- 1Clinic of Obstetrics and Gynecology, “S. Maria della Misericordia” University Hospital, Azienda Sanitaria Universitaria Friuli Centrale (ASUFC), Udine, Italy
- 2Dipartimento per le Scienze Della Salute Della Donna, del Bambino e di Sanità Pubblica, UOC Ginecologia Oncologica, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- 3Division of Gynaecology and Obstetrics, Santa Maria Annunziata Hospital, USL Toscana Centro, Florence, Italy
- 4General Surgery Clinic and Liver Transplant Center, University Hospital of Udine, Udine, Italy
- 5Gynecologic and Obstetric Clinic, Department of Medicine, Surgery and Pharmacy, University of Sassari, Sassari, Italy
- 6Department of Gynecology and Obstetrics of "San Giovanni Calibita" Fatebenefratelli Hospital-Gemelli Hospital, Rome, Italy
- 7Dipartimento di Ginecologia Oncologica e Chirurgia Ginecologica Miniinvasiva, Università degli studi di Messina, Policlinico G. Martino, Messina, Italy
- 8Department of Medicine, University of Udine, Udine, Italy
- 9Department of General Surgery and Liver Transplantation, San Camillo Forlanini Hospital, Rome, Italy
- 10Department of General Surgery, Sapienza Università di Roma, Rome, Italy
- 11Unit of Gynecologic Oncology, National Cancer Institute, IRCCS, Fondazione "G. Pascale", Naples, Italy
Introduction: Surgical-related injuries are frequent, in fact the reported percentage of musculoskeletal disorders in surgeons is between 47% and 87%. These conditions are caused by long periods of standing, incorrect postures, repeated movements, little rest between operations, the lack of integrated operator rooms, the correct number and arrangement of monitors and the use of non-ergonomic instruments. This survey aims to assess the Italian overview both highlighting how prevalent surgical-related injury is in our surgeons and whether there is an operating room ergonomics education program in Italian surgical specialty schools.
Methods: An anonymous questionnaire was designed through SurveyMonkey© web application. This survey was composed of 3 different sections concerning the general characteristics of the participants, their surgical background and any training performed, and any injuries or ailments related to the surgical activity. The survey was carried out in the period 1th of December 2022 and the 6th of February 2023.
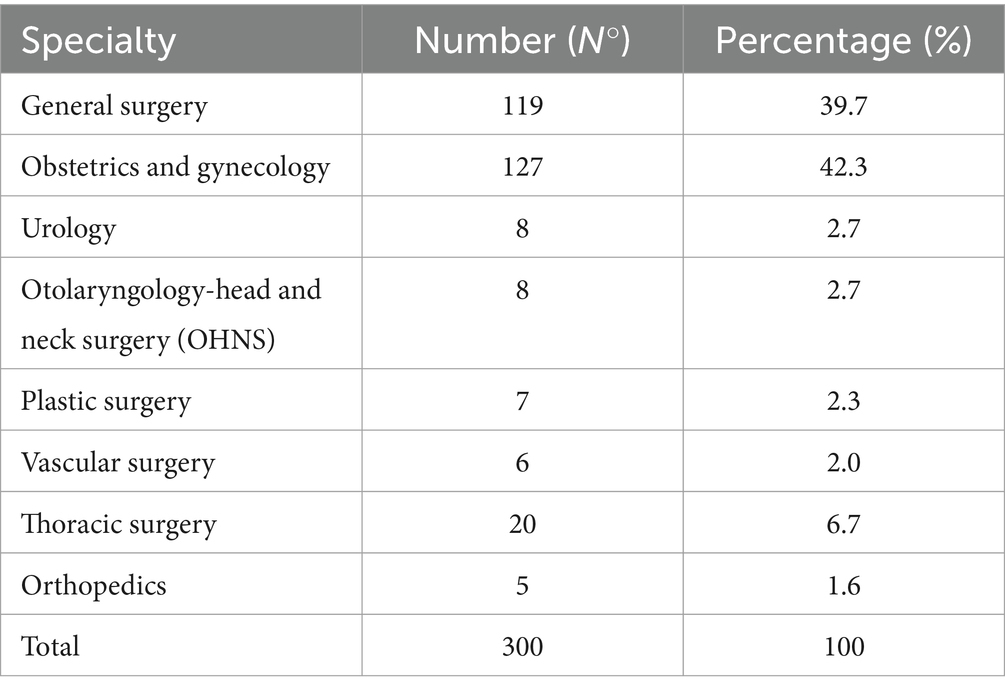
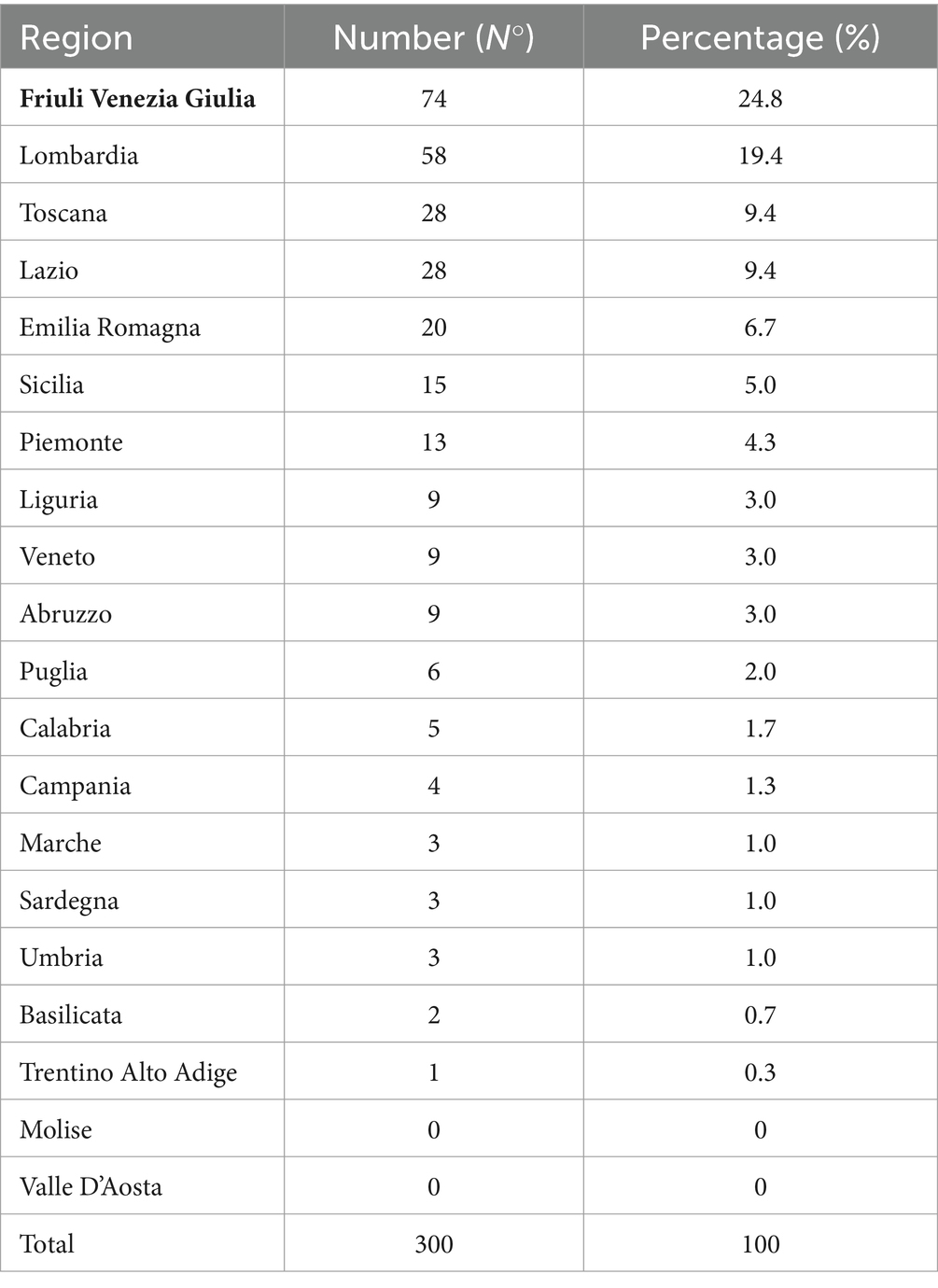
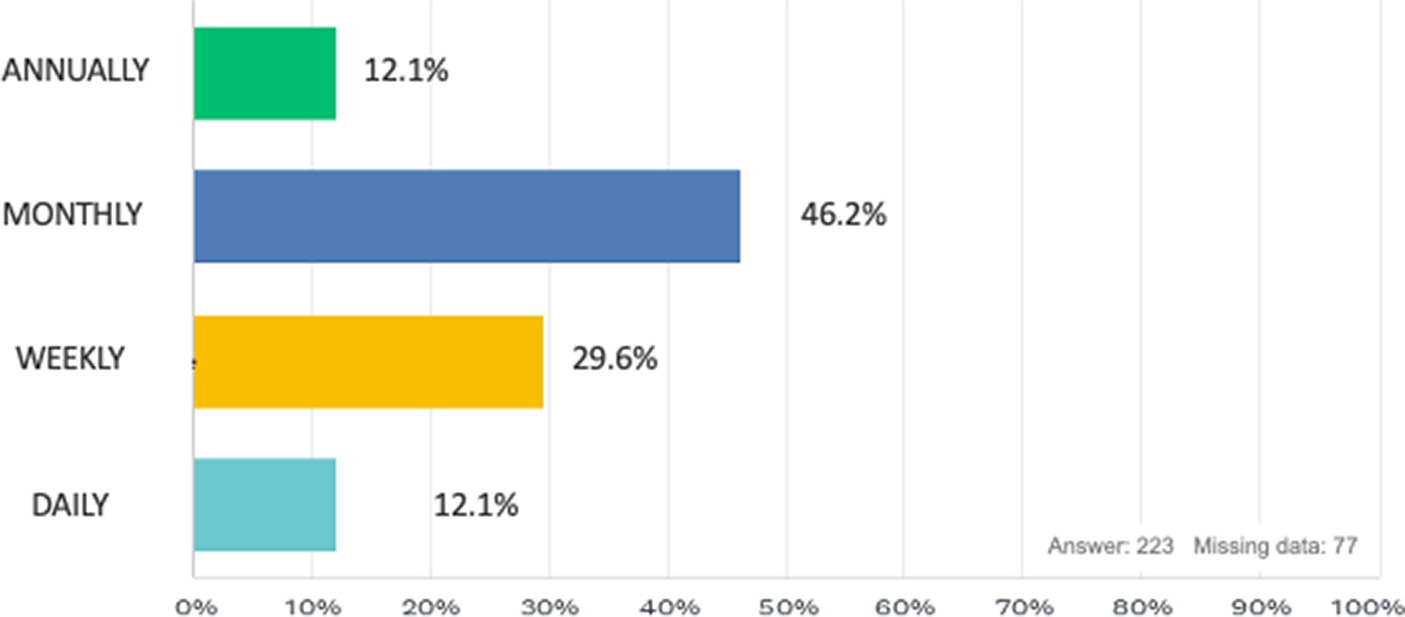
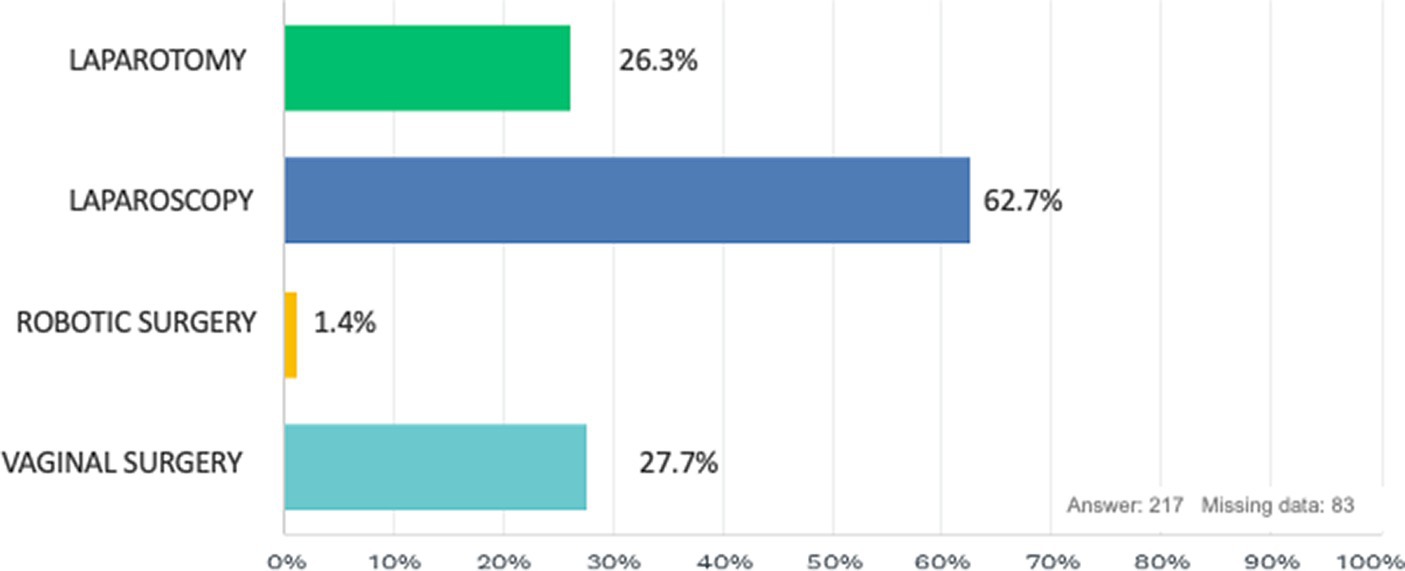
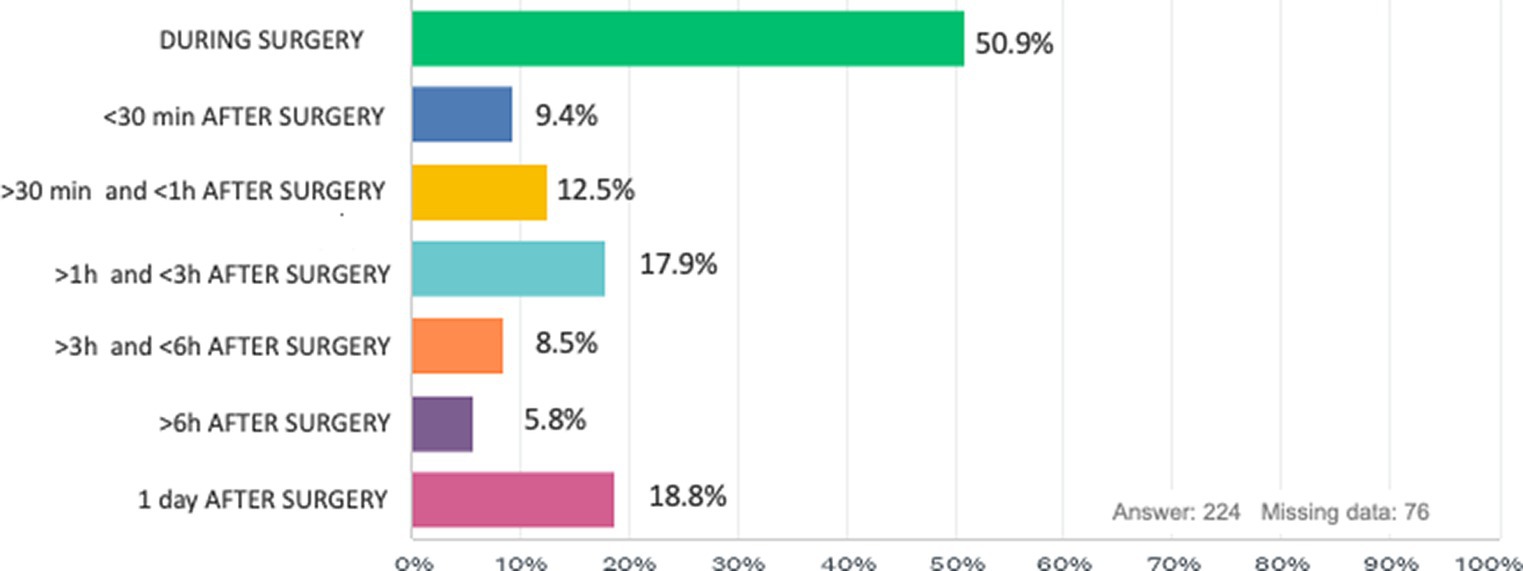
Results: At the close of our survey, 300 responses were collected. Among the participants, the two most represented specialties were Gynecology and Obstetrics (42.3%) and General Surgery (39.7%) and surgeons were mainly employed in the Northern regions of Italy (54.8%). Analyzing the participants’ background, 61.7% of the respondents had laparoscopic training during their training and only 53.1% had a pelvic trainer during their residency. In accordance with 98.7% of the respondents, during surgery we have the feeling of being in an uncomfortable position that causes discomfort or muscle pain, and regarding the frequency of these discomforts, the majority of our study population experiences these problems monthly (46.2%), while in 29.6% it is experienced weekly, 12.1% annually and finally 12.1% daily. The surgical approach that is most correlated with these disorders is laparoscopy (62.7%) while the one that causes the least discomfort is robotic surgery (1.4%). These discomforts cause 43.9% of our population to take a break or do short exercises to reduce pain during surgery, and the body areas most affected are the back (61.6%), neck (40.6%) and shoulders (37.8%).
Conclusion: Despite this, our survey allows us to highlight some now-known gaps present in the surgical training program of our schools and the lack of protection toward our surgeons during their long career.
1 Introduction
Over the past years, minimally invasive surgery (laparoscopic or robotic) has gained wide acceptance in gynecology compared to the laparotomic approach due to its surgical as well as clinical benefits for patients, such as reduced operating time, less intra-operative blood loss, shorter postoperative hospital stay, lower rates of postoperative fever and infection and finally a faster patient recovery (1–3).
While such surgery is certainly a benefit for our patients, the emergence and spread of minimally invasive surgery has introduced ergonomic risks for surgeons (for example, including instrument length and handle design, improper monitor position, and excessively high operating tables) (4) and, although this issue is well known, the safety and health of physicians have received less attention than that of patients (5).
Surgical-related injuries are frequent, in fact the reported percentage of musculoskeletal disorders in surgeons ranges between 47% and 87% (5–11). These conditions are caused by long periods of standing, incorrect postures, repeated movements, little rest between operations, the lack of integrated operator rooms, the incorrect number and arrangement of monitors and the use of non-ergonomic instruments (12–15). These situations are also exacerbated by the altruistic attitudes of surgeons who often maintain incorrect postures for long periods to benefit their patients’ health or to increase their productivity, to the detriment of their own (15–17).
To reduce these conditions, there has been a growing interest in implementing strategies that reduce work-related injuries in surgeons (15).
Implementing ergonomic guidelines involves several strategies aimed at minimizing musculoskeletal disorders risks:
• Adjustable Equipment: operating room tables and surgical instruments should be adjustable to accommodate different body sizes and postures. Tables should be set at a height that allows the surgeon to maintain a neutral spine position without bending or stretching excessively (18).
• Neutral Body Posture: Surgeons and OR staff should maintain a neutral body posture, which includes keeping the neck in a neutral position, the back straight, and avoiding rotation or tilt of the torso. Shoulders should be relaxed, and elbows kept close to the body (19).
• Regular Breaks and Microbreaks: Implementing scheduled breaks and microbreaks can help reduce physical strain. During these breaks, stretching exercises and movements to relieve tension in specific muscle groups are recommended (20).
• Ergonomic Training Programs: Regular training on ergonomic principles should be provided to OR staff. This training can include proper lifting techniques, posture correction, and the use of ergonomic tools and equipment (20).
Despite our knowledge of the problem and our efforts, to date an educational program in surgical schools regarding proper ergonomics in the operating room is still not widely available. In fact, not all surgeons are aware of the existence of guidelines on ergonomics in the operating room and ergonomics education programs are not yet firmly established within surgical schools (21, 22).
From this background, we wanted to assess the Italian overview both by highlighting the prevalence of surgical-related injury in our surgeons and by investigating the existence of an operating room ergonomics education program in Italian surgical residency programs.
2 Materials and methods
We designed an electronic anonymous questionnaire on SurveyMonkey© web application (SVMK Inc., One Curiosity Way, San Mateo, United States) (23). The aim of this survey was explained to all participants with a brief introduction. Participation to the survey was voluntary, and no incentives were offered. No institutional review board approval was required.
The survey was composed of three different sections (Supplementary material S1). The first section included questions regarding biographical information, one’s role (physician in specialty training, structured physician, or other), one’s place of employment, and one’s surgical specialty. The second section focused on type and frequency of surgical activity routinely performed, on laparoscopic surgical training, whether surgical training would have been useful in their surgical formation, and what tools are used to increase their skills.
The last section dealt with ergonomics in the operating room, the occurrence and frequency of surgical practice-related injuries, the correlation between ailments and the organization/arrangement of one’s operating room, and whether these injuries affected personal life or required specific medical treatments for their resolution or improvement.
The study was conducted from 1th of December 2022 to the 6th of February 2023 and promoted with a mailing list, instant message services, and through the main social media Official account of the authors on Facebook, Instagram, and Linked-in, thanks to the support of the Italian Polyspecialistic Society of Young Surgeons (SPIGC).
Italian surgeons coming from any surgical specialty and attending any year of the training program were considered eligible for the survey’s analysis. The eligibility has no relation to the residents’ curricular activities. All participants were informed that the results of the survey would have been used for further statistical evaluation and scientific publication. Anonymity was guaranteed by study design.
After the closing date for questionnaire submissions, results were downloaded as a CSV (comma-separated values) file to be analyzed via Excel (Microsoft Corporation, Redmond, United States).
Results of the survey were reported according to the CHERRIES Guidelines (24).
3 Results
At the close of our survey, 300 responses were collected. Among the participants, the two most represented specialties were Gynecology and Obstetrics (42.3%) and General Surgery (39.7%) (Table 1) and surgeons were mainly employed in the Northern regions of Italy (54.8%; Table 2). The characteristics of the participants are summarized in Table 3. 50.8% were men while 49.2% were women; the most represented age group was between 31 and 40 years (46.2%) while 46% of the population were surgeons in training while 54% were already specialized physicians. 41.8% had performed less than 50 operations in the last 12 months, while 28.1% had performed between 50 and 100 operations and 30.1% more than 100 operations. Lastly, the number of surgeons with more than 150 procedures as first operator was 95 (36.0%), while 126 participants had performed less than 50 procedures (47.7%).
3.1 Role of training in our surgical population
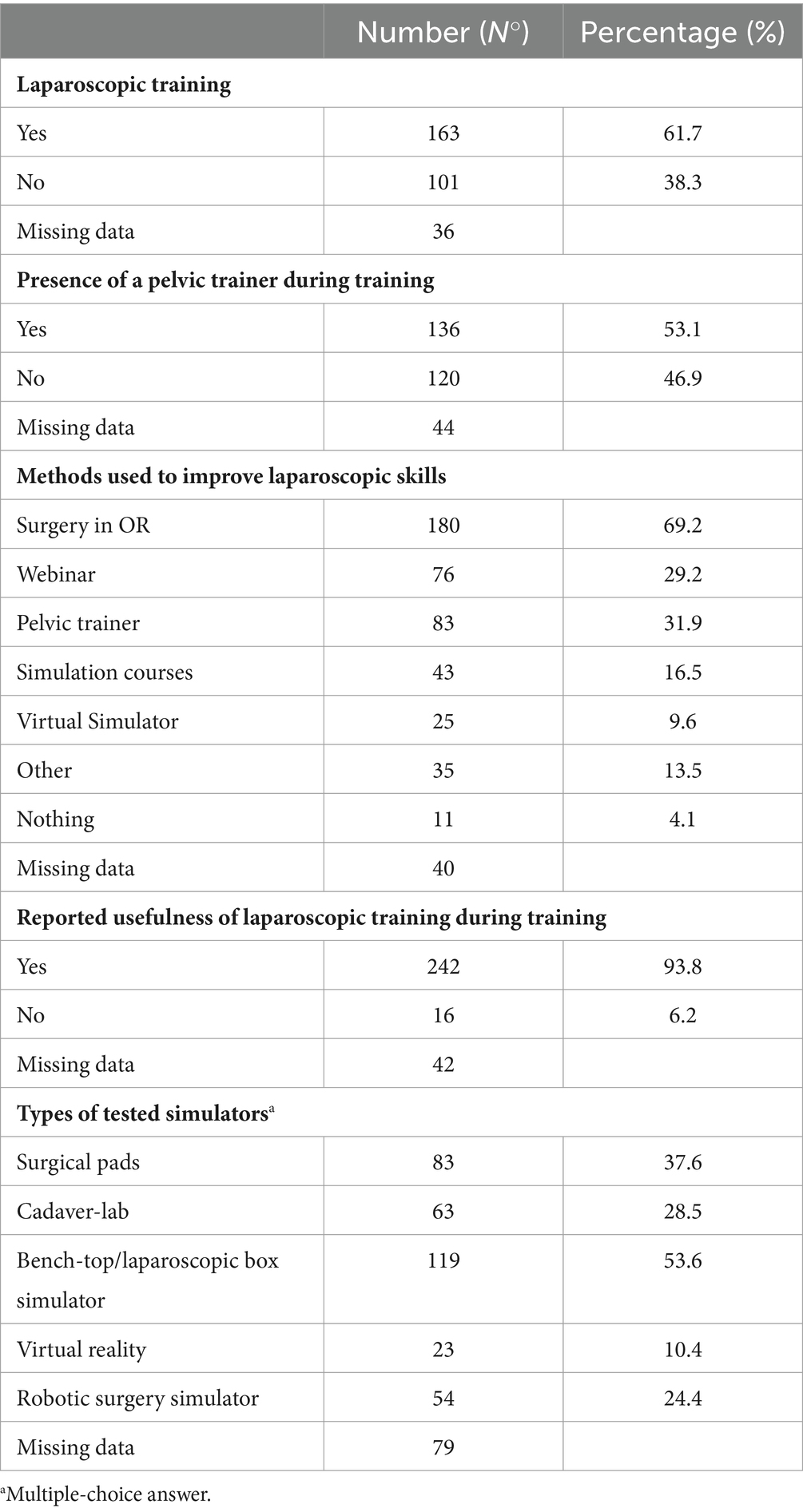
Analyzing the participants’ background, 61.7% of the respondents had laparoscopic training during their training and only 53.1% had a pelvic trainer during their residency (see Table 4). Regarding the opinion on the usefulness of laparoscopic training during their formation, 93.8% stated that it would be extremely useful. Concerning the activities used to implement their laparoscopic skills, 69.2% of the participants stated that they directly used the operating room while only 31.2% used the pelvic trainer, 29.2% webinars, 9.6% the virtual simulator and 4.1% no method. Among the most used surgical simulators we found the bench-top (53.6%), surgical pads (37.6%), cadaver-lab (28.5%), robotic simulator (24.4%) and virtual reality (10.4%).
3.2 Ergonomics and injuries in our surgical population
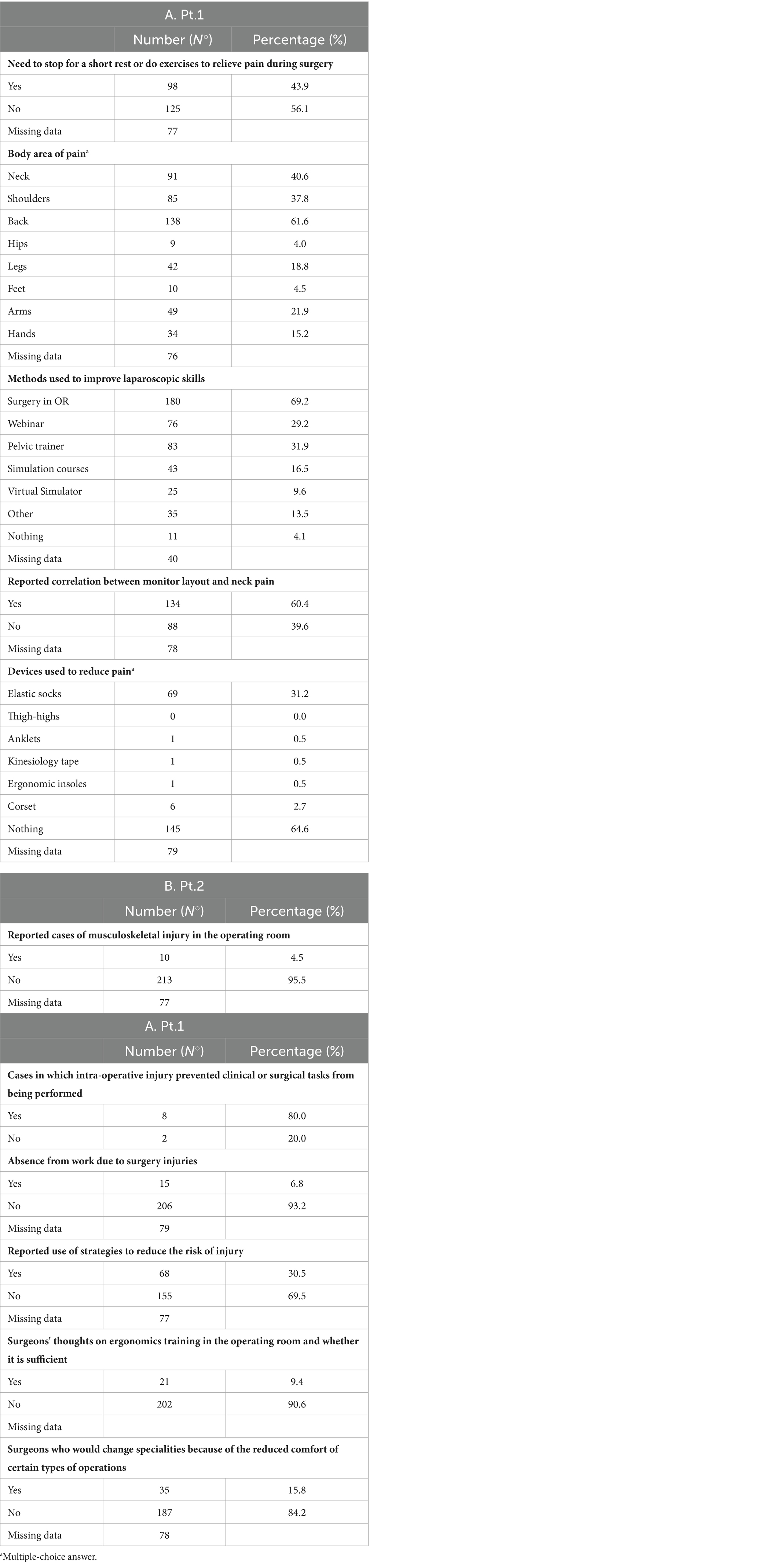
In accordance with 98.7% of the respondents, during surgery we have the feeling of being in an uncomfortable position that causes discomfort or muscle pain (Figure 1), and regarding the frequency of these discomforts, the majority of our study population experiences these problems monthly (46.2%), while in 29.6% it is experienced weekly, 12.1% annually and finally 12.1% daily (Figure 2). The surgical approach that is most correlated with these disorders is laparoscopy (62.7%) while the one that causes the least discomfort is robotic surgery (1.4%; Figure 3). Regarding the onset from surgery, problems occur most immediately during the surgical procedure (50.9%) or within 3 h after surgery (Figure 4).
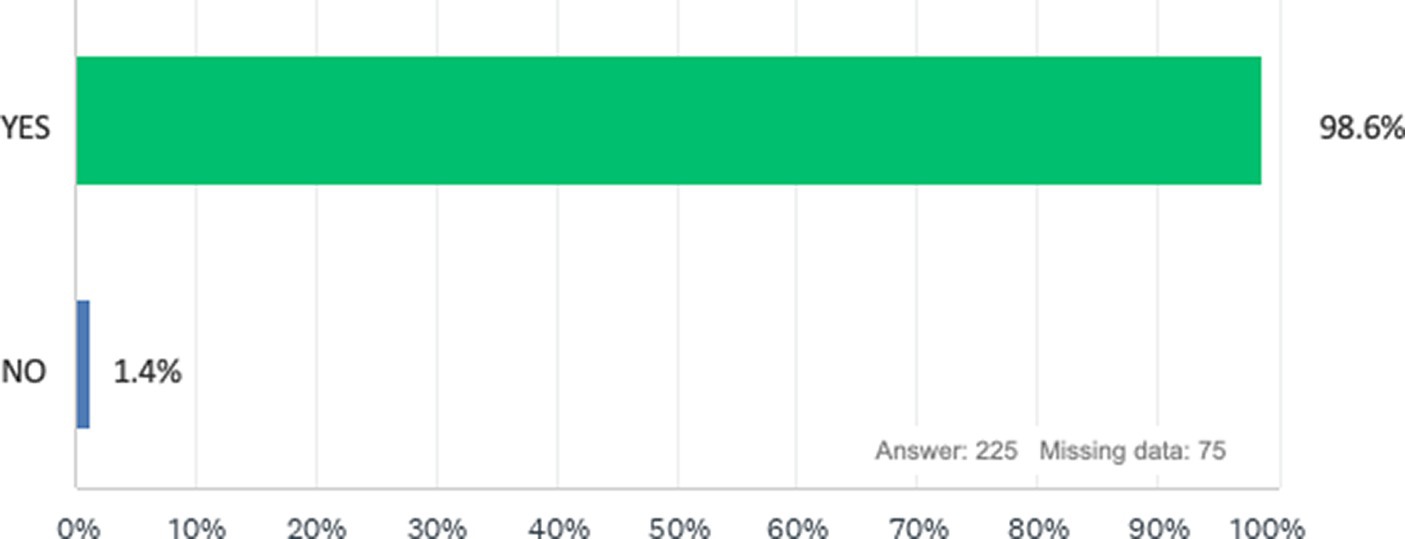
Figure 1. Have you ever had the feeling that your body was in an uncomfortable position in the operating room causing discomfort, muscle aches or pain during retraction, assistance or surgery?
These discomforts cause 43.9% of our population to take a break or do short exercises to reduce pain during surgery, and the body areas most affected are the back (61.6%), neck (40.6%) and shoulders (37.8%). 60.4% also report a correlation of their discomfort with the arrangement of monitors in the operating room.
Regarding the use of devices to reduce these discomforts, 64.6% of the population reports that they do not use any while only 31.2% use elastic stockings and 2.7% use a corset. In addition, cases of true muscle injuries were also reported in 4.5% of the population that in 80% of cases led to discontinuation of clinical or surgical practice and in 6.8% of cases required abstention from work. In addition, in our population 9.4% stated that their knowledge of ergonomics in the operating room was sufficient to avoid problems or discomfort, and as many as 15.8% stated that they would change their surgical specialty in favor of specialists who are less physically straining (Tables 5A,B).
4 Discussion
Our survey reveals that the perception of incorrect body position in the operating room and related physical disorders are extremely common among Italian surgeons, with 99% of surgeons reporting this perception in our study. These data highlight the need to improve ergonomic education in our surgeons during their training and to determine strategies that can avoid or reduce work-related injuries in the operating room. The purpose of our study was to investigate the availability of laparoscopic training and ergonomics training of Italian surgeons and to assess whether they suffer from physical complaints related to clinical practice during surgical activities. Our rates of musculoskeletal disorders are similar to those already reported in the scientific literature (5), and the most affected areas were the neck, shoulders, and low back. As reported in our survey, among the different surgical approaches the one most associated with discomfort is laparoscopy, reported by 63% of our participants, and this data is in line with those found in the literature. Due to previous studies, it is already known that the trapezius, deltoid and inferior spinal erector muscles are the ones most subjected to load from laparoscopy (25), which can lead to muscle injury or fatigue. The laparoscopic surgeon’s posture is characterized by increased elbow flexion with biceps activation and wrist flexion with ulnar carpal flexor activation (26). Non-ergonomic postures assumed in laparoscopic surgery can lead to an increased risk of fatigue during procedures and injury (27) while correct positioning, as proven in a 2012 study (28), may be associated with improved procedure performance, reduced excessive joint movements, and therefore lower risk of injury. Another interesting finding relates to laparoscopic training and ergonomics education in the operating room, which 94% of participants would have found useful during their specialized training and 61.7% of the respondents had laparoscopic training during their training. To date, there is little data available about ergonomic training programs in surgery and how they may affect surgical outcomes. A study performed by Franasaik et al. (29) developed a surgical ergonomics project for robotic surgery to demonstrate correct body positioning and strategies to avoid incorrect postures. The results of this study revealed that 88% of participants corrected their habits in the operating room and 74% reduced their physical stress during robotic surgery after taking part in the training course. Among surgery ergonomics programs, the one at Duke University is one of the few that focuses on residents in that it allows younger residents and students to be assisted and observed by older residents and also they are equipped with ergonomic lenses and have to use microbreaks and anti-fatigue mats during operations (30). In addition, another key role is assumed by ergonomics and the almost total absence of education during specialty training and consequent assumption of incorrect postures or attitudes during surgical practice. Lessons in surgical ergonomics can focus on explaining what are the main causes of physical stress and injuries (e.g., non-ergonomic postures, prolonged maintenance of the same posture, repeated physical stress) and showing what exercises can prevent these injuries (e.g., exercises to increase grip strength, wrist extension and/or flexion, or exercises to increase muscle strength). Our survey represents a picture of the current state of surgical education in Italy and of disorders related to the surgical profession, on which attention is rarely focused. There is now an urgent need for ergonomics in the operating room to be included within the training program of residents in order to better prepare surgeons for surgeries and prolong their careers, and for a reminder of proper postural habits to be included during surgical time-out to ensure proper operating room setup and improve surgical team members’ adherence to ergonomic principles.
Also, the importance of trainees’ opinions and benchmarks in laparoscopy is crucial for the continuous improvement of surgical education and practice. Several studies highlight this significance and underscore the value of incorporating feedback and structured training programs to enhance the skills and confidence of surgical trainees.
A study by De Franciscis et al. (31) emphasizes the need to assess the effects of tissue sealers in minor laparoscopic procedures. This prospective cohort study involving obstetrics and gynecology residents shows that trainee feedback is essential for evaluating new surgical technologies and their practical applications in clinical settings. By incorporating trainees’ perspectives, the study aims to enhance surgical outcomes and training efficiency.
Additionally, the development of a standardized laparoscopy curriculum for gynecology residents, as outlined by Shore et al. (32), demonstrates the critical role of trainee input in designing educational programs. This study used a Delphi approach to reach a consensus among experts, ensuring that the curriculum meets the educational needs of trainees and aligns with current surgical standards. The involvement of trainees in this process helps create a more relevant and effective training program.
Further validation of this standardized curriculum was conducted through a randomized controlled trial by Shore et al. (33), which highlighted the importance of structured training and assessment. This study confirmed that a well-designed curriculum improves laparoscopic skills and confidence among gynecology residents. The inclusion of trainee feedback in the validation process ensures that the curriculum addresses the practical challenges faced by residents during their training.
Regarding the powers of our paper, one of the primary strengths is its comprehensive data collection. By including 300 participants, the survey ensures a robust sample size that enhances the reliability and generalizability of its findings. The detailed demographic breakdown, with Gynecology and Obstetrics (42.3%) and General Surgery (39.7%) being the most represented specialties, offers targeted insights into the specific ergonomic challenges these surgeons face. Additionally, the survey highlights significant gaps in training, revealing that 61.7% had laparoscopic training and only 53.1% had access to a pelvic trainer during residency. This information is crucial for improving surgical education and training programs.
Another notable strength is the detailed reporting of ergonomic issues. The survey indicates that 98.7% of respondents experience discomfort or muscle pain during surgery, with varying frequencies of discomfort (monthly, weekly, annually, daily). This nuanced data underscores the prevalence and severity of ergonomic problems in the surgical field.
Despite its strengths, the survey has some notable weaknesses. The reliance on self-reported data introduces potential bias, as participants might underreport or overreport their experiences and discomfort levels. The absence of objective ergonomic assessments limits the precision and quantifiability of the data on physical strain experienced by surgeons.
Additionally, the variability in training experiences among respondents indicates a lack of standardized training programs, which could affect the consistency of the data. The focus on Gynecology, Obstetrics, and General Surgery, while providing specific insights, excludes other specialties that may also face significant ergonomic challenges.
Despite this, our survey allows us to highlight some now-known gaps present in the surgical training program of our schools and the lack of protection toward our surgeons during their long career. Certainly in support of this thesis, further studies will be needed to ascertain internationally the shortcomings in surgical training and injury rates related to operating room practice, and to this end, a new survey with worldwide dissemination is currently being conducted (ERGO Study) (34), whose data are currently being analyzed. The care of patients is essential but, to be able to treat them in the best manner possible, our health and physical care should also be a priority, and to achieve this target, technology should also be a valuable ally, always trying to use it in the best possible way.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
SR: Writing – review & editing. MD'I: Writing – original draft, Data curation. FP: Data curation, Investigation, Validation, Writing – review & editing. MA: Conceptualization, Formal analysis, Visualization, Writing – review & editing. VChe: Conceptualization, Visualization, Writing – review & editing. MP: Validation, Visualization, Writing – original draft. ACa: Supervision, Visualization, Writing – original draft. SC: Supervision, Visualization, Writing – original draft. GP: Investigation, Methodology, Writing – original draft. RM: Investigation, Supervision, Writing – original draft. ACo: Validation, Visualization, Writing – original draft. VChi: Supervision, Visualization, Writing – original draft. GS: Supervision, Visualization, Writing – original draft. LD: Supervision, Visualization, Writing – original draft. GV: Data curation, Formal analysis, Supervision, Visualization, Writing – original draft.
SPIGC working group
Collaborators to be indexed:
Executive Committee: Federico Berton, Luigi Conti, Giampaolo Formisano, Eleonora Guaitoli, Angelo Iossa, Michele Maruccia, Andrea Mazzari, Luigi Oragano, Alessandro Pasculli, Francesca Ratti, Matteo Serenari, Alberto Settembrini, Pasqualino Sirignano, Domenico Soriero, Carlo Vallicelli.
Regional Lead: Stefano Cianci (Sicilia), Giulia De Iaco (Puglia), Francesca Falcone (Campania), Sara Giaccari (Triveneto), Marco Giovenzana (Lombardia), Edoardo Pasqui (Toscana), Marco Petrillo (Sardegna), Luca Portigliotti (Piemonte), Giuseppe Sena (Calabria), Marco Sparavigna (Liguria).
Dissemination Committee: Giordana Bettini, Gianfranco Fanello, Paolo Mendogni, Lorenzo Monteleone, Davide Pertile Nicoletta Pia Ardò, Pasquina Tomaiuolo, Sara Negrello, Mattia Di Bartolomeo, Romeo Patini, Alberto Vito Marcuzzo, Alberto Campione, Giovanni Comacchio, Giacomo Murana, Martino Antonio, Mattia Manitto, Giuseppe Galzerano, Carlo Di Marco, Francesco Velluti, Gianmauro Berardi, Andrea Romboli, Jacopo Weindelmejer, Domenico Tamburrino, Alessandro Calarco, Luigi Losco, Eleonora Nacchiero, Rossella Elia, Federico Lo Torto, Giovanni Vicenti, Vincenzo Pappalardo, Dafne Pisani, Graziano Palmisano, Debora Brascia, Luigi Troisi, Federica Renzi, Fabio Melandro, Silvia Pecere, Carlo Gazia, Gregorio Di Franco, Gaetano Romano, Alberto Bolletta, Emanuele Botteri, Giovanna Di Meo, Carlo Ronsini, Sonia Chiappetta, Ilaria Sgaramella, Francesco Pennestri, Antonella Girardi, Donatella Mariniello, Marco Marcasciano, Michele Telegrafo, Simona Fragomeni, Francesca De Paoli, Giorgio Bogani, Salvatore Gueli Alletti, Luigi Pedone Anchora, Luigi Della Corte, Elisa Piovano, Martina Borghese, Cristina Taliento, Diego Raimondo, Antonio Raffone, Jvan Casarin, Emanuele Perrone, Guglielmo Stabile, Vito Capozzi.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1417250/full#supplementary-material
References
1. Aarts, J, Nieboer, T, Johnson, N, Tavender, E, Garry, R, Mol, BWJ, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. (2015) 2015:CD003677. doi: 10.1002/14651858.CD003677.pub5
2. Hajenius, PJ. Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev. (2007) 1:CD000324. doi: 10.1002/14651858.CD000324.pub2
3. Medeiros, LRF, Rosa, DD, Bozzetti, MC, Fachel, JMG, Furness, S, Garry, R, et al. Laparoscopy versus laparotomy for benign ovarian tumour. Cochrane Database Syst Rev. (2009) 2:CD004751. doi: 10.1002/14651858.CD004751.pub3
4. Matern, U. Ergonomic deficiencies in the operating room: examples from minimally invasive surgery. Work. (2009) 33:165–8. doi: 10.3233/WOR-2009-0862
5. Park, A, Lee, G, Seagull, FJ, Meenaghan, N, and Dexter, D. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. (2010) 210:306–13. doi: 10.1016/j.jamcollsurg.2009.10.017
6. Babar-Craig, H, Banfield, G, and Knight, J. Prevalence of back and neck pain amongst ENT consultants: national survey. J Laryngol Otol. (2003) 117:979–82. doi: 10.1258/002221503322683885
7. Bolduc-Begin, J, Prince, F, Christopoulos, A, and Ayad, T. Work-related musculoskeletal symptoms amongst otolaryngologists and head and neck surgeons in can-ada. Eur Arch Otorrinolaringol. (2018) 275:261–7. doi: 10.1007/s00405-017-4787-1
8. Rimmer, J, Amin, M, Fokkens, WJ, and Lund, VJ. Endo-scopic sinus surgery and musculoskeletal symp-toms. Rhinology. (2016) 54:105–10. doi: 10.4193/Rhino15.217
9. Little, RM, Deal, AM, Zanation, AM, McKinney, K, Senior, BA, and Ebert, CS Jr. Occupational hazards of endoscopic surgery. Int Forum Allergy Rhinol. (2012) 2:212–6. doi: 10.1002/alr.20108
10. Alleblas, CCJ, de Man, AM, van den Haak, L, Vierhout, ME, Jansen, FW, and Nieboer, TE. Prevalence of musculo-skeletal disorders among surgeons performing mini-mally invasive surgery: a systematic review. Ann Surg. (2017) 266:905–20. doi: 10.1097/SLA.0000000000002223
11. Alqahtani, SM, Alzahrani, MM, and Tanzer, M. Adult recon-structive surgery: a high-risk profession for work-related injuries. J Arthroplast. (2016) 31:1194–8. doi: 10.1016/j.arth.2015.12.025
12. Vijendren, A, Yung, M, and Sanchez, J. Occupational health issues amongst UK doctors: a literature review. Occup Med. (2015) 65:519–28. doi: 10.1093/occmed/kqv088
13. Wyatt, RW, Lin, CC, Norheim, EP, Przepiorski, D, and Nav Arro, RA. Occupation-related cervical spine disease in orthopaedic surgeons. J Am Acad Orthop Surg. (2020) 28:730–6. doi: 10.5435/JAAOS-D-19-00834
14. Davila, VJ, Meltzer, AJ, Fortune, E, MMB, M, Lowndes, BR, Linden, AR, et al. Intraproce-dural ergonomics of vascular surgeons. J Vasc Surg. (2020) 73:301–8. doi: 10.1016/j.jvs.2020.04.523
15. Fisher, SM, Teven, CM, and Song, DH. Ergonomics in the operating room: the cervicospinal health of today’s surgeons. Plast Reconstr Surg. (2018) 142:1380–7. doi: 10.1097/PRS.0000000000004923
16. Kroth, PJ, Morioka-Douglas, N, Veres, S, Babbott, S, Poplau, S, Qeadan, F, et al. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Netw Open. (2019) 2:e199609. doi: 10.1001/jamanetworkopen.2019.9609
17. Koshy, K, Syed, H, Luckiewicz, A, Alsoof, D, Koshy, G, and Harry, L. Interventions to improve ergonomics in the operating theatre: a systematic review of ergonomics training and intra-operative microbreaks. Ann Med Surg. (2020) 55:135–42. doi: 10.1016/j.amsu.2020.02.008
18. American College of Surgeons. Surgical Ergonomics Recommendations. (2023). Available at: https://www.facs.org/media/tdeemrnw/23_ed_surgicalergonomicsrecommendations_pdf_v4.pdf
19. Vural, F, and Sutsunbuloglu, E. Ergonomics: an important factor in the operating room. J Perioper Pract. (2016) 26:174–8. doi: 10.1177/1750458916026007-804
20. Alaqeel, M, and Tanzer, M. Improving ergonomics in the operating room for orthopaedic surgeons in order to reduce work-related musculoskeletal injuries. Ann Med Surg. (2020) 56:133–8. doi: 10.1016/j.amsu.2020.06.020
21. Wauben, LS, van Veelen, MA, Gossot, D, and Goossens, RH. Application of ergonomic guidelines during minimally invasive surgery: a questionnaire survey of 284 surgeons. Surg Endosc. (2006) 20:1268–74. doi: 10.1007/s00464-005-0647-y
22. Franasiak, J, Ko, EM, Kidd, J, Secord, AA, Bell, M, Boggess, JF, et al. Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol. (2012) 126:437–42. doi: 10.1016/j.ygyno.2012.05.016
23. Survey Monkey. Available at: https://www.surveymonkey.com (n.d.)
24. Eysenbach, G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res. (2004) 6:e34. doi: 10.2196/jmir.6.3.e34
25. Uhrich, ML, Underwood, RA, Standeven, JW, Soper, NJ, and Engsberg, JR. Assessment of fatigue, monitor placement, and surgical experience during simulated laparoscopic surgery. Surg Endosc. (2002) 16:635–9. doi: 10.1007/s00464-001-8151-5
26. Lee, GI, Lee, MR, Clanton, T, Sutton, E, Park, AE, and Marohn, MR. Comparative assessment of physical and cogånitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc. (2014) 28:456–65. doi: 10.1007/s00464-013-3213-z
27. Dalager, T, Søgaard, K, Bech, KT, Mogensen, O, and Jensen, PT. Musculoskeletal pain among surgeons performing minimally invasive surgery: a systematic review. Surg Endosc. (2017) 31:516–26. doi: 10.1007/s00464-016-5020-9
28. Xiao, DJ, Jakimowicz, JJ, Albayrak, A, and Goossens, RH. Ergonomic factors on task performance in laparoscopic surgery training. Appl Ergon. (2012) 43:548–53. doi: 10.1016/j.apergo.2011.08.010
29. Franasiak, J, Craven, R, Mosaly, P, and Gehrig, PA. Feasibility and acceptance of a robotic surgery ergonomic training program. JSLS. (2014) 18:e2014.00166. doi: 10.4293/JSLS.2014.00166
30. Walker, B. Duke surgery introduces ergonomics program to improve surgeon health. (2017). Available at: https://surgery.duke.edu/news/duke-surgery-introduces-ergonomics-program-improve-surgeon-health (Accessed 19 June 2020).
31. De Franciscis, P, La Verde, M, Cobellis, L, Mollo, A, Torella, M, De Simone, F, et al. Ascertaining the effects of tissue sealers on minor laparoscopic procedures between obstetrics and gynecology residents: a prospective cohort study. Medicina. (2022) 58:578. doi: 10.3390/medicina58050578
32. Shore, EM, Grantcharov, TP, Husslein, H, Shirreff, L, Dedy, NJ, CD, MD, et al. Validating a standardized laparoscopy curriculum for gynecology residents: a randomized controlled trial. Am J Obstet Gynecol. (2016) 215:204.e1-204.e11. doi: 10.1016/j.ajog.2016.04.037
33. Shore, EM, Lefebvre, GG, Husslein, H, Bjerrum, F, Sorensen, JL, and Grantcharov, TP. Designing a standardized laparoscopy curriculum for gynecology residents: a Delphi approach. J Grad Med Educ. (2015) 7:197–202. doi: 10.4300/JGME-D-14-00548.1
34. ERGO-study. Ergonomics in the operating room (ERGO-study). (n.d.) Available at: https://forms.gle/CwfBTyViTBGt8DPu8
Keywords: surgery, ergonomic, gyne and obstetrics, operatory room, survey
Citation: Restaino S, D’Indinosante M, Perelli F, Arcieri M, Cherchi V, Petrillo M, Cavaliere AF, Cianci S, Pellecchia G, Meniconi RL, Coppola A, Chiantera V, Scambia G, Driul L, Vizzielli G and SPIGC Working Group (2024) Ergonomics in the operating room and surgical training: a survey on the Italian scenario. Front. Public Health. 12:1417250. doi: 10.3389/fpubh.2024.1417250
Edited by:
Luigi Della Corte, University of Naples Federico II, ItalyReviewed by:
Mario Palumbo, Federico II University Hospital, ItalyGaetano Riemma, University of Campania Luigi Vanvitelli, Italy
Copyright © 2024 Restaino, D’Indinosante, Perelli, Arcieri, Cherchi, Petrillo, Cavaliere, Cianci, Pellecchia, Meniconi, Coppola, Chiantera, Scambia, Driul, Vizzielli and SPIGC Working Group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco D’Indinosante, bWFyY28uZGluZGlub3NhbnRlQGd1ZXN0LnBvbGljbGluaWNvZ2VtZWxsaS5pdA==
 Stefano Restaino
Stefano Restaino Marco D’Indinosante
Marco D’Indinosante Federica Perelli
Federica Perelli Martina Arcieri
Martina Arcieri Vittorio Cherchi4
Vittorio Cherchi4 Marco Petrillo
Marco Petrillo Anna Franca Cavaliere
Anna Franca Cavaliere Stefano Cianci
Stefano Cianci Roberto Luca Meniconi
Roberto Luca Meniconi Alessandro Coppola
Alessandro Coppola Vito Chiantera
Vito Chiantera Giovanni Scambia
Giovanni Scambia Lorenza Driul
Lorenza Driul Giuseppe Vizzielli
Giuseppe Vizzielli