- 1Hirosaki University, Radiation Emergency Medicine and Cooperation Promotion, Education Center for Disaster and Radiation Emergency Medicine, Hirosaki, Japan
- 2Advance Emergency and Critical Care Center, Hirosaki University Hospital, Hirosaki, Japan
- 3Graduate School of Health Sciences, Hirosaki University, Hirosaki, Japan
Since the Fukushima Daiichi Nuclear Power Plant accident in Japan, there has been a growing demand for radiological technologists to play active roles in radiation emergency medicine. This study administered a questionnaire survey to determine radiological technologists’ experience, interest, and confidence in disaster medicine and radiation emergency medicine as well as their educational needs, particularly regarding radiation emergency medicine. Findings showed that less than 10% of radiological technologists working at nuclear emergency core hospitals and nuclear emergency medical cooperative institutions for nuclear disaster medical care had studied disaster medicine, regardless of their affiliation, age, or years of service, and that they lacked educational experience. However, they showed interest in general disasters and emergency medicine, and all aspects necessary for the treatment of injured and sick patients in nuclear disasters, such as dosimetry and radiation control, and were willing to learn through online formats, such as e-learning, to expand their learning opportunities. This research seeks to promote a positive perception of disaster and radiation emergency medical education among radiological technologists.
1 Introduction
In March 2011, the Fukushima Daiichi Nuclear Power Plant (FDNPP) accident occurred in Japan following the Tohoku Pacific Ocean Earthquake. At the FDNPP, the earthquake and tsunami caused a loss of power supply, resulting in the meltdown of the reactor core, which lost its cooling function, and the release of a large amount of radionuclides from the reactor buildings (1, 2). Several medical facilities existed in the area where the evacuation order was issued; however, owing to the loss of core infrastructure and lifelines caused by the earthquake combined with the release of radionuclides, they were unable to fully perform their functions (1, 2). The release of radionuclides led to the evacuation of hospitals and older adult care facilities, placing a tremendous physical and psychological burden on evacuees due to the repeated expansion of evacuation zones and difficulties in receiving evacuees at evacuation centers (3). The medical system at the time did not anticipate that a large number of injured and sick people who may have been contaminated by radionuclides or exposed to radiation may overwhelm the healthcare system, suggesting that cooperation among related organizations was an issue in dealing with the large number of injured and sick people (4, 5).
These accidents and cases led the Japan Nuclear Regulation Authority to implement the Nuclear Emergency Response Guidelines in October 2012, and in 2015, the nuclear disaster medical care system was considerably revised to establish the current radiation emergency medical care system (6–8). At present, 24 local governments that own or are adjacent to nuclear power plants are in the process of designating “nuclear emergency core hospitals (NECH)” and “nuclear emergency medical cooperative institutions (NEMCI),” which will play a pivotal role in receiving contaminated/exposed injured patients. Furthermore, the NECH is required to have a “nuclear emergency medical assistance team (NEMAT)” to provide assistance to disaster-stricken areas in the event of a nuclear disaster. In addition to medical doctors and nurses, radiological technologists (RT) are required to register with NEMAT (9, 10).
Let us now focus on the roles and education of RT in Japan. In Japan, RTs are users of diagnostic imaging and radiation therapy equipment in clinical practice. They are also responsible for radiation safety management in each hospital. However, in nuclear disasters, in addition to knowledge of emergency medicine, knowledge of radiation protection, prevention of the spread of contamination, decontamination, and dosimetry is essential when managing patients with exposure/contaminated injuries. In addition, knowledge of disaster medicine is necessary to establish a system for dispatching or receiving support as a NEMAT. The International Atomic Energy Agency publication “Guidance for medical physicists responding to a nuclear or radiological emergency,” published in 2020, provides guidelines for professionals in the medical physics field to respond to a nuclear/radiological emergency (11). The guidelines state that it is important that national and regional plans for radiological emergencies in each country clearly define the roles and activities to be performed by medical physics specialists. Medical physics specialists, which in Japan primarily means RTs, suggests the importance of planning and education for the utilization of these very professionals in the event of a radiological emergency. However, RT training schools in Japan do not provide opportunities to learn emergency/disaster medicine as part of their pre-graduation education. It is only after the RTs are employed by medical institutions related to nuclear disasters that they learn emergency/disaster medicine related to radiation emergency medicine (REM), making the optimization of education a challenge (12). Thus, there is an urgent need to train RTs in emergency and disaster medicine in addition to radiation protection, and dosimetry.
This study investigated the current challenges and educational needs of RTs for REM education, including the extent to which RTs working for NECH and NEMCI were interested in emergency and disaster medicine related to REM as well as their learning history and confidence. Next, we analyzed the results, summarized the knowledge required for RT to be involved in REM, and offered recommendations that will contribute to the development of future educational materials.
2 Methods
2.1 Survey participants and period
RTs (n = 167) affiliated with 15 medical institutions in the Aomori Prefecture designated as NECH or NEMCI as of August 2023 were surveyed using a self-administered questionnaire regarding basic attributes and demand for REM education. The Aomori Prefecture was selected because it was the first local government in Japan to progressively designate an NECH, and the local government had permission to do so. To increase the collection rate, responses could be submitted by mail or online.
2.2 Questionnaire survey items
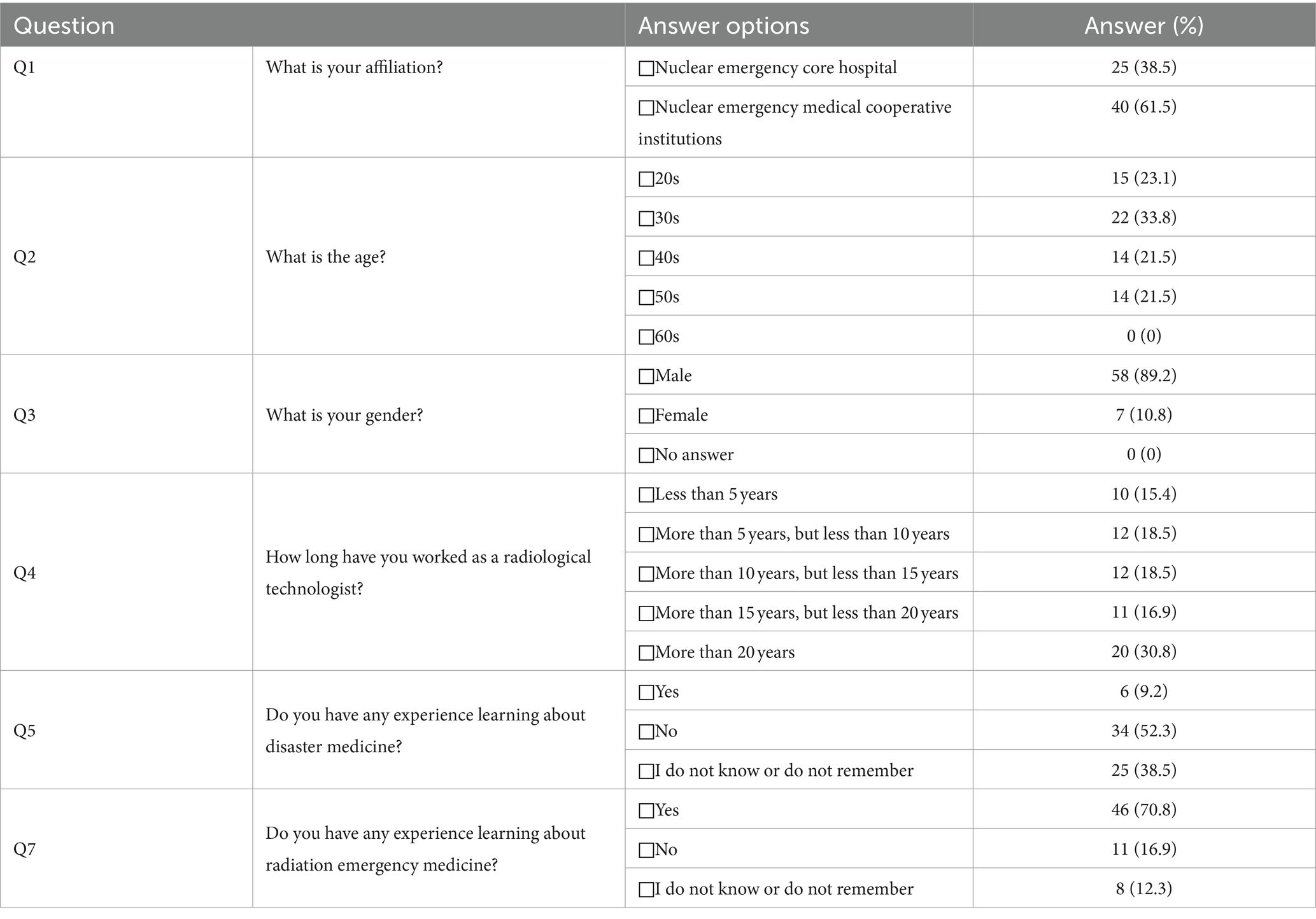
The questionnaire survey comprised 13 questions in total of which 8 questions were related to the basic attributes of the participants while 5 questions pertained to disaster medicine and REM. The response method was either multiple-choice, multiple-response, or open-ended, depending on the item (Table 1). The questions were developed by a group of experts consisting of medical doctors, nurses and radiological technicians who have been involved in the education of NEMAT.
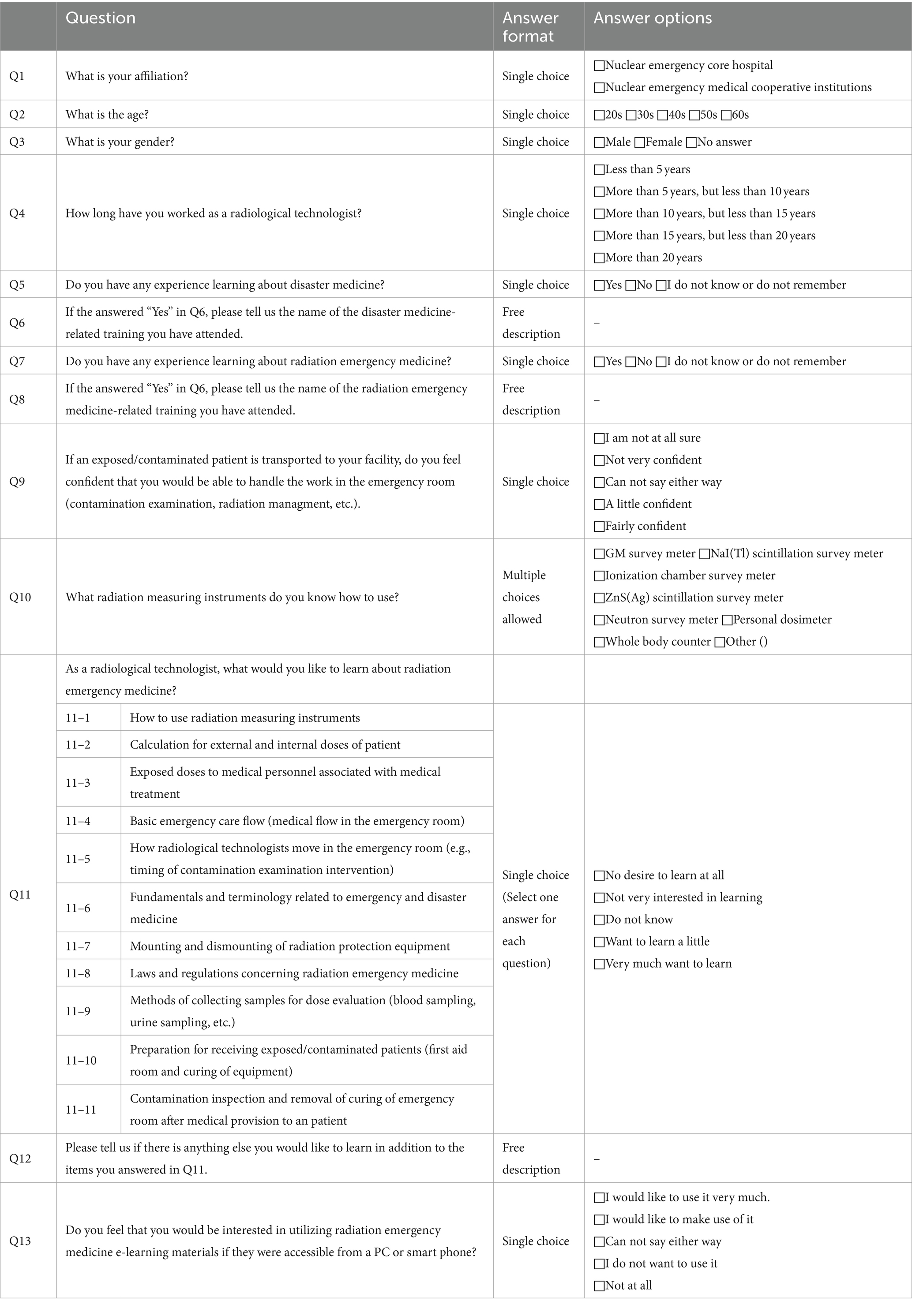
Table 1. Questions for radiological technologists regarding disaster medicine and radiation emergency medicine.
2.3 Statistical analysis
Fisher’s exact probability test was used to analyze the correlations between the data obtained from the questionnaire and to examine RTs’ interest in disaster medicine and REM. OriginPro 2020 (OriginLab) was used for the statistical analysis.
2.4 Ethical consideration
The target medical institutions and participants were informed of the purpose of the survey, the voluntary nature of responses, protection of privacy, and anonymity in writing or by email before the survey was conducted. The name of the institution was left blank when responding to the questionnaire, and consent to participate in this study was assumed to have been obtained upon submission of the questionnaire. This study was approved by the Ethics Committee of Hirosaki University Graduate School of Health Sciences (approval number: 2020–018).
3 Results
3.1 Questionnaire survey response rates and analysis of the basic attributes of participants
A questionnaire survey of 167 RTs affiliated with hospitals in Aomori Prefecture, designated as NECH and NEMCI, regarding their REM needs, resulted in 65 valid questionnaires (40.1% response rate). The results for the basic attributes of Q1–Q8 are listed in Table 2. Characteristically, even the RTs affiliated with NECH and NEMCI had few participants (9.2% of the total), indicating that they had learned about disaster medicine. Participants who reported that they had a history of learning about disaster medicine had attended the Japan Disaster Medical Assistance Team training, and none of the RTs stated that they had learned about disaster medicine in their pre-graduate education (analyzed from the free-field responses to Q6). Next, 70.8% of respondents had a history of learning about REM. In terms of the specific courses taken, all participants indicated that they had attended one of the nuclear disaster medical care training courses systematized under the leadership of the Japan Nuclear Regulation Authority after the FDNPP accident (excerpt from the free-field responses to Q8). No RTs responded that they had received REM training or disaster medical education before graduation. Incidentally, although we examined whether any differences existed due to affiliation, age, and educational attendance, no items showed significant differences (no significant differences were found when independence tests were conducted on Q1 vs. Q5/Q7 and Q2 vs. Q5/Q7).
3.2 RTs’ confidence, interest, and concern in disaster medicine and REM
In providing medical care to exposed or contaminated patients in the emergency room, RTs must contribute to contamination testing and radiation safety management. When asked if they were confident in their ability to provide appropriate interventions to the target population, 23 (35.3%) responded “very confident” or “confident” (results from Q9, partially shown in Table 3). When asked whether they were confident in their ability to use the radiation measuring instruments considered necessary to inspect the contamination of exposed/contaminated casualties and measure air dose rates when providing REM, 64 (98.5%), 63 (96.9%), and 62 (95.4%) respondents indicated that they understood how to use the Geiger-Mueller survey meters, NaI(Tl) scintillation survey meters, and pocket dosimeters, respectively. However, none of the participants could use large equipment, such as liquid scintillation counters and germanium semiconductor detectors, for external/internal exposure dose assessment using specimens from injured or sick people (Q10 results, no data posted as figures or tables). Q11 comprised 11 questions about the content of REM learning, which is considered necessary for RTs. Around 87.0% of the respondents said that they “want to learn a little” or “very much want to learn” for all items (data not shown in the chart). When asked in Q12 about additional items that they would like to learn, participants’ free-field responses indicated that they would like to learn about not only radiation control but also disaster medicine in general, such as “general knowledge necessary to work as a NEMAT” and “management of information in a disaster.” As there were no e-learning tools for RTs to learn about contamination examination techniques and radiation safety management, we asked the respondents about their expectations for such a learning format in Q13. A total of 45 (69.2%) participants responded that they would “very much like to utilize” such a tool, 13 (20.0%) responded that they “would like to utilize” such a tool, and 7 (10.8%) responded that they were “undecided.” None of the respondents answered that they did not want to use the e-learning tool (the results for Q13 are partially shown in Table 4).
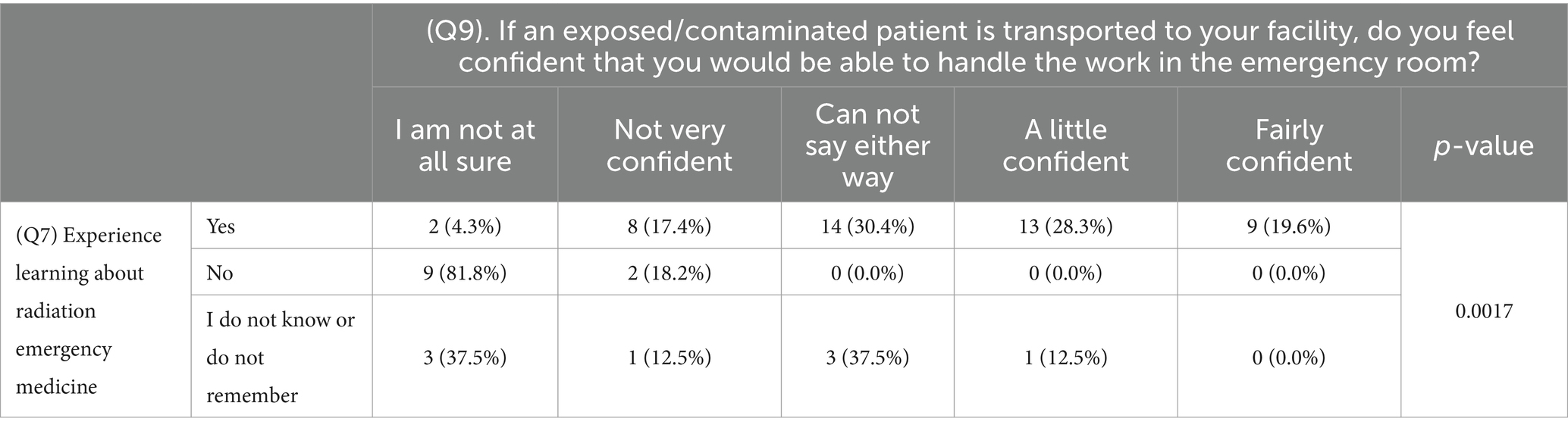
Table 3. Results of independence tests: experience of radiation emergency medicine education vs. intervene in radiation emergency medicine.
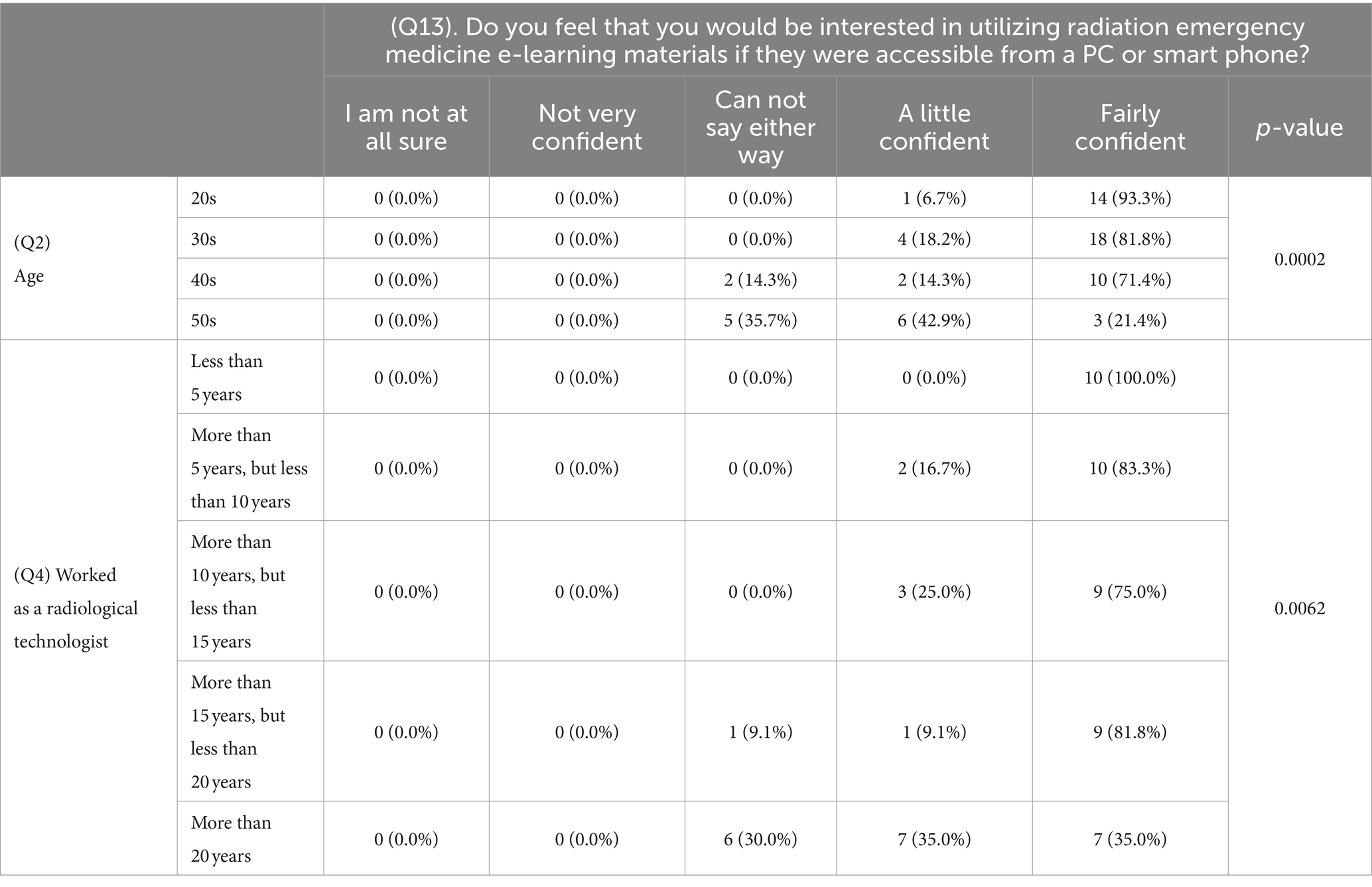
Table 4. Results of independence tests: age/period of employment vs. interest in e-learning materials.
3.3 Results of the independence test
Independence tests were conducted to examine the association between basic attributes and confidence, interest, interest in disaster medicine, and REM. Fisher tests were conducted for all 78 combinations of the 6 basic attributes (Q1, Q2, Q3, Q4, Q5, and Q7) and 13 questions on disaster medicine/REM (Q9, Q11-1, Q11-2, Q11-3, Q11-4, Q11-5, Q11-6, Q11-7, Q11-8, Q11-9, Q11-10, Q11-11, and Q13). Significant differences were observed for the following three combinations.
i. Q7 vs. Q9
ii. Q2 vs. Q13
iii. Q4 vs. Q13
No significant differences were identified for the combinations other than those listed above. The specific results for (i) are presented in Table 3 while those for (ii) and (iii) are shown in Table 4. An association between the groups was confirmed (p < 0.01).
4 Discussion
In this study, we evaluated the interest of RTs in disaster medicine and REM, as they are key personnel in the treatment of exposed/contaminated patients during a nuclear disaster and in providing support to affected areas as NEMATs. It should be noted that this is the first survey of RTs affiliated with NECH and NEMCI, and this is the first effort to set up the questions.
The NECH and NEMCI are medical institutions that are deeply involved in medical treatment and support during nuclear disasters and were designated in each region of Japan after the FDNPP accident. Therefore, the questionnaire survey was limited to RTs affiliated with these medical institutions. Although medical institutions located near nuclear facilities should have basic knowledge of the characteristics of nuclear disasters and radiation regardless of the type of job, the purpose of this study was to investigate RTs’ interest and educational needs in terms of medical treatment and dispatch/support to narrow the focus of the study. To receive the NEMCI designation, a nuclear disaster medical cooperation organization must fulfill one or more of the seven roles specified by the Japan Nuclear Regulation Authority and not necessarily treat exposed/contaminated patients or have an NEMAT (13, 14). Therefore, we assumed that NECH RTs were more likely than NEMCI RTs to have attended trainings related to disaster and exposure medicine, but as noted in Section 3–1, no significant difference was actually found. This result may indicate that RTs have few opportunities to learn about disaster medicine; however, REM education for RTs at NECH and NEMCI has been progressing since the FDNPP accident. The role of RTs in the event of a nuclear disaster is not limited to radiation control but rather covers a wide range of matters related to disaster medicine in general, and there is a need to train RTs on disaster medicine (15).
The results in Table 3 show the correlation between confidence in interventions related to the medical treatment of exposed/contaminated patients and REM educational experiences. The specific figures reveal that no RTs had never received REM education or were unaware about it and who also answered that they were highly confident in their intervention. Thus, the results are easily understandable and show that education and training can lead to confidence in intervention in clinical practice. Recently, in light of the COVID-19 pandemic, there have been several reports in the field of REM of the use of virtual reality (VR) technology to provide teaching materials for experiencing contamination testing as well as the creation of e-learning courses that can be delivered through videos or online (16, 17). The educational effectiveness of these VR and e-learning materials was examined. Findings revealed that using the latest tools may lead to increased interest in and RT confidence in REM. Furthermore, the results in Table 4 show a correlation among interest in e-learning materials, age, and employment duration. The figures show that people of all ages and employment durations have a high level of interest in e-learning materials. This suggests that even in the field of REM, cutting-edge educational devices are gradually becoming more widely accepted. Respondents showed a wide range of interest in not only radiation-related participants, such as radiation management and dose assessment, but also basic subjects in emergency and disaster medicine, indicating that RTs working at NECH and NEMCI have a strong desire to improve themselves.
In Japan, regulations governing the content of RT education are implemented by the Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labour and Welfare (18). Unfortunately, current training rules for RTs do not include terms, such as emergency medicine, disaster medicine, or REM. Based on the study findings, it can be seen that RTs working at medical institutions designated by local governments that own nuclear-related facilities show a high interest in areas, such as emergency care, disasters, and REM. Furthermore, emergency situations, such as nuclear terrorism and accidents caused by isotopes or radiation-generating devices, should be covered in medical student education. Additionally, many reports indicate that postgraduate education for working adults on REM has been improving in recent years (7, 10). Specific educational proposals include: (i) incorporate disaster medicine and radiation exposure medicine education into RT pre-graduate education, and (ii) include specific educational topics such as medical treatment of exposed/contaminated injured patients and physical biology related to dosimetry, not to mention how to use radiation measuring instruments. It should be noted that this is a self-administered survey of a small portion of Japan, but these findings contribute to the literature on disaster medicine, particularly with regard to the critical gaps in existing knowledge about RT education.
5 Conclusion
In conclusion, this study highlights the urgent need for enhanced education and training for radiological technologists (RTs) in disaster and radiation emergency medicine (REM) in Japan. Although RTs affiliated with nuclear emergency core hospitals (NECH) and nuclear emergency medical cooperative institutions (NEMCI) showed significant interest in REM, their pre-graduate education lacks sufficient coverage of disaster medicine. The findings underscore the importance of incorporating REM into RTs’ education and utilizing modern tools, such as e-learning and virtual reality, to improve their preparedness and confidence in managing nuclear or radiological emergencies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Hirosaki University Graduate School of Health Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. MN: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. TK: Conceptualization, Data curation, Investigation, Methodology, Project administration, Validation, Writing – review & editing. KY: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – review & editing. KI: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by JSPS KAKENHI Grant Numbers 22K16621 and 22K10409.
Acknowledgments
We are grateful to the RTs in Aomori prefecture who participated in the questionnaire survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ohtsuru, A, Tanigawa, K, Kumagai, A, Niwa, O, Takamura, N, Midorikawa, S, et al. Nuclear disasters and health: lessons learned, challenges, and proposals. Lancet. (2015) 386:489–97. doi: 10.1016/S0140-6736(15)60994-1
2. Hasegawa, A, Tanigawa, K, Ohtsuru, A, Yabe, H, Maeda, M, Shigemura, J, et al. Health effects of radiation and other health problems in the aftermath of nuclear accidents, with an emphasis on Fukushima. Lancet. (2015) 386:479–88. doi: 10.1016/S0140-6736(15)61106-0
3. Yanagawa, Y, Miyawaki, H, Shimada, J, Morino, K, Satoh, E, Ohtomo, Y, et al. Medical evacuation of patients to other hospitals due to the Fukushima I nuclear accidents. Prehosp Disaster Med. (2011) 26:391–3. doi: 10.1017/S1049023X11006418
4. Morimura, N, Asari, Y, Yamaguchi, Y, Asanuma, K, Tase, C, Sakamoto, T, et al. Emergency/disaster medical support in the restoration project for the Fukushima nuclear power plant accident. Emerg Med J. (2013) 30:997–1002. doi: 10.1136/emermed-2012-201629
5. Meineke, V, and Dörr, H. The Fukushima radiation accident: consequences for radiation accident medical management. Health Phys. (2012) 103:217–20. doi: 10.1097/HP.0b013e31825b5809
6. Tsujiguchi, T, Sakamoto, M, Koiwa, T, Suzuki, Y, Ogura, K, Ito, K, et al. A simple survey of the preparation situation for Resident's evacuation in Japanese prefectures after the Fukushima Daiichi nuclear power plant accident. Front Public Health. (2020) 8:496716. doi: 10.3389/fpubh.2020.496716
7. Tatsuzaki, H, Kumagai, A, Fuma, S, and Yamashita, S. Reorganization of advanced radiation emergency medicine systems in Japan after the Fukushima nuclear power plant accident. Environ Adv. (2022) 8:100197. doi: 10.1016/j.envadv.2022.100197
8. Nagata, T, Arishima, T, Yamaguchi, Y, Hirohashi, N, Usa, T, Hasegawa, A, et al. Radiation emergency medical preparedness in Japan: a survey of nuclear emergency Core hospitals. Disaster Med Public Health Prep. (2022) 17:e78. doi: 10.1017/dmp.2021.348
9. Iyama, K, Kakamu, T, Yamashita, K, Shimada, J, Tasaki, O, and Hasegawa, A. Current situation survey for establishing personally acceptable radiation dose limits for nuclear disaster responders. J Radiat Res. (2022) 63:615–9. doi: 10.1093/jrr/rrac026
10. Tsujiguchi, T, Yamaguchi, M, Mikami, J, Sato, D, Itaki, C, Hosokawa, Y, et al. Survey on training of the nuclear emergency medical assistance team and their educational needs. Radiat Environ Med. (2019) 8:16–20. doi: 10.51083/radiatenvironmed.8.1_16
11. International Atomic Energy Agency (IAEA). Guidance for medical physicists responding to a nuclear or radiological emergency. EPR-medical physicists. Vienna: IAEA (2020).
12. Ohba, T, Mabune, K, Kanno, S, and Hasegawa, A. Recommendations for optimising a human resource development training programme for a nuclear accident based on the personal backgrounds of radiological technologists: experiences from the Fukushima Daiichi nuclear power station accident. Nihon Hoshasen Gijutsu Gakkai Zasshi. (2022) 78:1282–94. doi: 10.6009/jjrt.2022-1307
13. Japan Nuclear Regulation Authority. (2023). Available at:https://www.nra.go.jp/data/000359967.pdf. Accessed July 12, 2024
14. Japan Nuclear Regulation Authority. (2022). Available at:https://www.nra.go.jp/data/000119566.pdf. Accessed July 12, 2024
15. Yashima, S, and Chida, K. Effective risk communications through personalized consultations with pregnant women and parents by radiologic technologists after the 2011 Fukushima Daiichi nuclear disaster. Tohoku J Exp Med. (2022) 256:259–69. doi: 10.1620/tjem.2022.J001
16. Tomisawa, T, Hosokawa, S, Kudo, H, Osanai, M, Ota, K, In, N, et al. Are online simulations for radiation emergency medical preparedness less effective in teaching than face-to-face simulations? Disaster Med Public Health Prep. (2023) 17:e520. doi: 10.1017/dmp.2023.188
17. Tsujiguchi, T, Yamanouchi, K, and Kashiwakura, I. Developing an educational program to help students learn about the resident evacuation protocols and contamination inspection undertaken during nuclear disasters. Jpn J Health Phys. (2019) 54:129–34. doi: 10.5453/jhps.54.129
18. Japan Ministry of Health, Labour and Welfare. (2022). Available at:https://www.mhlw.go.jp/content/10801000/000566738.pdf. Accessed July 12, 2024
Keywords: radiological technologist, disaster medicine, radiation emergency medicine, medical education, nuclear disaster medical care
Citation: Tsujiguchi T, Naraoka M, Koiwa T, Yamanouchi K and Ito K (2024) Japanese radiological technologists’ perceptions and interest in disaster medicine and radiation emergency medicine. Front. Public Health. 12:1463583. doi: 10.3389/fpubh.2024.1463583
Edited by:
Nagesh Bhat, Bhabha Atomic Research Centre (BARC), IndiaReviewed by:
Adela Salame-Alfie, NuRaC LLC, United StatesEman Alshaikh, Beth Israel Deaconess Medical Center and Harvard Medical School, United States
Copyright © 2024 Tsujiguchi, Naraoka, Koiwa, Yamanouchi and Ito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katsuhiro Ito, aXRvaGtjY2tAbmlmdHkuY29t
 Takakiyo Tsujiguchi
Takakiyo Tsujiguchi Masato Naraoka
Masato Naraoka Tomoki Koiwa3
Tomoki Koiwa3 Kanako Yamanouchi
Kanako Yamanouchi