- 1School of Health Management, Guangzhou Medical University, Guangzhou, China
- 2School of Public Health, Southern Medical University, Guangzhou, China
- 3School of Public Health, Peking University, Beijing, China
- 4Center for WHO Studies and Department of Health Management, School of Health Management of Southern Medical University, Guangzhou, China
Introduction: This study aimed to explore the influence of Intimate Partner Violence (IPV) on depression, the mediating role of social support, and the moderating role of the Big Five personality traits in the relationship between social support and depression.
Methods: Participants were recruited from Mainland China, using a stratified random sampling and quota sampling method. From June to August 2022, a diverse group of 21,916 participants (ranging from 12 to 100 years old) completed the Intimate Partner Violence Scale, Patient Health Questionnaire, Perceived Social Support Scale, and Big Five Inventory-Short Version.
Results: IPV was significantly positively correlated with depression and significantly negatively correlated with perceived social support. Perceived social support plays a mediating role in the link between IPV and depression.
Discussion: Healthcare workers should assess social support and provide adequate care or recommendations for increasing social support when patients with IPV report depressive symptoms. Patients can be coached by professionals to improve their resiliency by developing or nurturing more optimistic personality traits.
1 Introduction
Intimate partner violence (IPV) is a serious, prevalent, and preventable public health problem that disproportionately affects women worldwide. Intimate partner violence describes physical or sexual assault, or psychological harm, of a spouse or sexual intimate (1). Its prevalence varies by social, economic, and cultural background, although it exists in all demographic groups (2). Globally, 35% of women have experienced intimate partner violence (3). The regions of Africa and Southeast Asia have reported the highest rates of IPV; higher-income regions like Europe and the Western Pacific exhibit a lower incidence of IPV, with reported prevalence rates ranging from 23 to 25% (4). Regarding different types of IPV, prevalence rates among Chinese college students were reported as 16.7% for physical harm, 18.9% for sexual coercion, and 51.8% for psychological harm (5). Beyond physical harm, these other forms are likely underreported.
Owing to its high occurrence, IPV is a significant concern for public health, greatly affecting both physical and mental well-being. Fractures, cuts, head injuries, sexually transmitted infections, unintended pregnancies, and pain disorders are some of the physical consequences that can occur from physical or sexual violence. Increasing evidence indicates that individuals who have encountered IPV are more susceptible to mental health issues (6), such as heightened vulnerability to depression, anxiety, post-traumatic stress disorder (PTSD), and suicide (7). However, there is less epidemiological evidence of relevance in contemporary Chinese populations. Exploring the relationship between IPV and depression under the background of China’s characteristic culture and system is helpful to enrich the relevant theoretical framework from different cultures and institutional groups.
1.1 IPV may relate to depression
For victims, apart from physical injuries, mental health problems especially depression and anxiety, are common (8). According to Bonomi et al. (9), women who experienced IPV within the previous year had a risk 3.26 times higher of developing depression compared to women who were not subjected to abuse. A positive association was found between IPV and postpartum depression, with IPV emerging as a primary predictor of postpartum depression compared with women who did not experience IPV (10). Depression in those experiencing IPV can lead to poor recovery from continuing abuse and an overall decrease in health for these individuals. Therefore, we predicted that IPV is associated with clinical depression in severe cases.
1.2 The mediating role of perceived social support
Individuals can feel valued, loved, and appreciated when they have social support, and these feelings allow them to believe that they are part of a community. Sources can include family members, friends, neighbors, and colleagues. This support may improve feelings of self-efficacy and enhance one’s ability to seek help (11), as well as reduce exposure to IPV. For example, talking to a family member at least once a month during pregnancy may decrease risk of both IPV overall and repeated episodes of IPV (12). This indicates that social support may protect against IPV.
Social support also mitigates the influence of IPV on subsequent mental health problems (13). Studies conducted on impoverished urban populations in the US indicate that individuals who encounter IPV are more likely to face mental health challenges if they are exposed to higher levels of violence and endure various forms of abuse, and social support may be an important protective factor for them (14). Adams et al. (15) also found that social support was an important factor in preventing depressive symptoms, and a lack of perceived social support could result in a higher prevalence of depression. Family support may be a particularly significant mediator in the relationship between abuse and mental health outcomes, including anxiety, depression, and PTSD (16). Moreover, seeking social support can improve individual psychological capacity and mitigate the negative mental health consequences of IPV, including depression (17, 18).
1.3 The moderating role of personality traits
The Big Five personality theory (also called the five-factor model) is commonly used in personality research. The Big Five Model represents five basic and universal traits related to broad personality dimensions: extraversion, agreeableness, conscientiousness, neuroticism, and openness (19). Certain personality traits are associated with depression. According to a meta-analysis of 175 studies, major depression is linked to high neuroticism and low conscientiousness and extraversion: neuroticism was a risk factor while extraversion and conscientiousness acted as protective factors (20). Another meta-analysis showed links between depressive symptoms and neuroticism, extraversion, and conscientiousness (21). This same pattern has also been reported for COVID-19 anxiety syndrome (22). These studies demonstrated that some personality traits are closely related to depression. Therefore, we hypothesized that personality traits can regulate depression.
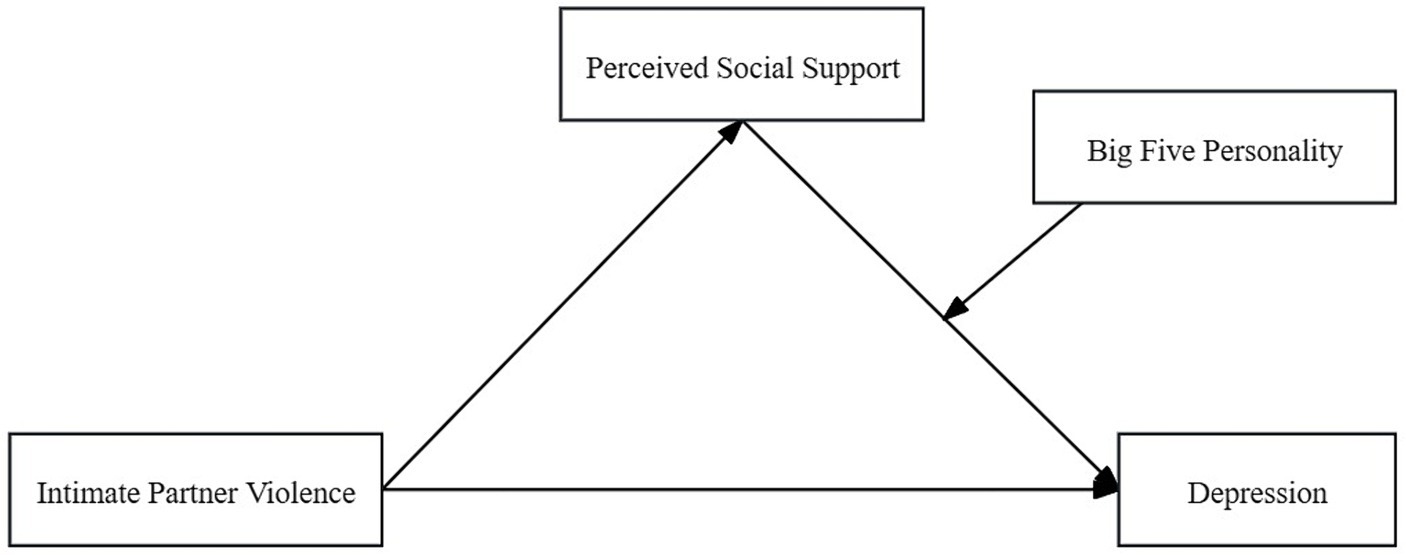
As shown in Figure 1, our study created a conceptual moderated mediation model to examine whether perceived social support mediates the relationship between IPV and depression and whether the Big Five personality traits moderate the relationship between perceived social support and depression.
We presented three hypotheses:
H1: IPV has a positive predictive effect on depression;
H2: Perceived social support mediates the relationship between IPV and depression;
H3: The Big Five personality traits moderate the relationship between perceived social support and depression.
2 Methods
2.1 Participants
The survey was conducted between June 20 and August 31, 2022, and was administered in 148 cities in the Chinese mainland, covering 23 provinces and 5 autonomous regions, including the capital cities of 4 municipalities and 2 to 6 non-provincial capitals. Data were collected through an anonymous electronic questionnaire on the WenJuanXing public online platform (https://www.wjx.cn), and 23,414 participants completed the questionnaire.
Responses were excluded if: (1) respondents completed the survey in less than 240 s; (2) the answers were logically inconsistent across items; or (3) the answers to all items were similar. Overall, 1,498 invalid responses were excluded, leaving 21,916 valid responses for further analysis. Participant ages ranged from 12 to 100 years (M = 39.43, SD = 18.85).
2.2 Procedure
The Institutional Ethics Committee of Shaanxi Provincial Key Research Base of Philosophy and Social Sciences-Health Culture Research Center (JKWH-2022-02) approved the research design. Before distributing the questionnaire, the investigators underwent comprehensive and specialized training that highlighted the fundamental aspects of the research, including the importance of maintaining anonymity, impartiality, and confidentiality. Participants provided informed consent before completing the questionnaire and the parents of the minor participants provided informed consent on behalf of the minor participants. The study excluded cognitively challenged participants.
2.3 Questionnaire
2.3.1 Intimate partner violence scale
We developed the Intimate Partner Violence Scale (IPVS) by referring to Straus et al.’s (23) revised Conflict Tactics Scale, which has five items that measure aspects of three dimensions: physical, sexual, and psychological harm. Examples of items include, “My intimate partner used to directly beat or use tools to hurt me” and “My intimate partner would compare me to other people, openly insult me, and make me feel embarrassed and unconfident.” Each item was rated from 0 (never) to 4 (often); therefore, a score of 1 indicated IPV and a higher score indicated a more severe experience. Cronbach’s alpha for the present sample was 0.908.
2.3.2 Patient health questionnaire
The 9-question Patient Health Questionnaire (PHQ-9), developed by Kroenke et al. (24), was used to measure depression severity in participants by surveying the participant’s psychological state over the past 2 weeks. Statements were assessed on a four-point Likert scale ranging from 0 (not at all) to 3 (nearly every day), and a higher composite score indicated more severe depression. Cronbach’s alpha for the present sample was 0.921.
2.3.3 Perceived social support scale
The Perceived Social Support Scale (PSSS) was used to identify an individual’s perceived level of social support from family, friends, and significant others. Developed by Zimet (25), it is reported to have good reliability and validity in Chinese social research. Items were rated from 1 (strongly disagree) to 7 (strongly agree), with a higher overall score indicating more perceived social support. Cronbach’s alpha for the present sample was 0.880.
2.3.4 Big Five inventory
The Big Five Inventory-short version (BFI-10), revised by Rammstedt and John (26), is a 10-item scale measuring the Big Five personality traits (e.g., “I see myself as someone who is reserved”). The statements were assessed on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The first, third, fourth, fifth, and seventh items were reverse-coded, and the sum of the corresponding question scores indicated which personality trait was most significant. Cronbach’s alpha for the present sample was 0.643.
2.4 Data analysis
Descriptive analyses, Pearson correlations, and common method bias tests were conducted in SPSS, version 26.0 (IBM Corp., Armonk, NY). The SPSS macro-PROCESS (model 4) was then adopted to examine the mediating role of perceived social support and the SPSS macro-PROCESS (model 14) was employed to investigate the moderating role of personality traits. To test statistical significance, 95% confidence intervals of the bias-corrected bootstrapped method were used based on 5,000 samples. Gender and age were used as control variables.
3 Results
3.1 Incidence of intimate partner violence
A total of 21,916 responses to the IPVS were included in data analysis (10,958 men and 10,958 women). Out of the 21,916 individuals surveyed, 4,454 individuals disclosed experiencing physical violence, accounting for a prevalence rate of 20.32%. Additionally, 3,869 respondents reported encountering sexual violence, resulting in a prevalence rate of 17.65%. Finally, 9,393 people reported at least one episode of psychological violence, for an incidence of 42.86%. A total of 9,709 reported experiencing IPV (determined by an IPVS score of 1 or greater), for an overall incidence of 44.30%.
3.2 Common method biases test
The Harman single-factor method was used to avoid the possibility of a common method bias problem. The results show that there were two factors with feature roots greater than one; the first factor explained 29.53% variation. Since it was below the 40% cut-off value, this indicated that there was no common methodological deviation.
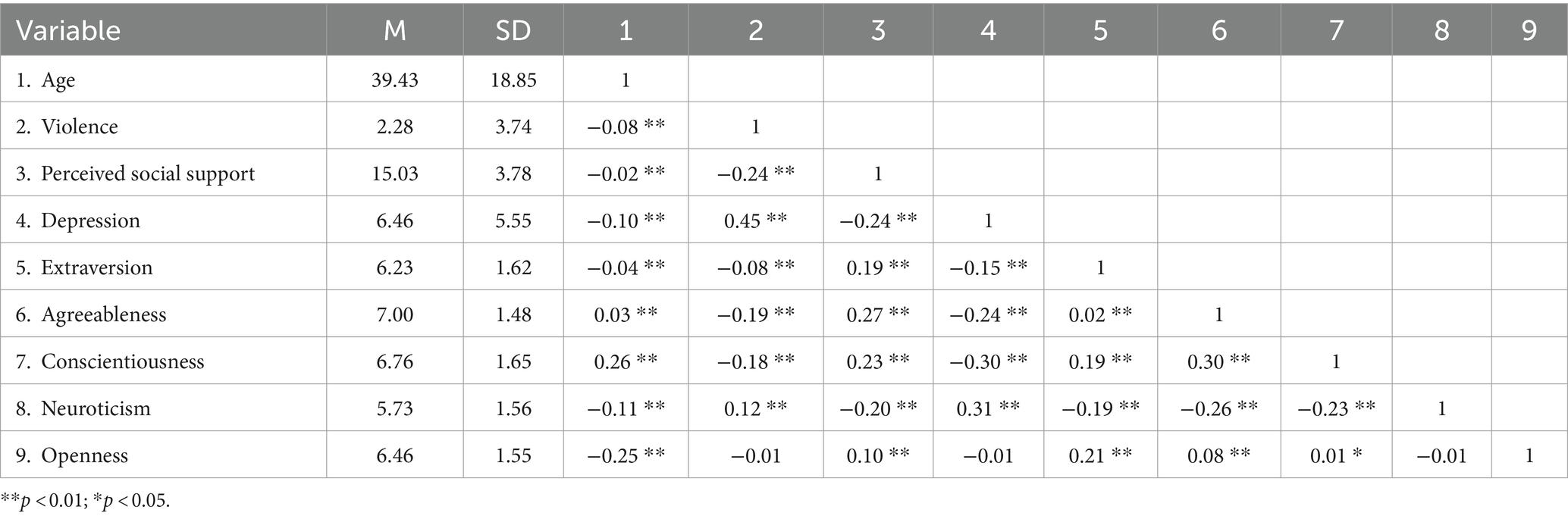
3.3 Descriptive statistics and correlations
The descriptive analyses and Pearson correlation results are shown in Table 1. IPV was significantly positively correlated with depression and significantly negatively correlated with perceived social support.
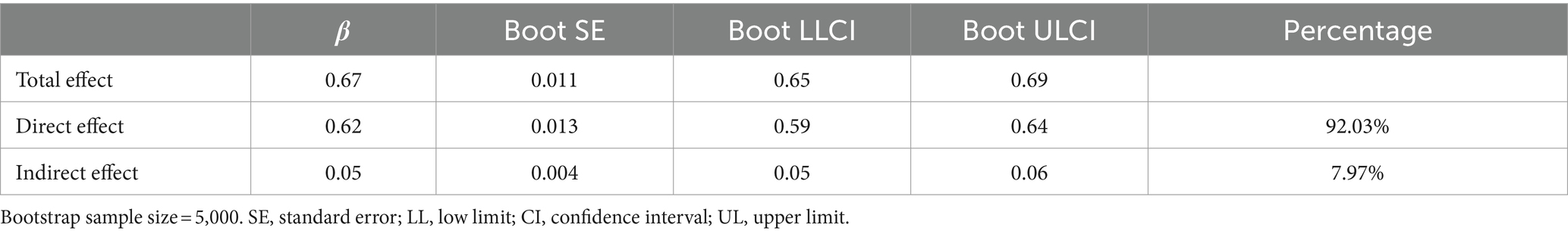
3.4 Exploring the mediating role of perceived social support
After controlling for age and gender, we used the SPSS macro-PROCESS (model 4) to examine the mediating effect of perceived social support on the link between IPV and depression (Table 2). Being subjected to violence was significantly positively correlated with experiencing depression (with a regression coefficient of β = 0.67, p < 0.05). When the mediating variable was included, IPV was significantly negatively correlated with perceived social support (β = −0.25, p < 0.05). Depression was also significantly negatively correlated with perceived social support (β = −0.22, p < 0.05), and was significantly positively correlated with being subjected to violence (β = 0.62, p < 0.05).
Additionally, the upper and lower bounds of the bootstrap (95% confidence interval) for the mediating effect of perceived social support did not contain zero (Table 3), indicating that perceived social support plays a mediating role in the link between IPV and depression.
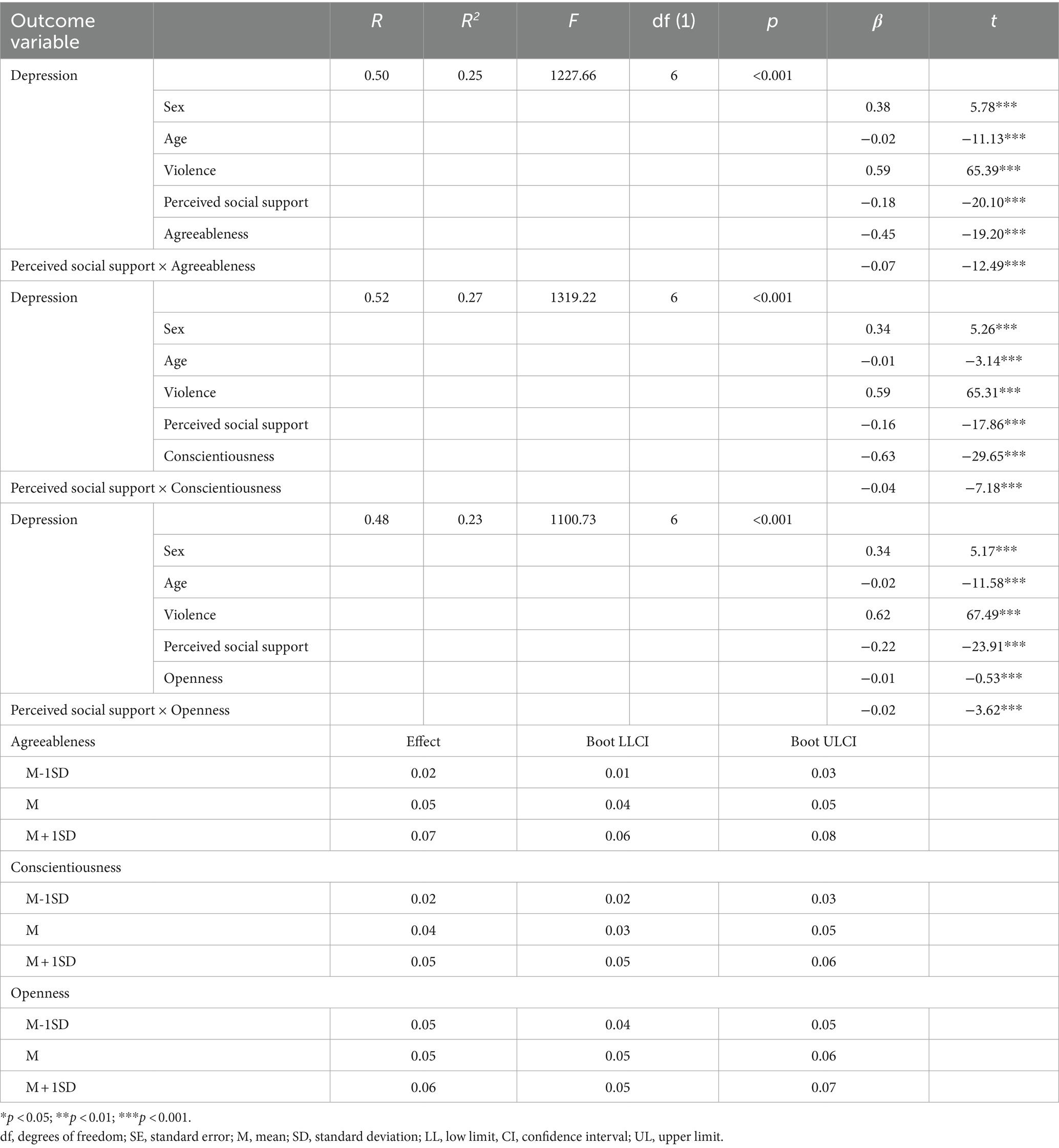
3.5 Exploring the moderating role of Big Five personality
Using gender and age as control variables, the SPSS macro-PROCESS (model 14) estimated the moderating effect of the five-factor model of personality traits within the mediation model (Table 4). Of the five traits, agreeableness, conscientiousness, and openness acted as moderators in the regression equation, while extraversion and neuroticism did not have a moderating effect in this equation; the interaction between social support and extraversion was non-statistically significant (β = 0.01, p > 0.05), as was the interaction between social support and neuroticism (β = 0.01, p > 0.05). After agreeableness (β = −0.18, p < 0.001), conscientiousness (β = −0.16, p < 0.001) and openness (β = −0.22, p < 0.001) were included as moderators in the regression equation, social support still negatively predicted depression. These findings indicate that even with moderators of agreeableness, conscientiousness, and openness, social support could still mediate the relationship between IPV and depression.
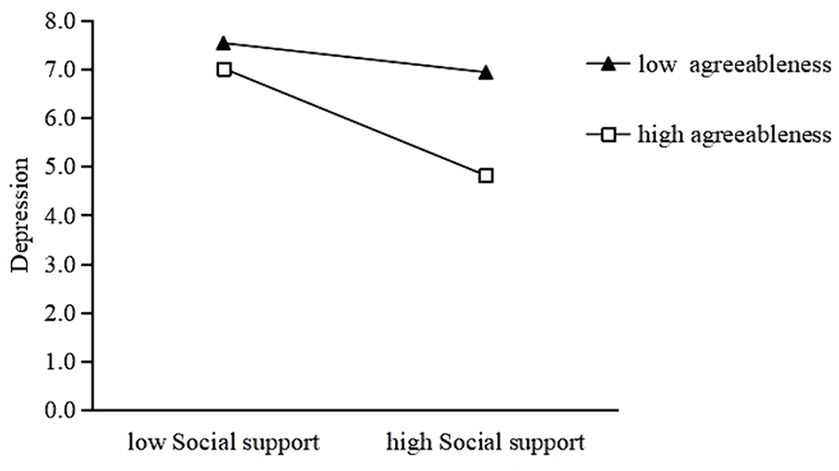
Moreover, the interaction of social support and agreeableness (β = −0.07, p < 0.001), conscientiousness (β = −0.04, p < 0.001), and openness (β = −0.02, p < 0.001) had a significantly negative effect on depression. On this basis, three simple slope analyses were performed to deconstruct these significant interaction effects between the three traits and PHQ-9 scores. Figure 2 shows that this effect was stronger for people with high agreeableness (simple slope = −0.29, p < 0.001) than for people with low agreeableness (simple slope = −0.08, p < 0.001).
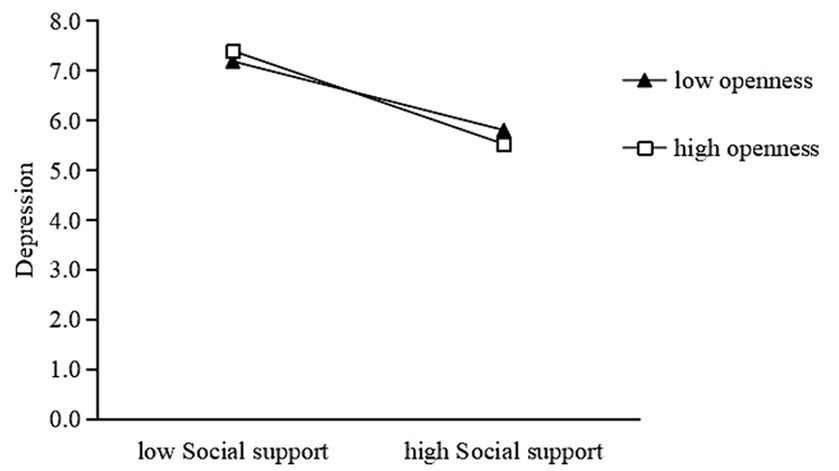
Figures 3, 4 show a similar effect for people with high conscientiousness (simple slope = −0.22, p < 0.001) and openness (simple slope = −0.25, p < 0.001) that was stronger than the effect in people with low conscientiousness (simple slope = −0.10, p < 0.001) and openness (simple slope = −0.18, p < 0.001). Thus, high levels of agreeableness, conscientiousness, and openness may strengthen the negative association between social support and depression.
4 Discussion
Based on previous research results and related theories, this study constructed a moderated mediation model to explore the relationship and mechanism between IPV and depression. We sought to answer questions about how IPV can affect depressive symptoms (mediating mechanisms) and the personality conditions under which the effects of IPV on depression were more significant (moderating mechanisms). Our findings reveal the impact of IPV on depression and provide potential direction for interventions in patients experiencing IPV.
4.1 Current incidence of intimate partner violence
The incidence of 44.30% in this study indicated that IPV is a serious and widespread public health problem which deserves attention. Further, participants reported a higher prevalence of psychological violence than physical or sexual violence. Psychological violence often accompanies physical and sexual violence in high proportions; however, psychological violence can exist independently (27, 28).
4.2 Perceived social support plays a mediating role in depression
Our results (consistent with and expanding upon previous studies) not only indicate that IPV is often accompanied by depression, but that social support could act as a mediator to reduce the negative effects of violence and symptoms of depression. Social support is an important protective factor against depression (29, 30). Nasser and Overholser (31) found that higher levels of emotional support from friends or family were significantly associated with lower levels of depression, which enhanced recovery from major depression and decreased the number of admissions to psychiatric facilities. IPV can have short- and long-term negative consequences on an individual’s physical, mental, and sexual health (32). When individuals are under stress, perceived social support can moderate their experience by enabling them to adjust their emotional stress and alleviate their depression symptoms (33). Therefore, healthcare workers should assess social support and provide adequate care or recommendations for increasing social support when patients with IPV report depressive symptoms.
4.3 The Big Five personality traits play a moderating role between social support and depression
The results revealed that traits of agreeableness, conscientiousness, and openness moderated the relationship between social support and depression, while extraversion and neuroticism did not. Agreeableness, conscientiousness, and openness also moderated the association between IPV and depressive symptoms; specifically, individuals with high agreeableness, conscientiousness, and openness were less likely to experience depression. Previous studies indicated links between depression and traits such as neuroticism, extraversion, and conscientiousness (34, 35). Consistent with the observations of Lewis and Cardwell (36), low conscientiousness was predictive of increased mental illness in this study, particularly depressive symptoms. Linley and Joseph (37) also found that personality traits such as extraversion, openness, agreeableness, and conscientiousness could all contribute to positive or beneficial responses after experiencing trauma and adversity. Social withdrawal and a lack of interest or engagement in activities are both manifestations of low agreeableness and openness, as well as symptoms of depression. Low conscientiousness may not cause depression directly, but it could lead to depressive experiences such as academic difficulties, job loss, and relationship problems (38). This study fills a gap between IPV and depression by revealing the personality factors that affect whether IPV leads to depression.
Our study focused on a specific sample of the Chinese mainland, which may have unique cultural factors influencing the relationship between extraversion and the variables studied. Thus, our findings are somewhat different from previous studies. In this study, the moderating effect of extraversion is non-significant on depression, whereas previous studies have shown that increased extraversion is beneficial to mental health (39). The reason may be the complexity of extraversion psychological factors. First, extraversion can be divided into two more specific aspects including Communal Extraversion and Agentic Extraversion (40). At the second level, these two aspects can be further divided into four consensual facets: Sociability, Liveliness, Venturesomeness, and Dominance (41). Communal Extraversion is negatively correlated with psychopathology, while Agentic Extraversion is often positively related to psychopathology, and too much Venturesomeness may lead to mania (42). Different features of extraversion are responsible for these positive and negative associations with psychopathology. Second, participants may have Counter dispositional behaviors, which refer to deliberately showing extraversion because they want to get better, even when this extroverted behavior is the opposite of a person’s (introverted) personality (43). Behaving discordant to one’s trait level is demanding and effortful to maintain and should therefore cause impaired levels of well-being (44).
4.4 Limitations
Despite the contributions of our study, we also must acknowledge this study has two limitations: First, our data are cross-sectional study which is difficult to verify the causal relationships. Second, the data were collected from self-report questionnaire measures, it is still inevitable for the information bias because of the over-reporting or under-reporting. Future studies might establish the causal relationship and mechanisms between IPV, depression, and social support by implementing longitudinal research designs. Additionally, a more objective measure of Big Five personality and depression can be used in future studies.
5 Conclusion
Our findings revealed that IPV is positively associated with depression and negatively associated with the mediating effect of social support. The indirect effects of IPV on depression were moderated by agreeableness, conscientiousness, and openness. The adverse effects of IPV on mental health may be mitigated by increasing available social support for patients experiencing IPV and require further research. Using these findings, patients can be coached by professionals to improve their resiliency by developing or nurturing more optimistic personality traits to bolster mental health during IPV or other setbacks, thereby helping to prevent depression.
Data availability statement
The datasets presented in this article are available from the corresponding author, JC, upon reasonable request. Persons who have made outstanding contributions or assisted in this study may apply for the use of the data only after submitting the study hypothesis and signing a data confidentiality agreement. There is no fee for the data opening plan. Publication of the study results will include processed data only, and personal information will remain anonymous. Requests to access the datasets should be directed to JC, Y2p5MTEyQGkuc211LmVkdS5jbg==.
Ethics statement
The studies involving humans were approved by the Shaanxi Provincial Key Research Base of Philosophy and Social Sciences-Health Culture Research Center (JKWH-2022-02). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
ZL: Writing – original draft, Writing – review & editing. YG: Writing – original draft, Data curation, Investigation, Methodology. YL: Methodology, Supervision, Writing – original draft. WX: Data curation, Investigation, Writing – original draft. LL: Investigation, Writing – original draft. SL: Investigation, Writing – original draft. HZ: Investigation, Writing – original draft. XY: Investigation, Writing – original draft. YW: Resources, Writing – review & editing. JC: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The work is supported by the Plan on Enhancing Scientific Research in GMU; the National Natural Science Foundation of China (grant number 72204107); the Medical Scientific Research Foundation of Guangdong Province (grant number A2023125); Accredited Scientific Research Project (Featured Innovation Project) of Universities in Guangdong Province (grant number 2021WTSCX072); Philosophy and Social Sciences Key Laboratory of Guangdong Higher Education Institutes for Health Governance Based on Big Data Utilization, Guangzhou Medical University.
Acknowledgments
Thanks to Editage for the language editing service.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
IPV, Intimate Partner Violence; CDC, Centers for Disease Control and Prevention; PTSD, Post-Traumatic Stress Disorder; COVID-19, Coronavirus Disease 2019; SD, Standard Deviation; IPVS, Intimate Partner Violence Scale; PHQ, Patient Health Questionnaire; PSSS, Perceived Social Support Scale; BFI, Big Five Inventory
References
1. Campbell, JC. Health consequences of intimate partner violence. Lancet. (2002) 359:1331–6. doi: 10.1016/S0140-6736(02)08336-8
2. Miller, E, and McCaw, B. Intimate partner violence. N Engl J Med. (2019) 380:850–7. doi: 10.1056/NEJMra1807166
3. World Health Organization (2014). Violence against women: intimate partner and sexual violence against women (fact sheet). Available at: https://apps.who.int/iris/handle/10665/112325. (Accessed August 13, 2023).
4. Chisholm, CA, Bullock, L, and Ferguson, JEJ. Intimate partner violence and pregnancy: epidemiology and impact. Am J Obstet Gynecol. (2017) 217:141–4. doi: 10.1016/j.ajog.2017.05.042
5. Kadir Shahar, H, Jafri, F, Mohd Zulkefli, NA, and Ahmad, N. Prevalence of intimate partner violence in Malaysia and its associated factors: a systematic review. BMC Public Health. (2020) 20:1550. doi: 10.1186/s12889-020-09587-4
6. Ahmadabadi, Z, Najman, JM, Williams, GM, Clavarino, AM, d’Abbs, P, and Tran, N. Intimate partner violence and subsequent depression and anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:611–20. doi: 10.1007/s00127-019-01828-1
7. Cho, H, and Kwon, I. Intimate partner violence, cumulative violence exposure, and mental health service use. Community Ment Health J. (2018) 3:259–266. doi: 10.1007/s10597-017-0204-x
8. Wathen, CN, MacGregor, JCD, and MacQuarrie, BJ. Relationships among intimate partner violence, work, and health. J Interpers Violence. (2018) 33:2268–90. doi: 10.1177/0886260515624236
9. Bonomi, AE, Anderson, ML, Reid, RJ, Rivara, FP, Carrell, D, and Thompson, RS. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med. (2009) 169:1692–7. doi: 10.1001/archinternmed.2009.292
10. Shwartz, N, O’Rourke, N, and Daoud, N. Pathways linking intimate partner violence and postpartum depression among Jewish and Arab women in Israel. J Interpers Violence. (2022) 37:301–21. doi: 10.1177/0886260520908022
11. Dias, NG, Costa, D, Soares, J, Hatzidimitriadou, E, Ioannidi-Kapolou, E, Lindert, J, et al. Social support and the intimate partner violence victimization among adults from six European countries. Fam Pract. (2019) 36:117–24. doi: 10.1093/fampra/cmy042
12. Navarrete, L, Nieto, L, and Lara, MA. Intimate partner violence and perinatal depression and anxiety: social support as moderator among Mexican women. Sex Reprod Healthc. (2021) 27:100569. doi: 10.1016/j.srhc.2020.100569
13. Pir, S, Hashemi, L, Gulliver, P, McIntosh, T, and Fanslow, J. Which aspects of social support enhance positive mental health in the context of intimate partner violence? Violence Against Women. (2023) 9:1787–1810. doi: 10.1177/10778012221114919
14. Humm, A, Kaminer, D, and Hardy, A. Social support, violence exposure and mental health among young south African adolescents. J Child Adolesc Ment Health. (2018) 30:41–50. doi: 10.2989/17280583.2018.1476358
15. Adams, TR, Rabin, LA, Da Silva, VG, Katz, MJ, Fogel, J, and Lipton, RB. Social support buffers the impact of depressive symptoms on life satisfaction in old age. Clin Gerontol. (2016) 39:139–57. doi: 10.1080/07317115.2015.1073823
16. Lagdon, S, Ross, J, Robinson, M, Contractor, AA, Charak, R, and Armour, C. Assessing the mediating role of social support in childhood maltreatment and psychopathology among college students in Northern Ireland. J Interpers Violence. (2021) 36:NP2112–2136NP. doi: 10.1177/0886260518755489
17. Kamimura, A, Parekh, A, and Olson, LM. Health indicators, social support, and intimate partner violence among women utilizing services at a community organization. Womens Health Issues. (2013) 23:e179–85. doi: 10.1016/j.whi.2013.02.003
18. Sylaska, KM, and Edwards, KM. Disclosure of intimate partner violence to informal social support network members: a review of the literature. Trauma Violence Abuse. (2014) 15:3–21. doi: 10.1177/1524838013496335
19. Goldberg, LR. The development of markers for the big-five factor structure. Psychol Assess. (1992) 4:26–42. doi: 10.1037/1040-3590.4.1.26
20. Kotov, R, Gamez, W, Schmidt, F, and Watson, D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. (2010) 136:768–821. doi: 10.1037/a0020327
21. Hakulinen, C, Elovainio, M, Pulkki-Råback, L, Virtanen, M, Kivimäki, M, and Jokela, M. Personality and depressive symptoms: individual participant meta-analysis of 10 cohort studies. Depress Anxiety. (2015) 32:461–70. doi: 10.1002/da.22376
22. Nikčević, AV, Marino, C, Kolubinski, DC, Leach, D, and Spada, MM. Modelling the contribution of the big five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. J Affect Disord. (2021) 279:578–84. doi: 10.1016/j.jad.2020.10.053
23. Straus, MA, Hamby, SL, Boney-McCoy, S, and Sugarman, DB. The revised conflict tactics scales (CTS2): development and preliminary psychometric data. J Fam Issues. (1996) 17:283–316. doi: 10.1177/019251396017003001
24. Kroenke, K, Spitzer, RL, and Williams, JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
25. Zimet, GD, Powell, SS, Farley, GK, Werkman, S, and Berkoff, KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. (1990) 55:610–7. doi: 10.1080/00223891.1990.9674095
26. Rammstedt, B, and John, OP. Measuring personality in one minute or less: a 10-item short version of the Big Five inventory in English and German. J Res Pers. (2007) 41:203–12. doi: 10.1016/j.jrp.2006.02.001
27. Coker, AL, Smith, PH, McKeown, RE, and King, MJ. Frequency and correlates of intimate partner violence by type: physical, sexual, and psychological battering. Am J Public Health. (2000) 90:553–9. doi: 10.2105/ajph.90.4.553
28. Hou, J, Yu, L, Ting, SR, Sze, YT, and Fang, X. The status and characteristics of couple violence in China. J Fam Viol. (2011) 26:81–92. doi: 10.1007/s10896-010-9343-3
29. Tonsing, K, Zimet, GD, and Tse, S. Assessing social support among south Asians: the multidimensional scale of perceived social support. Asian J Psychiatr. (2012) 5:164–8. doi: 10.1016/j.ajp.2012.02.012
30. Shih, TY, Cheng, SL, Chang, SH, and Sun, HF. Perceived social support and depression symptoms in patients with major depressive disorder in Taiwan: an association study. Arch Psychiatr Nurs. (2020) 34:384–90. doi: 10.1016/j.apnu.2020.06.004
31. Nasser, EH, and Overholser, JC. Recovery from major depression: the role of support from family, friends, and spiritual beliefs. Acta Psychiatr Scand. (2005) 111:125–32. doi: 10.1111/j.1600-0447.2004.00423.x
32. Oram, S, Fisher, HL, Minnis, H, Seedat, S, Walby, S, and Hegarty, K. The lancet psychiatry commission on intimate partner violence and mental health: advancing mental health services, research, and policy. Lancet Psychiatry. (2022) 6:487–524. doi: 10.1016/S2215-0366(22)00008-6
33. Serkut Bulut, N, Yorguner, N, and Akvardar, Y. Impact of COVID-19 on the life of higher-education students in İstanbul: Relationship between social support, health-risk behaviors, and mental/academic well-being. Alpha Psychiatry. (2021) 6:291–300. doi: 10.1530/alphapsychiatry.2021.21319
34. Klein, DN, Kotov, R, and Bufferd, SJ. Personality and depression: explanatory models and review of the evidence. Annu Rev Clin Psychol. (2011) 7:269–95. doi: 10.1146/annurev-clinpsy-032210-104540
35. Odachi, R, Takahashi, S, Sugawara, D, Tabata, M, Kajiwara, T, Hironishi, M, et al. The Big Five personality traits and the fear of COVID-19 in predicting depression and anxiety among Japanese nurses caring for COVID-19 patients: a cross-sectional study in Wakayama prefecture. PLoS One. (2022) 17:e0276803. doi: 10.1371/journal.pone.0276803
36. Lewis, EG, and Cardwell, JM. The Big Five personality traits, perfectionism and their association with mental health among UK students on professional degree programmes. BMC Psychol. (2020) 8:54. doi: 10.1186/s40359-020-00423-3
37. Linley, PA, and Joseph, S. Positive change following trauma and adversity: a review. J Trauma Stress. (2004) 17:11–21. doi: 10.1023/B:JOTS.0000014671.27856.7e
38. Roberts, BW, Kuncel, NR, Shiner, R, Caspi, A, and Goldberg, LR. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspect Psychol Sci. (2007) 2:313–45. doi: 10.1111/j.1745-6916.2007.00047.x
39. Tan, CS, Low, SK, and Viapude, GN. Extraversion and happiness: the mediating role of social support and hope. Psych J. (2018) 7:133–43. doi: 10.1002/pchj.220
40. DeYoung, CG, and Quilty, L. Between facets and domains: 10 aspects of the Big Five. J Pers Soc Psychol. (2007) 93:880–96. doi: 10.1037/0022-3514.93.5.880
41. Naragon-Gainey, K, and Watson, D. Consensually-defined facets of personality as prospective predictors of change in depression symptoms. Assessment. (2014) 21:387–403. doi: 10.1177/1073191114528030
42. David, W, Kasey, S, Shereen, K, and Sara, M. Extraversion and psychopathology: a multilevel hierarchical review. J Res Pers. (2019) 81:1–10. doi: 10.1016/j.jrp.2019.04.009
43. Kuijpers, E, Pickett, J, Wille, B, and Hofmans, J. Do you feel better when you behave more extraverted than you are? The relationship between cumulative Counterdispositional extraversion and positive feelings. Personal Soc Psychol Bull. (2022) 48:606–23. doi: 10.1177/01461672211015062
Keywords: intimate partner violence, depression, perceived social support, five-factor personality model, resiliency
Citation: Luo Z, Guan Y, Li Y, Xu W, Li L, Liu S, Zhou H, Yin X, Wu Y and Chen J (2024) The relationship of intimate partner violence on depression: the mediating role of perceived social support and the moderating role of the Big Five personality. Front. Public Health. 12:1402378. doi: 10.3389/fpubh.2024.1402378
Edited by:
Ashwani Kumar Mishra, All India Institute of Medical Sciences, IndiaReviewed by:
Julak Lee, Chung-Ang University, Republic of KoreaMomcilo Mirkovic, University of Pristina, Serbia
Copyright © 2024 Luo, Guan, Li, Xu, Li, Liu, Zhou, Yin, Wu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yibo Wu, YmptdXd1eWlib0BvdXRsb29rLmNvbQ==; Jiangyun Chen, Y2p5MTEyQGkuc211LmVkdS5jbg==
†These authors share first authorship
 Zhenni Luo
Zhenni Luo Yan Guan
Yan Guan Yun Li
Yun Li Weihong Xu
Weihong Xu Lu Li1
Lu Li1 Siyuan Liu
Siyuan Liu Yibo Wu
Yibo Wu Jiangyun Chen
Jiangyun Chen