- 1Department of Pediatrics and Child Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Medical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 3Department of Emergency and Critical Care Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Surgical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Introduction: Globally, nearly half of all deaths among children under the age of five are linked to undernutrition. These tragic outcomes are most prevalent in low- and middle-income countries. The far-reaching impact of malnutrition affects not only individuals but also their families, communities, and entire nations. By examining underweight, we gain valuable insights into the intricate network of factors influencing child health. Therefore, this study aims to assess underweight prevalence and its associated factors among under-five children in low and lower-middle-income African countries.
Method: We conducted a secondary analysis of standard demographic and health surveys in 30 low and lower-middle-income African countries spanning from 2012 to 2022. Our analysis included a total sample of 200,655 children under the age of 5 years. We employed a three-level hierarchical model to assess the determinants of underweight among children in this age group. Measures of association were evaluated using adjusted odds ratios with a 95% confidence interval. Explanatory variables with a p-value less than the level of significance (0.05) were considered statistically significant.
Result: The pooled prevalence of underweight among children under the age of five in low and lower-middle income African countries was estimated at 17.60%, with a 95% confidence interval (CI) ranging from 17.44 to 17.77%. The hierarchical analysis identified several factors significantly associated with underweight, including male gender, birth size, maternal body mass index, maternal educational level, household wealth index, antenatal care (ANC) visits, community poverty level, and income level of countries.
Conclusion: The high prevalence of underweight among children under the age of five in low and lower-middle income African countries underscores the need for targeted interventions. By addressing individual, community, and country-level factors, we can work toward improving child nutrition and well-being.
Introduction
Underweight refers to a low weight for age (weight-for-age less than −2 standard deviations (SD) of the WHO Child Growth Standards median) that can be a result of stunting, wasting, or frequently both (1–3). Globally, about half of the deaths among under-five children are related to undernutrition (4, 5). These primarily happen in low- and middle-income countries (4, 5). In terms of development, economics, social issues, and medicine, the worldwide burden of malnutrition has serious and enduring repercussions on individuals as well as their families, communities, and nations (1, 3, 5). Poor eating habits and inadequate nutrition are two of the biggest risk factors for chronic illnesses worldwide. Diabetes, several cancers, and cardiovascular disorders (heart attacks, strokes, and high blood pressure) are prominent instances of non-communicable diseases (NCDs) linked to malnutrition (5).
Malnutrition is one of the main agenda items for Sustainable Development by 2030—in particular, Sustainable Development Goal (SDG) 2 (set a concrete aim to end hunger, achieve food security and improved nutrition, and promote sustainable agriculture) and SDG 3 (to ensure healthy lives and promote wellbeing for all at all ages) (5, 6). However, undernutrition rates have increased globally since 2014 (7). In The State of Food Security and Nutrition in the World 2023, the Food and Agriculture Organization (FAO) of the United Nations reported that there were 122 million more undernourished people than there were in 2019—nearly 735 million people, or 9.2% of the world’s population (7). Most live in countries where food insecurity is pervasive. Undernutrition increased in frequency in Africa from 19.4% in 2021 to 19.7% in 2022 (7). About 45 million children under the age of five were wasted and 149 million stunted globally in 2022 (4, 5). Underweight is a direct composite indicator both chronic (stunting) and acute (wasting) undernutrition (8). Around 17.1% of children under five in the WHO’s Africa area were underweight in 2018, which corresponds to 29 million children (9, 10). These numbers represent real children facing nutritional challenges, and addressing their needs is essential for their health and well-being.
According to the evidence (11–13), the following are among the factors significantly associated with underweight among children under five: age, gender, place of residence, maternal educational levels, diarrhea, maternal occupational status, twin or triplet birth, birth order, birth weight, place of delivery, and the use of fortified baby food. In addition, this study aimed to determine individual, community, and country-level factors associated with underweight among under-five children.
Childhood underweight is a critical issue, especially in low and lower-middle-income countries (14). By studying this phenomenon, we gain insights into the complex web of factors affecting child health. Addressing childhood underweight is essential for building human capital, aligning with the Sustainable Development Goals (SDGs), and tailoring evidence-based interventions (15). Overall, studying childhood underweight in Africa lays the groundwork for targeted interventions, poverty reduction, and healthier futures for children. Hence, this study aimed to assess the underweight and associated factors among under-five children in low and lower-middle-income African countries using data from standard demographic and health surveillance data.
Methods
Data source, setting and sampling
This study conducted a secondary analysis of standard demographic and health surveys in low and lower-middle-income African countries from 2012 to 2022. The research utilized datasets known as the children’s recode (KR), which were obtained from the Monitoring and Evaluation to Assess and Use Results Demographic and Health Survey (MEASURE DHS) program. These datasets are publicly accessible at https://www.dhsprogram.com. The MEASURE DHS program offers researchers valuable data for formal requests related to project registration and submission. For this study, we selected a total of 30 low- and lower-middle-income African countries. The criteria for inclusion were the availability of Demographic and Health Surveys (DHS) data spanning the period from 2012 to 2022, as well as the availability of WHO weight-for-age Growth Standard scores within their DHS datasets.
The DHS data collection process employs a stratified two-stage cluster sampling technique. In the first stage, we select enumeration areas (also known as sampling clusters) based on their population size, using probability proportional to size. In the second stage, we choose a sample of households within these clusters, collecting actual data. As a result, the DHS data exhibit a hierarchical structure. Our analysis included a total sample of 200,655 children under the age of 5 years.
Variables and data management
The outcome variable of this study was underweight among children under age of five which was determined as weight-for-age less than −2 standard deviations of the WHO Child Growth Standards median (1). It was dichotomized as “yes” for children who were underweight and “no” for children who were not underweight.
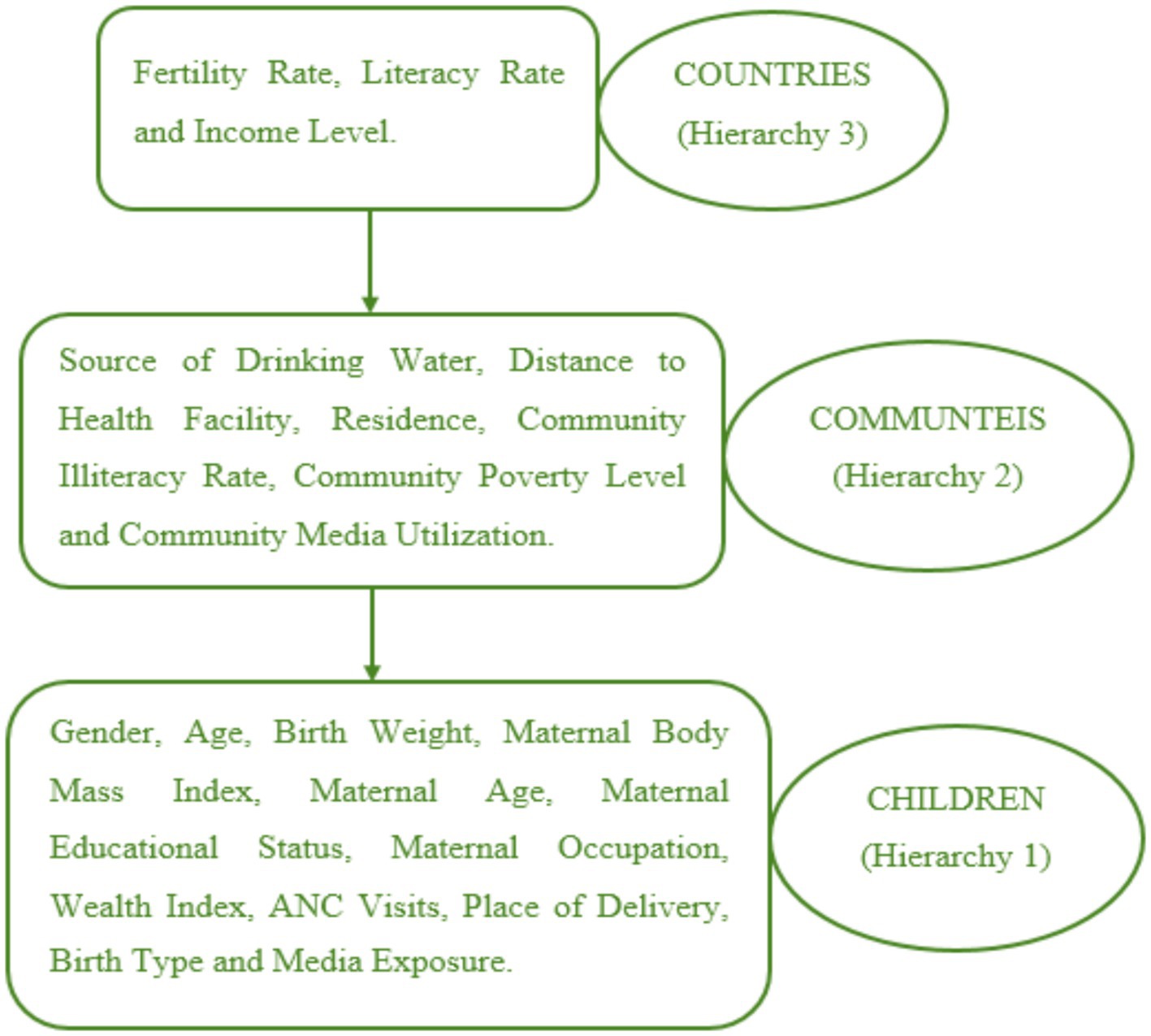
The study examined three hierarchical levels of independent variables. The first hierarchy included gender, age, birth weight, maternal body mass index, maternal age, maternal educational status, maternal occupation, wealth index, antenatal care (ANC) visits, place of delivery, birth type, and media exposure. The second hierarchy encompassed variables such as the source of drinking water, distance to health facilities, residence, community illiteracy rate, community poverty level, and community media utilization. Lastly, the third hierarchy consisted of fertility rate, literacy rate, and income level (as shown in Figure 1). Additionally, this study controlled for the effect of different survey years by including the year of the Demographic and Health Survey (DHS) as a control variable.
The World Bank classifies all countries’ economies into four income groups: low, lower-middle, upper-middle, and high-income. The thresholds for these classifications are updated annually based on the Gross National Income (GNI) per capita calculated using the World Bank Atlas method (16). For the 2022 fiscal year, which represents the most recent classification, low-income countries are defined as those with a GNI per capita of $1,165 or less (17). In contrast, lower-middle-income countries are defined as those with a GNI per capita between $1,166 and $4,565 (16, 17). This income-based categorization provides a standardized framework for analyzing economic development and comparing the relative prosperity of different nations around the world (16, 17).
The children’s recode data archive, available in Stata format for all countries, was extracted from the MEASURE DHS website, https://www.dhsprogram.com. After extraction, individual country datasets were combined, resulting in a single data file created using Stata version 14. To ensure valid conclusions, weighting was applied, accounting for the sampling design. The study’s findings were then presented in tables and charts, reflecting weighted frequencies and percentages.
Statistical analysis
The analysis in this study incorporated three levels of explanatory variables using a hierarchical model. We sequentially fitted five models: First, the null model: This model included only the outcome variable without any explanatory variables. Second, Model I: We incorporated the outcome variable, first-level explanatory variables, and a control variable. Thirdly, Model II: This model included the outcome variable, second-level explanatory variables, and the control variable. Then, Model III: We extended the model to include the outcome variable, third-level explanatory variables, and the control variable. Finally, in Model IV, we integrated all levels of explanatory variables, the control variable, and the outcome. In our assessment, we considered both random and fixed effects within these models.
In terms of the random effect structure, given the cross-sectional nature of the DHS data, we exclusively employed a random intercept model. Within this model, we calculated the variance, intra-class correlation coefficient, and median odds ratio. Moving to the fixed component of the model, we evaluated the adjusted odds ratio at a 95% confidence interval. Explanatory variables with a p-value less than the level of significance (0.05) were considered statistically significant. Deviance was used for model comparison, due to nested nature of the hierarchical mode.
The three-level hierarchical (multilevel) model, designed to account for the hierarchical data with three levels, is represented as (18, 19);
Where yijk is the dependent variable for the ith individual in the jth community in the kth country, β0k and β1k are the intercept and slope coefficients for the kth country, xijk is the independent variable for the ith individual in the jth community in the kth country, rjk is the random effect for the jth community in the kth country, uik is the random effect for the ith individual in the kth country and eijk is the residual error for the ith individual in the jth community in the kth country.
Results
The study included a total of 200,655 children under the age of 5, with 50.43% males and 49.57% females. More than half (57.16%) of the participants were 24 months of age or older. Out of these children, 99,865 (61.40%) were born to mothers with a normal body mass index. The majority (70.63%) of the study subjects were born to mothers aged 20–34 years, while approximately 41% had mothers with no formal education. Additionally, 57.41% of the subjects’ mothers had four or more antenatal care (ANC) visits during pregnancy. A bit less than two-thirds (62.07%) of the study participants were from communities where distance to health facilities was not a problem. Furthermore, 138,875 (69.21%) subjects resided in rural areas, and over half (52.26%) came from low-income countries.
Regarding underweight status, 18,879 (18.66%) of male and 16,440 (16.53%) of female participants were underweight. Additionally, 7,762 (12.56%) of urban and 27,557 (19.84%) of rural resident children were underweight. Furthermore, 22,225 (21.20%) children in low-income countries and 13,094 (13.67%) children in lower-middle-income countries exhibited underweight conditions (Table 1).
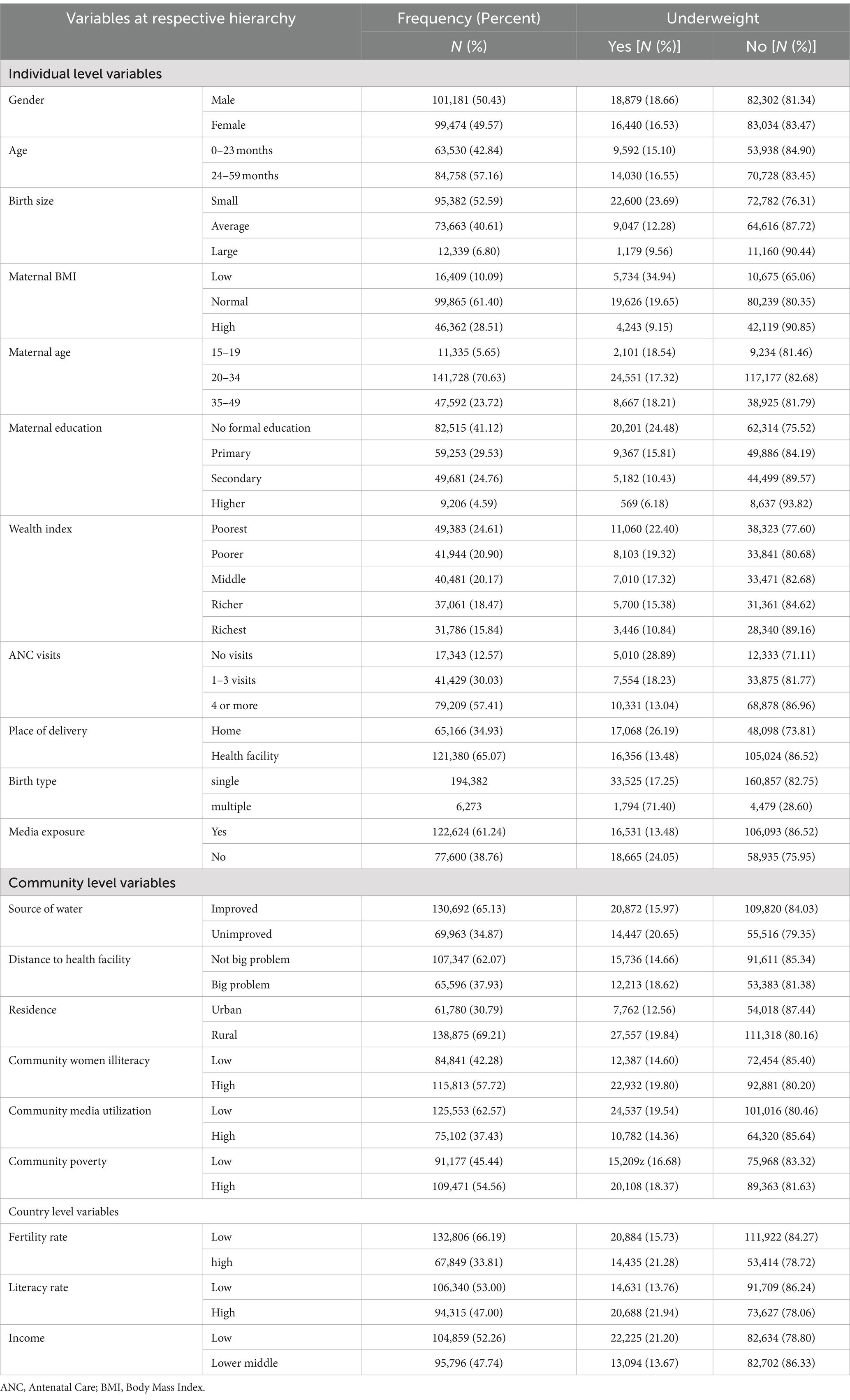
Table 1. Description of underweight by hierarchy of variables in low and lower-middle income African countries (N = 200,655).
Prevalence of underweight among under five children in low and lower-middle income African countries
The pooled prevalence of underweight among children under the age of five in low and lower-middle income African countries was determined to be 17.60%, with a 95% confidence interval (CI) ranging from 17.44 to 17.77%. Notably, Niger exhibited the highest prevalence of underweight (35.43%), while Egypt had the lowest prevalence (6.20%) (Figure 2).
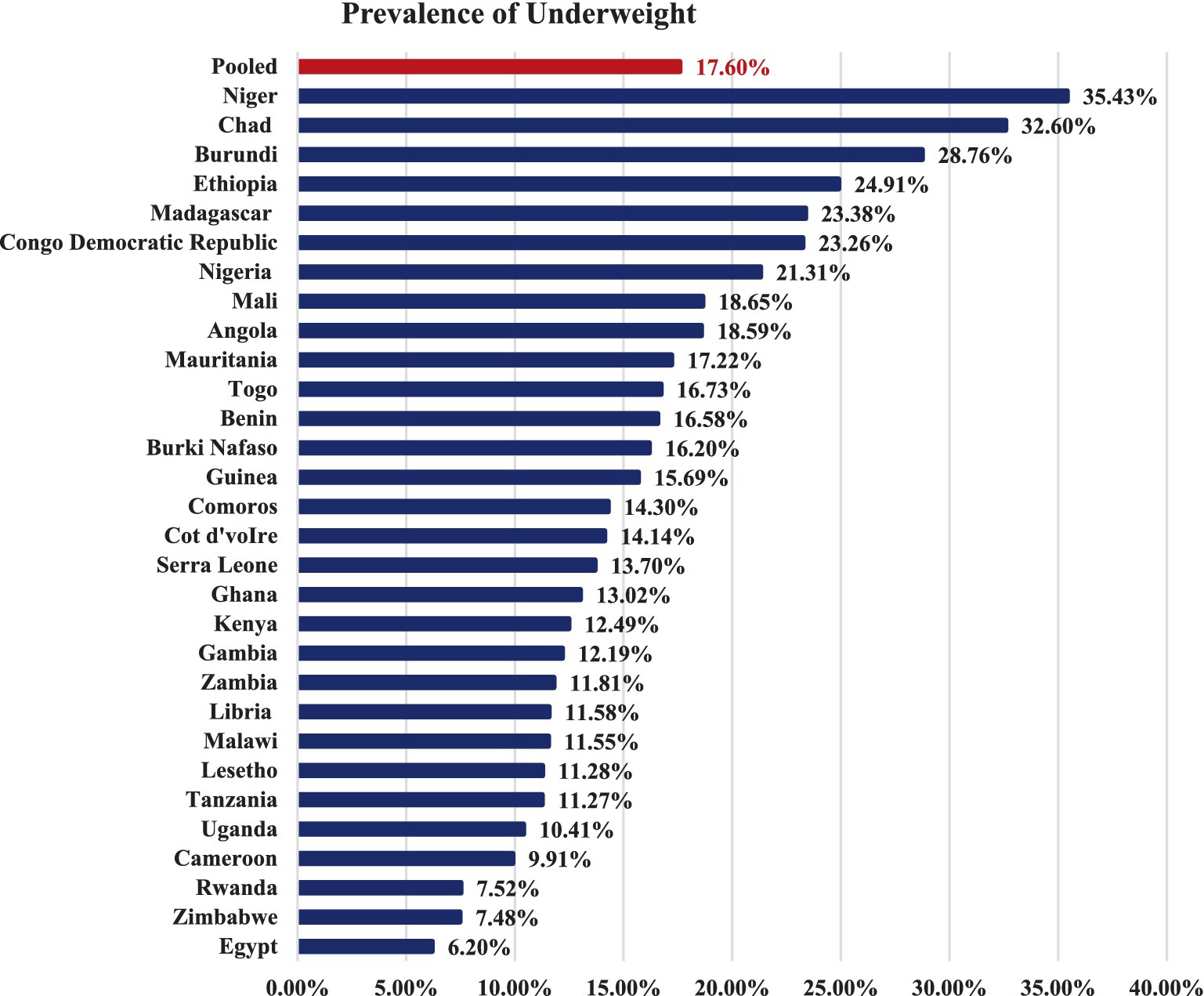
Figure 2. Prevalence of underweight among under five children in low and lower middle income African countries.
Random effect and model comparison
In the null model of the random effect model, we observed significant variation in underweight among children within communities (τ = 0.280, p < 0.001) and across countries (τ = 0.457, p < 0.00). This finding suggests that a hierarchical (multilevel) model is appropriate for analyzing the data. Specifically, the intra-community and intra-country correlation coefficients in the null model indicate that 7.84 and 12.25% of the total variation in underweight among children can be attributed to variations between communities and countries, respectively.
The unexplained heterogeneity (MOR) in underweight among communities and countries, without considering explanatory variables, was 1.65 and 1.90, respectively. However, after incorporating a full hierarchy of factors, the heterogeneity (MOR) decreased to 1.31 and 1.26. Model IV, which exhibited the smallest deviance value, was selected as the best-fitting model (Table 2).
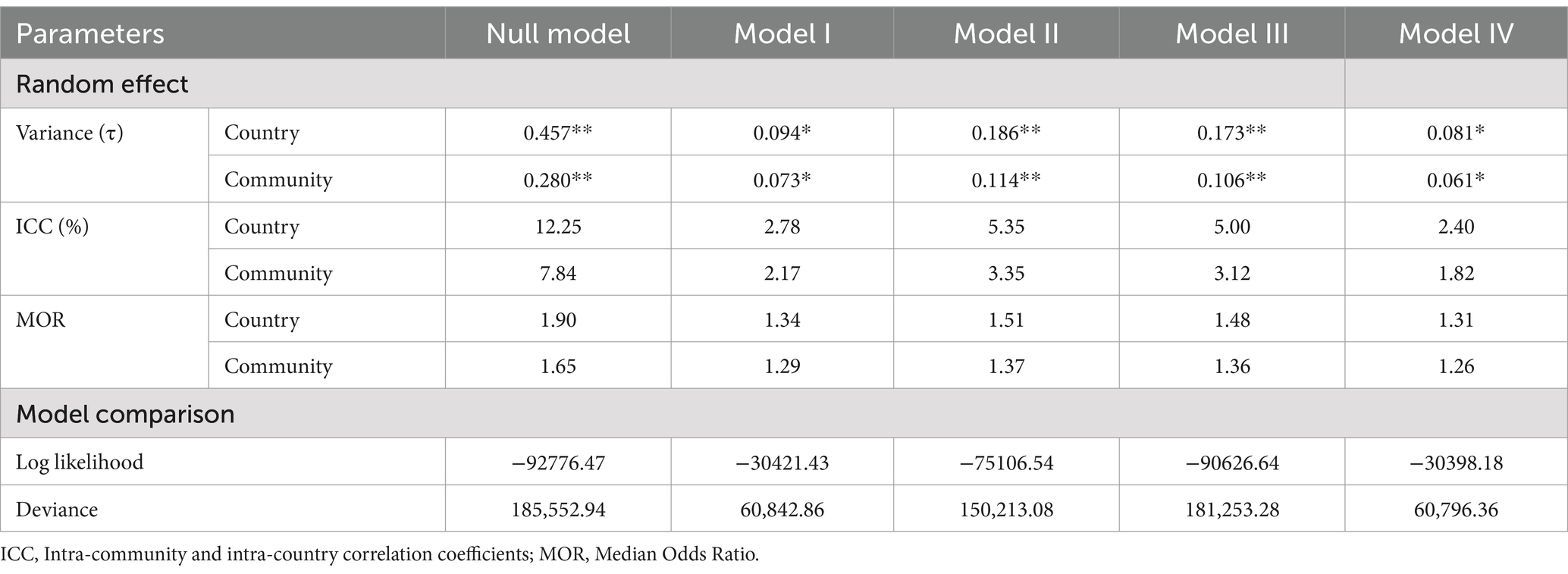
Table 2. Random effect and model comparison of underweight among under five children in low and lower-middle income African countries.
Fixed effect of underweight among under five children in low and lower-middle income African countries
The hierarchical analysis of this study found that gender, birth size, maternal BMI, maternal educational level, household wealth index, ANC visit, community poverty level, and income level of countries were significantly associated with underweight.
In this respect, the odds of being underweight were 1.29 times higher among male children (AOR = 1.29 at 95% CI: 1.24, 1.34) as compared to females. The odds of childhood underweight were 1.61 times higher among children with smaller sizes (AOR = 1.61 at 95% CI: 1.53, 1.70) than children with average sizes at birth. In addition, the odds of being underweight decreased by 39% for children of large birth size (AOR = 0.61 at 95% CI: 0.54, 0.67) compared to children with average weight. Likewise, the odds of underweight were 1.94 times higher among children born to mothers with a low body mass index (AOR = 1.94 at 95% CI: 1.83, 2.06) and reduced by 30% for children born to mothers with a high body mass index (AOR = 0.60 at 95% CI: 0.57, 0.64).
When compared to children born to mothers with a higher educational level, the odds of being underweight were 1.85, 1.44, and 1.27 times higher among children born to mothers with no formal education (AOR = 1.85 at 95% CI: 1.59, 2.16), primary schooling (AOR = 1.44 at 95% CI: 1.23, 1.67), and secondary schooling (AOR = 1.27 at 95% CI: 1.09, 1.47), respectively.
Regarding the wealth index, the odds of underweight were 1.10, 1.24, 1.34, and 1.44 times higher among children of households with richer (AOR = 1.10 at 95% CI: 1.02, 1.20), middle (AOR = 1.24 at 95% CI: 1.13, 1.35), poor (AOR = 1.34 at 95% CI: 1.22, 1.47) and poorer (AOR = 1.44 at 95% CI: 1.31, 1.58), respectively. The odds of underweight were 1.16 and 1.08 times higher among children who were born to mothers who had no ANC visits (AOR = 1.16 at 95% CI: 1.08, 1.24) and 1–3 ANC visits (AOR = 1.08 at 95% CI: 1.03, 1.13), respectively.
In addition, the odds of being underweight were 1.09 times higher among children born in a community with a high poverty level (AOR = 1.09, 95% CI: 1.03, 1.13). Moreover, the odds of being underweight were 1.11 times higher among children in countries with low income (AOR = 1.11 at 95% CI: 1.06, 1.16) (Table 3).
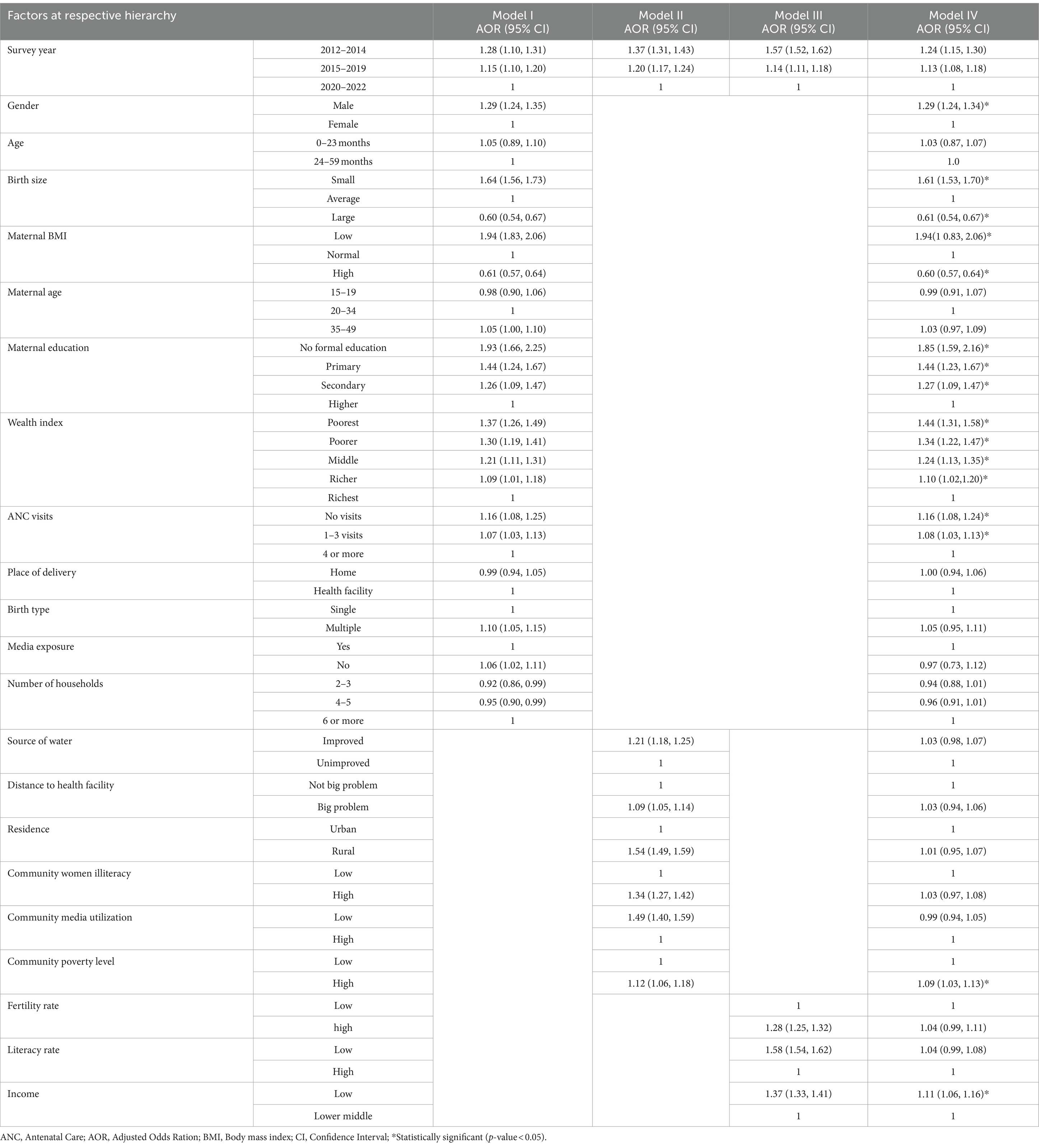
Table 3. Fixed effect of underweight among under five children in low and lower-middle income African countries.
Discussion
Addressing childhood underweight is essential for building human capital, aligning with the Sustainable Development Goals (SDGs), and tailoring evidence-based interventions (15). Studying childhood underweight in Africa lays the groundwork for targeted interventions, poverty reduction, and healthier futures for children. Hence, this study assessed the underweight and associated factors among under-five children in low and lower-middle-income African countries using data from standard demographic and health survey.
The pooled prevalence of underweight among children under the age of five in low and lower-middle income African countries was determined to be 17.60%, with a 95% confidence interval (CI) ranging from 17.44 to 17.77%. The prevalence of underweight among children under the age of five in this study was slightly higher than the prevalence of underweight children under the age of five in the WHO’s Africa region (17.1%) (9, 10). Additionally, the prevalence in our study was far higher than the global prevalence of childhood underweight, which was 13.4% (9, 10, 20). The observed discrepancy may be attributed to the inclusion of low and lower-middle-income African countries in this study, whereas subsequent studies estimated underweight prevalence without considering the income levels of the countries. This finding highlights the higher prevalence of underweight children in economically disadvantaged African nations, emphasizing the need for global strategies to prioritize a country’s income status when implementing childhood nutritional interventions.
This study revealed that gender, birth size, maternal BMI, maternal educational level, household wealth index, ANC visit, community poverty level, and income level of countries were significantly associated with underweight.
In this regard, the odds of underweight were high among male children than females. This finding is in agreement with previous evidences (21–23). On the other hand, a study in Pakistan reported that the likelihood of a girl child being underweight is greater than that of a boy child being underweight (12). The higher likelihood of underweight among male children compared to females can be attributed to several factors. First, biological differences play a significant role. Boys tend to have a slightly higher metabolic rate than girls, which means they may burn calories faster. If their nutritional intake is insufficient, this can lead to an underweight status (24). Additionally, boys often experience growth spurts during adolescence, requiring additional energy and nutrients. If their diet does not meet these demands, they may become underweight (24). Secondly, health conditions and infections also play a role. Boys are often more susceptible to infections, such as respiratory or gastrointestinal infections, which can affect their appetite and nutrient absorption. Additionally, certain chronic illnesses (like chronic diarrhea or malabsorption disorders) can impact boys’ weight gain (24). However, we could not ignore the cultural and social factors that contribute to disparity enabling males to be nourished than females. Gender norms, shaped by societal expectations, influence feeding practices (25, 26). For instance, boys might be encouraged to eat more or prioritize certain foods, while girls may receive smaller portions. Moreover, food distribution within households can impact boys’ overall nutrition. In some families, male members receive preferential treatment when it comes to food allocation (25).
Regarding the birth size of children, the odds of childhood underweight were higher among children with smaller sizes than children with average sizes at birth. In addition, children of large birth size had lower odds of being underweight than children of average weight. This finding is in line with existing evidences (27–31). There are multiple ways in which birth size and childhood underweight are interconnected. Contributing factors include changes in epigenetic patterns, inadequate maternal nutrition during pregnancy, intrauterine growth restriction (IUGR), and placental insufficiency (32). A child’s growth is influenced by nutrition, breastfeeding practices, and overall postnatal care. Babies born with low birth weights may struggle to reach their ideal growth (33). The nutritional status of the infant was significantly influenced by the child’s size at delivery, since low birth size is indicative of controlled intrauterine development (30, 34).
Likewise, the likelihood of childhood underweight was higher among children born to mothers with a low body mass index and lower for children born to mothers with a high body mass index. Studies have also witnessed the same (31, 35, 36). Proper nutrition is crucial for women during both prenatal and postnatal phases to support healthy child growth. Maternal body mass index (BMI) plays a significant role in determining child undernutrition, and it is influenced by maternal nutrition. Children born to healthy mothers are at a reduced risk of being undernourished (35).
Coherent with previous findings (12, 37, 38), this study found that no or lower level of maternal education was associated with higher odds of childhood underweight. The association could be due to the fact that educated mothers tend to have better knowledge about nutrition, hygiene, and child care practices (39). They also have improved access to resources such as nutritious food and healthcare. Maternal education empowers women to make informed decisions regarding their own health and their children’s well-being (40). It enhances health literacy, leading to better adherence to recommended practices. Additionally, educated mothers pass on knowledge and positive behaviors to their children, creating a cycle of improved health (38). Overall, promoting education among women is crucial for breaking the cycle of childhood underweight and improving overall health outcomes.
Significantly, the likelihood of underweight increased as the household wealth index declined from richer to the poorest, with the richest group serving as the reference. This observation aligns with previous research (13, 41, 42). This could be due to the fact that children from poorer households are more likely to experience underweight due to limited access to resources such as nutritious food and healthcare (41). Wealthier households, on the other hand, can invest more in their children’s well-being (41). This suggests addressing wealth-related disparities is crucial for preventing childhood underweight and improving overall child nutrition.
We found that children born to mothers who had no or 1–3 antenatal care (ANC) visits during pregnancy were more likely to be underweight compared to children born to mothers who had four or more ANC visits. This finding aligns with previous research studies (43–46). One possible reason for this association is that access to health care services, such as ANC, serves as a crucial source of information for women regarding nutrition and overall health (45). Additionally, mothers who received ANC follow-ups had opportunities for knowledge sharing related to optimal infant and young child feeding (47). Consequently, children whose mothers had ANC visits were less likely to experience underweight. Furthermore, ANC visits provided mothers with essential information about breastfeeding, which plays an indispensable role in minimizing underweight among children (46).
Consistent with prior research (48–50), this study revealed that children born in communities with high poverty levels had elevated odds of being underweight compared to their counterparts born in low-poverty communities. This implies that childhood underweight is a critical issue, particularly in communities grappling with high poverty levels. Several factors contribute to this concerning phenomenon. First, families living in poverty often struggle to provide adequate nutrition for their children due to limited financial resources (51). Poor living conditions, a lack of clean water, and inadequate sanitation facilities also impact child well-being (14, 52). Additionally, food insecurity, inadequate healthcare access, and indoor pollution further exacerbate underweight rates (52). Therefore, addressing poverty, education, healthcare, and tailored interventions in communities with high poverty are essential to combating childhood underweight in impoverished communities (14).
This study also revealed a significant association between the low income level of countries and higher odds of underweight, particularly when compared to lower-middle income countries. This finding aligns with results from another studies (14, 53). The economic challenges faced by low-income countries can directly impact child growth and development due to limited access to essential resources. These constraints include inadequate access to nutritious food, clean water, sanitation, and healthcare services (54). Investing in childhood nutrition and ensuring access to these fundamental needs can play a pivotal role in reducing underweight rates. By addressing these critical factors, we not only improve children’s health but also create a pathway for their future economic opportunities (54, 55).
The findings of this study should be regarded with the following limitations: First, it relies on data from standard demographic and health surveys conducted in specific low and lower-middle-income African countries, potentially introducing sampling bias. Second, the cross-sectional design captures data at a single point in time, limiting insights into causal relationships. Third, self-reported data may be subject to recall bias.
Conclusion
The high prevalence of underweight among children under the age of five in low and lower-middle income African countries underscores the need for targeted interventions. By addressing individual, community, and country-level factors, we can work toward improving child nutrition and well-being.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Author contributions
TT: Formal analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. AZ: Conceptualization, Data curation, Validation, Visualization, Writing – review & editing. BW: Conceptualization, Investigation, Project administration, Visualization, Writing – review & editing. EM: Conceptualization, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. de Onis, M . 4.1 the WHO child growth standards. Pediatr Nutri Prac. (2015) 113:278–94. doi: 10.1159/000360352
2. Meyers, A, Joyce, K, Coleman, SM, Cook, JT, Cutts, D, Ettinger de Cuba, S, et al. Health of children classified as underweight by CDC reference but normal by WHO standard. Pediatrics. (2013) 131:e1780–7. doi: 10.1542/peds.2012-2382
3. World Health Organization and United Nations Children’s Fund (UNICEF) . Recommendations for data collection, analysis and reporting on anthropometric indicators in children under 5 years old. World Health Organization. (2019).
4. Organization, W.H . UNICEF-WHO-the World Bank: Joint child malnutrition estimates: Levels and trends. Geneva: WHO (2019).
6. Varzakas, T, and Smaoui, S. Global food security and sustainability issues: the road to 2030 from nutrition and sustainable healthy diets to food systems change. Food Secur. (2024) 13:306. doi: 10.3390/foods13020306
7. Organization, W.H . The state of food security and nutrition in the world 2022: Repurposing food and agricultural policies to make healthy diets more affordable, vol. 2022 Rome, Italy: Food & Agriculture Org (2022).
8. Alemayehu, GM, Cherie, KT, and Chernet, AG. Severity of malnutrition among underweight children and family-related factors: a cross-sectional analysis of data from the 2019 Ethiopian demographic and health survey (EDHS). Health Sci Rep. (2022) 5:e860. doi: 10.1002/hsr2.860
9. GHO . Global and regional trends by WHO regions, underweight:1990–2020 WHO. Geneva, Switzerland: World Health Organization (1990-2020).
10. Bank, W ., Prevalence of underweight, weight for age (Washington, DC, USA: % of children under 5). (2023).
11. Enbeyle, W, Bitew, D, Marzo, RR, Pandey, D, Abebaw, S, and Belay, A. Multilevel analysis of factors associated with underweight among under-five children in Ethiopia. J Pediatr Neuropsychol. (2022) 8:45–51. doi: 10.1007/s40817-021-00118-6
12. Kumar, R, Abbas, F, Mahmood, T, and Somrongthong, R. Prevalence and factors associated with underweight children: a population-based subnational analysis from Pakistan. BMJ Open. (2019) 9:e028972. doi: 10.1136/bmjopen-2019-028972
13. Li, Z, Kim, R, Vollmer, S, and Subramanian, SV. Factors associated with child stunting, wasting, and underweight in 35 low-and middle-income countries. JAMA Netw Open. (2020) 3:e203386–6. doi: 10.1001/jamanetworkopen.2020.3386
14. Siddiqui, F, and Das, JK. The intertwined relationship between malnutrition and poverty. Front Public Health. (2020) 8:525026. doi: 10.3389/fpubh.2020.00453
15. Black, MM, Pérez-Escamilla, R, and Rao, SF. Integrating nutrition and child development interventions: scientific basis, evidence of impact, and implementation considerations. Adv Nutr. (2015) 6:852–9. doi: 10.3945/an.115.010348
16. Owusu-Peprah, NT . World development report 2022: Finance for an equitable recovery. Washington, DC: World Bank publications (2022).
17. Ott, J . World Bank world development reports In: AC Michalos , editor. Encyclopedia of quality of life and well-being research. Dordrecht: Springer (2024). 7858–9.
18. Heck, R, and Thomas, SL. An introduction to multilevel modeling techniques: MLM and SEM approaches New York, Routledge (2020).
19. Gibbons, RD, Hedeker, D, and DuToit, S. Advances in analysis of longitudinal data. Annu Rev Clin Psychol. (2010) 6:79–107. doi: 10.1146/annurev.clinpsy.032408.153550
20. World Bank . The World Bank and Nutrition: Malnutrition is one of the world’s most serious but least-addressed development challenges. Its human and economic costs are enormous, falling hardest on the poor, women, and children. Washington, DC, USA:World Bank (2023). https://www.worldbank.org/en/topic/nutrition/overview
21. Marphatia, AA, Cole, TJ, Grijalva-Eternod, C, and Wells, JCK. Associations of gender inequality with child malnutrition and mortality across 96 countries. Glob Health Epidemiol Genom. (2016) 1:e6. doi: 10.1017/gheg.2016.1
22. Mukabutera, A, Thomson, DR, Hedt-Gauthier, BL, Basinga, P, Nyirazinyoye, L, and Murray, M. Risk factors associated with underweight status in children under five: an analysis of the 2010 Rwanda demographic health survey (RDHS). BMC Nutr. (2016) 2:1–12. doi: 10.1186/s40795-016-0078-2
23. Masibo, PK, and Makoka, D. Trends and determinants of undernutrition among young Kenyan children: Kenya demographic and health survey; 1993, 1998, 2003 and 2008–2009. Public Health Nutr. (2012) 15:1715–27. doi: 10.1017/S1368980012002856
24. Sahiledengle, B, Mwanri, L, Blumenberg, C, and Agho, KE. Gender-specific disaggregated analysis of childhood undernutrition in Ethiopia: evidence from 2000–2016 nationwide survey. BMC Public Health. (2023) 23:2040. doi: 10.1186/s12889-023-16907-x
25. Coleman, A, O'Neil, J, and Ferris, AM. The mediation effect between everyday discrimination, gender role conflict, emotional eating, and obesity in African American fathers and sons. Psychol Men Masc. (2019) 20:182. doi: 10.1037/men0000201
26. Shah, B, Tombeau Cost, K, Fuller, A, Birken, CS, and Anderson, LN. Sex and gender differences in childhood obesity: contributing to the research agenda. BMJ Nutr Prev Health. (2020) 3:387–90. doi: 10.1136/bmjnph-2020-000074
27. Poda, GG, Hsu, C-Y, and Chao, JC-J. Factors associated with malnutrition among children< 5 years old in Burkina Faso: evidence from the demographic and health surveys IV 2010. Int J Qual Health Care. (2017) 29:901–8. doi: 10.1093/intqhc/mzx129
28. Pravana, NK, Piryani, S, Chaurasiya, SP, Kawan, R, Thapa, RK, and Shrestha, S. Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community-based case–control study. BMJ Open. (2017) 7:e017084. doi: 10.1136/bmjopen-2017-017084
29. Khan, S, Zaheer, S, and Safdar, NF. Determinants of stunting, underweight and wasting among children< 5 years of age: evidence from 2012-2013 Pakistan demographic and health survey. BMC Public Health. (2019) 19:1–15. doi: 10.1186/s12889-019-6688-2
30. Rahman, MS, Howlader, T, Masud, MS, and Rahman, ML. Association of low-birth weight with malnutrition in children under five years in Bangladesh: do mother’s education, socio-economic status, and birth interval matter? PLoS One. (2016) 11:e0157814. doi: 10.1371/journal.pone.0157814
31. Asmare, AA, and Agmas, YA. Determinants of coexistence of stunting, wasting, and underweight among children under five years in the Gambia; evidence from 2019/20 Gambian demographic health survey: application of multivariate binary logistic regression model. BMC Public Health. (2022) 22:1621. doi: 10.1186/s12889-022-14000-3
32. Namiiro, FB, Batte, A, Rujumba, J, Nabukeera-Barungi, N, Kayom, VO, Munabi, IG, et al. Nutritional status of young children born with low birthweight in a low resource setting: an observational study. BMC Pediatr. (2023) 23:520. doi: 10.1186/s12887-023-04356-9
33. Ntenda, PAM . Association of low birth weight with undernutrition in preschool-aged children in Malawi. Nutr J. (2019) 18:1–15. doi: 10.1186/s12937-019-0477-8
34. Sharma, D, Shastri, S, and Sharma, P. Intrauterine growth restriction: antenatal and postnatal aspects. Clin Med Insights Pediatr. (2016) 10:67–83. doi: 10.4137/CMPed.S40070
35. Talukder, A . Factors associated with malnutrition among under-five children: illustration using Bangladesh demographic and health survey, 2014 data. Children. (2017) 4:88. doi: 10.3390/children4100088
36. Mawa, R, and Lawoko, S. Malnutrition among children under five years in Uganda. Am J Health Res. (2018) 6:56. doi: 10.11648/j.ajhr.20180602.14
37. Chowdhury, TR, Chakrabarty, S, Rakib, M, Saltmarsh, S, and Davis, KA. Socio-economic risk factors for early childhood underweight in Bangladesh. Glob Health. (2018) 14:1–12. doi: 10.1186/s12992-018-0372-7
38. Vollmer, S, Bommer, C, Krishna, A, Harttgen, K, and Subramanian, SV. The association of parental education with childhood undernutrition in low-and middle-income countries: comparing the role of paternal and maternal education. Int J Epidemiol. (2017) 46:312–23. doi: 10.1093/ije/dyw133
39. Makoka, D, and Masibo, PK. Is there a threshold level of maternal education sufficient to reduce child undernutrition? Evidence from Malawi, Tanzania and Zimbabwe. BMC Pediatr. (2015) 15:1–10. doi: 10.1186/s12887-015-0406-8
40. Yorke, FR, Wahab, S, and Turkson, D. Maternal education and child malnutrition: evidence from selected west African countries. SN Soc Sci. (2023) 3:200. doi: 10.1007/s43545-023-00792-7
41. Organization, W.H . Underweight among children under 5 years of age (number in millions)(JME) Geneva, Switzerland: WHO (2022).
42. Kassie, GW, and Workie, DL. Determinants of under-nutrition among children under five years of age in Ethiopia. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-08539-2
43. Kuhnt, J, and Vollmer, S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. (2017) 7:e017122. doi: 10.1136/bmjopen-2017-017122
44. Yisak, H, Gobena, T, and Mesfin, F. Prevalence and risk factors for under nutrition among children under five at Haramaya district, Eastern Ethiopia. BMC Pediatr. (2015) 15:1–7. doi: 10.1186/s12887-015-0535-0
45. Ashorn, P, Alho, L, Ashorn, U, Cheung, YB, Dewey, KG, Gondwe, A, et al. Supplementation of maternal diets during pregnancy and for 6 months postpartum and infant diets thereafter with small-quantity lipid-based nutrient supplements does not promote child growth by 18 months of age in rural Malawi: a randomized controlled trial. J Nutr. (2015) 145:1345–53. doi: 10.3945/jn.114.207225
46. Fekadu, Y, Mesfin, A, Haile, D, and Stoecker, BJ. Factors associated with nutritional status of infants and young children in Somali region, Ethiopia: a cross-sectional study. BMC Public Health. (2015) 15:1–9. doi: 10.1186/s12889-015-2190-7
47. Abebe, Z, Haki, GD, and Baye, K. Health extension workers’ knowledge and knowledge-sharing effectiveness of optimal infant and young child feeding are associated with mothers’ knowledge and child stunting in rural Ethiopia. Food Nutr Bull. (2016) 37:353–63. doi: 10.1177/0379572116651209
48. Chowdhury, MRK, Rahman, MS, Khan, MMH, Mondal, MNI, Rahman, MM, and Billah, B. Risk factors for child malnutrition in Bangladesh: a multilevel analysis of a nationwide population-based survey. J Pediatr. (2016) 172:194–201.e1. doi: 10.1016/j.jpeds.2016.01.023
49. Adekanmbi, VT, Kayode, GA, and Uthman, OA. Individual and contextual factors associated with childhood stunting in Nigeria: a multilevel analysis. Matern Child Nutr. (2013) 9:244–59. doi: 10.1111/j.1740-8709.2011.00361.x
50. Ntenda, PAM, and Chuang, Y-C. Analysis of individual-level and community-level effects on childhood undernutrition in Malawi. Pediatr Neonatol. (2018) 59:380–9. doi: 10.1016/j.pedneo.2017.11.019
51. Sahiledengle, B, Mwanri, L, Petrucka, P, Kumie, A, Beressa, G, Atlaw, D, et al. Determinants of undernutrition among young children in Ethiopia. Sci Rep. (2022) 12:20945. doi: 10.1038/s41598-022-25160-y
52. Tzioumis, E, and Adair, LS. Childhood dual burden of under-and overnutrition in low-and middle-income countries: a critical review. Food Nutr Bull. (2014) 35:230–43. doi: 10.1177/156482651403500210
53. Mary, S . How much does economic growth contribute to child stunting reductions? Economies. (2018) 6:55. doi: 10.3390/economies6040055
54. McGovern, ME, Krishna, A, Aguayo, VM, and Subramanian, SV. A review of the evidence linking child stunting to economic outcomes. Int J Epidemiol. (2017) 46:1171–91. doi: 10.1093/ije/dyx017
Keywords: underweight, factors, children, low, lower middle, income, Africa
Citation: Tamir TT, Zegeye AF, Workneh BS and Mekonen EG (2024) Underweight and associated factors among children under age of five in low and lower-middle income African countries: hierarchical analysis of demographic and health survey data. Front. Public Health. 12:1423603. doi: 10.3389/fpubh.2024.1423603
Edited by:
Sajid Bashir Soofi, Aga Khan University, PakistanReviewed by:
Tanvi Kiran, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaMarta Cristina Sanabria, National University of Asunción, Paraguay
Copyright © 2024 Tamir, Zegeye, Workneh and Mekonen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tadesse Tarik Tamir, dGFkZXN0YXIxNDBAZ21haWwuY29t
 Tadesse Tarik Tamir
Tadesse Tarik Tamir Alebachew Ferede Zegeye
Alebachew Ferede Zegeye Belayneh Shetie Workneh
Belayneh Shetie Workneh Enyew Getaneh Mekonen
Enyew Getaneh Mekonen