- 1Department of Nursing, West China Second Hospital, Sichuan University/Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), Ministry of Education, Chengdu, Sichuan, China
- 2Department of Community Medicine, Faculty of Medicine, University of Ruhuna, Matara, Sri Lanka
Background: Disability is a global public health issue, affecting one in seven people worldwide. In China, there are about 5 million children under 14 years of age with cerebral palsy and about 40,000 new individuals occur every year. Previous studies have revealed that the caregivers of children with cerebral palsy were more likely to perceive a greater burden compared with caregivers of typically developing children. However, there is a lack of information available on the care burden experienced by parents of children with cerebral palsy in China.
Objectives: This study was conducted to determine the level of care burden and its related factors in the parents of children with cerebral palsy.
Methods: This descriptive cross-sectional study was conducted with parents of 165 children with cerebral palsy who were enrolled in children rehabilitation departments of three tertiary hospitals between September 2021 and December 2022. Besides demographic information, the Caregiver Burden Inventory, the Patient Health Questionaire-9, and the Fatigue Severity Scale were used to collect data. Data were analyzed by descriptive and inferential statistics (correlation and multiple linear regression analysis).
Results: The mean (±SD) Caregiver Burden Inventory score of the parents was 42.18 ± 18.79. The score of Fatigue Severity Scale and Patient Health Questionaire-9 demonstrated positive moderate to strong correlations with caregiver burden (r = 0.461, p < 0.001; r = 0.630, p < 0.001, respectively). The results of the multiple linear regression analysis showed that a low level of education, long caring time combined with visual impairment, higher depression, and fatigue had an influence on caregiver burden, and 46.4% of the variance in caregiver burden was explained by these factors.
Discussion: The key predictors of caregiver burden include the level of education, caring time, children with visual impairment, and the degree of depression and fatigue. Efforts should be made to relieve the burden on parents of children with cerebral palsy.
1 Introduction
Disability is a global public health issue, affecting one in seven people worldwide (1). The World Health Organization reported that about 15% of the world’s population was living with disability in the year 2020, including about 93 million children and 720 million adults with significant difficulties in functioning (2). Developmental disorders in children encompass a range of conditions that affect a child’s physical, cognitive, or emotional growth and development (3). These disorders can impact various areas, including learning, communication, social skills, and daily functioning (3). Some common developmental disorders in children include Autism Spectrum Disorder (ASD), Down Syndrome, Attention-Deficit/Hyperactivity Disorder (ADHD), Dyslexia, Cerebral Palsy (CP), and so on (4–6). The World Health Organization (WHO) defines “Quality of Life” (QoL) as the individual’s perception of their position in life in the context of the culture and value systems in which they live and about their goals, expectations, standards, and concerns (7). Previous studies showed that caregivers of children with ASD and ADHD have a higher score of stigmas, burden, depression, anxiety, and a poorer QoL than normal (8, 9). Surveys revealed that the primary themes of stressful experiences among parents of young children with Down syndrome included emotional burdens, caregiving responsibilities, struggles against stigma and discrimination, concerns about the future, and challenges related to health, education, and financial issues (10–13). Approximately 95% of mothers with dyslexic children experience anxiety about their child’s future and academic performance, in addition to distress related to dyslexia (14–16). In China, among the mothers of 252 children with ASD, 26.02, 17.34, and 3.57% had mild, moderate, and severe depression, respectively (17). Caregivers of children with ASD scored significantly lower on adaptability than that of the norm (18), 46% of parents scored above the cut-off for stress (19), the total score of the Zarit caregiver burden Scale for caregivers of children with ASD was reported (52.62 ± 14.65) in Henan Province, China (20). A qualitative study conducted in China revealed that parents of children with ADHD use individual, family, and school coping strategies to cope with their stress (21). A meta-synthesis included eight qualitative types of research indicated that feeding pressures, educational concerns, language difficulties, and discrimination and stigmatization led to psychological, economic, and family stress in caregivers of children with Down syndrome (22). Four key categories of potential factors contributing to parental stress were identified: cultural factors, parents’ psychopathological symptoms, problem behaviors in children with developmental conditions, and caregiver burden (23–25).
Cerebral Palsy, with a rate of about 2.5 per 1,000 live births (26, 27). In China, there are about 5 million children under 14 years of age with cerebral palsy and about 40,000 new individuals occur every year (27, 28). Cerebral Palsy is a chronic illness in childhood, defined as a group of functional limitations that stem from challenges in the development of the central nervous systems, the continuous rehabilitation and lifelong support care are essential components of the development plan for a child with cerebral palsy (29).
Parenting a child with CP can be a unique journey filled with both challenges and rewards (30, 31). The key factors that contribute to positive experiences, include support networks, resilience, and personal growth, alongside those that lead to negative experiences, such as emotional and psychological stress, financial strain, isolation, and social withdrawal, navigating healthcare systems, concerns about the future, guilt and balancing family needs, fatigue and burnout, limited personal time, impact on family dynamics (32–35). The high medical expenses and education costs may turn into an economic burden for parents of children with cerebral palsy (28). The continued provision of excessive care leaves caregiver experiencing fatigue and depression, which can negatively impact their quality of life (28, 36, 37). Families may find it challenging to participate in social activities or events due to their child’s needs, leading to feelings of isolation or exclusion (38). While there are significant challenges, many parents also discover immense joy, growth, and fulfillment in their journey (39). The key often lies in seeking support, celebrating progress, and finding ways to cope with the difficulties that arise (40). Many parents report a profound emotional connection with their child with CP. The challenges they face together can strengthen their bond and create a deeper understanding of one another (41). Additionally, family members often become more compassionate and supportive, learning valuable life lessons about diversity and inclusion (42). Furthermore, this experience can lead to personal growth and a new perspective on life, prompting parents to develop patience, empathy, and problem-solving skills (43).
Caregiver burden refers to a multidimensional response to physical, psychological, emotional, social, and financial stressors associated with caring experience’ (44). Surveys conducted in Brazil (45), Portugal (46), and Turkey (36) have revealed that the caregivers of children with cerebral palsy were more likely to perceive a greater burden compared with caregivers of typically developing children. Within the context of the stress process model, numerous factors may affect the degree of burden for parents of children with cerebral palsy. Stigma is an important source of psychological stress for families of children with disability (47). Regarding caregiver characteristics, several studies show that having a lower income and education, living in a rural area, greater age, and poor health status are related to a higher burden in caregivers (36, 44, 48, 49). In terms of child characteristics, age, number of functional deficits, type of cerebral palsy, degree of disability, Gross Motor Function Classification System (GMFCS) level, and disease severity were associated with higher burden in caregivers (44, 48–51). The caregiver’s social support, self-efficacy, anxiety, depression, and fatigue were found to have significant correlations with caregiver burden (36, 45, 46, 48, 50, 52). A recent study reported the COVID-19 pandemic worsened the psychological status and the care burden of caregivers of children with cerebral palsy (53).
In pediatric psychology, examining the role of families can create an opportunity for understanding and treatment of chronic illness is well-documented (46). Bella et al. study has shown the level of burden and psychological maladjustment of parents has been linked to behavioral and emotional disturbance of children (45). Furthermore, screening parents for excessive burden and assisting them in finding appropriate coping mechanisms significantly contributed to the successful management of stressors and better social function in their children (42, 50, 54). In China, however, there is a lack of information available on the care burden experienced by parents of children with cerebral palsy. Therefore, the main aim of the current study was to determine the levels, correlates, and predictive factors of care burden among parents of children with cerebral palsy in China.
1.1 Research questions
Q1. What is the level of caregiver burden among parents of children with cerebral palsy in southwest China?
Q2. What demographic and socio-economic factors are associated with caregiver burden among these parents? a. How do parental age, education level, and employment status correlate with caregiver burden? b. Does the severity of the child’s condition correlate with the level of caregiver burden?
Q3. What depression and fatigue are associated with caregiver burden?
1.2 Hypotheses
H1: The level of caregiver burden among parents of children with cerebral palsy in southwest China is significantly higher than the general population, indicating a substantial impact on their daily lives.
H2: There is a significant positive correlation between the severity of the child’s cerebral palsy and the level of caregiver burden, such that parents of children with more severe disabilities report higher levels of burden.
H3: Lower levels of parental education and employment status are associated with higher caregiver burden, suggesting that socioeconomic factors play a crucial role in the experience of caregiving.
H4: Higher levels of depression and fatigue among parents are significantly associated with higher levels of caregiver burden.
2 Methods
2.1 Design
This cross-sectional study was performed in children’s rehabilitation departments of three tertiary hospitals in XX between September 2021 and December 2022. A local hospital’s Institutional Review Board approved this study.
2.2 Participants
This study was conducted among parents of children with cerebral palsy who were enrolled in children’s rehabilitation departments of three tertiary hospitals in Chengdu, Sichuan Province between September 2021 and December 2022. It was aimed that all parents who have a child with cerebral palsy would agree to participate in this study, without using sample selection. A total of 173 parents agreed to participate in the study, 8 parents were excluded because they provided insufficient/unreliable data, and 165 parents were finally included in the data analysis. The inclusion criteria of parents were as follows: (i) Caring for child aged 1–14 with cerebral palsy, (ii) parents who are taking on the responsibilities for the daily provision of care, (iii) living with the child, could read and write in Chinese. The inclusion criteria of children were as follows: (i) the children with cerebral palsy were diagnosed according to the diagnostic criteria of China Cerebral Palsy Rehabilitation Guidelines (2015), (ii) the children were aged 0–14 years old.
All participants self-completed the questionnaire in the presence of the principal investigator. The overall time taken to collect data by completing the questionnaires was on average 30–45 min.
2.3 Measures
Besides demographic information, the Caregiver Burden Inventory (CBI), the Patient Health Questionaire-9 (PHQ-9), and the Fatigue Severity Scale (FSS) were used to collect data. The selection of the CBI, PHQ-9, and FSS is pivotal for gaining insights into the experiences of caregivers, particularly parents of children with cerebral palsy. Each of these tools has been validated and widely used in research, providing crucial data to understand the intricacies of caregiver experiences. By employing these validated instruments, researchers and healthcare providers can identify specific needs and challenges, ultimately leading to improved support systems that enhance the well-being of both caregivers and their children. This comprehensive approach fosters a deeper understanding of the factors influencing caregiver burden, paving the way for effective interventions.
2.3.1 Demographic characteristics of participants
The demographic characteristics questionnaire was composed of two parts. The first part included the basic information of parents, including the relationship to the child (father and mother), age, education level (primary school and below, junior high school, senior high school, university, master and above), occupation, marital status, average caring time (hours/day) and family systems (composed of nuclear family, stem family, joint family, single parent family). The definition of a nuclear family is a family unit that includes two married parents of opposite genders and their biological or adopted children living in the same residence (55). The stem family is composed of parents, unmarried children, and married sons and their wives (56). The joint family consists of parents and their unmarried children, two or more married sons, and their wives (56). The single-parent family consists of at least one dependent child and the mother or father, the other parent being dead or permanently absent (57).
The second part included the basic information about children with cerebral palsy, including age, gender, types of cerebral palsy, Gross Motor Function Classification System (GMFCS), visual impairment, and epilepsy. The types of cerebral palsy are comprised of Spastic hemiplegia, Spastic diplegia, Spastic tetraplegia, Ataxia, Dyskinetic, and Mixed types, according to China Cerebral Palsy Rehabilitation Guidelines (2015) (27). The gross motor skills (e.g., sitting and walking) of children and young people with cerebral palsy can be categorized into five different levels using a tool called the Gross Motor Function Classification System (58, 59).
2.3.2 Caregiver Burden Inventory (CBI)
The Caregiver Burden Inventory (CBI) is a self-administered, multidimensional scale for assessing caregiver burden among caregivers of persons with dementia (60), children with cancer (61), psychiatric patients (62), and rheumatoid arthritis patients (63). This measure consists of 24 items divided into five domains: Time-dependence (1–5 items), developmental burden (6–10 items), physical burden (11–14 items), social burden (15–18 items), and emotional burden (19–24 items) (64). Each item is rated on a 5-point (0–4) Likert-type scale, with the total score ranging from 0 to 96 (65). The internal consistency of the Chinese-CBI was reported as 0.95 in China (64). In the present study, the Cronbach’s alpha of the CBI was 0.944, suggesting the internal consistency of the CBI was adequate. The CBI has been validated in various populations, showing strong correlations with other measures of psychological distress and quality of life (66). This established correlation makes it a reliable instrument for assessing caregiver experiences, particularly in parents of children with CP.
2.3.3 Patient Health Questionaire-9 (PHQ-9)
The Patient Health Questionaire-9 (PHQ-9) is composed of nine items. It can be used to assess depressive symptoms of the general population over the last 2 weeks (67). The total score ranges from 0 to 27; a score of 10 or greater is defined as depression. In the Chinese validation study, the PHQ-9 was reported to have acceptable internal consistency (α = 0.90) (68). In the current study, the Cronbach’s alpha of the EPDS was 0.899, suggesting the internal consistency of the PHQ-9 was adequate. Research has shown that the PHQ-9 is strongly correlated with other measures of mental health and well-being (69). Its use in caregiving contexts has revealed significant associations between caregiver mental health and the burden they experience.
2.3.4 Fatigue Severity Scale (FSS)
The Fatigue Severity Scale (FSS) is a self-administered questionnaire measuring fatigue (70). It includes nine statements rated on a 7-point scale. The total score is calculated as the mean of the responses to the nine statements (71). A score of 4 or higher indicates a moderate to high level of fatigue (72). In the Chinese validation study, the FSS was found to have a very good internal reliability (α = 0.93) (73). In this study, the Cronbach’s alpha of the FSS was 0.929. Previous studies have demonstrated a strong correlation between the FSS and other measures of health-related quality of life and psychological well-being (74, 75). It has proven particularly valuable in evaluating fatigue among caregivers, providing insights into how fatigue influences their overall burden and caregiving experiences.
2.4 Statistical analysis
Data were analyzed by SPSS 21.0 software using descriptive and inferential statistics. The sample size of this study was less than 200, so the normality test was judged using Kurtosis and Skewness, with Kurtosis ≤ 3 and Skewness ≤ 10 indicating that the data basically conformed to a normal distribution. Mean and standard deviation (SD) were reported for continuous variables that conformed to a normal distribution, and Median and interquartile spacing were reported for continuous variables that conformed to a non-normal distribution. Number and percentage were reported for categorical variables.
A stepwise model in multiple linear regression is a systematic method for selecting a subset of predictor variables to include in a regression model. This approach is particularly useful when dealing with numerous potential predictors, allowing researchers to identify the most significant ones while avoiding overfilling. The stepwise regression process can be conducted in several ways, including forward selection, backward elimination, and bidirectional elimination. (i) Start with no predictors in the model. (ii) Add the predictor that has the lowest p-value (indicating the strongest relationship with the dependent variable) to the model. (iii) Continue adding predictors one by one, each time selecting the one with the lowest p-value until no remaining predictors meet the entry criterion. Criteria for entry: A common criterion is a significance level (alpha) such as 0.05. If the p-value for a predictor is less than 0.05, it is added to the model.
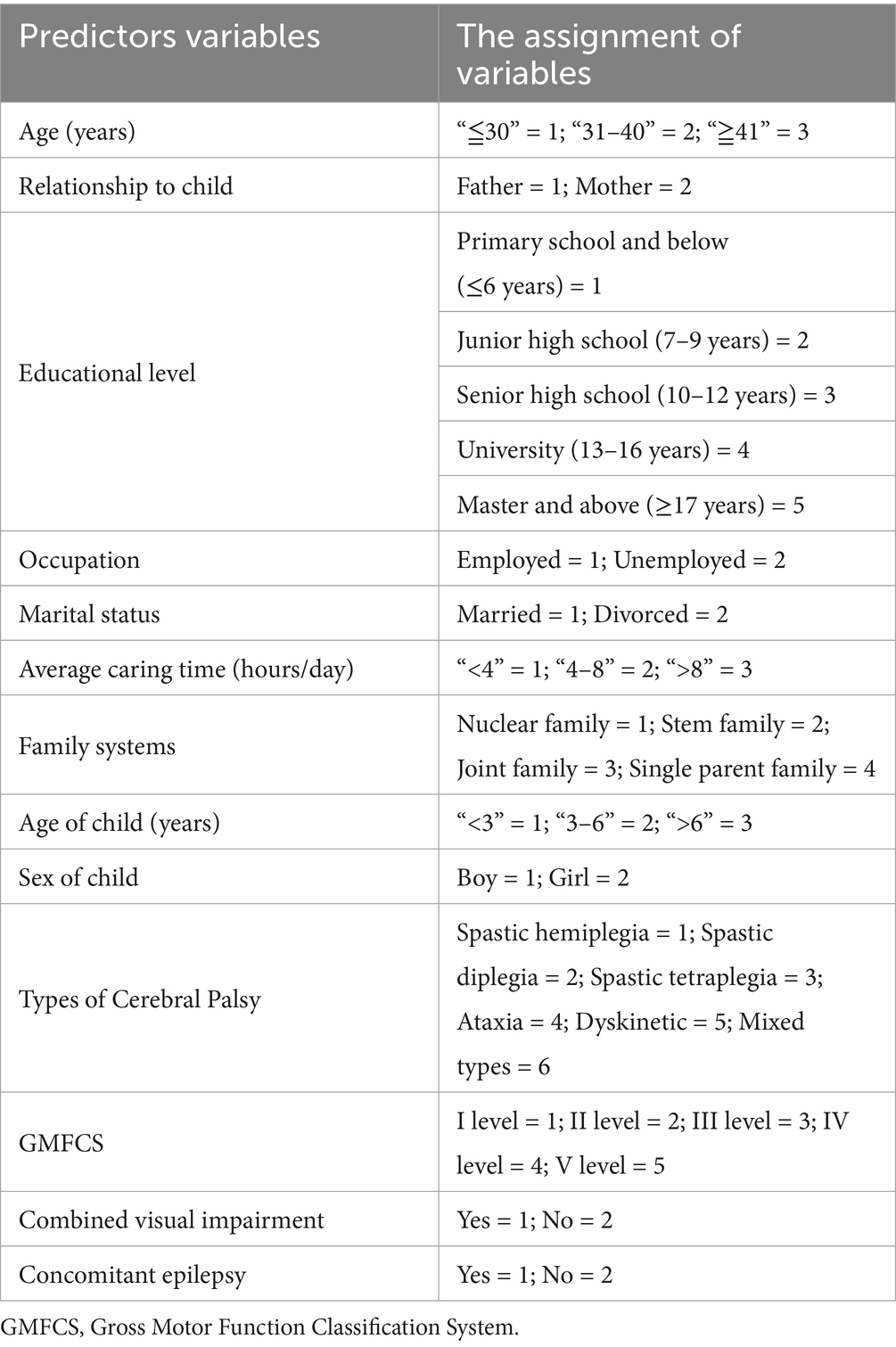
In the current study, predictor variables include the relationship to the child, age, education level, occupation, marital status, average caring time and family systems, the score of the PHQ-9 and FSS, the response variable is the score of CBI, and the stepwise regression process was conducted by forward selection. The multiple linear regression was undertaken to evaluate the statistical significance of the effect of demographic factors, depression, and fatigue on caregiver burden by forward selection of the stepwise method. The statistically significant value was p-value <0.05. The assignment of predictor variables is in Table 1.
3 Results
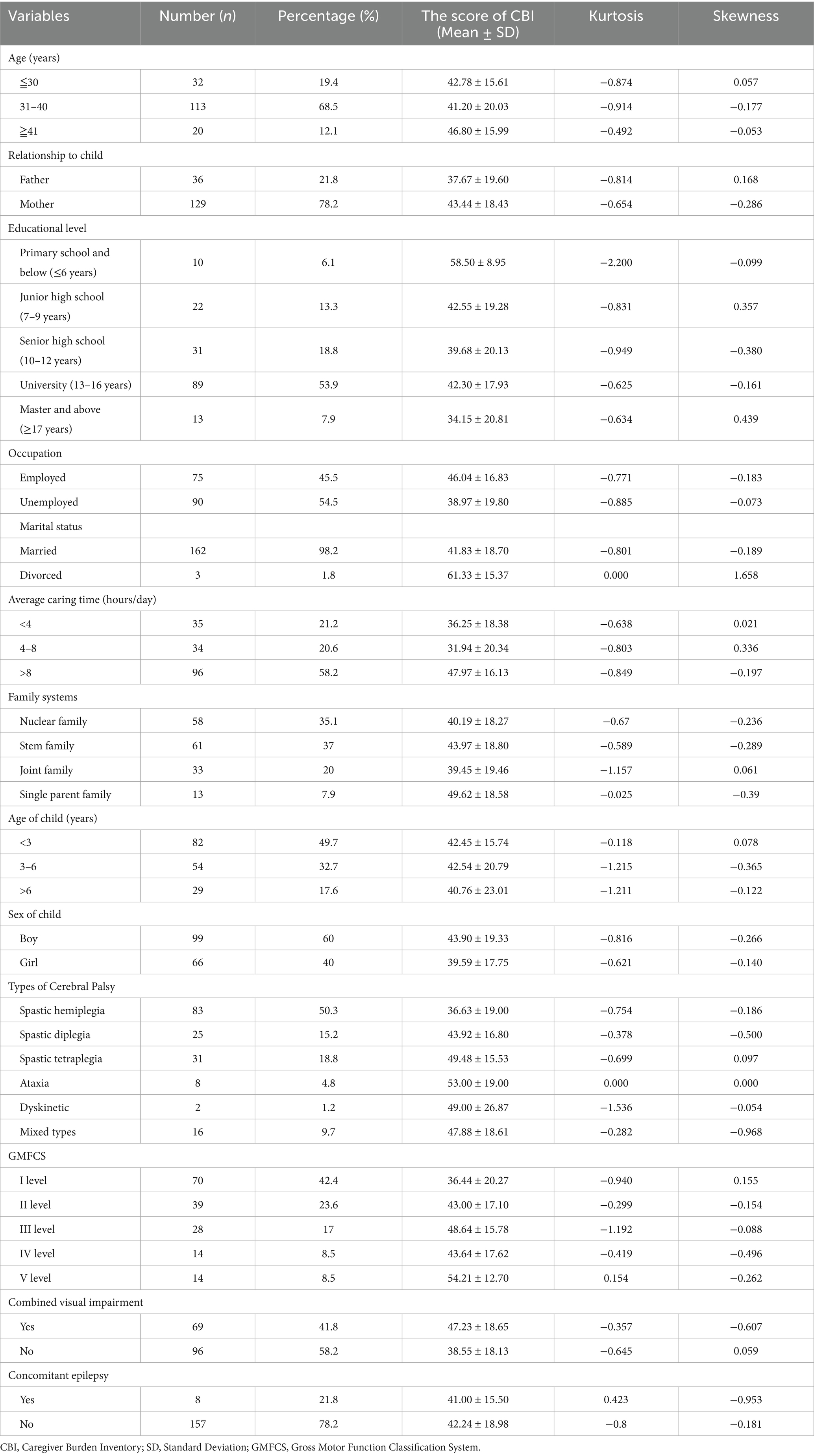
A total of 165 parents were included in this study. Regarding the age of participants, 32 (19.4%) were ≦30 years, 113 (68.5%) were 31–40 years, and 20 (12.1%) were ≧41 years. Most of the participants were child’s mothers (n = 129, 78.2%). Other demographic characteristics of participants are displayed in Table 2.
The result indicated that the mean and SD of the CBI score was 42.18 ± 18.79. Among the five domains, time-dependent burden scored the highest (14.64 ± 4.91), followed by developmental burden (12.38 ± 5.78), while emotional burden scored the lowest (2.79 ± 3.36).
The scores of total CBI and domains were positively correlated with PHQ-9 and FSS (r ranging from 0.420 to 0.630 and 0.250 to 0.447, respectively, all p < 0.001). The mean and standard deviations of the variables under the study and their Spearman correlations are given in Table 3. The total scores of the PHQ-9, which measures levels of depression, exhibited a positive correlation with the scores from the Caregiver Burden Inventory. This indicates that higher levels of depressive symptoms in individuals, as assessed by the PHQ-9, are associated with higher caregiver burden. In other words, caregivers who reported more significant depressive symptoms also tended to experience greater feelings of burden related to their caregiving responsibilities.
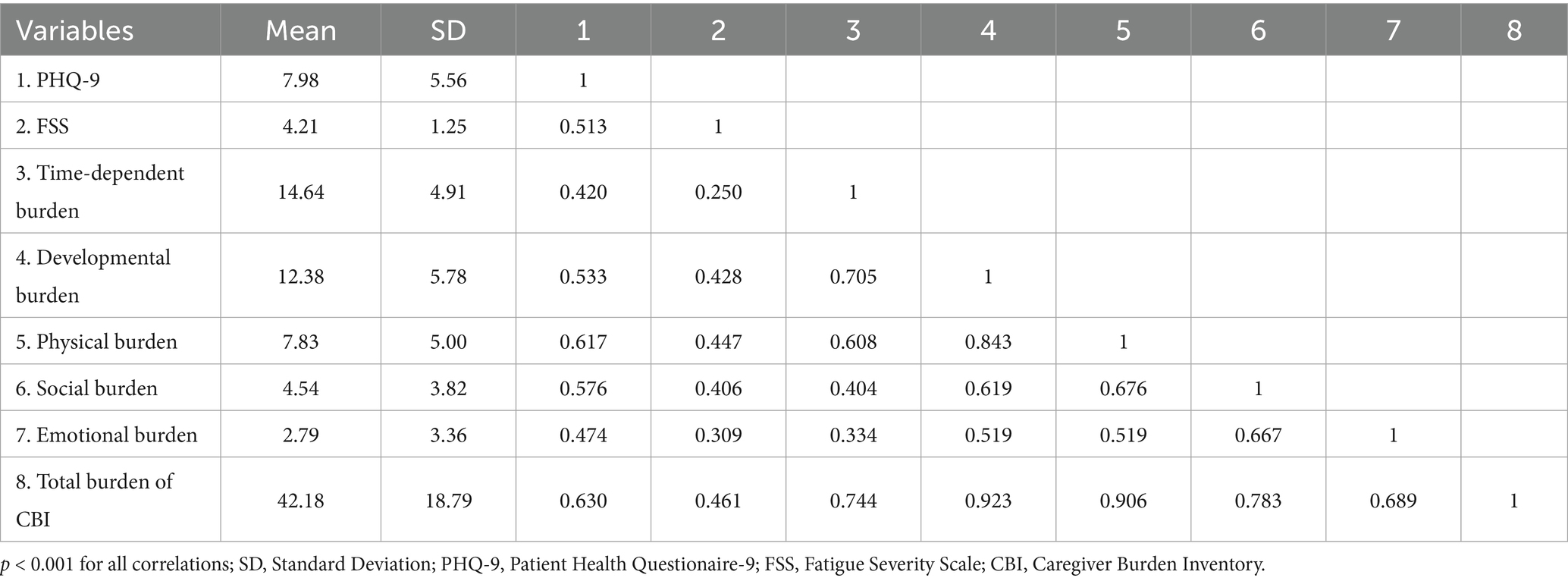
Table 3. The mean and standard deviations of the variables under the study and their correlations (n = 165).
The total scores on the FSS, which assesses the severity of fatigue and its impact on daily functioning, exhibited a positive correlation with the scores from the CBI. This finding indicates that higher levels of fatigue reported by caregivers are associated with increased feelings of burden related to their caregiving roles. The positive correlation likely extends to specific domains of both the FSS and the CBI. This means that not only the overall fatigue levels but also particular aspects of fatigue (such as physical fatigue, mental fatigue, or the impact of fatigue on daily activities) may correlate with specific dimensions of caregiver burden (such as emotional, physical, or social burden). For instance, caregivers reporting significant physical fatigue may also experience heightened emotional or role-related burdens in their caregiving tasks.
The multiple linear regressions analysis revealed that having a low level of education, long caring time, having a child with combined visual impairment, and higher scores of PHQ-9 and FSS pertained to higher scores of CBI (adjusted R2 = 0.464, F = 29.357, p < 0.001). The results of the multiple linear regression analysis for the factors related to the caregiver burden of parents of children with cerebral palsy are presented in Table 4. Caregivers with a lower level of educational attainment were found to report higher levels of caregiver burden. This suggests that educational background may influence coping strategies and resources available to caregivers. The duration of caregiving is significantly linked to increased caregiver burden. Those who have been providing care for a longer period tend to experience greater levels of stress and exhaustion, likely due to the cumulative effects of long-term caregiving responsibilities. Caregivers of children who have combined visual impairment reported higher burden levels. This may reflect the unique challenges and demands associated with caring for a child with such impairments, which may require more intensive support and resources. Higher scores on PHQ-9 indicate greater depressive symptoms among caregivers, which are associated with increased feelings of burden. This suggests that as caregivers experience more depressive symptoms, their perceived burden also rises. Higher scores on the FSS were also significantly related to higher CBI scores, indicating that greater fatigue levels experienced by caregivers correlate with an increased sense of burden. This may be due to the physical and emotional exhaustion that caregiving can entail.
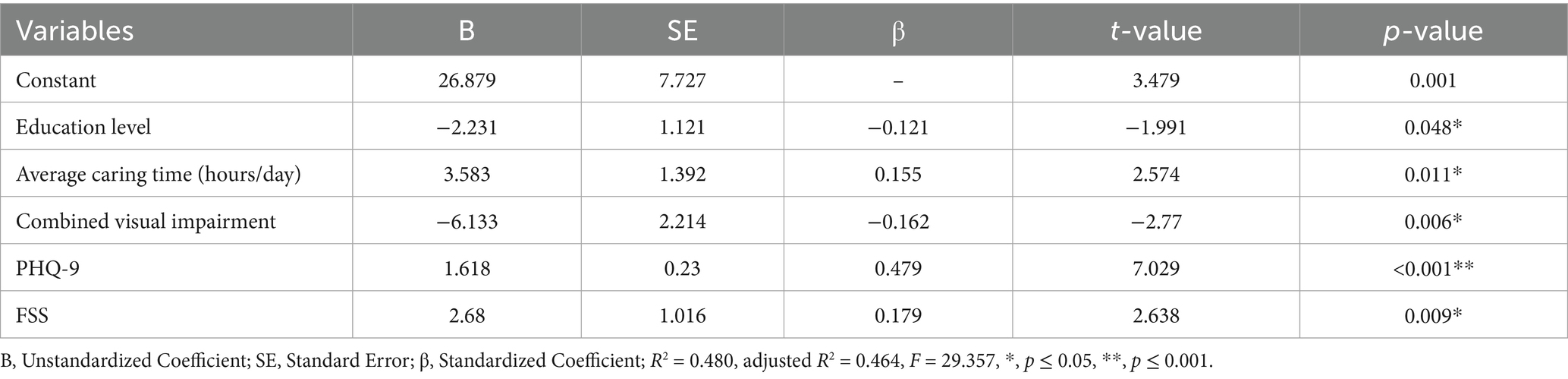
Table 4. The results of the multiple linear regressions analysis for the factors related to caregiver burden of parents of children with CP (n = 165).
4 Discussion
To the best of our knowledge, the current study presented the first quantitative research on caregiver burden related to parents of children with cerebral palsy in southwest China. This cross-sectional study was conducted to determine the level of care burden and its related factors in the parents of children with cerebral palsy. The finding of the study detected that the score of care burden in half of parents was of moderate level. In line with the studies conducted in South Africa (76), Spain (50), Turkey (36, 52), Nigeria (49), Poland (48), and Brazil (77), most of the parents of children with cerebral palsy endured moderate to severe care burden and various challenges on account of restricted access to alternative caring resources and the fear for children’s development. This high caregiver burden among parents of children with cerebral palsy calls for attention and action by healthcare institutions and disabled persons’ federations in China.
According to the result of this study, among of five domains of CBI, time-dependent burden received the highest score with a mean ± SD of 14.64 ± 4.9, followed by developmental burden scoring 12.38 ± 5.78 in comparison to other aspects. The heavy time-dependent burden can deplete the caregiver’s energy and increase negative emotions (78). The present study illustrated that parents of children with cerebral palsy tend to feel time-related pressure and restriction of their social and cultural activities due to multiple additional care tasks, which is consistent with previous studies (79, 80). The result of multiple linear regression analysis found that the level of education, caring time, visual impairment, the degree of depression, and fatigue remained statistically significant correlates of the caregiving burden.
According to a study conducted in Nigeria (77), parents of children with cerebral palsy who have higher education suffer less caring burden than those with low or no education. Barros et al. (77) pointed out that caregivers with lower educational levels are more likely to fall into poverty and undergo stress. Parents may face societal stigma regarding their child’s disability, which can be more pronounced for those who are less educated (66). This stigma can manifest as judgment or lack of understanding from others, leading to feelings of shame and isolation (37). Moreover, parents may internalize societal stigma, leading to feelings of worthlessness or failure in their parenting role (81). This can contribute to a negative self-image and increased caregiver burden (42). Addressing these issues requires targeted support, education, and community awareness to help alleviate the burdens faced by these families, fostering a more inclusive and understanding environment for parents and children with disabilities (82). By providing education and resources, communities can help reduce stigma and empower parents, ultimately improving their quality of life and the care they provide (83). Higher parental schooling, on the one hand, may enable them to search and acquire information and support resources more efficiently and on the other hand, foster self-efficacy in managing their children’s health issues and formulating effective plans to cope with their stressors (84). There is compelling evidence that education is one of the most important sources for caregivers to acquire competency, affecting the perception of stress, resilience, and psychological flexibility (85). For this reason, caregiver skill training was developed by the World Health Organization (WHO) aiming to facilitate access to parenting skills and strategies for caregivers of children with developmental delays or disabilities (86–89).
We found that the parents with longer caring time perceived a higher level of burden. This finding supports previous research that the length of caregiving is associated with caregiver burden. In terms of time cost, Park et al. (80) reported that parents of children with cerebral palsy spend about 14–15 h per day to support their children in Korea. A study conducted in Australia revealed a significant positive correlation between psychological problems and caring time (90). In the present study, the caring time on an average day was also fairly long, with 58.2% of parents spending more than 8 h per day devoted to caring for their children. On one hand, increased time allocated by the parents for their children might require one of the parents to quit work to care for the child, which adds a financial burden to the families. On the other hand, parents with longer caring time might feel more burnout and pain, which, in turn, enhances the care burden experienced as well (36).
The results of the current study demonstrated that the caregiver burden was higher in parents of children with visual impairment, which is consistent with previous research (44, 91). This might be attributed to the fact that visually impaired children need additional care for daily tasks due to their diminished independent living skills and increased likelihood of injury (44). Most of the qualitative studies conducted with caregivers of children with cerebral palsy documented that most caregivers worry about their children’s future (42). Thus, parents of visually impaired children with cerebral palsy are more likely to feel tiredness and pressure.
In keeping with the views in the literature (48, 92), it was observed that caregiving burden was significantly affected by depression and fatigue. Caregivers experiencing higher levels of depression may feel more overwhelmed by their responsibilities, which can create a cycle of increased stress and emotional strain (93). This highlights the importance of addressing the mental health needs of caregivers, as their psychological well-being is closely linked to their experience of burden (94). This has major clinical implications for medical practitioners and nurses in being able to identify parents at risk for burden. The current study suggests a significant relationship between the experience of fatigue and the perception of caregiver burden. Caregivers who report higher levels of fatigue may feel less capable or more drained in their caregiving roles, contributing to a greater sense of burden (95). This can create a vicious cycle where fatigue exacerbates feelings of burden, potentially leading to further fatigue and emotional distress (96). This highlights the necessity for interventions and support systems aimed at addressing fatigue among caregivers, which could, in turn, alleviate their burden and improve their overall quality of life (97). Parents with a greater number of depressive and fatigue symptoms may require more individualized support and interventions, such as problem-solving therapy and group educational intervention (98, 99).
The study contributes to providing existing evidence on caregiver burden in a Chinese context. However, there are a few limitations of this study. Firstly, the nature of cross-sectional study prevents the inference of causal relationships. Secondly, the overall multiple regression models explained only up to 46.4% of the variance in caregiver burden, which was relatively low, indicating the need for more extensive research on the correlates of caregiver burden. Third, limitation of quantitative approaches, particularly regarding the inability to capture the nuanced experiences and specific emotions that parents may face. While our quantitative design allowed for the measurement of broader trends and relationships, it did not provide the depth of understanding that qualitative methods offer.
5 Conclusion
In conclusion, this study showed that most parents of children with cerebral palsy experience moderate to severe caregiver burden, the time-dependent burden being the heaviest compared with other types of burden. A moderate burden may refer to caregivers who feel overwhelmed but can still manage their responsibilities, while a severe burden indicates that they are experiencing significant distress and may struggle to cope with their caregiving duties. The key predictors of caregiver burden include the level of education, caring time, children with visual impairment, and the degree of depression and fatigue. These findings underscore the multifaceted nature of caregiver stress and the importance of addressing these factors to support caregivers effectively. The current findings may prove useful for providing more effective family-oriented support programs for parents of children with cerebral palsy. Taking into account the factors linked to caregiver burden, further studies should examine the burden of care in different societies with diverse cultures.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The Ethics Committee approval of the West China Second University Hospital, Sichuan University (Approval ID: 2021/218). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
XZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CW: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was financially supported by Health Humanities Research Center, Key Research Base of Philosophy and Social Sciences, Zigong City (Project ID: JKRWY23-19) and (Project ID: JKRWY24-17), Centre for Innovative Research in Exercise and Health, Zigong City (Project ID: YDJKY24-22) and (Project ID: YDJKY24-23).
Acknowledgments
We would like to thank all the postpartum women for their participant in the current study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CP, Cerebral Palsy; GMFCS, Gross Motor Function Classification System; CBI, Caregiver Burden Inventory; PHQ-9, Patient Health Questionaire-9; FSS, Fatigue Severity Scale.
References
1. Daniel, JA, Okefienam, EC, Ugorji, TN, Agbasi, PU, Onyido, DC, Odoh, IO, et al. Challenges faced by Nigerian parents with disabled children in caring for them. Open J Soc Sci. (2021) 9:201–12. doi: 10.4236/jss.2021.910015
2. Olusanya, BO, Wright, SM, Nair, MKC, Boo, N-Y, Halpern, R, Kuper, H, et al. Global burden of childhood epilepsy, intellectual disability, and sensory impairments. Pediatrics. (2020) 146:e20192623. doi: 10.1542/peds.2019-2623
3. Jeste, SS, and Geschwind, DH. Developmental disorders. Curr Opin Neurol. (2015) 28:89–90. doi: 10.1097/WCO.0000000000000188
4. Huang, M, Huang, W, Chen, Y, Zhou, C, Cao, J, Peng, K, et al. Quality of instruments measuring activity and participation in children with developmental coordination disorder: a systematic review. Ann Phys Rehabil Med. (2025) 68:101889. doi: 10.1016/j.rehab.2024.101889
5. Meachon, EJ, Schaider, JP, and Alpers, GW. Motor skills in children with ADHD: overlap with developmental coordination disorder. BMC Psychol. (2025) 13:1–7. doi: 10.1186/s40359-024-02282-8
6. Hiebert, L, Weatherford, S, Curran, M, McGregor, K, and Van Horne, AO. Learning science concepts alongside language goals: a telehealth replication of a randomised controlled trial examining whether children with developmental language disorder can learn vocabulary or grammar in combination with curricular science content. Int J Speech Lang Pathol. (2025):1–13. doi: 10.1080/17549507.2024.2445155
7. Costa, DSJ, Mercieca-Bebber, R, Rutherford, C, Tait, M-A, and King, MT. How is quality of life defined and assessed in published research? Qual Life Res. (2021) 30:2109–21. doi: 10.1007/s11136-021-02826-0
8. Herrero, R, Díaz, A, and Zueco, J. The burden and psychological distress of family caregivers of individuals with autism spectrum disorder: a gender approach. J Clin Med. (2024) 13:2861. doi: 10.3390/jcm13102861
9. Gabra, RH, and Hashem, DF. Comparison of caregivers’ characteristics, stigma, and disease burden of children with autism spectrum disorder and attention-deficit disorder in Egypt. Middle East Curr Psychiatry. (2021) 28:1–8. doi: 10.1186/s43045-021-00162-0
10. Celik, P, and Kara Uzun, A. Stressful experiences and coping strategies of parents of young children with down syndrome: a qualitative study. J Appl Res Intellect Disabil. (2023) 36:881–94. doi: 10.1111/jar.13108
11. Ong, MBH, Davey, MJ, Nixon, GM, Walter, LM, and Horne, RSC. Effect of sleep disordered breathing severity in children with down syndrome on parental wellbeing and social support. Sleep Med. (2024) 116:71–80. doi: 10.1016/j.sleep.2024.02.037
12. AlShatti, A, AlKandari, D, AlMutairi, H, AlEbrahim, D, AlMutairi, A, AlAnsari, D, et al. Caregivers’ perceptions and experience of caring for persons with down syndrome in Kuwait: a qualitative study. Int J Dev Disabil. (2021) 67:381–90. doi: 10.1080/20473869.2021.1910780
13. Borthwick, C, Inchley, J, and Jones, J. Health promotion in adults with down’s syndrome: experiences of caregivers. J Intellect Disabil. (2021) 25:312–30. doi: 10.1177/1744629519890956
14. Peries, N, and Indrarathne, B. Lived experiences of primary caregivers of children with dyslexia: a phenomenological study. Indian J Psychol Med. (2024):02537176241274145. doi: 10.1177/02537176241274145
15. Wilmot, A, Pizzey, H, Leitao, S, Hasking, P, and Boyes, M. Growing up with dyslexia: child and parent perspectives on school struggles, self-esteem, and mental health. Dyslexia. (2023) 29:40–54. doi: 10.1002/dys.1729
16. Stephenson, N, Hvidberg, MF, and Rogish, M. The experience of parenting a child with dyslexia–a UK perspective with single parents. Res Dev Disabil. (2024) 147:104713. doi: 10.1016/j.ridd.2024.104713
17. Yanfei, Z. Clinical intervention of depression and anxiety in mothers of children with autism spectrum disorder East China Normal University (2019).
18. Roy, A Jr. A study on the caregiver’s burden of children with autism spectrum disorder (ASD). Indian J Psychiatry. (2024) 66:S85.
19. Su, X, Cai, RY, and Uljarević, M. Predictors of mental health in Chinese parents of children with autism spectrum disorder (ASD). J Autism Dev Disord. (2018) 48:1159–68. doi: 10.1007/s10803-017-3364-1
20. Zhang, X, and Zhao, J. Analysis of burden status and influencing factors for children with autism spectrum disorder. Nurs Res. (2022) 36:719–22.
21. Mo, KY-H, and Chan, ST-M. Parenting stress and coping strategies among parents of children with ADHD in China. J Child Fam Stud. (2024) 33:3826–39. doi: 10.1007/s10826-024-02916-w
22. Zhang, XN, Zhang, S, Liu, CY, Ni, ZH, and Lv, HT. Caregivers’ experience of having a child with down syndrome: a meta-synthesis. BMC Nurs. (2025) 24:66. doi: 10.1186/s12912-024-02652-y
23. Ng, CSM, Fang, Y, Wang, Z, and Zhang, M. Potential factors of parenting stress in Chinese parents of children with autism spectrum disorder: a systematic review. Focus Autism Other Dev Disabil. (2021) 36:237–48. doi: 10.1177/10883576211012599
24. Lin, J-D, Chen, W-X, Hsu, S-W, Lin, L-P, Lin, F-G, Tang, C-C, et al. Primary caregivers’ awareness and perception of early-onset dementia conditions in adolescents and young and middle-aged adults with down syndrome. Res Dev Disabil. (2014) 35:1934–40. doi: 10.1016/j.ridd.2014.04.026
25. Pang, X, Wang, H, Dill, S-E, Boswell, M, Pang, X, Singh, M, et al. Attention deficit hyperactivity disorder (ADHD) among elementary students in rural China: prevalence, correlates, and consequences. J Affect Disord. (2021) 293:484–91. doi: 10.1016/j.jad.2021.06.014
26. Germany, L, Ehlinger, V, Klapouszczak, D, Delobel, M, Hollody, K, Sellier, E, et al. Trends in prevalence and characteristics of post-neonatal cerebral palsy cases: a European registry-based study. Res Dev Disabil. (2013) 34:1669–77. doi: 10.1016/j.ridd.2013.02.016
27. Yuan, J, Wang, J, Ma, J, Zhu, D, Zhang, Z, and Li, J. Paediatric cerebral palsy prevalence and high-risk factors in Henan province, Central China. J Rehabil Med. (2019) 51:47–53. doi: 10.2340/16501977-2486
28. Barreto, TM, Bento, MN, Barreto, TM, Jagersbacher, JG, Jones, NS, Lucena, R, et al. Prevalence of depression, anxiety, and substance-related disorders in parents of children with cerebral palsy: a systematic review. Dev Med Child Neurol. (2020) 62:163–8. doi: 10.1111/dmcn.14321
29. Aisen, ML, Kerkovich, D, Mast, J, Mulroy, S, Wren, TAL, Kay, RM, et al. Cerebral palsy: clinical care and neurological rehabilitation. Lancet Neurol. (2011) 10:844–52. doi: 10.1016/S1474-4422(11)70176-4
30. Mori, Y, Downs, J, Wong, K, Anderson, B, Epstein, A, and Leonard, H. Impacts of caring for a child with the CDKL5 disorder on parental wellbeing and family quality of life. Orphanet J Rare Dis. (2017) 12:1–16. doi: 10.1186/s13023-016-0563-3
31. Sheng, N, Ma, J, Ding, W, and Zhang, Y. Effects of caregiver-involved interventions on the quality of life of children and adolescents with chronic conditions and their caregivers: a systematic review and meta-analysis. Qual Life Res. (2019) 28:13–33. doi: 10.1007/s11136-018-1976-3
32. Elangkovan, IT, and Shorey, S. Experiences and needs of parents caring for children with cerebral palsy: a systematic review. J Dev Behav Pediatr. (2020) 41:730–9. doi: 10.1097/DBP.0000000000000880
33. Whittingham, K, Wee, D, Sanders, MR, and Boyd, R. Sorrow, coping and resiliency: parents of children with cerebral palsy share their experiences. Disabil Rehabil. (2013) 35:1447–52. doi: 10.3109/09638288.2012.737081
34. Jankowska, AM, Włodarczyk, A, Campbell, C, and Shaw, S. Parental attitudes and personality traits, self-efficacy, stress, and coping strategies among mothers of children with cerebral palsy. Health Psychol Rep. (2015) 3:246–59. doi: 10.5114/hpr.2015.51903
35. Guimarães, A, Pereira, A, Oliveira, A, Lopes, S, Nunes, AR, Zanatta, C, et al. Parenting in cerebral palsy: understanding the perceived challenges and needs faced by parents of elementary school children. Int J Environ Res Public Health. (2023) 20:3811. doi: 10.3390/ijerph20053811
36. Albayrak, I, Biber, A, Caliskan, A, and Levendoglu, F. Assessment of pain, care burden, depression level, sleep quality, fatigue and quality of life in the mothers of children with cerebral palsy. J Child Health Care. (2019) 23:483–94. doi: 10.1177/1367493519864751
37. Vadivelan, K, Sekar, P, Sruthi, SS, and Gopichandran, V. Burden of caregivers of children with cerebral palsy: an intersectional analysis of gender, poverty, stigma, and public policy. BMC Public Health. (2020) 20:645. doi: 10.1186/s12889-020-08808-0
38. Dieleman, LM, Soenens, B, Prinzie, P, De Clercq, L, and Pauw, SSW. Parenting children with cerebral palsy: a longitudinal examination of the role of child and parent factors. Except Child. (2021) 87:369–90. doi: 10.1177/0014402920986462
39. Björquist, E, Nordmark, E, and Hallström, I. Parents’ experiences of health and needs when supporting their adolescents with cerebral palsy during transition to adulthood. Phys Occup Ther Pediatr. (2016) 36:204–16. doi: 10.3109/01942638.2015.1101041
40. Rentinck, ICM, Ketelaar, M, Jongmans, MJ, and Gorter, JW. Parents of children with cerebral palsy: a review of factors related to the process of adaptation. Child Care Health Dev. (2007) 33:161–9. doi: 10.1111/j.1365-2214.2006.00643.x
41. Cheshire, A, Barlow, J, and Powell, L. Coping using positive reinterpretation in parents of children with cerebral palsy. J Health Psychol. (2010) 15:801–10. doi: 10.1177/1359105310369993
42. Smith, M, and Blamires, J. Mothers’ experience of having a child with cerebral palsy. A systematic review. J Pediatr Nurs. (2022) 64:64–73. doi: 10.1016/j.pedn.2022.01.014
43. Pousada, M, Guillamón, N, Hernández-Encuentra, E, Muñoz, E, Redolar, D, Boixadós, M, et al. Impact of caring for a child with cerebral palsy on the quality of life of parents: a systematic review of the literature. J Dev Phys Disabil. (2013) 25:545–77. doi: 10.1007/s10882-013-9332-6
44. Wijesinghe, CJ, Cunningham, N, Fonseka, P, Hewage, CG, and Ostbye, T. Factors associated with caregiver burden among caregivers of children with cerebral palsy in Sri Lanka. Asia Pac J Public Health. (2015) 27:85–95. doi: 10.1177/1010539514548756
45. Bella, GP, Garcia, MC, and Spadari-Bratfisch, RC. Salivary cortisol, stress, and health in primary caregivers (mothers) of children with cerebral palsy. Psychoneuroendocrinology. (2011) 36:834–42. doi: 10.1016/j.psyneuen.2010.11.005
46. Carona, C, Crespo, C, and Canavarro, MC. Similarities amid the difference: caregiving burden and adaptation outcomes in dyads of parents and their children with and without cerebral palsy. Res Dev Disabil. (2013) 34:882–93. doi: 10.1016/j.ridd.2012.12.004
47. Fonzi, V, Sheriff, B, Dalglish, S, Anum, A, Agyei, ED, Diggs, D, et al. The multifaceted care-seeking practices among caregivers of children with cerebral palsy: perspectives from mothers and providers in Ghana. PLoS One. (2021) 16:e0258650. doi: 10.1371/journal.pone.0258650
48. Gugala, B. Caregiver burden versus intensity of anxiety and depression symptoms in parents of children with cerebral palsy as well as factors potentially differentiating the level of burden: a cross-sectional study (Poland). BMJ Open. (2021) 11:e036494. doi: 10.1136/bmjopen-2019-036494
49. Omole, JO, Adegoke, SA, Omole, KO, Mbada, CE, Adedeji, GA, and Adeyemi, OA. Levels, correlates, and predictors of stress and caregiver burden among caregivers of children with cerebral palsy in Nigeria. J Pediatr Neurol. (2019) 17:13–21. doi: 10.1055/s-0037-1612639
50. Marron, EM, Redolar-Ripoll, D, Boixados, M, Nieto, R, Guillamon, N, Hernandez, E, et al. Burden on caregivers of children with cerebral palsy: predictors and related factors. Univ Psychol. (2013) 12:767–77.
51. Yigman, F, Yigman, ZA, and Akyuz, EU. Investigation of the relationship between disease severity, caregiver burden and emotional expression in caregivers of children with cerebral palsy. Ir J Med Sci. (2020) 189:1413–9. doi: 10.1007/s11845-020-02214-6
52. Boztepe, H, Cinar, S, Ay, A, Yildiz, GK, and Kilic, C. Predictors of caregiver burden in mothers of children with leukemia and cerebral palsy. J Psychosoc Oncol. (2019) 37:69–78. doi: 10.1080/07347332.2018.1489441
53. Tarantino, D, Gnasso, R, Migliore, F, Iommazzo, I, Sirico, F, and Corrado, B. The effects of COVID-19 pandemic countermeasures on patients receiving botulinum toxin therapy and on their caregivers: a study from an Italian cohort. Neurol Sci. (2021) 42:3071–7. doi: 10.1007/s10072-021-05282-3
54. Whittingham, K, Wee, D, Sanders, MR, and Boyd, R. Predictors of psychological adjustment, experienced parenting burden and chronic sorrow symptoms in parents of children with cerebral palsy. Child Care Health Dev. (2013) 39:366–73. doi: 10.1111/j.1365-2214.2012.01396.x
55. Sear, R. Beyond the nuclear family: an evolutionary perspective on parenting. Curr Opin Psychol. (2016) 7:98–103. doi: 10.1016/j.copsyc.2015.08.013
56. Ruggles, S. Stem families and joint families in comparative historical perspective. Popul Dev Rev. (2010) 36:563–77. doi: 10.1111/j.1728-4457.2010.00346.x
57. Van Gasse, D, and Mortelmans, D. Reorganizing the single-parent family system: exploring the process perspective on divorce. Fam Relat. (2020) 69:1100–12. doi: 10.1111/fare.12432
58. Huroy, M, Behlim, T, Andersen, J, Buckley, D, Fehlings, D, Kirton, A, et al. Stability of the gross motor function classification system over time in children with cerebral palsy. Dev Med Child Neurol. (2022) 64:1487–93. doi: 10.1111/dmcn.15375
59. Garcia-Iniguez, J, Garcia-Contreras, AA, Vasquez-Garibay, EM, and Larrosa-Haro, A. Gurka vs slaughter equations to estimate the fat percentage in children with cerebral palsy from all subtypes and levels of the gross motor function classification system. BMC Pediatr. (2023) 23:152. doi: 10.1186/s12887-023-03970-x
60. Liu, Z, Sun, W, Chen, H, Zhuang, J, Wu, B, Xu, H, et al. Caregiver burden and its associated factors among family caregivers of persons with dementia in Shanghai, China: a cross-sectional study. BMJ Open. (2022) 12:e057817. doi: 10.1136/bmjopen-2021-057817
61. Chan, MF, Al-Dhawyani, AM, Al Hinai, K, and Al-Azri, M. A cluster analysis to explore the burden of primary caregivers of children with cancer in Oman. J Spec Pediatr Nurs. (2022) 27:e12389. doi: 10.1111/jspn.12389
62. Yildirim, S, Akyuz, O, Engin, E, and Gultekin, K. The relationship between psychiatric patients’ caregiver burden and anger expression styles. J Clin Nurs. (2018) 27:725–31. doi: 10.1111/jocn.14060
63. He, GX, and Ding, Y. Caregiver burden of rheumatoid arthritis patients with self-care deficit in China: a cross-sectional study. Arch Rheumatol. (2016) 31:371–6. doi: 10.5606/ArchRheumatol.2016.5779
64. Chou, KR, Jiann-Chyun, L, and Chu, H. The reliability and validity of the Chinese version of the caregiver burden inventory. Nurs Res. (2002) 51:324–31. doi: 10.1097/00006199-200209000-00009
65. Novak, M, and Guest, C. Application of a multidimensional caregiver burden inventory. Gerontologist. (1989) 29:798–803. doi: 10.1093/geront/29.6.798
66. Chu, SY, Rafi, ABM, Lee, J, Fierro, V, Gan, CH, Joginder Singh, S, et al. The relationship between affiliate stigma, stress, and quality of life for parents of individuals with cerebral palsy in Malaysia. Disabil Rehabil. (2023) 45:4035–47. doi: 10.1080/09638288.2022.2153304
67. Liu, W, Yu, F, Geldsetzer, P, Yang, J, Wang, Z, Golden, T, et al. Prevalence of depression in China during the early stage of the COVID-19 pandemic: a cross-sectional study in an online survey sample. BMJ Open. (2022) 12:e056667. doi: 10.1136/bmjopen-2021-056667
68. Li, X-y, Wang, J, Zhang, R-x, Chen, L, He, CK, Wang, C-y, et al. Psychological status among anesthesiologists and operating room nurses during the outbreak period of COVID-19 in Wuhan, China. Front Psych. (2020) 11:574143. doi: 10.3389/fpsyt.2020.574143
69. Chen, J, Zhang, M-y, Gao, Y-h, Zhang, L, and Li, J. Quality of life after idiopathic multicentric Castleman disease in China: a cross-sectional, multi-center survey of patient reported outcome and caregiver reported outcome. Orphanet J Rare Dis. (2024) 19:469. doi: 10.1186/s13023-024-03450-0
70. Zhang, X, Dai, XS, Jiao, J, and Lee, SY. Impact of sleep-wake features on fatigue among female shift work nurses. Ann Med. (2023) 55:2210843. doi: 10.1080/07853890.2023.2210843
71. Shen, Y, Shi, HC, Zhong, JG, Pan, PL, Wang, SF, Chen, MZ, et al. Factors correlated with excessive daytime sleepiness in patients with Parkinson’s disease: a polysomnography study. Brain Behav. (2023) 13:e3202. doi: 10.1002/brb3.3202
72. Alzhrani, AA, Alsuhail, AI, and Rababah, AA. Fatigue prevalence among palliative care cancer patients in comprehensive cancer center, King Fahad Medical City, Riyadh, Saudi Arabia: a cross-sectional study. J Palliat Care. (2023) 38:424–431. doi: 10.1177/08258597231191615
73. Feng, C, He, Q, Wu, Y, Hu, X, Wu, J, He, X, et al. Psychometric properties of fatigue severity scale in Chinese systemic lupus erythematosus patients. Health Qual Life Outcomes. (2019) 17:71. doi: 10.1186/s12955-019-1141-x
74. Pasin, T, Karatekin, BD, and Pasin, O. Chronic fatigue syndrome in caregivers of children with cerebral palsy and affecting factors. North Clin Istanbul. (2023) 10:642–650. doi: 10.14744/nci.2023.53533
75. Farajzadeh, A, Maroufizadeh, S, and Amini, M. Factors associated with quality of life among mothers of children with cerebral palsy. Int J Nurs Pract. (2020) 26:e12811. doi: 10.1111/ijn.12811
76. Dambi, JM, Jelsma, J, and Mlambo, T. Caring for a child with cerebral palsy: the experience of Zimbabwean mothers. Afr J Disabil. (2015) 4:168. doi: 10.4102/ajod.v4i1.168
77. Oliveira Barros, AL, de Gutierrez, GM, Barros, AO, and Botti Rodrigues Santos, MT. Quality of life and burden of caregivers of children and adolescents with disabilities. Spec Care Dentist. (2019) 39:380–8. doi: 10.1111/scd.12400
78. Sheikhbardsiri, H, Tavan, A, Afshar, PJ, Salahi, S, and Heidari-Jamebozorgi, M. Investigating the burden of disease dimensions (time-dependent, developmental, physical, social and emotional) among family caregivers with COVID-19 patients in Iran. BMC Prim Care. (2022) 23:165. doi: 10.1186/s12875-022-01772-1
79. Chaghazardi, M, Janatolmakan, M, Rezaeian, S, and Khatony, A. Care burden and associated factors in caregivers of children with cancer. Ital J Pediatr. (2022) 48:92–99. doi: 10.1186/s13052-022-01291-w
80. Park, E-Y, and Nam, S-J. Time burden of caring and depression among parents of individuals with cerebral palsy. Disabil Rehabil. (2019) 41:1508–13. doi: 10.1080/09638288.2018.1432705
81. Dako-Gyeke, M, Boateng, DA, Mills, AA, Kodom, RB, and Appiah-Kubi, J. Known by the children’s condition: associative stigma among family carers of children with cerebral palsy. Glob Soc Welf. (2021) 8:1–14. doi: 10.1007/s40609-021-00203-w
82. Strommen, J, Fuller, H, Sanders, GF, and Elliott, DM. Challenges faced by family caregivers: multiple perspectives on eldercare. J Appl Gerontol. (2020) 39:347–56. doi: 10.1177/0733464818813466
83. Somanadhan, S, McAneney, H, Awan, A, McNulty, S, Sweeney, A, Buckle, N, et al. Assessing the supportive care needs of parents of children with rare diseases in Ireland. J Pediatr Nurs. (2025) 81:31–42. doi: 10.1016/j.pedn.2025.01.003
84. Litzelman, K, Catrine, K, Gangnon, R, and Witt, WP. Quality of life among parents of children with cancer or brain tumors: the impact of child characteristics and parental psychosocial factors. Qual Life Res. (2011) 20:1261–9. doi: 10.1007/s11136-011-9854-2
85. Brandt, M, Johannsen, L, Inhestern, L, and Bergelt, C. Parents as informal caregivers of children and adolescents with spinal muscular atrophy: a systematic review of quantitative and qualitative data on the psychosocial situation, caregiver burden, and family needs. Orphanet J Rare Dis. (2022) 17:274. doi: 10.1186/s13023-022-02407-5
86. Glumbic, N, Grujicic, R, Stupar, S, Petrovic, S, and Pejovic-Milovancevic, M. Positive effects of the caregiver skill training program on children with developmental disabilities: experiences from Serbia. Front Psych. (2022) 13:13. doi: 10.3389/fpsyt.2022.913142
87. Hassan, M, Simpson, A, Danaher, K, Haesen, J, Makela, T, and Thomson, K. An evaluation of behavioral skills training for teaching caregivers how to support social skill development in their child with autism spectrum disorder. J Autism Dev Disord. (2018) 48:1957–70. doi: 10.1007/s10803-017-3455-z
88. Montiel-Nava, C, Tregnago, M, Marshall, J, Sohl, K, Curran, AB, Mahurin, M, et al. Implementing the WHO caregivers skills training program with caregivers of autistic children via telehealth in rural communities. Front Psych. (2022) 13:909947. doi: 10.3389/fpsyt.2022.909947
89. Wong, PW-C, Lam, Y-Y, Lau, JS-P, and Fok, H-K Team WC. Adapting and pretesting the World Health Organization’s caregiver skills training program for children with autism and developmental disorders or delays in Hong Kong. Sci Rep. (2022) 12:16932. doi: 10.1038/s41598-022-21343-9
90. Sawyer, MG, Bittman, M, La Greca, AM, Crettenden, AD, Borojevic, N, Raghavendra, P, et al. Time demands of caring for children with cerebral palsy: what are the implications for maternal mental health? Dev Med Child Neurol. (2011) 53:338–43. doi: 10.1111/j.1469-8749.2010.03848.x
91. Braich, PS, Lal, V, Hollands, S, and Almeida, DR. Burden and depression in the caregivers of blind patients in India. Ophthalmology. (2012) 119:221–6. doi: 10.1016/j.ophtha.2011.07.038
92. Lou, Q, Liu, S, Huo, YR, Liu, M, Liu, S, and Ji, Y. Comprehensive analysis of patient and caregiver predictors for caregiver burden, anxiety and depression in Alzheimer’s disease. J Clin Nurs. (2015) 24:2668–78. doi: 10.1111/jocn.12870
93. Oberoi, DV, White, V, Jefford, M, Giles, GG, Bolton, D, Davis, I, et al. Caregivers’ information needs and their ‘experiences of care’ during treatment are associated with elevated anxiety and depression: a cross-sectional study of the caregivers of renal cancer survivors. Support Care Cancer. (2016) 24:4177–86. doi: 10.1007/s00520-016-3245-8
94. Pan, Y-C, and Lin, Y-S. Systematic review and meta-analysis of prevalence of depression among caregivers of cancer patients. Front Psych. (2022) 13:817936. doi: 10.3389/fpsyt.2022.817936
95. Parker Oliver, D, Washington, K, Smith, J, Uraizee, A, and Demiris, G. The prevalence and risks for depression and anxiety in hospice caregivers. J Palliat Med. (2017) 20:366–71. doi: 10.1089/jpm.2016.0372
96. Lynch, SH, Shuster, G, and Lobo, ML. The family caregiver experience–examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes. Aging Ment Health. (2018) 22:1424–31. doi: 10.1080/13607863.2017.1364344
97. Lu, S-H, Yiin, J-J, Lin, Y-P, and Lee, K-C. Effect of a web-based integrative support intervention to improve family caregiver positive caregiving experience and quality of life: a randomized controlled trial. Cancer Nurs. (2022) 1090–1097. doi: 10.1097/NCC.0000000000001387
98. Hollister, B, Crabb, R, Kaplan, S, Brandner, M, and Arean, P. Effectiveness of case management with problem-solving therapy for rural older adults with depression. Am J Geriatr Psychiatry. (2022) 30:1083–92. doi: 10.1016/j.jagp.2022.03.001
Keywords: cerebral palsy, child, caregiver experience, parents, depression, fatigue
Citation: Zhong X and Wijesinghe CJ (2025) The level and factors associated with caregiver experience among parents of children with cerebral palsy: a cross-sectional study in Southwest China. Front. Public Health. 13:1482011. doi: 10.3389/fpubh.2025.1482011
Edited by:
Nuri Reyes, University of Colorado Anschutz Medical Campus, United StatesReviewed by:
Siva Priya Santhanam, Bowling Green State University, United StatesMaritza Cobian, University of Colorado Hospital, United States
Copyright © 2025 Zhong and Wijesinghe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoying Zhong, MjAyMDIyNDAyOTU1NkBhbHUuc2N1LmVkdS5jbg==
 Xiaoying Zhong
Xiaoying Zhong Champa J. Wijesinghe2
Champa J. Wijesinghe2