- 1Shandong Public Health Clinical Center, Shandong University, Jinan, Shandong, China
- 2Department of Psychiatry, Shandong Mental Health Center, Shandong University, Jinan, Shandong, China
Objectives: The isolation treatment and special care of COVID-19 patients expose frontline healthcare workers (HCWs) involved in treatment to more risks of infection exposure. Therefore, investigating the current status of personal protection KAP of HCWs in isolation wards and its influencing factors will be helpful in improving personal protection in major public health events.
Methods: Research data came from COVID-19 designated medical institutions in Shandong Province from October to December 2022, and were collected through questionnaire surveys. The questionnaire is self-designed and composed of general information questionnaire, KAP questionnaire and anxiety and depression questionnaire. Univariate factor analysis and multiple linear regression analysis were used to study the influencing factors of KAP of the research subjects.
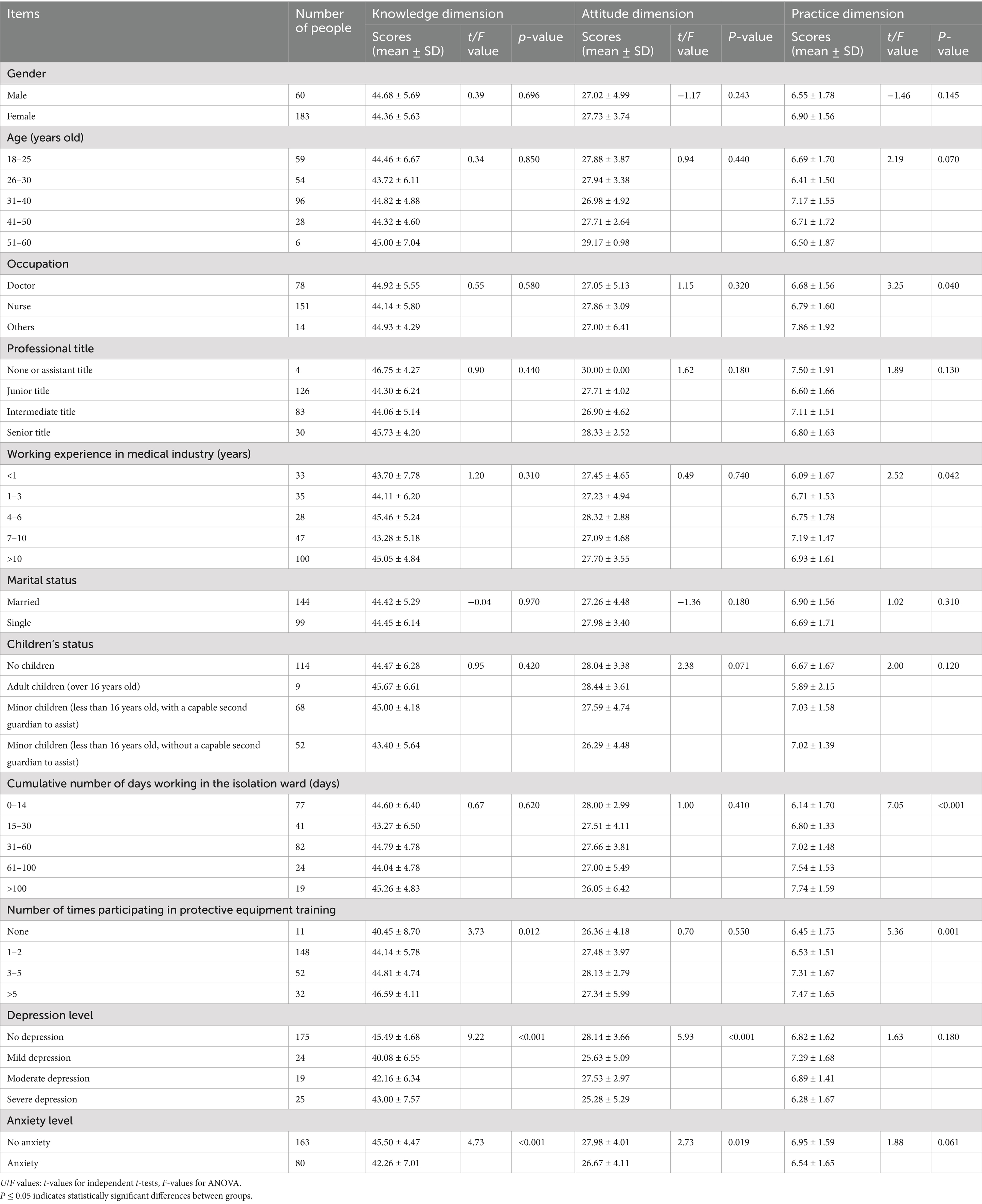
Results: In terms of KAP Scores, the mean knowledge score was 6.82 ± 1.6, with 85.60% scoring at a medium level or below. The attitude mean score was 27.56 ± 4.1, and 78.60% held a favorable disposition toward personal protection measures. For practice, the mean score was 44.44 ± 5.6, with approximately 30.86% demonstrating room for improvement. Univariate analysis indicated significant differences in knowledge scores among HCWs with varying numbers of personal protective equipment (PPE) trainings and levels of depression and anxiety (p ≤ 0.05). Attitude scores differed significantly based on depression and anxiety levels (p ≤ 0.05). Practice scores varied significantly according to occupation, work experience, cumulative working time in isolation wards, and PPE training frequency (p ≤ 0.05). Multiple linear regression analysis revealed that increased PPE training frequency (β = 0.168, p = 0.007) and lower anxiety levels (β = −0.256, p ≤ 0.001) were associated with higher knowledge scores. Depression levels (β = −0.208, p = 0.001) were negatively associated with attitudes. Longer medical experience (β = 0.132, p = 0.029), more cumulative working time in isolation wards (β = 0.310, p ≤ 0.001), and lower anxiety levels (β = −0.129, p = 0.034) positively influenced practice scores.
Conclusion: In summary, for HCWs in isolation wards, increasing the frequency of protective training and reducing anxiety will improve their personal protection knowledge; alleviating depression will cultivate a positive attitude toward personal protection; and relieving anxiety, along with longer job tenure and working hours, were associated with enhanced protective behaviors.
Introduction
The emergence of COVID-19 in late 2019 has presented a significant challenge to the global healthcare system. The pandemic’s case fatality rate is estimated at approximately 1–3% (1), surpassing that of SARS and general influenza viruses (2). Unprecedentedly, stringent social distancing measures have been universally implemented worldwide to combat the outbreak. In response to this unprecedented crisis, numerous countries have established specialized hospitals dedicated to providing comprehensive care for patients with COVID-19. These medical facilities incorporate designated isolation wards aimed at curtailing viral transmission and safeguarding healthcare professionals from potential infections (3).
The COVID-19 pandemic has significantly increased the challenges and risks faced by frontline healthcare workers (HCWs), and it is imperative to implement effective personal protective measures in COVID-19 isolation wards to reduce nosocomial infection. Investigations have shown that the relative risk of developing COVID-19 is related to factors such as PPE, occupation, and exposure (4). Globally, studies from European settings have corroborated similar challenges. A German study by Müller et al. (5) found 68% of dentists faced difficulties implementing COVID-19 protocols, highlighting universal training needs (5). Furthermore, Polish research by Malczynska et al. (6) revealed 42% HCWs developed PPE-related dermatoses, demonstrating cross-regional occupational health impacts. The KAP model, encompassing Knowledge (understanding of disease transmission mechanisms/prophylactic protocols), Attitude (willingness to adopt and improve preventive behaviors), and Practice (consistent adherence to infection control measures), due to its feasibility and effectiveness, has been widely applied in nosocomial infection control research (7–9). Previous studies have demonstrated that inadequate knowledge and negative attitudes toward PPE protocols are associated with suboptimal adherence in high-risk clinical settings (10). However, there is still a lack of research on the KAP of HCWs, especially those working in the COVID-19 isolation wards.
HCWs faced challenges in PPE compliance, with only 54.9% consistently using PPE in the Democratic Republic of the Congo (11) and 13.8% correctly donning PPE in Saudi Arabia (12). These gaps reflect KAP disconnects adequate knowledge but poor attitudes and practices, demonstrating incomplete translation of knowledge into action. Given the unique nature of COVID-19 and the demands on specialized care, it is critical to understand the current status of personal protection KAP among HCWs in isolation wards of designated hospitals for COVID-19, focusing on the HCWs directly involved in patient care. This study investigated these aspects to determine the factors that influence HCWs’ adherence to personal protective measures. The findings of this study will help develop effective strategies to promote personal protective measures in these settings, ultimately improving HCWs’ safety and helping prevent the spread of COVID-19.
Methods
Research participants
The study employed a cross-sectional design, recruiting a sample of 243 HCWs from the isolation ward of a designated hospital for COVID-19 treatment in Shandong Province between October and December 2022, including doctors, both registered and assistant nurses, and other medical professionals from supporting departments (laboratory, radiology and infection control specialists). Convenience sampling method was utilized to enroll participants who met the inclusion criteria, which encompassed (1) medical and related personnel engaged in close-loop work within isolation wards, and (2) voluntary willingness to participate in the study. Exclusion criteria were applied to staff not subjected to closed-loop management (i.e., personnel not residing in designated accommodations or permitted unrestricted movement outside isolation wards).
Research measures
(1) General information questionnaire: designed by the researchers, including various potential influencing factors on KAP, such as gender, age, professional title, working years, type of work, marital status, children’s status, frequency of hospital infection prevention training, etc. (Appendix 2). (2) KAP questionnaire: based on the theory of KAP, referring to relevant literature at home and abroad, and referring to the “Prevention and Control Plan of COVID-19 Disease (Third Edition)” and other relative national standards, combined with the discussion of the research group, and then through expert consultation and pre-survey, the formal questionnaire was gradually modified (Appendix 3). (3) Anxiety and depression questionnaire: the Chinese version of Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) were used to evaluate the mental health status of the HCWs in the isolation ward (Appendix 4). The design and reporting of this study followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
The knowledge dimension consisted of 10 multiple choice questions, encompassing the fundamental principles of personal protection, intricate details regarding protective clothing, and the selection process for protective equipment. A correct response was awarded 1 point, while an incorrect answer received 0 points, resulting in a maximum score of 10. The attitude dimension comprised 6 multiple choice questions that gauged individuals’ attitudes toward personal protection knowledge and skills, their perspective on training programs, as well as their commitment to implementing personal protection measures. The Likert scale with a range of 1 to 5 points was employed to assess responses from “strongly disagree” to “strongly agree,” yielding an overall score between 6 and 30. A higher score indicated a more positive attitude. The practice dimension included 10 multiple choice questions primarily focusing on active learning and practical application of personal protection-related knowledge and skills. The Likert scale with values ranging from 1 to 5 assigned scores corresponding to “never,” “occasionally,” “sometimes,” “often,” and “always” respectively. The total score ranged from 10 to 50, with a higher score indicating better adherence to desired behaviors. The standard score for each dimension is calculated by dividing the average score by the full score and multiplying it by 100. An excellent standard score is above 85, a moderate score ranges from 60 to 85, and a poor score is below 60.
Depressive status was assessed using the BDI. According to the rating criteria of the scale, scores ranging from 0 to 4 were categorized as absence of depression, scores between 5 and 13 indicated mild depression, scores between 14 and 20 denoted moderate depression, while scores ≥ 21 represented severe depression. Anxiety status was evaluated using the BAI, based on the assessment guidelines of this scale, a score of ≥45 indicated anxiety, whereas a score below <45 indicated no presence of anxiety.
The questionnaire content was evaluated by seven specialists in hospital infection management, resulting in a content validity index of 0.946. To ensure the reliability and validity of the questionnaire, a pre-survey was conducted with 20 isolation ward HCWs who met the inclusion and exclusion criteria. The Cronbach’s α coefficients for knowledge, attitude, and practice dimensions were found to be 0.749, 0.942, and 0.862 respectively; yielding a total Cronbach’s α coefficient of 0.894 for the questionnaire along with a retest reliability coefficient of 0.798. Previous studies have demonstrated good reliability and validity for Chinese versions of BAI and BDI (13, 14), thus further calculations were deemed unnecessary.
Data collection
Data collection was conducted using an online tool called ‘Wenjuanxing’ to create the questionnaire and generate a two-dimensional code image for distribution. The principal investigator of this study communicated with the department head and head nurse of the selected hospital to clarify the target population, research objectives, survey methodology, and informed consent considerations. Strict adherence to scientific research rules was maintained throughout. The questionnaire was administered anonymously with informed consent from participants, and a one-week timeframe was agreed upon for data retrieval. All questions were designated as mandatory, allowing only one response per IP address. A total of 300 questionnaires were distributed, resulting in 271 responses. After excluding incorrect or invalid responses, 243 valid questionnaires were obtained, yielding an effective response rate of 89.67%. The high response rate can be attributed to two factors: firstly, the occupational health survey was required in the closed-loop management policy at that time. Secondly, mobile based questionnaires allowed for real-time completion during work breaks, minimizing non-response bias to the greatest extent possible.
Statistical analysis
The outcome variables of this study included the knowledge dimension, assessed through a 10-item multiple-choice questionnaire; the attitude dimension, evaluated using a 6-item Likert scale questionnaire; and the practice dimension, measured with a 10-item Likert scale questionnaire. Exposure variables were the frequency of PPE training, years of work experience, cumulative working time in isolation wards, and levels of depression and anxiety. Potential confounders such as gender, age, profession, professional title, marital status, and parental status were considered in the univariate analysis. Multiple linear regression analysis was used to control for these confounders, focusing on the significant variables identified in the univariate analysis.
The data was imported into Excel and a database was established, which underwent a rigorous accuracy check by two individuals. Analysis was conducted using SPSS 22.0 software. Count data were described in terms of frequency and percentage (%), while normally distributed measurement data were expressed as mean ± standard deviation. Group comparisons were performed using either the two independent samples t-test or one-way analysis of variance. Multiple linear regression was employed to analyze the factors influencing personal protection KAP among HCWs in isolation wards of designated hospitals. Statistical significance was determined at p ≤ 0.05.
Results
Demographic characteristics of participants
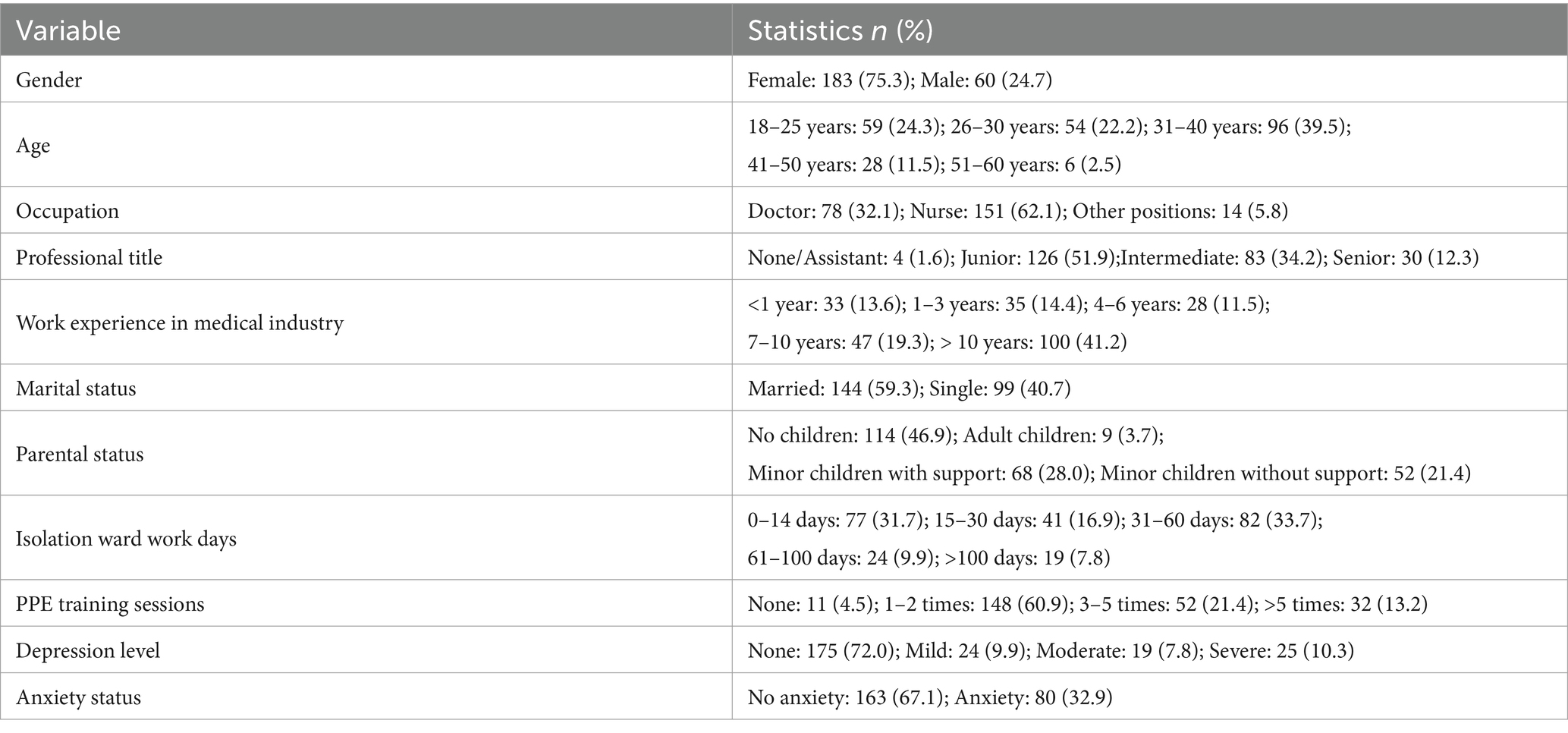
A total of 243 HCWs from COVID-19 isolation wards participated in this study. Key demographic and occupational characteristics are summarized in Table 1. The cohort predominantly comprised nurses (62.1%) and doctors (32.1%), with 41.2% having over 10 years of medical experience. Most participants (60.9%) attended 1–2 PPE training sessions, while 13.2% received more than 5 trainings. Psychological assessments revealed that 32.9% experienced anxiety, and 28% reported varying degrees of depression (10.3% severe). Factors significantly linked to KAP outcomes, including work experience, cumulative days in isolation wards, training frequency, and mental health status, are analyzed in subsequent sections. For additional details (e.g., age distribution, marital status, parental status), refer to Table 1.
The current status of personal protection KAP and psychological state
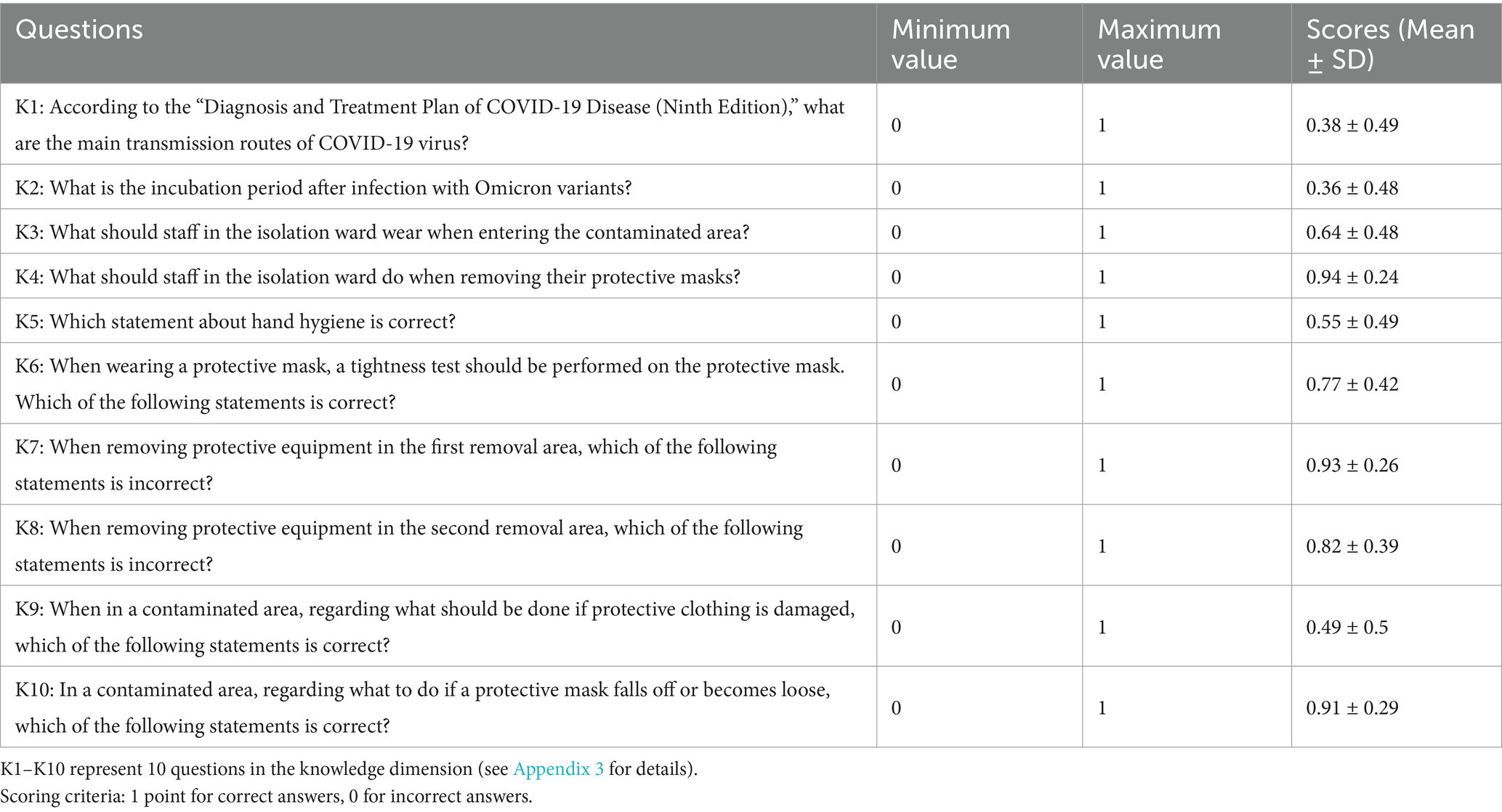
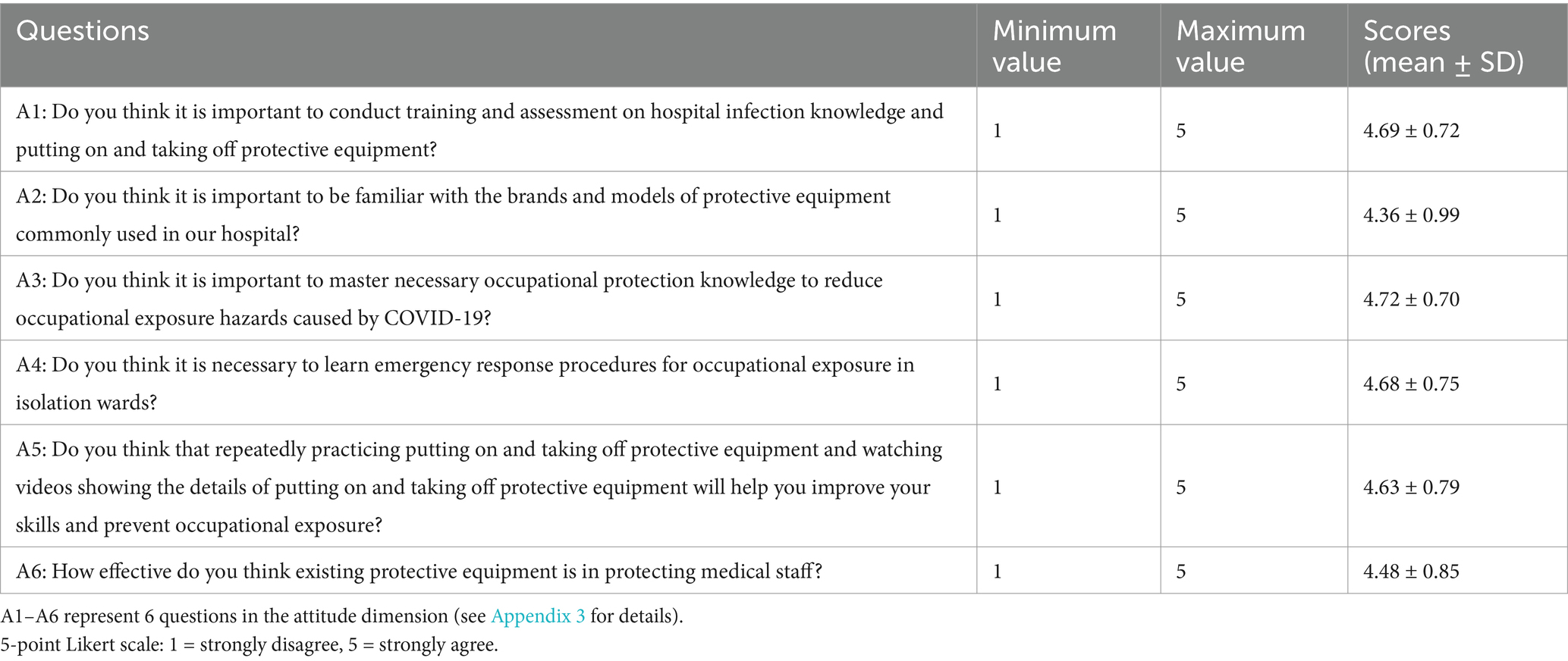
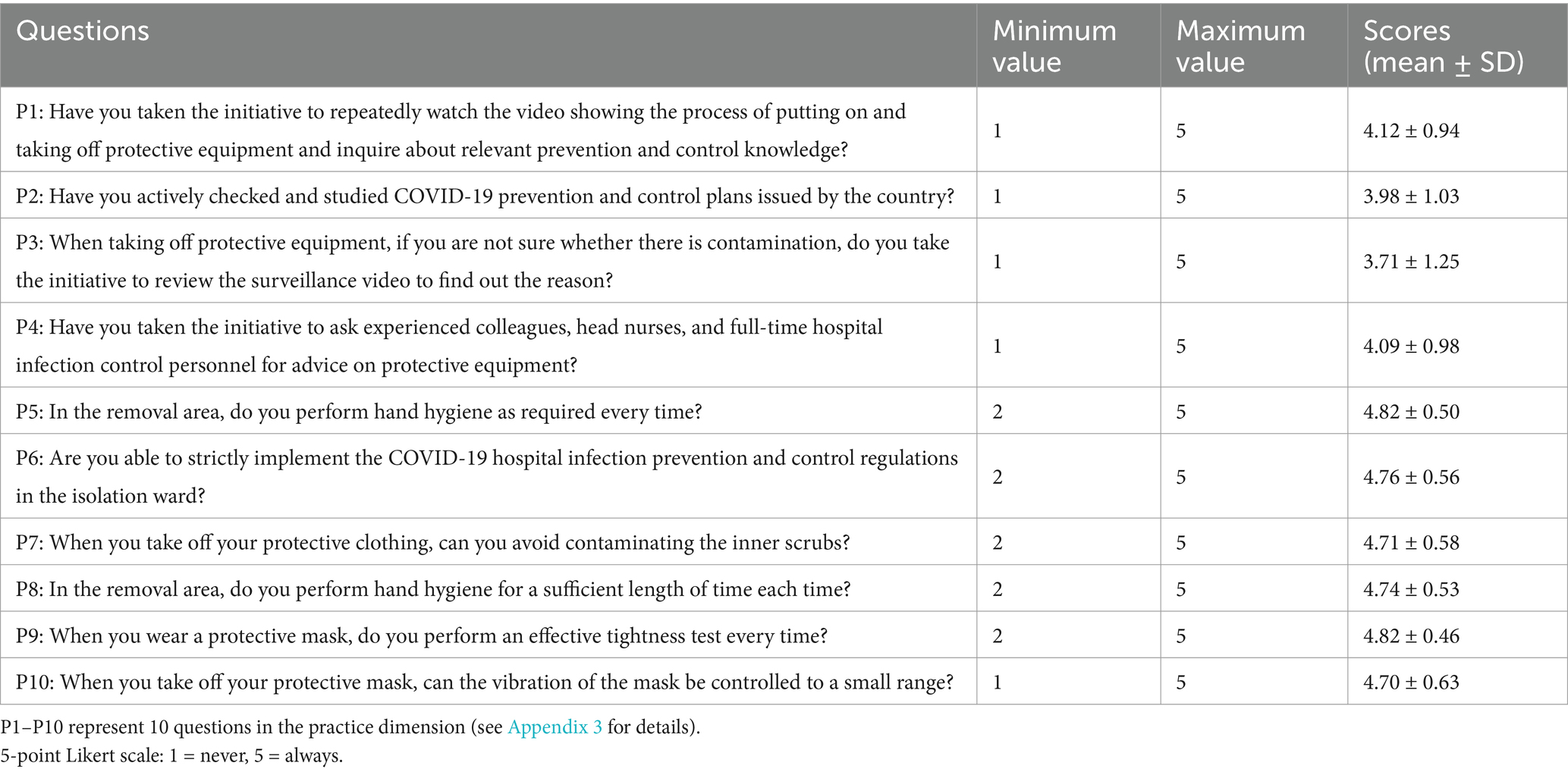
In the study, the knowledge dimension included 10 multiple-choice questions (0–10 points: 1 = correct, 0 = incorrect). The attitude dimension used a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), totaling 6–30 points. The practice dimension also employed a 5-point Likert scale (1 = never to 5 = always), with a range of 10–50 points. In the study, it was observed that the mean score for the dimension of personal protection knowledge among 243 workers was 6.82 ± 1.6, with a range from 2 to 10. Among them, a majority of 208 workers (85.60%) exhibited a moderate or lower level of knowledge in this domain. The mean score for the dimension of personal protection attitude was found to be 27.56 ± 4.1, ranging from 6 to 30, with approximately 52 individuals (21.40%) demonstrating a moderate or lower level of attitude toward personal protection practice. Furthermore, the mean score for the dimension of personal protection practice was determined as 44.44 ± 5.6, ranging from 20 to 50; within this group, around 75 participants (30.86%) displayed a moderate or lower level of adherence to recommended protective behaviors. The specific scores of each item are shown in Tables 2–4.
Univariate factor analysis of influencing factors of personal protection KAP
The results of the univariate analysis indicated significant differences in knowledge dimension scores among HCWs with varying numbers of protective equipment trainings and degrees of depression and anxiety (p ≤ 0.05). Attitude dimension scores also showed significant differences among HCWs with different levels of depression and anxiety (p ≤ 0.05). Furthermore, practice dimension scores exhibited significant differences among HCWs with diverse occupations, years of work experience, cumulative working time in isolation wards, and number of protective equipment trainings received (p ≤ 0.05). The specific analysis results are shown in Table 5.
Multiple linear regression analysis of influencing factors on personal protection KAP
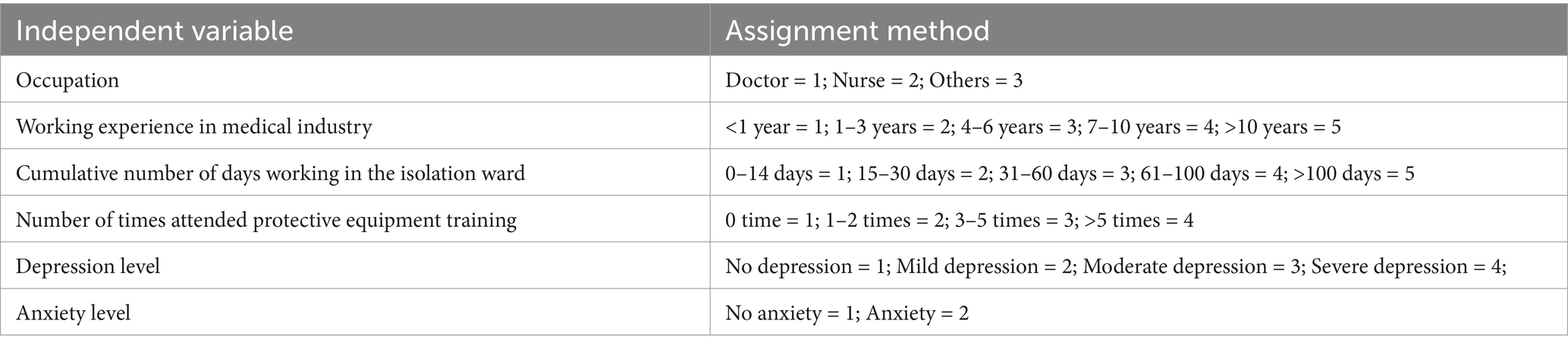
Multiple linear regression analysis was conducted using the KAP scores of HCWs in isolation wards as the independent variable. The independent variables for non-linear regression analysis were selected based on statistically significant differences observed in univariate analysis (αin = 0.05, αout = 0.10). The specific assignment method is described in detail in Table 6.
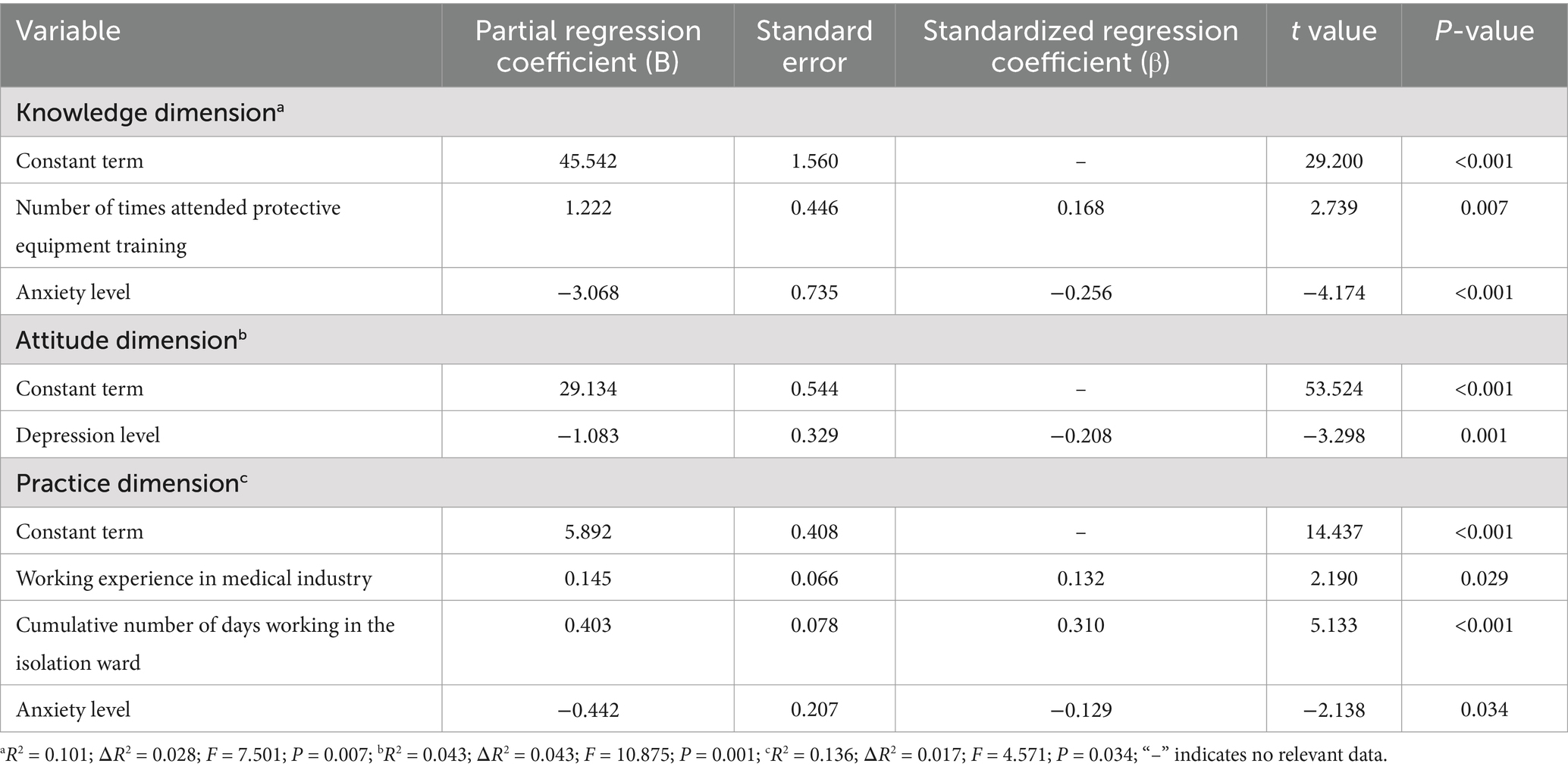
The multiple linear regression analysis identified statistically significant associations between predictors and KAP dimensions. For the knowledge dimension, each additional PPE training session was associated with a 1.222-point increase in knowledge scores (β = 0.168, p = 0.007). Higher anxiety levels showed a negative correlation with knowledge scores, with each unit increase in anxiety reducing scores by 3.068 points (β = −0.256, p < 0.001). In the attitude dimension, greater depression severity was linked to lower attitude scores, with each incremental increase in depression severity associated with a 1.08-point decrease (β = −0.208, p = 0.001). Regarding practice dimension, longer medical work experience correlated with higher practice scores (0.145-point increase per year, β = 0.132, p = 0.029), while cumulative days working in isolation wards had the strongest positive impact (0.403-point increase per day, β = 0.310, p < 0.001). Higher anxiety levels also negatively affected practice scores (0.442-point decrease, β = −0.129, p = 0.034). These results indicate independent associations between training frequency, psychological factors, and work-related experience with distinct dimensions of HCWs’ personal protection competencies. The data is shown in Table 7.
Discussion
This study aimed to evaluate the KAP related to personal protection among HCWs in the isolation wards of a designated COVID-19 treatment hospital. Employing a cross-sectional design, we surveyed 243 medical personnel using a structured questionnaire to assess KAP and mental health statuses through the BAI and BDI. The principal findings revealed that HCWs generally demonstrated positive attitudes and practices toward personal protection, although knowledge deficiencies were identified. Higher frequency of PPE training and lower anxiety levels were associated with improved personal protection knowledge, while lower depression levels were associated with a more positive attitude. HCWs with greater work experience, longer tenure in the isolation area, and lower anxiety levels showed a higher likelihood of adhering to personal protection practices.
Comprehensive analysis of KAP regarding personal protection among HCWs in isolation wards
The results of this survey provide a comprehensive analysis of the current status of KAP regarding personal protection among HCWs in isolation wards of designated hospitals. Our findings reveal that insufficient personal protection knowledge and skills, coupled with weak protection awareness, often lead to increased hazards in the prevention and control of infectious diseases. Specifically, the knowledge dimension score pertaining to personal protection is alarmingly low, with an average of 6.82 ± 1.6 points out of a possible 10. A staggering 85.60% of the HCWs (208 individuals) scored at the medium level or below, indicating a subpar understanding of personal protection measures. While this finding aligns with concerns raised by Müller et al. (5) regarding the importance of knowledge in infection control, our cross-sectional study design does not permit direct causal inferences between knowledge deficits and increased infection hazards. Further longitudinal or intervention studies are needed to elucidate the relationship between knowledge levels and actual infection outcomes. Nevertheless, the observed knowledge gaps highlight the urgent need for targeted educational interventions to optimize personal protection practices in high-risk clinical settings. Our observations further show that HCWs exhibit limited proficiency in fundamental theoretical knowledge related to the novel coronavirus (Table 2, K1, K2) and protocols for decontamination in the contaminated area (Table 2, K9). This could be attributed to their exposure to high psychological stress levels and demanding shift work schedules, which limit their time and energy for acquiring and staying updated with relevant professional knowledge (15). Given the ongoing evolution of the COVID-19 virus at that time and the need for constant updates and adjustments in prevention and control strategies, it is imperative for HCWs to receive enhanced theoretical training focusing on key aspects. In contrast, a study conducted in Saudi Arabia found that healthcare professionals received adequate training, which served as a foundational requirement for effective risk management and infection control policies (16).
Despite these deficiencies in knowledge, it is encouraging to note that the majority of HCWs in isolation wards exhibited a positive attitude toward personal protection, with an average score of 27.56 ± 4.1. Over 78.60% of the HCWs demonstrated a favorable disposition toward personal protection measures. This finding resonates with studies across diverse settings. Kim et al. (17) found that 81% of nurses in South Korea viewed PPE as essential for infection control, despite challenges in consistent adherence. Similarly, a multinational survey by Nwagbara et al. (8) noted that 76% of African HCWs expressed strong confidence in PPE efficacy, underscoring a global trend of positive attitudes amidst knowledge-practice gaps. Additionally, hospital leaders and colleagues may have influenced the formation of a culture that values personal protection. A positive outlook on personal protection can enhance motivation and confidence in implementing protective measures, thereby improving overall safety (18). Therefore, it is recommended to continue providing psychological support and encouragement to isolation ward working HCWs to boost their self-efficacy and confidence in personal protection.
At the level of personal protective practice, the research findings indicate that HCWs’ adherence to safety protocols is above average, with an average score of 44.44 ± 5.6. However, there is still room for improvement, particularly among a subset of HCW members who failed to actively seek information and familiarize themselves with newly issued national guides for COVID-19 prevention and control (Table 4, P2). Additionally, some HCWs neglected reviewing surveillance footage to identify potential sources of contamination when uncertain during PPE removal (Table 4, P3). These issues may reflect deficiencies in commitment toward enhancing personal protection practices. Conversely, HCWs demonstrated commendable efforts in implementing more explicit requirements outlined in the guidelines, such as hand hygiene within the removal area (Table 4, P5) which suggests high compliance with clearly specified requirements. The limitations in knowledge and skills, coupled with constraints imposed by the working environment and conditions, such as the availability, quality, and comfort of PPE, may impact the efficiency and effectiveness of implementing personal protective measures (19). Therefore, it is recommended to enhance operational guidance and supervision for HCWs in isolation wards, regularly evaluate and provide feedback on the utilization and efficacy of PPE, and promptly identify and rectify any existing issues or deficiencies. By establishing an organic and unified personal protection culture of KAP in the clinic, the health and safety of frontline HCWs in the prevention and control of infectious diseases can be truly guaranteed.
Analysis of factors affecting personal protection among HCWs in isolation wards
The analysis of factors affecting personal protection among HCWs in isolation wards of designated hospitals uncovers several significant influences. Notably, the frequency of trainings on protective equipment, years of experience, cumulative time spent working in isolation wards, and levels of anxiety and depression emerge as pivotal variables.
Our study observed a substantial positive correlation between the number of trainings attended and HCWs’ KAP regarding personal protection. By providing numerous training opportunities, the competence and confidence of HCWs in personal protection can be markedly enhanced (20). These training sessions often encompass both theoretical knowledge transfer and practical skill development, ensuring HCWs remain updated with the latest infection control guidelines and best practices. Consequently, this not only augments their knowledge but also refines their proficiency in practical applications, such as the proper donning and doffing of PPE. A Polish survey further underscores the necessity of educating medical staff on the appropriate use and selection of PPE (6). Our findings revealed that HCWs who participated in multiple trainings exhibited heightened levels of comprehensive knowledge and skills in managing infectious diseases, thereby bolstering their personal protection capabilities within isolation wards.
Additionally, the research indicates a significant positive correlation between the working years of medical personnel and their level of personal protection KAP. Healthcare practitioners with longer work experience generally demonstrate higher proficiency in personal protection, attributed to the extensive expertise accumulated over years of service in handling patients with infectious diseases (21). As healthcare professionals gain more experience, they develop a heightened awareness regarding hospital infection management, prompting them to implement personal protective measures more effectively to safeguard both their own and their patients’ safety.
The cumulative working hours of HCWs in isolation wards also positively correlate with their adherence to personal protective behaviors and their level of KAP. Prolonged exposure to the isolation ward environment allows HCWs to accumulate essential knowledge and practical experience in personal protection, enhancing their confidence and facilitating accurate execution, particularly in high-stress settings.
The presence of high anxiety levels among HCWs can result in a decline in their personal protection knowledge scores, indicating a significant impact on their knowledge dimension. Anxiety was linked to disruptions in learning and information processing, potentially reducing individuals’ ability to concentrate and acquire new knowledge effectively, as highlighted by Klassen’s self-efficacy theory (22). Cognitive disruptions such as distractibility, memory difficulties, and reduced information processing speed can render HCWs more susceptible to omissions or errors when adopting personal protective measures. Furthermore, anxiety significantly influences the personal protective practice dimensions of HCWs, with high levels negatively correlated with irregular personal protective behaviors. This may be attributed to decreased decision-making and behavioral execution abilities caused by anxiety, as suggested by LeBlanc’s study (23). Therefore, high anxiety levels may cause HCWs to feel nervous and make mistakes or omissions when applying personal protective measures, ultimately affecting their practice scores.
Similarly, the level of depression significantly influences the dimensions of personal protection attitude among HCWs. A depressive state is associated with negative attitudes toward personal protective measures, indicating that HCWs experiencing depression may develop unfavorable views toward their work and exhibit unsupportive behaviors regarding personal protection. This finding aligns with Li et al.’s (24) study, which revealed a strong correlation between depressive mood, mental health, and work-related attitudes among HCWs during the pandemic. Depressive moods were associated with feelings of exhaustion, helplessness, and disinterest in one’s job, and altered perceptions of personal protective measures. Such negative attitudes were linked to increased resistance toward work and lower adherence to personal protective measures, ultimately compromising their effectiveness in safeguarding HCWs against potential risks.
Personal protection beyond COVID-19
Although the immediate threat posed by COVID-19 has diminished, the findings of this study extend beyond the current pandemic context. For instance, while some researchers have explored interventions such as traditional medicine during and post-pandemic (25), our study specifically investigated the KAP of HCWs toward PPE in COVID-19 isolation wards, emphasizing how employment tenure, training frequency, and mental health status (e.g., anxiety and depression levels) shape their adherence to protective measures. These insights highlight that robust KAP frameworks are essential not only for COVID-19 but also for managing other infectious diseases (26). The identified principles, such as the critical role of frequent PPE training and the need to address mental health challenges (e.g., anxiety reduction), can be adapted to diverse high-risk clinical settings, including units managing highly contagious pathogens (17, 27). Importantly, mitigating mental health barriers (e.g., through targeted support for anxiety and depression) may enhance HCWs’ compliance with PPE protocols, thereby strengthening infection control practices in future outbreaks. It is imperative to maintain high standards of training and mental health support for healthcare workers, ensuring they are equipped to handle emerging threats or resurgence of known diseases effectively (28). Further research is needed to explore how the insights gained from this study could inform policies and practices in non-COVID-19 related infectious disease wards.
While this study was conducted in isolation wards of designated hospitals in Shandong Province, China, the findings have broader implications for healthcare systems worldwide. The importance of PPE training, mental health support, and work experience in enhancing HCWs’ KAP is not limited to a specific region or country. Studies from other countries, such as the United States (29), South America (30), and Europe (31), have similarly highlighted the critical role of PPE training and psychological well-being in ensuring effective personal protection during pandemics.
Conclusion
The results of this study indicate that the HCWs in the isolation wards of the designated COVID-19 treatment hospital demonstrated strong personal protection awareness and effective implementation of preventive measures, with favorable attitudes and practices. The study revealed associations between higher frequency of personal protective equipment training, lower anxiety levels and improved personal protection knowledge. Additionally, lower levels of depression were associated with more positive attitudes toward personal protective measures. HCWs with longer work experience and cumulative working time in isolation wards exhibited stronger adherence to personal protection regulations, which coincided with receiving mental health support, particularly interventions for anxiety.
However, the study has limitations: for instance, the use of convenience sampling and single-site data in this research may limit the generalizability of the findings. Additionally, the findings are specific to the isolation ward of a single designated hospital in Shandong Province, China, and thus may not represent the circumstances of HCWs in other hospitals or regions globally. The cross-sectional design also may restrict conclusions about long-term trends or causality. Self-reported data could be subject to social desirability bias. Future research should adopt broader sampling methods and longitudinal designs to validate these findings and enhance global applicability.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of Shandong Provincial Public Health Clinical Center. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
QLiu: Writing – review & editing, Data curation, Formal analysis, Methodology, Writing – original draft. YL: Investigation, Resources, Writing – review & editing. CH: Conceptualization, Methodology, Writing – review & editing. QLi: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Project funded by the Infection Prevention and Control Research Fund of the Chinese Geriatrics Society (Project number GRYJ-KLB2018027).
Acknowledgments
The authors wish to thank the study participants for their contribution to the research, as well as current and past investigators and colleagues. Thanks to Li Qiang, Public Health Clinical Center Affiliated to Shandong University, for research consultation. Thanks to Zhang Hong and other 6 hospital infection experts for questionnaire evaluation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1510015/full#supplementary-material
References
1. Asselah, T, Durantel, D, Pasmant, E, Lau, G, and Schinazi, RF. COVID-19: discovery, diagnostics and drug development. J Hepatol. (2021) 74:168–84. doi: 10.1016/j.jhep.2020.09.031
2. Read, JM, Bridgen, J, Cummings, D, Ho, A, and Jewell, CP. Novel coronavirus 2019-nCoV (COVID-19): early estimation of epidemiological parameters and epidemic size estimates. Philos Trans R Soc Lond Ser B Biol Sci. (1829) 376:20200265. doi: 10.1098/rstb.2020.0265
3. Ren, HF, Chen, FJ, He, LX, Liu, CQ, Liu, YY, Huang, YJ, et al. Nursing allocation in isolation wards of COVID-19 designated hospitals: a nationwide study in China. BMC Nurs. (2022) 21:23. doi: 10.1186/s12912-021-00795-w
4. Gholami, M, Fawad, I, Shadan, S, Rowaiee, R, and Ho, HSB. COVID-19 and healthcare workers: a systematic review and Metaanalysis. Int J Infect Dis. (2021) 104:335–46. doi: 10.1016/j.ijid.2021.01.013
5. Müller, A, Melzow, FS, Göstemeyer, G, Paris, S, and Schwendicke, F. Implementation of COVID-19 infection control measures by German dentists: a qualitative study to identify enablers and barriers. Int J Environ Res Public Health. (2021) 18:5710. doi: 10.3390/ijerph18115710
6. Malczynska, IU, Krych, G, Baran, A, Kaminski, TW, and Flisiak, I. Maskne-dermatosis of a pandemic. A survey on the impact of PPE on facial skin among HCW and N-HCW in Poland. Dermatol Ther. (2022) 12:2297–308. doi: 10.1007/s13555-022-00796-w
7. Mong, I, Ramoo, V, Ponnampalavanar, S, Chong, MC, and Wan, NW. Knowledge, attitude and practice in relation to catheter-associated urinary tract infection (CAUTI) prevention: a cross-sectional study. J Clin Nurs. (2022) 31:209–19. doi: 10.1111/jocn.15899
8. Nwagbara, UI, Osual, EC, Chireshe, R, Bolarinwa, OA, Saeed, BQ, Khuzwayo, N, et al. Knowledge, attitude, perception, and preventative practices towards COVID-19 in sub-Saharan Africa: a scoping review. PLoS One. (2021) 16:e0249853. doi: 10.1371/journal.pone.0249853
9. Van Nhu, H, Tuyet-Hanh, TT, Van, N, Linh, T, and Tien, TQ. Knowledge, attitudes, and practices of the Vietnamese as key factors in controlling COVID-19. J Community Health. (2020) 45:1263–9. doi: 10.1007/s10900-020-00919-4
10. Garg, M, Sridhar, B, Katyal, V, and Goyal, S. Assessment of knowledge, attitude, and practices (KAP) toward hepatitis B infection, its prevention, and vaccination among health care workers. Cureus. (2023) 15:e39747. doi: 10.7759/cureus.39747
11. Michel-Kabamba, N, Ngatu, NR, Leon-Kabamba, N, Katumbo-Mukemo, A, Mukuku, O, Ngoyi-Mukonkole, J, et al. Occupational COVID-19 prevention among Congolese healthcare workers: knowledge, practices, PPE compliance, and safety imperatives. Trop Med Infect Dis. (2020) 6:6. doi: 10.3390/tropicalmed6010006
12. Ashoor, M, Alshammari, S, Alzahrani, F, Almulhem, N, Almubarak, Z, Alhayek, A, et al. Knowledge and practice of protective personal equipment (PPE) among healthcare providers in Saudi Arabia during the early stages of COVID-19 pandemic in 2020. J Prev Med Hyg. (2022) 62:E830–40. doi: 10.15167/2421-4248/jpmh2021.62.4.2177
13. Shek, DT. Reliability and factorial structure of the Chinese version of the Beck depression inventory. J Clin Psychol. (1990) 46:35–43. doi: 10.1002/1097-4679(199001)46:1<35::AID-JCLP2270460106>3.0.CO;2-W
14. Kin-Wing, SC, Chee-Wing, W, Kit-Ching, W, and Heung-Chun, GC. A study of psychometric properties, normative scores and factor structure of Beck anxiety inventory Chinese version. Chinese. Chin J Clin Psychol. (2002). 1:4–6. doi: 10.3969/j.issn.1005-3611.2002.01.002
15. Rodríguez-Madrid, MN, Pastor-Moreno, G, Albert-Lopez, E, and Pastor-Valero, M. “You knew you had to be there, it had to be done”: experiences of health professionals who faced the COVID-19 pandemic in one public hospital in Spain. Front Public Health. (2023) 11:1089565. doi: 10.3389/fpubh.2023.1089565
16. Aleanizy, FS, and Alqahtani, FY. Risk management and infection control preparedness of Saudi healthcare facilities to overcome the COVID-19 pandemic. IJID Reg. (2022) 3:268–74. doi: 10.1016/j.ijregi.2022.04.005
17. Kim, EJ, Park, YH, and Choi, HR. Factors influencing nurses' compliance related to the use of personal protective equipment during the COVID-19 pandemic: a descriptive cross-sectional study. Nurs Open. (2024) 11:e2235. doi: 10.1002/nop2.2235
18. Ling, J, Jiang, H, Wang, X, and Rao, H. Health literacy affected the residents' knowledge, attitude, practice for prevention and control of COVID-19 in Shanxi Province, China. Sci Rep. (2023) 13:3567. doi: 10.1038/s41598-023-30730-9
19. Winter, S, Baratta, J, Zulman, D, Amano, A, Verano, MR, Brown-Johnson, C, et al. PPE portraits: patient and clinician experiences at a COVID-19 testing site. Ann Fam Med. (2022) 20:2771. doi: 10.1370/afm.20.s1.2771
20. Towning, R, Rennie, C, and Ferguson, M. Multi-disciplinary simulation training for surgical tracheostomy in patients mechanically ventilated secondary to severe acute respiratory syndrome Coronavirus-2. Ear Nose Throat J. (2021) 103:NP89–97. doi: 10.1177/01455613211042119
21. Ming, LI, You, HH, and Ying, HT. Occupational protection against infectious diseases among paramedics: an investigation and analysis. Chin J Nosoconmiol. (2004) 10:66–8. doi: 10.3321/j.issn:1005-4529.2004.10.028
22. Klassen, RM, and Klassen, J. Self-efficacy beliefs of medical students: a critical review. Perspect Med Educ. (2018) 7:76–82. doi: 10.1007/S40037-018-0411-3
23. LeBlanc, VR. The effects of acute stress on performance: implications for health professions education. Acad Med. (2009) 84:S25–33. doi: 10.1097/ACM.0b013e3181b37b8f
24. Li, X, Zhou, Y, and Xu, X. Factors associated with the psychological well-being among front-line nurses exposed to COVID-2019 in China: a predictive study. J Nurs Manag. (2021) 29:240–9. doi: 10.1111/jonm.13146
25. Kamoka, HM, and Elengoe, A. An investigation on use of traditional medicine during COVID-19 and post-COVID-19. Int J Adv Life Sci Res. (2024) 7:89–102. doi: 10.31632/ijalsr.2024.v07i01.010
26. Juttla, PK, Ndiritu, M, Milliano, F, Odongo, AO, and Mwancha-Kwasa, M. Knowledge, attitudes and practices towards COVID-19 among healthcare workers: a cross-sectional survey from Kiambu County, Kenya. PLoS One. (2024) 19:e0297335. doi: 10.1371/journal.pone.0297335
27. Shim, W, and Kim, KY. Effects of individual and environmental factors on COVID-19 infection control practices in small to medium-sized hospitals. Am J Infect Control. (2024) 52:1060–4. doi: 10.1016/j.ajic.2024.04.200
28. McBride, J, Allton, L, Torkington, S, and Smith, S. After COVID-19: preparing staff for future surges in respiratory illness in children and improving well-being. Nurs Child Young People. (2024) 36:26–33. doi: 10.7748/ncyp.2024.e1501
29. Gray, M, Monti, K, Katz, C, Klipstein, K, and Lim, S. A "mental health PPE" model of proactive mental health support for frontline health care workers during the COVID-19 pandemic. Psychiatry Res. (2021) 299:113878. doi: 10.1016/j.psychres.2021.113878
30. Romero-Cabrera, AB, Lindo-Cavero, A, Villarreal-Zegarra, D, Rodriguez, V, Luna-Matos, ML, Rojas-Mendoza, WN, et al. Perception of personal protective equipment availability and mental health outcomes in workers from two national hospitals during the COVID-19 pandemic. Heliyon. (2024) 10:e23327. doi: 10.1016/j.heliyon.2023.e23327
31. Candido, G, Tortù, C, Seghieri, C, Tartaglia, R, Baglioni, C, Citti, P, et al. Physical and stressful psychological impacts of prolonged personal protective equipment use during the COVID-19 pandemic: a cross-sectional survey study. J Infect Public Health. (2023) 16:1281–9. doi: 10.1016/j.jiph.2023.05.039
Keywords: COVID-19, HCW, personal protection, KAP, mental state
Citation: Liu Q, Li Y, Han C and Li Q (2025) Current status and influencing factors of knowledge, attitude and practice of personal protection of healthcare workers in isolation wards of COVID-19 designated hospitals. Front. Public Health. 13:1510015. doi: 10.3389/fpubh.2025.1510015
Edited by:
Marina Ruxandra Otelea, Carol Davila University of Medicine and Pharmacy, RomaniaReviewed by:
Linda Ahlstrom, University of Gothenburg, SwedenSigrún Eyrúnardóttir Clark, University College London, United Kingdom
Copyright © 2025 Liu, Li, Han and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chao Han, MzEwNzA2MDgzQHFxLmNvbQ==; Qi Li, bGlxaTgwMjNAMTYzLmNvbQ==
 Qian Liu1
Qian Liu1 Chao Han
Chao Han