- 1College of Nursing, Medical University of South Carolina, Charleston, SC, United States
- 2Department of Family Medicine, Medical University of South Carolina, Charleston, SC, United States
Unhoused individuals experience numerous barriers to healthcare access and higher morbidity and mortality rates than housed individuals. In collaboration with community-based organizations (CBOs) and healthcare profession learners we developed a program involving in-person and telehealth visits at a CBO clinic and via street medicine outreach to address healthcare needs of the unhoused in a small Southeastern city. In its fifth year of operation, from January through April 2024, we evaluated the program using key stakeholder interviews (patients, CBO staff learners) guided by the Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) framework. A template analysis approach was utilized to evaluate barriers and facilitators to implementation outcomes. Results demonstrated consistent themes across stakeholders. Factors central to reach included advertisement by word-of-mouth, location convenience, and perceived service benefits. For learners, barriers to reach included clinic hours conflicting with academic schedules and apprehension of providing medical care in this setting. Regarding effectiveness, facilitating themes included opportunities for autonomy and enhanced understanding of treatment of underserved populations (learners) and improvement in health (patients, CBO staff). There were no consistently identified unintended negative consequences of the program. For adoption, all stakeholders described strong perceptions of trust in providers and the importance of team communication and coordination of care, in addition to the need to add disciplines included in the multidisciplinary care team. Facilitating implementation themes included comprehensive access for existing patients, while barriers identified were adequacy of access to social resources (housing, food, transportation) and continued increase in numbers of unhoused individuals outpacing available services. Themes facilitating maintenance included continued outreach efforts and integration into existing healthcare and community-based systems. The addition of additional services and specialties was consistently identified as essential to health status of the patients and an opportunity for growth of the program. This implementation evaluation involving key stakeholders of a community engaged telehealth-based intervention for the unhoused provides thematic considerations to guide program implementation and sustainability to improve health equity for vulnerable populations.
1 Introduction
The Institute of Global Homelessness defines homelessness as people without accommodation (sleeping in open or roofed spaced not meant for human habitation), those living in temporary or crisis accommodation (shelters, camps), and those living in severely inadequate and insecure accommodation (temporary sharing with others, overcrowding) (1). Approximately 1.6 billion people worldwide lack adequate housing (2). Unhoused individuals are at significantly higher risk of numerous, complex health problems leading to higher morbidity and mortality than housed individuals. Due to the living conditions of the unhoused, whether living on the street or in a shelter, this population is prone to encounter multiple health risks and negative health outcomes including but not limited to exposure to communicable diseases, poor nutrition, as well as psychological stressors (3). Increased morbidity and mortality are multifactorial but includes higher incidence of chronic medical conditions including cancer and heart disease as well as substance use disorder (4). The unhoused also have high-cost healthcare utilization patterns including lower ambulatory care use and higher emergency department use and hospitalization (5). There are various barriers that contribute to the complexities of providing healthcare to unhoused populations. Common healthcare barriers affecting health care access for the unhoused include unaffordable cost of care, being uninsured, and little to no transportation to obtain health services (3). In order to address the barriers to healthcare access for those who experience homelessness, it is imperative to present accessible health care services that target the needs of this population in order to reduce morbidity and mortality rates (6). Thus, innovative methods of care delivery are key to reaching this population. Utilizing telehealth has been proven as an important factor to help connect vulnerable populations to health care and eliminate barriers for those who are unable to obtain appropriate health care (7, 8). Programs which deliver telehealth to the unhoused are most successful when there is collaboration between agencies for arrangement of health services to meet patient needs (7, 8). Telehealth as a mode of delivery has proved to be effective in providing healthcare access for Veterans experiencing homelessness, with telehealth tablets being used to overcome health and travel related barriers (7). However, there are limited published implementation evaluations related to telehealth delivery in the unhoused population. The Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) framework is used to evaluate program implementation by assessing program internal and external validity to enhance the sustainability and generalizability of interventions. It is a useful tool for these evaluations as it can guide modifications or replications of effective interventions and is practical for local settings while focusing on the multi- dimensional impact related to population health outcomes. Its components include Reach (program contact with target population), Effectiveness (impact of the program on outcomes), Adoption (willingness of relevant individuals and groups to initiate the program), Implementation (consistency of programmatic elements with the intended program including resource utilization and adaptations), Maintenance (integration of the program into routine practice) (9). The RE-AIM framework has previously been utilized to evaluate telehealth within primary care during the COVID-19 pandemic as well as implementation of telehealth in oncology (10, 11). This framework has also been applied to the use of telehealth in the unhoused population to investigate the effectiveness of various delivery models of primary care to people experiencing homelessness in England (12). The RE-AIM framework has demonstrated efficacy in these evaluation contexts.
2 Context
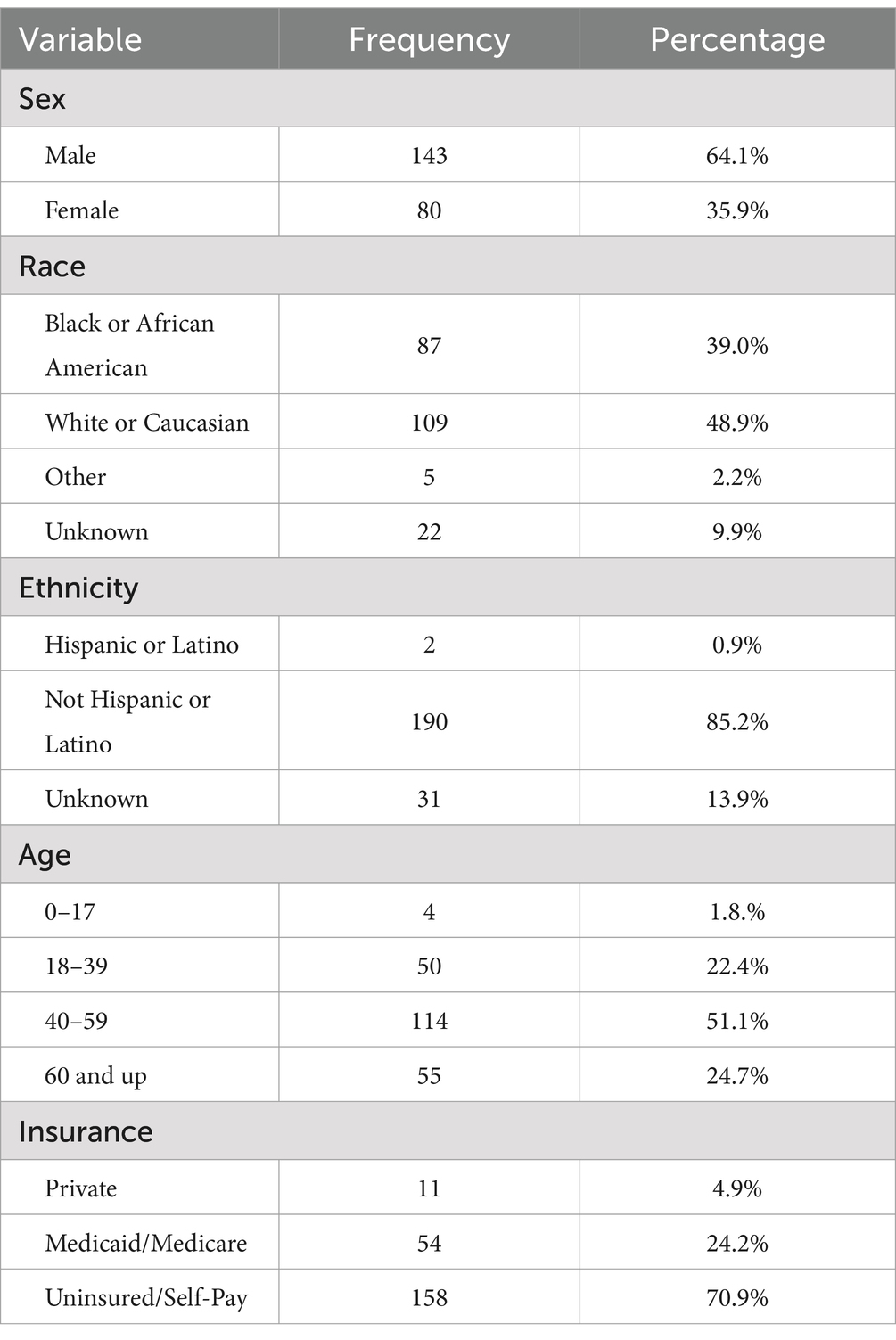
The CARES for the Unhoused program (CFU) serves the unhoused and those with unstable housing in Charleston, South Carolina, a small Southeastern city with limited infrastructure supporting the unhoused community including lack of Medicaid expansion leading to a significant number of uninsured individuals. CFU provides over 500 primary care visits for more than 250 unique patients each year with a demographic makeup (Table 1) that is mostly male (64.1%) and disproportionately African American (39%) compared with the South Carolina population (26%) (13) and predominantly uninsured (70.9%). CFU treats acute and chronic conditions and offers preventive care and specialist referrals as needed. The most common diagnoses treated are musculoskeletal conditions (22%), mental health conditions (21.7%) and cardiovascular conditions (21.3%). The program operates in partnership with two community-based organizations (CBOs) serving the unhoused and their respective staff social workers. Two attending family medicine physicians at the Medical University of South Carolina (MUSC) lead our program and oversee healthcare profession learners that include approximately 20 family medicine and internal medicine resident physicians per year and more than 100 MUSC medical and pharmacy students.
3 Key programmatic elements
Our program consists of three arms: (1) in-person visits at a CBO, (2) video visits at a CBO, and (3) street medicine outreach with CBO staff. For our clinic in-person and video visits we partner with The Navigation Center (TNC) which is a full spectrum drop-in social resource center focused on those experiencing homelessness. TNC provides physical clinical space to conduct visits. For telehealth visits, pre-professional students are in-person at TNC and facilitate visits between patients and remote attending physicians. For street medicine outreach, MUSC physicians and learners partner with TNC, the local homeless shelter (One80 Place), the Department of Mental Health and Emergency Medical Services. In person clinic and street medicine visits are conducted by resident physicians with either in-person oversight or tele-precepting. Tele-precepting is when a remote attending physician supervises healthcare profession learners that are in the same location as the patient, incorporating audio and video interface via cell phone, tablet or computer. The Doxy.me HIPPA compliant platform is used for video visits and tele-precepting on a laptop or tablet for both clinic and street medicine. Over 150 learners participate in the program annually. The program hours are 9 AM-5 PM every Tuesday and Thursday, a schedule developed with input from all stakeholders. Each day of clinical operations consists of a combination of each of the three visit types, with proportions based on the needs identified that day.
Our team completed a qualitative implementation evaluation of the CFU program using the RE-AIM framework measuring Reach, Effectiveness, Adoption, Implementation and Maintenance (9). This study was recognized as Quality Improvement by the MUSC IRB. Key stakeholder interviews were completed from January 2024 to May 2024 with patients (n = 9), CBO staff (n = 3) and learners (n = 7) to gain multidisciplinary perspectives on program moderators. Key stakeholders that were invited to participate were identified for CBO staff based on current staff members working in collaborating CBOs that had interacted with the CFU program. Healthcare profession learners were identified by having volunteered with the program in the past year. Patients were identified by having been seen for a medical visit by the program in the past year. Patient interviews were conducted by medical students that were not part of the healthcare team. Other key stakeholder interviews were conducted by a research coordinator not involved in program implementation. Interviews were completed in patient care sites including at the community organization facilities and street medicine outreach sites as well as virtually and lasted from 5 min to 30 min. All interviews were transcribed verbatim. Two trained coders utilized a template analysis approach (14, 15) in Microsoft Word, with an initial codebook derived from the RE-AIM framework to code the first set of two interviews. Template analysis utilizes a structured (“template”), yet flexible coding process for analysis of qualitative data. Since the interview guides in this study were based on the RE-AIM framework, template analysis allowed researchers to utilize an a priori template, based on the domains of the RE-AIM framework, while also allowing codes to be updated in the coding process. The codebook was updated in a dynamic fashion, allowing additional codes to emerge from the data. After each round of coding, code definitions were refined and coding discrepancies between the coders were discussed to arrive at consensus. After coding was completed, themes were summarized and compared by role (patients, CBO staff, learners).
4 Discussion
An implementation evaluation of the CFU program was conducted using key stakeholder interviews including healthcare profession learners, CBO staff, and patients seen in different care settings to identify barriers and facilitators to reach, effectiveness, adoption, implementation and maintenance, based on the RE-AIM framework (9). Interview themes were similar by role and identified barriers and facilitators to implementation outcomes of the program, based on RE-AIM. See Table 2 for illustrative quotations. Identified program moderators can be utilized to enhance future adaptations of medical programs for underserved, vulnerable populations.
4.1 Reach
4.1.1 Opportunity to improve reach
Optimizing reach, and in this case the number of individuals served by a program, is central to maximizing positive impact. Patients within the CFU program were seen both at TNC and in the unsheltered community locations where they reside. Patients reported initiating participation in the program following hospital admission, being brought to TNC by someone, and having an outreach provider approach them. Patients suggested opportunities to improve reach by recruiting new patients including creating and promoting more awareness of the program via word of mouth, providing handouts, being present at events that provide meals, and visiting additional areas where the target population lives (parks, etc). CBO staff described the importance of encouragement and trust in reaching more patients and treating patients with high levels of respect to establish rapport. The importance of collaborations with other organizations that support this population was also a strategy suggested to reach more patients.
Strategies to enhance reach to recruit more learners (students, residents) included education on the positive learning effects of the program and future clinical career benefits. This increased awareness could be accomplished during orientation activities, and by ongoing informational flyers, email communication from medical university program directors, word of mouth from other residents and students that participate in the program, and communication from an appointed liaison between CFU and the medical university.
4.1.2 Facilitators/barriers to reach
Patients conveyed the need to have an innate desire to receive medical care, as someone that is averse to receiving medical care or adhering to medical recommendations will be difficult to reach. People who use substances and those with communicable diseases were mentioned as subpopulations that may be particularly difficult to reach due to fear of stigma associated with these conditions and concurrent patient reluctancy to receive care. However, it was suggested that building rapport with these patients has proven successful in facilitating trust and ultimately delivering any needed health care. Patients reported a common barrier to expanding treatment reach included lack of transportation to complete diagnostic workups such as labs or imaging, which is challenging since often these specific services cannot be delivered to them in the setting in which they reside.
In discussing willingness to participate in the medical program, students reported a common barrier to participation is their general lack of education and experience with the unhoused community and population, leading to fear of providing care in a potentially dangerous situation. Residents and students also reported that participating in this program was at times challenging with their existing schedules and that incentives to volunteer could be favorable to eliciting more participation.
4.2 Effectiveness
4.2.1 Perceived benefits
Describing positive and negative outcome effects of an intervention, including potential impact on quality of life, is vital to the understanding of comprehensive intervention effectiveness. By defining individual differences in intervention effectiveness, strategies can be created as opportunities to improve intervention efficacy of care.
All patients expressed appreciation for the program overall and specifically for provider reliability and the ease with which they could receive care in the setting where they reside or were already receiving services, with no additional need for travel. Patients noted that the providers really listened to them and were concerned, caring, and understanding and identified these as essential components of care delivery. One patient explained that he knew the provider was trying to help, so he was motivated to do his best to do everything the provider suggested. Benefits of the program that were discussed included support to end a substance addiction, gaining access to needed medications, and improvements in mental and physical health. Patients described the program as “helpful and wonderful” and one patient described the improved quality of life experienced after this program as he stated his “perception of life has changed….”
CBO staff described some of the multi-faceted benefits of the program, most notably offering essential comprehensive health care for unhoused individuals, who have limited access to care. The care can be obtained quickly and is flexible since it is provided in the setting where individuals reside or at a CBO where they are already seeking social services. The program was described as providing a source of comfort to this population, which they do not often experience from their lifestyle. CBO staff also discussed the benefits of the program to learners, as they can gain experience with this medical setting and population.
Similarly, learners stated they were able to learn more about resources for the underserved and unhoused communities through participation in this program, allowing them to feel more “well rounded” in their career training. They described their role in the program as “rewarding and fulfilling” as it provided tangible reminders and motivation of their desire to help others and enforced the reasons they chose a career in the health care field. Learners enjoyed seeing the direct impact their participation had, as they were able to provide health care to those that may not otherwise have had access to medical services. They also appreciated the welcoming and enthusiastic response they received from unhoused patients with whom they engaged. For learners, providing care to this population demonstrated gaps in health care services and encouraged one resident to commit to continue to consider these gaps and implications for health care policy in the future.
4.2.2 Unintended consequences
It is important to identify negative or unintended consequences of interventions to help devise strategies to overcome these negative effects and maximize intervention adoption and sustainability.
One patient disclosed that they felt some personal negativity related to the program initially, likely due to negative discussions with others. However, this patient reported their negativity quickly dissolved and was unwarranted as they learned the providers intent was to deliver beneficial medical care. All of the other patients reported no unintended consequences or negative effects from the program, while some additionally emphasized the positive and helpful aspects of the program.
One resident and one student both described safety concerns related to the setting of this program, although both agreed the medical university had recently addressed this by starting initial triage for setting safety with outreach workers familiar with specific unhoused community camps. The medical university program sponsors also emphasize the optional nature of visiting specific sites based on individual comfort level of learners. Similarly, one CBO staff member described the occasional “rough” setting in which care is provided on the street to this population. Yet, all stakeholders emphasized gratitude for the support the program provides to the unhoused population.
4.2.3 Opportunity to improve efficacy of care
Patients only discussed a few opportunities for improving the efficacy of program care, which included more frequent visits with providers and additional program workers to expand program scope.
CBO staff agreed that additional program workers would be beneficial, including a program specific case manager or social worker. While one CBO staff member stated that they have always been able to have the program provide visit patients when requested, it was agreed that to have capacity to treat the increasing patient case load and expanding community locations additional staff will be increasingly needed. Additional clinical private space for exchange of health information was also identified as a potential area of need.
One healthcare professional learner discussed the program could benefit from additional resources (availability of on-site lab testing, affordable medications) to meet the increasing patient case load and complex medical needs. Other learners described the need for additional initial education prior to working with the unhoused population to have a more clear understanding of the unique challenges this population experiences, including basic education on housing infrastructure, medication costs, insurance, and addiction treatment. Efficiency challenges with EMR documentation related to lack of administrative support for the walk-in nature of appointments was also cited by learners. However, they also described the ability to learn processes quickly and gain confidence in their skills in this setting and appreciated the opportunity for autonomy, while having oversight and mentorship by the lead program attending physicians. Learners generally felt that after working a few shifts for this program, they felt more comfortable in the setting. Learners cited increasing interdisciplinary team members involved such as nursing and pharmacy students and mental health providers, would benefit the program and patients.
4.3 Adoption
4.3.1 Patient-provider communication
Communication is central to the patient-provider relationship in the healthcare setting. Patients overwhelmingly reported that the medical team communicated with them in a way they were able to understand. The importance of listening, not rushing, and limiting use of technical terms during medical communication were identified as facilitators to improved communication. One patient specifically identified the importance of the way questions were asked as a factor which could either promote or impair effective communication.
Learners and CBO staff identified the importance of building rapport with patients when providing care and the importance of developing relationships over time, with a focus on individualized interactions based on respect. A student identified the concern for distrust of authority figures in this population and the need to foster relationships to limit the impact of this potential barrier.
4.3.2 Team communication
Interdisciplinary team communication was discussed with learners and CBO staff and included communication practices among health professions students, resident physicians, attending physicians, and CBO staff. Team communication was generally reported as effective and need for open communication was accentuated along with need for flexibility, trust, support and acceptability amongst all team members. The program learning environment was reported as open and inviting, and new learners reported initial benefit from receiving additional information and communication with more experienced team members. Learners reported attending physician supervision was available when needed with both in person and telehealth based precepting modalities. There was a specific theme discussed among learners related to “closed-loop communication,” which included informing members of the care team who were not present for the patient encounter of their responsibilities for patient care follow up. This was reported as effective, yet occasionally redundant leading to increased work load. Strategies to streamline follow up communication to limit burden for team members are important to sustain efficacy.
4.3.3 Trust
Trust was an important theme across multiple axes in the interactions between key stakeholders. Patients strongly reported trust in the medical recommendations of the care team, however; they also identified the individual motivation needed to seek help as part of the process of accessing care. While patients directly mentioned trusting the recommendations of the program medical director, one patient stated they were still attempting to find trust in the hospital system. Trust among medical team members (students, residents, and attending physicians) was highly reported and the importance of an interdisciplinary team and leveraging of community resources was identified as critical to providing care. Finally, the importance of building and maintaining trust with patients was identified by two CBO staff members as essential to supporting unhoused individuals who may fear being stigmatized and who are often in vulnerable situations.
4.3.4 Coordination of care
Coordination of care was discussed by patients, learners and CBO staff. There was a focus on coordination of program medical care with mental health services and social workers and the need for flexibility with time and location to see patients since patients are potentially treated outside of typical business hours and in their own environment. CBOs directly and indirectly working with the CFU program as well as hospital systems were mentioned as integral to facilitate this coordinated care as was the closed loop communication described above.
4.4 Implementation
4.4.1 Access
Factors relevant for access to program care included frequency of encounters and clinic sessions as well as consideration for whether program availability was adequate to meet patient needs. Patients appreciated the consistency of the timing of clinic sessions with regard to available days and times. However, some patients did report potential benefit of increased options for times in clinic or additional time slots and continued expansion of access to resources to support patient needs. Learners noted the clinic has expanded over the course of the year and some learners were surprised by the size of the population served by this program, although also noted needed for additional expansion to meet growing patient demand. CBO staff believed that patients were typically seen within adequate amounts of wait times and reported the clinic walk-in structure without direct appointments had not resulted in prohibitive wait times.
4.4.2 Follow up
Patients reported that they were able to obtain follow up care including medication, lab work, and other services with few limitations. At times, accessing these follow up services required a return visit to TNC. Patient reported barriers for follow up services were transportation and more expensive medications without more affordable alternatives. Learners commented specifically on the limitations of transportation for lab work and medications and also noted that screening recommendations were less likely to be recommended or completed within this program. CBO staff appreciated the opportunity for patients to receive labs and imaging but identified that increased access to a variety of services and available care locations would be beneficial due to transportation barriers. Patients who may not have regular phone access were more likely to have challenges with follow up services. CBO staff commented on efforts of both TNC and MUSC to reduce costs and assist in transportation when possible.
4.5 Maintenance
4.5.1 Factors promoting sustainability
Patients endorsed that they would continue to receive care from the clinic, based on perceptions of consistency, reliability, dependability, and availability of the care provided. From a learner perspective, integration in the curriculum was noted as a facilitator. Others discussed intention for continued participation due to flexible program specific work hours. CBO staff discussed the sustained benefit of the clinic as a flexible option for patient care, outside of emergency care, that offers team-based outreach with flexible locations.
4.5.2 Outreach efforts
All stakeholders identified the potential benefit of additional outreach services including ophthalmology, dental, physical therapy, and mental health including psychiatry. In addition, opportunity for additional onsite or outreach services, including labs, was identified. Additional student services including physical therapy were identified as potential new multidisciplinary team members.
5 Limitations
There are a few constraints for this implementation study. There is the potential for response bias as individuals more likely to continue to receive care may be more likely to volunteer to participate in interviews about the program. Although interviews were not conducted by or in the vicinity of residents or attending physicians and were conducted by student volunteers not actively engaged in the care team at the time of the interview, the interviewers seen alongside the outreach team at times may have impacted perceived roles during interviews and the expressed opinions of patients. Due to the nature of the unhoused population, those that are more difficult to reach were inherently not included in interviews. Finally, the data collection focused on obtaining interviews from a variety of stakeholders limiting the number of individuals interviews within each group which can impact the sample size and representativeness of each group. We believe the consistency of themes across groups supports the themes and conclusions from qualitative interviews.
6 Conclusion
This implementation evaluation of the CFU program described the benefits and moderators of this innovative care model. The program provides convenient comprehensive medical care to the unhoused population using a hybrid model of telehealth and in-person care while concurrently providing needed hands-on educational opportunities for health professional learners. For long term improvement and sustainability of the program, it is necessary to have adequate resources, staffing, and space to meet increasing patient demand as well as added care involving additional areas of specialty to improve the breadth of services. For learners, it will be important to continue to adapt their educational schedules to allow for program participation while also providing initial training and education on the unique aspects of treating this population. Based on the results of this study, recent efforts have centered around increasing point of care lab testing, enhancing access to cancer screening and other preventive health measures for patients, enhancing preparatory materials for learners, and further partnering with community-based organizations to expand staffing and the variety of services offered. To continue to provide the highest level of quality care, it is vital to maintain open communication among all program team members and patients as well as coordination of care with health care and community- based systems. The identified facilitators and barriers can be utilized in the future to modify and adapt program components to expand equitable health care access to a vulnerable population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Medical University of South Carolina’s Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants and where this was not possible verbal consent was obtained. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
EJ: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. SM: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing. CS: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This publication was made possible by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) as part of the National Telehealth Center of Excellence Award (U66RH31458). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the US Government. The Telehealth Center of Excellence aims to fill important knowledge gaps in the national telehealth landscape through ongoing telehealth research, regional and national collaborations, and proactive dissemination of telehealth resources; Main areas of research focus include: (1) the impact of telehealth on federal and local healthcare spending; (2) use of telehealth to support HIV prevention and treatment; (3) use of telehealth to address behavioral health (BH) and substance use disorders (SUD); (4) use of telehealth to support of rural hospitals; and (5) evaluation of direct-to consumer telehealth.
Acknowledgments
The authors would like to acknowledge MUSC’s Center for Telehealth for support of clinical effort for CARES for the Unhoused and MUSC’s College of Medicine and College of Pharmacy for supporting volunteerism with the CARES for the Unhoused program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ruff Institute of Global Homelessness. Defining and Measuring Homelessness. (2019). Available inline at: https://ighomelessness.org/hub/ (Accessed March 17, 2025).
2. United Nations Department of Social and Economic Affairs. Homelessness could happen to anyone. (2020). Available online at: https://www.un.org/en/desa/homelessness-could-happen-anyone (Accessed March 17, 2025).
3. Lee, A. Disparities in health care for the homeless. LLU Institute for Health Policy and Leadership. Loma Linda University Health. (2021). Available online at: https://ihpl.llu.edu/blog/disparities-health-care-homeless.
4. Taylor, SN, and Munson, D. Health care of people experiencing homelessness: part II. NEJM Evid. (2023) 2:EVIDra2300175. doi: 10.1056/EVIDra2300175
5. Kim, MM, Swanson, JW, Swartz, MS, Bradford, DW, Mustillo, SA, and Elbogen, EB. Healthcare barriers among severely mentally ill homeless adults: evidence from the five-site health and risk study. Admin Pol Ment Health. (2007) 34:363–75. doi: 10.1007/s10488-007-0115-1
6. Thorndike, AL, Yetman, HE, Thorndike, AN, Jeffrys, M, and Rowe, M. Unmet health needs and barriers to health care among people experiencing homelessness in San Francisco's mission district: a qualitative study. BMC Public Health. (2022) 22:1071. doi: 10.1186/s12889-022-13499-w
7. Garvin, LA, Hu, J, Slightam, C, McInnes, DK, and Zulman, DM. Use of video telehealth tablets to increase access for veterans experiencing homelessness. J Gen Intern Med. (2021) 36:2274–82. doi: 10.1007/s11606-021-06900-8
8. DeLaCruz-Jiron, EJ, Hahn, LM, Donahue, AL, and Shore, JH. Telemental health for the homeless population: lessons learned when leveraging care. Curr Psychiatry Rep. (2023) 25:1–6. doi: 10.1007/s11920-022-01400-w
9. Holtrop, JS, Estabrooks, PA, Gaglio, B, Harden, SM, Kessler, RS, King, DK, et al. Understanding and applying the RE-AIM framework: clarifications and resources. J Clin Trans Sci. (2021) 5:e126. doi: 10.1017/cts.2021.789
10. Bediako, JE. Using the RE-AIM framework to evaluate telemedicine and compare with clinic-based visits during the COVID-19 pandemic. Wake Forest University School of Medicine. (2022). Available online at: https://school.wakehealth.edu/education-and-training/nursing-programs/doctor-of-nursing-practice-program/projects/using-re-aim-to-evaluate-telemedicine-during-pandemic.
11. Bu, S, Smith, A, Janssen, A, Donnelly, C, Dadich, A, Mackenzie, LJ, et al. Optimising implementation of telehealth in oncology: a systematic review examining barriers and enablers using the RE-AIM planning and evaluation framework. Crit Rev Oncol Hematol. (2022) 180:103869. doi: 10.1016/j.critrevonc.2022.103869
12. Crane, M, Joly, L, Daly, BJ, Gage, H, Manthorpe, J, Cetrano, G, et al. Integration, effectiveness and costs of different models of primary health care provision for people who are homeless: an evaluation study. Health Soc Care Deliv Res. (2023) 11:1–217. doi: 10.3310/WXUW5103
13. U.S. Census Bureau. QuickFacts: South Carolina. (2023). Available online at: https://www.census.gov/quickfacts/fact/table/SC,US/PST040221
14. Brooks, J, McCluskey, S, Turley, E, and King, N. The utility of template analysis in qualitative psychology research. Qual Res Psychol. (2015) 12:202–22. doi: 10.1080/14780887.2014.955224
Keywords: unhoused, homeless, dissemination implementation, telehealth, healthcare access
Citation: Johnson E, Marrison ST, Banks M and Swords Adams C (2025) Evaluating the implementation of a community engaged telehealth based intervention to improve health equity for the unhoused. Front. Public Health. 13:1487842. doi: 10.3389/fpubh.2025.1487842
Edited by:
Tamra Burns Loeb, University of California, Los Angeles, United StatesReviewed by:
Bassey Ebenso, University of Leeds, United KingdomTran Nguyen, Augusta University, United States
Copyright © 2025 Johnson, Marrison, Banks and Swords Adams. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cristin Swords Adams, c3dvcmRzY0BtdXNjLmVkdQ==
 Emily Johnson
Emily Johnson Sarah Tucker Marrison
Sarah Tucker Marrison Mattie Banks
Mattie Banks Cristin Swords Adams
Cristin Swords Adams