- The Department of Nursing, First Affiliated Hospital, Guangxi Medical University, Nanning, Guangxi, China
Background: Mental health issues among the older people are increasingly becoming a focus of societal concern, with depression and anxiety being common psychological problems that affect their quality of life and physical health. However, research on anxiety and depression among ethnic minorities in China remains relatively limited. This study investigates ethnic disparities in mental health among older adults (≥65 years) in China’s Guangxi Zhuang Autonomous Region, employing a Social Determinants of Health (SDH) framework.
Methods: A cross-sectional study was conducted using a multi-stage stratified sampling method among 1,671 older individuals aged 65 and above in five communities in Guangxi from April to May 2024. A total of 1,550 completed questionnaires were collected. Descriptive analysis, univariate analysis, and two-factor logistic regression analysis were employed to explore the influencing factors of depression and anxiety among the older people in ethnic minority areas.
Results: The prevalence rates of anxiety and depression were 11.42 and 15.94%, respectively. Logistic regression analysis indicated that being female, belonging to ethnic minorities (such as Jing, Yao, Mulao, and Zhuang), cognitive impairment, holding negative attitudes towards aging, and poor psychological resilience were common and significant predictors of both anxiety and depression. Support from children and access to medical insurance emerged as common protective factors against anxiety and depression.
Conclusion: The incidence of anxiety and depression symptoms among the older people in the Guangxi Zhuang Autonomous Region is relatively high. Specifically, ethnic minorities such as Jing, Yao, Mulao, and Zhuang exhibited a higher likelihood of experiencing anxiety and depression compared to non-ethnic minorities like Han. This finding highlights the multiple mental health challenges faced by these groups in terms of socioeconomic status, culture, education, and healthcare access. The government should prioritize the mental health of ethnic minorities by optimizing the allocation of social resources and promoting culturally adapted mental health services to address these challenges.
1 Introduction
With globalization, population aging is accelerating at an unprecedented rate, turning healthy aging into a global challenge (1). In China, by 2023, the population aged 65 and above surpassed 217 million, representing 15.4% of the total population, with a dependency ratio of 22.5% (2). This marks China’s entry into a deep aging stage, with a higher-than-average global aging level. This demographic shift poses challenges to socio-economic development but also creates opportunities for public health system construction, particularly in addressing the health and social needs of the older people (3). Mental health issues among the older people, particularly depression and anxiety, which have higher incidence rates compared to other age groups, cannot be ignored (4). The latest China Mental Health Survey shows that the lifetime prevalence of anxiety disorders in China is 7.6%, the highest reported (5). In 2012, depression became the second largest disease burden in China, and globally, it accounted for 10.3% of the total disease burden, ranking first (6). In China, the overall prevalence of depression among the older people is 22.7% (7). These psychological problems not only threaten the physical and mental health of the older people but also increase the risk of disability and suicide, imposing a significant economic burden on individuals and society (8).
China is a unified multi-ethnic nation, with ethnic minorities inhabiting 60% of the country’s territory. Minority regions have a higher ageing rate than the national average. Take the Guangxi Zhuang Autonomous Region as an example. It has the largest population of ethnic minorities in China. The proportion of people aged 65 and above is 13.81% (9), but there is an uneven distribution of mental health resources in these minority regions. For example, the psychiatric resources in the western regions are only 1/7 to 1/11 of those in the eastern regions (10). Data from the 2021 China Mental Health Survey shows that the 12-month treatment rate for depressive disorders was only 9.5%, with less than 0.5% receiving adequate treatment (11). Such structural inequality may lead to a higher rate of untreated mental illnesses among older people ethnic minorities. In addition, older people from ethnic minority groups face significant barriers in accessing mental health services due to language differences, cultural practices, and social exclusion (12). Minority regions also face socioeconomic and status segregation. Studies show that in border minority areas, older people often have low education and income levels. Combined with poor transportation, these factors lead to poor accessibility to health services, reflecting health inequities that disproportionately affect the poor and less educated (13).
The health status of ethnic minority groups is pivotal not only to their individual health and quality of life but also to the preservation of amicable ethnic relations and the stability of the nation. However, among individuals from historically marginalized ethnic groups, depression and anxiety are often underreported and undertreated, with these conditions frequently presenting with greater severity. Although prevalence rates of anxiety and depression appear relatively similar across different ethnic groups, extant research suggests that individuals from minoritized racial and ethnic backgrounds tend to experience more persistent mental illness and have lower rates of treatment utilization (14). In addition, there is a paucity of research on the mental health of ethnic minorities within China, particularly in underdeveloped regions such as Guangxi, where mental health services remain comparatively underdeveloped relative to more socioeconomically advanced provinces. Against this backdrop, this study systematically explores for the first time the ethnic differences in mental health among older people from ethnic minorities under the framework of Social Determinants of Health (SDH), providing evidence support for the formulation of precise intervention strategies.
2 Method
2.1 Samples and procedure
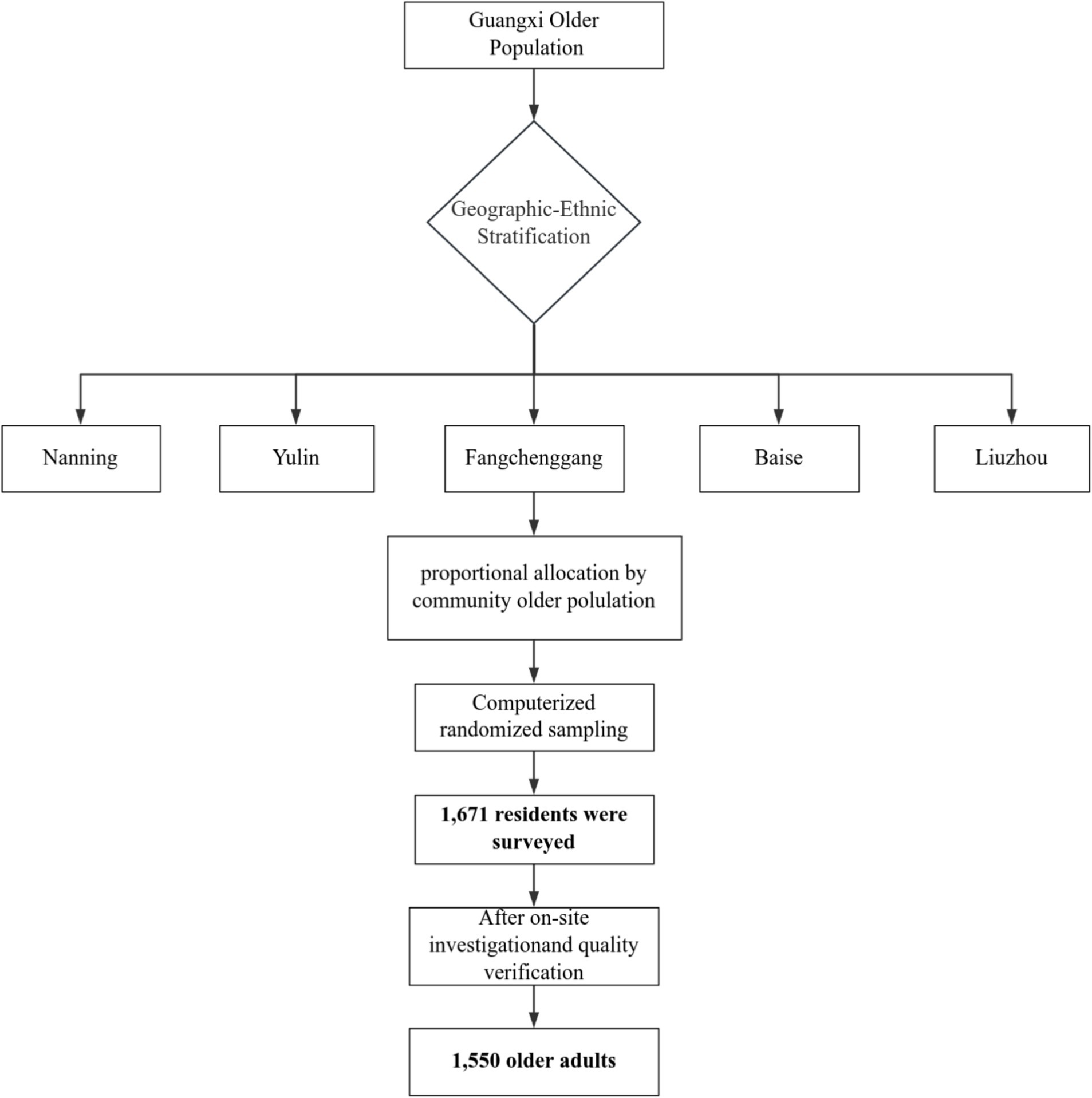
Data were collected between April and May 2024 in Guangxi Zhuang Autonomous Region, a southern Chinese border area characterized by ethnic diversity, including the Zhuang, Yao, Miao, Dong, Hui, Mulao, and Jing communities. Employing a multi-stage stratified sampling framework, we focused on five municipalities (Nanning, Yulin, Fangchenggang, Baise, Liuzhou) selected through geographic-ethnic stratification to represent predominant minority groups: Zhuang (Nanning), Han (Yulin), Jing (Fangchenggang), Yao (Baise), and Mulao (Liuzhou). Communities within each city were proportionally sampled based on older adult population registries. Using computer-generated random sampling, we identified potential participants aged ≥65 years who had resided locally for >6 months. Exclusion criteria included dementia or severe mental disorders, as reported by family members. The minimum sample size was determined using (15):, with Z1-/2 = 1.96, = 0.05 and d = 0.05, p = 0.211 (the prevalence of anxiety among the older adults was reported to be 21.1% based on previous studies) (16). Accounting for 20% non-response, we recruited 1,671 participants via telephone screening. After excluding 121 non-compliant cases, 1,550 subjects comprised the final sample. While stratification enhanced representativeness, the telephone recruitment may have excluded individuals with hearing difficulties or limited technology access. The sampling framework of this study as shown in Figure 1.
2.2 Variables and instruments
2.2.1 Dependent variable
(1) Anxiety status was assessed using the Generalized Anxiety Disorder (GAD-7) questionnaire. This scale has strong reliability, validity, repeatability and applicability among different populations and has been widely used in clinical practice (17). A score ≥5 is regarded as the presence of an anxious state, with 5, 10 and 15 points, respectively, serving as the cut-off points for mild, moderate and severe anxiety (18). (2) Depressive status was evaluated using the Patient Health Questionnaire-9 Questionnaire. This questionnaire is simple in design, easy to administer and score, and widely adopted in community mental health screenings. A score of 5 or above indicates a positive screening result and may reflect depressive symptoms. Scores of 5–9, 10–14 and 15–27, respectively, indicate the possible existence of mild, moderate and severe depression (19).
2.2.2 Independent variable
The Social Determinants of Health (SDH) encompass a wide range of factors that influence health outcomes, including economic, social, environmental, and psychosocial dimensions (20). These determinants are fundamental in shaping individuals’ health and disease trajectories, extending from birth through aging and encompassing all aspects of life, including growth, living conditions, and work environments (21). While SDH are primarily utilized to trace the origins of diseases, they also provide a comprehensive framework for understanding health disparities. For instance, a study previously employed SDH to examine the prevalence of depression among African American adults in the United States (22). In this study, SDH were categorized into five dimensions: individual characteristics, behavioral patterns, social support networks, socioeconomic status, and other social structural factors. Drawing on this framework, the current study identifies variables that may influence anxiety and depression among older adults in Guangxi: (1) individual characteristics: age, gender, ethnics, chronic diseases, cognitive impairment; (2) behavioral patterns: living alone or not, exercise frequency, psychological resilience, attitude towards aging; (3) social support networks: marital status, relationships with neighbors, support from couple, support from children, and support from friends; (4) socioeconomic status: residential area, employment, education level; (5) other social structural factors: medical insurance. Cognitive impairment was assessed using the Ascertain Dementia 8 (AD8). An AD8 score of ≥2 suggests cognitive impairment. The study found that the AD8 is particularly suitable for cognitive function screening in older community populations (23), and it is a quick, simple, sensitive, and reliable screening method (24).
2.2.3 Statistical analysis
Data were analyzed using SPSS software version 26.0 for iOS, with a p-value < 0.05 considered statistically significant. Descriptive statistics were employed for summarization, including frequencies and percentages for categorical data, as well as means and standard deviations for continuous data. Chi-square tests were used for bivariate analysis to identify significant differences in categorical variables between groups. Statistically significant variables from univariate analysis were included in the logistic regression model. Two binary logistic regression models were established to analyze the association between depression, anxiety, and predictor variables, calculating unadjusted odds ratios (UOR), adjusted odds ratios (AOR) and their 95% confidence intervals (CI).
2.2.4 Quality control
Subjects were selected, and questionnaires were collected according to established inclusion and exclusion criteria, ensuring on-site retrieval. All investigators underwent standardized training before the survey. During data collection, researchers were limited to clarifying and guiding doubts, strictly prohibiting any prompting, or influencing of respondents’ answers. To ensure accuracy, two research assistants were assigned to data entry. In case of discrepancies, a third party would review the original records and make corrections.
3 Results
3.1 Sample characteristics
Altogether, we invited 1,671 older people to participate in the study and 1,550 agreed and completed the survey questionnaire (response rate: 92.76%). The study sample mainly comprised older adults aged 65–74 years (61.0%), with an average age of 73.77 years (SD = 6.47), and the oldest respondent was 101 years old. Regarding gender distribution, 57.4% were female and 42.6% were male. Most participants were married (67.7%) and had an elementary school level (54.4%). In this study, the Han ethnic group, as a non-minority ethnic group, has the largest population, accounting for 26.8%. Meanwhile, the proportions of ethnic minorities such as the Jing, Yao, Mulao and Zhuang were 15.7, 17.9, 13.2 and 26.5%, respectively. Characteristics of the survey sample and prevalence rates of anxiety and depression among different subgroups are shown in Table 1. Chi-square tests revealed statistically significant differences (P1,2<0.05) in anxiety and depression symptoms across factors such as age, gender, ethnics, chronic diseases, cognitive impairment, exercise frequency, psychological resilience, aging attitude, marital status, relationship with neighbors, support from couple, Support from children, education level and medical insurance. Besides, Chi-square test results also indicated statistically significant differences (P1 = 0.035) in anxiety among older people based on the residential area.
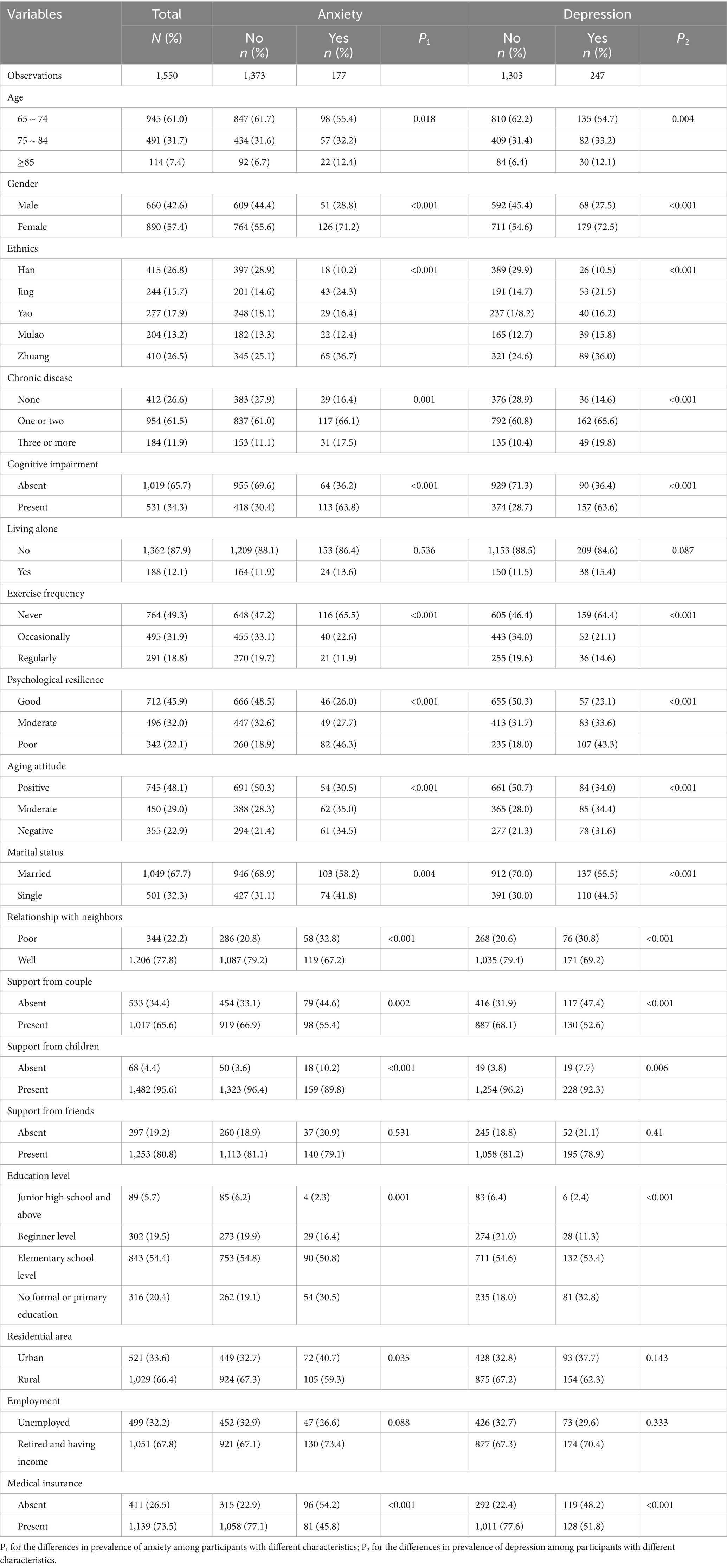
Table 1. Descriptive analysis of the general characteristics of the older people in ethnic minority areas by anxiety and depression.
3.2 Distribution of anxiety and depression symptoms
Figures 2, 3 illustrates the mental health characteristics of the participants. Comprehensive analysis shows that 11.42% of participants exhibited anxiety symptoms, 15.94% exhibited depression symptoms, and 8.19% reported mixed anxiety and depressive disorder. Among the older adult population with anxiety and depression, the proportion of mild cases is the largest, accounting for 77.97 and 77.73%, respectively. Figure 4 displays the distribution of anxiety and depression symptoms among different ethnic groups. The Jing nationality shows the highest incidence of mild to moderate symptoms and the total incidence rate, while the Zhuang ethnic group has the highest incidence of severe anxiety. For depression, The Jing nationality has the highest rate of mild depression, while the Zhuang nationality has the highest rates for moderate and severe depression. Collectively, ethnic minority groups demonstrated significantly higher overall prevalence rates of anxiety and depression compared to the Han Chinese population. This disparity persisted across all severity levels, with minority populations exhibiting elevated incidence rates for mild, moderate, and severe symptom presentations.
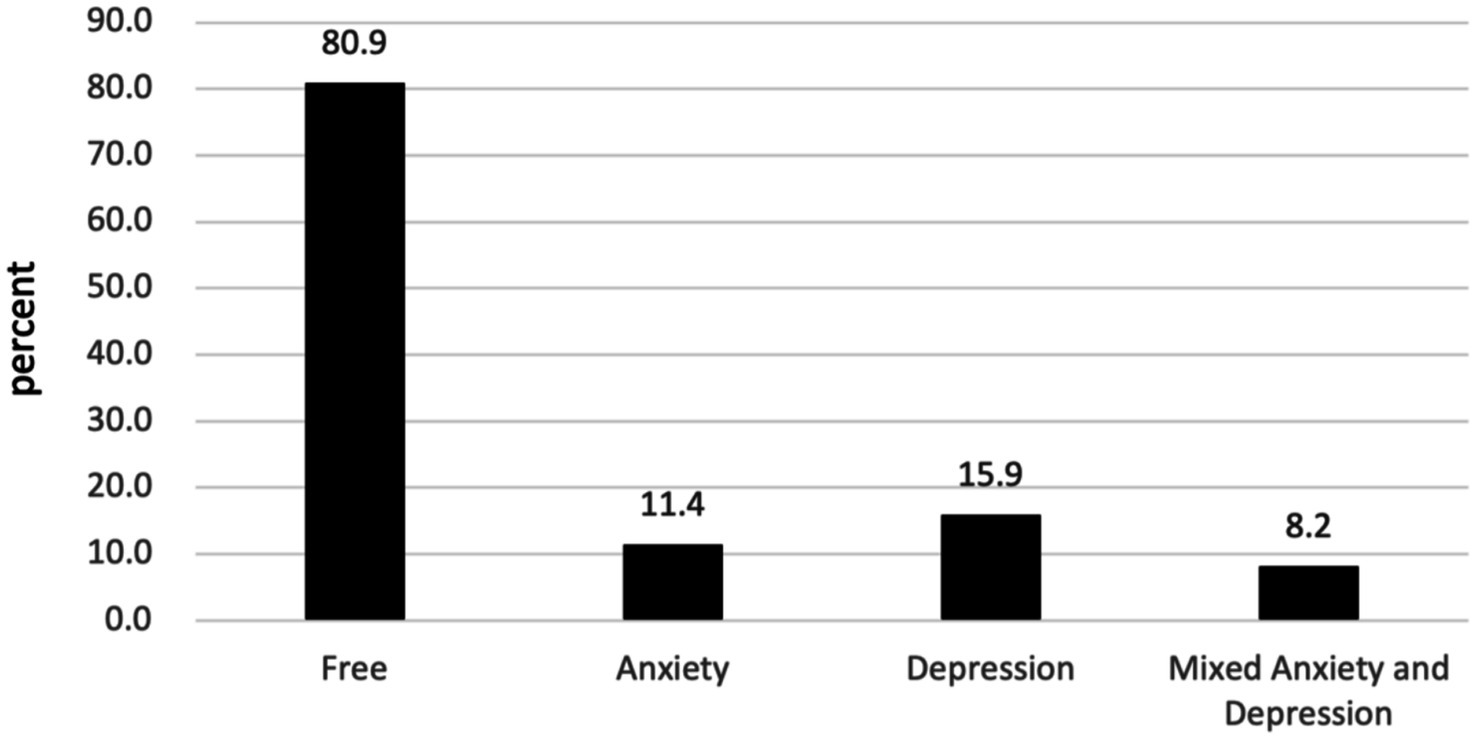
Figure 2. Psychological health problems among the studied group (N = 1,550). ‘Free,’ for group without anxiety or depression; ‘Anxiety’ for group with only anxiety; ‘Depression’ for group with only depression; and ‘Mixed Anxiety and Depression’ for group experiencing both conditions.
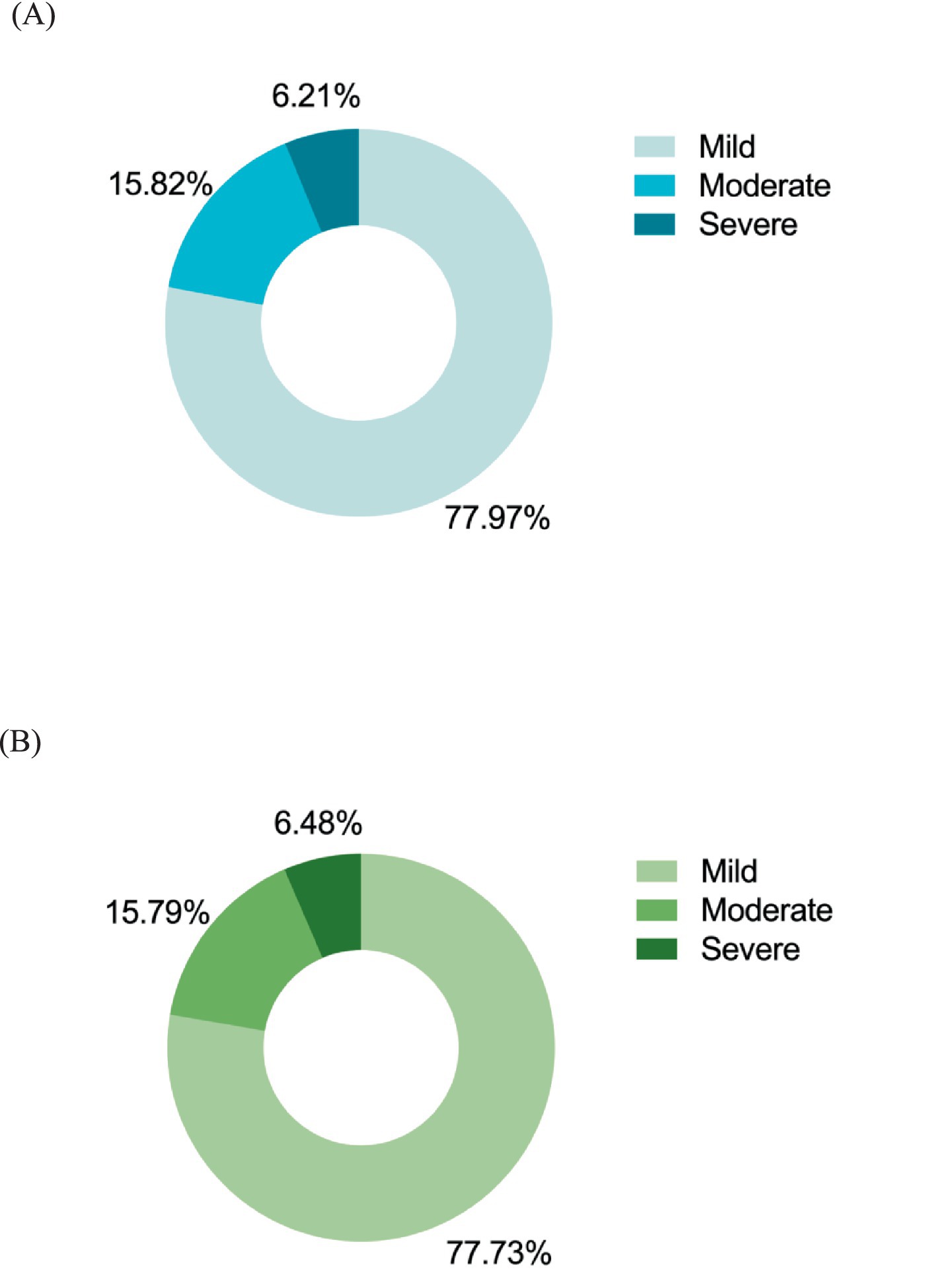
Figure 3. The prevalence of anxiety and depression of different severity. Mild, with GAD and PHQ scores ranging from 5 to 9; Moderate, GAD and PHQ scores in the 10–14 range; Sever, GAD and PHQ scores of 15 and above. (A) The rate of various severity levels of anxious older people (N = 177). (B) The rate of various severity levels of depressed older people (N = 247).
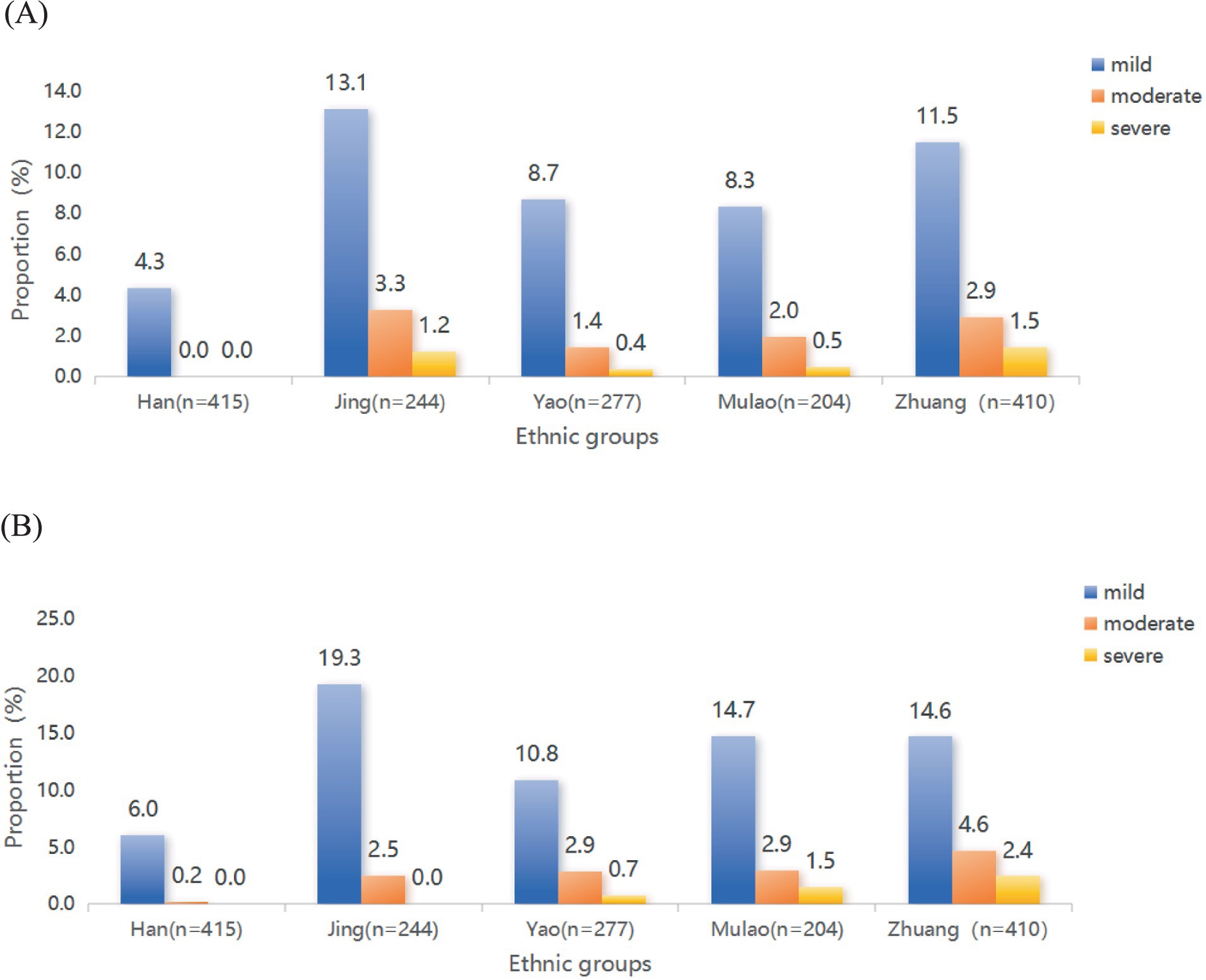
Figure 4. The prevalence of varying degrees of anxiety and depression among the older people in ethnic minority areas. (A) The rate of different severities of anxiety among multiple ethnic groups. (B) The rate of different severities of depression among multiple ethnic groups.
3.3 Correlates of anxiety and depression symptoms
Logistic regression analyses were conducted to test for significant predictors of anxiety, as detailed in Table 2. Based on the results of the bivariate analysis, significant variables were accessed in the regression model. In the multivariable model, those of female gender showed a higher risk factor for anxiety (AOR: 1.836, 95% CI: 1.213–2.78). The older adults from the Jing (AOR: 3.199, 95%CI: 1.629–6.284), Yao (AOR: 2.304, 95%CI: 1.15–4.619), Mulao (AOR: 1.999, 95% CI: 1.113–4.078) and Zhuang ethnic groups (AOR: 2.373, 95% CI: 1.305–4.316) all exhibit a heightened vulnerability to anxiety than those older adults from Han ethnic. Furthermore, those with cognitive impairment (AOR: 2.621, 95%CI: 1.804 ~ 3.809), poor psychological resilience (AOR: 2.276, 95%CI: 1.464 ~ 3.544) and a negative attitude towards aging (AOR: 1.555, 95%CI: 1.213 ~ 2.455) were also at an increased risk for anxiety. We also found that older residents receiving support from their children (AOR: 0.489, 95%CI: 0.308 ~ 0.778), living in rural (AOR: 0.434, 95%CI: 0.217 ~ 0.87) and having health insurance (AOR: 0.424, 95%CI: 0.287 ~ 0.626) exhibited a reduced likelihood of anxiety.
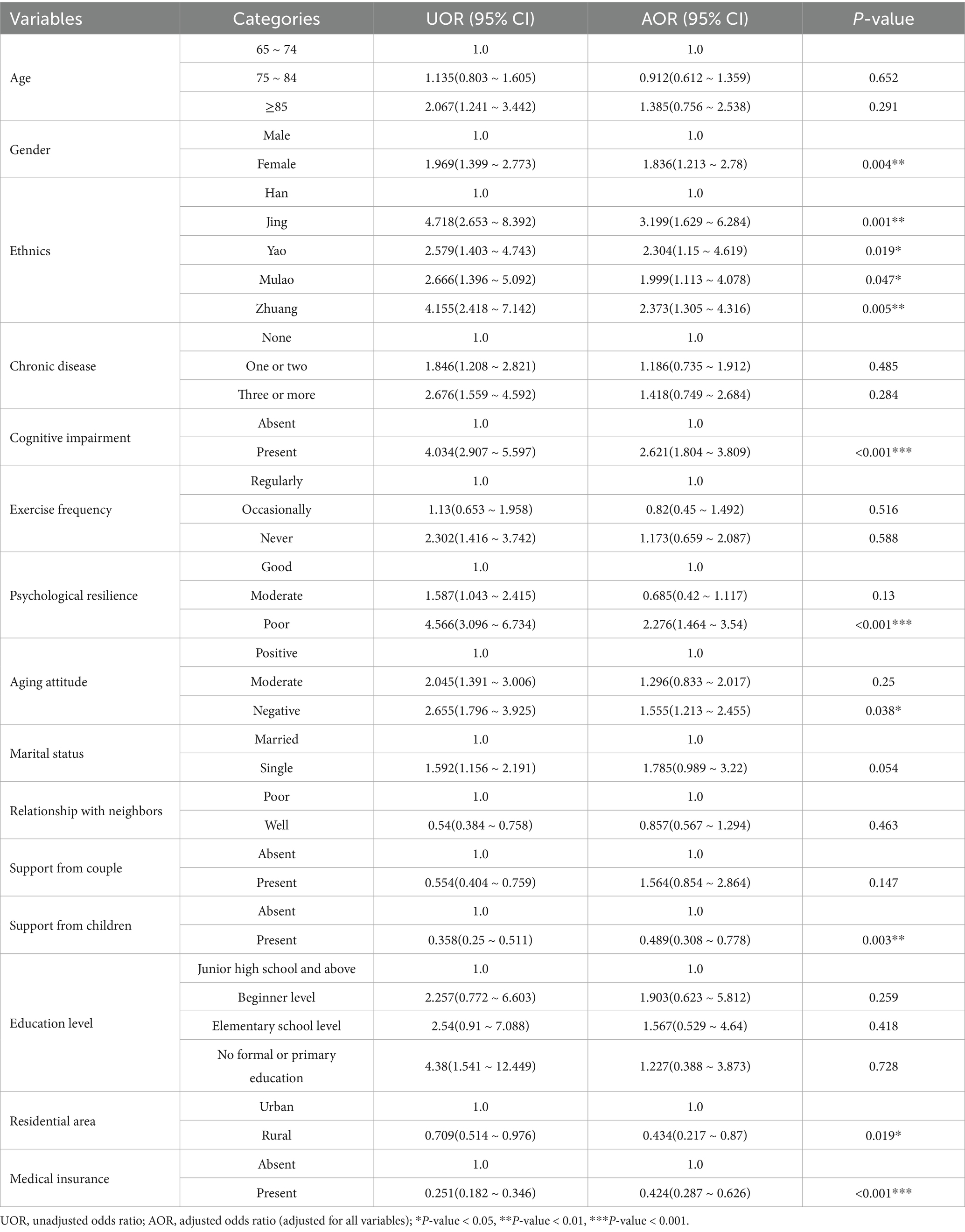
Table 2. Simple and multiple logistic regression for relationships between related variables and anxiety of the older people in ethnic minority areas (N = 1,550).
In the depression group, multiple logistic regression analysis identified nine significant factors associated with depressive symptoms, as detailed in Table 3. The findings indicate that older women (AOR: 1.632, 95% CI: 1.133 ~ 2.349) are at a higher risk of developing depression compared to men. Additionally, certain ethnic groups, including the Jing (AOR: 2.222, 95% CI: 1.226 ~ 4.026), Yao (AOR: 2.498, 95% CI: 1.369 ~ 4.559), Mulao (AOR: 3.195, 95% CI: 1.751 ~ 5.83), and Zhuang (AOR: 2.327, 95% CI: 1.39 ~ 3.894), were identified as having a higher likelihood of experiencing depressive symptoms. The presence of chronic diseases (AOR1: 1.597, 95% CI1: 1.038 ~ 2.456; AOR2:2.442, 95% CI2: 1.394 ~ 4.278) and cognitive impairment (AOR: 2.94, 95% CI: 2.122 ~ 4.073) were also found to be significantly associated with an increased risk of depression. Psychological resilience emerged as a crucial factor, with lower levels of resilience (AOR: 2.839, 95% CI: 1.903 ~ 4.236) and negative attitude (AOR: 1.455, 95% CI: 1.171 ~ 2.18) of aging identified as strong predictors of depression. Conversely, occasional physical exercise (AOR: 0.545, 95% CI: 0.357 ~ 0.833), support from children (AOR: 0.619, 95% CI: 0.405 ~ 0.945), and access to medical insurance (AOR: 0.583, 95% CI: 0.411 ~ 0.828) were found to be protective factors against depression.
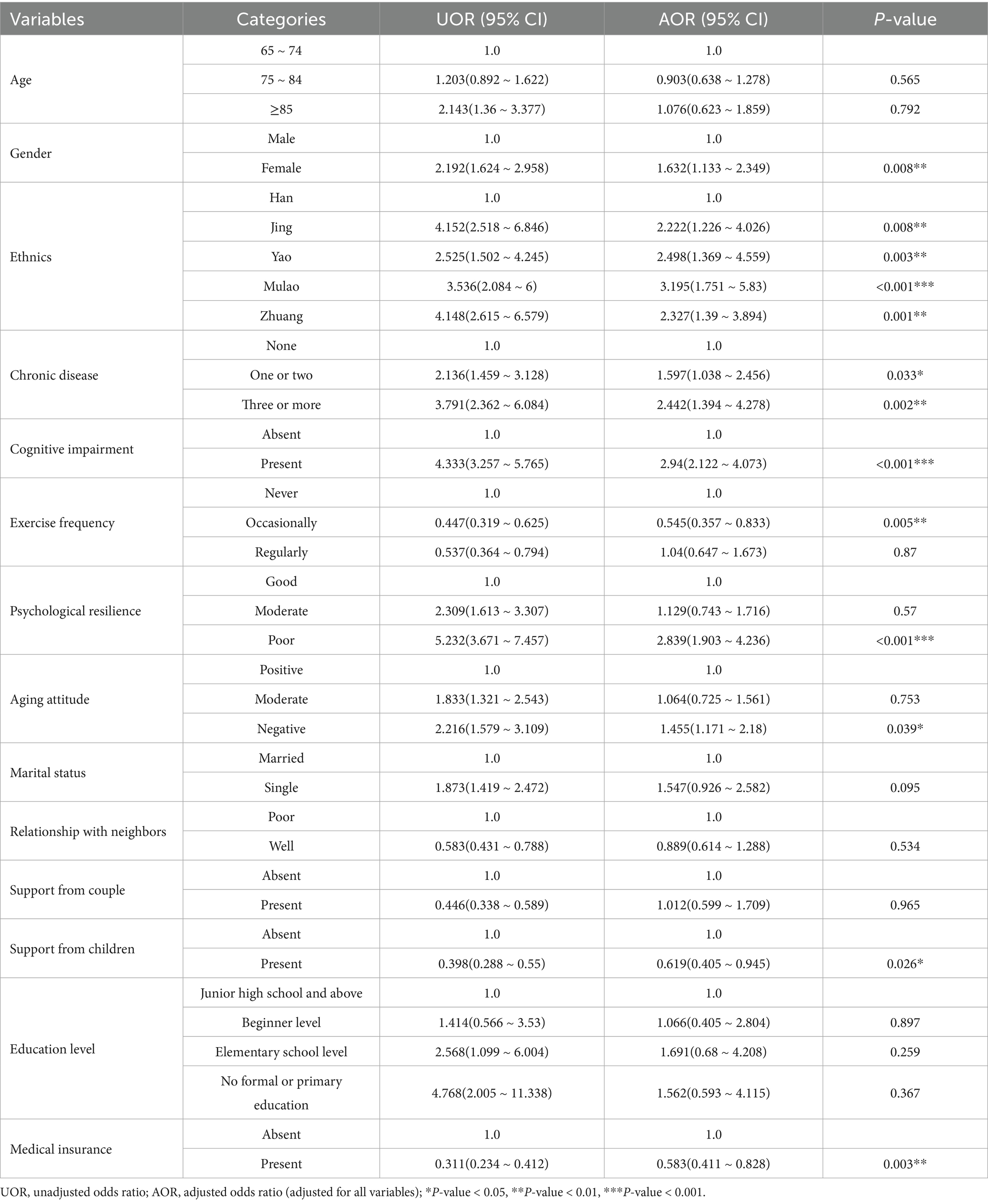
Table 3. Simple and multiple logistic regression for relationships between related variables and depression of the older people in ethnic minority areas (N = 1,550).
4 Discussion
The prevalence of anxiety symptoms among the older adults in ethnic minority regions of Guangxi, China is 11.42%, and the prevalence of depressive symptoms is 15.94%. The observed higher prevalence of depression in this study compared to urban Sri Lankan older adults (13.9%) may be due to the age distribution (25). The study’s depression rate is lower than in other developing countries such as India (52.5%) (26), Nepal (57.8%) (27), rural Egypt (44.4%) (28), and Ethiopia (45%) (29), possibly due to the socioeconomic status of the study populations (30). A study in Botswana reported a higher anxiety prevalence of 18.5%, which may be related to a higher proportion of older adults with chronic diseases and social impairments, affecting their ability to access quality healthcare (31). Despite lower detection rates of anxiety and depression compared to other developing countries, the rates in Guangxi Zhuang Autonomous Region remain significant, underscoring the necessity for research and attention to the mental health of the older people in ethnic minority areas of China.
This study identifies elevated depression and anxiety prevalence among Guangxi’s ethnic minorities (Jing, Zhuang, Mulao, Yao) compared to the Han majority (Tables 2, 3), aligning with Western China’s mental health disparity patterns (32). The Zhuang ethnic group is the largest ethnic minority group in Guangxi. As a distinct ethnic group with their own language, cultural and linguistic differences may present communication and adaptation challenges when interacting with the broader society (33). For the Jing ethnic group, we speculated that their proximity to Vietnam and the resulting environmental, cultural, and customary similarities may have an impact on the mental health of the older adults (34). The majority of older individuals from the Mulao and Yao ethnic groups reside in remote mountainous areas, which are characterized by poor transportation and limited access to information. These geographical and infrastructural limitations significantly impede their ability to access adequate medical security and mental health services (35). Structural socioeconomic inequalities exhibit robust associations with mental health disparities, particularly in economically underdeveloped multiethnic regions like Guangxi (30, 36). These vulnerabilities are exacerbated by persistent social exclusion and identity struggles, as evidenced by Snowden and Hannah’s frameworks on minority mental health (37, 38). Despite regional development initiatives, the interplay of cultural marginalization and socioeconomic deprivation perpetuates psychological distress among ethnic elders, necessitating interventions that address both biomedical service gaps and sociocultural determinants (Table 4).
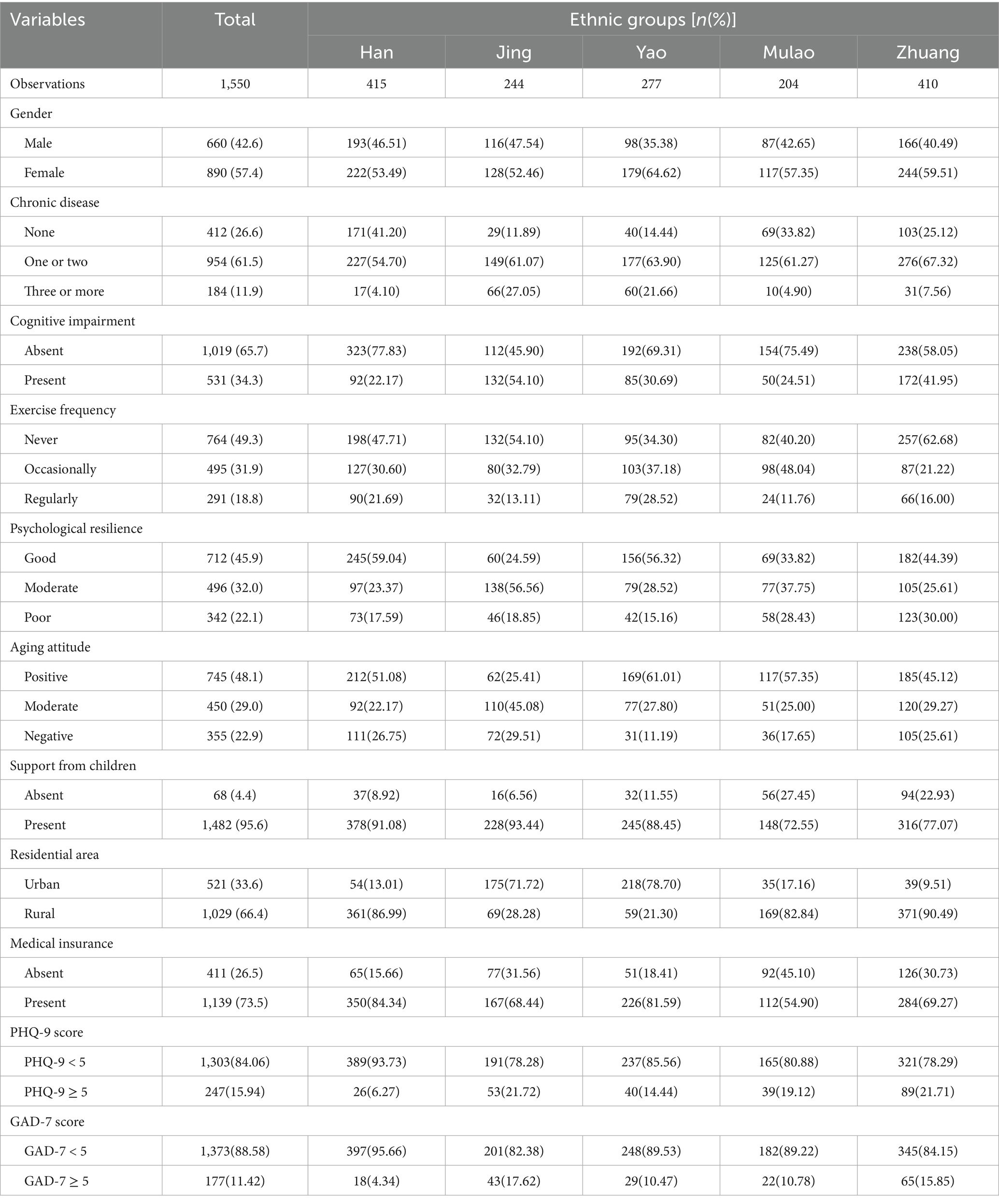
Table 4. Descriptive analysis of the general characteristics of the older people in different ethnic groups (N = 1,550).
Chronic illnesses significantly elevate depression risk in older adults, particularly among ethnic minorities. Meta-analytic evidence indicates that poor self-rated health and cardiovascular multimorbidity substantially increase depression susceptibility (39). Similarly, older adults with elevated scores on the AD8 scale also exhibit an increased susceptibility to anxiety and depressive disorders. Physical deterioration from chronic diseases often restricts daily functioning and social engagement, exacerbating mental health decline (40). This study highlights striking multimorbidity disparities, with Jing (88.12%) and Yao (85.56%) ethnic groups demonstrating exceptionally high rates. Contributory factors include culturally entrenched practices: sustained high-sodium/high-fat diets and normalized smoking/alcohol use as social rituals (41). These risk behaviors, compounded by systemic healthcare deficits – inadequate chronic disease screening and fragmented follow-up care in minority regions – create synergistic health threats (42). To disrupt this cycle, we propose: (1) culturally-tailored interventions integrating bilingual nutrition education (e.g., Zhuang language materials) into ethnic festivals to promote dietary modification and substance use reduction; (2) healthcare system strengthening through portable diagnostic deployment and village health worker training in early detection protocols; (3) equity-driven policy reforms prioritizing targeted subsidies and chronic care metrics in regional governance. Community-based chronic disease management coupled with mental health monitoring could optimize public health outcomes in aging populations (43, 44).
In this study, older individuals who with negative views of aging and poorer psychological resilience tend to be at a higher risk for anxiety and depressive symptoms, consistent with previous research (45, 46). Based on stereotype theory, Levy (47) proposed that aging attitudes influence the health status of the older people through physiological, behavioral, and psychological pathways. Internalized ageist stereotypes diminish self-efficacy and health behavior motivation (48–50), while multimorbidity exacerbates negative aging cognition through impaired self-care capacity (47, 51). Psychological resilience moderates this relationship, with enhanced emotional regulation buffering mental health impacts (52, 53). Our findings reveal critical disparities: Zhuang older adults demonstrated the poorer psychological resilience and more negative aging attitudes (Figure 4), correlating with their heightened anxiety/depression prevalence. To counteract these effects, we advocate: (1) An Intangible Cultural Heritage (ICH)-integrated intervention model utilizing traditional practices (e.g., ethnic dance, paper-cutting) to simultaneously preserve cultural identity and bolster self-worth; (2) Lifelong learning initiatives combining ethnic cultural studies with health literacy curricula to enable proactive aging engagement. These culturally grounded strategies target stereotype restructuring while promoting psychosocial resource accumulation, potentially disrupting the adverse aging perception-mental morbidity cycle.
This study corroborates the multifactorial protective effects against geriatric depression and anxiety. Regular physical exercise, particularly moderate-intensity aerobic and strength training, demonstrates dual benefits by enhancing physiological resilience and self-efficacy (54–57). Concurrently, filial support rooted in China’s cultural norms significantly mitigates mental health risks, with children serving as pivotal anchors in elders’ psychosocial support networks—a critical buffer against loneliness among ethnic minority populations (58–60). Notably, rural elders exhibited lower anxiety prevalence than urban counterparts (49), potentially attributable to traditional value systems that foster adaptive coping with life transitions (61, 62). These findings collectively underscore the necessity of culturally informed interventions that synergize biopsychosocial mechanisms to optimize mental health outcomes in aging populations.
Our article also illustrates that participation in medical insurance programs has a beneficial impact on mitigating symptoms of depression and anxiety. With insured middle-aged and older adults achieved higher life satisfaction compared to their uninsured counterparts (63, 64). Liu’s analysis confirms insurance’s critical role in geriatric mental health (65), while Baicker’s research highlights Medicaid expansion decreasing undiagnosed and untreated depression by 50 and 60%, respectively (66). However, Cheruvu and Chiyaka (67) observed elevated depression risks among insured seniors facing substantial out-of-pocket costs, suggesting coverage adequacy, not mere availability, determines mental health outcomes. These divergent findings likely stem from methodological variations, particularly in assessing financial toxicity thresholds. Our findings extend this discourse through ethnic disparity analysis (Figure 4): Han Chinese show highest insurance coverage (84.34%) versus Mulao minority’s lowest rates (54.90%), attributable to geographical remoteness compounding systemic barriers inadequate insurance promotion, complex reimbursement protocols, and income constraints limiting commercial insurance access. Crucially, basic insurance schemes in minority regions inadequately cover mental health services (68), maintaining suboptimal reimbursement rates for depression/anxiety treatments.
Furthermore, our findings demonstrate a significant association between female gender and the prevalence of anxiety and depressive symptoms, consistent with systematic reviews identifying gender as a critical predictor of mental health disparities among older adults (69). This gender disparity may be mediated by multifaceted determinants including socioeconomic status disparities, traumatic life experiences, and hormonal fluctuations (70–72). Community-based mental health initiatives should prioritize geriatric females through targeted interventions: implementing mental health literacy programs to enhance disease awareness, and establishing dedicated counseling channels (hotlines or in-person sessions) to provide timely psychological support and counseling.
This study identified the influencing factors of anxiety and depression among older adult from ethnic minorities and made relevant analyses on ethnic differences. Guided by Scott’s theory of weak ethnic groups (73), we proposes a culturally adaptive intervention framework addressing structural mental health disparities among ethnic minorities. The multipronged approach integrates: (1) a multilingual digital platform featuring AI-driven speech interaction (dialect recognition accuracy≥92%) and a cross-linguistic terminology repository spanning eight ethnic languages (Zhuang, Yao, Jing, etc.), enabling culturally congruent mental health screening; (2) a tiered training system for bilingual cultural coordinators (1.5 per 10,000 residents) requiring dual certification in ethnic linguistic proficiency and traditional healing practices, supported by mobile service kits and health behavior incentive programs; (3) a three-tier clinical network (village-town-city) incorporating digital PHQ-9/GAD-7 screening, VR-based relaxation therapy, and cross-cultural CBT, enhanced by blockchain medical records and UAV-delivered emergency supplies (≤12 h response); (4) policy innovations including formulating relevant laws to stipulate an 85% screening insurance coverage rate, as well as conducting cross-border intervention exchanges through the ASEAN Mental Health Alliance. This framework systematically bridges cultural competence gaps while addressing healthcare access inequities through technological, human resource, and policy synergies.
While this study provides novel insights into ethnic mental health disparities among older adults in China, several limitations warrant consideration. First, although validated scales were employed, cultural variations in symptom expression among ethnic minorities might affect measurement accuracy, as standardized cutoff scores may not fully account for culturally specific manifestations of distress. Second, the cross-sectional design precludes causal inferences regarding observed associations between social determinants and mental health outcomes. Third, while the SDH framework was comprehensively applied, unmeasured confounders such as historical trauma or acculturative stress—known mediators of minority mental health—were not assessed. These limitations underscore the need for longitudinal designs integrating mixed methods to elucidate causal pathways. Future studies should validate mental health instruments through cognitive interviewing with minority elders and employ geospatial analytics to quantify healthcare accessibility barriers.
5 Conclusion
This study reveals ethnic minority older adults (Jing, Zhuang, Yao, Mulao) in Guangxi, China, face 2 ~ 3 times higher anxiety/depression risks than Han Chinese, driven by structural inequities (geographic isolation, cultural-linguistic barriers) and socioeconomic deprivation. Key risk factors include female gender, chronic multimorbidity, cognitive dysfunction, poor psychological resilience and negative aging attitudes, while occasional exercise, child support and medical insurance emerged as vital protective buffers. We propose a culturally adaptive intervention framework integrating: (1) AI-powered multilingual screening platforms; (2) bilingual cultural coordinators bridging traditional/modern care; (3) digital-physical hybrid clinical networks; (4) policy reforms ensuring 85% insurance coverage for mental health services. Although cross-sectional data limit causal analysis, this first Social Determinants of Health (SDH)-based study in China’s ethnic aging context provides actionable strategies to address healthcare inequities. Future work should validate interventions through longitudinal designs and quantify historical trauma’s role. This model offers a blueprint for achieving health equity in multiethnic aging societies globally.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the First Affiliated Hospital of Guangxi Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SW: Conceptualization, Data curation, Investigation, Visualization, Writing – original draft. LY: Data curation, Investigation, Validation, Writing – original draft. HM: Investigation, Validation, Writing – original draft. LL: Formal analysis, Investigation, Writing – original draft. ZL: Investigation, Methodology, Software, Writing – original draft. YY: Funding acquisition, Project administration, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Peak Project of Nursing Clinical Research of the First Affiliated Hospital of Guangxi Medical University (Program no. YYZS2020025), Research project of mental health status and intervention suggestions of the older people in Guangxi and Health appropriate Technology development and application project of Health Commission of Guangxi Zhuang Autonomous Region, China (Program no. S2021111).
Acknowledgments
The authors acknowledge the time and effort that participants expended on this survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization: Aging and health (2022). Available online at: https://www.who.int/newsroom/factsheets/detail/ageing-and-health (accessed March 1, 2024)
2. National Bureau of Statistics. Annual data (2023). Available online at: https://data.stats.gov.cn/easyquery.htm?cn=C01 (accessed March 2, 2024).
3. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
4. Xia, YL, and Liu, ZH. A study on the impact of economic welfare on the depression status of the elderly in urban and rural areas of China. World Survey Res. (2020) 30:1–4. doi: 10.13778/j.cnki.11-3705/c.2018.01.003
5. Huang, Y, Wang, Y, and Wang, H. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
7. Fu, XL, and Zhang, K. Blue book of mental health status of the elderly in China. Health and Life. (2021) 17:48–9.
8. Byers, AL, Yaffe, K, Covinsky, KE, Friedman, MB, and Bruce, ML. High occurrence of mood and anxiety disorders among older adults: the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2010) 67:489–96. doi: 10.1001/archgenpsychiatry.2010.35
9. Guangxi Zhuang Autonomous Region Bureau of Statistics. (2023). Regional annual statistical bulletin. Available online at: http://tjj.gxzf.gov.cn/tjsj/tjgb/qqgb/t18207923.shtml (accessed May 1, 2024)
10. Ma, N, Chen, RZ, Zhang, WF, Wang, YF, Bai, Y, and Su, RC. Analysis of mental health resources in China in 2020. Chin J Psychiatry. (2022) 55:459–68. doi: 10.3760/cma.j.cn113661-20220617-00158
11. Lu, J, Xu, XF, Huang, YQ, Li, T, Ma, C, and Xu, GM. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2021) 8:981–90. doi: 10.1016/S2215-0366(21)00251-0
12. Spencer, LH, Cooledge, BA, and Hoare, Z. The experiences of minority language users in health and social care research: a systematic review. Int J Health Plann Manag. (2025) 40:3–24. doi: 10.1002/hpm.3825
13. He, LP, Yu, Z, Meng, Q, Wu, S, Mu, F-t, and Li, X-m. The study of health equity among the older people in border minority areas. Soft Sci Health. (2019) 33:31–5. doi: 10.3969/j.issn.1003-2800.2019.08.008
14. Cook, BL, Trinh, NH, Li, Z, Hou, SS, and Progovac, AM. Trends in racial-ethnic disparities in access to mental health care, 2004-2012. Psychiatr Serv. (2017) 68:9–16. doi: 10.1176/appi.ps.201500453
15. Charan, J, and Biswas, T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. (2013) 35:121–6. doi: 10.4103/0253-7176.116232
16. Xie, Q, Xu, YM, and Zhong, BL. Anxiety symptoms in older Chinese adults in primary care settings: prevalence and correlates. Front Public Health. (2022) 10:1009226. doi: 10.3389/fpubh.2022.1009226
17. He, XY, Li, CB, and Qian, J. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatry. (2010) 22:200–3. doi: 10.3969/j.issn.1002-0829.2010.04.002
18. Wang, Y, Chen, R, and Zhang, L. Evaluation of the reliability and validity of the generalized anxiety disorder 7-item scale among inpatients in general hospital. J Clin Psychiatry. (2018) 28:168–71. doi: 10.3969/j.issn.1005-3220.2018.03.007
19. Xu, Y, Wu, HS, and Xu, YF. The reliability and validity of patient health questionnaire depression module (PHQ-9) in Chinese elderly. Shanghai Arch Psychiatry. (2007) 5:257–59+276. doi: 10.3969/j.issn.1002-0829.2007.05.001
20. World Health Organization. Social determinants of health. Available online at: http://www.who.int/publications/i/item/9789241500852 (accessed March 3, 2024).
21. Goldstein, SP, Tovar, A, Espel-Huynh, HM, and Stowers, KC. Applying a social determinants of health framework to guide digital innovations that reduce disparities in chronic disease. Psychosom Med. (2023) 85:659–69. doi: 10.1097/PSY.0000000000001176
22. Yelton, B, Friedman, DB, Noblet, S, Lohman, MC, Arent, MA, Macauda, MM, et al. Social determinants of health and depression among African American adults: a scoping review of current research. Int J Environ Res Public Health. (2022) 19:1498. doi: 10.3390/ijerph19031498
23. Zhang, SR, Jin, Y, Xu, SH, and Liu, XL. Application of Mini-cog and AD8 in early cognitive status evaluation and predicting cognitive deterioration of aged population. Chin J Geriatr Res. (2020) 7:17–21. doi: 10.3877/cma.j.issn.2095-8757.2020.02.005
24. Usarel, C, Dokuzlar, O, Aydin, AE, Soysal, P, and Isik, AT. The AD8 (dementia screening interview) is a valid and reliable screening scale not only for dementia but also for mild cognitive impairment in the Turkish geriatric outpatients. Int Psychogeriatr. (2019) 31:223–9. doi: 10.1017/S1041610218000674
25. Rajapakshe, OBW, Sivayogan, S, and Kulatunga, PM. Prevalence and correlates of depression among older urban community-dwelling adults in Sri Lanka. Psychogeriatrics. (2019) 19:202–11. doi: 10.1111/psyg.12389
26. Paul, NSS, Ramamurthy, PH, Paul, B, Saravanan, M, Santhosh, SR, Fernandes, D, et al. Depression among geriatric population; the need for community awareness. Clin Epidemiol Glob Health. (2019) 7:107–10. doi: 10.1016/j.cegh.2018.02.006
27. Chalise, HN. Depression among elderly living in Briddashram (old age home). Adv Aging Res. (2014) 3:1002. doi: 10.4236/aar.2014.31002
28. Mohamed, E, and Abd-Elhamed, M. Depression among elderly attending geriatric clubs in Assiut city, Egypt. J Am Sci. (2011) 7:386–91.
29. Mulat, N, Gutema, H, and Wassie, GT. Prevalence of depression and associated factors among elderly people in Womberma district, north-west, Ethiopia. BMC Psychiatry. (2021) 21:1–3. doi: 10.1186/s12888-021-03205-2
30. Lund, C, Brooke-Sumner, C, Baingana, F, Baron, EC, Breuer, E, Chandra, P, et al. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. (2018) 5:357–69. doi: 10.1016/S2215-0366(18)30060-9
31. Mutepfa, MM, Motsamai, TB, Wright, TC, Tapera, R, and Kenosi, LI. Anxiety and somatization: prevalence and correlates of mental health in older people (60+years) in Botswana. Aging Ment Health. (2021) 25:2320–9. doi: 10.1080/13607863.2020.1822289
32. Liu, X, Zhao, W, Hu, F, Hao, Q, Hou, L, Sun, X, et al. Comorbid anxiety and depression, depression, and anxiety in comparison in multi-ethnic community of West China: prevalence, metabolic profile, and related factors. J Affect Disord. (2022) 298:381–7. doi: 10.1016/j.jad.2021.10.083
33. de Queiróz Coutinho, AT, de Lima Silva, V, da Silva, MEF, de Lima, AC, de Lima, MLLT, de Almeida Queiróz, AAF, et al. Anxiety, depression, and other factors associated with voice handicaps in active older people during the COVID-19 pandemic. J Voice (2023). [Epubh ahead of preprint]. doi: 10.1016/j.jvoice.2023.05.016
34. Dao, ATM, Nguyen, VT, Nguyen, HV, and Nguyen, LTK. Factors associated with depression among the elderly living in urban Vietnam. Biomed Res Int. (2018) 2018:2370284. doi: 10.1155/2018/2370284
35. Tan, CC. Analysis of the current status, causes, and optimization path of medical and health development in ethnic regions from the perspective of ethnic unity. Adv Soc Sci. (2024) 13:176–181. doi: 10.12677/ass.2024.139798
36. Marmot, MG, Smith, GD, Stansfeld, S, Patel, C, and North, F. Health inequalities among British civil servants: the Whitehall II study. Lancet. (1991) 337:1387–93. doi: 10.1016/0140-6736(91)93068-k
37. Snowden, LR. Barriers to effective mental health services for African Americans. Ment Health Serv Res. (2001) 3:181–7. doi: 10.1023/a:1013172913880
38. Jongsma, HE, Karlsen, S, Kirkbride, JB, and Jones, PB. Understanding the excess psychosis risk in ethnic minorities: the impact of structure and identity. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1913–21. doi: 10.1007/s00127-021-02042-8
39. Qiu, QW, Qian, S, Li, JY, Jia, RX, Wang, YQ, and Xu, Y. Risk factors for depressive symptoms among older Chinese adults: a meta-analysis. J Affect Disord. (2020) 277:341–6. doi: 10.1016/j.jad.2020.08.036
40. Chow, LS, Gerszten, RE, Taylor, JM, Pedersen, BK, and van Praag, H. Exerkines in health, resilience, and disease. Nat Rev Endocrinol. (2022) 18:273–89. doi: 10.1038/s41574-022-00641-2
41. Su, HB, Qin, YQ, Chen, Q, Zhang, D, Ming, LL, and Qin, XM. Study on the basic characteristics and influencing factors of elderly chronic diseases in minority communities of Guangxi, China. Strait J Prevent Med. (2022) 28:19–21.
42. Li, T, Hou, WW, Kang, H, Tian, YH, and Hegefu, E. Analysis on prevalence of chronic diseases among rural residents in ethnic minority areas. Health Educ Health Promot. (2021) 16:241–4. doi: 10.16117/j.cnki.31-1974/r.202103241
43. Chen, D, Zhang, Y, Huang, T, and Jia, J. Depression and risk of gastrointestinal disorders: a comprehensive two-sample Mendelian randomization study of European ancestry. Psychol Med. (2023) 53:7309–21. doi: 10.1017/S0033291723000867
44. Irwin, MR, Carrillo, C, Sadeghi, N, Bjurstrom, MF, Breen, EC, and Olmstead, R. Prevention of incident and recurrent major depression in older adults with insomnia: a randomized clinical trial. JAMA Psychiatry. (2022) 79:33–41. doi: 10.1001/jamapsychiatry.2021.3422
45. Castellano Fuentes, CL. An analysis of the relationship between the attitudes towards old age and ageing, and well-being indicators in a sample of old people. Rev Esp Geriatr Gerontol. (2014) 49:108–14. doi: 10.1016/j.regg.2013.06.001
46. Trigg, R, Watts, S, Jones, R, Tod, A, and Elliman, R. Self-reported quality of life ratings of people with dementia: the role of attitudes to aging. Int Psychogeriatr. (2012) 24:1085–93. doi: 10.1017/S1041610212000038
47. Levy, B. Stereotype embodiment: a psychosocial approach to aging Curr Dir Psychol Sci (2009) 18 332–336 doi: 10.1111/j.1467-8721.2009.01662.x
48. Chasteen, AL. The role of age and age-related attitudes in perceptions of elderly individuals. Basic Appl Soc Psychol. (2000) 22:147–56. doi: 10.1207/S15324834BASP2203_3
49. Liu, D, Xi, J, Hall, BJ, Fu, M, and Zhang, B. Attitudes toward aging, social support, and depression among older adults: difference by urban and rural areas in China. J Affect Disord. (2020) 274:85–92. doi: 10.1016/j.jad.2020.05.052
50. Bellingtier, JA, and Neupert, SD. Negative aging attitudes predict greater reactivity to daily stressors in older adults. J Gerontol B Psychol Sci Soc Sci. (2018) 73:1155–9. doi: 10.1093/geronb/gbw086
51. Siebert, JS, Wahl, HW, and Schröder, J. The role of attitude toward own aging for fluid and crystallized functioning: 12-year evidence from the ILSE study. J Gerontol B Psychol Sci Soc Sci. (2018) 73:836–45. doi: 10.1093/geronb/gbw050
52. Sun, J, and Li, W. Mediating effect of psychological resilience between depression in the elderly in communities and social support. Chin Gen Pract. (2015) 18:827–30. doi: 10.3969/j.issn.1007-9572.2015.07.023
53. Gong, Y, Wen, HJ, Wen, K, Xu, ML, and Zhang, YT. The relationship between social support and anxiety among urban empty-nesters: the mediating role of psychological resilience. Chin J Gerontol. (2023) 43:5109–12. doi: 10.3969/j.issn.1005-9202.2023.20.066
54. He, ZF, Tan, WY, Ma, H, Shuai, Y, Shan, Z, Zhai, J, et al. Prevalence and factors associated with depression and anxiety among older adults: a large-scale cross-sectional study in China. J Affect Disord. (2024) 346:135–43. doi: 10.1016/j.jad.2023.11.022
55. Aguiñaga, S, Ehlers, DK, Salerno, EA, Fanning, J, and Motl, RW. Home-based physical activity program improves depression and anxiety in older adults. J Phys Act Health. (2018) 15:692–6. doi: 10.1123/jpah.2017-0390
56. Callow, DD, Arnold-Nedimala, NA, Jordan, LS, Pena, GS, and Won, J. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am J Geriatr Psychiatry. (2020) 28:1046–57. doi: 10.1016/j.jagp.2020.06.024
57. Maula, A, LaFond, N, Orton, E, Iliffe, S, and Audsley, S. Use it or lose it: a qualitative study of the maintenance of physical activity in older adults. BMC Geriatr. (2019) 19:349. doi: 10.1186/s12877-019-1366-x
58. He, H, Tan, T, and Wang, HSQ. Research on the influence of adults’ support on the physical and mental health of urban and rural elderly——empirical analysis based on China longitudinal aging social survey 2014. Populat Dev. (2020) 26:35–42+13.
59. Abolfathi Momtaz, Y, Ibrahim, R, and Hamid, TA. The impact of giving support to others on older adults’ perceived health status. Psychogeriatrics. (2014) 14:31–7. doi: 10.1111/psyg.12036
60. Chen, JY, Fang, Y, and Zeng, YB. A study on the impact of diversified social involvement and family support on the mental health of elderly people in China. Chin J Health Policy. (2021) 14:45–51. doi: 10.3969/j.issn.1674-2982.2021.10.007
61. Li, C, Jiang, S, and Zhang, X. Intergenerational relationship, family social support, and depression among Chinese elderly: a structural equation modeling analysis. J Affect Disord. (2019) 248:73–80. doi: 10.1016/j.jad.2019.01.032
62. Wu, M, Yang, Y, Zhang, D, Zhao, X, and Sun, Y. Association between social support and health-related quality of life among Chinese rural elders in nursing homes: the mediating role of resilience. Qual Life Res. (2017) 27:783–92. doi: 10.1007/s11136-017-1730-2
63. Sun, J, Coyte, PC, Liu, Y, and Wang, Q. Association between medical insurance and life satisfaction among middle-aged and older adults in China: the mediating role of depression. Cost Eff Resour Alloc. (2025) 23:10. doi: 10.1186/s12962-024-00584-7
64. Sun, J, Yao, N, and Lyu, S. The association between urban and rural resident basic medical insurance and depressive symptoms among Chinese middle-aged and older adults: evidence from the China health and retirement longitudinal study. Int J Health Plann Manag. (2021) 36:3305. doi: 10.1002/hpm.3305
65. Liu, H, Zhou, Z, Fan, X, Shen, C, Ma, Y, Sun, H, et al. Association between multiple chronic conditions and depressive symptoms among older adults in China: evidence from the China health and retirement longitudinal study (CHARLS). Int J Public Health. (2023) 68:1605572. doi: 10.3389/ijph.2023.1605572
66. Baicker, K, Allen, HL, Wright, BJ, Taubman, SL, and Finkelstein, AN. The effect of Medicaid on management of depression: evidence from the Oregon health insurance experiment. Milbank Q. (2018) 96:29–56. doi: 10.1111/1468-0009.12311
67. Cheruvu, VK, and Chiyaka, ET. Prevalence of depressive symptoms among older adults who reported medical cost as a barrier to seeking health care: findings from a nationally representative sample. BMC Geriatr. (2019) 19:192. doi: 10.1186/s12877-019-1203-2
68. Donohue, JM, Cole, ES, James, CV, Jarlenski, M, Michener, JD, and Roberts, ET. The US Medicaid program: coverage, financing, reforms, and implications for health equity. JAMA. (2022) 328:1085–99. doi: 10.1001/jama.2022.14791
69. Ciuffreda, G, Cabanillas-Barea, S, Carrasco-Uribarren, A, Albarova-Corral, MI, Arguello-Espinosa, MI, and Marcen-Roman, Y. Factors associated with depression and anxiety in adults≥60 years old during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2021) 18:11859. doi: 10.3390/ijerph182211859
70. Li, SH, and Graham, BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry. (2017) 4:73–82. doi: 10.1016/S2215-0366(16)30358-3
71. Altemus, M, Sarvaiya, N, and Epperson, CN. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. (2014) 35:320–30. doi: 10.1016/j.yfrne.2014.05.004
72. Deecher, D, Andree, TH, Sloan, D, and Schechter, LE. From menarche to menopause: exploring the underlying biology of depression in women experiencing hormonal changes. Psychoneuroendocrinology. (2008) 33:3–17. doi: 10.1016/j.psyneuen.2007.10.006
Keywords: older people, community, anxiety, depression, ethnic minority
Citation: Wu S, Yang L, Mo H, Li L, Li Z and Ying Y (2025) Prevalence and factors associated with anxiety and depression among the older people in ethnic minority areas in southern China: a cross-sectional study. Front. Public Health. 13:1494629. doi: 10.3389/fpubh.2025.1494629
Edited by:
Ivy Yan Zhao, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Graciela Rojas, University of Chile, ChileAndrew Wister, Simon Fraser University, Canada
Yuhang Zhou, University of Florida, United States
Copyright © 2025 Wu, Yang, Mo, Li, Li and Ying. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanping Ying, eWFucGluZ3lpbmcwMTE2QDEyNi5jb20=
 Suyi Wu
Suyi Wu Liu Yang
Liu Yang Yanping Ying
Yanping Ying