- 1Department of Statistics, College of Natural and Computational Science, Samara University, Samara, Ethiopia
- 2Department of Health Informatics, Institute of Public Health, University of Gondar, Gondar, Ethiopia
- 3Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Rural Health Research Institute, Charles Sturt University, Orange, NSW, Australia
Introduction: In Ethiopia, 16% of deaths among children aged less than 5 years are attributable to diseases that can be prevented through vaccination. However, studies carried out in Ethiopia to date have not investigated how community- and individual-level factors affect children who receive no vaccine at all. Hence, this study aimed to assess the factors associated with unimmunized children in Ethiopia.
Methods: This study is a secondary analysis of Demographic and Health Survey (DHS) data. A weighted sample of 6,219 children aged less than 5 years was included after a stratified two-stage cluster sampling. To determine the factors that influence unimmunized children, a multivariable multilevel logistic regression model was developed. In addition, adjusted odds ratio (AOR) with 95% confidence interval (CI) was used to select variables that have statistically significant effects on unimmunized children.
Results: The prevalence of unimmunized children aged less than 5 years in Ethiopia was 22.45% (95% CI: 21.4–23.5). In the multivariable multilevel analysis, individual-level factors associated with increased odds of having unimmunized children included no media exposure (AOR 1.33, 95 CI: 1.02–1.63), place of delivery (AOR 1.5, CI: 1.22–1.91), and the child’s relationship to the household head—specifically between the household head and a daughter (AOR 1.5, 95 CI: 1.05–2.41) or categorized as others (AOR 1.8, 95, CI: 1.15–2.74). Community-level predictors associated with unimmunized children included place of residence (AOR 1.8, 95, CI: 1.12–2.58), distance from the health facility (AOR 1.32, 95, CI: 1.09–1.60), and community poverty level (AOR 1.4, 95, CI: 1.05–1.78).
Conclusion: In Ethiopia, approximately one-fourth of children could not get basic vaccinations. Media exposure, place of delivery, relationship with the household head, place of residence, distance from the health facility, and community poverty were found to be factors significantly associated with unimmunized children.
Background
One of the most effective public health initiatives for reducing childhood morbidity and mortality is immunization of children (1). It has been estimated that basic immunizations prevent 2.5 million child deaths globally each year (2, 3). The Expanded Programme on Immunization (EPI) was launched in 1974 to ensure that all children regularly obtain the recommended immunizations. However, many children below 5 years of age remain unvaccinated.
Immunization plays a vital role in improving public health worldwide, benefiting both developed and developing countries alike. It not only protects individuals from preventable diseases but also has significant societal and economic benefits. Thus, the implementation of effective immunization programs is crucial for reducing morbidity and mortality rates, promoting overall well-being, and advancing the development of these country (4, 5).
It is projected that, by 2055, the global population will approach approximately 10 billion, which is largely attributable to the effectiveness of vaccines in preventing diseases and thus extending life expectancy worldwide. However, substantial efforts are needed to guarantee the funding, delivery, distribution, and uptake of vaccines among all communities, especially among those that are remote, skeptical about vaccine efficacy, or affected by civil unrest (6).
In 1980, Ethiopia became one of the member states to adopt the EPI service as recommended by the WHO, with the aim of reducing child morbidity and mortality due to vaccine-preventable diseases (VPDs). However, the EPI faced challenges and did not achieve its intended success (7). Moreover, since 2003, Ethiopia has been following the Reaching Every District (RED) and Sustainable Outreach Services (SOS) approaches to improve immunization coverage (8).
Ethiopia provides the following basic: one dose of Bacillus Calmette–Guerin (BCG) and oral polio vaccine (OPV) given at birth; three doses each of each pentavalent, OPV, and pneumococcal conjugate vaccine (PCV) given at the 6th, 10th, and 14th weeks; and lastly measles vaccine at the 9th month (9–11).
Almost Approximately 29% of child fatalities can be prevented by vaccination (12). In 2011, one in out of five infants around the world did not receive life-saving vaccinations’ according to the statistics showing that 1.5 million children died and 22.4 million did not obtain the recommended three doses of DPT (13). Globally, 19.5 million children were incompletely immunized in 2016 (14). Approximately 60% of these children live in 10 countries, including Ethiopia (15). Furthermore, approximately one out of 10 infants lack access to any child vaccine worldwide (15).
In Ethiopia, infections that can be prevented by vaccination account for approximately 16% of deaths among children aged less than 5 years (16). The EPI service of the country aims to protect roughly 3 million newborns every year from VPDs (17), but a significant proportion of children remain unimmunized, which is the highest contributor to child mortality (mostly caused by VPDs) in Ethiopia (18, 19).
According to the 2016 Ethiopian Demographic and Health Survey (EDHS) data, full immunization coverage increased from 24% in 2011 to 39% in 2016 (19, 20); however, this achievement remains markedly below the goal set in sustainable development goals (11, 21). Even though EPI services are available to every kebele (i.e., a small administrative unit), children still remain unvaccinated in Ethiopia, with only 50% of children between 12 and 23 years of age receiving all of their recommended vaccinations (22).
Various studies have been carried out to determine the factors associated with immunization both in Ethiopia and worldwide (11, 23–33). However, these studies have seldom focused on how circumstances can affect children being unimmunized. In addition, using a single-level logistic regression analysis to examine data with a hierarchical structure (i.e., children nested within communities) violates the independence assumptions in basic logistic regression models (34, 35). Furthermore, even though there are a variety of interrelated characteristics associated with unvaccinated children, they are not always consistent throughout the study areas and researchers. Moreover, research prioritization is a dynamic and iterative process that requires ongoing review and updates as new findings are made and additional issues are identified, to further strengthen and document the already-existing evidence in support of the significant impact of individual- and contextual-level factors in the field of public health.
Therefore, to address the aforementioned challenges, we carried out this study to identify community- and individual-level factors associated with unimmunized children, which is a crucial first step in preventing child mortality.
Methods
Data and sample
This study is a secondary analysis of Demographic and Health Survey (DHS) data, which were sourced from the official database website of the DHS program.1 These data were collected during the period from 18 January 2016 to 27 June 2016. The EDHS is conducted every 5 years and is nationally representative. It covers Ethiopia’s nine regional states: (Afar; Amhara; Benishangul-Gumuz; Gambela; Harari; Oromia; Somali; Southern Nations, Nationalities, and People’s Region (SNNPR); and Tigray), as well as two administrative cities (Addis Ababa and Dire Dawa) (36).
The source population for this study comprised all children aged 0 to 59 months residing in Ethiopia, whereas the study population included all children less than 5 years of age residing in the chosen enumeration areas during EDHS data collection. A total of 6,219 children aged 0 to 59 months who met the inclusion criteria were included in this study. A two-stage probability sampling method, stratified by geographic region and urban/rural areas within each region, was used to select study participants, covering the entire target population of Ethiopia (37).
Measures of variables
Dependent variable
Unimmunized children was the dependent variable with binary outcomes categorized into 1 = yes (children who had not received basic vaccination) and 0 = no (those who had received at least one dose of any basic vaccination and at most full dose of vaccination).
Independent variables
Independent variables included individual-level variables and community-level variables. The following are the individual-level variables: sociodemographic factors (mother’s age, mother’s educational level, marital status, sex of the household head, wealth index, occupation, religion, and relationship with the household head), obstetric factors (parity and place of delivery), and information communication (listening to the radio, watching television, reading the newspaper, and having a mobile phone). The following were the community-level variables: residence, region, distance from the health facility, community education, community poverty level, and community media exposure, among which the latter three variables were produced by aggregating individual-level variables.
Model and data analysis
Based on the recommendation of the EDHS, proportions and frequencies were estimated after applying sample weights to the data to adjust for disproportionate sampling and non-responses since the allocation of the sample in the EDHS to different regions, as well as urban and rural areas, was non-proportional.
Variables were fitted into four models. To test for random variation in the intercept and calculate the intraclass correlation coefficient (ICC) and proportionate change in variance (PCV), model I (the empty model) was fitted without explanatory variables. Model II analyzed how individual-level traits affected individuals; model III analyzed how community-level factors affected individuals; and model IV (full model) analyzed how both individual- and community-level factors affected individuals simultaneously. The PCV and ICC were also used to measure variation. The Akaike Information Criterion (AIC) values were calculated for each model and compared, and the model with the lowest AIC value was chosen as the best-fit model.
As the full model (model with individual- and community-level variables) had the lowest AIC value, it was the model that best fit the data. AOR with 95% CI in the multivariable model was used to select variables that have a statistically significant association with unimmunized children.
Results
Sociodemographic characteristics of respondents
A total of 6,219 children aged less than 5 years were included in this study. Regarding maternal education, the majority of children (3,854, 61.97%) had no formal education, and the majority of children (5,500, 88.44%) were rural residents (Table 1). Regarding sex, 49.46% (3,076) were male and 50.54% (3,143) were female. The majority of mothers (51.75%, 3,218) were between 25 and 34 years of age, 27.43% (1,706) were between 15 and 24 years, and 20.82% (1,295) were between 35 and 49 years. In addition, 62.6% of mothers (3,894) were not employed, while 37.4% (2,324) were employed. In most of the cases, caregivers were the wives of the household heads (79.8%, 4,965). A small proportion of caregivers were daughters (5.5%, 338) or other relatives (4.8%, 299) such as daughter-in-law, granddaughter, and sister.
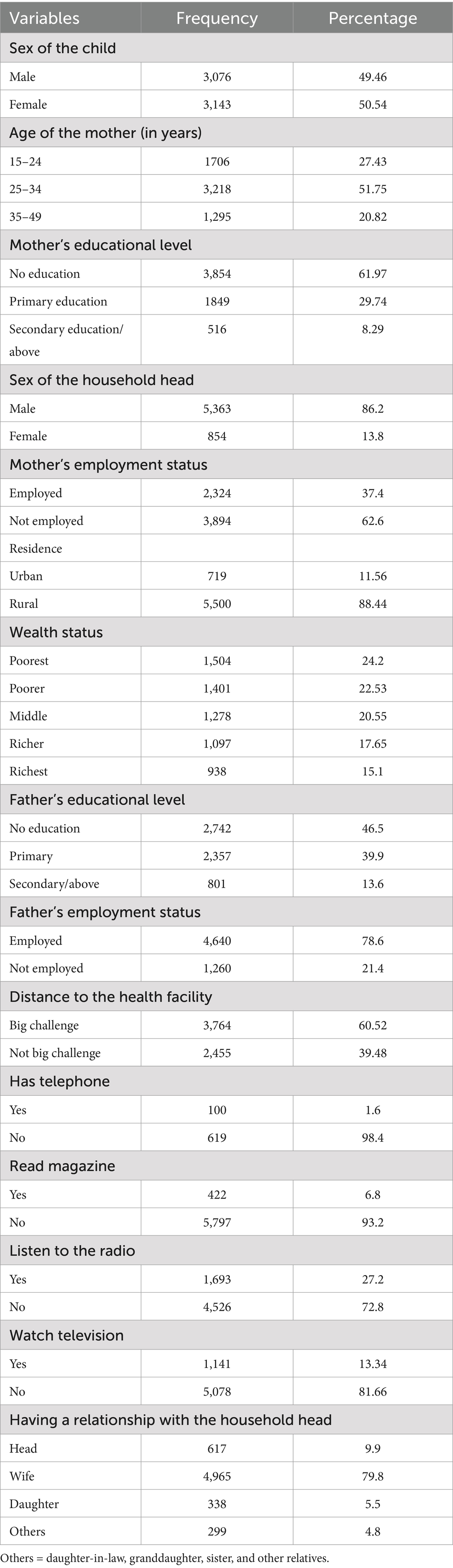
Table 1. Sociodemographic characteristics of respondents associated with unimmunized children in Ethiopia.
In this study, 6,219 children and 6,217 caregivers were included. The sociodemographic characteristics of both children and caregivers were analyzed, highlighting the influence of key factors such as sex, age, educational level, and employment status on vaccination status. Children were nearly equally distributed between both sexes, while the majority of mothers were aged 25–34 years, with a significant proportion having no education. Households were predominantly rural, with the majority being male-headed households. Disparities were observed in wealth index and access to telecommunication tools, and healthcare access was limited due to the distance for many respondents (Table 1).
Several sociodemographic factors were associated with unimmunized children in Ethiopia. Children from rural areas, those from poorer households, and those whose mother had no formal education were more likely to be unimmunized. Maternal employment status influenced immunization rates, with children of unemployed mothers showing lower coverage. Household characteristics, such as male-headed households and perceived difficulty in accessing healthcare facilities, were also associated with lower immunization rates. In addition, limited media exposure (such as radio, television, or magazines) and lack of access to telecommunication devices further contributed to disparities in immunization coverage.
Prevalence of unimmunized children
In Ethiopia, the prevalence of unimmunized children aged less than 5 years was 1,396 (22.45%) (95% CI: 21.4–23.5). A variation among unimmunized children was observed across regions of Ethiopia. The proportion of unimmunized children was lowest in Addis Ababa (3%) and highest in Afar (41%).
Random effect model and model fitness
The community-level variance ICC was 46%, which indicates significant variation in unimmunized children across the enumeration areas. This difference declined from 46 to 23% when different variables were controlled; however, there were some variables that should be incorporated into the model to better explain the reset variability. In addition, the PCV result revealed that 61% of variation was explained by community-level variables, 60% by individual-level variables, and 71% by both individual-level and community-level variables. Based on the model comparisons, model IV was found to be the best-fit model, and therefore, interpretations were made for model IV (Table 2).
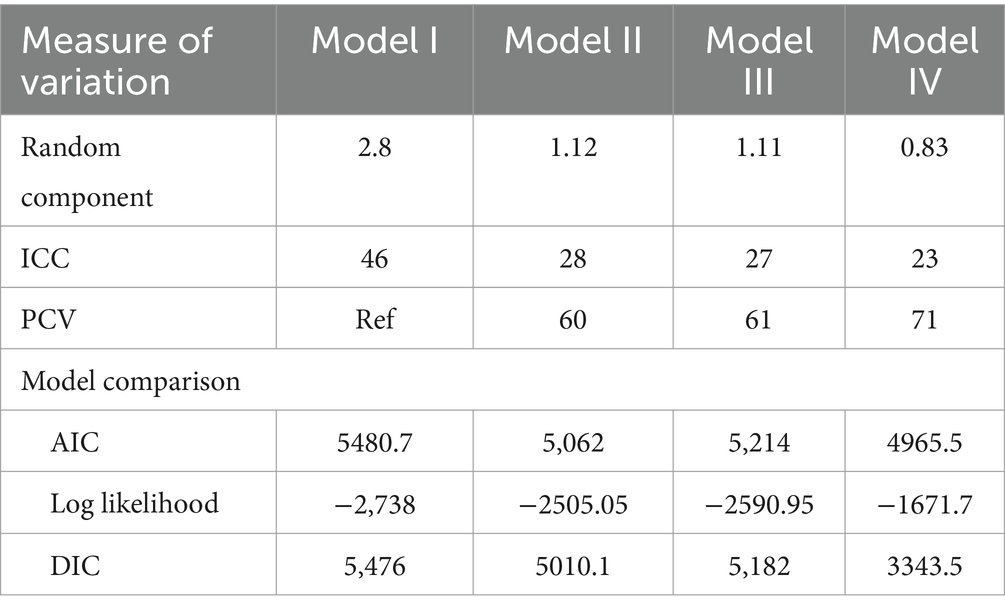
Table 2. Model comparison and model fitness results with respect to factors associated with unimmunized children in Ethiopia.
Factors associated with unimmunized children
The odds of having unimmunized children increased by 1.5 times (AOR 1.5, 95% CI 1.22–1.91) when women gave birth at home. It increased by 1.8 times (AOR 1.8, 95% CI 1.12–2.58) among rural women Compared to urban residents. In addition, the odds of having unimmunized children increased by 1.33 times (AOR 1.33, 95% CI 1.02–1.63) among women who had no media exposure compared to those who had exposure to media. Similarly, it increased by 1.4 times (AOR 1.4, 95% CI 1.05–1.78) among women from high-poverty communities compared to those from a low-poverty community. Among women who perceived distance from the health facility as a big challenge, the odds of having unimmunized children increased by 1.32 times (AOR 1.32, 95% CI 1.097–1.6) compared to those who did not. Furthermore, the odds of having unimmunized children among women who had low community media exposure increased by 1.9 times (AOR 1.9, 95% CI 1.39–2.58) compared to those who had high media exposure. Finally, the odds of having unimmunized children among women whose relationship with household head as a daughter increased by 1.5 times (AOR 1.5, 95% CI 1.05 2.41) and as others by 1.8 times (AOR 1.8, 95% CI 1.15–2.74) compared to women who were the household head (Table 3).
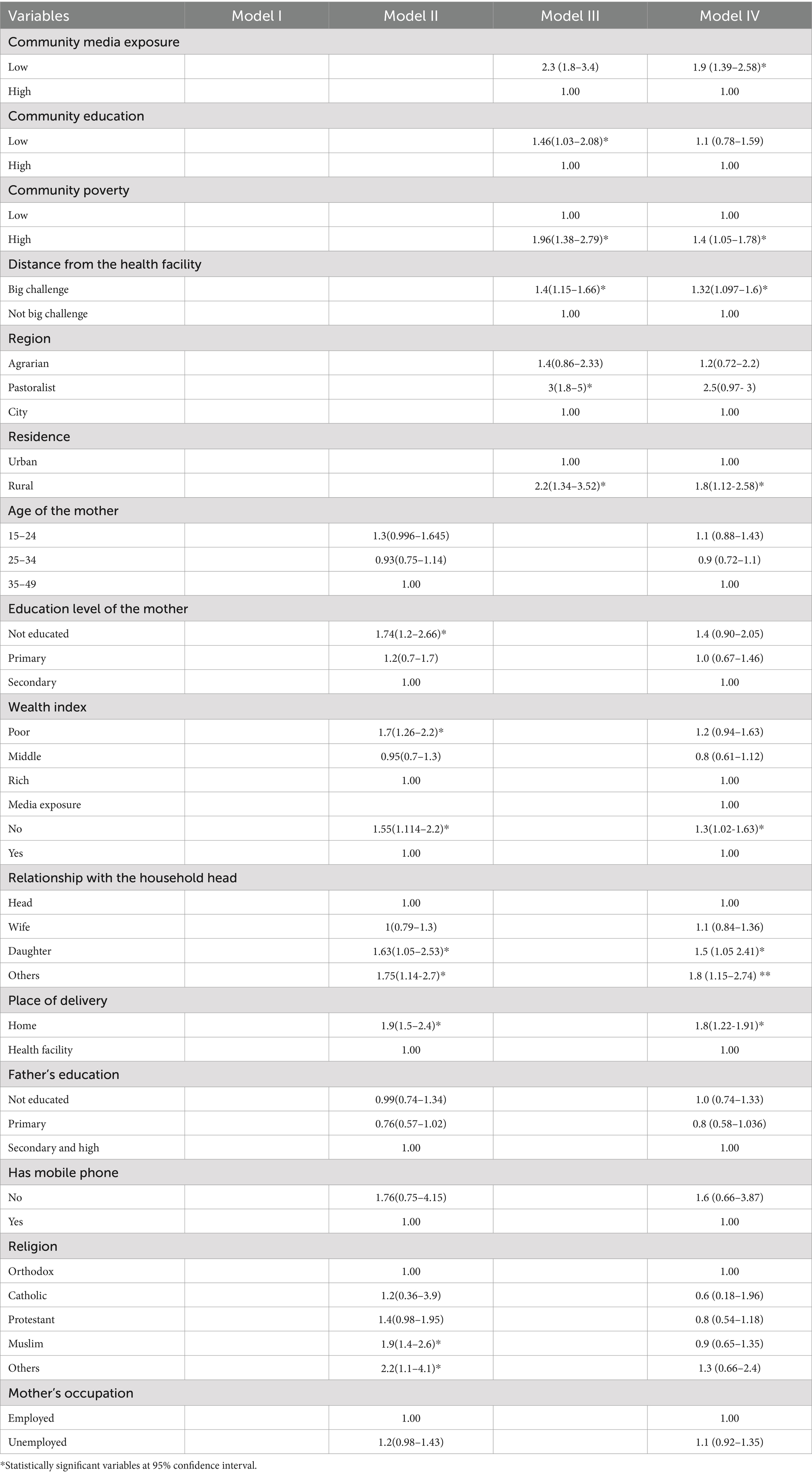
Table 3. Multilevel multivariable logistic regression of the individual- and community-level variables associated with unimmunized children in Ethiopia.
Discussion
Unimmunized children remain a significant public health problem in Ethiopia even though efforts have been made to contain this issue. In this study, the prevalence of unimmunized children was found to be 22.45% (95% CI 21.4–23.5). In addition, the proportion of unimmunized children varied across the administrative regions of Ethiopia. The number of unimmunized children remains critically high and was not evenly distributed across the country. The EDHS reports also show only a slight reduction in the number of unimmunized children. A number of studies have also revealed that low immunization coverage across different parts of the country and in the entire country as well (23–25, 27). This high percentage of unimmunized children might be because Ethiopia is a developing country and its childhood vaccination strategies are poorly implemented by different agents working toward immunization services. In addition, inconsistent implementation of immunization services across the country might have led to a high percentage of unimmunized children. Furthermore, some areas are not accessible for transportation, which also contributes to the high percentage of unimmunized children.
After controlling for clustering/random effect, this study identified both individual- and community-level factors with a significant association with unimmunized children.
Among individual-level factors, media exposure, place of delivery, and relationship with the household head were significantly associated with unimmunized children. Among community-level factors, place of residence, distance from the health facility, media exposure, and community poverty were significantly associated with unimmunized children.
This study also revealed that home delivery had a significant positive association with unimmunized children. However, some studies have reported the negative impact of home delivery on vaccination coverage (28, 29). In addition, previous studies have also reported the positive impact of giving birth at home on incomplete immunization (23, 25, 38). This finding might be attributable to mothers gaining awareness of the health benefits of immunization through health education programs in the facility where they are going to give birth and through frequent counseling by healthcare professionals regarding having fully immunized children to protect children from VPDs, which is a common cause of death among children. In addition, mothers have a chance to vaccinate their children against polio and can have information on the subsequent schedule.
Women who had low media exposure had a significant positive association with unimmunized children. A number of studies have also reported the positive impact of media exposure on incomplete immunization (23, 25). The role of information in choosing the best strategical intervention to improve the immunization service was obvious, which is supported by different findings and governmental reports. When mothers understand the benefits of immunization, their interest in availing the service increases. Therefore, advertisements are circulated through mass media, which enables them to gain better knowledge about immunization.
Women whose relationship with the household head was that of daughters and others had a positive significant association with unimmunized children. A number of studies have also reported the positive impact of women having a relationship with the household head as daughters and others on vaccination coverage. If the relationship with the household head is not intimate, the communication between the head and the caregiver can be less interactive. In addition, women are too busy to handle plenty of activities, which leads them to forget immunization schedules. Furthermore, since they are less influential than head caregivers and are taking care of household activities as well as immunization schedules, there is a possibility that they are likely to miss the scheduled immunization day.
On the other hand, the community-level factors place of residence, distance from the health facility, media exposure, and community poverty level were significantly associated with unimmunized children. Mothers who perceived distance from the health facility as a big challenge were more likely to have unimmunized children than those who did not. Previous studies conducted in Ethiopia and in other countries have also reported the positive impact of being distant from health facilities on incomplete immunization (24, 26, 33, 39, 40). This finding might be attributable to the fact that when women are far away from the vaccination site, they may face transportation challenges, which may make them miss the scheduled vaccination date.
Mothers from rural residences were more likely to have unimmunized children than those from urban residences. Studies conducted in Ethiopia and in other countries have also reported the positive impact of being a rural resident on incomplete immunization and the negative impact on vaccination coverage (38). This finding is attributable to the fact that rural women may not have access to education regarding child health services. Furthermore, they may face challenges in accessing health facilities, which might lead to having unimmunized children.
Mothers from high-poverty communities were more likely to have unimmunized children than those from low-poverty communities. The intensity of poverty and the lifestyle of the community can affect the vaccination status of children. High-poverty communities with a low wealth index can result in unimmunized children, as people who are poor may prioritize daily activities, the food they are going to have, and other acute problems rather than unobservable health problems. In addition, people who are poor, on most occasions, tend to worry more about the daily need for food supply than about vaccination of children.
Strengths and limitations of the study
The findings of this study can be generalized to all children aged less than 5 years in Ethiopia. These findings are dependent on the quality of the DHS program. The DHS collects a huge amount of information on households, important childhood health indicators, and maternal health in developing countries and is considered one of the reliable sources of information on maternal and child health. Thus, the findings of this study can be generalized for the source population of the participants and can be used as reliable evidence.
In this study, a multilevel analytical approach was used, which enabled the identification of a multilevel determinant of unimmunized children and provided insights for the Ethiopian Federal Ministry of Health to design appropriate interventions that reduce the proportion of unimmunized children in the country, which is a major indicator of a healthy childhood. Furthermore, the results of this study are representative of the Ethiopian population since appropriate estimation adjustments, such as weighting, were carried out before analysis.
This study has some limitations. First, the analysis was conducted using potential variables extracted from the DHS dataset. However, variables other than those mentioned in the DHS dataset could also be important factors associated with unimmunized children. Some of these variables may include distance to health service centers and quality of immunization services. Second, the cross-sectional survey data used in this study make it more difficult to conclude causality. Therefore, it is necessary to use longitudinal data that have been collected several times to confirm the validity of the observed associations.
Conclusion
This study found a high prevalence of unimmunized children in Ethiopia, among whom nearly one-fourth of children did not get basic vaccinations.
Among individual factors, media exposure, place of delivery, and relationship with the household head were significantly associated with unimmunized children. Place of residence, distance from the health facility, community media exposure, and community poverty were the community-level factors significantly associated with unimmunized children.
In conclusion, immunization plays a vital role in improving public health in developing countries. It not only protects individuals from preventable diseases but also has significant societal and economic benefits. Implementation of effective immunization programs is crucial for reducing morbidity and mortality rates, promoting overall wellbeing, and advancing the development of a country.
Extending immunization programs can act as a catalyst for positive economic development and institutional changes at both the local and global levels. It is an investment for the well-being of communities, which contributes to a more prosperous and sustainable future.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
GM: Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Software. MM: Conceptualization, Writing – review & editing. SA: Conceptualization, Methodology, Software, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors acknowledge the ICF International for granting access to use the 2016 EDHS dataset for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; DHS, Demographic and Health Survey; EDHS, Ethiopian Demographic and Health Survey; ICC, intraclass correlation coefficient; PCV, proportionate change in variance; VPD, vaccine-preventable disease.
Footnotes
References
1. Wongleedee, K. The influence of organizational culture management and fresh hiring on the pharmacies performance: mediating role of existing employees. Syst Rev Pharm. (2020) 11:398–406. doi: 10.5530/srp.2020.1.51
2. Burton, A, Kowalski, R, Gacic-Dobo, M, Karimov, R, and Brown, D. A formal representation of the WHO and UNICEF estimates of national immunization coverage: a computational logic approach. PLoS One. (2012) 7:e47806. doi: 10.1371/journal.pone.0047806
3. Theiss-Nyland, K, and Avan, B. Knowledge summary 25: integrating immunization and other services for women and children. Policy brief. (2013)
5. Gavi, T.V.A. Annual Progress Report 2021. The impact of vaccines. Gavi, the Vaccine Alliance (2021). Available at: https://www.gavi.org/progress-report-2021
6. UNDOI World Population Prospects 2024: Summary of Results. United Nations, Department of Economic and Social Affairs, Population Division. (2024). Available at: https://population.un.org/wpp/assets/Files/WPP2024_Summary-of-Results.pdf
7. Abdi, AG. The Ethiopian civil society law in light of the principle of the best interest of the child. Interdisc J Hum Rts L. (2012) 7:127.
8. Tesfaye, F, Tamiso, A, Birhan, Y, and Tadele, T. Predictors of immunization defaulting among children age 12-23 months in Hawassa Zuria District of southern Ethiopia: community based unmatched case control study. Int J Public Health Sci. (2014) 3:4692. doi: 10.11591/ijphs.v3i3.4692
9. Belete, H, Kidane, K, Filimona, B, Mitikie, M, and Mounier-Jack, S. Routine immunization in Ethiopia. Ethiop J Heal Dev. (2015) 1:1–34. Available at: https://ejhd.org/index.php/ejhd/article/view/1395
10. Tesfaye, TD, Temesgen, WA, and Kasa, AS. Vaccination coverage and associated factors among children aged 12–23 months in Northwest Ethiopia. Hum Vaccin Immunother. (2018) 14:2348–54. doi: 10.1080/21645515.2018.1502528
11. Negussie, A, Kassahun, W, Assegid, S, and Hagan, AK. Factors associated with incomplete childhood immunization in Arbegona district, southern Ethiopia: a case–control study. BMC Public Health. (2015) 16:27. doi: 10.1186/s12889-015-2678-1
12. Ortiz, JR, Perut, M, Dumolard, L, Wijesinghe, PR, Jorgensen, P, Ropero, AM, et al. A global review of national influenza immunization policies: analysis of the 2014 WHO/UNICEF joint reporting form on immunization. Vaccine. (2016) 34:5400–5. doi: 10.1016/j.vaccine.2016.07.045
13. Burton, A, Monasch, R, Lautenbach, B, Gacic-Dobo, M, Neill, M, Karimov, R, et al. WHO and UNICEF estimates of national infant immunization coverage: methods and processes. Bull World Health Organ. (2009) 87:535–41. doi: 10.2471/BLT.08.053819
14. Feldstein, LR, Mariat, S, Gacic-Dobo, M, Diallo, MS, Conklin, LM, and Wallace, AS. Global routine vaccination coverage, 2016. MMWR Morb Mortal Wkly Rep. (2017) 66:1252–5. doi: 10.15585/mmwr.mm6645a3
15. Pagliusi, S, Dennehy, M, and Kim, HDCVMN AGM Organizing Committee. Vaccines, inspiring innovation in health. Vaccine. (2018) 36:7430–7. doi: 10.1016/j.vaccine.2018.05.035
16. Abebe, AM, Kassaw, MW, and Birara, A. Coverage, opportunity and challenges of expanded program on immunization among 12-23 months old children in Woldia town, northeast, Ethiopia, 2018.: mixed cross sectional study. Biomed Res Int. (2018) 2019:5302307. doi: 10.1155/2019/5302307
17. Lakew, Y, Bekele, A, and Biadgilign, S. Factors influencing full immunization coverage among 12–23 months of age children in Ethiopia: evidence from the national demographic and health survey in 2011. BMC Public Health. (2015) 15:728. doi: 10.1186/s12889-015-2078-6
18. CSA and ICF. Ethiopia Demographic and Health survey 2016: Key indicators report. Addis Ababa, Rockville: CSA and ICF (2016).
20. WHO. Global vaccine action plan: Regional vaccine action plans 2016 progress reports. Geneva: WHO (2016).
21. Kelbessa, Z, Baraki, N, and Egata, G. Level of health extension service utilization and associated factors among community in Abuna Gindeberet District, west Shoa zone, Oromia regional state, Ethiopia. BMC Health Serv Res. (2014) 14:324. doi: 10.1186/1472-6963-14-324
22. Glauber, JH. The immunization delivery effectiveness assessment score: a better immunization measure? Pediatrics. (2003) 112:e39–45. doi: 10.1542/peds.112.1.e39
23. Bugvi, AS, Rahat, R, Zakar, R, Zakar, MZ, Fischer, F, Nasrullah, M, et al. Factors associated with non-utilization of child immunization in Pakistan: evidence from the Demographic and Health survey 2006-07. BMC Public Health. (2014) 14:232. doi: 10.1186/1471-2458-14-232
24. Abdulraheem, I, Onajole, AT, and Jimoh, AA. Reasons for incomplete vaccination and factors for missed opportunities among rural Nigerian children. J Public Health Epidemiol. (2011) 3:194–203. Available at: https://academicjournals.org/article/article1379427155_Abdulraheem%20et%20al.pdf
25. Landoh, DE, Ouro-kavalah, F, Yaya, I, Kahn, AL, Wasswa, P, Lacle, A, et al. Predictors of incomplete immunization coverage among one to five years old children in Togo. BMC Public Health. (2016) 16:968. doi: 10.1186/s12889-016-3625-5
26. Xeuatvongsa, A, Hachiya, M, Miyano, S, Mizoue, T, and Kitamura, T. Determination of factors affecting the vaccination status of children aged 12–35 months in Lao People’s Democratic Republic. Heliyon. (2017) 3:e00265. doi: 10.1016/j.heliyon.2017.e00265
27. Adokiya, MN, Baguune, B, and Ndago, JA. Evaluation of immunization coverage and its associated factors among children 12–23 months of age in Techiman municipality, Ghana, 2016. Arch Public Health. (2017) 75:28. doi: 10.1186/s13690-017-0196-6
28. Etana, B, and Deressa, W. Factors associated with complete immunization coverage in children aged 12–23 months in ambo Woreda, Central Ethiopia. BMC Public Health. (2012) 12:566. doi: 10.1186/1471-2458-12-566
29. Meleko, A, Geremew, M, and Birhanu, F. Assessment of child immunization coverage and associated factors with full vaccination among children aged 12–23 months at Mizan Aman town, bench Maji zone, Southwest Ethiopia. Int J Pediatr. (2017) 2017:1–11. doi: 10.1155/2017/7976587
30. Kassahun, MB, Biks, GA, and Teferra, AS. Level of immunization coverage and associated factors among children aged 12–23 months in lay Armachiho District, North Gondar zone, Northwest Ethiopia: a community based cross sectional study. BMC Res Notes. (2015) 8:239. doi: 10.1186/s13104-015-1192-y
31. Lake, MW, Boulanger, L, Wasswa, P, Merbratu, M, and Fenta, A. Factors for low routine immunization performance: a community-based cross-sectional study in Dessie town, south Wollo zone, Ethiopia, 2014. Adv Appl Sci. (2016) 1:7–17. doi: 10.11648/j.aas.20160101.12
32. Gualu, T, and Dilie, A. Vaccination coverage and associated factors among children aged 12–23 months in debre markos town, Amhara regional state, Hindawi Limited: Ethiopia. Adv. Public Health. (2017) 2017:5352847. doi: 10.1155/2017/5352847
33. Okwaraji, YB, Mulholland, K, Schellenberg, JRMA, Andarge, G, Admassu, M, and Edmond, KM. The association between travel time to health facilities and childhood vaccine coverage in rural Ethiopia. A community based cross sectional study. BMC Public Health. (2012) 12:476. doi: 10.1186/1471-2458-12-476
34. Snijders, TA, and Bosker, RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Cham: Sage (2011).
35. Goldstein, H. Multilevel statistical models. Chichester, United Kingdom: John Wiley & Sons (2011).
36. Fekadu, GA, Ambaw, F, and Kidanie, SA. Facility delivery and postnatal care services use among mothers who attended four or more antenatal care visits in Ethiopia: further analysis of the 2016 demographic and health survey. BMC Pregnancy Childbirth. (2019) 19:64. doi: 10.1186/s12884-019-2216-8
37. CSACE Ethiopia Demographic and Health survey 2016: key indicators report. Addis Ababa, Ethiopia: CSACE. (2016).
38. Mohamud, AN, Feleke, A, Worku, W, Kifle, M, and Sharma, HR. Immunization coverage of 12–23 months old children and associated factors in Jigjiga District, Somali National Regional State, Ethiopia. BMC Public Health. (2014) 14:865. doi: 10.1186/1471-2458-14-865
39. Aregawi, HG, Gebrehiwot, TG, Abebe, YG, Meles, KG, and Wuneh, AD. Determinants of defaulting from completion of child immunization in Laelay Adiabo District, Tigray region, northern Ethiopia: a case-control study. PLoS One. (2017) 12:e0185533. doi: 10.1371/journal.pone.0185533
Keywords: unimmunized children, multilevel, associated factors, Ethiopia, health survey data
Citation: Mamo Habtie G, Melaku MS and Aychiluhm SB (2025) A multilevel analysis of factors associated with unimmunized children in Ethiopia. Front. Public Health. 13:1433606. doi: 10.3389/fpubh.2025.1433606
Edited by:
Md. Moyazzem Hossain, Jahangirnagar University, BangladeshReviewed by:
Ibrahim Dadari, United Nations Children’s Fund, United StatesAna Afonso, NOVA University of Lisbon, Portugal
Copyright © 2025 Mamo Habtie, Melaku and Aychiluhm. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Getnet Mamo Habtie, Z2V0bmV0bWFtbzIxQGdtYWlsLmNvbQ==
 Getnet Mamo Habtie
Getnet Mamo Habtie Mequannent Sharew Melaku
Mequannent Sharew Melaku Setognal Birara Aychiluhm
Setognal Birara Aychiluhm