- 1Department of Clinical Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Curtin Medical School, Faculty of Health Sciences, Curtin University, Bentley, WA, Australia
- 3Department of Pharmaceutics and Social Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Pharmacognosy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 5Department of Pharmaceutical Chemistry, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 6School of Medicine, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
- 7Department of Pharmacy, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
- 8College of Medicine and Health Sciences, Woldia University, Woldia, Ethiopia
- 9School of Population Health, Curtin University, Bentley, WA, Australia
Background: Pharmacists play a crucial role in the prevention and management of noncommunicable diseases (NCDs) by providing medication therapy management, disease monitoring, and patient education. However, existing evidence on the roles and barriers of community pharmacy professionals (CPPs) in preventing and managing noncommunicable diseases in Ethiopia remains inconsistent. This study aimed to synthesize available research on the roles and barriers faced by CPPs in noncommunicable diseases prevention and management among adults in Ethiopia.
Methods: A comprehensive literature search using four electronic databases, including Scopus, Medline/Ovid, Web of Science, and Embase was conducted. In addition, further studies were identified through Google Scholar searches and manual reference searches. The review included studies published before 30 July 2024 without any limitations on the starting time.
Results: A total of 15 studies were included in this review, with most studies focused on CPPs’ involvement in the prevention and management of non-specific NCDs and diabetes. CPPs were involved in a variety of roles in the prevention, screening, and management of NCDs. Their scope of practice included providing health promotion on lifestyle changes and nutrition, medication therapy management, chronic disease screening, disease-specific counseling, and general self-care promotion. This review identified different barriers CPPs encountered during their provision of NCD care, which were mainly categorized under four classes: CPP-related, pharmacy setting and working environment-related, policy/healthcare system-related, and patient/public-related barriers.
Conclusion: CPPs provide a wide range of services, from health promotion to disease screening and management of noncommunicable diseases. However, potential barriers such as limited training and resources, lack of reimbursement for noncommunicable disease services, and inadequate integration into the healthcare system can limit them from effectively providing these services. Addressing these barriers is essential to enhance the role of CPPs in noncommunicable diseases prevention and management.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42023486384, Unique Identifier: CRD42023486384.
Introduction
Chronic diseases are major public health challenges worldwide, accounting for a significant portion of morbidity and mortality. According to the World Health Organization (WHO), noncommunicable diseases (NCDs), including heart disease, stroke, cancer, diabetes, and chronic lung disease, are collectively responsible for 74% of all deaths worldwide. Over 75% of all NCD deaths, and 86% of the 17 million people who died before the age of 70, occur in low- and middle-income countries (1).
Ethiopia has made significant progress on social development, including poverty reduction, with encouraging results in communicable disease control, improved nutrition, and maternal and child health (2). However, the country is also experiencing an epidemiological shift, with a rapidly increasing prevalence of NCDs, which calls for new and innovative public health strategies to address the double burden of diseases. Studies conducted by the Federal Ministry of Health in 2015 (STEPS Survey) showed evidence of an increasing burden of NCDs and their risk factors, driven by factors such as population aging, urbanization, and lifestyle changes (3). The four most common NCDs in Ethiopia are cardiovascular diseases, diabetes, cancer, and chronic respiratory diseases, which account for a significant portion of the country’s healthcare burden, both in terms of cost and lost productivity (4).
The Ethiopian healthcare system faces numerous challenges in preventing and managing NCDs (5). These challenges include a shortage of healthcare workers, particularly specialists in chronic disease management, limited access to essential medications and diagnostics, low patient awareness of NCDs and their risk factors, and lack of adherence to treatment regimens (6, 7). These factors hinder effective prevention and management, leaving many Ethiopians undiagnosed, untreated, or with inadequate care (8–10).
The International Pharmaceutical Federation reveals that pharmacists are increasingly being recognized as valuable members of the healthcare team in the prevention and management of NCDs (11). Pharmacists are readily accessible to patients, have a strong understanding of medications, and can provide individualized counseling and support to patients with different medical conditions (12–21). Studies worldwide have demonstrated that community pharmacists can effectively deliver chronic disease prevention and management services, including medication therapy management, disease monitoring, and patient education (15, 22–29).
In Ethiopia, patients with noncommunicable diseases are typically diagnosed and initiated on treatment by clinicians at the primary healthcare level (30). Once their condition stabilizes, they may obtain medication refills at community pharmacies using valid prescriptions. This shift is largely driven by the higher cost and limited accessibility of services, such as physician consultations, laboratory services, and medicines, within the primary healthcare facilities. Convenience and accessibility are also the main reasons that patients choose community pharmacies.
Community pharmacy professionals (CPPs) have increasingly contributed to the prevention and management of noncommunicable diseases (31–35). Beyond dispensing medications, pharmacists provide minor illness management, lifestyle counseling, and health education. Their strong understanding of pharmacotherapy management enables them to provide effective medication counseling, monitor adherence and adverse effects, and refer patients to other healthcare providers when necessary (22, 34). Given the wide availability of pharmacies across the country, CPPs are well-position to support chronic disease care and improve access to prevention and management services (36).
A preliminary review of existing studies on CPPs’ roles in noncommunicable disease prevention and management in Ethiopia revealed a lack of generalizability and inconsistent findings due to varying study designs, methodologies, and outcomes. This gap highlights the need for a comprehensive study that assesses the scope of practices and barriers to effective engagement in preventing and managing noncommunicable diseases among CPPS. Therefore, this study aimed to comprehensively synthesize existing evidence regarding CPPs’ roles and perceived barriers in the prevention and management of noncommunicable diseases in Ethiopia. The review first discusses CPPs’ scopes of practice and then follows a presentation of the barriers hindering their full engagement in the prevention and management of noncommunicable diseases.
Methods
Registration and reporting
The protocol for this review was registered in the PROSPERO database (CRD42023486384) and is publicly accessible. The protocol has been revised after observing the works of literature in the initial search outcome. Modifications were made and expanded regarding inclusion and exclusion criteria. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 checklist was used to guide the reporting of this systematic review (37) (Supplementary file S1).
Eligibility criteria
We included eligible studies that examined the roles and/or barriers of CPPs in preventing and managing NCDs in adults within community settings. Studies that addressed both roles and barriers, or either one, were included based on the following inclusion and exclusion criteria.
Inclusion criteria
Articles that met the following criteria were considered for inclusion in this systematic review.
i. Study population: CPPs [pharmacists with bachelor’s degree holders and above and diploma holders (pharmacy technicians)].
ii. Intervention (counseling, screening, health promotion and education, and medication management): studies reported about potential roles CPPs played in counseling, screening, medication management, and health promotion and education in the prevention and/or management of NCDs and/or barriers in providing these practices.
iii. Outcome (preventing and managing NCDs): studies conducted on one or more of these NCDs, including cardiovascular diseases, diabetes, chronic respiratory diseases, and cancer in adults.
iv. Context: Ethiopia.
v. Study design: no restriction.
vi. Study setting: community drug retail outlets (CDROs), including pharmacies and drug stores located in Ethiopia.
vii. Population served by CPPs: adults (age ≥ 18 years).
viii. Time: no restriction for starting and articles published until July 30, 2024.
ix. Language: studies conducted in English.
x. Type of studies: limited to published peer-reviewed primary studies and thesis and/or dissertations were included in this study.
Noncommunicable chronic diseases
This review determined chronic disease based on the WHO definition. Chronic diseases are not contagious and typically last a long time, often progressing slowly (38). Our review also ensured the inclusion of articles that involved these main types of NCDs, such as cardiovascular diseases (including hypertension, heart attacks, and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma), and diabetes. Although metabolic syndrome is not classified among the four main categories of NCDs, it was included in our review due to its association with cardiovascular and high blood glucose issues, and its role as a major risk factor for other NCDs.
Therefore, this review included all articles focused on the roles and barriers of CPPs in the management and prevention of one or more specific or non-specified NCDs in adults.
Exclusion criteria
Research articles such as reviews, letters to editors, short communications, commentaries, book chapters, and conference abstracts were excluded from this review.
Data sources
A comprehensive literature search was conducted, with an initial database search on 15 January 2024 and finalized on 30 July 2024, using four electronic databases: Scopus, Medline/Ovid, Web of Science, and Ovid Embase. In addition, further studies were identified through a manual Google Scholar search and manual reference searching of included studies. This study included all studies published in Ethiopia before 30 July 2024 without any other limitations.
Search strategy
The search strategy aimed to identify studies reporting on the roles and barriers of CPPs in the prevention and management of NCDs in Ethiopia. Search terms related to CPPs, NCDs, chronic diseases, roles, and barriers were combined using Boolean operators “OR” and “AND” to develop the search strategy (Figure 1). The comprehensive search strategies used in the Medline and Scopus searches are available in the Supplementary file S2.
Study selection process
Identified records from individual databases were exported to EndNote version 20 and then to Covidence for screening. After de-duplication, eligible records were screened starting from 30 July 2024 using title and abstract for full-text retrieval by the first investigator (AKS). Finally, a full-text screening was carried out by three investigators (AKS, EAB, and LWL) independently to identify eligible articles using predetermined inclusion and exclusion methods. Disagreements were resolved through discussion using specified criteria.
Data extraction process
After identifying full-text screened studies, data were extracted by three investigators (GSC, ADD, YBT) using a tailored data extraction format prepared by the research team in Microsoft Excel. Data extracted included the name of the first author, publication year, study design, total number of participants, level of pharmacy professionals (bachelor’s and above and diploma), types of NCDs, reported roles in preventing and managing NCDs, and reported barriers of CPPs in preventing and managing NCDs. Disagreements between authors that arose during screening and data extraction were resolved through discussion using specified criteria and the involvement of other investigators (KYG, FBT, BBA).
Quality assessment
The quality of the included articles was assessed using the Joanna Briggs Institute (JBI) quality appraisal tools for analytical cross-sectional studies (39). Three investigators (AKS, GKB, BBA) independently assessed the quality of the included articles using the JBI critical appraisal checklist, which consists of eight criteria: (1) clear inclusion and exclusion criteria; (2) description of the study subject and setting; (3) use of a valid and reliable method to measure exposure; (4) standard criteria used for measurement of the condition; (5) identification of potential confounding factors; (6) development of strategies to deal with confounding factors; (7) use of a valid and reliable method to measure the outcomes; and (8) use of appropriate statistical analysis. To determine the risk of bias, studies were classified into three categories based on their total scores: Low risk (score of 6 to 8), moderate risk (score of 3 to 5), and high risk (score of 0 to 2). Only studies with low or moderate risk of bias were included in this review. Disagreements that arose during the full-text quality assessment were resolved through evidence-based discussion with the involvement of other review authors (AKS, LWL, FBT).
Data synthesis
The data for both roles and barriers were thematized for synthesis and presentation. Thematic areas in terms of types of NCDs: (I) NCDs (non-specified), (II) diabetes, (III) cardiovascular diseases, (IV) asthma, and (V) metabolic syndrome. The roles of CPPs were categorized under: (I) general health education and promotion services, (II) promotion related to nutrition and lifestyle modification, (III) medication therapy management, (IV) chronic disease screening and counseling, and (V) disease-specific and other counseling. Barriers were categorized under four themes based on the sources and nature of the barriers: (I) CPP-related, (II) pharmacy setting and work environment-related, (III) policy and healthcare system-related, and (IV) patient/client or public-related barriers.
Results
Screening results
A total of 393 articles were identified using electronic databases and two manual searches of other relevant sources. After removing duplicate records, 341 records were screened. Following the exclusion of 324 articles based on titles and abstracts, 17 were assessed in full text. Two articles were excluded (one for not addressing the phenomena of interest and one for including a non-target population), resulting in 15 studies included in the review. The PRISMA flow diagram summarizes the selection process (Figure 2).
Characteristics of included studies
The included studies were published between 2017 and 2024. Except for one non-peer-reviewed master’s thesis study found in the repository of Addis Ababa University (40), all were peer-reviewed articles. Most studies were conducted in Gondar City and nearby (22, 34, 41–44) and Amhara region using multi-center study designs (31–33, 45–47). Two studies were carried out in Addis Ababa City (40, 48), and one study in Injibara City (49). Most of the studies were conducted using a cross-sectional survey design, except two studies used cross-sectional plus simulated patient (SP)-based scenarios to observe actual practices (31, 42). The reviewed studies included several participants ranging from 24 (49) up to 412 (46, 47) (Table 1).
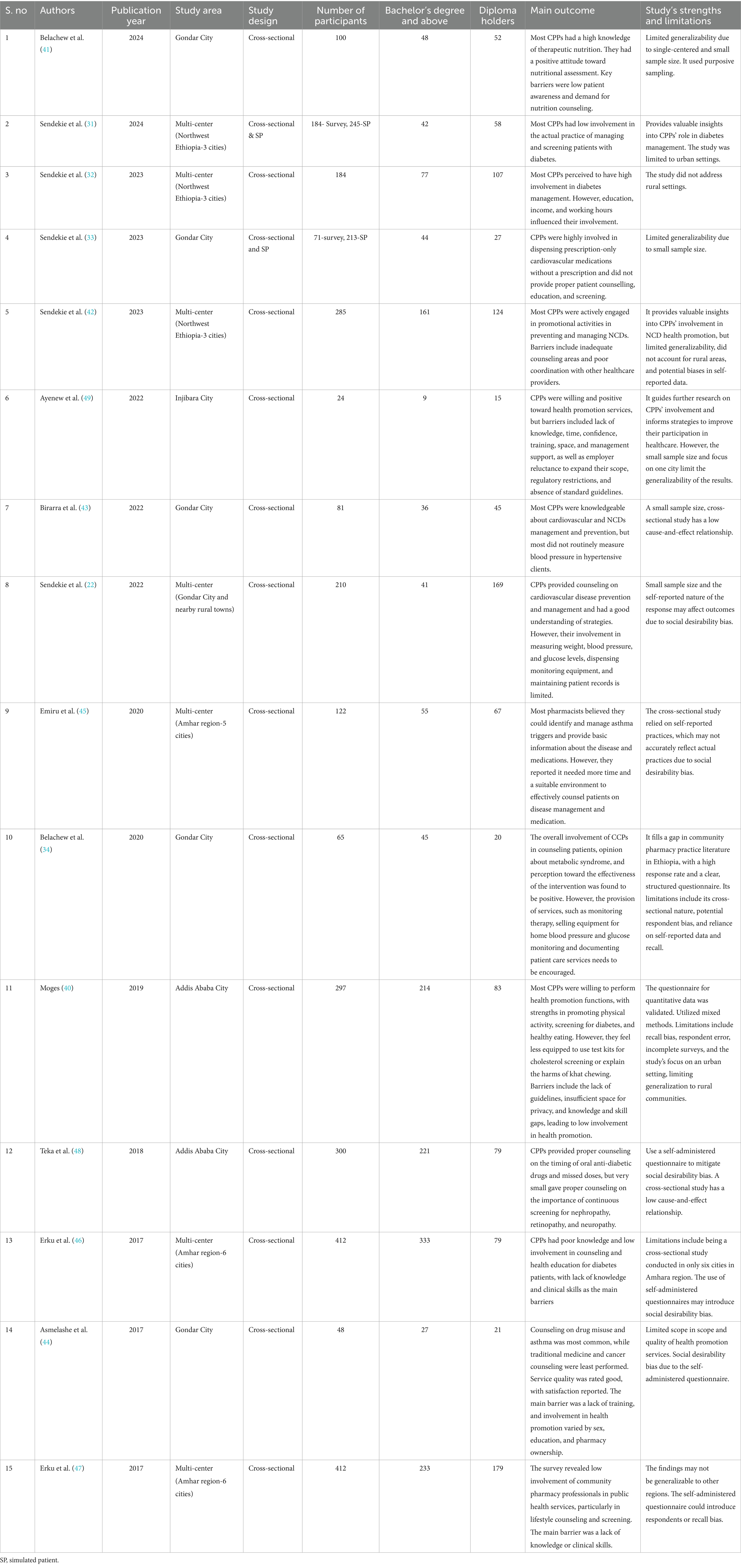
Table 1. Characteristics of included articles related to roles and barriers of community pharmacy professionals in the prevention and management of noncommunicable diseases in Ethiopia.
Quality assessment
The quality assessment results, conducted using the JBI quality appraisal tools for analytical cross-sectional studies, showed that all included articles scored 6–7 out of 8 and were found to be in the range of low risk of bias (22, 31–34, 40–49) (Supplementary file S3).
Types of NCDs managed by community pharmacy professionals
Among the included studies in this review, six studies explored the involvement of CPPs in non-specific NCD prevention and management practices (33, 40, 41, 44, 47, 49) and addressing the most common chronic diseases such as diabetes, cardiovascular diseases, asthma, and cancer. Four studies were conducted about the involvement of CPPs in the management of patients with diabetes (31, 32, 46, 48), and three studies were conducted focusing on CPPs’ involvement in managing cardiovascular diseases (22, 42, 43). The remaining two studies assessed CPPs’ practices regarding asthma (45) and metabolic syndrome (34) (Table 2).
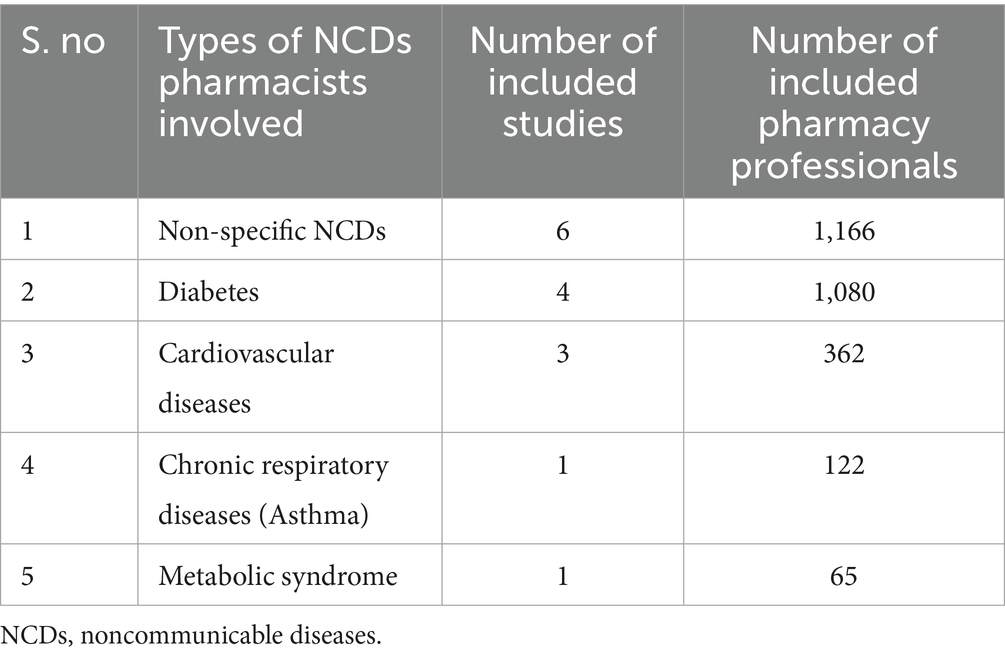
Table 2. Studies explored community pharmacy professionals’ involvement regarding types of noncommunicable diseases in the prevention and management in Ethiopia.
Roles of community pharmacy professionals in preventing and managing NCDs
Studies revealed that CPPs were involved in various health education services, including health education on screening, risk factors, and the burden of NCDs (complications and economic and social problems) (22, 32–34, 44), primary health prevention activities related to counseling on nutrition and lifestyle changes (22, 31–34, 40–44, 46–49), and medication therapy management counseling (22, 31–34, 45, 46, 48). Additionally, despite limitations in terms of the number of CPPs involved, CPPs were involved in the screening of chronic diseases such as hypertension and diabetes (22, 31–34, 40, 43, 47), asthma (45, 47), cholesterol screening (40, 43, 47), and cancer screening (44). Although the number of CPPs involved varied across studies, disease-specific and other counseling practices, such as counseling on retinopathy, nephropathy, neuropathy screening, foot care, and eye care for patients with diabetes (40, 46), counseling patients to consult clinicians/physicians (22, 31–34), and immunization counseling related to certain NCDs, including cancer, for an adult population were within the scope of CPPs’ practices (44, 49) (Table 3).
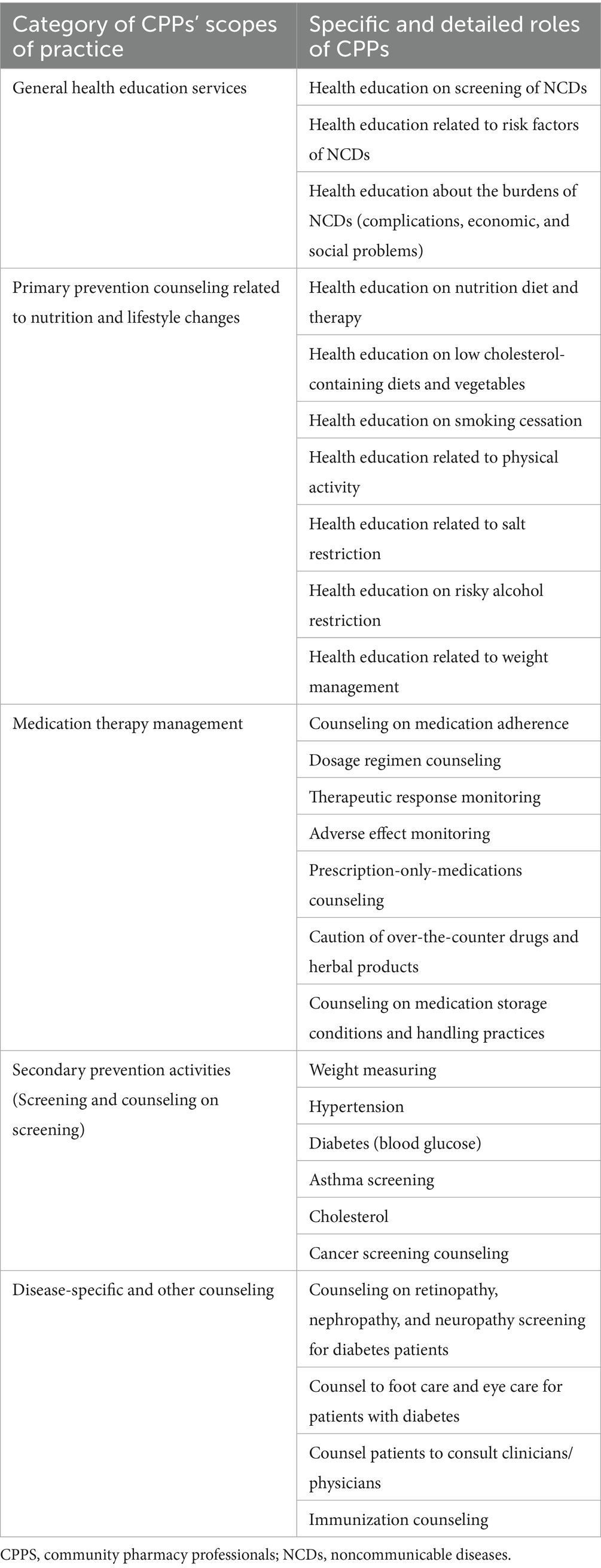
Table 3. Scopes of practice and specific activities of community pharmacy professionals involved in the prevention and management of noncommunicable diseases in Ethiopia.
Barriers to community pharmacy professionals in preventing and managing NCDs
Of the 15 studies included in this review, 10 studies reported potential barriers that influence CPPs’ active involvement in preventing and managing NCDs. The identified barriers were mainly related to CPP-related factors, pharmacy setting and working environment factors, policy and healthcare system factors, and patient/client and public factors (22, 33, 40, 41, 43–47, 49). The most reported high levels of barriers were workload/lack of time, lack of clinical knowledge and skills, lack of resources such as updated and standardized guidelines, limited on-the-job training and continuing education, and lack of appropriate and standardized private counseling areas, and lack of follow-up and service monitoring from regulatory bodies (Table 4).
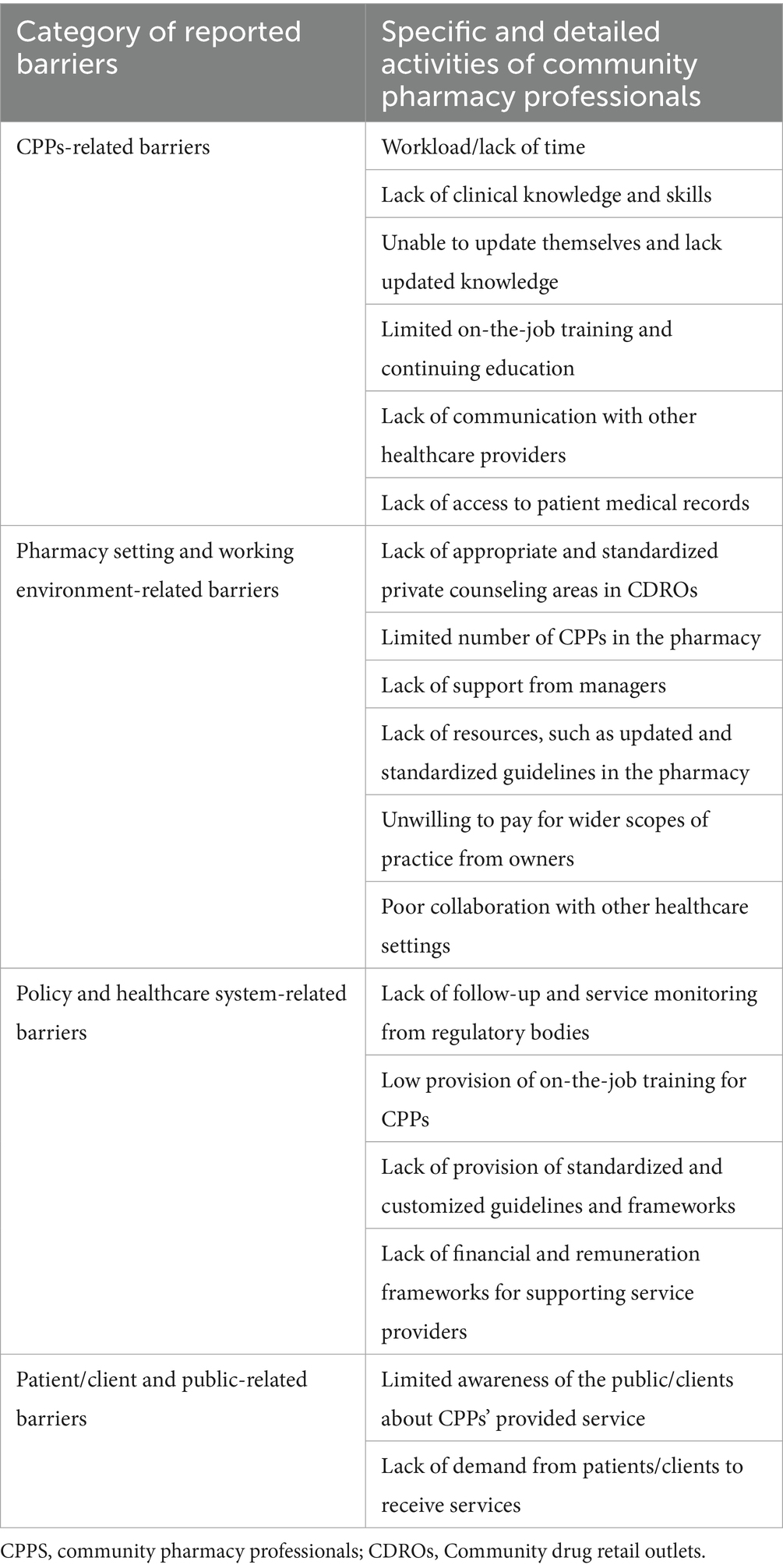
Table 4. Barriers to the involvement of community pharmacy professionals in noncommunicable disease prevention and management in Ethiopia.
Discussion
NCDs pose a significant global health challenge, and CPPs are increasingly recognized as key players in their prevention and management. This review highlights the role of Ethiopian CPPs in NCD care, revealing a range of activities from health promotion to disease screening and counseling. However, different barriers that need to be addressed are also identified in this review.
Community pharmacy professionals’ roles in the prevention and management of NCDs
To tackle the increasing burden of chronic diseases, the involvement of stakeholders is crucial, and incorporating CPPs in this role could be instrumental. The findings from this review revealed that CPPs are involved in general health promotion, nutrition, lifestyle education, and medication therapy management. They also engage in screening for chronic diseases such as hypertension, diabetes, asthma, and cholesterol. Furthermore, CPPs provide disease-specific counseling services, demonstrating a level of care that is often lacking in primary healthcare settings. However, inconsistency in the scope of CPPs’ practices across different studies raises concerns about the accessibility and availability of these services. Further research is warranted to understand the factors influencing the variation in CPPs’ involvement across different regions of Ethiopia.
This review highlights the potential of CPPs in preventing and managing NCDs. The current findings align with evidence from reviews in low- and middle-income countries, which has shown a positive impact of community pharmacies in NCD services (50–53). Another primary study in low- and middle-income countries, such as Nepal, has shown a positive impact of the community pharmacy workforce in preventing and managing NCDs (54). Studies from Lesotho (55), Ghana (25, 56) and Nigeria (23, 24, 57) report similar involvement in health promotion, medication therapy management, and disease screening. A study in Kuwait also revealed a significant role of CPPs in preventing and managing metabolic syndrome (26). These findings have the potential to expand the role of the pharmacy workforce in primary healthcare globally. However, the extent of these activities varies significantly across countries, influenced by regulatory frameworks, healthcare system structures, and level of economic development.
There is a growing trend worldwide toward expanding the role of CPPs in NCD care (28, 58). Countries such as the United Kingdom (59), Australia (60, 61), and Canada (62–64) have implemented pharmacist-led models that include disease management programs, medication reviews, and chronic disease screening. Evidence shows a significant impact of pharmacists on diabetes management and screening (65, 66). In countries with well-established healthcare systems, community pharmacists play a vital role in NCD prevention and management, with an umbrella review demonstrating their contributions to improved clinical outcomes in diabetes, hyperlipidemia, cardiovascular diseases, and respiratory conditions (67). However, findings from this review reveal that CPPs’ involvement in Ethiopia varies based on their educational background. Many practitioners are diploma-level graduates or did not receive regular on-the-job training, influencing their capacity for service delivery. This underscores the need for training and continuing education to enhance their effectiveness.
The findings from this review indicate a strong focus on health promotion and education related to nutrition and lifestyle changes, which are crucial for NCD prevention. This aligns with global recommendations for pharmacists’ role in promoting healthy behaviors (68). Other African countries have reported similar efforts in NCD prevention, with pharmacists providing counseling on diet, exercise, and smoking cessation (50, 69). A systematic review also highlights community pharmacists’ significant role in preventing cardiovascular disease risk factors through health promotion and education related to nutrition and lifestyle changes (70). However, the intensity and reach of pharmacists’ roles vary considerably. For instance, in developed countries, pharmacists are actively involved in vaccination programs, such as HPV and hepatitis B, which, while targeting infectious agents, contribute to the prevention of certain NCDs like cervical and liver cancers (71). While this aspect is not explicitly covered in the studies reviewed here, it is a critical component of pharmacists’ health promotion role in other regions.
This review also highlights the involvement of CPPs in screening for hypertension, diabetes, asthma, and cholesterol, which is commendable given the resource constraints. Screening for NCDs is gaining momentum in many African countries, with pharmacists playing an increasingly important role (72–74). However, access to diagnostic tools and trained personnel remain a challenge. A study in Saudi Arabia reveals pharmacists’ roles in cardiovascular disease screening (75), while studies in Brazil, India, South Africa, and the United States (76), Australia (66) showed a significant engagement of pharmacists in chronic disease screening. However, findings from this review indicate that screening practices are limited and vary across settings, highlighting the need for further evaluation of the sustainability of these services and their impact on patient outcomes.
Notably, none of the included studies in this review explicitly address the involvement of CPPs in cancer screening, except for one study that reported CPPs providing cancer screening counseling (44). However, findings from other systematic reviews (77) and studies in Canada (78) suggest that community pharmacists can contribute to cancer screening. The current findings indicate the need to empower CPPs to play a greater role in cancer screening, thereby increasing their public health impact.
This review also highlights CPPs’ role in medication therapy management for patients with NCDs. In many developed countries, pharmacists are at the forefront of NCD management, providing comprehensive medication reviews, adherence counseling, and self-management support (79–81). They work closely with patients, physicians, and other healthcare professionals to optimize treatment outcomes. While medication therapy management is recognized as a crucial role for CPPs in NCD management, findings from this study indicate wide variations in implementation across studies, largely influenced by CPPs’ educational backgrounds and training levels. These disparities underscore the need for further research and policy reforms to strengthen and standardize the role of CPPs in NCD prevention and management in developing countries.
Barriers to community pharmacy professionals in the prevention and management of NCDs
The review’s findings underscore the significant challenges CPPs face in Ethiopia in their efforts to contribute to chronic disease prevention and management. Identified barriers were categorized into four key barrier categories—CPPs-related, pharmacy setting and working environment-related, policy and healthcare system-related, and patient/client and public-related barriers.
The review identified CPPs-related barriers such as lack of knowledge, skills, workload, lack of resources, limited training and continuing education, and lack of collaboration with other healthcare providers as potential barriers. These challenges are not unique to Ethiopia and are commonly reported in other African countries (51, 69). However, the extent of these barriers may vary depending on the level of pharmaceutical education and training available.
This review discloses that CPPs in Ethiopia lack adequate training and resources to effectively manage chronic diseases. Most studies indicated that a significant number of CPPs had attained a diploma-level education. They may not have access to up-to-date clinical guidelines, diagnostic tools, or patient education materials (22, 33). Globally, there is a growing recognition of the need for continuous professional development for pharmacists to equip them with the necessary competencies to manage chronic diseases (82). Many countries have implemented structured training programs and certification schemes to address this gap (83). To improve the public health services provided in community pharmacies, training must aim to increase CPPs’ confidence in providing these services.
Workload and time constraints are also mentioned as main sources of barriers. CPPs face multiple demands in their roles, including dispensing medications, managing administrative tasks, responding to urgent patient needs, and providing counseling and clinical services. These pressures often limit their capacity to deliver optimal patient care. This finding is in line with findings from Senegal (84) and Australia (85). The finding suggests that assigning enough CPPs can help provide optimal service provisions.
As highlighted in the review, the pharmacy setting and working environment in Ethiopia present significant challenges, such as inadequate counseling areas and resources, a limited number of CPPs and a lower workforce, lack of support from managers, and inadequate integration of pharmacies with other healthcare settings. These conditions are common in many African countries due to limited healthcare infrastructure and economic constraints (51, 86). Globally, there is a wide variation in pharmacy settings (87). While some countries have relatively advanced pharmacy systems, many others, particularly in parts of sub-Saharan Africa, face similar challenges to those in Ethiopia, where the healthcare system struggles with limited resources, inadequate staffing, and infrastructure issues (88). However, the impact of these barriers on CPPs’ ability to provide optimal care for patients with chronic diseases can be mitigated through innovative service delivery models and the use of technology (89, 90).
The review identified healthcare system-related barriers such as a lack of follow-up and service monitoring from regulatory bodies, a lack of standardized and customized guidelines and frameworks, a lack of financial and remuneration frameworks for supporting service providers, and a lack of integration frameworks of pharmacies into the healthcare system. These challenges are prevalent in many low- and middle-income countries, including those in Africa (51, 86). Globally, healthcare systems vary widely in terms of their organization, financing, and delivery (91). A communication and collaboration framework between CPPs and other healthcare providers should be instrumental in facilitating the integration of CPPs into chronic disease management teams (92). In addition, CPPs engaging in clinical practice in Ethiopia often receive inadequate remuneration, which can lead to recruitment and retention challenges (93). Furthermore, their professional contributions may not be fully recognized or valued within the healthcare system. The policy and regulatory framework governing community pharmacy practice in Ethiopia may not fully support their involvement in chronic disease management. Clear guidelines and protocols are needed to define their role, responsibilities, and scope of practice.
Patient and/or public-related barriers, such as limited awareness of the services provided by CPPs and lack of demand from patients/clients to receive these services, have been identified in the review. These challenges are common across different populations and cultural contexts. Public-related barriers, such as negative attitudes toward chronic diseases and a lack of awareness of the role of CPPs, may also have been highlighted (94). Addressing these barriers requires comprehensive public health campaigns and educational initiatives to raise awareness of the benefits of CPPs’ services and to promote positive attitudes toward chronic disease management.
In general, beyond the barriers discussed in this review, patients with NCDs have multiple healthcare needs and multiple medications, usually because of comorbidities and complications. Access to healthcare services, including the availability of physicians, consistent supply of essential medicines and affordability, and broader socioeconomic factors, can significantly influence the prevention and management of NCDs in Ethiopia, as well as in other resource-limited countries across Africa (95). These systemic and structural challenges may lead patients to seek alternative sources of care other than primary healthcare levels, such as community pharmacies. To leverage the accessibility of community pharmacies in managing NCDs in Ethiopia and similar settings, a strategic approach is needed. This includes formally integrating pharmacies into the primary healthcare system and expanding pharmacists’ roles to include counselling, screening, and referrals. Training and clear clinical guidelines should support this shift. Ensuring consistent access to affordable medicines through strengthened supply chains is essential. Digital linkages with primary healthcare facilities can improve care coordination, while pharmacies can also serve as key platforms for raising health awareness and promoting treatment adherence.
Strengths and limitations of this study
This study is the first of its kind and presents comprehensive findings regarding CPPs’ roles and barriers in preventing and managing NCDs in Ethiopia. These findings can be used to enhance the practice of CPPs and as an instrument to update policies and frameworks to incorporate CPPs as potential stakeholders in addressing the burden of NCDs. However, this review has some limitations that should be considered when interpreting the findings. The included studies were not evenly distributed across the country’s regions, with a particular concentration in the Amhara region and Addis Ababa, primarily focusing on urban settings. Additionally, the included studies addressed the role of CPPs in limited types of NCDs, which may limit the generalizability of the findings. Furthermore, the review did not differentiate between pharmacists and diploma-level pharmacy technicians in the analysis, although their roles and training differ significantly. This lack of distinction may affect the interpretation of both roles and barriers when compared to similar studies that focused exclusively on pharmacists. Finally, this review could not address the level and proportion of CPPs’ involvement in each scope of practice, and the magnitude of the barriers CPPs face.
Implication of findings
Implications for policymakers: This review can inform the development of evidence-based guidelines and policies that empower CPPs to effectively contribute to NCD prevention and management in the Ethiopian context. Recognizing the potential of CPPs in NCD care, policymakers should develop policies and strategies to:
• Integrate CPPs into the broader healthcare system.
• Strengthening the role of CPPs by allocating adequate resources and investing in infrastructure.
• Develop and implement comprehensive training programs to enhance CPPs’ knowledge and skills in NCD prevention, screening, and management.
• Establish and implement appropriate reimbursement mechanisms for CPP-provided NCD services.
• Foster collaboration between CPPs, physicians, and other healthcare providers.
Implications for CPPs: CPPs should actively engage in continuing education to enhance their knowledge and skills in NCD management. They should also advocate for policies that support their expanded role in NCD care. Building strong collaboration with other healthcare providers can improve patient outcomes and enhance CPP’s role. CPPs can also explore innovative service delivery models to address the challenges of NCD care in resource-limited settings, such as telepharmacy or point-of-care testing.
Implications for research: Further research is needed to identify effective interventions to address CPPs’ barriers in Ethiopia’s NCD care. Studies should evaluate the impact of CPP-led NCD care programs on patient outcomes, healthcare costs, and patient satisfaction. Exploring patient perspectives on CPP-provided NCD services would be important to inform service improvement and ensure these services align with patient needs.
Recommendations to tackle potential barriers
To address barriers hindering CPPs in NCD prevention and management in Ethiopia, targeted interventions are needed.
CPPs-related barriers can be mitigated through structured continuous professional development programs, on-the-job training, and access to updated guidelines and digital health tools. Strengthening interprofessional collaboration and expanding access to electronic medical records will enhance service delivery.
Pharmacy setting barriers require investment in private counseling areas, workforce expansion, and regulatory enforcement of standardized guidelines. Strengthening managerial support and fostering collaboration with healthcare institutions will improve working conditions and service integration.
Policy and healthcare system barriers can be addressed by enhancing regulatory oversight, routine follow-ups, and sustainable financing models, including reimbursement schemes. Standardized, Ethiopia-specific guidelines should be developed to ensure clarity in CPPs’ roles.
Patient and public-related barriers require awareness campaigns through media and community engagement to highlight CPPs’ contributions to NCD care. Integrating CPPs into primary healthcare teams can enhance public trust and service demand.
By implementing these targeted strategies, Ethiopia can optimize the role of CPPs in reducing the NCD burden and improving public health.
Conclusion
The findings from this review highlight the significant potential of CPPs in supporting the prevention and management of NCDs in resource-limited settings such as Ethiopia. However, as most of the current studies are from the Amhara region and Addis Ababa, the findings may not reflect pharmacy practices in other Ethiopian regions and remote areas. Although CPPs are already engaged in NCD prevention, screening, and management, there remains considerable room for improvement in terms of service consistency, accessibility, and integration within the broader healthcare system. By addressing these challenges and drawing lessons from the experiences of other African countries and global best practices, Ethiopia can enhance the role of CPPs in NCD care. Key strategies include investing in CPP training, ensuring the provision of adequate resources, and developing clear guidelines and protocols for delivering NCD-related services.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. EB: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing, Software, Visualization. LL: Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – review & editing, Software, Validation. GC: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. AD: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. YT: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. KG: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. FT: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. BA: Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – review & editing. GB: Writing – review & editing, Methodology, Formal analysis, Validation, Visualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer SW declared a shared affiliation with the author FT to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1485327/full#supplementary-material
Abbreviations
CPP, Community pharmacy professional; CDRO, Community drug retail outlets; JBI, Joanna Briggs Institute; NCD, noncommunicable disease; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SP, simulated patient; WHO, World Health Organization.
References
1. World Health Organization. Home/health topics/noncommunicable diseases. Available online at: https://www.who.int/health-topics/noncommunicable-diseases (Accessed: 25 February 2024).
2. Ministry of Health of the Federal Democratic Republic of Ethiopia and AICS Addis Abeba (2020). Unite stakeholders against NCDs. The double burden of diseases and challenges on service provision and integration in Ethiopia: Evidence generated from different experiences. Available at: https://addisabeba.aics.gov.it/news/il-ministero-della-salute-etiopico-e-aics-addis-abeba-si-fanno-promotori-della-lotta-alle-malattie-non-trasmissibili/?lang=en
3. EPHI-FMoH-WHO (2016) STEPS survey on risk factors for non-communicable diseases and prevalence of selected NCDs in Ethiopia. Summary report. Available at: https://www.issup.net/files/2021-05/Ethiopia%20--%20STEPS%20Report%20on%20Risk%20Factors%20of%20NCDs.pdf
4. Federal Ministry of Health (FMoH). (2019–2025). National Strategic Action Plan (NSAP) for prevention and control of major non-communicable diseases in Ethiopia 2018–2025. Available at: https://extranet.who.int/ncdccs/Data/ETH_B3_NSAP%20for%20Prevention%20and%20Control%20of%20Major%20NCDs%20_2018-2025_Version%20April%2011,2019.pdf
5. World Health Organization Ethiopia. (2018). Health workforce—The health system. Available online at: http://www.aho.afro.who.int/profiles_information/index.php/Ethiopia:Health_workforce_-_The_Health_System (Accessed May 29, 2019).
6. Fenta, ET, Ayal, BG, Kidie, AA, Anagaw, TF, Mekonnen, TS, Ketema Bogale, E, et al. Barriers to medication adherence among patients with non-communicable disease in north Wollo zone public hospitals: socio-ecologic perspective, 2023. Patient Prefer Adherence. (2024) 18:733–44. doi: 10.2147/PPA.S452196
7. Defar, A, Zeleke, GT, Berhanu, D, Lemango, ET, Bekele, A, Alemu, K, et al. Health system's availability and readiness of health facilities for chronic non-communicable diseases: evidence from the Ethiopian national surveys. PLoS One. (2024) 19:e0297622. doi: 10.1371/journal.pone.0297622
8. Abate, TW, Genanew, A, Gedamu, H, Tegenaw, A, Ayalew, E, Berhie, AY, et al. Unmasking the silent epidemic: a comprehensive systematic review and meta-analysis of undiagnosed diabetes in Ethiopian adults. Front Endocrinol (Lausanne). (2024) 15:1372046. doi: 10.3389/fendo.2024.1372046
9. Solbana, LK, Chaka, EE, and Tola, DE. Undiagnosed hypertension and its associated factors in Ethiopia: a systematic review and meta-analysis. Health Sci Rep. (2023) 6:e1696. doi: 10.1002/hsr2.1696
10. Yitbarek, GY, Ayehu, GW, Asnakew, S, Chanie, ES, Bayih, WA, Feleke, DG, et al. Undiagnosed diabetes mellitus and associated factors among adults in Ethiopia: a systematic review and meta-analysis. Sci Rep. (2021) 11:24231. doi: 10.1038/s41598-021-03669-y
11. Sousa Pinto, G, Bader, L, Billberg, K, Criddle, D, Duggan, C, El Bizri, L, et al. Beating non-communicable diseases in primary health care: the contribution of pharmacists and guidance from FIP to support WHO goals. Res Soc Adm Pharm. (2020) 16:974–7. doi: 10.1016/j.sapharm.2019.10.008
12. Fentie, AM, Huluka, SA, Gebremariam, GT, Gebretekle, GB, Abebe, E, and Fenta, TG. Impact of pharmacist-led interventions on medication-related problems among patients treated for cancer: a systematic review and meta-analysis of randomized control trials. Res Soc Adm Pharm. (2024) 20:487–97. doi: 10.1016/j.sapharm.2024.02.006
13. Tsige, AW, Kotiso, TA, Ayenew, KD, and Ayele, SG. Pharmacist intervention to improve adherence to medication among heart failure patients at north East Ethiopia hospital. Pharmacol Res Perspect. (2024) 12:e1199. doi: 10.1002/prp2.1199
14. Billoro, BB, Abdi, AM, Abero, WA, Fite, AB, and Basgut, B. A preliminary study to evaluate the impact of pharmaceutical care services on clinical outcome and medication adherence in type 2 diabetes mellitus patients from Ethiopian perspective. Afr Health Sci. (2022) 22:104–18. doi: 10.4314/ahs.v22i4.14
15. Amorha, KC, Okonta, MJ, and Ukwe, CV. Impact of pharmacist-led educational interventions on asthma control and adherence: single-blind, randomised clinical trial. Int J Clin Pharm. (2021) 43:689–97. doi: 10.1007/s11096-020-01187-x
16. Rampamba, EM, Meyer, JC, Helberg, EA, and Godman, B. Empowering hypertensive patients in South Africa to improve their disease management: a pharmacist-led intervention. J Res Pharm Pract. (2019) 8:208–13. doi: 10.4103/jrpp.JRPP_18_74
17. Nelissen, HE, Cremers, AL, Okwor, TJ, Kool, S, van Leth, F, Brewster, L, et al. Pharmacy-based hypertension care employing mHealth in Lagos, Nigeria - a mixed methods feasibility study. BMC Health Serv Res. (2018) 18:934. doi: 10.1186/s12913-018-3740-3
18. Omboni, S, and Caserini, M. Effectiveness of pharmacist’s intervention in the management of cardiovascular diseases. Open Heart. (2018) 5:e000687. doi: 10.1136/openhrt-2017-000687
19. Santschi, V, Chiolero, A, Paradis, G, Colosimo, AL, and Burnand, B. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. (2012) 35:2706–17. doi: 10.2337/dc12-0369
20. Tsuyuki, RT, Beahm, NP, Okada, H, and Al Hamarneh, YN. Pharmacists as accessible primary health care providers: review of the evidence. Can Pharm J (Ott). (2018) 151:4–5. doi: 10.1177/1715163517745517
21. Wu, M, Xu, X, Zhao, R, Bai, X, Zhu, B, and Zhao, Z. Effect of pharmacist-led interventions on medication adherence and glycemic control in type 2 diabetic patients: a study from the Chinese population. Patient Prefer Adherence. (2023) 17:119–29. doi: 10.2147/PPA.S394201
22. Sendekie, AK, and Netere, AK. Multicenter cross-sectional study on perceptions and roles of community pharmacists in the prevention and Management of Cardiovascular Disorders in Northwest Ethiopia. Integr Pharm Res Pract. (2022) 11:21–31. doi: 10.2147/IPRP.S348260
23. Amadi, C, Lawal, F, Ajiboye, W, Agbim, R, Mbakwem, A, Ajuluchukwu, J, et al. Opportunistic screening of cardiovascular disease risk factors in community pharmacies in Nigeria: a cross-sectional study. Int J Clin Pharm. (2020) 42:1469–79. doi: 10.1007/s11096-020-01112-2
24. Amadi, CE, Lawal, FO, Mbakwem, AC, Ajuluchukwu, JN, and Oke, DA. Knowledge of cardiovascular disease risk factors and practice of primary prevention of cardiovascular disease by community pharmacists in Nigeria: a cross-sectional study. Int J Clin Pharm. (2018) 40:1587–95. doi: 10.1007/s11096-018-0744-3
25. Marfo, AF, and Owusu-Daaku, FT. Evaluation of a pharmacist-led hypertension preventative and detection service in the Ghanaian community pharmacy: an exploratory study. Int J Pharm Pract. (2016) 24:341–8. doi: 10.1111/ijpp.12263
26. Katoue, MG, Awad, AI, and Kombian, SB. Role of community pharmacists in the prevention and management of the metabolic syndrome in Kuwait. Int J Clin Pharm. (2013) 35:57–64. doi: 10.1007/s11096-012-9705-4
27. McLean, DL, McAlister, FA, Johnson, JA, King, KM, Makowsky, MJ, and Jones, CA. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN). Arch Intern Med. (2008) 168:2355–61. doi: 10.1001/archinte.168.21.2355
28. Deters, MA, Laven, A, Castejon, A, Doucette, WR, Ev, LS, Krass, I, et al. Effective interventions for diabetes patients by community pharmacists: a Meta-analysis of pharmaceutical care components. Ann Pharmacother. (2018) 52:198–211. doi: 10.1177/1060028017733272
29. Melton, BL, and Lai, Z. Review of community pharmacy services: what is being performed, and where are the opportunities for improvement? Integr Pharm Res Pract. (2017) 6:79–89. doi: 10.2147/IPRP.S107612
30. Ministry of Health Ethiopia (MoHE). National strategic plan for the prevention and control of major non-communicable diseases. 2013–2017 EFY (2020/21–2024/25). Available at: https://www.iccp-portal.org/sites/default/files/plans/ETH_B3_s21_National_Strategic_Plan_for_Prevention_and_Control_of_NCDs2021.pdf (Accessed June 17, 2025).
31. Sendekie, AK, Tesfaye, AH, Tadesse, YB, Dagnaw, AD, and Belachew, EA. Actual practices of community pharmacists in the management of diabetes: a comparison of simulated patient-based study with perceived role of involvement. J Pharm Policy Pract. (2024) 17:2326381. doi: 10.1080/20523211.2024.2326381
32. Sendekie, AK, Tadesse, YB, Kasahun, AE, and Belachew, EA. Determine the perceived level of involvement and factors affecting diabetes management by community pharmacy professionals at drug retails in northwestern Amhara region, Ethiopia. Heliyon. (2023) 9:e20091. doi: 10.1016/j.heliyon.2023.e20091
33. Sendekie, AK, Dagnaw, AD, and Dagnew, EM. Pharmacists' involvements and barriers in the provision of health promotion services towards noncommunicable diseases: community-based cross-sectional study in Northwest Ethiopia. Arch Public Health. (2023) 81:31. doi: 10.1186/s13690-023-01038-x
34. Belachew, SA, Muluneh, NY, Erku, DA, and Netere, AK. A cross sectional study on beliefs and roles of community pharmacy professionals in preventing and managing metabolic syndrome in an Ethiopian setting. PLoS One. (2020) 15:e0244211. doi: 10.1371/journal.pone.0244211
35. Tesfaye, ZT, and Yismaw, MB. Community's extent of use and approval of extended pharmacy services in community pharmacies in Southwest Ethiopia. PLoS One. (2020) 15:e0230863. doi: 10.1371/journal.pone.0230863
36. Teni, FS, Birru, EM, Surur, AS, Belay, A, Wondimsigegn, D, Gelayee, DA, et al. Pattern and predictors of medicine use among households in Gondar town, northwestern Ethiopia: a community-based medicine utilization study. BMC Res Notes. (2017) 10:357. doi: 10.1186/s13104-017-2669-7
37. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
38. World Health Organization Home/newsroom/factsheets/detail/noncommunicable diseases. Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (Accessed: 25 February 2024).
39. Moola, S, Munn, Z, Tufanaru, C, Aromataris, E, Sears, K, Sfetcu, R, et al. Systematic reviews of etiology and risk In: E Aromataris and Z Munn, editors. JBI manual for evidence synthesis : JBI (2020). Available: https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-08
40. Moges, H. (2019). Assessment of health promotion services in community pharmacies of Addis Ababa, Ethiopia: Unpublished master’s thesis. Addis Ababa University, School of Pharmacy. Available: https://etd.aau.edu.et/items/beeb8ee4-3883-40bb-a69f-7555dfa70a18
41. Belachew, EA, Shibe, BS, Tefera, AM, and Wondm, SA. Community pharmacy professionals' knowledge, attitude, and practice toward nutrition and lifestyle counseling in Gondar City, Ethiopia. SAGE Open Med. (2024) 12:20503121241256569. doi: 10.1177/20503121241256569
42. Sendekie, AK, Ergena, AE, Belachew, EA, Kasahun, AE, Teklie, MT, and Netere, AK. Extent of cardiovascular medications dispensing practice without a prescription: self-reported and simulated patient-based study at community pharmacies in Northwest Ethiopia. J Pharm Policy Pract. (2023) 16:28. doi: 10.1186/s40545-023-00533-4
43. Birarra, MK, Baye, E, Tesfa, W, and Kifle, ZD. Knowledge of cardiovascular disease risk factors, practice, and barriers of community pharmacists on cardiovascular disease prevention in Northwest Ethiopia. Metab Open. (2022) 16:100219. doi: 10.1016/j.metop.2022.100219
44. Asmelashe Gelayee, D, Binega Mekonnen, G, and Asrade Atnafe, S. Practice and Barriers towards Provision of Health Promotion Services among Community Pharmacists in Gondar, Northwest Ethiopia. Biomed Res Int. (2017) 2017:7873951. doi: 10.1155/2017/7873951
45. Emiru, YK, Hammeso, WW, Adelo, ES, Siraj, EA, Bizuneh, GK, Adamu, BA, et al. Role of community pharmacists in educating asthmatic patients: a multi-centered cross-sectional study in Ethiopia. Chron Respir Dis. (2020) 17:1479973120952679. doi: 10.1177/1479973120952679
46. Erku, DA, Belachew, SA, Mekuria, AB, Haile, KT, Gebresillassie, BM, Tegegn, HG, et al. The role of community pharmacists in patient counseling and health education: a survey of their knowledge and level of involvement in relation to type 2 diabetes mellitus. Integr Pharm Res Pract. (2017) 6:137–43. doi: 10.2147/IPRP.S140777
47. Erku, DA, and Mersha, AG. Involvement of community pharmacists in public health priorities: a multi-center descriptive survey in Ethiopia. PLoS One. (2017) 12:e0180943. doi: 10.1371/journal.pone.0180943
48. Teka, NT, and Baye, AM. Counseling practice of community pharmacists for diabetes mellitus patients in Addis Ababa, Ethiopia. BMC Res Notes. (2018) 11:700. doi: 10.1186/s13104-018-3807-6
49. Ayenew, W, Seid, AM, Kasahun, AE, Ergena, AE, Geremaw, DT, Limenh, LW, et al. Assessment of community pharmacy professionals' willingness, involvement, beliefs, and barriers to offer health promotion services: a cross-sectional study. BMC Health Serv Res. (2022) 22:1539. doi: 10.1186/s12913-022-08944-w
50. Gebresillassie, BM, Howells, K, and Ashiru-Oredope, D. Public health interventions delivered by pharmacy professionals in low- and middle-income countries in Africa: a systematic scoping review. Pharmacy (Basel). (2023) 11:24. doi: 10.3390/pharmacy11010024
51. Okoro, RN, and Nduaguba, SO. Community pharmacists on the frontline in the chronic disease management: the need for primary healthcare policy reforms in low and middle income countries. Explor Res Clin Soc Pharm. (2021) 2:100011. doi: 10.1016/j.rcsop.2021.100011
52. Gentilini, A, Kasonde, L, and Babar, ZU. Expanding access to NCD services via community retail pharmacies in LMICs: a systematic review of the literature. J Pharm Policy Pract. (2025) 18:2462450. doi: 10.1080/20523211.2025.2462450
53. Sabater-Hernández, D, Sabater-Galindo, M, Fernandez-Llimos, F, Rotta, I, Hossain, LN, Durks, D, et al. A systematic review of evidence-based community pharmacy services aimed at the prevention of cardiovascular disease. J Manag Care Spec Pharm. (2016) 22:699–713. doi: 10.18553/jmcp.2016.22.6.699
54. Khanal, S, Nissen, L, Veerman, L, and Hollingworth, S. Pharmacy workforce to prevent and manage non-communicable diseases in developing nations: the case of Nepal. Res Soc Adm Pharm. (2016) 12:655–9. doi: 10.1016/j.sapharm.2015.09.005
55. Motlohi, NF, Mensah, KB, Padayachee, N, Petrus, R, and Bangalee, V. The role of Lesotho community pharmacists in preventing and controlling cardiovascular diseases: the perceived facilitators and barriers. PLoS One. (2024) 19:e0301525. doi: 10.1371/journal.pone.0301525
56. Marfo, AFA, and Owusu-Daaku, FT. Exploring the extended role of the community pharmacist in improving blood pressure control among hypertensive patients in a developing setting. J Pharm Policy Pract. (2017) 10:39. doi: 10.1186/s40545-017-0127-5
57. Ihekoronye, MR, and Osemene, KP. Evaluation of the participation of community pharmacists in primary healthcare Services in Nigeria: a mixed-method survey. Int J Health Policy Manag. (2022) 11:829–39. doi: 10.34172/ijhpm.2020.224
58. Motlohi, NF, Wiafe, E, Mensah, KB, Padayachee, N, Petrus, R, and Bangalee, V. A systematic review of the role of community pharmacists in the prevention and control of cardiovascular diseases: the perceptions of patients. Syst Rev. (2023) 12:160. doi: 10.1186/s13643-023-02338-7
59. George, PP, Molina, JA, Cheah, J, Chan, SC, and Lim, BP. The evolving role of the community pharmacist in chronic disease management - a literature review. Ann Acad Med Singap. (2010) 39:861–7. doi: 10.47102/annals-acadmedsg.V39N11p861
60. Buss, VH, Shield, A, Kosari, S, and Naunton, M. The impact of clinical services provided by community pharmacies on the Australian healthcare system: a review of the literature. J Pharm Policy Pract. (2018) 11:22. Available at: https://joppp.biomedcentral.com/articles/10.1186/s40545-018-0149-7
61. Dineen-Griffin, S, Benrimoj, SI, and Garcia-Cardenas, V. Primary health care policy and vision for community pharmacy and pharmacists in Australia. Pharm Pract (Granada). (2020) 18:1967. doi: 10.18549/PharmPract.2020.2.1967
62. Al Hamarneh, YN, Marra, C, Gniadecki, R, Keeling, S, Morgan, A, and Tsuyuki, R. RxIALTA: evaluating the effect of a pharmacist-led intervention on CV risk in patients with chronic inflammatory diseases in a community pharmacy setting: a prospective pre-post intervention study. BMJ Open. (2021) 11:e043612. doi: 10.1136/bmjopen-2020-043612
63. Kolodziejak, L, Rémillard, A, and Neubauer, S. Integration of a primary healthcare pharmacist. J Interprof Care. (2010) 24:274–84. doi: 10.3109/13561820903130149
64. Tsuyuki, RT, Houle, SK, Charrois, TL, Kolber, MR, Rosenthal, MM, Lewanczuk, R, et al. Randomized trial of the effect of pharmacist prescribing on improving blood pressure in the community: the Alberta clinical trial in optimizing hypertension (RxACTION). Circulation. (2015) 132:93–100. doi: 10.1161/CIRCULATIONAHA.115.015464
65. Al Assaf, S, Zelko, R, and Hanko, B. The effect of interventions led by community pharmacists in primary Care for Adults with type 2 diabetes mellitus on therapeutic adherence and HbA1c levels: a systematic review. Int J Environ Res Public Health. (2022) 19:6188. doi: 10.3390/ijerph19106188
66. Woodhams, L, Chalmers, L, Hillis, GS, and Sim, TF. Developing community pharmacists' role in the management of type 2 diabetes and related microvascular complications: a nationwide survey in Australia. Peer J. (2023) 11:e14849. doi: 10.7717/peerj.14849
67. Newman, TV, San-Juan-Rodriguez, A, Parekh, N, Swart, ECS, Klein-Fedyshin, M, Shrank, WH, et al. Impact of community pharmacist-led interventions in chronic disease management on clinical, utilization, and economic outcomes: an umbrella review. Res Soc Adm Pharm. (2020) 16:1155–65. doi: 10.1016/j.sapharm.2019.12.016
68. Kumar, S, and Preetha, G. Health promotion: an effective tool for global health. Indian J Community Med. (2012) 37:5–12. doi: 10.4103/0970-0218.94009
69. Nsengimana, A, Biracyaza, E, Hategekimana, JC, Tuyishimire, J, Nyiligira, J, and Rutembesa, E. Attitudes, perceptions, and barriers of community pharmacists in Rwanda towards health promotion: a cross sectional study. Arch Public Health. (2022) 80:157. doi: 10.1186/s13690-022-00912-4
70. Chiazor, EI, Evans, M, van Woerden, H, and Oparah, AC. A systematic review of community pharmacists’ interventions in reducing major risk factors for cardiovascular disease. Value Health Reg Issues. (2015) 7:9–21. doi: 10.1016/j.vhri.2015.03.002
71. Le, LM, Veettil, SK, Donaldson, D, Kategeaw, W, Hutubessy, R, Lambach, P, et al. The impact of pharmacist involvement on immunization uptake and other outcomes: an updated systematic review and meta-analysis. J Am Pharm Assoc. (2003) 62:1499–1513.e16. doi: 10.1016/j.japh.2022.06.008
72. Juma, PA, Mohamed, SF, Matanje Mwagomba, BL, Ndinda, C, Mapa-Tassou, C, Oluwasanu, M, et al. Correction to: non-communicable disease prevention policy process in five African countries. BMC Public Health. (2018) 18:1112. doi: 10.1186/s12889-018-5993-5
73. Nyaaba, GN, Stronks, K, de-Graft Aikins, A, Kengne, AP, and Agyemang, C. Tracing Africa's progress towards implementing the non-communicable diseases global action plan 2013-2020: a synthesis of WHO country profile reports. BMC Public Health. (2017) 17:297. doi: 10.1186/s12889-017-4199-6
74. Michael, D, Kezakubi, D, Juma, A, Todd, J, Reyburn, H, and Renju, J. The feasibility and acceptability of screening for hypertension in private drug retail outlets: a pilot study in Mwanza region, Tanzania. Int Health. (2016) 8:360–6. doi: 10.1093/inthealth/ihw023
75. Almansour, HA, Mekonnen, AB, Aloudah, NM, Alhawassi, TM, Mc Namara, K, Chaar, B, et al. Cardiovascular disease risk screening by pharmacists: a behavior change wheel guided qualitative analysis. Res Soc Adm Pharm. (2020) 16:149–59. doi: 10.1016/j.sapharm.2019.04.009
76. Flor, LS, Wilson, S, Bhatt, P, Bryant, M, Burnett, A, Camarda, JN, et al. Community-based interventions for detection and management of diabetes and hypertension in underserved communities: a mixed-methods evaluation in Brazil, India, South Africa and the USA. BMJ Glob Health. (2020) 5:e001959. doi: 10.1136/bmjgh-2019-001959
77. Lindsey, L, Husband, A, Nazar, H, and Todd, A. Promoting the early detection of cancer: a systematic review of community pharmacy-based education and screening interventions. Cancer Epidemiol. (2015) 39:673–81. doi: 10.1016/j.canep.2015.07.011
78. Havlicek, AJ, and Mansell, H. The community pharmacist's role in cancer screening and prevention. Can Pharm J (Ott). (2016) 149:274–82. doi: 10.1177/1715163516660574
79. Ndefo, UA, Moultry, AM, Davis, PN, and Askew, R. Provision of medication therapy management by pharmacists to patients with type-2 diabetes mellitus in a federally qualified health center. P T. (2017) 42:632–7. Available at: https://pubmed.ncbi.nlm.nih.gov/29018299/
80. Smith, AJ, Scahill, SL, Harrison, J, Carroll, T, and Medlicott, NJ. Service provision in the wake of a new funding model for community pharmacy. BMC Health Serv Res. (2018) 18:307. doi: 10.1186/s12913-018-3120-z
81. Pharmaceutical Society of New Zealand and New Zealand Medical Association. Integrated health care framework for pharmacists and doctors. Available at: https://www.psnz.org.nz/Folder?Action=View%20File&Folder_id=96&File=IntegratedHealthCareFramework_Final.pdf (Accessed: 18 August 2024).
82. Ballaram, S, Perumal-Pillay, V, and Suleman, F. A scoping review of continuing education models and statutory requirements for pharmacists globally. BMC Med Educ. (2024) 24:343. doi: 10.1186/s12909-024-05322-4
83. Dwyer, G, Popoola, A, Seiler, N, Therrien, N, Karacuschansky, A, Fulmer, E, et al. Chronic disease management service opportunities for community pharmacists during the COVID-19 pandemic. Prev Chronic Dis. (2022) 19:E1. doi: 10.5888/pcd19.210280
84. Kovacs, R, and Lagarde, M. Does high workload reduce the quality of healthcare? Evidence from rural Senegal. J Health Econ. (2022) 82:102600. doi: 10.1016/j.jhealeco.2022.102600
85. Karia, A, Norman, R, Robinson, S, Lehnbom, E, Laba, TL, Durakovic, I, et al. Pharmacist's time spent: space for pharmacy-based interventions and consultation tim E (SPICE)-an observational time and motion study. BMJ Open. (2022) 12:e055597. doi: 10.1136/bmjopen-2021-055597
86. Azevedo, MJ. The state of health system (s) in Africa: Challenges and opportunities. Historical Perspect State Health Health Syst Africa. (2017) 2:1–73. doi: 10.1007/978-3-319-32564-4_1
87. Joyce, A, Berbatis, C, and Sunderland, VB. Analysis of primary prevention services for cardiovascular disease in Australia’s community pharmacies. Aust N Z J Public Health. (2007) 31:516–9. doi: 10.1111/j.1753-6405.2007.00135.x
88. King, RC, and Fomundam, HN. Remodeling pharmaceutical care in sub-Saharan Africa (SSA) amidst human resources challenges and the HIV/AIDS pandemic. Int J Health Plann Manag. (2010) 25:30–48. doi: 10.1002/hpm.982
89. Emmons, RP, Harris, IM, Abdalla, M, Afolabi, TM, Barner, AE, Baxter, MV, et al. Impact of remote delivery of clinical pharmacy services on health disparities and access to care. JACCP J Am Coll Clin Pharm. (2021) 4:1492–501. doi: 10.1002/jac5.1535
90. Goode, JV, Owen, J, Page, A, and Gatewood, S. Community-based pharmacy practice innovation and the role of the community-based pharmacist practitioner in the United States. Pharmacy. (2019) 7:106. doi: 10.3390/pharmacy7030106
91. Kruk, ME, Gage, AD, Arsenault, C, Jordan, K, Leslie, HH, Roder-DeWan, S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. (2018) 6:e1196–252. doi: 10.1016/S2214-109X(18)30386-3
92. Hall, NJ, Donovan, G, and Wilkes, S. A qualitative synthesis of pharmacist, other health professional and lay perspectives on the role of community pharmacy in facilitating care for people with long-term conditions. Res Soc Adm Pharm. (2018) 14:1043–57. doi: 10.1016/j.sapharm.2018.01.002
93. Bilal, AI, Tilahun, Z, Gebretekle, GB, Ayalneh, B, Hailemeskel, B, and Engidawork, E. Current status, challenges and the way forward for clinical pharmacy service in Ethiopian public hospitals. BMC Health Serv Res. (2017) 17:359. doi: 10.1186/s12913-017-2305-1
94. Eades, CE, Ferguson, JS, and O'Carroll, RE. Public health in community pharmacy: a systematic review of pharmacist and consumer views. BMC Public Health. (2011) 11:582. doi: 10.1186/1471-2458-11-582
Keywords: community pharmacy professionals, community pharmacy, roles, barriers, noncommunicable diseases, Ethiopia
Citation: Sendekie AK, Belachew EA, Limenh LW, Chanie GS, Bizuneh GK, Dagnaw AD, Tadesse YB, Gete KY, Tamene FB and Abate BB (2025) Roles and barriers of community pharmacy professionals in the prevention and management of noncommunicable diseases in Ethiopia: a systematic review. Front. Public Health. 13:1485327. doi: 10.3389/fpubh.2025.1485327
Edited by:
Fernanda Jannuzzi, Independent Researcher, Crown Point, United StatesReviewed by:
Brian Godman, Sefako Makgatho Health Sciences University, South AfricaSatabdi Mitra, KPC Medical College and Hospital, India
Samuel Agegnew Wondm, Debre Markos University, Ethiopia
Copyright © 2025 Sendekie, Belachew, Limenh, Chanie, Bizuneh, Dagnaw, Tadesse, Gete, Tamene and Abate. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashenafi Kibret Sendekie, YXNodWtpYjAyQHlhaG9vLmNvbQ==; QXNoZW5hZmkua2licmV0QHVvZy5lZHUuZXQ=
 Ashenafi Kibret Sendekie
Ashenafi Kibret Sendekie Eyayaw Ashete Belachew
Eyayaw Ashete Belachew Liknaw Workie Limenh
Liknaw Workie Limenh Gashaw Sisay Chanie
Gashaw Sisay Chanie Gizachew Kassahun Bizuneh4
Gizachew Kassahun Bizuneh4 Abera Dessie Dagnaw
Abera Dessie Dagnaw Yabibal Berie Tadesse
Yabibal Berie Tadesse Kalab Yigermal Gete
Kalab Yigermal Gete Fasil Bayafers Tamene
Fasil Bayafers Tamene Biruk Beletew Abate
Biruk Beletew Abate
