- 1Department of Medical Communication, School of Pharmacy and Pharmaceutical Sciences, Hoshi University, Tokyo, Japan
- 2Department of Health Communication, School of Public Health, The University of Tokyo, Tokyo, Japan
- 3University Hospital Medical Information Network (UMIN) Center, The University of Tokyo Hospital, Tokyo, Japan
- 4School of Pharmacy and Pharmaceutical Sciences, Hoshi University, Tokyo, Japan
- 5Chichibu Municipal Hospital, Saitama, Japan
Introduction: Women undergoing infertility treatment are often tagged with negative labels, subjected to negative reactions and behaviors by laypeople (public stigma), and they internalize these negative values (self-stigma). As self-stigma is associated with poor mental health, a measure is needed to determine the current state of public stigma in Japan and to evaluate the effectiveness of efforts to reduce it. However, existing instruments to measure public stigma in this context are limited. Therefore, this article aims to describe the research protocol for the development of the Infertility Public Stigma Scale for Japanese women and examination of its reliability and validity.
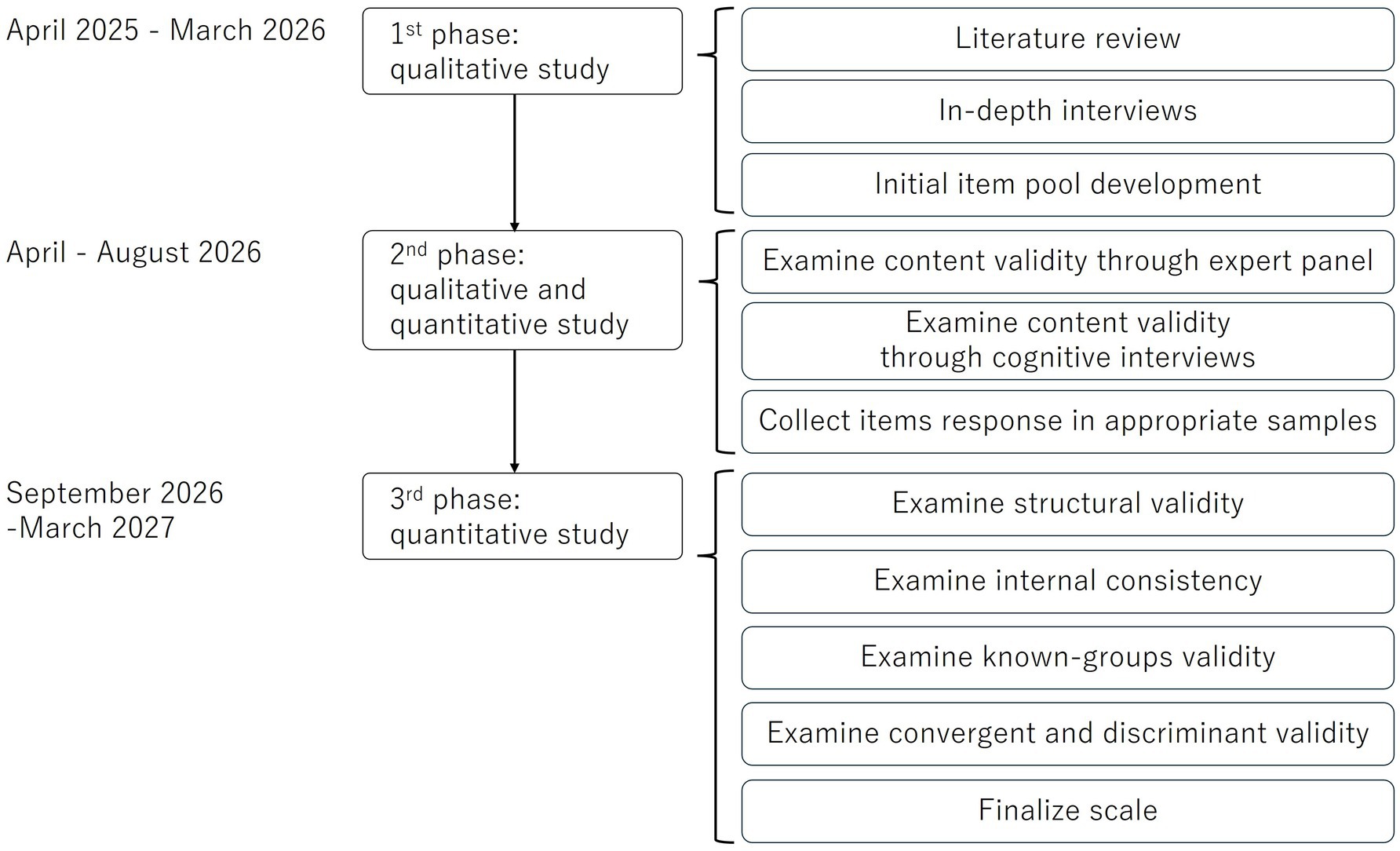
Methods and analysis: This study will adopt an exploratory, sequential, mixed-methods design. In the qualitative research phase, the constructs and components of public stigma toward women undergoing infertility treatment will be explored based on interviews with Japanese laypeople. Eligible participants will be recruited through purposive sampling, ensuring maximum variation in sex, age, occupation, place of residence, medical history, and contact with women with primary or secondary infertility. Data will be analyzed using qualitative-descriptive methods and inductive thematic analysis to develop the initial scale. After examining the content validity through an expert panel and cognitive debriefing, laypeople will be surveyed online to test the scale’s validity and reliability. Quantitative research will be conducted using the initial scale. Structural validity will be examined using exploratory and confirmatory factor analyses. Known-groups validity will be tested based on the hypothesis that laypeople aged over 60 years exhibit higher levels of public stigma than younger individuals. Convergent validity will be tested under the hypothesis that individuals with higher levels of fertility knowledge will also report higher levels of public stigma. Convergent and discriminant validity will be examined using a multitrait-scaling analysis. Internal consistency will also be examined by calculating Cronbach’s alpha coefficients and item-total and item-remainder correlations.
Discussion: The development of a reliable and validated public stigma scale for Japanese women undergoing infertility treatment will help understand the current state of public stigma. Simultaneously measuring the effectiveness of intervention studies to reduce public stigma toward women undergoing infertility treatment is also important.
1 Introduction
Infertility is the inability to get pregnant despite having unprotected intercourse for 1 year (1). Globally, 186 million people experience infertility (2). According to a survey conducted in Japan in 2021, 22.7% of couples (1 in 4.4) were undergoing or had undergone infertility testing or treatment (3). In Japan, infertility treatment has been covered by insurance since April 2022, and the number of women receiving such treatment is expected to increase.
Approximately half of the women undergoing infertility treatment have symptoms of anxiety, depression, or suspected anxiety or depression (4). Although there are many causes of psychological distress, a higher degree of self-stigma among women undergoing infertility treatment is associated with symptoms of anxiety or depression (4).
Infertility stigma refers to a series of processes in which (1) women undergoing infertility treatment are perceived as deviating from social expectations and are subjected to negative reactions and behaviors by the lay public (public stigma) and (2) they perceive these expectations, reactions, and behaviors (perceived stigma) and internalize these values (self-stigma) (5–7). Therefore, efforts to reduce self-stigma in women undergoing infertility treatment, as well as public stigma against them, are essential for maintaining their mental health (4, 8, 9). According to a Japanese survey in 2022, 20.2% of respondents stated that married couples were socially acceptable only after having a child (10).
Several scales have been developed and validated to measure self-stigma of women undergoing infertility treatment (8, 11, 12). In addition, public stigma scales have been developed for mental illnesses, cancer, HIV/AIDS, and other chronic diseases (13, 14). In the same fields, intervention programs to reduce public stigma have been implemented, including psychoeducation, educational materials, patient contact, and anti-stigma campaigns (videos and media) (13). However, no studies have examined the concept and components of public stigma toward women undergoing infertility treatment. In addition, no measures of public stigma toward this population exist in Japan or worldwide. Therefore, this research protocol describes a plan for the development of the Infertility Public Stigma Scale for Japanese women and the examination of its reliability and validity. This scale is expected to help understand the current state of public stigma toward women undergoing infertility treatment and measure the effectiveness of programs to reduce it.
2 Methods and analysis
This is an exploratory, sequential, mixed-methods study (Figure 1). In this design, qualitative research is followed by quantitative research based on the hypotheses derived from the former (15). This design is suitable for scale development and validation (16). In the qualitative research phase, the constructs and components of public stigma toward women undergoing infertility treatment will be explored through interviews with the Japanese lay population, developing the initial items of the Infertility Public Stigma Scale for Japanese women. This phase is planned between April 2025 and March 2026 (Figure 1). After examining the content validity of the initial scale though expert panel discussions and cognitive interviews (April–August 2026), the psychometric properties of the scale will be examined quantitatively based on the initial items. This phase is expected to be completed by March 2027.
2.1 The qualitative phase: item generation
Multiple procedures are involved in item generation. First, stigma theories were reviewed, and the multidimensional concept of public stigma was extracted. Second, items will be pooled by reviewing previous studies on existing public stigma scales. Third, data will be collected through in-depth, semi-structured interviews. This phase aims to explore the constructs and components of public stigma toward women undergoing infertility treatment in Japan.
2.1.1 Identification of the multidimensional concept of public stigma
Stigma is a multidimensional concept (17). Corrigan et al. (18) identified three components of mental health-related public stigma using social attribution theory. First, stereotyping (cognitions), pertains to beliefs of laypeople regarding the members of the minority group. Second, prejudice (emotional reactions), refers to the endorsement of negative stereotypes by laypeople, resulting in negative emotional reactions. Third, discrimination (behavioral responses), highlights the aspects of harm based on prejudice against the minority group including social distance and interpersonal avoidance. In addition, a fourth component, attitudes toward cultural and institutional context, contributes to deviance (19).
2.1.2 Data collection through literature review
The item pool will be generated through a review of literature on existing scales measuring various illness-related stigmas in laypeople and relevant items. Based on systematic reviews and previous studies (17, 20, 21), illness-related public stigma scales were identified. Supplementary material 1 indicates the studies to be included in the item pool. A total of 722 items from 32 public stigma scale development studies on mental health, HIV/AIDS, leprosy, stroke, cancer, COVID-19, dementia, pregnant smoker, epilepsy, and chronic diseases will be included in the item pool, along with 86 items from three studies that developed scales to measure perceptions of infertility-related stigma, resulting in 808 items from 35 studies. All items extracted from the literature review will be translated into Japanese. Duplicate items and those not easily adaptable to infertility-related situations will be removed. The remaining items will be organized into four categories—cognitions, emotional reactions, behavioral responses, and attitudes toward the cultural and institutional context —based on the identification of the multidimensional concept of public stigma.
2.1.3 Data generation through interviews
To construct more applicable items, we will interview laypeople using a semi-structured open-ended method. An interview guide consisting of open-ended questions will be developed by an expert panel (n = 7; four doctors, one nurse, and two researchers) to identify the components of infertility-related public stigma: cognitions, emotional reactions, behavioral responses, and attitudes toward cultural and institutional contexts. The potential interview outlines include: (1) What do you know about women undergoing infertility treatment? How do you feel about them? (2) Have you ever interacted with a woman undergoing infertility treatment? How were they? How did you feel during these experiences? (3) What do you think are the causes of infertility? (4) What actions do you take toward women undergoing infertility treatment? Do you think they should be treated differently from others? (5) How is infertility regarded in Japanese culture?
Participants will be selected using a purposive sampling with maximum variation in sex, age, occupation, place of residence, medical history, and experience of contact with women with primary or secondary infertility (22). Interviews will be transcribed by RY. Because this phase follows a qualitative research design, the sample size does not need to be determined in advance (22), and participants will be recruited until data saturation is reached (i.e., when no new themes emerge) (22).
2.1.4 Participant characteristics and research setting
We will not use convenience or snowball sampling to recruit participants from across Japan. Laypeople over 20 years enrolled in a Japanese research firm’s database will be invited via email to participate in an interview. After logging in, potential participants will select the study from a list of surveys. If they wish to participate, they will proceed to screening based on eligibility criteria and purposive sampling. The eligible participants will then be sampled to maximize diversity. The inclusion criteria are as follows: (1) individuals over 20 years of age and (2) those who consent to participate in this study. The exclusion criteria are as follows: (1) currently undergoing or having undergone infertility treatment, (2) couples currently undergoing or having undergone infertility testing, (3) couples diagnosed with male factor infertility, (4) individuals with a background or experience in healthcare, and (5) individuals diagnosed with dementia. Eligible participants will be selected using maximum variation sampling based on sex, age, occupation, place of residence, medical history, and contact with women undergoing infertility treatment. Sampled participants will receive an email with the scheduled interview date, time, Zoom meeting ID, and password. Interviews will be conducted individually by RY via Zoom. The older adult may not have access to the Internet. If older participants cannot be recruited through the Japanese research firm’s database, they will be recruited from users of home-visit care providers. When interviewing older adults, obtaining accurate responses is especially important to minimize memory bias. To achieve this, the following strategies will be implemented (23, 24). (1) Minimizing the impact of the interviewer: efforts will be made to reduce the interviewer’s impact. For example, open-ended questions will be asked after closed-ended ones to encourage further elaboration. (2) Using clear, unambiguous and plain language: the interviewer will use expressions that are less ambiguous and less likely to cause misunderstandings. This includes avoiding double-barreled questions, maintaining clear sentence structures, and refraining from using technical terms. (3) Preparing paraphrases in advance: before conducting interviews, alternative phrasing or synonymous expressions will be prepared to enhance clarity and comprehension. (4) Observing facial expressions: during interviews, attention will be paid to participants’ facial expressions to assess their understanding of the questions. (5) Using repetition, summarization, and paraphrasing techniques: these methods will be used to clarify key points and ensure accurate responses. (6) Increasing sample size when necessary: in some cases, the number of participants may be increased.
2.1.5 Data analysis
Qualitative-descriptive methods and inductive thematic analysis will be used in this phase (25–30). A qualitative-descriptive study is a comprehensive summary of events in everyday terms (29). That is, this study will have less abstract findings than other qualitative research methods because they are described in everyday terms (29). Additionally, the qualitative-descriptive research method is suitable for examining people’s reactions (thoughts, feelings, and attitudes) to an event (26). Because the items of the scale use everyday terms and the components of stigma reflect people’s responses, a qualitative-descriptive research method was chosen. We will also use thematic analysis in this phase because it is often used in qualitative-descriptive studies (28). Thematic analysis is the systematic process of identifying patterns in qualitative data (30).
To ensure the rigor of this qualitative-descriptive research, the following techniques will be used to increase the credibility, transferability, dependability, and confirmability of the study (22): purposive sampling, maximum variation sampling, thick description, data (source) triangulation, researcher triangulation, audit trail, and peer review. All data will be analyzed using Microsoft Excel version 2,407.
2.2 Development of the initial items
The results of the literature review and qualitative-descriptive study will be used to create an item pool, which will be reviewed by an expert panel (n = 7; four doctors, one nurse, and two researchers) to create the initial items of the Infertility Public Stigma Scale for Japanese women.
2.2.1 Content validity through expert panel
Content validity will be assessed according to the guidelines and previous research (31–35). In general, expert panels assessing the content validity of a scale consist of 3 to 20 panel members (31). Accordingly, the expert panel of this phrase comprises four doctors, one nurse, two researchers, and two women who had undergone infertility treatment (n = 9). They will engage in a consensus group discussion on grammar conformity, appropriate word choice, word order in each item, and the scoring method to be employed (36). The items will be revised accordingly. The expert panel members will respond to a questionnaire about the essentiality, relevance, clarity of each item, and comprehensiveness of each dimension and the entire instrument. The content validity ratio, item-level content validity index (I-CVI) for relevance and clarity, modified kappa, and scale-level content validity index/average and universal agreement will allow assessment of consensus. Based on these results, the items will be modified or deleted.
2.2.2 Content validity through cognitive interviews
Following the empirical literature (37, 38), this scale will be tested in two or three rounds with seven laypeople, selected using convenience and snowball sampling. This is because the ideal sample size for cognitive interviews assessing content validity ranges from 5 to 15 participants, conducted in two or three rounds (37). Interviews will be conducted using a guide based on previous studies (39, 40) and carried out via the Zoom application. The participants will be interviewed on (1) their general impression of the scale; (2) the comprehensibility of the items; (3) relevance to laypeople’s cognitive, emotional, and behavioral reactions; (4) the comprehensiveness of the items; (5) suggested revisions; and (6) appropriateness of the response options. Accordingly, the scale or items will be modified or deleted.
2.3 The quantitative phase: scale validation
The quantitative phase will examine the reliability and validity of the Infertility Public Stigma Scale for Japanese women, including structural validity, internal consistency, inter-rater reliability, and known-groups, convergent, and discriminant validity.
2.3.1 Participants and recruitment procedure
A cross-sectional study based on an online survey of laypeople will be conducted to examine the scale’s reliability and validity. The participants will be recruited from a Japanese research firm’s database of individuals over 20 years old. Potential participants will be invited via email and screened to determine eligibility if they wish to participate. Eligible individuals will respond to a questionnaire on the company’s website. The inclusion criteria will be as follows: (1) individuals over 20 years old and (2) those who have consented to participate in this study. Exclusion criteria will be as follows: (1) individuals currently undergoing or who have undergone infertility treatment, (2) couples currently undergoing or those who have undergone infertility testing, (3) couples diagnosed with male factor infertility, (4) individuals with a background or experience in healthcare, and (5) individuals diagnosed with dementia.
Convenience sampling will be used to recruit both male and female participants of diverse ages in order to represent the Japanese population. Older adult may not have access to the Internet. If it is not possible to recruit elderful individuals from the databases of the Japanese research firm, they will be recruited from users of home-visit care providers. To examine the reliability and validity of the scale, 10–15 participants are needed per candidate item (41). Therefore, the target sample size will be calculated by multiplying the number of candidate items by 10–15.
2.3.2 Data collection
Data will be collected on sociodemographics, health status, contact with women undergoing infertility treatment, and fertility knowledge.
Sociodemographic factors and health status will include age, sex, education, occupation, annual household income, residential area, medical history, and contact with women having primary or secondary infertility.
In addition, we will collect data using the Japanese version of the Cardiff Fertility Knowledge Scale (CFKS-J) (42), developed by Maeda et al. The original version was developed by Bunting et al. (43). The CFKS-J consists of 13 items that measure risks for reduced fertility, misconceptions about fertility, and basic facts about infertility, with each item rated on a 3-point scale.
2.3.3 Data analysis
The data will be analyzed using the R version 4.4.1 for Windows. Statistical significance will be set at p < 0.05. Descriptive statistics of means, percentages, and standard deviations (SD) will be calculated for sociodemographic factors and health status.
2.3.3.1 Item exclusion criteria
We will remove items that show either ceiling or floor effects. We will also remove the items if item-total and item-remainder correlations are below 0.4 or above 0.85. Items with factor loadings less than 0.4 in the exploratory factor analysis will be considered for deletion.
2.3.3.2 Examination of the structural validity
Exploratory factor analysis will be conducted to examine the structural validity of the Infertility Public Stigma Scale for Japanese women. After confirming the factor numbers using a scree plot, we will check whether the data are multivariate normally distributed, using Mardia’s kurtosis test, and determine the extraction method accordingly (44). In addition, a confirmatory factor analysis will be conducted based on the results of the exploratory factor analysis. The extraction method will be determined based on whether the data follows a multivariate normal distribution (45). A chi-square statistic / degrees of freedom less than or equal to 3 will be considered appropriate (46). In addition, a good fit will be considered if (1) the goodness of fit index, comparative fit index, Tucker-Lewis index, adjusted goodness of fit index, and normed fit index are greater than or equal to 0.95 and (2) the root mean square error of approximation and standardized root mean square residual are less than or equal to 0.05 (47–49).
2.3.3.3 Examination of reliability
To examine internal consistency, Cronbach’s alpha coefficients, as well as item-total and item-remainder correlations, will be calculated. A Cronbach’s alpha coefficients greater than 0.7 will be considered optimal (50). To assess test–retest reliability, we will administer the Infertility Public Stigma Scale to more than 50% of the participants 3 days after the initial survey (33). If the data follow a normal distribution, we will calculate an intraclass correlation coefficient based on the Infertility Public Stigma Scale scores at baseline and after 3 days (51).
2.3.3.4 Examination of the known-groups, convergent, and discriminant validity
A known-groups comparison will be conducted using a t test if the data follow a normal distribution. We assume that the mean scores for individuals aged 60 and older will be higher than that for those who are younger (3).
To examine convergent validity, Pearson’s correlation coefficient will be calculated between the Infertility Public Stigma Scale and the CFKS-J. In the context of mental illness, stereotyping arises when responsibility for the illness is attributed to the individual and they are blamed (18). Therefore, we expect a significant positive correlation coefficient between infertility public stigma and the CFKS-J.
Convergent and discriminant validity will be assessed using a multitrait-scaling analysis. Convergent validity is sustained if modest correlation of 0.4 or greater is observed between an item and its own scale (51). Discriminant validity is sustained when the correlation between an item and its own scale is higher than the item’s correlation with other scales (51). Scaling errors and successes will then be calculated (51).
3 Discussion
This protocol article described a plan for the development of the Infertility Public Stigma Scale for Japanese women and the examination of its reliability and validity. This study will describe the concept and components of public stigma toward infertile patients and develop the Infertility Public Stigma Scale for Japanese women. The results of this study are expected to accelerate our understanding of the situation faced by women undergoing infertility treatment and contribute to the development of programs aimed at reducing public stigma toward them. The results of this study (scale development) are expected to be academically significant, as they can be used to measure the effectiveness of programs aimed at reducing public stigma of infertility. Furthermore, the need to reduce public stigma regarding infertility may be revealed by determining its extent.
3.1 Limitations
This study has some limitations. Participants in the interviews conducted during the qualitative phase of this study will be recruited from online research firm monitors. Participant selection and sampling biases must be considered when interpreting the findings of this study. However, the ability to collect data from both men and women across Japan allows for sampling with maximum variation. Second, the nature of the participant recruitment process for the assessment of the scale’s reliability and validity may introduce participant selection and sampling bias. Despite these limitations, this study will be the first to examine the reliability and validity of the Infertility Public Stigma Scale for Japanese women.
Ethics statement
The study will be conducted according to the guidelines of the Declaration of Helsinki and the Ethical Guidelines for Medical and Biological Research Involving Human Subjects issued by the Japanese Government (52). The qualitative phase of this study design was approved by the Ethics Committee of Hoshi University, Tokyo, Japan (approval number: 2024-19, 27 August 2024). To ensure voluntary participation based on informed consent, we will provide prospective participants with a prior explanation covering the following aspects: (1) the purpose of the research, (2) the study methods, (3) potential benefits and risks, (4) measures to protect participants’ privacy, and (5) the voluntary nature of participation. To protect participants’ privacy, we will analyze anonymized data with direct identifiers removed. When publishing our findings, we will present the results in a way that ensures individual participants cannot be identified. To minimize respondent burden, we will carefully evaluate their physical and mental condition. Furthermore, we will inform them in advance that they may withdraw from participation if the burden is too great.
Author contributions
RY: Conceptualization, Funding acquisition, Methodology, Project administration, Writing – original draft. TO: Conceptualization, Methodology, Writing – review & editing. HO: Conceptualization, Methodology, Writing – review & editing. EF: Writing – review & editing. RS: Writing – review & editing. TA: Writing – review & editing. HK: Writing – review & editing. TK: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work has been supported by the JSPS KAKENHI under grant number 24K20135.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. The generated AI (GPT-4 version of ChatGPT) was used only for language editing in a small portion of this article.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1504842/full#supplementary-material
References
1. Anderson, K, Norman, RJ, and Middleton, P. Preconception lifestyle advice for people with subfertility. Cochrane Database Syst Rev. (2010) 4:CD008189. doi: 10.1002/14651858.CD008189.pub2
2. Inhorn, MC, and Patrizio, P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. (2015) 21:411–26. doi: 10.1093/humupd/dmv016
3. National Institute of Population and Social Security Research. Marriage and childbirth in Japan today: the sixteenth Japanese national fertility survey, 2021 (results of singles and married couples survey) (2023). Available online at: https://www.ipss.go.jp/ps-doukou/j/doukou16/JNFS16_reportALL.pdf [Accessed September 17, 2024]
4. Yokota, R, Okuhara, T, Okada, H, Goto, E, Sakakibara, K, and Kiuchi, T. Association between stigma and anxiety, depression, and psychological distress among Japanese women undergoing infertility treatment. Healthcare. (2022) 10:1300. doi: 10.3390/healthcare10071300
5. Goffman, E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ, USA: Prentice Hall (1963).
6. Kashihara, J, Kawai, T, and Umegaki, Y. A comprehensive review of research on stigmatizing attitudes toward depression: proposing the use of implicit measures for future investigation. Jap Psychol Rev. (2014) 57:455–71. doi: 10.24602/sjpr.57.4_455
7. Corrigan, PW, and Watson, AC. The paradox of self-stigma and mental illness. Clin Psychol Sci Pract. (2002) 9:35–53. doi: 10.1093/clipsy.9.1.35
8. Yokota, R, Okada, H, Okuhara, T, Goto, E, Furukawa, E, Shirabe, R, et al. Development of the Japanese version of the infertility stigma scale: examination of its reliability and validity. Healthcare. (2022) 10:505. doi: 10.3390/healthcare10030505
9. Yokota, R, Okuhara, T, Okada, H, Goto, E, Sakakibara, K, and Kiuchi, T. Associations between stigma, cognitive appraisals, coping strategies and stress responses among Japanese women undergoing infertility treatment. Healthcare. (2022) 10:1907. doi: 10.3390/healthcare10101907
10. National Institute of Population and Social Security Research. The 7th National Survey on family in Japan, 2022. (2024). Available online at: https://www.ipss.go.jp/ps-katei/j/NSFJ7/Mhoukoku/kateidoukou7_kekka_20240426.pdf [Accessed September 17, 2024]
11. Fu, B, Qin, N, Cheng, L, Tang, G, Cao, Y, Yan, C, et al. Development and validation of an infertility stigma scale for Chinese women. J Psychosom Res. (2015) 79:69–75. doi: 10.1016/j.jpsychores.2014.11.014
12. Taebi, M, Kariman, N, Montazeri, A, Alavi Majd, H, and Jahangirifar, M. Development and psychometric properties of female infertility stigma instrument (ISI-F): a sequential mixed method study. BMC Womens Health. (2022) 22:557. doi: 10.1186/s12905-022-02139-5
13. Walsh, DAB, and Foster, JLH. A Call to action. A critical review of mental health related anti-stigma campaigns. Front Public Health. (2020) 8:569539. doi: 10.3389/fpubh.2020.569539
14. Wan, M, Tan, Y, Huang, Y, Zhang, Q, Qin, F, Sun, X, et al. Development and psychometric evaluation of public stigma of stroke scale (PSSS). Sci Rep. (2023) 13:545. doi: 10.1038/s41598-023-27504-8
15. Creswell, JW, and Creswell, JD. Research design - qualitative, quantitative, and mixed methods approaches. Fifth ed. Los Angeles, USA: Sage Publication, Inc. (2018).
16. Creswell, JW, and Plano Clark, VL. Designing and conducting mixed methods research. Third ed. Los Angeles, USA: Sage Publications, Inc. (2017).
17. Marlow, LA, and Wardle, J. Development of a scale to assess cancer stigma in the non-patient population. BMC Cancer. (2014) 14:285. doi: 10.1186/1471-2407-14-285
18. Corrigan, P, Markowitz, FE, Watson, A, Rowan, D, and Kubiak, MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. (2003) 44:162–79. doi: 10.2307/1519806
19. Visser, MJ, Kershaw, T, Makin, JD, and Forsyth, BW. Development of parallel scales to measure HIV-related stigma. AIDS Behav. (2008) 12:759–71. doi: 10.1007/s10461-008-9363-7
20. Kaushik, A, Kostaki, E, and Kyriakopoulos, M. The stigma of mental illness in children and adolescents: a systematic review. Psychiatry Res. (2016) 243:469–94. doi: 10.1016/j.psychres.2016.04.042
21. Rodríguez-Rivas, ME, Cangas, AJ, Cariola, LA, Varela, JJ, and Valdebenito, S. Innovative technology-based interventions to reduce stigma toward people with mental illness: systematic review and Meta-analysis. JMIR Serious Games. (2022) 10:e35099. doi: 10.2196/35099
22. Liamputtong, P. Qualitative research methods. Fifth ed. South Melbourne, Australia & New Zealand: Oxford Univiversity Press (2019).
23. West, M, Bondy, E, and Hutchinson, S. Interviewing institutionalized elders: threats to validity. Image J Nurs Sch. (1991) 23:171–6. doi: 10.1111/j.1547-5069.1991.tb00664.x
25. Bradshaw, C, Atkinson, S, and Doody, O. Employing a qualitative description approach in health care research. Glob Qual Nurs Res. (2017) 4:2333393617742282. doi: 10.1177/2333393617742282
26. Sandelowski, M. Whatever happened to qualitative description? Res Nurs Health. (2000) 23:334–40. doi: 10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G
27. Guest, G, MacQueen, KM, and Namey, EE. Applied thematic analysis. Calfornia, USA: Sage Publications, Inc. (2012).
28. Sandelowski, M. What’s in a name? Qualitative description revisited. Res Nurs Health. (2010) 33:77–84. doi: 10.1002/nur.20362
29. Greg, G, Asahara, K, and Yokoyama, M. How to conduct and summarize qualitative research: Toward expertise in nursing research. Second ed. Tokyo, Japan: Ishiyaku Publishers, Inc. (2016).
31. Almanasreh, E, Moles, R, and Chen, TF. Evaluation of methods used for estimating content validity. Res Social Adm Pharm. (2019) 15:214–21. doi: 10.1016/j.sapharm.2018.03.066
32. Caruso, R, Arrigoni, C, Groppelli, K, Magon, A, Dellafiore, F, Pittella, F, et al. Italian version of Dyspnoea-12: cultural-linguistic validation, quantitative and qualitative content validity study. Acta Biomed. (2018) 88:426–34. doi: 10.23750/abm.v88i4.6341
33. Mokkink, LB, Prinsen, CA, Patrick, DL, Alonso, J, Bouter, LM, De Vet, HC, et al. COSMIN study design checklist for patient-reported outcome measurement instruments (2019). Available online at: https://www.cosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdf. Accessed September 17, 2024
34. Polit, DF, and Beck, CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. (2006) 29:489–97. doi: 10.1002/nur.20147
35. Rodrigues, IB, Adachi, JD, Beattie, KA, and MacDermid, JC. Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis. BMC Musculoskelet Disord. (2017) 18:540. doi: 10.1186/s12891-017-1914-5
36. Zamanzadeh, V, Ghahramanian, A, Rassouli, M, Abbaszadeh, A, Alavi-Majd, H, and Nikanfar, AR. Design and implementation content validity study: development of an instrument for measuring patient-centered communication. J Caring Sci. (2015) 4:165–78. doi: 10.15171/jcs.2015.017
37. Boateng, GO, Neilands, TB, Frongillo, EA, Melgar-Quiñonez, HR, and Young, SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. (2018) 6:149. doi: 10.3389/fpubh.2018.00149
38. Willis, GB. Cognitive interviewing: A tool for improving questionnaire design. Thousand Oaks, CA, USA: Sage (2005).
39. Collins, D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. (2003) 12:229–38. doi: 10.1023/a:1023254226592
40. Irwin, DE, Varni, JW, Yeatts, K, and DeWalt, DA. Cognitive interviewing methodology in the development of a pediatric item bank: a patient reported outcomes measurement information system (PROMIS) study. Health Qual Life Outcomes. (2009) 7:3. doi: 10.1186/1477-7525-7-3
41. Nochaiwong, S, Ruengorn, C, Awiphan, R, Kanjanarat, P, Ruanta, Y, Phosuya, C, et al. COVID-19 public stigma scale (COVID-PSS): development, validation, psychometric analysis and interpretation. BMJ Open. (2021) 11:e048241. doi: 10.1136/bmjopen-2020-048241
42. Maeda, E, Sugimori, H, Nakamura, F, Kobayashi, Y, Green, J, Suka, M, et al. A cross-sectional study on fertility knowledge in Japan, measured with the Japanese version of Cardiff fertility knowledge scale (CFKS-J). Reprod Health. (2015) 12:10. doi: 10.1186/1742-4755-12-10
43. Bunting, L, Tsibulsky, I, and Boivin, J. Fertility knowledge and beliefs about fertility treatment: findings from the international fertility decision-making study. Hum Reprod. (2013) 28:385–97. doi: 10.1093/humrep/des402
44. Toyoda, H. Introduction to factor analysis: Latest data analysis using R. Tokyo, Japan: Tokyo Tosho Co., Ltd. (2012).
45. Toyoda, H. Covariance structure analysis- structural equation modeling using R. Tokyo, Japan: TokyoTosho Co., Ltd (2014).
46. Kwon, MY, and Kim, NY. Validity and reliability of a Korean version of the ConCom safety management scale. Int J Environ Res Public Health. (2021) 18:12514. doi: 10.3390/ijerph182312514
47. Çapık, A, Aksoy, M, Yılmaz, E, and Yılmaz, F. Infertility stigma scale: a psychometric study in a Turkish sample. Perspect Psychiatr Care. (2019) 55:328–35. doi: 10.1111/ppc.12360
48. Toyoda, H. Covariance structure analysis [Q&a]-structural equation modeling. Tokyo, Japan: Asakura Publishing Co., Ltd. (2003).
49. Asano, H, Suzuki, T, and Kojima, T. Introduction to covariance structure analysis in practice. Tokyo, Japan: Kodansha Ltd. (2005).
50. Terwee, CB, Bot, SD, de Boer, MR, van der Windt, DA, Knol, DL, Dekker, J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
51. Fayers, PM, and Machin, D. Quality of life: Assessment, analysis and interpretation. West Sussex, UK: John Wiley & Sons Ltd. (2000).
52. Ministry of Education, Culture, Sports, Science and Technology, Ministry of Health, Labour and Welfare, Ministry of Economy, Trade and Industry. (2021) Ethical guidelines for medical and biological research involving human subjects. Available online at: https://www.mext.go.jp/a_menu/lifescience/bioethics/seimeikagaku_igaku.html [Accessed March 29, 2025]
Keywords: infertility, public stigma, scale development, exploratory sequential mixed method study, validity, reliability, psychometric evaluation, health communication
Citation: Yokota R, Okuhara T, Okada H, Furukawa E, Shirabe R, Agawa T, Kato H and Kiuchi T (2025) Development and psychometric evaluation of the Infertility Public Stigma Scale for Japanese women: protocol for an exploratory sequential mixed method study of the Japanese population. Front. Public Health. 13:1504842. doi: 10.3389/fpubh.2025.1504842
Edited by:
Christos Theleritis, University General Hospital Attikon, GreeceReviewed by:
Keerti Singh, The University of the West Indies, Cave Hill, BarbadosBenjamin Salvador Simon, Autonomous University of Nuevo Leon, Mexico
Copyright © 2025 Yokota, Okuhara, Okada, Furukawa, Shirabe, Agawa, Kato and Kiuchi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rie Yokota, eW9rb3RhLnJpZUBob3NoaS5hYy5qcA==
 Rie Yokota
Rie Yokota Tsuyoshi Okuhara
Tsuyoshi Okuhara Hiroko Okada
Hiroko Okada Emi Furukawa3
Emi Furukawa3