- 1Medical School, University of Cyprus, Nicosia, Cyprus
- 2Department of Clinical Sciences and Psychiatry, Umeå University, Umeå, Sweden
Background: Genetic testing in psychiatry has gained attention, raising questions about its application and impact. Understanding stakeholders’ perspectives, including healthcare providers and patients, is vital for informed policy development. The aim of this systematic review was to focus on the perceptions and concerns of patients and healthcare workers in psychiatry regarding the use of genetic testing.
Methods: We conducted a systematic review following PRISMA guidelines, for the period 1/2/2014, to 1/1/2024, via PubMed and Embase databases identifying 50 articles in total. After excluding duplicates (n = 12), 38 articles went through screening. After careful full-text article assessment for eligibility and applying the inclusion and exclusion criteria, only fifteen (n = 15) of the articles were included.
Results: Among 15 selected studies involving 3,156 participants (2,347 healthcare professionals; 809 patients), thematic analysis identified four primary themes: Organizational-implementation concerns, Ethical Considerations, Concerns on changes in clinical praxis, and Legal implications. Despite these concerns, seven out of eleven studies indicated that healthcare workers viewed genetic testing in psychiatry positively. Patients’ perspectives varied, with two of the four studies reflecting positive attitudes. No pervasive negative sentiment was observed.
Conclusion: Our review highlights the multidimensional perspectives of healthcare professionals and patients surrounding the application of genetic testing in psychiatry. These considerations need to be addressed to facilitate the implementation of genetic testing in clinical praxis in psychiatry. Further research is needed for validation of the results and to guide policies and clinicians in the integration of genetic testing into mental healthcare practice.
Introduction
Modern medicine is constantly improving its tools and modernizing its methods to be able to provide patients with the most effective and personalized treatment and genetic testing is in the frontline of precision medicine. The Center for Disease Control and Prevention, defines “genetic testing” as the process of scanning a person’s genetic sequence in search of alterations (mutations, variants) in DNA that may have clinical relevance (1).
A variety of clinical conditions in different fields of medicine are associated with genetic abnormalities and genetic testing is gaining ground in clinical praxis in different specialties (2–4). Genetic testing helps to identify the genetic component of some disorders, can be used in diagnosis, to guide treatment and for genetic counseling of the patient’s relatives. Additionally, monitoring of genetic markers during treatment can guide clinicians adjust treatment plans according to one’s genetic variations (5).
Psychiatry is a promising field for the application of genetic testing as, in comparison with other medical specialties, is still well behind in identifying biomarkers for diagnosis, prognosis and treatment response. However, epidemiological and genetic studies have shown a strong association between certain genetic alterations and psychiatric diseases, with expanding research in genetic causality and familial inheritance models (6). Due to the high prevalence of psychiatric disorders attributable to genetic alterations, the medical community has increased its interest in researching the genetic etiology of these disorders through genetic testing and familial risk classification (7). Considering the major impact of psychiatric diseases on society, investigation from such a revolutionary perspective could be crucial (8–11).
Psychiatric genetic testing can be helpful in unraveling the pathophysiology of common mental disorders such as schizophrenia, depression, bipolar disorders, and autism spectrum disorder. For instance, in schizophrenia, genetic testing examines variations in genes impacting functions like brain development, neurotransmission, and immune homeostasis (12). Information derived from genetic testing can be used as predictors and thus enable early interventions and empower individuals to make informed decisions about their health. Overall, psychiatric genetic testing serves as a crucial advancement in addressing complex psychiatric disorders and enhancing personalized healthcare strategies (13).
In addition to Mendelian models, genes-diseases correlation, and prenatal screening for genotypic abnormalities, the application of pharmacogenomics is increasing. Pharmacogenomics can revolutionize drug prescribing through tailoring treatments to each genetic profile, optimizing efficacy and minimizing unfavorable outcomes (14). It can reduce the trial-and-error period of treatment and provide actionable information in special populations (15). Variations in metabolic enzymes, including cytochrome P450 and especially within the CYP2D6 enzyme can impact the metabolism of antipsychotics and antidepressants, affecting treatment response. The use of diagnostic genetic tests remains relatively rare in current clinical practice, largely due to the complex polygenic nature of psychiatric disorders, which complicates direct genetic diagnosis (16). In contrast, pharmacogenomic tests are used more often, can help tailor medication, with growing evidence suggesting that they can improve both the tolerability and effectiveness of treatment. This has been shown in randomized clinical trials, systematic reviews and meta-analyses especially in managing mood disorders and schizophrenia (17–24). Thus, this distinction between the two test types is crucial, as their roles in psychiatric practice differs significantly.
Although there is increasing utility of genetic testing in medicine, the existing literature on the perceptions of healthcare professionals and patients regarding this practice is still growing. Initial studies report skepticism from both the medical community and patients regarding the efficacy and utility of these tests, and ethical concerns have been raised related to privacy, security of patient data, confidentiality, economic impact and possible harms such as psychological impact, stigmatization and discrimination (25, 26). Preliminary studies reported that the type of genetic condition can influence the mental health of patients when genetic testing is applied, with neurodegenerating disorders such as Huntington’s disease having a profound impact (27).
At present, there is a lack of comprehensive studies on the perspectives of healthcare professionals and patients regarding the utilization of genetic tests in psychiatry. Given the stigma often associated with psychiatric disorders and the vulnerability of psychiatric patients, it is important to investigate the perspectives of those directly involved. Additional concerns might include the capacity of psychiatric patients and their relatives to consent to genetic testing and whether they understand the implications and possible benefits. Also, questions arise about the necessity of such tests in severely mentally ill patients and the usefulness of the results (28). Therefore, the identification of perceptions of healthcare professionals and patients has important implications in the application of genetic testing in psychiatric clinical praxis.
Thus, the aim of this systematic review was to identify, categorize and discuss the perceptions, opinions and concerns of patients and healthcare workers in psychiatry regarding the use of genetic testing.
Materials and methods
The systematic review was based on the Preferred Reporting Items for Systematic reviews and Meta-Analysis statement (Prisma) guidelines (29).
Data sources and searches
The research of the medical literature was executed in PubMed and Embase and was confined to the preceding decade encompassing the timeframe of 1/12014 to 1/1/2024. The selection of this research timeframe was based on the recognition that while genetic testing in psychiatric applications had been apparent earlier, more advanced applications including pharmacogenetics, were developed in recent years (30). Published articles were collected using a standard search strategy search query: (“Genetic testing” OR “Genetic screening” OR “Molecular diagnostics”) AND (“Psychiatry” OR “Mental health” OR “Psychiatric disorders” OR “Mental illness”) AND (“Perceptions” OR “Attitudes” OR “Beliefs” OR “Opinions”) AND (“Healthcare workers” OR “Clinicians” OR “Healthcare professionals” OR “Medical staff”) AND (“Patients” OR “Individuals” OR “Participants” OR “Subjects”).
Study selection
This systematic overview encompassed articles that investigated the attitudes, perspectives, beliefs, and views of healthcare providers and patients concerning genetic testing in psychiatry. Research articles on Alzheimer’s disease (n = 2) were excluded due to the primary characteristics of this disease including memory and cognitive dysfunctions. Νo other exclusion criteria referring to gender, age, or ethnicity have been applied. Only articles written in English were considered for inclusion. The PRISMA 2009 checklist guided any similarly restrictions that were imposed on the articles.
Data extraction, study quality assessment and analysis
The systematic search resulted in the identification of 50 articles in total. Out of the 50 articles, 12 were excluded as duplicates resulting in 38 articles for further screening. After careful full-text article assessment for eligibility and applying the inclusion and exclusion criteria, only 20 (n = 20) of the articles were deemed eligible to be further assessed in full study. Three (n = 3) articles were excluded as identified as a review while two (n = 2) more articles were excluded as being out of the scope of this systematic review since they did not include opinions or beliefs for genetic testing in psychiatry but in another specialties. All the references of the identified review articles were also checked for eligibility. Thus, finally, 15 studies reporting on the patients’ and healthcare provider’s perspectives regarding genetic testing in psychiatry were included. The Prisma Flowchart for exclusion/inclusion criteria is presented in Supplementary Figure S1.
All included studies were thematically analyzed for identifying themes related to genetic testing in psychiatry. The thematic analysis was performed separately on healthcare professionals and patients’ opinion/perspectives regarding the topic. Data were retrieved from each study and classified through thematic analysis first in subthemes and subsequently into the different themes.
Results
Studies characteristics
The studies included (n = 15) had a total population of 3,156 participants including 2,347 healthcare professionals and 809 patients. The studies were carried out in diverse locations, most common the United States (n = 8). The mental healthcare professionals included were psychiatrists, psychiatric pharmacists, child and adolescent psychiatrists, psychiatric genetics researchers and general practitioners working in mental health clinics. The patients included in the studies suffered from depression, bipolar disorder, schizophrenia, and patients receiving treatment for a mental health condition. The studies are shown in Table 1.
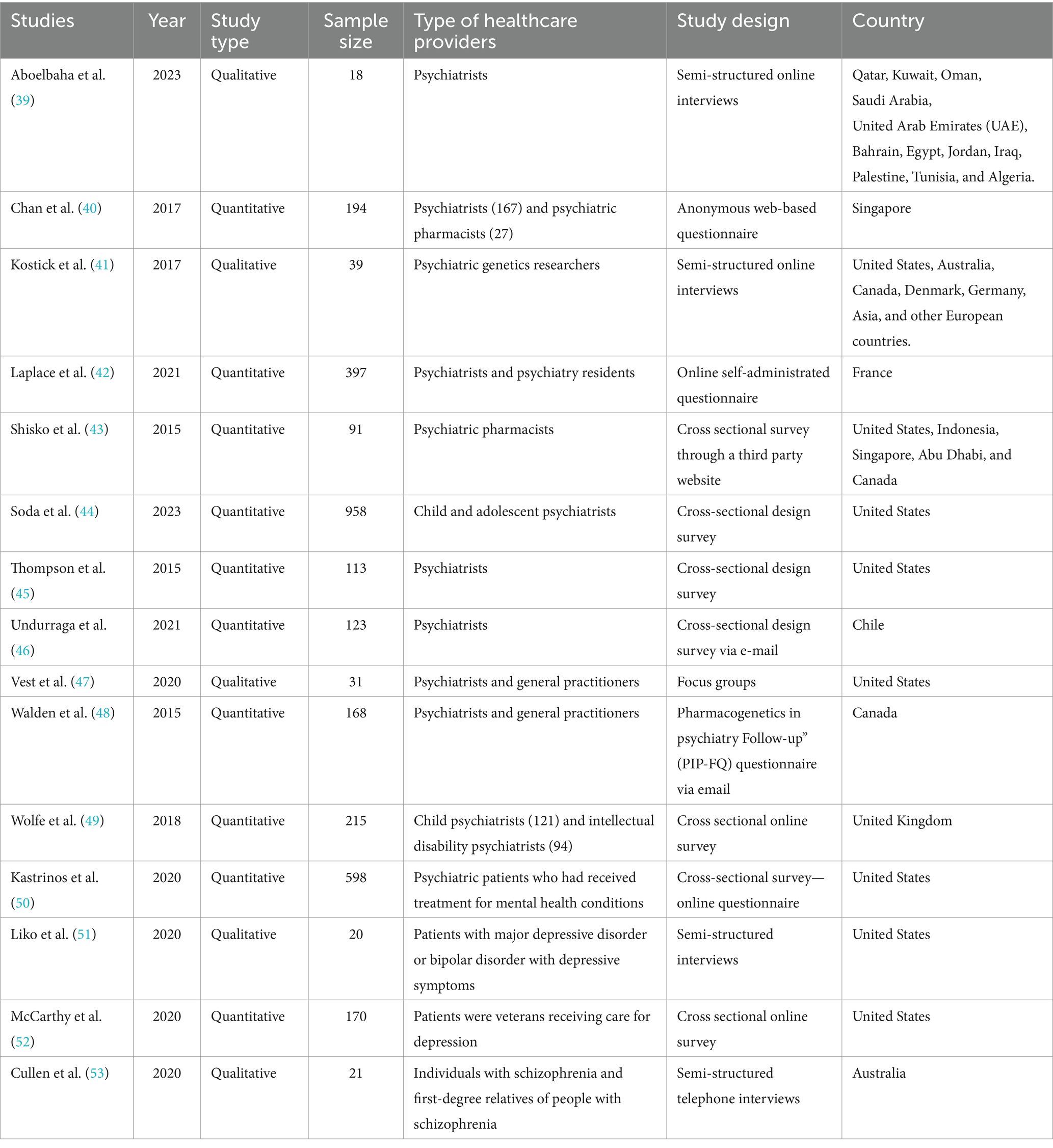
Table 1. Studies including perspectives of mental health providers (n = 2,347) and patients’ perspectives.
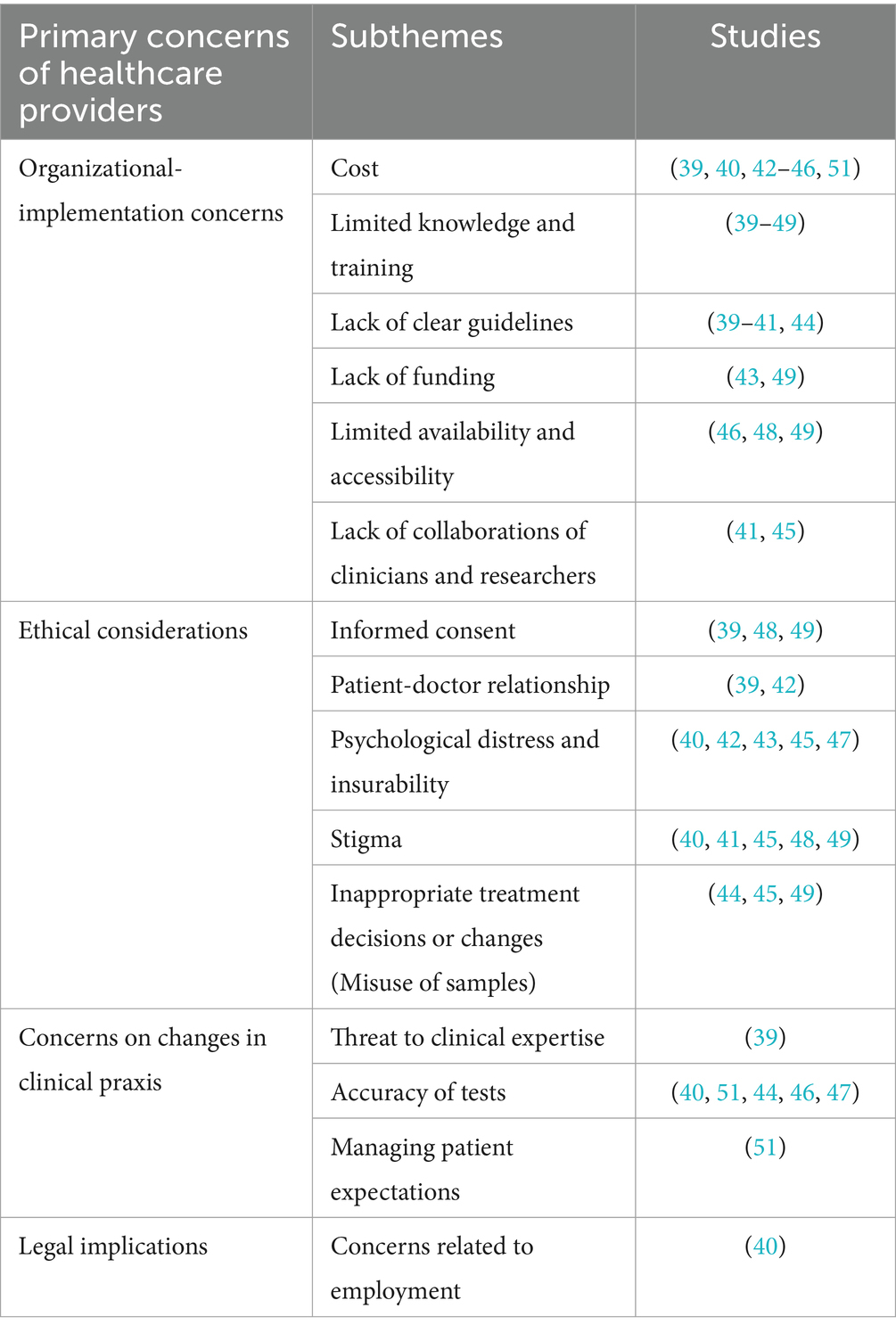
Healthcare professionals’ perspectives on genetic testing in psychiatry
Four themes and fifteen subthemes were identified, the most common theme was Organizational-Implementation concerns, including six subthemes: cost, limited knowledge and training, lack of clear guidelines, lack of funding, limited availability and accessibility, and lack of collaborations among clinicians and researchers. The second theme, Ethical Considerations, encompasses subthemes such as informed consent, patient-doctor relationship, psychological distress, stigma, and inappropriate treatment decisions or changes. The third theme, Concerns on changes in clinical praxis, includes three subthemes: threat to clinical expertise, accuracy of tests, and managing patient expectations. The final theme, Legal Implications, includes concerns related to employment.
All themes, subthemes, and studies identifying them are shown in Table 2.
Patients’ perspectives on genetic testing in psychiatry
Four main categories, with a total of 11 subcategories were identified. These primary categories mirror those identified in the case of healthcare professionals including organizational-implementation concerns, ethical considerations, implications for clinical practice, and legal implications. A more comprehensive overview of the themes observed in each individual study is presented in Supplementary Table S1.
What was the general sentiment among healthcare providers and patients?
Out of the eleven (n = 11) studies where mental health providers were involved, seven (n = 7) studies suggested that the consensus among psychiatry professionals was that genetic testing is a valuable tool in psychiatry. However, in four (n = 4) studies, mental health professionals have expressed mixed perspectives on the matter.
Regarding the patients’ perspective, positive opinions regarding genetic tests in psychiatry were expressed, in two (n = 2) studies, while in two (n = 2) studies, patients had mixed perspectives. It is important to note that among the studies included in this systematic review, there was no indication of a general negative opinion regarding genetic tests among healthcare providers in psychiatry and psychiatric patients.
Discussion
To our knowledge, this is the first systematic review to investigate the perspectives of patients and healthcare workers associated with genetic testing in psychiatry with the findings contributing to a deeper understanding of the utilization of genetic testing in psychiatry and shed light on ethical considerations and potential risks from various perspectives. The theme that was most frequently identified was the concerns expressed by professionals regarding the limited education, training, and professional experience on genetic testing and genetic information. Indeed, although genetic testing and counseling have many applications in medicine, are still not included as part of the fundamental curriculum in the majority of medical schools across the world (31). Consequently, this leads to a dearth of professional education and specific training in clinical settings that directly impacts the perspectives of healthcare providers with regards to the utilization of these technologies and techniques in their daily practice. Thus, it is imperative that practitioners receive adequate training to be able to fully utilize newer technologies in clinical praxis such as pharmacogenetic testing (32).
The concern ranking second in frequency among professionals was the cost associated with genetic testing. The cost was deemed a prominent barrier hindering the implementation of pharmacogenomics testing. Physicians expressed concerns regarding the affordability of these tests suggesting that enhancing accessibility and affordability, potentially through the public health sector, would be of utmost importance (33). Given the novelty and innovative nature of genetic counseling applications, it becomes evident that the public health sectors are ill-prepared to handle the demand and coverage for such tests, resulting in an unfortunate situation where patients bear the economic burden and their perspective on genetic testing becomes adversely affected. Especially in the field of Psychiatry with vulnerable patients of often poor socioeconomic status and services underfunded, it is crucial to advocate for cost coverage of new technology. Nevertheless, in order for genetic testing to truly become a routine practice in the field of medicine and to be fully covered by insurance companies or public health sectors, it is imperative that it provides the scientific community with more clear and consistent results, as well as a wider range of applications.
One of the most prevalent concerns among healthcare providers related to the potential mental health stigma experienced by their patients, which, if left unaddressed, could result in discrimination and self-stigmatization for individuals identified as having risk variants. To mitigate the potential negative consequences on participants and their families, clinicians who integrate genetic counseling into their daily practice must actively consider strategies for alleviating such impacts. Furthermore, an extended educational approach targeting both patients and the general public could play a pivotal role in eradicating the stigmatization endured by these patients, as the limited knowledge surrounding genetics has been identified as the primary factor influencing such behavior (34). By equipping individuals with a comprehensive understanding of the genetic components underlying mental health, it becomes possible to combat the stigma associated with it, fostering an environment of inclusivity and support. This comprehensive approach ensures that patients receive the necessary care without facing unnecessary barriers or prejudice stemming from a lack of awareness or understanding.
Special concerns were raised regarding the potential psychological impact of genetic testing in psychiatry. Indeed, it was previously reported that mental health professionals expressed concerns regarding the possible influence of genetic testing on the mental well-being of patients (28). The characteristics of psychiatric disorders affecting the cognitive function of patients, together with the stigma of psychiatric disorders has the risk for increased misunderstandings and negative psychological impact from genetic testing results. In addition, patients may undergo distress regarding their condition, alterations in treatment, or anxiety regarding possible consequences such as employability. Such concerns, subsequently, tend to overshadow the consideration of the delicate equilibrium associated with the “right to know.” As previous studies have suggested, clinicians are confronted with the task of meticulously evaluating the patients’ entitlement to access their genetic information against the potential psychosocial detriments that may emerge from receiving certain outcomes, including heightened stress, anxiety, stigma, and discrimination (14). However, it is reasonable to mention that, to the best of our knowledge, there is currently no evidence supporting a high risk of psychological harm related to genetic testing among psychiatric patients, and previous studies suggest that the severity of psychological risks posed by genetic testing is not substantial (35, 36). At this juncture, further research is necessary to identify specific patient groups, such as individuals with mental health conditions, who may have a heightened susceptibility to psychological harm. It is possible that some patients might assert that knowledge of genetics and genetic testing could dampen the hopes of individuals afflicted with mental disorders. The awareness of patients regarding their genetic predisposition could potentially engender a sense of fatalism or hopelessness regarding their condition.
Alongside the possible psychological impact of genetic testing results, the uncertainty surrounding the outcomes of the tests is also important. Certain patients express worries regarding the efficacy of genetic testing in the event of inconclusive or non-actionable results. In such cases, patients believe that genetic testing would offer limited benefits. It is widely acknowledged that not all genes that can predict the response to psychiatric treatment have been discovered (16). While there is strong evidence and available guidelines for genes associated with drug metabolism, such as CYP2C19 and CYP2D6, as well as other pharmacokinetic implications, the evidence for other genes is still limited (37). This lack of comprehensive identification of genes can potentially hinder the effectiveness of pharmacogenetic testing and raise concerns within the medical community regarding the accuracy and applicability of such tests.
In the context of the two aforementioned concerns, clinicians have a valid and justifiable concern about effectively managing patient expectations. It is imperative to emphasize that pharmacogenetic testing serves as a clinical decision-making instrument utilized by healthcare providers alongside other pertinent factors to facilitate the process of medication selection. It is crucial for healthcare providers to adeptly handle patients’ expectations in terms of acknowledging the limitations of pharmacogenetic testing as well as the varying degrees of evidence associated with the genes being tested (38).
Considering the unique concerns of professionals, psychiatrists expressed concerns regarding an excessive reliance on genetic tests, as it may undermine their clinical expertise and experience. There were concerns that this reliance may replace clinical judgment and impact the patient-doctor rapport, ultimately leading to the dehumanization of the therapeutic alliance and psychiatric care. Furthermore, psychiatrists also expressed worries about the feasibility of incorporating discussions about testing and patient education within the time constraints of routine care visits. Conversely, some professionals believed that genetic testing could streamline the process by identifying the most appropriate medication for each patient, potentially reducing the trial-and-error approach. These varying perspectives among professionals highlight concerns surrounding the actual utility and potentials of genetic counseling.
This study has several limitations. A key limitation of this review is the use of the vote-counting method, which treats all studies equally, regardless of differences in sample size, quality, or bias control. This approach can oversimplify findings, as it does not account for the weight or statistical significance of individual studies, potentially leading to skewed conclusions. Given these limitations, the findings presented should be interpreted cautiously. Future research would benefit from qualitative or meta-analytic approaches to better capture the complexity and variation across studies on genetic testing in psychiatry. As the literature search was conducted in PubMed and Embase only in the English language, possible bias cannot be excluded. Also, the timeframe of the study, including the last decade, might have resulted in missing earlier studies in the subject. However, genetic testing in psychiatry has mainly been used the most recent years. Also, a bias toward healthcare professionals in psychiatry from developed countries, especially USA was evident. As there was a large variation in the methodology of the included studies, including interviews, focus groups, questionnaires and surveys in different patient populations and settings, a meta-analysis was not possible. Finally, as a selection bias cannot be excluded, in combination with the small number of studies, with some themes derived from a small number of studies, the results should be viewed with caution. Although within the studies, the review reached thematic saturation, further research might illuminate new aspects contributing new themes. The relatively emerging nature of this field may have contributed to the lack of research on this topic, thereby limiting the range of insights that could be obtained from existing literature. In this review diagnostic and pharmacogenomic tests were grouped together as a separate analysis was not feasible due to lack of data and data heterogeneity. While both are forms of genetic testing, diagnostic genetic testing is rarely employed due to the complexity of psychiatric disorders, while pharmacogenomic testing has an increasing role in clinical praxis (17–24). Future research should focus more specifically on the evolving evidence surrounding pharmacogenomic testing, which holds greater relevance to current psychiatric practice. Despite these limitations, this study provides valuable insights into the current landscape of attitudes and perceptions toward genetic testing in psychiatry, highlighting the need for further research to address these gaps in understanding.
In conclusion, this review systematically examined the perceptions of healthcare providers and patients regarding genetic testing in psychiatry highlighting concerns, including the limited knowledge, training and the high costs of genetic tests. This study also emphasizes the importance of establishing clear and updated guidelines to minimize errors, improve test accuracy, and enhance patient confidence in genetic testing. To achieve these goals, increased funding and further investigation into this subject are imperative.
Author contributions
KI: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. ACo: Conceptualization, Writing – original draft, Writing – review & editing. ACh: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1466585/full#supplementary-material
References
1. CDC. Genetic Testing. (2024) Available at: https://www.cdc.gov/genomics-and-health/about/genetic-testing.html?CDC_AAref_Val=https://www.cdc.gov/genomics/gtesting/genetic_testing.htm. (Accessed January 8, 2024).
2. Schienda, J, and Stopfer, JE. Cancer genetic counseling—current practice and future challenges. Cold Spring Harb Perspect Med. (2019) 10:a036541. doi: 10.1101/cshperspect.a036541
3. Kelly, M, and Semsarian, C. Multiple mutations in genetic cardiovascular disease: a marker of disease severity? Circ Cardiovasc Genet. (2009) 2:182–90. doi: 10.1161/circgenetics.108.836478
4. Singh, DN, Daripelli, S, Elamin, MO, Polevoy, G, and Prasanna, ML. Genetic testing for successive cancer treatment. Curēus. (2023) 15:e49889. doi: 10.7759/cureus.49889
5. Sholl, LM, and Halmos, B. Biomarker testing in cancer management-can one size fit all? Br J Cancer. (2022) 127:1177–9. doi: 10.1038/s41416-022-01967-4
6. Sullivan, PF, and Geschwind, DH. Defining the genetic, genomic, cellular, and diagnostic architectures of psychiatric disorders. Cell. (2019) 177:162–83. doi: 10.1016/j.cell.2019.01.015
7. Ali, F, Sreeraj, VS, Nadella, RK, Holla, B, Mahadevan, J, Ithal, D, et al. Estimating the familial risk of psychiatric illnesses: a review of family history scores. Asian J Psychiatr. (2021) 56:102551. doi: 10.1016/j.ajp.2021.102551
8. Walker, ER, McGee, RE, and Druss, BG. Mortality in mental disorders and global disease burden implications. JAMA Psychiatry. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502
9. Dohrenwend, BP, Levav, I, Shrout, PE, Schwartz, S, Naveh, G, Link, BG, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. (1992) 255:946–52. doi: 10.1126/science.1546291
10. Momen, NC, Plana-Ripoll, O, Agerbo, E, Benros, ME, Børglum, AD, Christensen, MK, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. (2020) 382:1721–31. doi: 10.1056/NEJMoa1915784
11. Young, C, and MacDougall, D. An overview of pharmacogenomic testing for psychiatric disorders. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health (2023).
12. Friesen, P, Lawrence, RE, Brucato, G, Girgis, RR, and Dixon, LB. Hopes and expectations regarding genetic testing for schizophrenia among young adults at clinical high-risk for psychosis. J Psychiatr Pract. (2016) 22:442–9. doi: 10.1097/pra.0000000000000188
13. Lu, Y, Pouget, JG, Andreassen, OA, Djurovic, S, Esko, T, Hultman, CM, et al. Genetic risk scores and family history as predictors of schizophrenia in Nordic registers. Psychol Med. (2017) 48:1201–8. doi: 10.1017/s0033291717002665
14. Calvo, E, Walko, C, Dees, EC, and Valenzuela, B. Pharmacogenomics, pharmacokinetics, and pharmacodynamics in the era of targeted therapies. Am Soc Clin Oncol Educ Book. (2016) 35:e175–84. doi: 10.1200/EDBK_159061
15. Shulman, RW, and Ozdemir, V. Psychotropic medications and cytochrome P450 2D6: pharmacokinetic considerations in the elderly. Can J Psychiatr. (1997) 42:4S–9S.
16. Pinzón-Espinosa, J, van der Horst, M, Zinkstok, J, Austin, J, Aalfs, C, Batalla, A, et al. Barriers to genetic testing in clinical psychiatry and ways to overcome them: from clinicians' attitudes to sociocultural differences between patients across the globe. Transl Psychiatry. (2022) 12:442. doi: 10.1038/s41398-022-02203-6
17. Santenna, C, Shubham, A, Ratinder, J, Abhijit, R, Tamonud, M, Jitendra, S, et al. Drug metabolizing enzymes pharmacogenetic variation-informed antidepressant therapy approach for common mental disorders: a systematic review and meta-analysis. J Affect Disord. (2024) 367:832–44. doi: 10.1016/j.jad.2024.09.041
18. Saadullah Khani, N, Hudson, G, Mills, G, Ramesh, S, Varney, L, Cotic, M, et al. A systematic review of pharmacogenetic testing to guide antipsychotic treatment. Nat Ment Health. (2024) 2:616–26. doi: 10.1038/s44220-024-00240-2
19. Tesfamicael, KG, Zhao, L, Fernández-Rodríguez, R, Adelson, DL, Musker, M, Polasek, TM, et al. Efficacy and safety of pharmacogenomic-guided antidepressant prescribing in patients with depression: an umbrella review and updated meta-analysis. Front Psych. (2024) 15:1276410. doi: 10.3389/fpsyt.2024.1276410
20. Milosavljević, F, Molden, PE, Ingelman-Sundberg, PM, and Jukić, APMM. Current level of evidence for improvement of antidepressant efficacy and tolerability by pharmacogenomic-guided treatment: a systematic review and meta-analysis of randomized controlled clinical trials. Eur Neuropsychopharmacol. (2024) 81:43–52. doi: 10.1016/j.euroneuro.2024.01.005
21. Wang, X, Wang, C, Zhang, Y, and An, Z. Effect of pharmacogenomics testing guiding on clinical outcomes in major depressive disorder: a systematic review and meta-analysis of RCT. BMC Psychiatry. (2023) 23:334. doi: 10.1186/s12888-023-04756-2
22. Bunka, M, Wong, G, Kim, D, Edwards, L, Austin, J, Doyle-Waters, MM, et al. Evaluating treatment outcomes in pharmacogenomic-guided care for major depression: a rapid review and meta-analysis. Psychiatry Res. (2023) 321:115102. doi: 10.1016/j.psychres.2023.115102
23. Arnone, D, Omar, O, Arora, T, Östlundh, L, Ramaraj, R, Javaid, S, et al. Effectiveness of pharmacogenomic tests including CYP2D6 and CYP2C19 genomic variants for guiding the treatment of depressive disorders: systematic review and meta-analysis of randomised controlled trials. Neurosci Biobehav Rev. (2023) 144:104965. doi: 10.1016/j.neubiorev.2022.104965
24. Islam, F, Hain, D, Lewis, D, Law, R, Brown, LC, Tanner, JA, et al. Pharmacogenomics of clozapine-induced agranulocytosis: a systematic review and meta-analysis. Pharmacogenomics J. (2022) 22:230–40. doi: 10.1038/s41397-022-00281-9
25. Ahmed, L, Constantinidou, A, and Chatzittofis, A. Patients’ perspectives related to ethical issues and risks in precision medicine: a systematic review. Front Med. (2023) 10:1215663. doi: 10.3389/fmed.2023.1215663
26. Bonomi, L, Huang, Y, and Ohno-Machado, L. Privacy challenges and research opportunities for genomic data sharing. Nat Genet. (2020) 52:646–54. doi: 10.1038/s41588-020-0651-0
27. Oliveri, S, Ferrari, F, Manfrinati, A, and Pravettoni, G. A systematic review of the psychological implications of genetic testing: a comparative analysis among cardiovascular, neurodegenerative and Cancer diseases. Front Genet. (2018) 9:624. doi: 10.3389/fgene.2018.00624
28. Appelbaum, PS, and Benston, S. Anticipating the ethical challenges of psychiatric genetic testing. Curr Psychiatry Rep. (2017) 19:39. doi: 10.1007/s11920-017-0790-x
29. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DGPRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. (2010) 8:336–41. doi: 10.1016/j.ijsu.2010.02.007
30. Andreassen, OA, Hindley, GFL, Frei, O, and Smeland, OB. New insights from the last decade of research in psychiatric genetics: discoveries, challenges and clinical implications. World Psychiatry. (2023) 22:4–24. doi: 10.1002/wps.21034
31. Campion, M, Goldgar, C, Hopkin, RJ, Prows, CA, and Dasgupta, S. Genomic education for the next generation of health-care providers. Genet Med. (2019) 21:2422–30. doi: 10.1038/s41436-019-0548-4
32. Schaibley, VM, Ramos, IN, Woosley, RL, Curry, S, Hays, S, and Ramos, KS. Limited genomics training among physicians remains a barrier to genomics-based implementation of precision medicine. Front Med. (2022) 9:757212. doi: 10.3389/fmed.2022.757212
33. Montanez, K, Berninger, T, Willis, M, Harding, A, and Lutgendorf, MA. Genetic testing costs and compliance with clinical best practices. J Genet Couns. (2020) 29:1186–91. doi: 10.1002/jgc4.1285
34. Rothstein, MA, and Anderlik, MR. What is genetic discrimination, and when and how can it be prevented? Genet Med. (2001) 3:354–8. doi: 10.1097/00125817-200109000-00005
35. Lerman, C, Croyle, R, Tercyak, K, and Hamann, H. Genetic testing: psychological aspects and implications. J Consult Clin Psychol. (2002) 70:784–97. doi: 10.1037/0022-006X.70.3.784
36. Wakefield, CE, Hanlon, LV, Tucker, KM, Patenaude, AF, Signorelli, C, McLoone, JK, et al. The psychological impact of genetic information on children: a systematic review. Genet Med. (2016) 18:755–62. doi: 10.1038/gim.2015.181
37. Koopmans, A. ‘CYP2D6 and CYP2C19 genotyping in psychiatry: Bridging the gap between practice and lab’, Maastricht university, (2021). Available at: https://doi.org/10.26481/dis.20210512ak
38. American College of Obstetricians and Gynecologists , ‘Counseling About Genetic Testing and Communication of Genetic Test Results’. Available at: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/04/counseling-about-genetic-testing-and-communication-of-genetic-test-results. Accessed: Jan. 08, 2024
39. Aboelbaha, S, Zolezzi, M, Abdallah, O, and Eltorki, Y. ‘Mental health prescribers’ perceptions on the use of Pharmacogenetic testing in the Management of Depression in the Middle East and North Africa region’. Pharmgenomics Pers Med. (2023) 16:503–18. doi: 10.2147/PGPM.S410240
40. Chan, CYW, Chua, BY, Subramaniam, M, Suen, ELK, and Lee, J. Clinicians’ perceptions of pharmacogenomics use in psychiatry. Pharmacogenomics. (2017) 18:531–8. doi: 10.2217/pgs-2016-0164
41. Kostick, K, Pereira, S, Brannan, C, Torgerson, L, and Lázaro-Muñoz, G. Psychiatric genomics researchers’ perspectives on best practices for returning results to individual participants. Genet Med. (2020) 22:345–52. doi: 10.1038/s41436-019-0642-7
42. Laplace, B, Calvet, B, Lacroix, A, Mouchabac, S, Picard, N, Girard, M, et al. Acceptability of Pharmacogenetic testing among French psychiatrists, a National Survey. JPM. (2021) 11:446. doi: 10.3390/jpm11060446
43. Shishko, I, Almeida, K, Silvia, RJ, and Tataronis, GR. Psychiatric pharmacists’ perception on the use of pharmacogenomic testing in the mental health population. Pharmacogenomics. (2015) 16:949–58. doi: 10.2217/pgs.15.22
44. Soda, T, Merner, AR, Small, BJ, Torgerson, LN, Muñoz, K, Austin, J, et al. Child and adolescent psychiatrists’ use, attitudes, and understanding of genetic testing and pharmacogenetics in clinical practice. Psychiatry Res. (2023) 325:115246. doi: 10.1016/j.psychres.2023.115246
45. Thompson, C, Hamilton, SP, and Hippman, C. Psychiatrist attitudes towards pharmacogenetic testing, direct-to-consumer genetic testing, and integrating genetic counseling into psychiatric patient care. Psychiatry Res. (2015) 226:68–72. doi: 10.1016/j.psychres.2014.11.044
46. Undurraga, J, Bórquez-Infante, I, Crossley, NA, Prieto, ML, and Repetto, GM. Pharmacogenetics in psychiatry: perceived value and opinions in a Chilean sample of practitioners. Front Pharmacol. (2021) 12:657985. doi: 10.3389/fphar.2021.657985
47. Vest, BM, Wray, LO, Brady, LA, Thase, ME, Beehler, GP, Chapman, SR, et al. Primary care and mental health providers’ perceptions of implementation of pharmacogenetics testing for depression prescribing. BMC Psychiatry. (2020) 20:518. doi: 10.1186/s12888-020-02919-z
48. Walden, LM, Brandl, EJ, Changasi, A, Sturgess, JE, Soibel, A, Notario, JFD, et al. Physicians’ opinions following pharmacogenetic testing for psychotropic medication. Psychiatry Res. (2015) 229:913–8. doi: 10.1016/j.psychres.2015.07.032
49. Wolfe, K, Stueber, K, McQuillin, A, Jichi, F, Patch, C, Flinter, F, et al. Genetic testing in intellectual disability psychiatry: opinions and practices of UK child and intellectual disability psychiatrists. J Appl Res Intellect Disabil. (2018) 31:273–84. doi: 10.1111/jar.12391
50. Kastrinos, A, Campbell-Salome, G, Shelton, S, Peterson, EB, and Bylund, CL. PGx in psychiatry: patients’ knowledge, interest, and uncertainty management preferences in the context of pharmacogenomic testing. Patient Educ Couns. (2021) 104:732–8. doi: 10.1016/j.pec.2020.12.021
51. Liko, I, Lai, E, Griffin, RJ, Aquilante, CL, and Lee, YM. ‘Patients’ perspectives on psychiatric Pharmacogenetic testing’. Pharmacopsychiatry. (2020) 53:256–61. doi: 10.1055/a-1183-5029
52. McCarthy, MJ, Chen, Y, Demodena, A, Fisher, E, Golshan, S, Suppes, T, et al. Attitudes on Pharmacogenetic testing in psychiatric patients with treatment resistant depression. Depress Anxiety. (2020) 37:842–50. doi: 10.1002/da.23074
Keywords: genetic testing, psychiatry, mental health, patients’ perspective, healthcare workers, precision medicine
Citation: Ioannou KI, Constantinidou A and Chatzittofis A (2024) Genetic testing in psychiatry, the perceptions of healthcare workers and patients: a mini review. Front. Public Health. 12:1466585. doi: 10.3389/fpubh.2024.1466585
Edited by:
Mario R. Louzã, University of São Paulo, BrazilReviewed by:
Richa Tripathi, All India Institute of Medical Sciences Gorakhpur, IndiaGabriel Beraldi, University of São Paulo, Brazil
Copyright © 2024 Ioannou, Constantinidou and Chatzittofis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andreas Chatzittofis, QW5kcmVhcy5jaGF0eml0dG9maXNAdW11LnNl
 Kyriakos I. Ioannou
Kyriakos I. Ioannou Anastasia Constantinidou
Anastasia Constantinidou Andreas Chatzittofis
Andreas Chatzittofis