- Healthcare-Associated Infection Control Center, Sichuan Academy of Medical Sciences, Sichuan Provincial People's Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, Sichuan, China
Background and aim: Various reasons have hindered accurate reporting of the central line-associated bloodstream infection (CLABSI) rates in China’s hospital ICUs. This study conducts a meta-analysis to provide a precise assessment of CLABSI rates in these units.
Methods: Adhering to the PRISMA guidelines, a systematic search was conducted in PubMed, Web of Science, Embase, CNKI, Wanfang and Weipu from January 2008 to December 2023. Selection of literature followed strict criteria, ensuring relevant data extraction. A random-effects model facilitated the meta-analysis.
Results: The analysis incorporated 23 studies (PubMed: 5, Web of Science: 4, Embase: 1, CNKI: 9, Wanfang: 2, Weipu: 2). It revealed an overall weighted CLABSI rate in China’s ICUs of 2.65‰ (95% CI: 2.57–2.73‰), with 3.12‰ in adult ICU (95% CI: 2.70–3.54‰) and 2.57‰ in pediatric ICUs (95% CI: 2.49–2.66‰). Notably, adult ICUs in North of China recorded the highest rate at 5.13‰ (95% CI: 4.23–6.02‰), and pediatric ICUs in East of China had 3.35‰ (95% CI: 2.85–3.85‰).
Conclusion: The study indicates that CLABSI rates in China’s ICUs surpass those reported in national healthcare reports and the US CDC-NHSN data. This underscores the urgency for enhanced surveillance and infection control. The findings stress the need for standardized surveillance definitions and methods to truly represent CLABSI epidemiology and develop effective prevention strategies.
Introduction
Central line-associated bloodstream infection (CLABSI) is one of the common healthcare-associated infections (HAIs) encountered in intensive care units (ICUs), adversely affecting patient prognoses and resulting in significant economic costs. Surveillance of HAIs initiated by the International Nosocomial Infection Control Consortium (INICC) across various countries globally indicates that the CLABSI rates range from 2–147.3 per 1,000 central line days. CLABSI is associated with an additional mortality rate of 3.2 to 75.1%, an increase of 1.3–26.2 days in hospital stay, and additional costs ranging from US $ 4,888.42 to11,590.93 (1).
In February 2021, the National Health Commission of China established the 2021 National Medical Quality and Safety Improvement Goals, which included the reducing the incidence rate of intravascular catheter-related bloodstream infections as the ninth goal. It emphasized the need for comprehensive measures to intervene, ensuring medical safety and patient rights. The National Medical Service and Quality Safety Report reveals considerable variation in the reported CLABSI rates across different medical specialties. The specialty of intensive care medicine has reported a rate of 2.07–3.10 per 1,000 central line days (2), whereas the specialty of HAI management reported a notably lower rate of only 0.57–1.01per 1,000 central line days (3). While these discrepancies may be due to differences in the hospitals and time frames of the reports, other factors cannot be overlooked, such as unclear definitions for surveillance, subjective methods of surveillance, and varying definitions of the same indicators among different specialties. The actual CLABSI rates in ICUs of Chinese hospitals remains unclear and may be underestimated.
To address these challenges and provide a more accurate depiction of CLABSI rates in ICUs of Chinese hospitals, our study conducted a comprehensive meta-analysis. Relevant data from both Chinese and English literature rigorously selected and published from January 2008 to December 2023 were collated.
Methods
Search strategy
Following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: PRISMA Statement, a comprehensive literature search was conducted in the PubMed, Web of Science, Embase, CNKI, Wanfang, and Weipu database. For each database, the search strategy was provided in the Supplementary file. All the literature published from January 2008 to November 2023 were searched.
Selection criteria
Inclusion criteria
Descriptive studies about or involving CLABSI in Chinese hospitals ICUs.
Exclusion criteria
Abstract Exclusion Criteria: (1) non-descriptive (experimental) studies and analytical studies such as case–control studies and cohort studies. (2) Studies not involving CLABSI. (3) Studies with subjects who are not patients in ICUs.
Full-text Exclusion Criteria: (1) studies solely focusing on CLABSI caused by a specific pathogen. (2) Catheters other than central lines, such as arterial catheters, arteriovenous fistulas, atrial catheters, extracorporeal membrane oxygenation (ECMO), hemodialysis catheters, intra-aortic balloon pump (IABP) devices, peripheral veins catheters, ventricular assist devices (VAD), etc. (3) Studies that do not describe the definition of CLABSI, or use a definition of CLABSI that is inconsistent with the definition by the U.S. CDC NHSN, or only describe the use of China’s Nosocomial Infection Diagnostic Criteria (2001 Trial version) as definition. (4) Studies with original data that only report the CLABSI rates without reporting the number of central line days or the number of CLABSI cases.
Data extraction
The following information from the eligible full texts was extracted: title, the first author, publication year, study period, city or region, number of hospitals, number of ICUs, catheter type, number of CLABSI cases, and central line days. Data verification was performed through cross-checking by two researchers.
Quality assessment
Two researchers independently conducted literature screening and quality assessment based on inclusion and exclusion criteria. In cases of disagreement, a third researcher was involved in the discussion to resolve the issue. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement checklist was used to assess the quality of all studies. The standards were as follows: High Quality (meeting more than 75% of the criteria), Medium Quality (meeting 50–75% of the criteria), and Low Quality (meeting less than 50% of the criteria).
Statistical analysis
All statistical analyses were performed with Statistical Software-STATA, version 18.0. A meta-analysis was conducted using the Metaprop command. The CLABSI rate = the number of CLABSI cases/the number of central line days*1000. The pooled and weighted CLABSI rates, along with the 95% Confidence Intervals (95% CI), were calculated within a random-effects model and represented in forest plots. Heterogeneity was evaluated using the I2 index, and given the substantial heterogeneity (I2 > 75%), we employed a random-effects model, which is methodologically more appropriate for meta-analysis with considerable inter-study variability. The subgroup analysis was subjected based on ICU types and regions. During the subgroup analysis, different types of adult ICUs were categorized into medical ICUs, surgical ICUs, and general ICUs according to their specialty. When the city of the ICU was not clearly identifiable, the subgroup analysis was conducted based on the region. The subgroup analysis was performed to characterize the distribution of CLABSI rates across different ICU types and geographic regions, rather than to test for intergroup differences. Due to the imbalanced sample sizes among subgroups, formal statistical comparisons between groups were not conducted. Publication bias was assessed by funnel plots.
Results
Search results
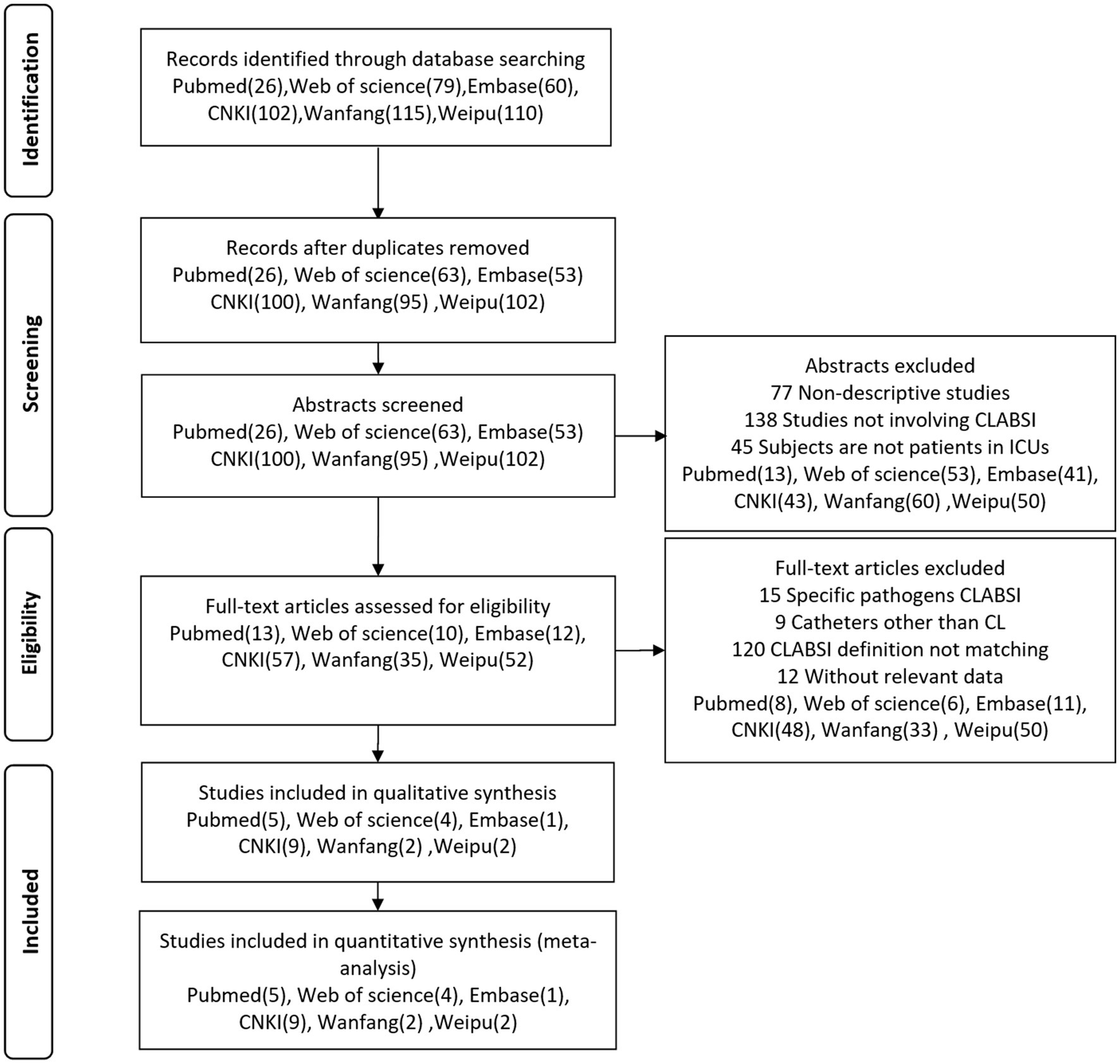
We retrieved 395 relevant articles from the PubMed (26), Web of Science (79), Embase (60), CNKI (102), Wanfang (115) and Weipu (110) databases, which were reduced to 333 after removing duplicates. Upon initial screening of titles and abstracts, 260 articles were excluded, and another 156 were excluded after full-text review. Ultimately, 23 articles (PubMed: 5, Web of Science: 4, Embase: 1, CNKI: 9, Wanfang: 2, Weipu: 2) were included for data extraction and analysis. Figure 1 showed the literature screening and selection process.
Studies included for analysis, quality assessment and publication bias
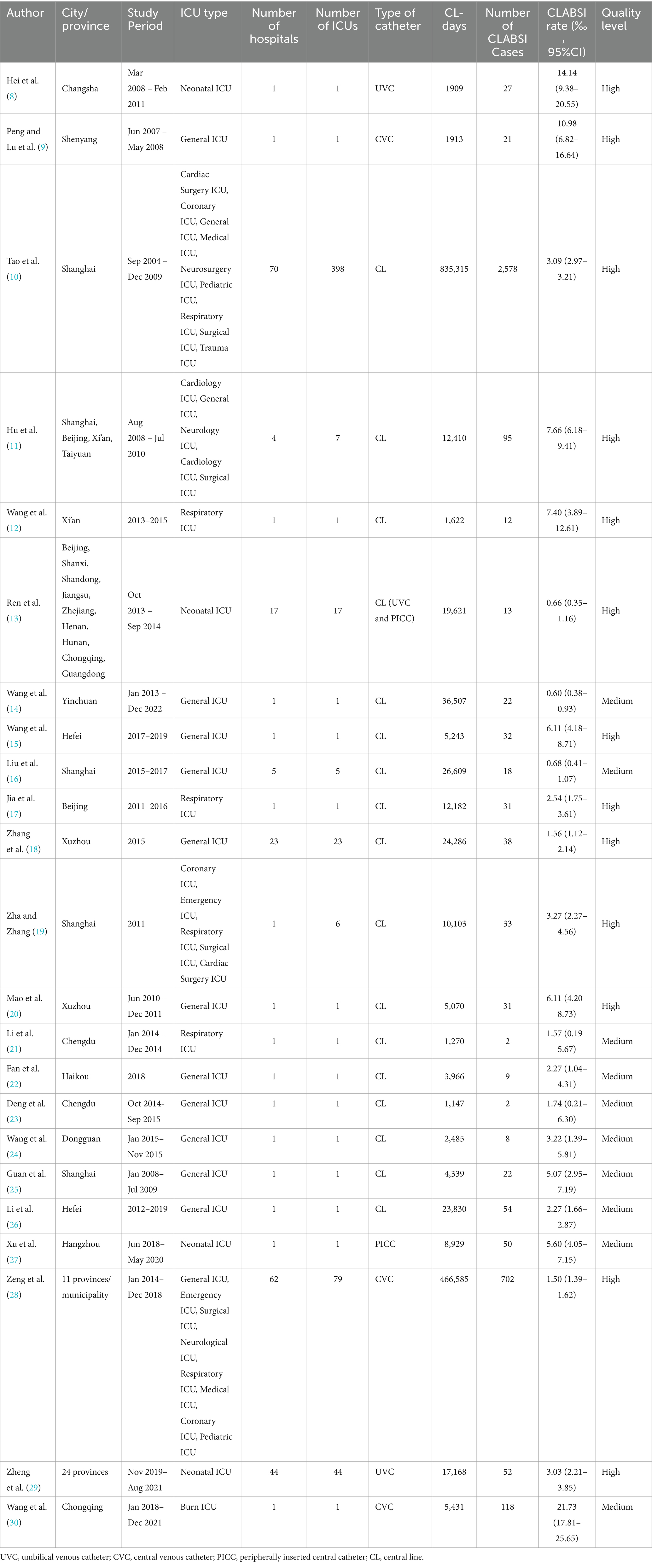
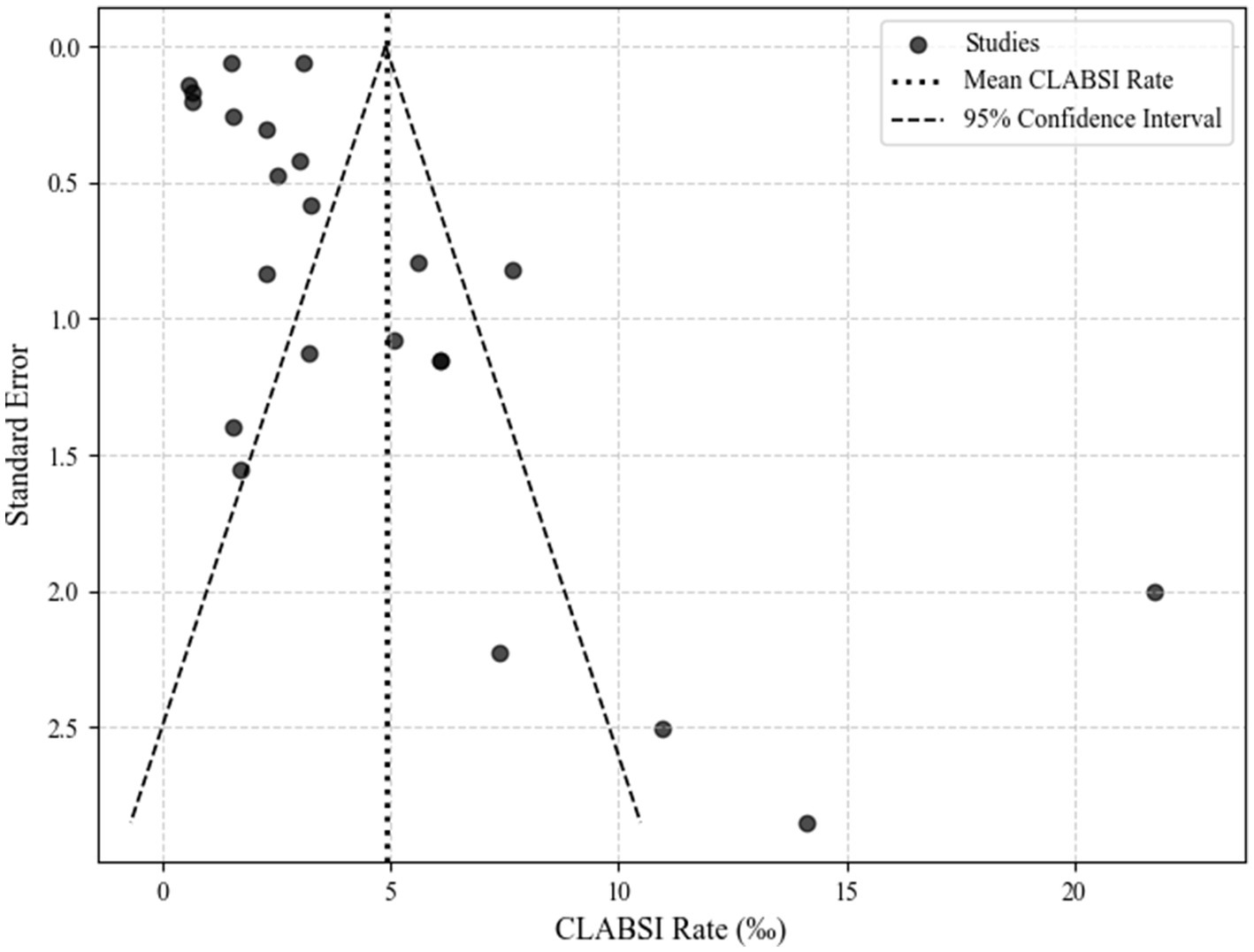
This manuscript encompasses an analysis of 23 studies, spanning from 2008 to 2023, which report on the CLABSI rates in various types of ICUs across different cities and areas. The quality of these studies was rigorously assessed using the STROBE checklist. Information and quality assessment results of each study are presented in Table 1. The funnel plot revealed that the studies included in this analysis were distributed asymmetrically outside the funnel’s symmetry range, suggesting the presence of publication bias. The publication bias assessment funnel plot is detailed in Figure 2.
The CLABSI rates in different types of ICUs
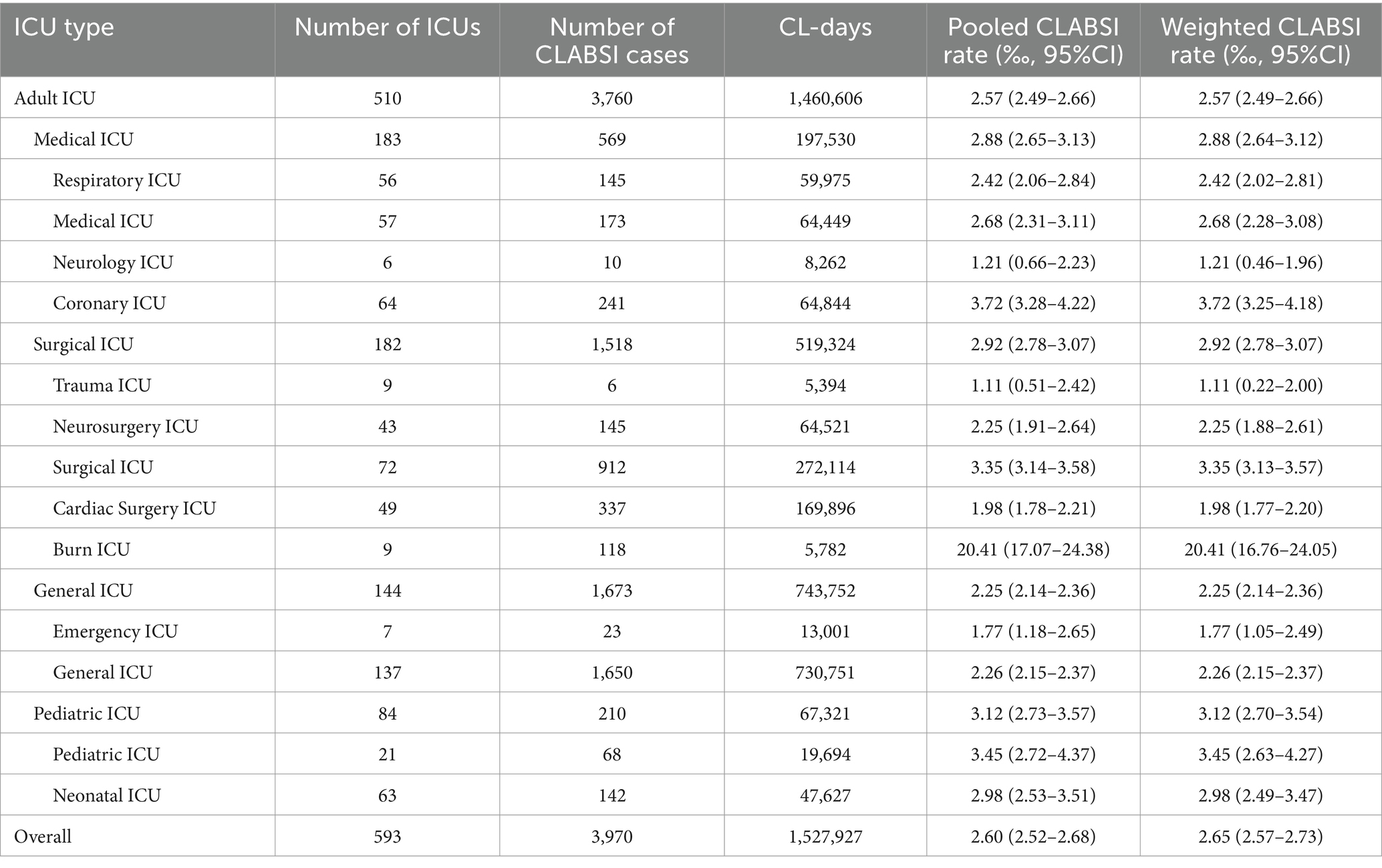
The overall weighted CLABSI rate across all ICU types is 2.65‰ (95% CI: 2.57–2.73‰). A notable observation is that pediatric ICUs exhibit a slightly higher rate compared to adult ICUs, with pediatric ICUs at 3.12‰ (95% CI: 2.70–3.54‰) versus 2.57‰ (95% CI: 2.49–2.66‰) in adult ICUs. Within the adult ICU category, Surgical ICUs recorded the highest rate at 2.92‰ (95% CI, 2.78–3.07‰). Table 2 provides a detailed breakdown of pooled and weighted CLABSI rates across different ICU types.
The CLABSI rates in adult and pediatric ICUs
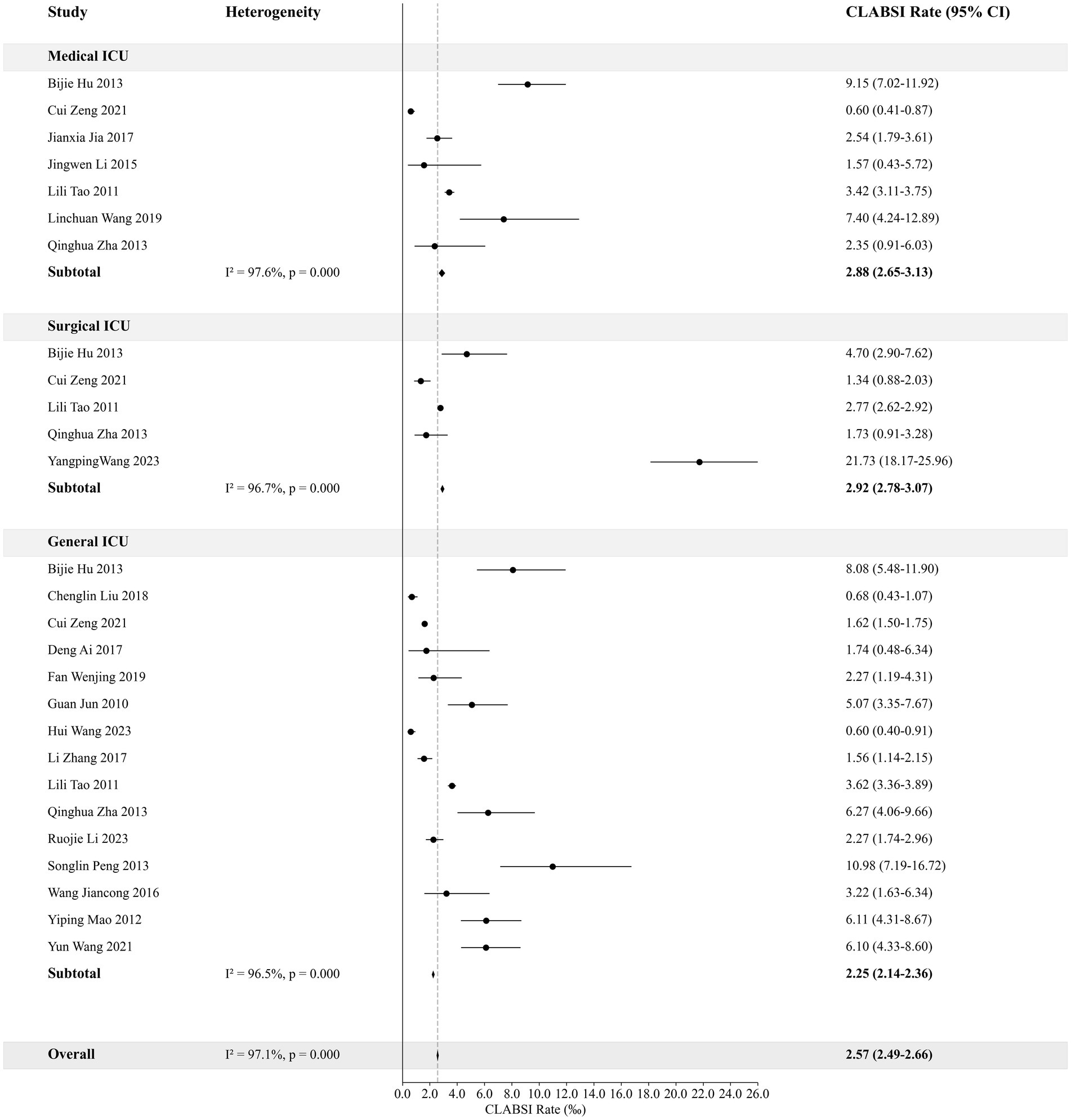
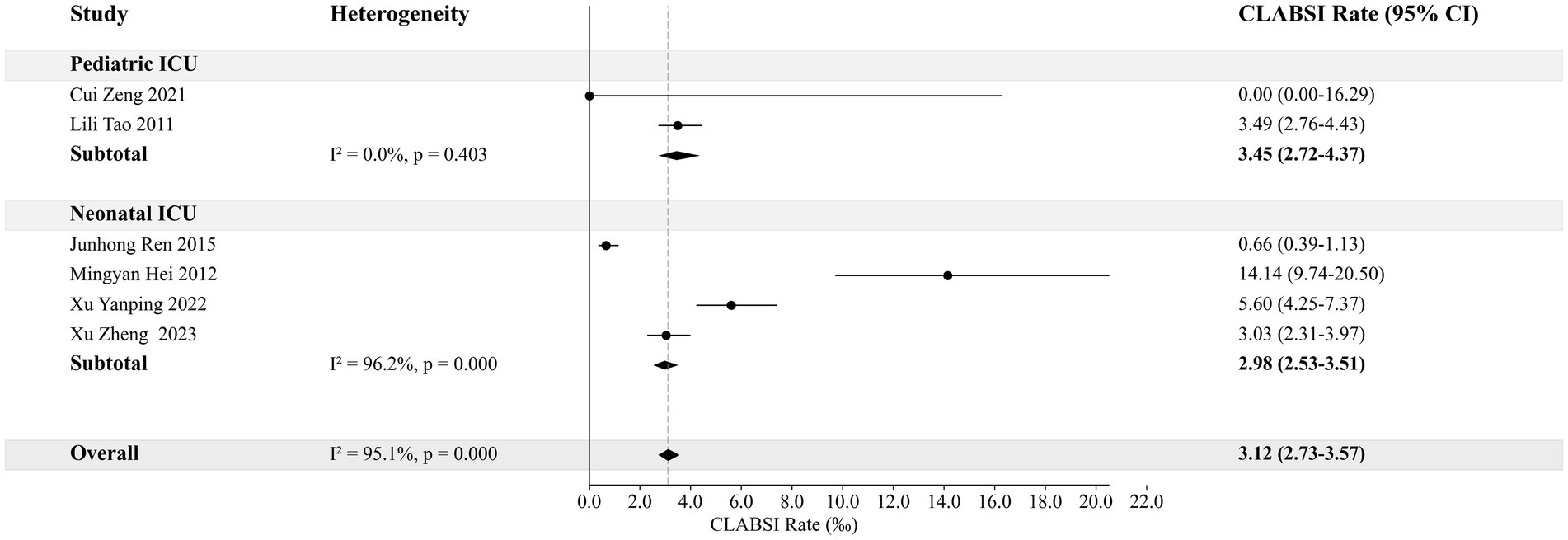
This analysis categorizes adult ICUs based on their specialty into Medical ICU, Surgical ICU, and General ICU, and compares their CLABSI rates. The weighted rate for Medical ICU is 2.88‰ (95% CI: 2.65–3.13‰), for Surgical ICU is 2.92‰ (95% CI: 2.78–3.07‰), and for General ICU is 2.25‰ (95% CI: 2.14–2.36‰). For pediatric ICUs, the weighted rates are 3.45‰ (95% CI: 2.72–4.37‰) for Pediatric ICU and 2.98‰ (95% CI: 2.53–3.51‰) for Neonatal ICU. Figures 3, 4 provide detailed visual representations of these data.
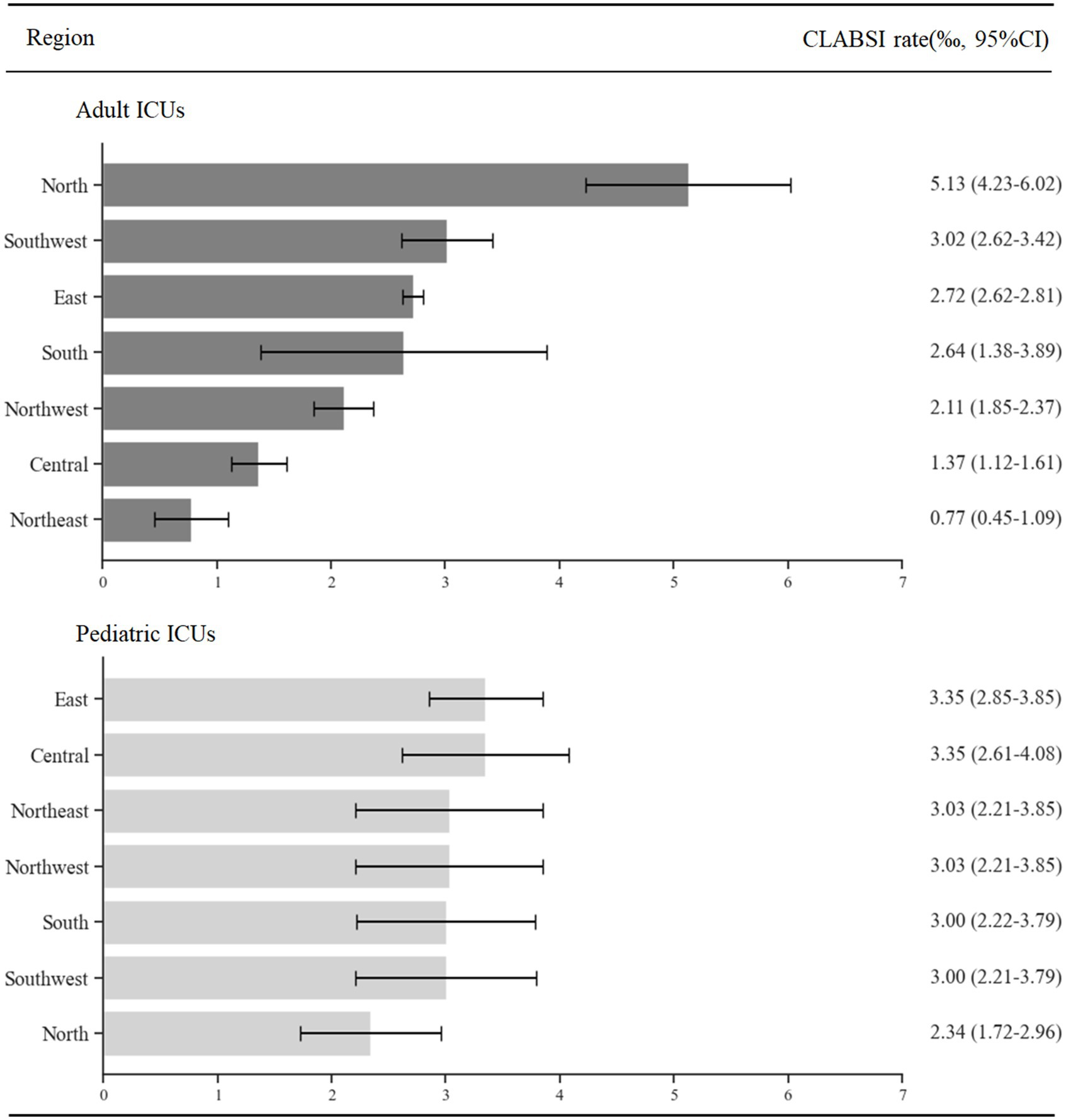
The CLABSI rates in ICUs of different regions
This section presents a detailed analysis of CLABSI rates in ICUs, organized by the region. The data, derived from various studies, categorizes hospitals by their location. For adult ICUs, the CLABSI rates, in descending order, are observed as follows: North, Southwest, East, South, Northwest, Central and Northeast of China, in pediatric ICUs, the rates follow this sequence from highest to lowest: East, Central, Northeast, Northwest, South, Southwest and North of China. Figure 5 provides a comprehensive display of the weighted rates of CLABSI in the ICUs across each mentioned region.
Discussion
In the literature on catheter-associated bloodstream infections, two definitions are commonly discussed: Catheter-Related Bloodstream Infection (CRBSI) and Central Line–Associated Bloodstream Infection (CLABSI). CRBSI, a clinical definition used for diagnosis, involves the patient’s symptoms and requires the culture of the same pathogen from both peripheral and catheter blood, often showing higher bacterial quantification in the latter. This definition pinpoints the catheter as the bacteria source (4). Despite its rigor, CRBSI’s practical application in clinical settings faces challenges, such as the lack of quantitative cultures in some hospitals, suboptimal practices in blood culture sample submission, and a generally low positivity rate in blood cultures. These factors could lead to an underestimation of CRBSI incidence. On the other hand, CLABSI is an epidemiological definition used for disease surveillance, focusing on laboratory-confirmed bloodstream infections in patients with central lines, when no other infection source is identified (5). The CDC in the United States has adopted CLABSI for surveillance in NHSN reports since 2008 due to its greater sensitivity and accessibility compared to CRBSI, making it a globally used definition for HAI surveillance and infection control quality improvement. This is the reason why January 2008 was selected as the starting point for the literature search in this study.
The National Health Commission of China, recognizing these international standards, integrated both CRBSI and CLABSI definitions in its 2010 Guideline for Prevention and Control of Catheter-Related Bloodstream Infection (Trial version). This guideline, however, did not mandate simultaneous positivity and identical pathogens in peripheral and catheter blood, leaning closer to the CLABSI definition (6). Further expanding the scope, the 2021 Guideline for Prevention and Control of Vessel Catheter-Associated Infection included all intravascular catheters and both bloodstream and local infections at the insertion site (7). Despite these advancements, discrepancies in catheter duration definitions among CRBSI, CLABSI, and VCAI persist (4–7), with clinicians often favoring CRBSI, potentially leading to underreported incidence rates. Our study, focusing on clarity and precision, favored studies using CLABSI or similar definitions, aiming to reduce the impact of these discrepancies.
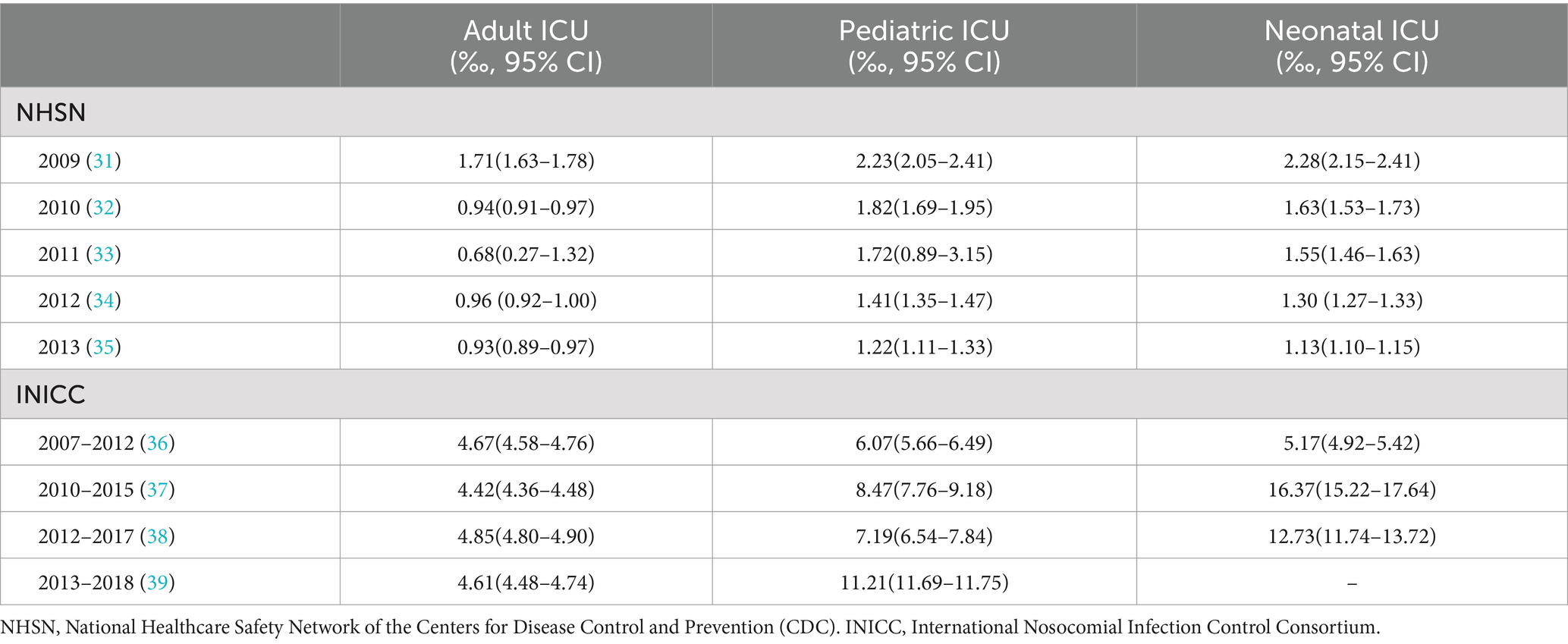
Our study revealed that the CLABSI rates in Chinese hospital ICUs (both adult and pediatric) were higher than the rates reported by the NHSN for American hospital ICUs (adult ICU: 2.57‰ vs. 0.93–1.71‰, pediatric ICU: 3.12‰ vs. 1.22–2.23%, neonatal ICU: 2.98‰ vs. 1.13–2.28‰). However, these rates were lower than those reported by the INICC (showed in Table 3), reflecting the National Health Commission of China’s and hospitals’ achievements in HAI prevention and control. The 2010 guideline played a pivotal role in reducing CLABSI rates in China by raising healthcare personnel awareness and compliance with prevention and control practices. Yet, this also underlined the existing gaps in CLABSI prevention and control between Chinese and U.S. hospitals. China needs to continue striving for improvements in policy enforcement, healthcare personnel training, medical resource optimization, and HAI surveillance enhancement.
However, significant challenges remain in standardizing China’s HAI surveillance. The overall CLABSI rate showed in our study was slightly higher than that reported in the National Medical Service and Quality Safety Report for the intensive care specialty (2.65‰ vs. 0.57–3.1‰), and significantly higher than the data reported by the HAI management specialty (2.65‰ vs. 0.57–1.01‰). Discrepancies in CLABSI rates between different data sources highlight these challenges, emphasizing the need for updated HAI definitions and surveillance method standardization.
Our study also had limitations, such as strict inclusion and exclusion criteria preventing comprehensive data aggregation from numerous Chinese hospitals. Particularly, the number of studies meeting the criteria for CLABSI in pediatric and neonatal ICUs is extremely limited. Nonetheless, this stringent approach preserved the integrity of our meta-analysis results. Secondly, there was a high degree of heterogeneity among the studies, although methods such as employing a random-effects model and conducting subgroup analyses were attempted. This might be related to the differences in time periods, geographical regions, hospital levels, healthcare service quality, and adherence to infection prevention and control measures, particularly those specific to CLABSI prevention in the included studies. Lastly, since the data were not from a systematic surveillance system, it was not feasible to categorize and analyze the data by year, nor to demonstrate the dynamic trends in CLABSI rates. We believe the ongoing development of the Chinese Medical Institution Infection Surveillance System (CMIISS) will address these issues.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
MC: Data curation, Writing – original draft. XJ: Data curation, Writing – review & editing. JC: Data curation, Writing – review & editing. JW: Supervision, Writing – review & editing. YL: Conceptualization, Methodology, Writing – review & editing. QX: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the National Natural Science Foundation of China (No. 21976046) and 2023 Natural Science Foundation of Sichuan Province (No. 2023NSFSC0534).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1480428/full#supplementary-material
References
1. Javis, WR Bennett and Brachman hospital infections. Shanghai: Shanghai Science and Technology Press, (2018). 135–136.
2. National Health Commission of China. National Report on medical service and quality safety 2019. Beijing: Science and Technology Literature Press (2020). 334 p.
3. National Health Commission of China. National Report on medical service and quality safety 2018. Beijing: Science and Technology Literature Press (2019). 391 p.
4. Bell, T, and O'Grady, NP. Prevention of central line-associated bloodstream infections. Infect Dis Clin N Am. (2017) 31:551–9. doi: 10.1016/j.idc.2017.05.007
5. Central line-associated bloodstream infections: resources for patients and healthcare providers. Available online at: https://www.cdc.gov/hai/bsi/clabsi-resources.html (Accessed April 8, 2025).
6. General Office of Ministry of Health of China. Ministry of Health general office notice on printing and distributing the technical guidelines for prevention and control of surgical site infection (trial) and two other technical files. Available online at: https://www.gov.cn/govweb/gzdt/2010-12/14/content_1765450.htm (Accessed April 8, 2025).
7. General Office of the National Health Commission of China. (2021) Guideline for prevention and control of vessel catheter-associated infection. Available online at: http://www.nhc.gov.cn/yzygj/s7659/202103/dad04cf7992e472d9de1fe6847797e49.shtml (Accessed April 8, 2025).
8. Hei, MY, Zhang, XC, Gao, XY, Zhao, LL, Wu, ZX, Tian, L, et al. Catheter-related infection and pathogens of umbilical venous catheterization in a neonatal intensive care unit in China. Am J Perinatol. (2012) 29:107–14. doi: 10.1055/s-0031-1295650
9. Peng, S, and Lu, Y. Clinical epidemiology of central venous catheter-related bloodstream infections in an intensive care unit in China. J Crit Care. (2013) 28:277–83. doi: 10.1016/j.jcrc.2012.09.007
10. Tao, L, Hu, B, Rosenthal, VD, Gao, X, and He, L. Device-associated infection rates in 398 intensive care units in Shanghai, China: international nosocomial infection control consortium (INICC) findings. Int J Infect Dis. (2011) 15:e774–80. doi: 10.1016/j.ijid.2011.06.009
11. Hu, B, Tao, L, Rosenthal, VD, Liu, K, Yun, Y, Suo, Y, et al. Device-associated infection rates, device use, length of stay, and mortality in intensive care units of 4 Chinese hospitals: international nosocomial control consortium findings. Am J Infect Control. (2013) 41:301–6. doi: 10.1016/j.ajic.2012.03.037
12. Wang, L, Zhou, KH, Chen, W, Yu, Y, and Feng, SF. Epidemiology and risk factors for nosocomial infection in the respiratory intensive care unit of a teaching hospital in China: a prospective surveillance during 2013 and 2015. BMC Infect Dis. (2019) 19:145. doi: 10.1186/s12879-019-3772-2
13. Ren, JH, Yin, H, Wu, AH, Hu, BJ, Zhang, XY, Hou, TY, et al. A multicenter epidemiological study of device-related infections in neonatal intensive care units. Chin J Infect Control. (2015) 8:530–4. doi: 10.3969/j.issn.1671-9638.2015.08.006
14. Wang, H, Zhang, D, Zhang, Z, Zhao, Y, Ma, G, Yang, B, et al. Targeted monitoring on healthcare-associated infection in the general intensive care unit of a tertiary first-class hospital in Northwest China for 10 consecutive years. China J Infect Control. (2023) 22:802–8. doi: 10.12138/j.issn.1671-9638.20234134
15. Wang, Y, Guan, Z, Sheng, B, and Yan, P. Continuous monitoring of hospital infection targets and risk factors in the new comprehensive ICU of a teaching hospital for three consecutive years. Chin J Infect Control. (2021) 20:735–41. doi: 10.12138/j.issn.1671-9638.20217575
16. Liu, C, Yuan, Y, Weng, X, Tan, J, and Wang, J. Analysis of the status of device-related infections in the comprehensive ICU of a district in Shanghai from 2015 to 2017. Chinese Journal of Nosocomial Infection. (2018) 28:2778–82. doi: 10.11816/cn.ni.2018-182210
17. Jia, J, Wu, F, Yao, X, Li, L, Zhao, X, Zhao, Y, et al. Analysis of trends in device-related nosocomial infections in respiratory intensive care unit. Chin J Nosocomial Infect. (2017) 27:1747–50. doi: 10.11816/cn.ni.2017-170449
18. Zhang, L, Zhou, F, Mao, Y, and Song, H. Targeted monitoring analysis in comprehensive ICUs of 23 hospitals. Chin J Nosoc Infection. (2017) 27:1875–8. doi: 10.11816/cn.ni.2017-170464
19. Zha, Q, and Zhang, Y. Analysis and countermeasures of catheter-related infections in different intensive care units. Chin J Nurs Manag. (2013) 13:82–4. doi: 10.3969/j.issn.1672-1756.2013.010.029
20. Mao, Y, Han, F, Zhou, H, Zheng, W, and Zhai, R. Targeted monitoring analysis of catheter-related infections in ICU. Chin J Nosoc Infect. (2012) 22:2506–8.
21. Li, J, Wu, L, Yin, W, Zong, Z, Zhu, S, Zhang, H, et al. Targeted monitoring of nosocomial infections in respiratory intensive care unit of a teaching hospital. Chin J Nosoc Infect Control. (2015) 14:708–710+712. doi: 10.3969/j.issn.1671-9638.2015.10.016
22. Fan, WJ, Yang, LH, Ou, WQ, Xu, H, Chen, J, Lou, D, et al. Targeted surveillance of nosocomial infections in an ICU of a teaching hospital in 2018. Liaoning Med J. (2019) 33:2–5.
23. Deng, A, Xu, SL, Zhu, DZ, and Zhao, N. Targeted surveillance analysis of nosocomial infections in a newly established general ICU. Chin J Nosocomiol. (2017) 27:215–7. doi: 10.11816/cn.ni.2017-162157
24. Wang, JC, Mo, QJ, and Qi, KX. Targeted surveillance and analysis of catheter associated nosocomial infections in the ICU. Chin J Infect Control. (2016) 15:902–6. doi: 10.3969/j.issn.1671-9638.2016.12.002
25. Guan, J, Zhang, Q, and Lin, ZF. Analysis of catheter-associated nosocomial infections and related factors in a general ICU. Chin J Nosocomiol. (2010) 20:1692–4.
26. Li, RJ, Wu, YL, Huang, K, Hu, XQ, Zhang, JJ, Yang, LQ, et al. A prospective surveillance study of healthcare-associated infections in an intensive care unit from a tertiary care teaching hospital from 2012-2019. Medicine (Baltimore). (2023) 102:e34469. doi: 10.1097/MD.0000000000034469
27. Xu, YP, Shang, ZR, Dorazio, RM, and Shi, LP. Risk factors for peripherally inserted central catheterization-associated bloodstream infection in neonates. Zhongguo Dang Dai Er Ke Za Zhi. (2022) 24:141–6. doi: 10.7499/j.issn.1008-8830.2109147
28. Zeng, C, Wu, A, Li, L, and Jia, H. Multi-center prospective study on central line-associated bloodstream infections in 79 ICUs of China. BMC Infect Dis. (2021) 21:1208. doi: 10.1186/s12879-021-06871-5
29. Zheng, X, He, D, Yang, Z, Chen, L, Jiang, M, Qi, Y, et al. Dwell time and bloodstream infection incidence of umbilical venous catheterization in China. Pediatr Investig. (2023) 7:239–46. doi: 10.1002/ped4.12403
30. Wang, Y, Li, Q, Shu, Q, Liu, M, Li, N, Sui, W, et al. Clinical epidemiology and a novel predicting nomogram of central line associated bloodstream infection in burn patients. Epidemiol Infect. (2023) 151:e90. doi: 10.1017/S0950268823000766
31. Dudeck, MA, Horan, TC, Peterson, KD, Allen-Bridson, K, Morrell, G, Anttila, A, et al. National Healthcare Safety Network (NHSN) report, data summary for 2009, device-associated module. Am J Infect Control. (2011) 39:349–67. doi: 10.1016/j.ajic.2011.04.011
32. Dudeck, MA, Horan, TC, Peterson, KD, Allen-Bridson, K, Morrell, G, Pollock, DA, et al. National Healthcare Safety Network (NHSN) Report, data summary for 2010, device-associated module. Am J Infect Control. (2011) 39:798–816. doi: 10.1016/j.ajic.2011.10.001
33. Dudeck, MA, Horan, TC, Peterson, KD, Allen-Bridson, K, Morrell, G, Anttila, A, et al. National Healthcare Safety Network report, data summary for 2011, device-associated module. Am J Infect Control. (2013) 41:286–300. doi: 10.1016/j.ajic.2013.01.002
34. Dudeck, MA, Weiner, LM, Allen-Bridson, K, Malpiedi, PJ, Peterson, KD, Pollock, DA, et al. National Healthcare Safety Network (NHSN) report, data summary for 2012, Device-associated module. Am J Infect Control. (2013) 41:1148–66. doi: 10.1016/j.ajic.2013.09.018
35. Dudeck, MA, Edwards, JR, and Allen-Bridson, K. National Healthcare Safety Network (NHSN) report, data summary for 2013, device-associated module. Am J Infect Control. (2015) 43:206–21. doi: 10.1016/j.ajic.2014.11.014
36. Rosenthal, VD, and Al-Abdely, HM. International nosocomial infection control Consortium (INICC) report, data summary of 43 countries for 2007-2012. Device-associated module. Am J Infect Control. (2014) 42:942–56. doi: 10.1016/j.ajic.2014.05.029
37. Rosenthal, VD, Al-Abdely, HM, El-Kholy, AA, AlKhawaja, SAA, Leblebicioglu, H, Mehta, Y, et al. International Nosocomial Infection Control Consortium report, data summary of 50 countries for 2010-2015: Device-associated module. Am J Infect Control. (2016) 44:1495–1504. doi: 10.1016/j.ajic.2016.08.007
38. Rosenthal, VD, and Al-Abdely, HM. International nosocomial infection control consortium (INICC) report, data summary of 45 countries for 2012-2017: device-associated module. Am J Infect Control. (2020) 48:423–32. doi: 10.1016/j.ajic.2019.08.023
Keywords: central line-associated bloodstream infection, ICU, China, meta-analysis, CLABSI
Citation: Cai M, Jiang X, Chen J, Wu J, Lyu Y and Xiang Q (2025) Central line-associated bloodstream infection rates in intensive care units of China’s hospitals: a meta-analysis. Front. Public Health. 13:1480428. doi: 10.3389/fpubh.2025.1480428
Edited by:
Fu Qiao, Sichuan University, ChinaReviewed by:
Tuuli Metsvaht, University of Tartu, EstoniaKaiwen Ni, Zhejiang University, China
Letao Chen, Central South University, China
Copyright © 2025 Cai, Jiang, Chen, Wu, Lyu and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Lyu, MjkzODE2MzZAcXEuY29t; Qian Xiang, M2FsbEAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
 Minghong Cai†
Minghong Cai† Jing Chen
Jing Chen Yu Lyu
Yu Lyu Qian Xiang
Qian Xiang