- 1Research Center, King Fahad Medical City, Riyadh Second Health Cluster, Riyadh, Saudi Arabia
- 2Prince Sultan Military Medical City, Riyadh, Saudi Arabia
- 3Family Medicine, King Abdulaziz University, Jeddah, Makkah, Saudi Arabia
- 4College of Nursing, University of Hail, Ha'il, Saudi Arabia
- 5Gulf Health Council, Riyadh, Saudi Arabia
- 6King Abdul Aziz University Hospital, Jeddah, Makkah, Saudi Arabia
- 7Department of Food Science and Human Nutrition, College of Agriculture and Food, Qassim University, Buraydah, Saudi Arabia
- 8National Institute of Health and Care Research, Applied Research Collaboration North East and North Cumbria, Newcastle, United Kingdom
- 9UK Health Security Agency (UKHSA), London, United Kingdom
- 10American College of Lifestyle Medicine (ACLM), Chesterfield, MO, United States
- 11Preventive Medicine, Sher-I-Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India
- 12College of Nursing, University of Qassim, Buraydah, Saudi Arabia
- 13Medical Research Center, Sultan Qaboos University, Muscat, Oman
Background and importance: Lifestyle choices and practices are often the primary contributors to most preventable chronic diseases encountered in both outpatient and inpatient settings worldwide. Lifestyle medicine (LM) therapeutic interventions have consistently been shown through numerous scientific studies to improve and, in many cases, reverse chronic diseases. Globally, there is widespread acceptance of the 15 core competencies, 6 pillars, and the overarching definition of Lifestyle Medicine (LM) established by the American College of Lifestyle Medicine and its partners. While these 6 pillars provide a robust framework, they may not fully address the diverse needs of individuals and populations across various cultures, countries, and communities. The implementation of LM is inherently context-sensitive, influenced by factors such as local legislation, culinary traditions, food availability, economic conditions, agricultural development, whole-food retail accessibility, healthcare infrastructure, training opportunities, community resources, and faith or religious practices at both the individual and community levels. Furthermore, the MENA region, in particular, experiences a disproportionately high prevalence of lifestyle-related non-communicable diseases (NCDs) such as obesity, impaired glucose tolerance (IGT), type 2 diabetes mellitus (T2DM), hypertension (HTN), coronary artery disease (CAD), polycystic ovary syndrome (PCOS), and various forms of cancer, along with other related syndromes and co-morbid conditions. Addressing these challenges requires careful consideration of the local context—a complex interplay of culture, traditions, beliefs, and behaviors—that significantly shapes lifestyle choices, resource availability, and their subsequent impact on health and wellness outcomes. Significantly, the Hail Lifestyle Medicine International Conferences held in 2022 and 2023 have emphasized the strategic importance of Lifestyle Medicine in the MENA region, particularly in Saudi Arabia. These conferences underscored the need to define the scope of practice for Lifestyle Medicine in alignment with the ongoing Saudi healthcare transformation, the region's unique societal features, available local resources, and the specific needs of the population. Furthermore, these conferences served as pivotal platforms for convening experts, facilitating knowledge exchange, and fostering collaborations to tackle the distinct health challenges prevalent in the region. To provide a more comprehensive understanding, information regarding the establishment of the technical working group for the MENA region—critical to conceptualizing and adapting the LM pillars—should be included in the background or methods section earlier in the paper. This addition would offer readers insights into the foundational steps and collaborative efforts that initially shaped the initiative.
Establishment of the technical working group for the MENA region: In response to the rising prevalence of non-communicable diseases (NCDs) and the pressing need for a tailored approach to Lifestyle Medicine (LM) in the MENA region, a Technical Working Group (TWG) was established. The initiative sought to adapt the six pillars of LM to align with the region's unique cultural, economic, and social contexts. The TWG comprised experts from various disciplines, including family medicine, preventive medicine, public health, nutrition, and related fields, ensuring diverse perspectives and expertise in primary care and lifestyle interventions. The concept of adopting expanded LM pillars was initially formulated during a series of international and regional conferences, notably the Hail Lifestyle Medicine International Conferences held in 2022 and 2023. These conferences highlighted the urgent need for a region-specific approach to mitigate the high prevalence of lifestyle-related NCDs in the MENA region. The TWG was tasked with conducting a comprehensive review of the existing LM pillars while taking into account critical factors such as local legislation, culinary traditions, food resources, economic conditions, and health systems infrastructure. To achieve expert consensus on the adapted LM pillars, the Delphi process was employed. This structured communication method involved several rounds of anonymous questionnaires, enabling experts to provide their input and refine their responses based on collective feedback. The process ensured a balanced, inclusive approach that minimized potential power imbalances and produced LM pillars tailored to the MENA region's specific needs.
Methods: A survey was distributed to professional group panels representing multiple healthcare specialties, as well as to researchers and healthcare academic leaders of Lifestyle Medicine (LM) across Saudi Arabia and the broader Middle East. A Strength, Weakness, Opportunity, and Threat (SWOT) analysis was conducted, and the Delphi method was employed for structured communication and opinion formation. Using the nominal polling technique, formal responses were collected to develop an official written consensus position statement. The survey questions were validated and approved by an expert panel before being disseminated to the national Lifestyle Medicine group via WhatsApp for voting. Participants were asked to select one of three options: retain the American LM pillars, expand to the newly validated Saudi Arabian (MENA) LM pillars, or abstain from voting (neutral).
Conclusions and relevance: Out of 815 members in the national Lifestyle Medicine (LM) group, 136 responses were received, while 679 members abstained from voting, indicating neutrality. Among the 136 votes, 36 supported retaining the LM pillars developed by the American College of Lifestyle Medicine AMCL and its partners without modifications. In contrast, 118 voted in favor of the newly developed MENA/Saudi Arabian pillars, acknowledging the need to address local healthcare needs that extend beyond traditional or classical medicine. The new pillars incorporated motor vehicle driving disturbances as a leading modifiable lifestyle factor contributing to death and disability in the region. Additionally, the impact of smart technology, particularly mobile phones and other devices, was recognized as a key contributor to motor vehicle accidents (MVAs), which significantly increase mortality and disability rates. Further, the new pillars emphasized emotional and mental health, spirituality, and sexuality, driven by the growing demand for comprehensive mental and emotional healthcare combined with faith-based and spiritual empowerment. Finally, the inclusion of sexuality as a pillar was prompted by rapid societal changes, the rising prevalence of risky sexual behaviors, and the increased incidence of sexually transmitted infections (STIs). These challenges, coupled with the ambiguity surrounding who should manage such patients and the need for timely access to care, highlighted amajor gap in addressing this critical aspect of human health and quality of life. This addition ensures that LM physicians can provide appropriate care to close the gap in services related to sexual health.
1 Introduction
All healthcare professionals, particularly frontline consultants and trainees in family medicine, general pediatrics, preventive medicine, internal medicine, and OB-GYN, must understand the impact of evidence-based Lifestyle Medicine (LM) therapeutic interventions. These interventions influence genetics, epigenetics, and chronic disease management, ultimately affecting generational traits, including the potential emergence and prevalence of chronic diseases in future generations (1–5).
Approximately 80% of health-related conditions are attributed to factors beyond the control or scope of healthcare systems. For instance, public health policies and practices, access to healthy foods, physical activity empowerment, urban planning, housing, environmental pollution, social interaction norms and dynamics, faith-based local traditional practices in nutrition, human connectedness, emotional wellbeing, mental and social security, freedom of movement, water, sanitation, traffic calming and safety, substance use and abuse, and smart technology use and abuse (6, 7).
Lifestyle Medicine (LM) has been increasingly recognized as a global medical specialty. For example, the British Society of Lifestyle Medicine (BSLM), established in 2016, has played a pivotal role in advancing LM within the UK. The BSLM offers a diploma in Lifestyle Medicine, certified by the International Board of Lifestyle Medicine, and has incorporated LM into academic curricula at institutions such as Cambridge University (8).
In the United States, LM is also well-established, with numerous medical schools integrating it into their programs. Professional organizations like the American College of Lifestyle Medicine (ACLM) are at the forefront of these efforts. The ACLM offers certification for healthcare professionals and advocates for the widespread adoption of LM within mainstream healthcare (9, 10).
Globally, the Lifestyle Medicine Global Alliance (LMGA) connects regional members from around the world and provides online training to advance Lifestyle Medicine (LM). This alliance underscores the critical role of LM in addressing non-communicable diseases (NCDs) and improving overall health outcomes (9, 10).
These examples illustrate the increasing global acceptance and adaptation of LM as a recognized medical specialty. They highlight its transformative potential to enhance healthcare systems and improve patient outcomes.
In the MENA region, where Arabic is the most widely used official language, and Islam is the predominant religion, many shared values are accepted as societal norms across the population (11).1 These norms, combined with modern life and living practices, community and environmental interactions, nutritional choices, globalized economies, and the adoption of westernized meals and beverages, have contributed to a significant and exponential rise in the prevalence of preventable chronic diseases across all age groups, irrespective of economic status.
This statement was voted on by 815 members of the national Lifestyle Medicine (LM) group, who served as delegates at the Second Hail LM International Conference held in May 2023. Additional polling and voting were conducted through surveys of LM professional group panels comprising practicing healthcare specialists, researchers, and academic leaders from Saudi Arabia and other Middle Eastern countries. A SWOT analysis was performed, employing the Delphi method for communication and opinion formation. The nominal polling technique was used to collect opinions and formal votes.
The objective was to provide a MENA perspective on this emerging medical specialty to ensure a deeper and more effective application for the local population, including both healthcare practitioners and patients. This approach utilizes culturally adapted Lifestyle Medicine (LM) pillars designed to enhance the efficacy and efficiency of interventions for greater impact.
This initiative reflects and summarizes a cumulative effort spanning the last 6 years aimed at formulating the best medical practices for chronic disease management, improving quality of life and longevity, and reducing the disease burden and healthcare economic costs for the MENA population. Furthermore, this statement serves as an example of local contextualization, which could be extrapolated and adapted by other regions or countries worldwide.
2 Methods
To evaluate the degree of understanding, applicability, sensitivity, contextualization, and formalization of the newly adapted and expanded Lifestyle Medicine (LM) pillars and specialty in addressing the healthcare needs of Hail Province, Saudi Arabia, and the MENA region, a two-phase method was utilized.
Initially, the Hail Health Cluster initiatives were implemented as part of a broader effort to transform the healthcare sector in the Hail region in alignment with Saudi Arabia's Vision 2030 (12). These initiatives focus on several key areas:
1. Disease Prevention: Emphasizing lifestyle medicine, family medicine preventive services, and early disease detection to reduce and or reverse the incidence of pre-chronic diseases and chronic diseases.
2. Improving Disease Management: Enhancing the quality and safety of healthcare services to better manage existing conditions and improve patient outcomes.
3. Shifting the Patient Pathway: Encouraging the use of lifestyle medicine interventions in primary care centers as the first point of contact, thereby reducing the burden on hospitals and ensuring more efficient use of healthcare resources.
These initiatives aim to provide faster and more accessible healthcare services to all population segments, enhance population health through continuous assessment and targeted interventions, and measure outcomes to facilitate ongoing improvements.
2.1 Phase I Delphi exercise (drafting the questions and significance of the pillars)
The Hail conference was utilized as a platform to implement the Delphi exercise. The Delphi consensus process, employed by the panel, is a structured communication technique designed to achieve expert agreement. The panel consisted of expert leaders and local pioneers in the field, representing the Lifestyle Medicine National Group, the LM Scientific Foundation, and the LM Research Task Force.
The Delphi method involved multiple rounds of questionnaires, allowing experts to provide their opinions anonymously. After each round, a facilitator summarized the responses, and participants were encouraged to revise their answers based on the group's feedback. This iterative process continued until consensus was achieved or no further changes were noted (13–16).
In the first two rounds of the Delphi process, ideas and notes gathered from prior communications—including workshops, Zoom meetings, and social media interactions—were presented. These discussions, held among panel members between 2018 and 2023, served as a foundation for developing regionally adapted definitions and pillars. The nominal group technique was employed during these meetings to propose definitions and pillars that align with the region's cultural and religious context.
Additionally, a Key Care Indicator (KCI)® was proposed as a valid measurement tool for evaluating Lifestyle Medicine outcomes in both community and medical clinic settings. By the end of the second round, the panel achieved an 80% consensus on the definitions presented.
The last Delphi rounds drafted the list of proposed questions and collected answers to compile a list of definitions.
The following questions have been proposed:
1. What are the unique features of dominant MENA cultures that influence lifestyle choices and practices that need to be addressed in a healthcare setting?
2. How can Lifestyle Medicine's definition, pillars, and core competencies be adapted, expanded, and built upon to meet local needs?
3. Who should receive training to practice lifestyle medicine, and why?
4. What are the research opportunities of LM in the MENA region?
4.1. National LM research initiatives
4.1.1. NCD continuous yearly mapping
4.1.2. NCD LM therapeutic intervention studies
4.1.3. NCD LM therapeutic intervention-pharmaceutical studies
4.1.4. NCD LM pillars validation studies
4.1.5. Mindset and mindfulness studies
4.1.6. Faith, customs, and health interaction
5. What is the Saudi Arabia, Hail Province, and Hail City experience?
5.1. Experience and outcome of LM scientific conferencing (20%), combined with public, private, community, individual, and family engagement (80%), i.e., (20+80) conferencing.
5.2. LM academic programs initiatives
5.3. LM Training of Trainers (TOT) initiative
5.4. LM speaker training initiative
5.5. LM CPG development initiative
5.6. Community, private, and public organizations engagement
6. What was learned from Saudi Arabia's LM conferencing model (SALM-CM), Hail's Pilot?
6.1. Science presentation to specialists and the public
6.2. Public research engagement
6.3. Community Physical Activity Engagement Initiatives
6.4. Community nutrition display, healthy food prep, and training initiatives
6.5. Community awareness programs
6.6. Public entities engagement initiatives
6.7. Eco-conferencing and environmental awareness initiatives
The expert panel members were predominantly family medicine consultants certified in Lifestyle Medicine (LM). The majority of the panel comprised practicing physicians (70%), followed by allied health professionals (20%) and researchers or academics (10%). With extensive experience in primary care, preventive medicine, and lifestyle interventions, the panel members brought diverse expertise across clinical practice, research, and teaching. This multidisciplinary background equipped them to provide valuable insights into the integration of LM into primary care.
To ensure the validity of the consensus, the panel assessed potential power imbalances among its members. This assessment included evaluating the panel's diversity in terms of geographical representation, professional roles, and years of experience. By addressing these factors, the panel aimed to minimize any potential influence of power imbalances on the consensus-making process.
2.2 Phase II online survey to external experts to vote for the proposed draft list
We used convenience sampling to identify social media platforms, selecting WhatsApp professional groups and professional email contacts from a database of 815 individuals. An online survey was distributed to these individuals, consisting of two main questions regarding the selection of either the American Lifestyle Medicine pillars or the newly developed MENA Lifestyle Medicine pillars (see Appendix A). Responses were recorded on a 5-point Likert scale.
Only 20% of respondents identified themselves as eligible to answer the questions, while the remaining 80% remained neutral, stating that they were not experts in Lifestyle Medicine.
Survey data were downloaded from Google Forms and analyzed using SPSS v.12. Descriptive analyses, including bar charts and percentages, were employed to describe the collected variables.
3 Results
3.1 Phase I
3.1.1 Lifestyle medicine and related Saudi Arabia, MENA contextual definitions
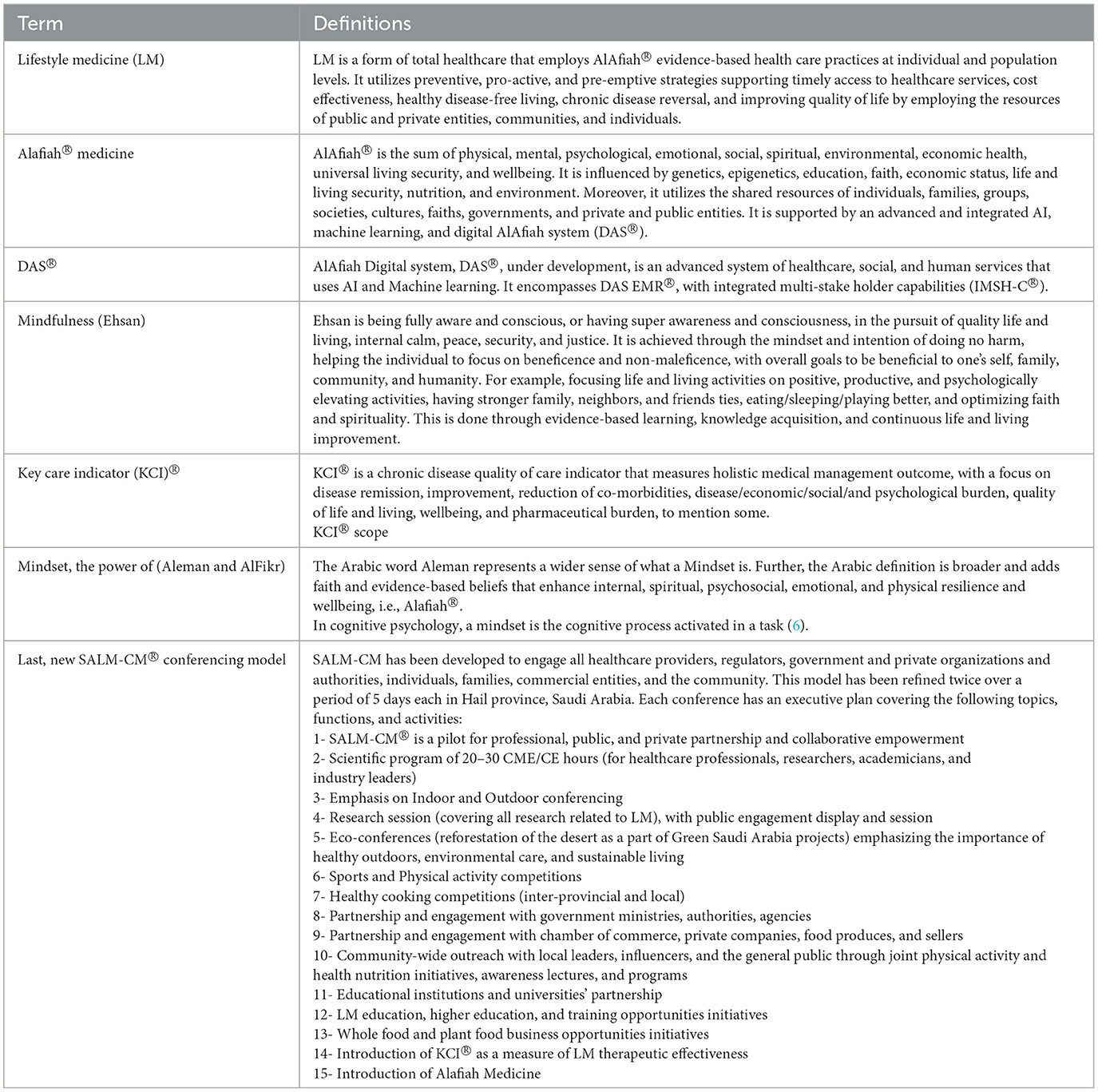
For Saudi Arabia and MENA countries, the consensus panel has unanimously adopted Dr. Alrajhi's definition of Lifestyle medicine. It is best suited to meet current and future healthcare system transformation needs, published goals, and objectives. It puts LM at the heart of the Saudi Arabian Model of Care (MoC), where it is needed the most (Table 1). In addition, the group agreed on the newly adapted pillars of LM, which are presented in Table 2.
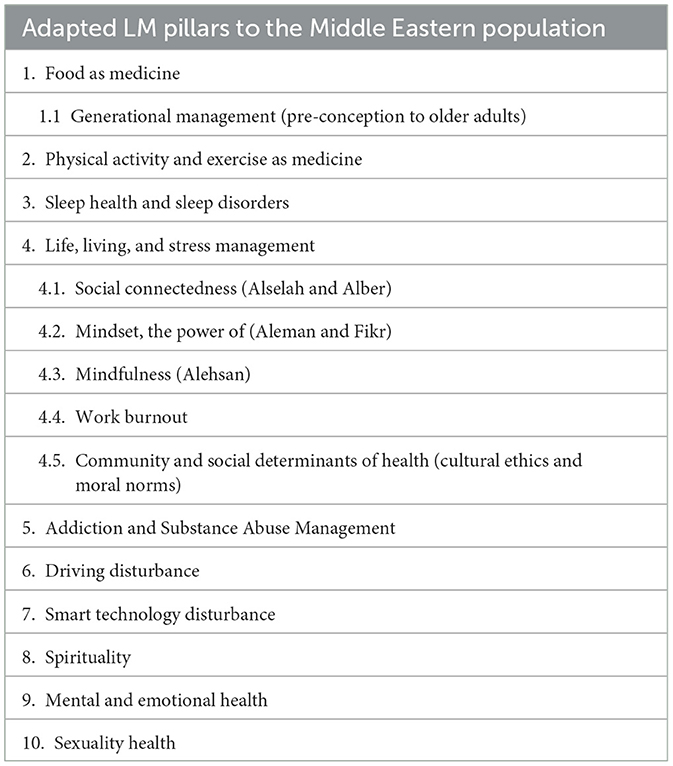
Table 2. The newly adapted LM pillars to the Middle Eastern population according to the task force analysis.
3.2 Phase II
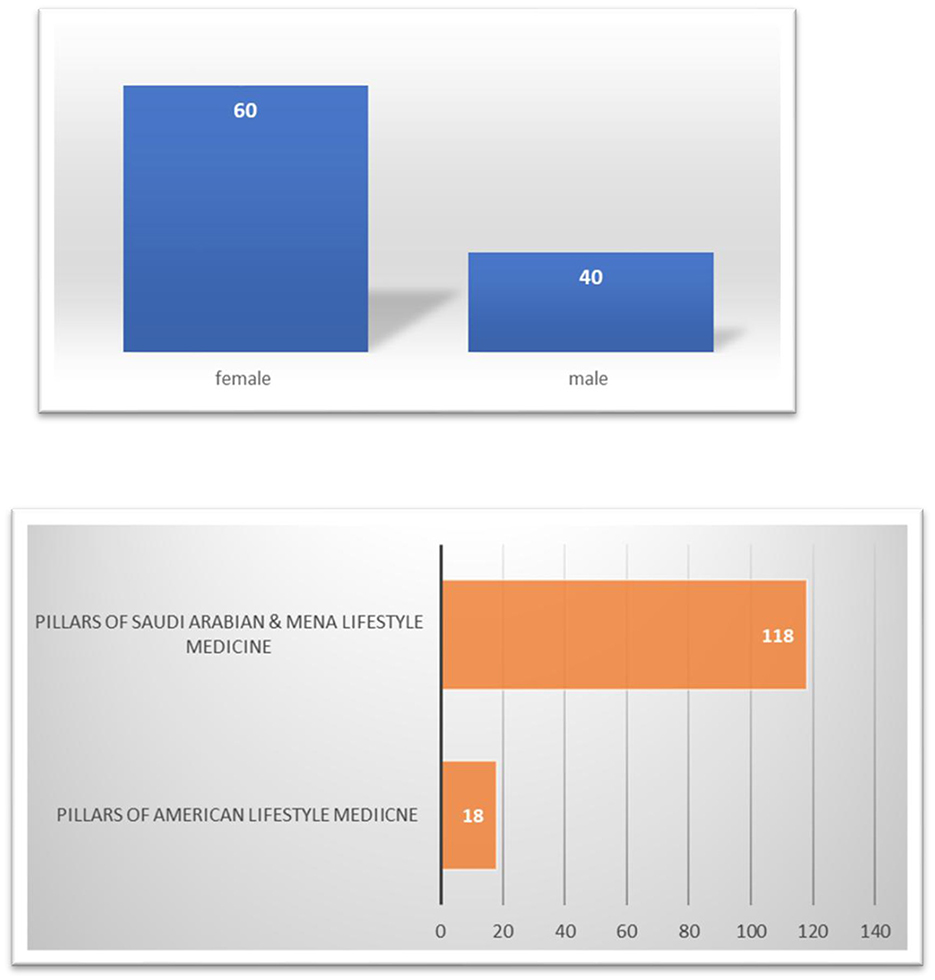
Out of 815 participants who received the survey, 136 completed the questions, while the remaining 679 participants chose to remain neutral and abstained from voting, citing a lack of adequate experience or certification in Lifestyle Medicine.
Among the 136 respondents, 118 professionals voted in favor of adopting the newly adapted pillars tailored for Saudi Arabia and the MENA region, whereas 18 professionals opted to retain the American Lifestyle Medicine pillars (Figure 1). The majority of respondents were female (60%), with the remaining 40% being male. Regarding occupations, 70% of participants were physicians, followed by allied health professionals (20%) and researchers or academics (10%).
More than half of the professionals work within healthcare systems, providing direct Lifestyle Medicine (LM) care alongside their primary specialties. The majority of participants (80%) work and live in Saudi Arabia, while a smaller proportion (20%) are from the broader MENA region. The common age range among respondents was 30 to 60 years, with an average age of 45 years.
The neutrality of the 679 participants underscores the importance of having sufficient experience and certification in Lifestyle Medicine to make informed decisions. It also highlights the need for ongoing education and training in this field, ensuring that more healthcare professionals feel confident participating in similar surveys in the future.
4 Discussion
The interplay between Lifestyle Medicine and mental and emotional health is complex and multifaceted. It involves the Social Determinants of Health (SDH) and lifestyle, which are increasingly recognized as critical factors in predicting health outcomes for both populations and individuals. These determinants include the conditions into which people are born, grow, work, live, and age, as well as the broader forces and systems shaping the conditions of daily life. Thus, an individual's lifestyle is inherently intertwined with SDH. Research suggests that up to 80% of chronic diseases and premature deaths could be prevented by avoiding smoking, engaging in regular physical activity, and adhering to a healthy diet (17). Moreover, a healthy lifestyle is positively associated with mental health and wellbeing, reducing the risk of developing mental health conditions or worsening existing ones.
The MENA region faces an increasing burden of lifestyle-related chronic diseases, including obesity, impaired glucose tolerance (IGT), type 2 diabetes mellitus (T2DM), hypertension (HTN), coronary artery disease (CAD), various cancers, and ~242 co-morbid conditions linked to adiposity. This challenge is compounded by inadequate public health policies, high tobacco use, sedentary lifestyles, sleep disorders, and limited access to whole and plant-based foods. Additionally, the widespread consumption of refined and ultra-refined foods, the Standard American Diet (SAD), and processed pre-prepared meals, drinks, snacks, and food items exacerbates the situation (18).
The populations in MENA countries also have unique, faith-oriented factors influencing their lifestyle choices and daily practices. These factors include food preferences, meal frequency, social relationships, physical activity, and decision-making. About 90% of the MENA population shares a common faith, which plays a pivotal role in the lifestyle determinants of health. Faith serves as a core cultural value for both medical staff and patients, guiding concepts such as EMAN (mindset) and EHSAN [mindfulness; (19–21)]. When these concepts are incorporated into medical consultations, they significantly enhance patient acceptance and compliance with chronic disease management.
The region is undergoing an international transformation toward modernization and technology adoption, leading to Westernized food habits and increasingly sedentary lifestyles. Over the past 30–50 years, non-communicable diseases (NCDs) have risen sharply due to lifestyle and environmental changes (22–24), placing an unsustainable demand on healthcare systems globally. This surge in NCDs, including cardiovascular diseases, cancers, respiratory diseases, and diabetes, has escalated healthcare costs and created significant resource allocation challenges, emphasizing the urgent need for effective prevention and management strategies.
In response, the Saudi National Lifestyle Medicine Group has developed an adaptation of the six pillars of Lifestyle Medicine, as originally defined by the American College of Lifestyle Medicine. This initiative, which began in 2018 and concluded in 2023, resulted in a consensus statement from delegates representing various Arab countries, with the majority of participants residing and working in Saudi Arabia.
A local expert panel, comprising professionals from diverse healthcare specialties, researchers, and academic leaders, formulated a consensus opinion defining the scope and practice of Lifestyle Medicine from both a MENA and Saudi Arabian perspective. This work aligns with the ongoing healthcare transformation in the region, addressing unique societal features, available local resources, and the specific needs of the population. The panel considered the interplay of local factors influencing illness and wellness, including the role of faith, beliefs, food choices, and social determinants of health.
This statement introduces contextualized Lifestyle Medicine (LM) pillars tailored for the Arab and MENA populations, integrating cultural and historical contexts, ethical and moral foundations, mental health, and self-satisfaction. It incorporates new concepts such as Eman and Fikr as fundamental components of mindset.
The definition of mindset within this framework includes beliefs, values, social and marital principles, financial dealings, and an individual's outlook on life, all shaped by personal experiences and acquired knowledge (19).
The MENA contextual definition of mindset refers to an established set of beliefs, concepts, doctrines, and attitudes shaped by experience and/or knowledge. It applies to individuals, families, communities, tribes, nations, or faith-based homogeneous groups and encompasses perspectives on morality, generational and global relationships, history, virtue, culture, social and marital principles, financial and economic dealings, values, and life principles.
Additionally, this mindset definition includes interpretations of justice, human rights, civil rights, hierarchies, governance, leadership, meaning of life, frame of mind, worldview, judgment principles, and overall disposition.
The collective components of a mindset drive decision-making, actions, reactions, acceptance and rejection, motivation, effort, allegiance, change, creativity, adaptation, and innovation in navigating life's continuum. It serves as the reference framework against which all aspects of life are evaluated for approval, adoption, rejection, disapproval, action, or reaction. Mindset is a complex set of cognitive processes that individuals use to arrive at justified, actionable decisions with minimal regrets (19, 21).
Additionally, the concept of EHSAN (mindfulness) emphasizes total effort and the pursuit of optimal outcomes, promoting better sleep, healthier eating habits, stress reduction, productivity, leisure, and physical activity. New pillars also address driving disturbances and the misuse of smart technology, acknowledging their significant impact on health.
Integrating spirituality into Lifestyle Medicine can enhance health outcomes by fostering wellness, increasing satisfaction with care, and improving medical decision-making (25). Spirituality and Lifestyle Medicine are interconnected in multiple ways. Research demonstrates a strong association between medicine, faith, religion, and spirituality. Spirituality is defined as the way individuals and groups seek and express meaning and purpose in life, experiencing social and faith-based connectedness with themselves, others, and the Almighty. It significantly influences wellness, satisfaction with care, medical decision-making, and overall health outcomes.
Despite its significance, the healthcare industry largely overlooks the role of faith and spirituality in wellbeing and illness. Research indicates that participation in faith-based religious communities is associated with healthier lives, greater longevity, lower rates of depression, reduced suicidal tendencies, and minimal to no substance abuse. Thus, integrating spirituality into Lifestyle Medicine pillars has the potential to enhance health outcomes and patient care (26).
Additionally, new concepts such as B'err and S'lah have been adopted to reflect the MENA region's strong emphasis on social connectedness, family ties, and community cohesion.
Furthermore, Lifestyle Medicine, sexuality, sexually transmitted infections (STIs), sexual behavior, and human connectedness are deeply interconnected. Sexuality is fundamental to human life, influencing healthy relationships from early adulthood through old age. Risky sexual behaviors can increase the likelihood of STIs, underscoring the need for preventive strategies within Lifestyle Medicine. This discipline seeks to understand the physical and psychological factors contributing to sexual health concerns. Unhealthy lifestyle choices—such as obesity, tobacco smoking, alcohol and substance abuse, and chronic stress—can lead to sexual dysfunctions, further highlighting the importance of integrating Lifestyle Medicine principles into sexual health management.
Human connectedness plays a crucial role in sexual health. Healthy relationships contribute to planned pregnancies and disease prevention, while sexual dysfunction may serve as an early indicator of future non-communicable diseases (NCDs), such as cardiovascular and metabolic disorders. Therefore, promoting healthy lifestyles is essential for ensuring a satisfying sexual quality of life (27).
Additionally, driving disturbances and smart technology disturbances were introduced as additional Lifestyle Medicine pillars. Maladaptive motor vehicle driving, which leads to serious car accidents, is the leading cause of death in Saudi Arabia. Similarly, the maladaptive use and abuse of smart technology have been identified as major contributors to sleep disturbances, mental and psychosocial disorders, obesity, and co-morbid diseases.
The phase two statement had several limitations, including its reliance on web-based surveys and a cross-sectional study design. The online platform restricted participation to individuals with internet access and those known to the statement group. Nonetheless, the statement's unique structure and its representation of the region remain significant.
5 Policymakers and lifestyle academy recommendation
A consensus opinion was formulated stating the following:
1. Maintaining and building upon the 6 pillars of commonly accepted lifestyle medicine specialty
2. Adapting the 6 pillars in number 1 to serve the local population, healthcare resources, and application needs.
3. Adding new pillars or sub-pillars to cover lifestyle-rooted causes of morbidity and mortality unique to the MENA, Saudi Arabia, region/country.
4. Expanding some pillars to suit local needs
5. Employing the full potential of LM for professional development, stakeholders, and community engagement.
6 Research recommendation or thoughts
6.1 Points for reflection and food for thought
Can the Saudi healthcare system adopt preventive, proactive, and pre-emptive care alongside wellness-focused initiatives, leveraging the strength of its infrastructure? Is there a determined commitment to positioning Saudi Arabia as a global leader in proactive health and wellness care? Furthermore, is there a formal strategy to incentivize wellness and sustain it effectively? Could the development of a medically driven reward system motivate individuals and contribute to achieving Alafiah?
Does Saudi Arabia have any way to re-distinguish itself, as it did with vaccinations?
7 Conclusions
The LM pillars have been expanded to address the professional and community needs in Saudi Arabia, serving as a model for other MENA countries and societies.
Rather than focusing solely on stress management as a contributor to ill health, a broader pillar, Life and Living Management, has been introduced. This expanded pillar encompasses stress, social and work interpersonal interactions, interdependence, work-related and social stress, as well as life and living resource management.
Additionally, concepts such as mindset, mindfulness, and social connectedness, which are deeply embedded in local faith teachings and practices, have been redefined and expanded to reflect local orientations. These elements have been integrated as highly effective tools to deliver care plans, facilitate life and living management, provide resilience training, and enhance compliance with LM therapeutic interventions.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Review Board at King Fahad Medical City, Riyadh second cluster. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SAlr: Conceptualization, Resources, Validation, Writing – original draft, Writing – review & editing. AK: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. NAlh: Data curation, Investigation, Formal analysis, Writing – review & editing. FA: Project administration, Resources, Validation, Writing – review & editing. AA: Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. RA: Methodology, Investigation, Writing – review & editing. HA: Data curation, Writing – review & editing. SAlb: Data curation, Formal analysis, Conceptualization, Writing – review & editing. NAls: Data curation, Formal analysis, Methodology, Writing – review & editing. FA: Writing – review & editing. MA: Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing. EK: Investigation, Validation, Writing – review & editing. SL: Data curation, Validation, Writing – review & editing. ST: Investigation, Validation, Writing – review & editing. RT: Investigation, Validation, Writing – review & editing. TA: Investigation, Methodology, Writing – review & editing. KA: Investigation, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction note
This article has been corrected with minor changes. These changes do not impact the scientific content of the article.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AI, Artificial intelligence; CAD, coronary artery disease; CPG, clinical practice guidelines; DAS®, Digital AlAfiah system; DAS EMR®, Digital AlAfiah system Electronic health record; HTN, hypertension; IGT, impaired glucose tolerance (regulation); IMSH-C, integrated multi-stake holder capabilities; LM, Lifestyle medicine; MENA, Middle eastern and north African countries; MoC, Model of Care; NCDs, Non-Communicable Diseases; PCOS, polycystic ovarian syndrome; SALM-CM®, Saudi Arabia, LM conferencing model; SSDH, society-specific determinants of health; T2DM, type 2 diabetes mellitus; TOT, training of trainers.
Footnotes
References
1. Vodovotz Y, Barnard N, Hu FB, Jakicic J, Lianov L, Loveland D, et al. Prioritized research for the prevention, treatment, and reversal of chronic disease: recommendations from the lifestyle medicine research summit. Front Med. (2020) 7:585744. doi: 10.3389/fmed.2020.585744
2. ScienceDaily. How Lifestyle Affects Our Genes. (2019). Available at: https://www.sciencedaily.com/releases/2019/04/190423133451.htm (accessed April 23, 2019).
3. International Journal of Molecular Sciences. Genes and Diet in the Prevention of Chronic Diseases in Future Generations. (2020). Available at: https://www.mdpi.com/1422-0067/21/7/2633 (accessed April 10, 2020).
4. The Journals of Gerontology. Genetic Risks for Chronic Conditions: Implications for Long-term Wellbeing. (2018). Available at: https://academic.oup.com/biomedgerontology/article/73/4/477/4079819 (accessed March, 2018).
5. Frontiers in Public Health. Transforming Global Approaches to Chronic Disease Prevention and Management Across the Lifespan. (2023). Available at: https://www.frontiersin.org/journals/publichealth/articles/10.3389/fpubh.2023.1248254/full (accessed October 13, 2023).
6. Mahmood FM. Prevalence and prevention of lifestyle-related diseases in Saudi Arabia. Int J Health Sci. (2018) 12:1–2.
7. Tyrovolas S, El Bcheraoui C, Alghnam SA, Alhabib KF, Almadi MA, Al-Raddadi RM, et al. The burden of disease in Saudi Arabia 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Planet Health. (2020) 4:e195–208. doi: 10.1016/S2542-5196(20)30075-9
8. Sayburn A. Lifestyle medicine: a new medical specialty? BMJ. (2018) 363:k4442. doi: 10.1136/bmj.k4442
9. Institute for Population Health (IPH) of Weill Cornell Medicine-Qatar (WCM-Q). The Doha Declaration on Lifestyle Medicine. (2024). Available at: https://www.eurekalert.org/news-releases/1045437 (accessed May 18, 2024).
10. Lifestyle Medicine Global Alliance (LMGA). Lifestyle Medicine Global Alliance. (2024). Available at: https://www.lifestylemed.org/
11. Barakat H. The Arab World: SOCIETY, Culture, and State. Oakland, CA: Univ of California Press (1993).
12. Chowdhury S, Mok D, Leenen L. Transformation of health care and the new model of care in Saudi Arabia: kingdom's vision 2030. J Med Life. (2021) 14:347–54. doi: 10.25122/jml-2021-0070
13. Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. (2007) 12:10.
14. Keeney S, Hasson F, McKenna H. The Delphi Technique in Nursing and Health Research. Wiley-Blackwell (2011).
15. Kennedy HP. Enhancing Delphi research: methods and results. J Adv Nurs. (2004) 45:504–11. doi: 10.1046/j.1365-2648.2003.02933.x
16. Linstone HA, Turoff M. The Delphi Method: Techniques and Applications. Oklahoma: Addison-Wesley Educational Publishers Inc. (2011).
17. Banerjee A, Modha S, Perel P. Non-communicable diseases: research priorities to mitigate impact of health system shocks. BMJ. (2024) 387:e078531. doi: 10.1136/bmj-2023-078531
18. World Health Organization (WHO). WHO Maps Noncommunicable Disease Trends in All Countries. (2011). Available at: https://www.who.int/news/item/21-10-2011-who-maps-noncommunicable-disease-trends-in-all-countries
19. French RP II. The fuzziness of mindsets: divergent conceptualizations and characterizations of mindset theory and praxis. Int J Organ Anal. (2016) 24:673–91. doi: 10.1108/IJOA-09-2014-0797
20. Chang MC, Chen PF, Lee TH, Lin CC, Chiang KT, Tsai MF, et al. The effect of religion on psychological resilience in healthcare workers during the coronavirus disease 2019 pandemic. Front Psychol. (2021) 12:628894. doi: 10.3389/fpsyg.2021.628894
21. Barakat S. Postwar reconstruction and the recovery of cultural heritage: critical lessons from the last fifteen years. Cultural heritage in postwar recovery. (2007) 2:26–37.
22. Oni T, Unwin N. Why the communicable/non-communicable disease dichotomy is problematic for public health control strategies: implications of multimorbidity for health systems in an era of health transition. Int Health. (2015) 7:390–9.
23. EurekAlert!. Global Leaders in Lifestyle Medicine Mark Lifestyle Medicine Week with Declaration for Urgent Actions to Address Burden of Non-communicable Diseases. (2024). Available at: https://www.eurekalert.org/news-releases/1045437 (accessed May 18, 2024).
24. Taheri Soodejani M. Non-communicable diseases in the world over the past century: a secondary data analysis. Front Public Health. (2024) 12:1436236. doi: 10.3389/fpubh.2024.1436236
25. Puchalski CM. The role of spirituality in health care. Proc (Bayl Univ Med Cent). (2001) 14:352–7. doi: 10.1080/08998280.2001.11927788
26. Isaac KS, Hay JL, Lubetkin EI. Incorporating spirituality in primary care. J Relig Health. (2016) 55:1065–77. doi: 10.1007/s10943-016-0190-2
27. World Economic Forum. Non-communicable Diseases (NCD) Heat Map. (2024). Available at: https://www.weforum.org/pages/non-communicable-diseases-heat-map/ (accessed January 14, 2024).
Appendix A
Survey questions
1-Do you think that the 6 pillars of lifestyle medicine are sufficient for the needs of Saudi Arabia and MENA region's population?
Whole Food, Plant-based Nutrition
Physical Activity
Stress Management
Avoidance of Risky Substances
Restorative Sleep
Social Connection
Strongly agree: Agree: Neutral: Disagree: Strongly disagree:
2-Do you think that the 6 pillars of lifestyle medicine's practice and principles can be adapted, expanded, and customized to meet regional and local population healthy living needs?
MENA Saudi Arabia Lifestyle Medicine Pillars adapted and expanded from ACLM pillars
1. Food as medicine
1.1. Generational management (pre-conception to older adults)
2. Physical activity as medicine
3. Sleep health
4. Life and Chronic Stress Management
4.1 Social connectedness (Alselah and Alber)
4.2 Mindset, the power of (Aleman and Fikr)
4.3 Mindfulness (Alehsan)
4.4 Work burnout
4.5 Community and social determinants of health (cultural ethics and moral norms)
5. Addiction and Substance Abuse Management
5.1 Tobacco use
5.2 Alcohol use
5.3 Illegal drugs use
6. Driving disturbance
6.1 MVA reduction and prevention
7. Smart technology disturbance
8. Sexuality health
Strongly agree: Agree: Neutral: Disagree: Strongly disagree:
Keywords: Hail Lifestyle Medicine consensus, Lifestyle Medicine, Middle Eastern and North African countries (MENA), Saudi Arabia, LM conferencing model (SALM-CM®), digital AlAfiah system (DAS®)
Citation: Alrajhi S, Konswa AA, Alhamdi N, Alshammari F, Alqurashi A, Alraddadi R, Alfheeaid H, Albattal S, Alsoqih N, Almuhaileb F, Alnais M, Kunonga E, Latif S, Tanigawa Guimaraes S, Tariq R, Albishri T and Alrasadi K (2025) Hail Lifestyle Medicine consensus position statement as a medical specialty: Middle Eastern perspective. Front. Public Health 13:1455871. doi: 10.3389/fpubh.2025.1455871
Received: 27 June 2024; Accepted: 05 February 2025;
Published: 20 June 2025; Corrected: 16 September 2025.
Edited by:
Fahad Hanna, Torrens University Australia, AustraliaReviewed by:
Abel Negussie, Yirgalem Hospital Medical College, EthiopiaCopyright © 2025 Alrajhi, Konswa, Alhamdi, Alshammari, Alqurashi, Alraddadi, Alfheeaid, Albattal, Alsoqih, Almuhaileb, Alnais, Kunonga, Latif, Tanigawa Guimaraes, Tariq, Albishri and Alrasadi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alaa Alqurashi, QS5BbFF1cmFzaGlAZ3VsZmNkYy5vcmc=
†Present address: Alaa Alqurashi, Gulf Center for Disease Control and Prevention (CDC), Riyadh, Saudi Arabia
 Saleh Alrajhi1
Saleh Alrajhi1 Ayman Afify Konswa
Ayman Afify Konswa Nisreen Alhamdi
Nisreen Alhamdi Alaa Alqurashi
Alaa Alqurashi Rajaa Alraddadi
Rajaa Alraddadi Rabbanie Tariq
Rabbanie Tariq