- 1Sciences, Achva Academic College, Arugot, Israel
- 2Business School, Ono Academic College, Kiryat Ono, Tel Aviv District, Israel
Introduction: Patient-centered care (PCC) is the preferred health policy approach that emphasizes responding to individual patient preferences, wishes, and needs. PCC requires active patient engagement. While there has been extensive research on physicians' robes, there is limited research on hospital-issued patient gowns during hospitalizations. How does the gown affect the cognitive–emotional experience of hospitalized patients? How is the gown associated with PCC?
Methods: The sample of this cross-sectional study consisted of 965 patients who were hospitalized at least once during the past year in a tertiary hospital. Measures were previously published.
Results: The gown was strongly associated with lack of control and increased distress, and was negatively associated with patient proactiveness, engagement, and taking responsibility for self-management of chronic illness. Compared to male patients, female patients wearing the gown had stronger negative emotions and cognitively strong associations with the external locus of control, which inhibited engagement.
Discussion: The hospital gown is an unacknowledged barrier to achieving PCC, inhibits patient engagement, and reflects the paradoxes of inadvertently excluding patients' needs from hospital practice. The hospital gown must be modified to protect the patient's voice and enhance engagement. Policymakers are called to apply design thinking to facilitate patient participation in decision-making to accord hospital clothing to PCC and improve healthcare delivery.
1 Introduction
Patient-centered care (PCC) is the preferred policy for delivery of care (1–6). PCC is care that fundamentally responds to individual patient preferences, wishes, needs, and values, ensuring that patient values direct decisions (7). This policy was proven to reduce costs while improving clinical outcomes, patient experiences, and provider experiences (1–4). Delivery of the PCC policy stresses the patient–provider relationship and aims at optimizing the use of information that patients provide to achieve the outcomes that are most important to patients (1–8). As health systems move toward value-based care, PCC becomes foundational to delivering high-quality care, especially because it is fully consistent with population health management, which improves the health of the whole population (9, 10). Therefore, implementing PCC is a high priority for hospitals, but hospitals are far from achieving PCC (11, 12). Acknowledged barriers to achieving PCC are lack of knowledge on integrating PCC into practice, deficient skills of physicians, and professional burnout (13–15). This study focuses on the patient gown within PCC as an additional barrier to PCC, calling for design thinking to remove this barrier.
The PCC policy intentionally directs patients to play a central and active role as meaningfully engaged and responsible for their health (16, 17). Patients move along a continuum from passive to active engagement (18–22). An acceptable definition of patient engagement focuses on the relationship between patients and providers as they work together, during and beyond the care experience, to promote and support active patient involvement in healthcare, strengthening their influence on decisions, at both the individual and collective levels (23–25). To be engaged, patients need to become active in obtaining knowledge and acquiring skills and confidence for managing their illness (26). Patient engagement can occur in direct care, organizational design, and policymaking, influencing patients' capacity to be engaged, leading to improved quality of care, better outcomes, and greater cost efficiency (23). Patient engagement ranges along a continuum characterized by the amount of information that flows between patient and provider, the extent to which the patient adopts an active role in decisions, and the extent to which patient organizations influence decisions of healthcare organizations and policies cultivating engagement (23). Thus, patient engagement refers to the cognitive and emotional conditions that patients express through observable behaviors of the authentic self (27).
At the patient–provider level, every interaction may foster patient engagement that, in turn, can facilitate patient trust, resulting in higher medication adherence, fewer readmissions, and self-management of illness (22, 28). Many stakeholders are therefore interested in patient engagement in capturing the patient's voice and incorporating it into practice (29, 30). PCC differs from patient engagement, conveying a vision of healthcare as a partnership between providers and patients, who become active, informed, and influential, to ensure that decisions respect the preferences, needs, and beliefs of patients (31, 32).
Physicians are encouraged to facilitate PCC when interacting with patients by helping them become knowledgeable regarding their illnesses, express their expectations, and share decision-making (33–35). Physicians, however, identified patient reluctance to be engaged as a barrier to achieving PCC (33, 34). PCC encourages patients to ask questions, share their anxiety, take on an assertive approach to reciprocal communication, and share their health-related concerns when interacting with physicians (15, 36, 37). Communication of patients, however, may be affected by the hospital-issued gown, which is an integral component of the hospital environment across countries (30, 38, 39).
Hospital gowns are routinely worn by hospitalized patients as a form of standardized attire in hospitals in the U.S., Canada, China, the Middle East, Italy, Hungary, and the UK (40–43). The hospital gown provides benefits to all stakeholders (44–46). For patients, the gown provides an accessible clothing option during their hospitalization that can be easily changed in the event of incontinence, bleeding, etc. Gowns are meant to be functional, non-constricting, and provide patients with an effortless experience (47). For clinicians, the gown allows easy care for patients who are sedated, unconscious, in surgical or intensive care settings, weak, or with mobility difficulties (47). For hospitals, gowns are an easy, one-size-fits-all, cheap, versatile, easily washed, and re-used attire (47). In the past decade, tremendous efforts were invested in developing tools to assess patient engagement and indicators of PCC, but insights from the patients, as primary stakeholders, regarding the hospital gown and its effect on their capacity for engagement are insufficient (1, 9, 48–50).
The gown is a symbol of the passage into a new role as a patient, carrying low status due to worn-out clothing, lacking privacy, and constructing the social identity of hospitalized patients (38, 51–54). A handful of qualitative studies found that the hospital gown can be perceived as dehumanizing, as the gown was associated with lower wellbeing of inpatients due to an increased sense of vulnerability, feeling more exposed, self-conscious, uncomfortable, cold, embarrassed, disempowered, and because the gown limited patients from being active (55–59).
Thus, although PCC stipulates a two-sided, mutually involved communication and calls for patients to be engaged, the patient's hospital gown may affect cognition and emotions, inhibit self-expression, and negatively impact patient engagement when interacting with physicians. Research on the cognitive–emotional effect of the gown on patient engagement within the PCC framework is scant (60). The importance of patient engagement when wearing the hospital gown calls for revisiting the issue of patient attire during hospitalizations. Self-expression while wearing the gown may also be affected by the locus of control (LOC).
LOC is the most frequently studied perception in healthcare (58). The social learning theory classifies people along a continuum of perceived control ranging from internal locus of control (ILOC) to external locus of control (ELOC) (59). People with an ILOC believe that success or failure is due to their own efforts and consequently take self-directed actions, while people with an ELOC believe that their achievements are directed by luck, chance, or others (60). Traditionally, ILOC reflected personal mastery and referred to the assumed internal states of individuals who seek information, have higher alertness, and make decisions (59). People with ILOC actively and willingly rely on internal resources to deal with difficult circumstances (61).
A study on patients' trust in physicians extended the concept of ILOC beyond personal attributes to one's perceived ability to resolve health-related problems and to interact more effectively with physicians (62). While patients with ILOC were proactive and took responsibility for improving their health, patients with ELOC believed that they could influence their health or recovery, and they depended on chance, externality, and physicians. Patients with high ILOC were more active in interactions with physicians and used efficient problem-focused coping strategies (55). Hospitalized patients with ILOC were able to make more effective decisions, had higher self-efficacy, and took care of themselves (63). A significant positive relationship was found between ILOC and high adjustment to situations linking ILOC to better healing (64–67). The association between the gown and LOC is understudied (39, 55). What is the association between wearing the hospital gown and the LOC of patients? Is the gown a potential barrier to achieving PCC?
Patients' sense of self is defined through interactions with others (68). Patients may adjust their engagement behaviors with physicians, based on perceived role relations, relative power, and status (69). The patient's inner world underlies interactions either orienting the patient toward engagement or away from it in interactions with physicians (70). We explored the cognitive–emotional effect of the gown on patients and its association with their capacity to be engaged when wearing the hospital gown. Much has been written about the symbolic function of the whitecoat, but the patient gown has not received similar attention (39). From a PCC perspective, it is essential to understand the association of the gown with the patient's emotions and LOC, which may shape self-expression and patient engagement during hospitalizations. The research question was “how is the patient gown in hospitalizations associated with the emotions and the LOC of patients?”
Since the patient's gown is a symbolic embodiment of the “sick” role, namely, relinquishing control to clinicians and experiencing emotional vulnerability (71, 72), we expected that the emotions of patients when wearing the gown might be related to LOC forming an inclination to proactively communicate with physicians during hospitalizations. A previous study found that female patients felt more exposed, self-conscious, vulnerable, uncomfortable, cold, embarrassed, and disempowered when wearing the gown compared to male patients and patients with a short illness (73). We, therefore, expected that the negative emotions of patients when wearing the gown would be related to higher ELOC in chronically ill patients and female patients. Furthermore, we expected that compared to male patients, female patients might have stronger negative emotions when wearing the gown and stronger associations with ELOC. Finally, we expected that compared to male patients with a short illness, chronically ill female patients would have stronger negative emotions when wearing the gown, which would be associated with ELOC.
The few studies that were performed on the patient gown were qualitative. This is a quantitative study testing the association between the gown and the LOC of hospitalized patients.
2 Methods
2.1 Ethical approval and sample size
The ethics board of the academic institution with which the first author is affiliated granted ethical approval (IRB# 117). “G*Power (v. 3.1.9.7) statistical software was utilized to determine the minimal sample size for the analyses using a standard α error probability of 5%, a power of 95%, and a fixed effect size of 0.15 for a ratio of 5:1 (predictors: outcomes); the minimal a-priori sample size is n = 138 (and n = 204 for an effect size of 0.10). Based on these a-priori analyses, a sample size above 204 (as the stricter upper bound) is considered adequate for the subsequent analysis. The sample consisted of 1,008 Israeli participants who were hospitalized in the 6 months in tertiary public hospitals.
2.2 Procedure
Following ethical approval, this cross-sectional research was carried out through the academic research laboratory using a digital questionnaire. A digital questionnaire was created. Students pursuing a bachelor's degree in health management, who have studied quantitative and qualitative methods, identified a relative or acquaintance who was hospitalized in the last 6 months. Each student screened the participant for the department in which she or he was hospitalized, omitting new mothers from maternity wards and people who were hospitalized and discharged from the emergency department.
Students explained the study goals, and once participants agreed, students sent them the digital link to the questionnaire. The purpose of the research was to learn about the inpatient experience when wearing a gown. Participants marked a box in the introduction part of the questionnaire for their consent for participation and publication. Older participants who were not averse to technology had the questionnaire read to them. The average time to fill out the questionnaire was 10 min. From July 2022 to July 2023, 1,008 questionnaires were completed under the supervision of the second author.”
2.3 Measures
To assess Patients' feelings when wearing a hospital gown, the Cogan et al. (44), a 34-item questionnaire was used. An example item is “I feel vulnerable when wearing the gown” (α = 0.67).
To assess Perception of the gown, the Frankel et al. (74) six-item questionnaire was used. An example item was “I was able to move about easily when walking and while in bed” (α = 0.92).
To assess the locus of control, the 10-item brief questionnaire was used (75). An example item is: “My quality of life is affected by others” (α = 0.70).
Demographic control variables were age, gender, education, family status, religious affiliation, religiousness, ethnicity, number of children, occupational status, and household income.
Health control variables were hospitalization frequency, type of illness, and department in which the patient was hospitalized.
3 Results
3.1 Descriptive statistics
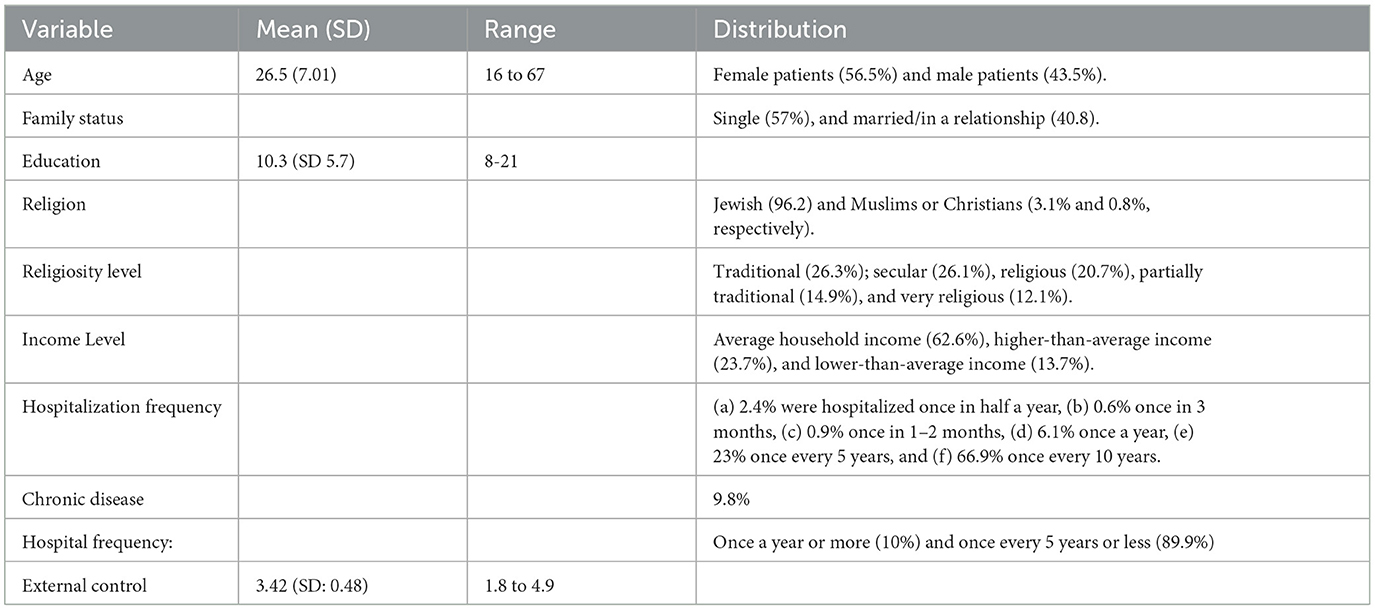
After deleting missing data, this study included 956 inpatients, with a mean age of 26.5 years (SD: 7.01), ranging from 16 to 67 years, of which 56.5% were women and 46.5% were men. Most of the patients reported being single (57%), and 40.8% stated that they were married or in a relationship. The average completed school years was 10.3 (SD: 5.7), ranging from 8 complete school years to 21 years. The majority of the patients were identified as Jewish (96.2), and the rest were either Muslims or Christians (3.1% and 0.8%, respectively).
Most patients self-identified as traditional (26.3%), followed by secular (26.1%), religious (20.7%), partially traditional (14.9%), and very religious (12.1%). Most patients reported an average household income (62.6%), 23.7% reported a higher-than-average income, and 13.7% reported a lower-than-average income.
The distribution of the hospitalization frequency was as follows: (a) 2.4% were hospitalized once in half a year; (b) 0.6% once in 3 months; (c) 0.9% once in 1–2 months; (d) 6.1% once a year; (e) 23% once every 5 years; and (f) 66.9% once every 10 years. Most of the respondents (90.2%) did not have any prolonged or chronic disease, while only 9.8% reported they did. Approximately 10% of the patients reported being hospitalized once a year or more, and 89.9% reported a hospitalization once every 5 years or less. ELOC average was 3.42 (SD: 0.48), ranging from 1.8 to 4.9. Perceptions of the gown average was 2.7 (SD 0.64), ranging from 1 to 5. Table 1 presents the sample demographic distribution.
3.2 Pearson correlation tests and independent T-tests
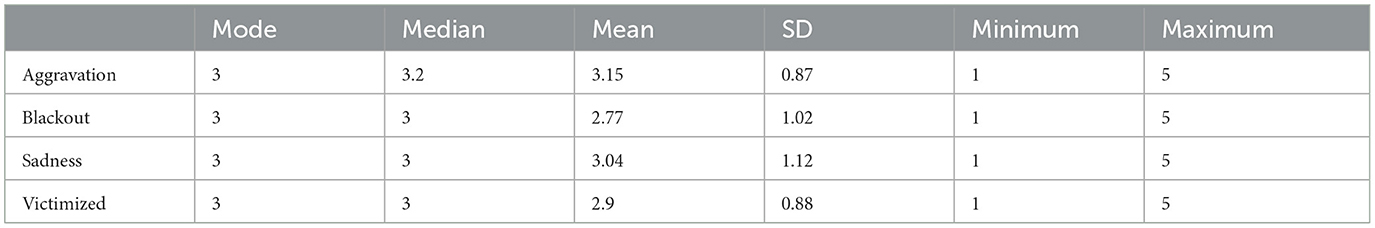
The Pearson correlation tests were performed to test the relationships between negative emotions when wearing the gown and ELOC. Negative significant correlations were found between each emotion and ELOC including aggravation (r = −0.16, p < 0.001), alienation (r= −0.16, p < 0.001.16), sadness (r = −0.15, p < 0.001), and victimization (r = −0.16, p < 0.001). Table 2 presents the emotional central tendencies and their distributions.
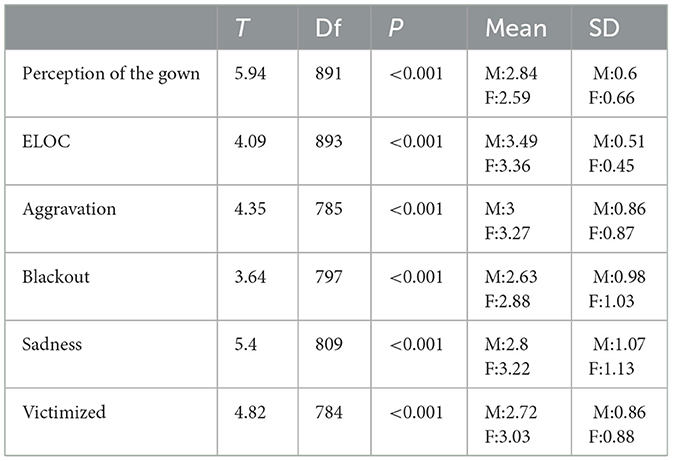
Independent T-tests were performed to compare male patients and female patients on their perceptions of the gown, negative feelings, and ELOC. Significant differences were found between male patients and female patients. Compared to male participants, the mean score of perceptions of the gown was lower in female participants, as was the mean score of ELOC, while the mean score of all negative emotions was higher for female participants. Table 3 presents the t-test results.
Next, the perceptions of the gown. The positive perceptions of the gown were rated low to medium on a scale from 1 to 5. “I am able to move better when wearing the gown” (M = 1.95, SD = 0.98); “It is easy to wear the gown” (M = 2.14, SD = 1.12); “I feel protected when wearing the gown” (M = 2.48, SD = 1.25); I feel comfortable when wearing the gown” (M = 2.50, SD = 1.27). Negative emotions when wearing the gown and ELOC were compared among male participants and female participants, and significant differences were found. Perceptions of the gown and ELOC were higher in male participants, while all negative emotions were higher in female participants. Finally, participants with chronic illnesses were compared with participants with short-term illnesses. In participants with a chronic illness, ELOC was not significantly different. The perceptions of the gown were significantly higher in male participants, yet all negative emotions were significantly higher in female participants, as presented in Table 4 by gender and type of illness.
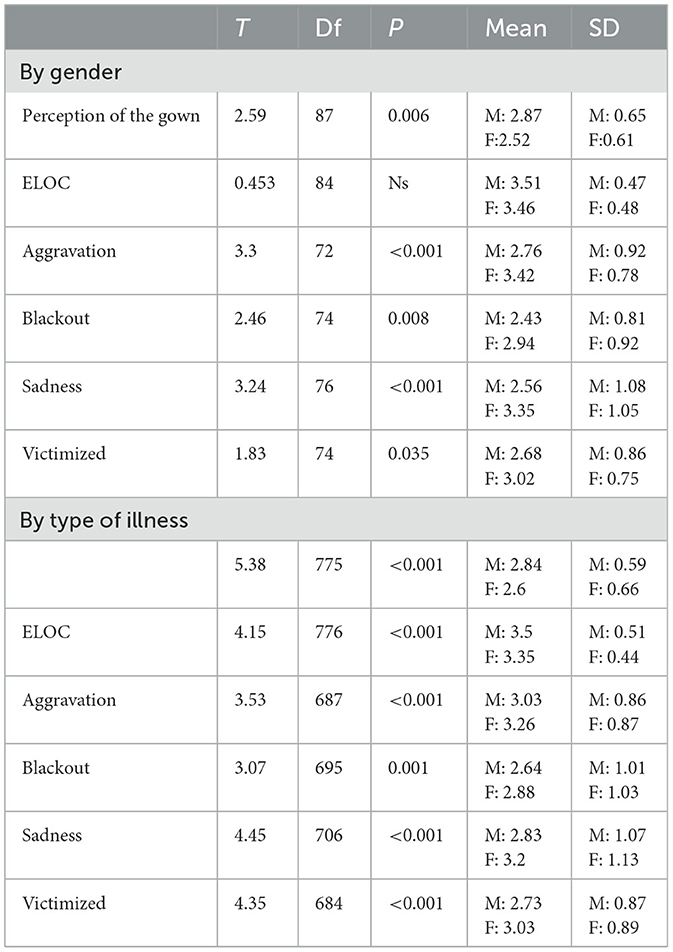
Table 4. Independent t-tests comparing perceptions of the gown, negative emotions, and ELOC by gender and type of illness.
4 Discussion
Failing to meet patient preferences to be engaged was significantly associated with dissatisfaction, distrust, and reduced capacity for self-management of illness post-discharge (29, 76). The gown was associated with a lack of control and increased distress and was negatively associated with ILOC, which comprised proactiveness, learning, and taking responsibility (62). The findings support a previous study in which the patient gown caused psychological distress, disempowerment, and lower self-esteem, as well as deepened the intense vulnerability of hospitalized patients (77, 78). The self-concept of the patient was lacking control when adhering to the standard of wearing a gown upon hospitalization, thereby impeding patient engagement and PCC achievement.
Our findings suggested that the gown failed to meet the needs of patients and was negatively associated with ILOC, which was essential for active patient engagement, effective communication with clinicians, and disease management (17–21, 62, 79).
The gown was associated with sadness, alienation, and victimization, all of which were inconsistent with PCC (80, 81). Looking at the patient's inner world as underlying communication with physicians, the cognitive–emotional experience of wearing the gown may diverge patients from engaging with physicians (82). The findings indicated that the patient's experience with the gown was related to ELOC, inhibiting engagement (62, 64, 67). The gown seems to be paramount to a patient's dignity in hospitalizations and may shape an overall negative hospital experience (46). Negative hospital experiences of patients due to hospital culture, work environment, and providers' deficient capacity to provide PCC contributed to provider dissatisfaction and burnout (83). Therefore, addressing patient experiences may have the double benefit of improving patient care and reducing provider burnout.
Although achieving PCC is a primary goal, patient needs and emotions are not incorporated into the co-design of clothing in hospitalizations, which is solely controlled by policymakers and hospitals. Thus, while the PCC policy and medical practice advocate PCC calling for respect, privacy, and dignity as fundamental cornerstones in the care of each individual patient, when patients remove their own clothes and wear hospital gowns, their self-expression as individuals is diminished (3). In addition to the physical vulnerability that requires hospitalization, the negative emotional effect of the gown on LOC is an additional barrier to PCC, strengthening ELOC and weakening the patient as an engaged partner in the communication rather than empowering the patient as an engaged partner.
The acceptance of the backless hospital gown when advocating PCC is a clash that should challenge current policies and practices and encourage new moral thinking and new policies relating to hospital clothing to improve the emotional experience of hospitalized patients and promote engagement and PCC. Policymakers and hospital management must evaluate the messages emerging from the requirement to wear the gown vis-à-vis the importance of implementing PCC as a primary goal (70). The patient gown may represent the lower end of the engagement continuum, where the flow of information is in one direction, and patients have limited power for decision-making. At the lower end, organizations and policymakers define their own agendas, and information flows bi-directionally and then back to the system (23).
A second clash is between the declarations of hospitals that patients should openly ask questions and the policy of forcing patients to wear gowns. This gown requirement conveys inequality and distance, diminishing individuality, impeding engagement, and inhibiting the primary goal of PCC. A third clash relates to the patient–physician relationship, which is essential for PCC (8). This relationship has been critically viewed as asymmetrical in power, inhibiting patient engagement (84). Physicians have the knowledge, enable treatment, possess control over how decisions and what decisions are made, and may use a range of strategies to shape interactions with patients (85). The whitecoat of the physician vs. the degrading gown of the patient may manifest an additional asymmetry that, although common, raises ethical concerns about how the patients are treated as engaged partners. Patients acknowledge the gowns as a “necessary evil”, but it is a medical myth persisting through tradition and serving as a mechanism for anonymity rather than for PCC promotion (55, 86). Figure 1 presents the three clashes between PCC and the patient gown.
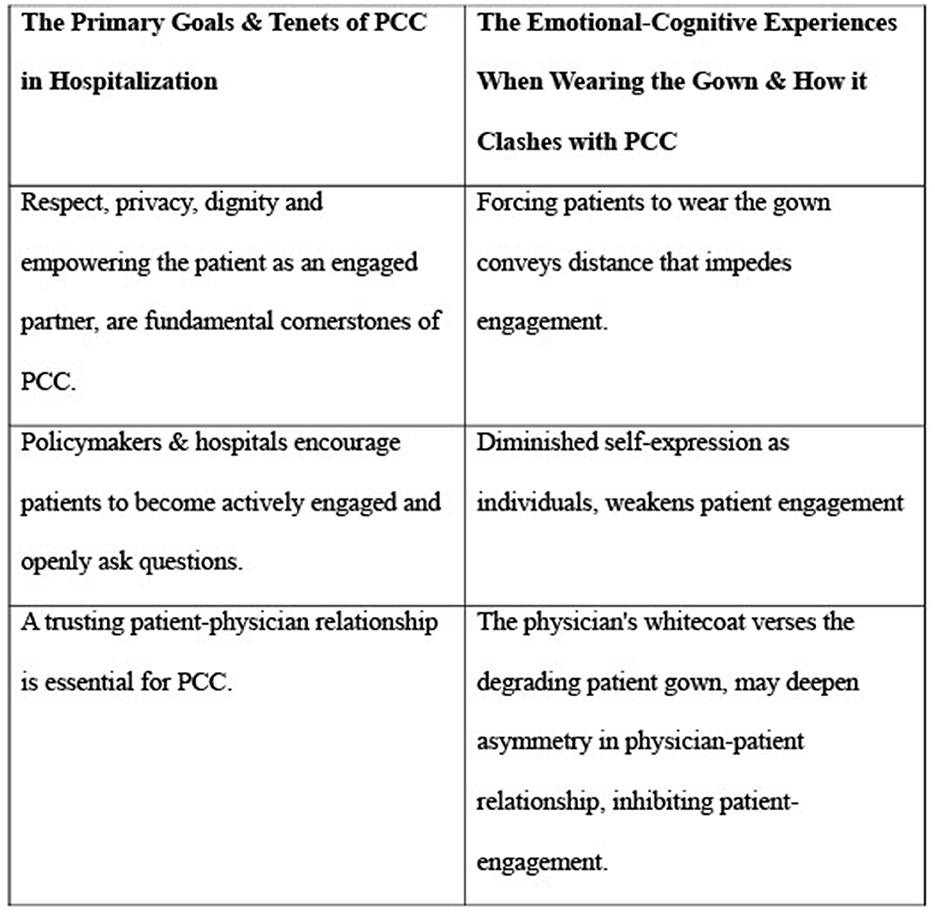
Figure 1. Misalignment of the hospital-issued patient gown with patient-centered care. Clashes between the primary goals and Tenets of PCC in Hospitalization and the emotional-cognitive experiences when wearing gowns.
While backless gowns, held together with ties at the back, are needed for initial pre-operative and post-operative care of the patient, in the recuperation phase of the hospitalization, the gown impedes PCC. The above three clashes between the primary goal commonly framed to meet patients' needs and the secondary goal of operative care fail to guard against medical paternalism (87, 88). Indeed, there may be tension in hospitals between operative care and PCC delivery, but high-performing hospitals are expected to exhibit an organizational culture of patient empowerment, meeting patient expectations and fostering multidirectional communication that facilitates engagement and PCC (6).
While previous research explained deficient PCC by lack of skills and called for better training for physicians, it is time to raise more fundamental questions regarding the values that are encompassed in the PCC concept (e.g., patient autonomy, engagement, and perceived control) (9, 21). The insights of this study call upon policymakers and hospital managements to not only declare their aspiration to achieve PCC but also to manage the messages that are incorporated in the requirement to wear the gown, consider its meaning within the structure of power, and effectively manage the primary goal of PCC achievement.
Policies that inadvertently exclude patient emotional needs from core practices must be modified to protect the patient's voice, enhance patient engagement, and promote PCC (89). Since the inclusion of the patient voice falls short on hospitalizations in general and specifically, on the emotional–cognitive experience of patients when wearing the gown, policymakers are called upon to redesign the clothing of inpatients. In fact, it is long overdue to challenge the status quo of the open-backed gown, focus on the emotional needs of hospitalized patients, and enhance patient engagement as a partner. The gown should be limited to operative medical necessities, enabling patients to change into clothing they prefer, as soon as possible, to preserve their self-worth and ILOC (29, 90).
To challenge the status quo of the gown requirement and align patient hospitalization clothing with PCC, policymakers are called upon to apply design thinking by conducting meetings to assess what patients, clinicians, healthcare leaders, and policymakers perceive as attire that promotes ILOC and patient engagement and may better translate PCC into healthcare practice (91). Design thinking is a human-centered methodology proposed as a systematic approach to innovation in healthcare through the active participation of patients (92). Design thinking prioritizes patient desires and needs, which implements PCC, resulting in a better understanding of the problem and developing effective solutions (91). Using design thinking to implement an effective change in hospital clothing requires patient participation in the process, not only for input but also as an equitable participant in the decision-making processes on clothing and related work processes (92).
Co-design of the gown may promote engagement at the end of the continuum of high engagement. Patients may be more active partners. Information may flow bi-directionally; patients may communicate with clinicians about their health situation, understand the risks and benefits of treatment options, ask questions, share beliefs and preferences, and decision-making responsibility may be shared, as called for by the PCC strategy (23). At the policymaking level, engagement may focus on developing, implementing, and evaluating national, state, and local healthcare policies. Patients may engage in shaping policies to ensure that they are responsive to the perspectives and needs of patients (23). More active patients may influence clinicians in giving patients timely, complete, and understandable information; elicit patients' values, beliefs, and risk tolerance regarding care choices, and encourage patients to be engaged according to the patient's wishes (93). Patients can propose novel ideas that will create value for all stakeholders, promote engagement, and identify a range of priorities to better achieve PCC in hospitalizations (89).
This novel study is not without limitations. Cultural attributes of inpatients and clinicians, the convenient rather than non-representative sample of hospitalized patients, and the demographic composition of the sample, with only 3.1% Muslims who comprise 22% of the population, and only 0.8% Christians who comprise 4% of the population, limit the generalization of the study. Future studies may replicate this study in diverse populations of hospitalized patients with a larger sample and also test potential differences in experiences for patients wearing a cotton (reusable) gown vs. a polypropylene (disposable) hospital gown.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Board of Achva Academic College #117. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
GG: Methodology, Formal analysis, Writing – review & editing, Writing – original draft, Conceptualization. HO: Methodology, Formal analysis, Data curation, Writing – review & editing, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Diaby V, Ali AA, Montero AJ. Value assessment frameworks in the United States: a call for patient-engagement. Pharmacoecon Open. (2019) 3:1–3. doi: 10.1007/s41669-018-0094-z
2. Fagotto E, Burgués VA, Fung A. A taxonomy to engage patients: objectives, design, and patient activation. NEJM Catalyst. (2019) 5:4.
3. Fix GM, VanDeusen Lukas C, Bolton RE, Hill JN, Mueller N, LaVela SL, et al. Patient-centered care is a way of doing things: how healthcare employees conceptualiz e patient-centered care. Health Expect. (2018) 21:300–7. doi: 10.1111/hex.12615
4. Venhuizen G. Can patient centered care plus shared decision making equal lower costs? BMJ. (2019) 15:367. doi: 10.1136/bmj.l5900
5. Jarrar MT, Al-Bsheish M, Aldhmadi BK, Albaker W, Meri A, Dauwed M, Minai MS. Effect of practice environment on nurse reported quality and patient safety: the mediation role of person-centeredness. Healthcare. (2021) 9:1578. doi: 10.3390/healthcare9111578
6. Engle RL, Mohr DC, Holmes SK, Seibert MN, Afable M, Leyson J, et al. Evidence-based practice and patient-centered care: doing both well. Health Care Manage Rev. (2021) 46:174. doi: 10.1097/HMR.0000000000000254
7. Wolfe A. Institute of Medicine report: crossing the quality chasm: a new health care system for the 21st century. Policy, Polit Nurs Pract. (2001) 2:233–5. doi: 10.1177/152715440100200312
8. Nundy S, Oswald J. Relationship-centered care: a new paradigm for population health management. Healthcare. (2014) 2:216–219. doi: 10.1016/j.hjdsi.2014.09.003
9. National Health Council. The National Health Council Rubric to Capture the Patient Voice: a Guide to Incorporating the Patient Voice into the Health Ecosystem. (2019). Available at: https://nationalhealthcouncil.org/wp-content/uploads/2019/12/NHC_Patient_Engagement_Rubric.pdf (accessed August 18, 2023).
10. Iyamu I, Plottel L, Snow ME, Zhang W, Havaei F, Puyat J, et al. Culture change in long-term care-post COVID-19: adapting to a new reality using established ideas and systems. Can J Aging. (2023) 42:351–8. doi: 10.1017/S0714980822000344
11. Tieu M, Matthews S. The relational care framework: promoting continuity or maintenance of selfhood in person-centered care. J Med Philos. (2024) 49:85–101. doi: 10.1093/jmp/jhad044
12. Tomaselli G, Buttigieg SC, Rosano A, Cassar M, Grima G. Person-centered care from a relational ethics perspective for the delivery of high quality and safe healthcare: a scoping review. Front Public Health. (2020) 8:44. doi: 10.3389/fpubh.2020.00044
13. Gabay G, Netzer D, Elhayany A. Shared trust of resident physicians in top-management and professional burnout: a cross-sectional study towards capacity for patient-focused care, peer support and job expectations. Int J Health Plann Manage. (2022) 37:2395–409. doi: 10.1002/hpm.3479
14. Luxford K, Safran DG, Delbanco T. Promoting patient-centered care: a qualitative study of facilitators and barriers in healthcare organizations with a reputation for improving the patient experience. Int J Qual Health Care. (2011) 23:510–5. doi: 10.1093/intqhc/mzr024
15. National Health Council. Glossary of Patient-Engagement Terms. (2019). Available at: https://nationalhealthcouncil.org/glossary-of-patient-engagement-terms/ (accessed August, 2023).
16. Biddle MSY, Gibson A, Evans D. Attitudes and approaches to patient and public involvement across Europe: a systematic review. Health Soc Care Community. (2021) 29:18–27. doi: 10.1111/hsc.13111
17. Locatelli SM, Hill JN, Bokhour BG, Krejci L, Fix GM, Mueller N, et al. Provider perspectives on and experiences with engagement of patients and families in implementing patient-centered care. Healthcare. (2015) 3:209–14. doi: 10.1016/j.hjdsi.2015.04.005
18. Hemphill R, Forsythe LP, Heckert AL, Amolegbe A, Maurer M, Carman KL, et al. What motivates patients and caregivers to engage in health research and how engagement affects their lives: qualitative survey findings. Health Expect. (2020) 23:328–36. doi: 10.1111/hex.12979
19. Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N, et al. Patient-engagement in research: a systematic review. BMC Health Serv Res. (2014) 14:89. doi: 10.1186/1472-6963-14-89
20. Shippee ND, Domecq Garces JP, Prutsky Lopez GJ, Wang Z, Elraiyah TA, Nabhan M, et al. Patient and service user engagement in research: a systematic review and synthesized framework. Health Expect. (2015) 18:1151–66. doi: 10.1111/hex.12090
21. Kelders SM, van Zyl LE, Ludden GDS. The concept and components of engagement in different domains applied to eHealth: a systematic scoping review. Front Psychol. (2020) 11:926. doi: 10.3389/fpsyg.2020.00926
22. Kahn WA. Psychological conditions of personal engagement and disengagement at work. Acad Manag J. (1990) 33:692–724. doi: 10.5465/256287
23. Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Affairs. (2013) 32:223–31. doi: 10.1377/hlthaff.2012.1133
25. Institute of Medicine. Engaging patients to improve science and value in a learning health system, Ch. 4 in: Institute of Medicine. In: Patients Charting the Course: Citizen Engagement in the Learning Health System: Workshop Summary. Washington DC: National Academies Press (2011). p. 103–110.
26. Hibbard JH, Mahoney E. Toward a theory of patient and consumer activation. Patient Educ Couns. (2010) 78:377–81. doi: 10.1016/j.pec.2009.12.015
27. Gabay G. Patient self-worth and communication barriers to Trust of Israeli Patients in acute-care physicians at public general hospitals. Qual Health Res. (2019) 29:1954–66. doi: 10.1177/1049732319844999
28. Harter JK, Schmidt FL, Hayes TL. Business-unit-level relationship between employee satisfaction, employee engagement, and business outcomes: a meta-analysis. J Appl Psychol. (2002) 87:268. doi: 10.1037//0021-9010.87.2.268
29. National Institute for Health and Care Excellence. Patient and Public Involvement Policy. (2013). Available at: https://www.nice.org.uk/media/default/About/NICE-Communities/Public-involvement/Patient-and-public-involvement-policy/Patient-and-public-involvement-policy-November-2013.pdf (accessed August 8, 2023).
30. Perfetto EM, Oehrlein EM, Love TR, Schoch S, Kennedy A, Bright J. Patient-centered core impact sets: what they are and why we need them. Patient-Pati-Cent Outcom Res. (2022) 15:619–27. doi: 10.1007/s40271-022-00583-x
31. Institute of Medicine. Envisioning the National Health Care Quality Report. Washington, DC: National Academies Press (2001).
32. Epstein, R., Street, R. Patient-Centered Care for the 21st Century: Physicians' Roles, Health Systems and Patients' Preferences. Philadelphia, PA: ABIM Foundation (2008).
33. Schuttner L, Hockett Sherlock S, Simons CE, Johnson NL, Wirtz E, Ralston JD, et al. My goals are not their goals: barriers and facilitators to delivery of patient-centered care for patients with multimorbidity. J Gen Intern Med. (2022) 37:4189–96. doi: 10.1007/s11606-022-07533-1
34. Charosaei F, Rostami S, Esmaeili M, Molavynejad S, Vanaki Z. Effective strategies for implementing patient-centered care in cardiac care unit: an opportunity for change. J Educ Health Promot. (2021) 10:20. doi: 10.4103/jehp.jehp_1662_20
35. Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. (2013) 70:351–79. doi: 10.1177/1077558712465774
36. Kuluski K, Peckham A, Williams AP, Upshur RE. What gets in the way of person-centered care for people with multimorbidity? Lessons from Ontario, Canada. Healthc Q. (2016) 19:17–23. doi: 10.12927/hcq.2016.24694
37. Miller L. Race, Gender and Health Literacy in the Medical Encounter: a Test of Cultural Health Capital and Status Characteristics Theory. (2016). Available at: https://shareok.org/handle/11244/34583
38. Topo P, Iltanen-Tähkävuori S. Scripting patient hood with patient clothing. Soc Sci Med. (2010) 70:1682–9. doi: 10.1016/j.socscimed.2010.01.050
39. Wellbery C, Chan M. Whitecoat, patient gown. Med Humanit. (2014) 40:90–6. doi: 10.1136/medhum-2013-010463
40. Holder H. The Older Adult Inpatient Experience and the Hospital Gown (Doctoral dissertation). Case Western Reserve University, Cleveland, OH, United States. (2022).
41. Lorts A. Hospital Gowns in the Health Care System: a Study Exploring Whether the Hospital Gown Preserves a Patient's Dignity, Modesty, and Comfort (Doctoral dissertation). University of Missouri—Columbia, Columbia, MO, United States. (2022).
42. Vaskooi-Eshkevari K, Mirbazegh F, Soltani-Kermanshahi M, Sabzali-Poursarab-Saeedi M, Alipour S. Customized patient clothing and patient satisfaction. Int J Health Care Qual Assur. 32:635–44. doi: 10.1108/IJHCQA-02-2018-0047
43. Zhao Y, Zhou F, Zhao Y, Zou Y, Wei X. Development of an emotional response model for hospital gown design using structural equation modeling. AUTEX Res J. (2024) 24:20230010. doi: 10.1515/aut-2023-0010
44. Cogan N. Exploring the effect of the hospital gown on wellbeing: a mixed methods study. Lancet. (2019) 394:32. doi: 10.1016/S0140-6736(19)32829-6
45. Lucas, C. Don't let the gown get you down: how patients and physicians perceive hospital gowns. J Hosp Med. (2019). Available at: https://www.the-hospitalist.org/hospitalist/article/225598/mixed-topics/exposing-hospital-gowns
46. Rabin, J. Compassionate coverage: a patient access linen system. J Patient Exp. (2019) 6:185–93. doi: 10.1177/2374373518793411
47. Arunachalam P, D'Souza B. Patient-centered hospital gowns: a novel redesign of inpatient attire to improve both the patient and provider experience. Front Biomed Devi. (2022) 84815:V001T04A008. doi: 10.1115/DMD2022-1058
48. Innovation and Value Initiative. IVI Methods Summit: Defining Needs and Progress Toward Improving Methods in Value Assessment: Convening Proceedings Report. (2022). Available at: https://www.thevalueinitiative.org/wp-content/uploads/2020/05/Methods-Summit-Report_FINAL_Digital.pdf (accessed August 17, 2023).
49. Linthicum MT, dosReis S, Slejko JF, Mattingly TJ, Bright JL. The importance of collaboration in pursuit of patient-centered value assessment. Patient. (2021) 14:381–4. doi: 10.1007/s40271-020-00446-3
50. Walton MK, Powers JH III, Hobart J, Patrick D, Marquis P, Vamvakas S, et al. Clinical outcome assessments: conceptual foundation: report of the ISPOR clinical outcomes assessment: emerging good practices for Outcomes Research Task Force. Value Health. (2015) 18:741–52. doi: 10.1016/j.jval.2015.08.006
51. McNeill LS. Fashion and women's self-concept: a typology for self-fashioning using clothing. J Fash Market Manage. (2018) 22:82–98. doi: 10.1108/JFMM-09-2016-0077
52. Crutzen C, Adam S. “What if it's not just an item of clothing?”–a narrative review and synthesis of the whitecoat in the context of aged care. Psychologica Belgica. (2022) 62:62. doi: 10.5334/pb.1138
53. Houchens N, Saint S, Petrilli C, Kuhn L, Ratz D, De Lott L, et al. International patient preferences for physician attire: results from cross-sectional studies in four countries across three continents. BMJ Open. (2022) 12:e061092. doi: 10.1136/bmjopen-2022-061092
54. Morton L, Cogan N, Georgiadis E. 'Why Does it Have to be Open at the Back?' The Impact of the Hospital Gown on Recovery and Wellbeing. (2019).
55. Lucas CM, Dellasega C. Finding common threads: how patients, physicians and nurses perceive the patient gown. Patient Exp J. (2020) 7:51–64. doi: 10.35680/2372-0247.1387
56. Punchihewa C. The Impact of The Hospital Gown on Patient Experiences of Dehumanisation: A Randomised Trial (Doctoral dissertation). Auckland: ResearchSpace@ Auckland.
57. Syed S, Stilwell P, Chevrier J, Adair C, Markle G, Rockwood K. Comprehensive design considerations for a new hospital gown: a patient-oriented qualitative study. Can Med Assoc Open Access J. (2022) 10:E1079–87. doi: 10.9778/cmajo.20210271
58. McAlister AL, Perry CL, Parcel GS. How individuals, environments, and health behaviors interact. Health Behavior. (2008) 169:169–88.
59. Rotter JB. Some problems and misconceptions related to the construct of internal versus external control of reinforcement. J Consult Clin Psychol. (1975) 43:56. doi: 10.1037/h0076301
60. Anderson C, Turner AC, Heath RD, Payne CM. On the meaning of grit… and hope… and fate control… and alienation… and locus of control… and… self-efficacy… and… effort optimism… and…. Urban Rev. (2016) 48:198–219. doi: 10.1007/s11256-016-0351-3
61. Zimmerman BJ. Self-efficacy: an essential motive to learn. Contemp Educ Psychol. (2000) 25:82–91. doi: 10.1006/ceps.1999.1016
62. Gabay G. Perceived control over health, communication and patient–physician trust. Patient Educ Couns. (2015) 98:1550–7. doi: 10.1016/j.pec.2015.06.019
63. Miličić D, Brajković L, Ljubas Maček J, Andrić A, Ardalić Ž, Buratović T, et al. Type a personality, stress, anxiety and health locus of control in patients with acute myocardial infarction. Psychiatr Danub. (2016) 28:409–14.
64. Moradi Y, Al Shara SA, Namadi F, Mollazadeh F. The relationship between health locus of control and self-efficacy in patients with heart failure. Nurs Midwif Stud. (2022) 11:31–6. doi: 10.4103/nms.nms_75_21
65. Bjørkløf GH, Engedal K, Selbæk G, Maia DB, Coutinho ES, Helvik AS. Locus of control and coping strategies in older persons with and without depression. Aging Ment Health. (2016) 20:831–9. doi: 10.1080/13607863.2015.1040722
66. Kesavayuth D, Poyago-Theotoky J, Zikos V. Locus of control, health and healthcare utilization. Econ Model. (2020) 86:227–38. doi: 10.1016/j.econmod.2019.06.014
67. Mikaeili N, Einy S, Taghavy R. Role of coping styles, locus of control, and emotional intelligence in predicting social adjustment of veterans with post-traumatic stress disorder. Iran J War Public Health. (2018) 10:195–201. doi: 10.29252/ijwph.10.4.195
68. Dillard JP, Segrin C, Harden JM. Primary and secondary goals in the production of interpersonal influence messages. Commun Monographs. (1989) 56:19–38. doi: 10.1080/03637758909390247
69. Dillard, JP. A goal-driven model of interpersonal influence. In:Dillard JP, , editor. Seeking Compliance: The Production of Interpersonal Influence Messages. Scottsdale, AZ: Gorsuch Scarisbrick (1990) p. 41–56.
70. Dillard JP, Baxter L, Braithwaite DO. Goals-plans-action theory of message production. In: Engaging Theories in Interpersonal Communication: Multiple Perspectives. Thousand Oaks, CA (2008) p. 65–76. doi: 10.4135/9781483329529.n5
71. Soliz J, Colaner CW. Communication accommodation theory and communication theory of identity: theories of communication and identity. In: Engaging Theories in Family Communication. London: Routledge (2017) p. 75–86. doi: 10.4324/9781315204321-7
72. Farzadnia S, Giles H. Patient-provider interaction: a communication accommodation theory perspective. Int J Soc Cult Lang. (2015) 3:17–34.
73. Morton L, Cogan N, Kornfält S, Porter Z, Georgiadis E. Baring all: the impact of the hospital gown on patient well-being. Br J Health Psychol. (2020) 25:452–73. doi: 10.1111/bjhp.12416
74. Frankel R, Peyser A, Farner K, Rabin JM. Healing by leaps and gowns: a novel patient gowning system to the rescue. J Patient Exp. (2021) 8:23743735211033152. doi: 10.1177/23743735211033152
75. Smith PB, Trompenaars F, Dugan S. The Rotter locus of control scale in 43 countries: a test of cultural relativity. Int J Psychol. (1995) 30:377–400. doi: 10.1080/00207599508246576
76. Ruhnke GW, Tak HJ, Meltzer D. Association of preferences for participation in decision-making with care satisfaction among hospitalized patients. JAMA Netw Open. (2020) 3:e2018766. doi: 10.1001/jamanetworkopen.2020.18766
77. Barbosa HC, de Queiroz Oliveira JA, da Costa JM, de Melo Santos RP, Miranda LG, de Carvalho Torres H, et al. Empowerment-oriented strategies to identify behavior change in patients with chronic diseases: an integrative review of the literature. Patient Educ Couns. (2021) 104:689–702. doi: 10.1016/j.pec.2021.01.011
78. Cole C, Wellard S, Mummery J. Problematizing autonomy and advocacy in nursing. Nurs Ethics. (2014) 21:576–82. doi: 10.1177/0969733013511362
79. Gabay G. Exploring perceived control and self-rated health in re-admissions among younger adults: a retrospective study. Patient Educ Counsel. (2016) 99:800–6. doi: 10.1016/j.pec.2015.11.011
80. Walburg V, Friederich F, Callahan S. Embarrassment and modesty feelings during pregnancy, childbirth, and follow-up care: a qualitative approach. J Reprod Infant Psychol. (2014) 32:126–36. doi: 10.1080/02646838.2013.860518
81. Ling EJ, Shanafelt TD, Singer SJ. Understanding memorably negative provider care delivery experiences: why patient experiences matter for physicians. Healthcare J. (2021) 9:100544. doi: 10.1016/j.hjdsi.2021.100544
83. Stevanovic M. On the ideals of interaction and why and how they fail. Healthc J. (2023) 9:100544.
84. Dunn M. At the moral margins of the doctor–patient relationship. New Eng J Med. (2019) 45:149–50. doi: 10.1136/medethics-2019-105407
85. Gabay G, Bokek-Cohen Y. What do patients want? Surgical informed-consent and patient-centered care–An augmented model of information disclosure. Bioethics. (2020) 34:467–77. doi: 10.1111/bioe.12703
86. Black S, Torlei K. Designing a new type of hospital gown: a user-centered design approach case study. Fash Pract. (2013) 5:153–60. doi: 10.2752/175693813X13559997789005
87. Pitts P. Can there be value-based medicine without values? J Commer Biotechnol. (2018) 23:6–8. doi: 10.5912/jcb823
88. Schmittdiel JA, Desai J, Schroeder EB, Paolino AR, Nichols GA, Lawrence JM, et al. Methods for engaging stakeholders in comparative effectiveness research: a patient-centered approach to improving diabetes care. Healthcare. (2015) 3:80–8doi: 10.1016/j.hjdsi.2015.02.005
89. Bergbom I, Pettersson M, Mattsson E. Patient clothing—practical solution or means of imposing anonymity? J Hosp Med Manage. (2017) 3:1–6.
90. Hendricks S, Conrad N, Douglas TS, Mutsvangwa T. A modified stakeholder participation assessment framework for design thinking in health innovation. Healthcare. (2018) 6:191–6. doi: 10.1016/j.hjdsi.2018.06.003
91. Gordon L, Guttmann S. A user-centered approach to the redesign of the patient hospital gown. Fash Pract. (2013) 5:137–51. doi: 10.2752/175693813X13559997788961
92. Carlgren L, Rauth I, Elmquist M. Framing design thinking: the concept in idea and enactment. Creat Innovat Manage. (2016) 25:38–57. doi: 10.1111/caim.12153
Keywords: design thinking, hospitalization, patient-engagement, patient gown, patient-centered care, locus of control, patient-clinician communication
Citation: Gabay G and Ornoy H (2024) Revisiting the hospital-issued gown in hospitalizations from a locus of control and patient-centered care perspectives: a call for design thinking. Front. Public Health 12:1420919. doi: 10.3389/fpubh.2024.1420919
Received: 21 May 2024; Accepted: 27 August 2024;
Published: 16 September 2024.
Edited by:
Yibo Wu, Peking University, ChinaReviewed by:
Szymon Szemik, Medical University of Silesia, PolandEmily Elstad, American Institutes for Research, United States
Nurcan Kolaç, Marmara University, Türkiye
Eva Turk, St. Pölten University of Applied Sciences, Austria
Copyright © 2024 Gabay and Ornoy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gillie Gabay, Z2lsbGllLmdhYmF5QGdtYWlsLmNvbQ==
 Gillie Gabay
Gillie Gabay Hana Ornoy2
Hana Ornoy2