveness and efficiency of data collection through (1) an initial visit to the senior center sites to establish a partnership with the administration, orientation, acquire permission, and establish rapport among the prospective subjects, (2) technical set-up and training, and (3) health screening and actual sampling.
Step 2: quantitative evaluation of preferences: this phase involves the initial assessment of the older adults’ preferences for the mixed reality technology-driven exercise program via conjoint analysis. Results will be generated to inform the mixed reality technology system programming for the system’s actual development and initial pilot. This will follow the baseline assessment of participant data, actual exposure to the intervention, and post-intervention assessment of the subjects. The intervention will run for a month consisting of the first 2 weeks of the twice-weekly (Tuesday and Thursday) schedule to be followed by the second 2 weeks of trice weekly (Monday, Wednesday, Friday) schedule. Each intervention session program will last approximately 1.5 h, including orientation, warm-up, and stretching. All participants will be supervised by the health team and trained personnel at the senior center and follow a standard protocol.
Step 3: qualitative evaluation: this phase focuses on the individual interviews to assess views and opinions of study participants. An aide-memoire will be constructed as an interview tool to capture the stories and experiences of the older adult participants. Specifically, a responsive interviewing approach (83) will be used. Individual interviews will be transcribed, coded, and thematized. Qualitative findings will be used to substantiate the quantitative outcomes of the study.
Sample size
To identify the acceptable sample size, the difference in repeated measures between two independent groups using MANOVA with a power set at 0.80 with medium to high effect size at 0.05 alpha level was computed using R software. The estimated sample size is 128 or 64 participants per senior center group.
Data collection, management and statistical methods
A robust research data management (84) and analysis plan will be implemented to maintain the privacy, confidentiality, integrity, validity, and reliability of the gathered data in all stages of the data lifecycle (84). Only members of the research group will be given access through a double authentication procedure. The institutions currently utilize the latest Sophos SG series UTM firewall system and the Sophos UTM 9 management system that provides comprehensive gateway protection, including network intrusion prevention management. Backup is done every 7 PM daily, and every server is connected to an uninterruptible power supply. In terms of data analysis, the following approaches shall be used:
Assessment older adults’ preferences for an ideal mixed reality technology-driven health enhancing physical activity program
Descriptive statistics will be used to describe the respondent demographics. In the conjoint method, regression analysis is adopted to relate the probability of choosing several profiles simultaneously. The regression model assumes that “the probability of choosing one profile is a linear function of the attribute levels in the profile” (85). Sawtooth Software Lighthouse Studio version 9.11 statistical package will be employed to calculate individual preference coefficients (utilities) in each attribute level and attribute importance scores (79, 80). In addition, the primary and joint effects of the preference attributes, average importance, and utility values will also be generated (86). In interpreting and reporting the conjoint outcomes, the ESTIMATE checklist (85) developed by the ISPOR Conjoint Analysis Good Research Practices Task Force shall be used.
Comparing the effects of the mixed reality technology-driven health enhancing physical activities with the usual health enhancing physical activities (live coach and video-based) on participants’ physical, cognitive status, and quality of life measures
Repeated measures analysis of variance (RM-ANOVA)
Repeated Measures Analysis of Variance (RM-ANOVA) will be used to investigate the effects of the type of intervention on health variables across three assessment points using SPSS version 22. Mauchly’s Test will be utilized to verify the sphericity assumption with degrees of freedom correction using the Greenhouse–Geisser method. Effect sizes will also be reported.
Assessing the older adults’ perception of mixed reality technology-driven health enhancing physical activity system’s usability and predictors of intention to participate in the program
Structural equation modeling
Structural Equation Modeling (SEM) through Partial Least Squares (PLS) will be employed to model the older adults’ perception of HT-HEPA’s system usability and predictors of intention to participate in the program. PLS-SEM is the most appropriate considering the number of older adult participants because of its power to precisely examine and estimate relationships among a set of variables (87, 88). This study will adopt the published guidelines for analyzing, interpreting, and reporting SEM outcomes (89) using the PLS Graph software package (90). For PLS-SEM, the measurement model’s evaluation is based on the reliability, construct, and discriminant validity of the measures associated with individual variables (89). Construct reliability assessment via composite reliability and Cronbach’s alpha (91) will measure the extent to which a set of items is consistent in what it intends to measure (90, 92). Convergent validity, on the other hand, is a measure of measurement instrument quality that can be assessed using two approaches: (a) evaluating the statistical significance (p < 0.05) of the item loadings associated with the construct and should be equal to or greater than 0.50 (90, 91) and (b) the use of average variance extracted (AVE) that quantifies the amount of variance that a construct captures from its items relative to the amount due to measurement error (93), greater than.50 (91, 94). The average variance extracted (AVE) can also be used to test if an instrument has discriminant validity, as evidenced by the AVE of each construct greater than its correlations with the other constructs (95).
Understanding the older adult participants’ experiences during the mixed reality technology-driven health enhancing physical activities program
Thematic analysis
Interview texts will be transcribed, coded, and analyzed using MAXQDA® Analytics Pro (VERBI Software, Germany). Member checking procedure (96) and reflective logs (97) will be adopted to ensure trustworthiness and reflexivity, respectively within the research team. Reflective notes or memos will be created to accumulate ideas, concepts, and connections with the generated quantitative data. Themes and/or subthemes shall be developed and reported using the COREQ guidelines (98). A code book will be created and maintained.
Dissemination plans
The outcomes and changes in the study will be shared with the clients and stakeholders through post-study result dissemination and newsletter at the senior centers.
Discussion
This protocol paper outlines the objectives, rationale, methods, and design for a multiple phase study that will examine the impact of a mixed reality-driven intervention through an exercise program directed toward community-dwelling older adults.
There has been increased research on older adult representations and studies focusing on technology interventions in the past decades (99). Although this upward trend is considered favorable in general, concerns related to ethical issues and the welfare of older adults participants are on the rise (100, 101), more so in aging studies involving technology interventions (42, 102). Older adults are essential to study subjects and clients in healthcare but are considered a vulnerable cohort in research studies.
As with other studies involving technologies, potential risks include loss of autonomy, privacy, data protection, safety, isolation prevention, and user overstressing. To minimize the risks, proper orientation will be held. The research team will undergo training and acquire good clinical practice certificate. Procedures will align with the currently accepted standards by the Philippine Department of Health, the research team will recruit social workers and healthcare providers to monitor the interventions and for potential health and wellness issues during the study. Reporting untoward events will comply with the current protocol and standards of the Philippine Health Research Ethics Board. Also, measurement error can be a potential challenge to the study and will be addressed by frequent recalibration and testing of instruments. Internet service interruptions needed to load exercise modules from the system storage might be an issue. This will be addressed by downloading the programs to the local server at the senior center sites.
This study protocol will provide an outstanding reference for future researchers for potential replication in other settings, timeline, and territories. It may also offer an outline of the necessary steps to ensure a robust but practical approach in technology studies in healthcare. The protocol supports the value of interdisciplinary and cross-disciplinary efforts and partnership in advancing the knowledge in the field of technology, health, and informatics. Outputs informing policies and standards are expected to be generated in this protocol for practice and research methods improvement.
Ethics statement
The studies involving humans were approved by Johns Hopkins Medicine Institutional Research Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MD: Writing – original draft, Writing – review & editing. KD: Writing – original draft, Writing – review & editing. PA: Writing – original draft, Writing – review & editing. CB: Writing – original draft, Writing – review & editing. C-MH: Writing – original draft, Writing – review & editing. WP: Writing – original draft, Writing – review & editing. CH: Writing – original draft, Writing – review & editing. PD: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study is being supported by the Sigma Theta Tau International Honor Society’s Sigma Foundation for Nursing and the National League of Nursing via the Edmund J. Pajarillo Informatics and Innovation Scholarship. Special thanks are given to the Department of Science and Technology – Philippine Council for Industry, Energy, and Emerging Technology (DOST-PCIEERD), the Our Lady of Fatima University, and its Research Development and Innovation Center for providing the grant and support in the development of the Multiple Applications for Reality Virtuality Experience Laboratory (MARVEL) which will be used in the creation of the different versions and platforms for the virtual coach. Sawtooth Software provides the license to use the conjoint analysis tool under its Academic Grant program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cunningham, C, O' Sullivan, R, Caserotti, P, and Tully, MA. Consequences of physical inactivity in older adults: a systematic review of reviews and meta-analyses. Scand J Med Sci Sports. (2020) 30:816–27. doi: 10.1111/sms.13616
2. Guthold, R, Stevens, GA, Riley, LM, and Bull, FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/S2214-109X(18)30357-7
3. Ding, D, Kolbe-Alexander, T, Nguyen, B, Katzmarzyk, PT, Pratt, M, and Lawson, KD. The economic burden of physical inactivity: a systematic review and critical appraisal. Br J Sports Med. (2017) 51:1392–409. doi: 10.1136/bjsports-2016-097385
4. Lee, I-M, Shiroma, EJ, Lobelo, F, Puska, P, Blair, SN, and Katzmarzyk, PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. (2012) 380:219–29. doi: 10.1016/S0140-6736(12)61031-9
5. Keadle, SK, McKinnon, R, Graubard, BI, and Troiano, RP. Prevalence and trends in physical activity among older adults in the United States: a comparison across three national surveys. Prev Med. (2016) 89:37–43. doi: 10.1016/j.ypmed.2016.05.009
6. Lippi, G, Henry, BM, and Sanchis-Gomar, F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur J Prev Cardiolog. (2020) 27:906–8. doi: 10.1177/2047487320916823
7. Roschel, H, Artioli, GG, and Gualano, B. Risk of increased physical inactivity during COVID-19 outbreak in older people: a call for actions. J Am Geriatr Soc. (2020) 68:1126–8. doi: 10.1111/jgs.16550
8. Machado, CLF, Pinto, RS, Brusco, CM, Cadore, EL, and Radaelli, R. COVID-19 pandemic is an urgent time for older people to practice resistance exercise at home. Exp Gerontol. (2020) 141:111101. doi: 10.1016/j.exger.2020.111101
9. Rappler Philippines (2021). Survey says 67% of Filipinos move less. Here’s why you should be concerned. Manila, Philippines. Available at: https://www.rappler.com/brandrap/health-beauty-and-wellness/less-exercise-filipinos-covid-19-pandemic-anlene-survey/ (Accessed June 10, 2022).
10. Kirwan, R, McCullough, D, Butler, T, Perez de Heredia, F, Davies, IG, and Stewart, C. Sarcopenia during COVID-19 lockdown restrictions: long-term health effects of short-term muscle loss. Gero Sci. (2020) 42:1547–78. doi: 10.1007/s11357-020-00272-3
11. Sallis, R, Young, DR, Tartof, SY, Sallis, JF, Sall, J, Li, Q, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. (2021) 55:1099–105. doi: 10.1136/bjsports-2021-104080
12. Markotegi, M, Irazusta, J, Sanz, B, and Rodriguez-Larrad, A. Effect of the COVID-19 pandemic on the physical and psychoaffective health of older adults in a physical exercise program. Exp Gerontol. (2021) 155:111580. doi: 10.1016/j.exger.2021.111580
13. Cunningham, C, and O’ Sullivan, R. Why physical activity matters for older adults in a time of pandemic. Eur Rev Aging Phys Act. (2020) 17:16. doi: 10.1186/s11556-020-00249-3
14. Whiting, S, Mendes, R, Morais, ST, Gelius, P, Abu-Omar, K, Nash, L, et al. Promoting health-enhancing physical activity in Europe: surveillance, policy development and implementation 2015–2018. Health Policy. (2021) 125:1023–30. doi: 10.1016/j.healthpol.2021.05.011
15. Eckstrom, E, Neukam, S, Kalin, L, and Wright, J. Physical activity and healthy aging. Clin Geriatr Med. (2020) 36:671–83. doi: 10.1016/j.cger.2020.06.009
16. Mora, JC, and Valencia, WM. Exercise and older adults. Clin Geriatr Med. (2018) 34:145–62. doi: 10.1016/j.cger.2017.08.007
17. Arovah, NI, and Heesch, KC. Social cognitive measures related to exercise behaviour: validation in Indonesian middle-aged and older adults. Clin Epidemiol Glob Health. (2022) 14:100975. doi: 10.1016/j.cegh.2022.100975
18. Watson, KB, Carlson, SA, Gunn, JP, Galuska, DA, O’Connor, A, Greenlund, KJ, et al. Physical inactivity among adults aged 50 years and older — United States, 2014. MMWR Morb Mortal Wkly Rep. (2016) 65:954–8. doi: 10.15585/mmwr.mm6536a3
19. Van Hoye, A, Vandoorne, C, Absil, G, Lecomte, F, Fallon, C, Lombrail, P, et al. Health enhancing physical activity in all policies? Comparison of national public actors between France and Belgium. Health Policy. (2019) 123:327–32. doi: 10.1016/j.healthpol.2019.01.008
20. Abdi, J, Al-Hindawi, A, Ng, T, and Vizcaychipi, MP. Scoping review on the use of socially assistive robot technology in elderly care. BMJ Open. (2018) 8:e018815. doi: 10.1136/bmjopen-2017-018815
21. Diño, MJS, and Ong, IL. Research, technology, education & scholarship in the fourth industrial revolution [4IR]: influences in nursing and the health sciences. J Med Investig. (2019) 66:3–7. doi: 10.2152/jmi.66.3
22. Sato, M, Yasuhara, Y, Osaka, K, Ito, H, Dino, MJS, Ong, IL, et al. Rehabilitation care with pepper humanoid robot: a qualitative case study of older patients with schizophrenia and/or dementia in Japan. Enferm Clin. (2020) 30:32–6. doi: 10.1016/j.enfcli.2019.09.021
23. Castro e Melo, JAGM, and Faria Araújo, NM. Impact of the fourth industrial revolution on the health sector: a qualitative study. Healthc Inform Res. (2020) 26:328–34. doi: 10.4258/hir.2020.26.4.328
24. Evangelista de Lima, B, Passos, GS, Youngstedt, SD, Bandeira Santos Júnior, LC, and Gonçalves, SM. Effects of Xbox Kinect exercise training on sleep quality, anxiety and functional capacity in older adults. J Bodyw Mov Ther. (2021) 28:271–5. doi: 10.1016/j.jbmt.2021.07.029
25. Hurmuz, MZM, Jansen-Kosterink, SM, Beinema, T, Fischer, K, op den Akker, H, and Hermens, HJ. Evaluation of a virtual coaching system eHealth intervention: a mixed methods observational cohort study in the Netherlands. Internet Interv. (2022) 27:100501. doi: 10.1016/j.invent.2022.100501
26. Tanioka, R, Yasuhara, Y, Osaka, K, Kai, Y, Zhao, Y, Tanioka, T, et al. Autonomic nervous activity of patient with schizophrenia during pepper CPGE-led upper limb range of motion exercises. Enfermeria Clinica. (2020) 30:48–53. doi: 10.1016/j.enfcli.2019.09.023
27. Loveys, K, Sagar, M, Pickering, I, and Broadbent, E. A digital human for delivering a remote loneliness and stress intervention to at-risk younger and older adults during the COVID-19 pandemic: randomized pilot trial. JMIR Ment Health. (2021) 8:e31586. doi: 10.2196/31586
28. Riva, G, and Wiederhold, BK. What the Metaverse is (really) and why we need to know about it. Cyberpsychol Behav Soc Netw. (2022) 25:355–9. doi: 10.1089/cyber.2022.0124
29. Yang, D, Zhou, J, Chen, R, Song, Y, Song, Z, Zhang, X, et al. Expert consensus on the metaverse in medicine. Clinical eHealth. (2022) 5:1–9. doi: 10.1016/j.ceh.2022.02.001
30. Betriana, F, Tanioka, R, Gunawan, J, and Locsin, RC. Healthcare robots and human generations: consequences for nursing and healthcare. Collegian. (2022) 29:767–73. doi: 10.1016/j.colegn.2022.01.008
31. Dino, MJS, Davidson, PM, Dion, KW, Szanton, SL, and Ong, IL. Nursing and human-computer interaction in healthcare robots for older people: an integrative review. Int J Adv Nurs Stud. (2022) 4:100072. doi: 10.1016/j.ijnsa.2022.100072
32. Zhao, J, Lu, Y, Zhou, F, Mao, R, and Fei, F. Systematic bibliometric analysis of research hotspots and trends on the application of virtual reality in nursing. Front Public Health. (2022) 10:906715. doi: 10.3389/fpubh.2022.906715
33. Leng, M, Liu, P, Zhang, P, Hu, M, Zhou, H, Li, G, et al. Pet robot intervention for people with dementia: a systematic review and meta-analysis of randomized controlled trials. Psychiatry Res. (2019) 271:516–25. doi: 10.1016/j.psychres.2018.12.032
34. Park, S, Bak, A, Kim, S, Nam, Y, Kim, HS, Yoo, D-H, et al. Animal-assisted and pet-robot interventions for ameliorating behavioral and psychological symptoms of dementia: a systematic review and Meta-analysis. Biomedicines. (2020) 8:150. doi: 10.3390/biomedicines8060150
35. Clawson, J, Pater, JA, Miller, AD, Mynatt, ED, and Mamykina, L No longer wearing: investigating the abandonment of personal health-tracking technologies on craigslist. Proceedings of the 2015 ACM international joint conference on pervasive and ubiquitous computing-Ubi Comp’15.
36. Lazar, A, Koehler, C, Tanenbaum, J, and Nguyen, DH (2015). Why we use and abandon smart devices. Proceedings of the 2015 ACM international joint conference on pervasive and ubiquitous computing - UbiComp’15.
37. Neven, L. ‘But obviously not for me’: robots, laboratories and the defiant identity of elder test users. Sociol Health Illn. (2010) 32:335–47. doi: 10.1111/j.1467-9566.2009.01218.x
38. Fattal, C, Cossin, I, Pain, F, Haize, E, Marissael, C, Schmutz, S, et al. Perspectives on usability and accessibility of an autonomous humanoid robot living with elderly people. Disabil Rehabil Assist Technol. (2020) 17:418–30. doi: 10.1080/17483107.2020.1786732
39. Gulliksen, J. Institutionalizing human-computer interaction for global health. Glob Health Action. (2017) 10:1344003. doi: 10.1080/16549716.2017.1344003
40. Siek, K. Expanding human computer interaction methods to understand user needs in the design process of personal health systems. Yearb Med Inform. (2018) 27:074–8. doi: 10.1055/s-0038-1667073
41. Søgaard Neilsen, A, and Wilson, RL. Combining e-mental health intervention development with human computer interaction (HCI) design to enhance technology-facilitated recovery for people with depression and/or anxiety conditions: an integrative literature review. Int J Mental Health Nurs. (2019) 28:22–39. doi: 10.1111/inm.12527
42. de Guzman, AB, and Diño, MJS. Examining the role of Filipino elderly attitudes toward computer and internet on their behavioral intention for telehealth participation. Educ Gerontol. (2020) 46:140–9. doi: 10.1080/03601277.2020.1715589
43. Brandsma, T, Stoffers, J, and Schrijver, I. Advanced technology use by care professionals. IJERPH. (2020) 17:742. doi: 10.3390/ijerph17030742
44. Singleton, JL, Remillard, ET, Mitzner, TL, and Rogers, WA. Everyday technology use among older deaf adults. Disabil Rehabil Assist Technol. (2019) 14:325–32. doi: 10.1080/17483107.2018.1447609
45. Bálint, L. Adaptive human-computer interfaces for man-machine interaction in computer-integrated systems. Comput Integr Manuf Syst. (1995) 8:133–42. doi: 10.1016/0951-5240(95)00007-G
46. Park, YS, Konge, L, and Artino, AR. The positivism paradigm of research. Acad Med. (2020) 95:690–4. doi: 10.1097/ACM.0000000000003093
47. Tenny, S, Brannan, GD, Brannan, JM, and Sharts-Hopko, NC (2022). Qualitative study Stat pearls. Treasure Island: Stat Pearls Publishing http://www.ncbi.nlm.nih.gov/books/NBK470395/ (Accessed June 17, 2022).
48. Bridges, JFP, Hauber, AB, Marshall, D, Lloyd, A, Prosser, LA, Regier, DA, et al. Conjoint analysis applications in health—a checklist: A report of the ISPOR good research practices for conjoint analysis task force. Value Health. (2011) 14:403–13. doi: 10.1016/j.jval.2010.11.013
49. Bagozzi, RP ed. Advanced methods of marketing research. Cambridge, Mass: Blackwell Business (1994).
50. Szeinbach, S, Beyer, A, Qureshi, Z, Uhas, A, Visaria, J, and Seoane-Vazquez, E. Use of conjoint analysis in health outcome research: an examination of the literature. Value Health. (2009) 12:A34. doi: 10.1016/S1098-3015(10)73231-9
51. Herrmann, A, Schmidt-Gallas, D, and Huber, F. Adaptive conjoint analysis: understanding the methodology and assessing reliability and validity In: A Gustafsson, A Herrmann, and F Huber, editors. Conjoint Measurement. Berlin, Heidelberg: Springer Berlin Heidelberg (2003)
52. Birlo, M, Edwards, PJE, Clarkson, M, and Stoyanov, D. Utility of optical see-through head mounted displays in augmented reality-assisted surgery: a systematic review. Med Image Anal. (2022) 77:102361. doi: 10.1016/j.media.2022.102361
53. Behi, R, and Nolan, M. Quasi-experimental research designs. Br J Nurs. (1996) 5:1079–81. doi: 10.12968/bjon.1996.5.17.1079
54. Miller, CJ, Smith, SN, and Pugatch, M. Experimental and quasi-experimental designs in implementation research. Psychiatry Res. (2020) 283:112452. doi: 10.1016/j.psychres.2019.06.027
56. Babin, BJ, Hair, JF, and Boles, JS. Publishing research in marketing journals using structural equation modeling. J Mark Theory Pract. (2008) 16:279–86. doi: 10.2753/MTP1069-6679160401
57. Hair, JF, Sarstedt, M, Hopkins, L, and Kuppelwieser, VG. Partial least squares structural equation modeling (PLS-SEM): an emerging tool in business research. Eur Bus Rev. (2014) 26:106–21. doi: 10.1108/EBR-10-2013-0128
58. Sarstedt, M, Ringle, CM, Smith, D, Reams, R, and Hair, JF. Partial least squares structural equation modeling (PLS-SEM): a useful tool for family business researchers. J Fam Bus Strat. (2014) 5:105–15. doi: 10.1016/j.jfbs.2014.01.002
59. Maramba, I, Chatterjee, A, and Newman, C. Methods of usability testing in the development of eHealth applications: a scoping review. Int J Med Inform. (2019) 126:95–104. doi: 10.1016/j.ijmedinf.2019.03.018
60. Matua, GA. Choosing phenomenology as a guiding philosophy for nursing research. Nurse Res. (2015) 22:30–4. doi: 10.7748/nr.22.4.30.e1325
61. Sundler, AJ, Lindberg, E, Nilsson, C, and Palmér, L. Qualitative thematic analysis based on descriptive phenomenology. Nurs Open. (2019) 6:733–9. doi: 10.1002/nop2.275
62. Paley, J. Husserl, phenomenology and nursing. J Adv Nurs. (1997) 26:187–93. doi: 10.1046/j.1365-2648.1997.1997026187.x
63. Matua, GA, and Van Der Wal, DM. Differentiating between descriptive and interpretive phenomenological research approaches. Nurse Res. (2015) 22:22–7. doi: 10.7748/nr.22.6.22.e1344
64. Izquierdo, M, Merchant, RA, Morley, JE, Anker, SD, Aprahamian, I, Arai, H, et al. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging. (2021) 25:824–53. doi: 10.1007/s12603-021-1665-8
65. Fragala, MS, Cadore, EL, Dorgo, S, Izquierdo, M, Kraemer, WJ, Peterson, MD, et al. Resistance training for older adults: position statement from the National Strength and conditioning association. J Strength Cond Res. (2019) 33:2019–52. doi: 10.1519/JSC.0000000000003230
66. Sherrington, C, Tiedemann, A, Fairhall, N, Close, JCT, and Lord, SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull. (2011) 22:78–83. doi: 10.1071/NB10056
67. Civil Service Commission (2011). Memorandum circular 8 series of 2011: Reiteration of the physical Fitness program “great Filipino workout. Available at: http://www.csc.gov.ph/phocadownload/userupload/itduser/mc08s2011.pdf (Accessed June 15, 2022).
68. Department of Health (2020). Philippine sports commission launches health Fitness campaign for FIlipinos amidst the pandemic. Available at: https://doh.gov.ph/press-release/PSC-LAUNCHES-HOME-FITNESS-CAMPAIGN-FOR-FILIPINOS-AMID-PANDEMIC (Accessed June 15, 2022).
69. Kostov, G, and Wolfartsberger, J. Designing a framework for collaborative mixed reality training. Procedia Comput Sci. (2022) 200:896–903. doi: 10.1016/j.procs.2022.01.287
70. Bekele, MK. Walkable mixed reality map as interaction interface for virtual heritage. Digit Appl Archaeol Cult Herit. (2019) 15:e00127. doi: 10.1016/j.daach.2019.e00127
71. Vorraber, W, Gasser, J, Webb, H, Neubacher, D, and Url, P. Assessing augmented reality in production: remote-assisted maintenance with Holo Lens. Procedia CIRP. (2020) 88:139–44. doi: 10.1016/j.procir.2020.05.025
72. Lewis, JR. Psychometric evaluation of the post-study system usability questionnaire: the PSSUQ. Proc Hum Factors Ergon Soc Annu Meet. (1992) 36:1259–60. doi: 10.1177/154193129203601617
73. Venkatesh, M, and Davis, D. User acceptance of information technology: toward a unified view. MIS Q. (2003) 27:425. doi: 10.2307/30036540
74. Rikli, RE, and Jones, CJ. Development and validation of a functional Fitness test for community-residing older adults. J Aging Phys Act. (1999) 7:129–61. doi: 10.1123/japa.7.2.129
75. Bruijnen, CJWH, Dijkstra, BAG, Walvoort, SJW, Budy, MJJ, Beurmanjer, H, De Jong, CAJ, et al. Psychometric properties of the Montreal cognitive assessment (MoCA) in healthy participants aged 18–70. Int J Psychiatry Clin Pract. (2020) 24:293–300. doi: 10.1080/13651501.2020.1746348
76. Eum, K-D, Li, J, Lee, H-E, Kim, S-S, Paek, D, Siegrist, J, et al. Psychometric properties of the Korean version of the effort–reward imbalance questionnaire: a study in a petrochemical company. Int Arch Occup Environ Health. (2007) 80:653–61. doi: 10.1007/s00420-007-0174-3
77. Ware, JEJ, Kosinski, M, Dewey, JE, Gandek, B, Kisinski, M, Ware, JE, et al. How to score and interpret single-item health status measures: A manual for users of the SF-8™ health survey. Boston: ScienceOpen, Inc. (2001).
78. Tzeng, H-M, Okpalauwaekwe, U, and Li, C-Y. Older adults’ socio-demographic determinants of health related to promoting health and getting preventive health Care in Southern United States: a secondary analysis of a survey project dataset. Nurs Rep. (2021) 11:120–32. doi: 10.3390/nursrep11010012
79. Tzeng, H-M, and Pierson, JM. What are the highly important and desirable patient engagement actions for self-care as perceived by individuals living in the southern United States? Patient Prefer Adherence. (2017) 11:181–91. doi: 10.2147/PPA.S127519
80. Kondo, S, Sato, K, Hozumi, Y, and Aso, K. Culture of uninvolved and involved psoriatic and normal epidermis with 3T3 feeder layers: morphological and biochemical comparison. J Dermatol. (1983) 10:585–91. doi: 10.1111/j.1346-8138.1983.tb01184.x
81. Zsido, AN, Teleki, SA, Csokasi, K, Rozsa, S, and Bandi, SA. Development of the short version of the spielberger state—trait anxiety inventory. Psychiatry Res. (2020) 291:113223. doi: 10.1016/j.psychres.2020.113223
82. Buysse, DJ, Reynolds, CF, Monk, TH, Berman, SR, and Kupfer, DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
83. Rubin, HJ, and Rubin, I. Qualitative interviewing: The art of hearing data. 3rd ed. Thousand Oaks, Calif: SAGE (2012).
84. Surkis, A, and Read, K. Research data management. J Med Libr Assoc. (2015) 103:154–6. doi: 10.3163/1536-5050.103.3.011
85. Hauber, AB, González, JM, Groothuis-Oudshoorn, CGM, Prior, T, Marshall, DA, Cunningham, C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR conjoint analysis good research practices task force. Value Health. (2016) 19:300–15. doi: 10.1016/j.jval.2016.04.004
86. Tasdemir Yigitoglu, G, Yilmaz, A, and Yilmaz, H. The effect of Covid-19 on sleep quality, anxiety and depression on healthcare staff at a tertiary hospital in Turkey. Arch Psychiatr Nurs. (2021) 35:504–10. doi: 10.1016/j.apnu.2021.07.001
87. Diño, MJS, and de Guzman, AB. Using partial least squares (PLS) in predicting behavioral intention for telehealth use among Filipino elderly. Educ Gerontol. (2015) 41:53–68. doi: 10.1080/03601277.2014.917236
88. Teo, T. Students and teachers’ intention to use technology: assessing their measurement equivalence and structural invariance. J Educ Comput Res. (2019) 57:201–25. doi: 10.1177/0735633117749430
89. Hulland, J. Use of partial least squares (PLS) in strategic management research: a review of four recent studies. Strat Mgmt J. (1999) 20:195–204. doi: 10.1002/(SICI)1097-0266(199902)20:2<195::AID-SMJ13>3.0.CO;2-7
90. Hair, JF, Hult, GTM, Ringle, CM, Sarstedt, M, Danks, NP, and Ray, S. Partial least squares structural equation modeling (PLS-SEM) using R: a workbook. Cham: Springer International Publishing (2021).
91. Kock, N. Common method Bias in PLS-SEM: a full collinearity assessment approach. Int J e-Collab. (2015) 11:1–10. doi: 10.4018/ijec.2015100101
92. Straub, D, and Gefen, D. Validation guidelines for IS positivist research. CAIS. (2004) 13, 380–427. doi: 10.17705/1CAIS.01324
93. Chin, W. The partial least squares approach for structural equation modeling In: GA Marcoulides, editor. Modern methods for business research. Mahwah: Lawrence Erlbaum Associates Publishers (1998)
94. Hair, JF, Sarstedt, M, Ringle, CM, and Mena, JA. An assessment of the use of partial least squares structural equation modeling in marketing research. J Acad Mark Sci. (2012) 40:414–33. doi: 10.1007/s11747-011-0261-6
95. Fornell, C, and Larcker, DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. (1981) 18:39. doi: 10.2307/3151312
96. Birt, L, Scott, S, Cavers, D, Campbell, C, and Walter, F. Member checking: a tool to enhance trustworthiness or merely a nod to validation? Qual Health Res. (2016) 26:1802–11. doi: 10.1177/1049732316654870
97. Berger, R. Now I see it, now I don’t: researcher’s position and reflexivity in qualitative research. Qual Res. (2015) 15:219–34. doi: 10.1177/1468794112468475
98. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
99. Coto, M, Lizano, F, Mora, S, and Fuentes, J. Social media and elderly people: research trends In: G Meiselwitz, editor. Social computing and social media. Applications and analytics. Cham: Springer International Publishing (2017)
100. Blažun Vošner, H, Železnik, D, Kokol, P, Vošner, J, and Završnik, J. Trends in nursing ethics research: mapping the literature production. Nurs Ethics. (O) 24:892–907. doi: 10.1177/0969733016654314
101. Suhonen, R, Stolt, M, Launis, V, and Leino-Kilpi, H. Research on ethics in nursing care for older people: a literature review. Nurs Ethics. (2010) 17:337–52. doi: 10.1177/0969733010361445
Keywords: humanoid technologies, health-enhancing physical activity, healthy lifestyle, older adults, Fourth Industrial Revolution, mixed method research
Citation: Dino MJS, Dion KW, Abadir PM, Budhathoki C, Huang C-M, Padula WV, Himmelfarb CRD and Davidson PM (2024) The impact of a mixed reality technology-driven health enhancing physical activity program among community-dwelling older adults: a study protocol. Front. Public Health. 12:1383407. doi: 10.3389/fpubh.2024.1383407
Edited by:
Vitor Parola, Coimbra Nursing School, PortugalReviewed by:
Rui Paulo, Polytechnic Institute of Castelo Branco, PortugalAngel Saez-Berlanga, University of Valencia, Spain
Copyright © 2024 Dino, Dion, Abadir, Budhathoki, Huang, Padula, Himmelfarb and Davidson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael Joseph S. Dino, bWRpbm8xQGpodS5lZHU=
 Michael Joseph S. Dino
Michael Joseph S. Dino Kenneth W. Dion
Kenneth W. Dion Peter M. Abadir
Peter M. Abadir Chakra Budhathoki1,3
Chakra Budhathoki1,3 Chien-Ming Huang
Chien-Ming Huang