- 1Department of Medical Rehabilitation Sciences, King Khalid University, Abha, Saudi Arabia
- 2Department of Physiotherapy, University of Hail, Hail, Saudi Arabia
- 3Department of Physical Therapy and Health Rehabilitation, Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia
The study explores global trends in adolescent health using data from the health behavior in school-aged children (HBSC) study, focusing on the role of education, socioeconomic status, and school-based health programs. It examines cross-country comparisons to assess disparities in adolescent wellbeing and health behaviors. Findings highlight that nations with comprehensive public health policies report lower adolescent obesity rates and better mental wellbeing, whereas regions with limited resources, experience greater health inequalities. The key factors contributing to these disparities include economic conditions, access to healthcare, and variations in school health programs. The study underscores the need for evidence-based, culturally adaptable interventions to improve adolescent health outcomes. By analyzing current policies and identifying gaps, this review aims to guide future public health strategies toward reducing inequalities and strengthening school-based health initiatives worldwide.
Introduction
The Health Behavior in School-aged Children (HBSC) study, initiated in 1983, is the largest study on child and adolescent health and one of the utmost eminent sources of data for the WHO’s global health monitoring system (1). The Helsinki-based international research project coordinated by the WHO analytically collected statistics on the health behaviors, lifestyles, and wellbeing of children across various countries (2–4). For decades, HBSC has examined the influence of social, economic, and environmental factors on adolescent health (5). These encompassed a variety of structural and practical variables, such as differences in the educational systems where fieldwork was carried out, adherence to a standard research protocol, problems with language and translation, and disparities in statistical capacities within nations.
The HBSC study has been widely regarded as a crucial tool for understanding adolescent health and wellbeing. However, like any large-scale cross-national study, it is not without controversies or different schools of thought.
Here are some key debates, criticism point of view and counterpoint perspectives surrounding the HBSC study:
Cultural and socioeconomic contexts
Debate and critique
National-level data may be incomprehensible and may provide significant regional disparities, leading to generalized health policies. In Canada, for example, 24% of adolescents state low life satisfaction, but rural areas experience greater dissatisfaction levels than urban centers (6). Similarly, in Mexico, more than 32% of adolescents report low life satisfaction, with prominent variances between richer urban regions and poorer rural areas (7). In Mozambique, where 40% of adolescents report low life satisfaction, national economic uncertainty and limited mental health sources likely influence the issue (8).
Counterpoint
However, HBSC allows between-country comparisons and is therefore useful to illustrate the influence of local contexts in specifying health behavior determinants that should address country specificities for future initiatives targeting adolescent wellbeing.
Measurement and validity concerns
Debate and critique
The HBSC depend comprehensively on self-reported statistics, raising interests about reliability and social suitability bias. For instance, self-reported alcohol consumption differs considerably, 16% of 15-year-olds in Norway conveyed drinking alcohol in previous years (9), compared to 38% in Hungary (10) and 8% in Nepal (11). Cultural norms perhaps influence these changes, with Hungarian adolescents more oriented to report drinking due to superior societal acceptance, while Nepalese adolescents may underreport due to religious and social humiliation.
Counterpoint
The HBSC uses confidentiality the protections to decrease social appropriateness, bias, and enormous sample sizes to help to balance individual reporting miscalculations. Despite potential biases, the study provides constructive data for identifying public health concerns and guiding policy interventions.
Focus on school-based interventions
Debate and critique
Focusing primarily on schools as sites for intervention may ignore other important influences on adolescent health, such as family dynamics or community environments. For example, in high-income country like Germany, 17% of adolescents reported being bullied at school (12), while in middle-income Brazil, the figure is 26% (13). In a low-income country like Ethiopia, 21% of adolescents reported being bullied at school (14). While schools remain critical environments for intervention, focusing solely on school settings may miss other important factors, such as family dynamics or community issues. For instance, in Brazil, social inequality and gang violence might play a significant role in bullying, while in Ethiopia, economic hardship and family stress might contribute to bullying behaviors, extending beyond the classroom environment.
Counterpoint
The schools remain important settings for intervention because they provide structured environments where policies (such as anti-bullying programs) can be implemented effectively. The HBSC’s emphasis on schools can guide policymakers in creating interventions that target students while also considering external influences.
Scope of data and health indicators
Debate and critique
Critics argue that the HBSC should expand its scope to include emerging health issues like the impact of digital technologies on adolescent wellbeing.
For example, in high-income Finland, 32% of adolescents report spending more than 4 h per day on screens (e.g., smartphones or computers) (15). In middle-income Mexico, this number is higher, with 44% of adolescents reporting excessive screen time (16). In a low-income country like Uganda, 29% of adolescents report spending too much time on screens (17). Although the HBSC tracks screen time, it may not fully account for the complex impacts of digital culture and social media on adolescent health, especially in countries like Mexico where cyberbullying and social media-related anxiety are growing concerns.
Counterpoint
The HBSC’s optional modules allow countries to investigate emerging trends like social media use and its health impacts. In Finland, for instance, additional questions on cyberbullying have been added to better understand the digital landscape and its effects on youth.
Policy implications and real-world impact
Debate and critique
While the HBSC provides valuable data, translating it into effective public health policies can be challenging, especially in countries with varying resources.
For example, in high-income country like Sweden, 24% of adolescents meet the World Health Organization’s (WHO) physical activity recommendations of at least 60 min of daily exercise (18). Sweden has successfully implemented national policies promoting physical activity through schools and public health campaigns (19). In middle-income country like Bulgaria, 18% of adolescents meet the recommendation, reflecting lower investment in public health infrastructure and fewer school-based programs (20, 21). In a low-income country like Haiti, only 10% of adolescents meet the daily activity recommendation (22). Haiti faces significant challenges, such as limited funding for school sports programs and a lack of public recreational facilities, making it difficult to translate HBSC findings into policy improvements (23).
Translating HBSC findings into actionable policies can be difficult, especially in countries with limited public health resources, like Haiti. Implementing wide-reaching programs to encourage physical activity may require external funding or international partnerships.
Counterpoint
The HBSC provides governments with the evidence needed to advocate for policies promoting physical activity. Even in low-income countries the data can be used to attract support from international organizations or guide efforts to improve health outcomes despite resource limitations.
These examples illustrate how high, middle, and low-income countries experience varying challenges and opportunities in adolescent health, based on HBSC data. Cultural, economic, and policy contexts heavily influence health behaviors and outcomes, and the HBSC helps identify these differences to inform targeted interventions across different regions.
Multidimensional approach to health: adolescent/school oriented view
The HBSC study is unique in its multi-dimensional perspective on adolescent health (24). Typical health-related surveys commonly evaluate only one behavior such as smoking or dietary habit. In contrast, various items were measured by HBSC including mental health problems (high depressive mood, stress and headache), obesity indexes substance use, sexual behavior indicators and knowledge on sexually transmittable infections as well early complications of having offspring with adolescent’s pregnancy rate (25). By using this overarching perspective, investigators are then able to assess not only individual behaviors but also at the interplay between these behaviors and a plethora of social determinants on health (26). For example, there is also research to suggest that dietary habits in young people are linked with levels of physical activity and mental health outcomes (27).
Objectives of the study
This review aims to:
To critically examine the scope, methodology, and evolution of the HBSC study across different survey cycles and participating countries.
To assess the contribution of HBSC data to the understanding of key adolescent health behaviors, including mental health, substance use, screen time, and dietary habits.
To compare and contrast international and country-specific findings from official HBSC reports and peer-reviewed literature to highlight consistencies, gaps, and divergences.
To identify methodological challenges and data validity concerns in existing HBSC-related research and reporting practices.
To highlight research gaps and propose future directions for leveraging HBSC data in policy development, school-based interventions, and global health strategies.
Methodology
This study is a narrative review that synthesizes results from existing research on adolescent health behaviors, focusing on education, socioeconomic status, and wellbeing.
Data collection and selection criteria
Data was collected from peer-reviewed journal articles, reports from international organizations (e.g., WHO, HBSC), and government health surveys published from 1983 until 2024. Literature was categorized through systematic searches in MEDLINE, EMBASE, CINAHL, LILACS, SCIELO, DOAJ, PubMed, PEDro, Saudi digital library, NHS EED, PROSPERO, Google Scholar, Scopus, and Web of Science using keywords such as “adolescent health,” “socioeconomic status,” “education and health behaviors,” and “school-based interventions.”
Studies were included mainly which focused on school-aged children (11–15 years old), provided cross-national comparisons of adolescent health indicators, and examined socioeconomic influences on adolescent wellbeing.
Exclusion criteria included articles with limited regional focus or lacking relevance to adolescent health behaviors.
Data analysis and synthesis
Extracted information was categorized under key themes: (1) socioeconomic disparities, (2) education and school health programs, (3) mental health trends, (4) obesity and physical activity, and (5) substance use.
A comparative thematic analysis was performed to identify patterns, disparities, and policy implications across different countries. The findings were critically evaluated to highlight gaps in research and policy recommendations for improving adolescent health outcomes. This approach ensures a structured synthesis of evidence, enabling meaningful cross-national comparisons without statistical testing.
In this study, we conducted cross-national comparisons using data from the Health Behavior in school-aged children (HBSC) study, which includes over 50 participating countries. The comparisons focused on adolescent health indicators such as obesity rates, mental health outcomes, physical activity levels, and school-based health interventions. Specifically, we examined countries with well-established public health programs (e.g., Norway, Sweden, Denmark), nations facing higher social inequalities and health disparities (e.g., Romania, Lithuania, Poland), and middle-income countries with diverse adolescent health profiles (e.g., Mexico, Bulgaria, Turkey). The selection of countries was based on available HBSC data and their relevance to the study’s objectives.
By specifying the countries and the criteria for comparison, this study aims to provide a clearer understanding of how national policies and socioeconomic contexts influence adolescent health outcomes globally.
Countries with comprehensive school-based health policies, such as Norway, Sweden, and Denmark, report lower adolescent obesity rates and enhanced mental health outcomes due to well-established nutrition programs, physical activity initiatives, and mental health support services. In contrast, Romania, Lithuania, and Poland experience higher adolescent health disparities, largely driven by socioeconomic inequalities and limited access to school-based health services. Additionally, middle-income countries like Mexico, Bulgaria, and Turkey show varied adolescent health outcomes, influenced by differing levels of investment in health promotion and school-based interventions.
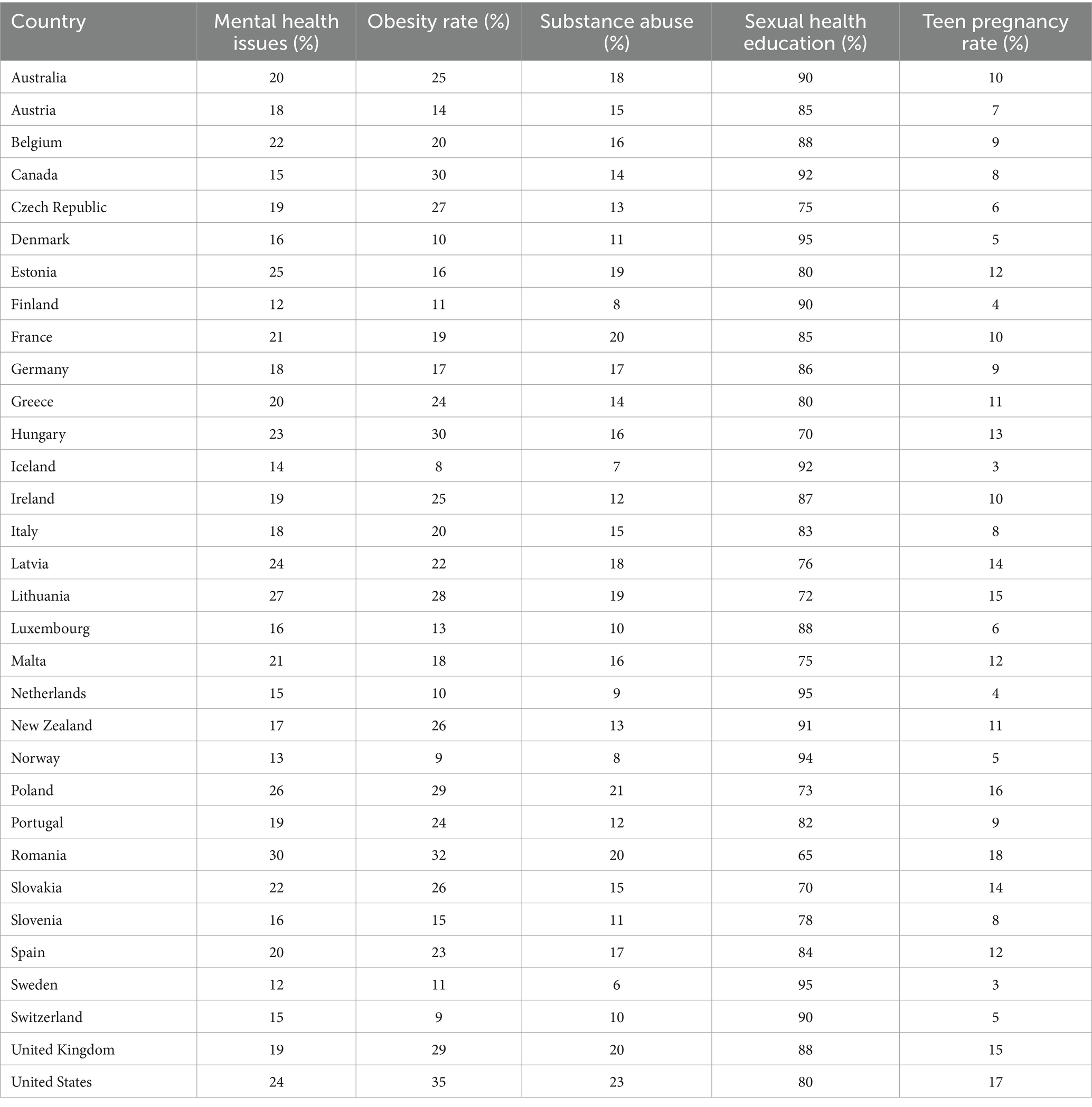
For example, in countries, where strong public health policies are in place, adolescent obesity rates remain relatively low, with Norway and Sweden reporting rates of 8 and 9%, respectively. In contrast, Romania and Lithuania, where socioeconomic disparities limit access to school-based health interventions, report higher obesity rates of 32 and 28%. Similarly, mental health concerns are more prevalent in European nations, with Estonia, Lithuania, and Romania reporting 25, 27, and 30% of adolescents experiencing anxiety and depression, respectively, compared to 12% in Finland. These variations highlight the role of national policies in shaping adolescent health outcomes (12, 28–32). The comparative nature of the HBSC study also provides an informative model for public health responses to adolescent wellbeing, worldwide (1, 33–36) (Table 1).
Understanding adolescent health (key observations)
Mental health issues
Estonia (25%), Lithuania (27%), and Romania (30%) reported the highest proportions of 11–15 year olds with mental health difficulties such as anxiety and depression are reported (37). These countries may need to boost their provision of mental health services and interventions for young people. Iceland and Norway have the lowest percentages (14% for both) followed by Finland with 12%, indicating better mental health access to support the intensity of psychiatric follow-up in due to socioeconomic background/counselor activity/surrounding social environment (31, 38).
Obesity rates
Top ranked in the world, for obesity rates of adolescent obesity, some of the highest worldwide with examples including United States (35%), Romania (32%) and Lithuania both at 28% highlighting challenges to dietary habits and physical activity (29, 39). Iceland (8%), Norway (9%), and Switzerland (9%) have significantly lower obesity rates, likely reflecting better access to healthy foods and more active behaviors in daily activities of life (40, 41).
Substance abuse in adolescents is higher among the United States and Poland (23%), Romania, 20%, making for a call up on prevention programs and public education to combat drug usage (42). Countries like Sweden (6%), Iceland (7%), and Finland (8%) report the lowest substance abuse rates, possibly due to comprehensive school-based prevention programs (5, 43).
Sexual health education
Unequivocally the top three countries for sexual health education are Denmark, Sweden and Netherlands with 95% each, all benefiting from established school-based programs focusing on teaching adolescents safe practices. In Romania, 65% and in Hungary only 70% of adolescents reported having had information on sexual health which points toward an important gap concerning a key topic influencing adolescent wellbeing (44–46).
Teen pregnancy rates
Romania (18%), United States (17%), and Poland (16%) report the highest rates of teen pregnancy, highlighting the need for more effective sexual education and access to reproductive health services. Iceland (3%), Sweden (3%), and Finland (4%) have the lowest teen pregnancy rates, suggesting strong sexual education and healthcare systems (46–48).
Cross-national comparisons and global insights
One of the HBSC study’s defining features is its international range. The survey has been conducted in more than 50 countries and regions. Health behaviors and outcome differences across countries can be readily examined within this cross-national framework. For instance, studies have shown that different countries eat and exercise differently because of their culture and government efforts around health issues. Such insights highlight the need for health interventions tailored to the adolescent population in various regions (49).
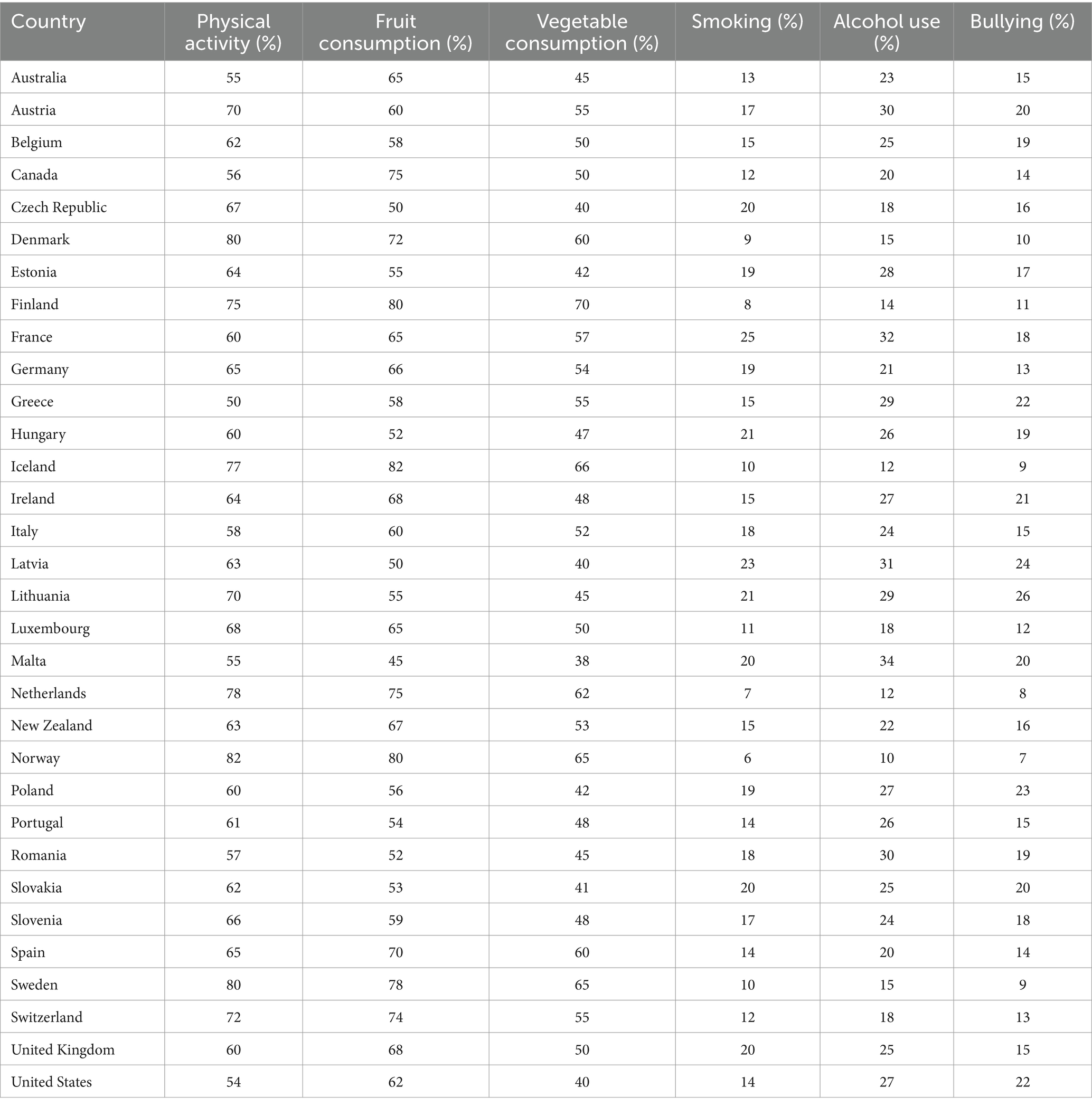
This aspect of this study revealed factors such as physical activity, fruit consumption, vegetable consumption, smoking, alcohol use, and bullying across various countries. Countries that promote health well, e.g., Norway and Sweden have shared their successes with countries with high rates of adolescent health problems such as obesity and mental illness. This joint effort has the potential to enhance worldwide initiatives aimed at enhancing adolescent health results through evidence-based policy creation (50–54) (Table 2).
Key findings from the cross-national comparisons regarding health indicators
Physical activity
In Norway, Sweden and Denmark over four in five, 11-to 15-year-olds report doing physical activity (more than 80%) which is among the highest levels in European countries reflecting the importance of active lifestyles and the importance of sports activities. Greece (50%), United States (54%), and Australia (55%) had the lowest, which could reflect the less emphasis on levels of physical education or activities (39, 55).
Fruit and vegetable consumption
Iceland and Norway has the highest rates (both 80% fruit consumption, overall half respondents eating either on a daily basis) implying good nutrition education or availability of healthy food. At the lowest end of both fruit and vegetable intake are Malta (45% fruit, 38% vegetables consumption) and Czech Republic (50% fruit, 40% vegetables consumption) representing potential gaps in promoting healthy eating behaviors among adolescents (56, 57).
Smoking and alcohol use
Norway (6% smoking, 10% alcohol routine) and Netherlands (7% smoking, 12% alcohol routine) have the lowest rates of teenage smoking and alcohol intake, likely reflecting effective prevention programs and firmer policies. Higher rates are reported in France (25% smoking, 32% alcohol use) and Latvia (23% smoking, 31% alcohol use), implying that more tailored interventions are necessary to reduce substance use should be implemented among adolescents (58–60).
Bullying
Netherlands (8%), Norway (7%), and Sweden (9%) show the lowest rates of bullying, likely because they have anti-bullying policies that are much more comprehensive and support systems. Latvia (24%), Lithuania (26%), and Poland (23%) have higher rates, pointing to current trials in focusing bullying in these regions (61, 62).
Revising social inequalities to provide the equal adolescent health opportunities is imperative
First and foremost, the existence of simple physical health adolescence opportunities is essential to eliminate these inherent social differences. This study too identified family affluence, neighborhood safety and access to healthcare and education as some of the socio-economic factors related to health outcome inequalities within adolescents. Addressing these inequities demands system change that goes beyond health systems to schools, communities and the broader social policy environment. In other words, the study underscores schools as not only important for both health and learning adolescent effectively a concept I have long argued but also provide boundary conditions aspect of wellbeing of adolescents.
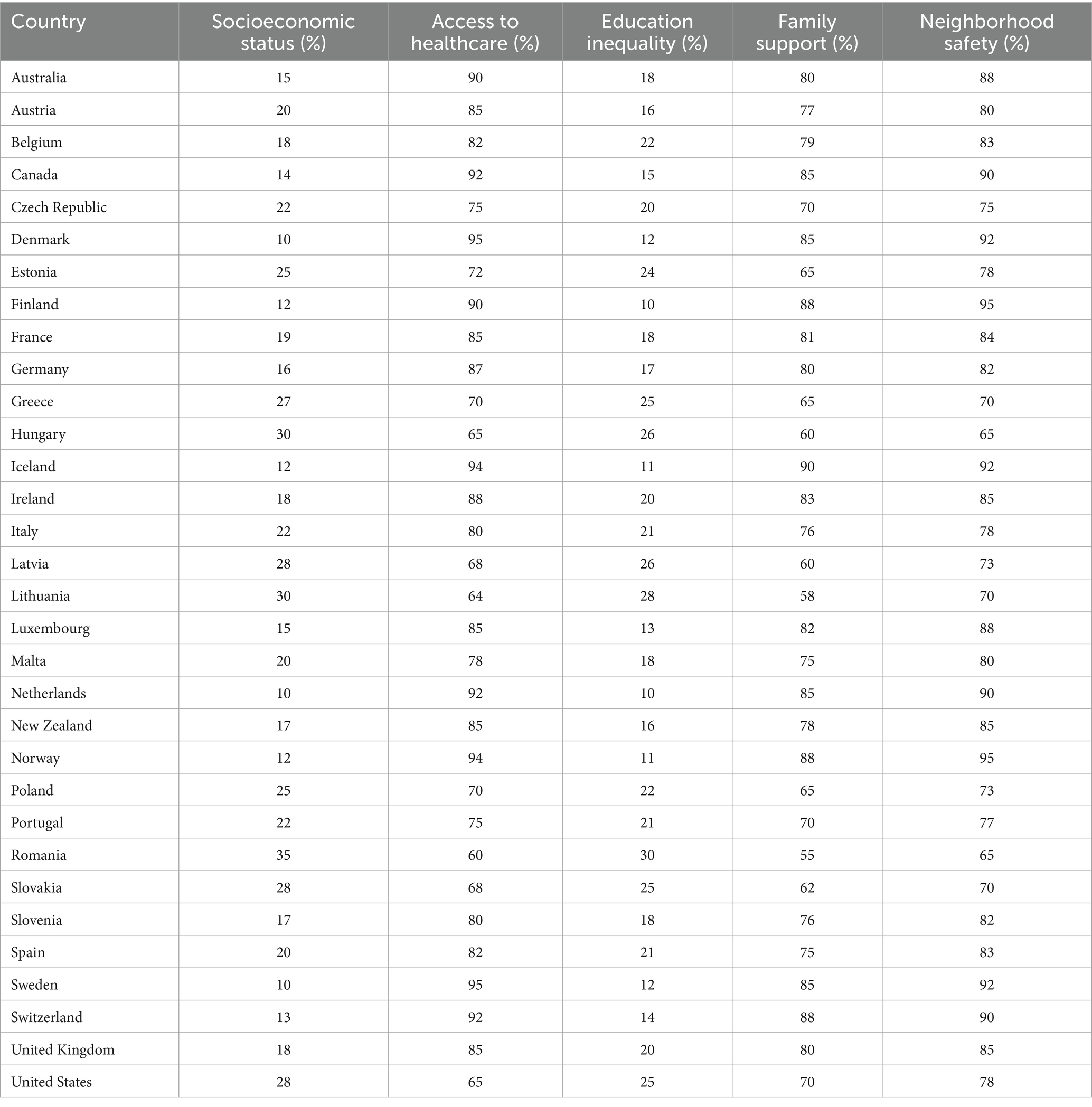
For example, states that have in combination invested both in national school-based health services (free healthy meals and mental health service/extracurricular programs) alongside social policies which target to the most unequal forms of inequality using an index tool-witnessed improved adolescents’ wellbeing (24, 52, 63–66) (Table 3).
Key observations from social inequalities perspective in HBSC studies
Socioeconomic status
Countries with lower socioeconomic inequality like Norway, Sweden, and Denmark exhibit smaller health gaps between adolescents from different income groups. Adolescents from all backgrounds in these countries report better overall health, reflecting the impact of strong social safety nets and equitable welfare systems. In contrast, Romania, Lithuania, and Poland show marked disparities, where adolescents from lower socioeconomic backgrounds report higher rates of mental health issues, obesity, and lower physical activity, indicating that socioeconomic inequality directly affects adolescent health outcomes (28).
Access to healthcare
Scandinavian countries such as Finland and Iceland, where healthcare is universally accessible, show minimal differences in health outcomes across socioeconomic groups. Adolescents in these countries have more consistent access to preventative healthcare services, reducing disparities in physical and mental health. Countries with more fragmented healthcare systems, like Hungary and Latvia, show significant inequalities in healthcare access, particularly for adolescents from lower-income families, who experience higher rates of untreated health conditions and lower access to health education (67, 68).
Education inequality
Education systems that promote equity, such as those in Finland and Netherlands, show lower disparities in adolescent health outcomes. Adolescents across all income levels benefit from comprehensive health education, which includes physical education, mental health support, and sexual health programs. In countries with greater educational inequality, such as Romania and Hungary, adolescents from lower-income families receive less comprehensive health education, contributing to higher rates of health issues like obesity, substance abuse, and mental health disorders (28, 52, 69).
Family support and neighborhood safety
Countries with high levels of family support and neighborhood safety, such as Iceland, Sweden, and Denmark, report better health outcomes across all income levels. Adolescents benefit from secure, stable environments, which buffer against the effects of social and economic stressors. In contrast, countries like Poland and Romania, where social inequalities are more pronounced, show greater disparities in mental health and wellbeing. Adolescents from lower-income families often report lower levels of family support and live in neighborhoods with higher risks, contributing to poorer health outcomes (32, 33, 70).
These observations from the HBSC study emphasize that reducing social inequalities through targeted interventions in healthcare, education, and community support systems is essential for improving adolescent health outcomes across all socioeconomic groups.
Adapting to changing circumstances: handling emerging health issues
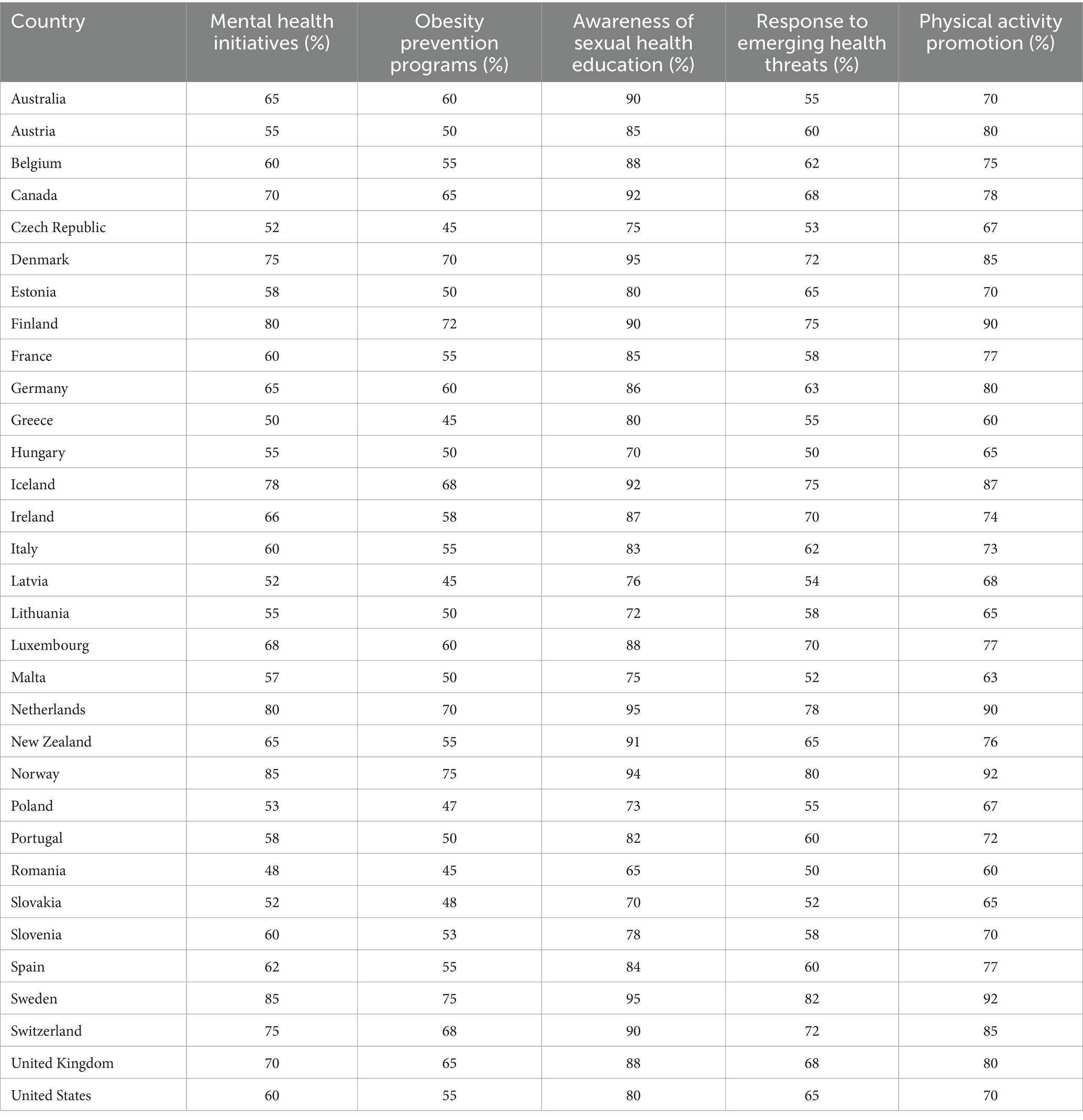
The HBSC survey has recently been adjusted to address emerging health concerns for adolescents. The rise of digital technology and social media has significantly impacted these people’s lives. These gadgets influence mental health, social relationships, and health behaviors. Analysis of HBSC data have revealed links between screen time, social media usage, and mental health outcomes. Heavy social media users express heightened feelings of loneliness and anxiety (1, 35, 71–75) (Table 4).
As a response to these changing challenges, the HBSC study has included new measures and questions on digital behaviors and consequences on health. With this proactive approach, the study will enhance the relevance of the study and thus offer valuable insights on the subject matter. Innovative Research will be required to understand how changes in behavior and new technologies are affecting adolescent health.
Key observations handling emerging health issues perspective in HBSC studies
Mental health initiatives
Countries like Denmark (75%), Norway (85%), and Finland (80%) have implemented robust mental health initiatives, ensuring a significant proportion of adolescents have access to support services. This highlights the importance of proactive mental health strategies in fostering resilience and wellbeing among youth (75, 76).
Obesity prevention programs
Countries such as Canada (65%) and Denmark (70%) suggest a strong obligation to obesity prevention, indicating an awareness of the rising obesity epidemic among adolescents. These numbers reflect social norms befitting nations that are seeing increasing rates of adolescent adiposity. It is important that funding be provided so that these programs may continue to exist promote weight-related healthy lifestyle choices and prevent downstream health outcomes (29, 77).
Awareness of sexual health education
High percentages of sexual health education awareness in countries like Norway (94%), Finland (90%), and Netherlands (95%) suggest an indicative about widespread coverage for a comprehensive sexual health curricula. Adolescent sexual education is essential in providing adolescents with the information to make sexually healthy choices (78, 79).
Response to emerging health threats
Countries such as Sweden (82%) and Denmark (72%) exhibit strong responses to emerging health threats, including infectious diseases and public health emergencies. This indicates a proactive approach to health crisis management, which is vital in protecting adolescent populations (28, 32).
Physical activity promotion
High levels of physical activity promotion in countries like Norway (92%) and Finland (90%) reflect a commitment to encouraging active lifestyles among adolescents. Such initiatives can play a significant role in reducing obesity rates and improving overall health outcomes (12, 80).
Awareness of Sexual Health Education: Sizable proportions reporting awareness of sexual health education in countries such as Norway (94%), Finland (90%) and the Netherlands (95%) are indicative about widespread coverage for a comprehensive sexual health curricula. Adolescent sexuality education is essential in providing adolescents with the information to make sexually healthy choices (72, 73).
Response to Emerging Health Threats — More than 80% of countries have a standardized plan for combating emerging health threats, such as infectious diseases and public health emergencies [e.g., Sweden (82%), Denmark (72%)]. This represents a preventative stance toward the management of health crisis and needful in safeguarding adolescent populations (60, 64).
Overall insights
The data reveals a correlation between the availability of health initiatives and improved health indicators among adolescents. Countries with comprehensive mental health support, effective obesity prevention programs, and high awareness of sexual health education tend to report better health outcomes. This underscores the need for integrated public health strategies that address multiple aspects of adolescent health.
The role of schools in promoting adolescent health
The HBSC study has also highlighted the important influence that schools have on adolescents’ health-related behaviors and results.
Schools play a vital role in fostering good health by providing opportunities for holistic growth through education, physical activity, and social interaction (28). Research indicates that students enrolled in schools with comprehensive health programs, which include components such as nutrition education, mental health support, and physical exercise, tend to perform better academically (81). These programs not only address physical health but also enhance students’ ability to focus and succeed in their studies, reinforcing the interconnectedness of health and academic achievement (82, 83).
Additionally, findings from the HBSC study emphasize the importance of a supportive school environment in fostering healthy behaviors (84). When students perceive their school as encouraging and conducive to health, they are more likely to adopt healthy habits and report better overall wellbeing (34). A positive school climate, one that promotes health and wellness, can have a profound impact on students’ daily choices, ranging from their diet and physical activity to their mental and emotional health (85). This sense of belonging and support within the school community can lead to long-lasting benefits that extend well beyond the school years (84, 86).
Schools also play a crucial role in the development of adolescents, not only in terms of academics but also in shaping their overall wellbeing (87). As the primary environment where young people spend a significant portion of their time, schools are uniquely positioned to promote adolescent health in a comprehensive manner (88). Beyond just addressing physical health, schools can foster mental, emotional, and social wellbeing through integrated programs that cater to the diverse needs of students (89). By incorporating health education into everyday learning, schools empower adolescents to make informed choices, develop positive habits, and build resilience as they navigate the complexities of growing up (83, 90).
Schools serve as a foundation for healthy behaviors, introducing young people to the importance of nutrition, mental health, hygiene, and social responsibility (91). Whether it is promoting balanced meals in school cafeterias or encouraging stress management through mindfulness practices and mental health support, schools are actively shaping the future health of adolescents (92). When schools prioritize health, they not only improve student outcomes but also lay the groundwork for lifelong wellbeing (86). By investing in comprehensive health programs, schools become more than academic institutions; they evolve into key players in shaping healthier, more resilient communities. This holistic approach positions schools as powerful agents of change in promoting the overall health and success of adolescents (Table 5).
Key findings concerning role of schools in promoting adolescent health
Mental health education
Integrated mental health education is common in countries like the USA, Canada, the UK, Sweden, and Israel. These countries emphasize comprehensive support for adolescents’ mental wellbeing. Moderate levels of mental health education are found in countries such as Germany, France, and Brazil, focusing on awareness but less on comprehensive programs. Limited mental health education is more prevalent in countries like India, China, Nigeria, and Pakistan, indicating gaps in addressing adolescent mental health (75).
Nutrition programs
Comprehensive nutrition programs are implemented in many developed nations, such as the USA, Canada, Germany, Australia, and the Netherlands, providing broad nutritional support in schools. Basic nutrition programs are common in countries like India, Nigeria, and Bangladesh, indicating less emphasis on extensive school nutrition plans. Moderate nutrition programs are found in countries like the UK, France, and Mexico, balancing between awareness and implementation of healthier eating habits (93).
Sexual education
Comprehensive sexual education is emphasized in countries such as the USA, Canada, and Brazil, ensuring that adolescents receive full and accurate information about sexual health. Moderate sexual education is implemented in countries like Germany, France, and South Africa. Basic or limited sexual education is more common in countries like India, Japan, and Nigeria, where sexual health education may be stigmatized or minimally addressed (94, 95).
Substance abuse prevention
National campaigns for substance abuse prevention are a priority in countries such as the USA, Canada, the UK, Brazil, and Israel, focusing on reducing adolescent drug use through large-scale initiatives. Regional initiatives are common in countries like South Korea and Germany, targeting specific regions rather than national efforts. Basic awareness campaigns are seen in countries like India, China, and Nigeria, reflecting less extensive substance abuse prevention efforts (96–98).
Hygiene promotion
Emphasized hygiene promotion is common in developed countries such as the USA, Canada, and Sweden, where schools heavily promote cleanliness and health hygiene. Moderate hygiene promotion is found in countries like South Korea, China, and South Africa, indicating attention to hygiene but less of a schoolwide campaign. Limited hygiene promotion is common in countries like India, Nigeria, and Bangladesh, where hygiene education in schools is not a primary focus (99, 100).
Parental involvement programs
Strong, school-based parental involvement programs are seen in countries like the USA, Canada, and Israel, highlighting the role of parents in supporting adolescent health through school channels. Community-based parental involvement is prevalent in countries like Brazil and Argentina, where the wider community plays a part in fostering adolescent health. Limited parental involvement is common in countries like India, Pakistan, and Nigeria, indicating less engagement between schools and parents in promoting health (24, 72).
General trends
Developed countries (USA, Canada, and Western Europe) generally offer comprehensive programs across various adolescent health aspects, indicating a holistic approach (29, 61). Developing countries (India, Nigeria, Pakistan) often show limited or basic programs, reflecting challenges in resources, societal attitudes, and policy emphasis on adolescent health (101–103). Parental involvement varies greatly, with developed nations favoring strong school-based programs and some developing nations favoring community-based approaches (104, 105). In contrast, certain countries still have minimal parental involvement in adolescent health promotion.
Discussion
The results of this research study indicate that there are considerable differences in adolescent health outcomes between countries due to the education systems, socioeconomic factors, and public health systems in place. The HBSC study has been critical in flagging important trends in these adolescent health outcomes, but there are still a number of gaps in the methods used and the concepts. By focusing these limitations, it can advance the study’s ability to inform targeted public health interventions and policies.
HBSC research has significantly advanced our understanding of adolescent health, but its approach to intersectionality remains limited (106). The majority of the studies target on individual health behaviors, such as physical activity, nutrition, or mental health, without effectively reflecting the complex relations between gender, socioeconomic status, migration background, and disability (107–109). For example, in Sweden, adolescent girls from low-income immigrant families may face various health challenges than those from wealthier background families (110). More research is needed should to provide the understanding of persistent health inequalities through policy changes.
The impact of climate change on adolescent wellbeing has become an emerging global concern (111). Displacement related to climate change, extreme weather events and environmental degradation can worsen mental health problems, disrupt access to education and limit opportunities for physical exercise, especially in vulnerable regions (112, 113). Future research should also assess the interaction between climate-related stressors and adolescent health, including effects on social engagement, lifestyle behaviors, and overall wellbeing of adolescents.
With the rapid rise of digital technologies, adolescents are increasingly exposed to screen time, social media interactions, and online gaming (114). While HBSC tracks basic indicators of technology use, it does not fully capture the psychological and behavioral impacts of cyber-wellness, including digital peer pressure, cyberbullying, and virtual relationships (114). Future research needs to develop much more sophisticated metrics that evaluate the quality of digital interactions, emphasizing both risks and potential benefits of online engagement. Currently, most HBSC research is based on cross-sectional data, limiting its ability to track long-term health trajectories (115, 116). Understanding how adolescent behaviors impact adult health outcomes requires longitudinal research and predictive modeling.
The HBSC network has successfully facilitated cross-national comparisons of adolescent health behaviors (84, 117). However, cultural differences can influence self-reporting and perceptions of health behaviors, leading to potential misinterpretations. For example, mental illness stigma, body image concerns, and attitudes toward substance use vary significantly across countries, impacting survey responses (118). Future studies should incorporate culturally tailored research methods, ensuring more accurate international comparisons while maintaining scientific validity.
Despite being the primary focus of the HBSC study, adolescents themselves are rarely involved in research design, data interpretation, or policy discussions (119). Integrating youth participatory research methods could ensure that HBSC studies better reflect the lived experiences of young people (120). By co-creating survey tools and research priorities with adolescents, studies can become more relevant, engaging, and impactful in addressing key youth health concerns (121).
Although the HBSC study has expanded to include over 50 countries, much of its research is still centered on high-and middle-income nations, leaving significant gaps in the Global South (122, 123). Adolescents in low-income regions, conflict zones, and areas with high infectious disease burdens face unique health challenges that remain underexplored (124). Expanding HBSC coverage to these regions, using ethically and culturally appropriate methodologies, would enhance global adolescent health research and improve policy relevance in underserved populations.
While HBSC findings provide valuable insights, their translation into policy change remains a challenge (125). Future research should evaluate the effectiveness of different health interventions in reducing disparities across socioeconomic groups and geographic regions. For instance, understanding which school-based mental health programs work best in low-income versus high-income settings could optimize resource allocation (126). Strengthening policy research integration in HBSC studies can enhance its impact on adolescent health equity.
This study underscores the importance of refining HBSC methodologies to address intersectional inequalities, emerging health threats, and digital influences on adolescent wellbeing. By incorporating longitudinal tracking, cultural adaptations, and participatory research approaches, future HBSC studies can better inform global health policies. These advancements will enhance the ability of governments and organizations to develop evidence-based, equity-focused interventions aimed at improving adolescent health outcomes worldwide.
Conclusion
To conclude, this review aims to support many approaches to adolescent health that schools employ globally, as demonstrated by HBSC’s work. Places where there is strong health infrastructure, comprehensive mental health programmes and substantial family and community support tend to have better results among young people. Moreover, in the context of social inequalities principally found within resource-limited countries, this bolsters a call for more organized global approach. Combatting these disparities would call for programs that focus on equal access to health education, mental wellness resources and parent engagement systems in schools. Moreover, increasing presence of health challenges like obesity and the mental health crisis demand novel approaches that can be adapted to variate cultural or socio-economic settings. The aforementioned slogans and the framework of risk factors, priorities, strategies can be used to justify action but should also guide all actors in future work that benefits from assuming schools already serve as primary health promoting centers.
Although the HBSC study has made a substantial contribution to our understanding of adolescent health, several research gaps remain. In order to alleviate the existing dependence on cross-sectional data, future research should use longitudinal designs to monitor the long-term effects of teenage activities on adult health outcomes. Additionally, more analyses studies are needed to examine the collective impact of gender, socioeconomic status, and migration background on adolescent health, as previous studies have primarily assessed these factors individually. The rising influence of digital technology on adolescent wellbeing also necessitates further investigation, particularly concerning cyberbullying, screen time, and digital mental health interventions. Addressing these gaps will enhance the effectiveness of public health policies and school-based interventions aimed at improving adolescent wellbeing.
Author contributions
MA: Methodology, Writing – review & editing. VG: Formal analysis, Writing – review & editing, Project administration. VK: Conceptualization, Data curation, Formal analysis, Project administration, Writing – original draft, Writing – review & editing. KA: Software, Writing – review & editing, Visualization. BA: Conceptualization, Writing – review & editing, Supervision, Data curation. RR: Data curation, Writing – review & editing, Funding acquisition. JT: Project administration, Writing – review & editing. SD: Writing – review & editing, Formal analysis. LK: Writing – review & editing, Data curation. GN: Visualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors extend their appreciation to the Deanship of Scientific Research and Graduate Studies at King Khalid University, KSA, for funding this work through large Research group under grant number RGP 2/98/46.
Acknowledgments
The authors extend their appreciation to the Deanship of Scientific Research and Graduate Studies at King Khalid University, KSA, for funding this work through large Research group under grant number RGP 2/98/46.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Moor, I, Winter, K, Bilz, L, Bucksch, J, Finne, E, John, N, et al. The 2017/18 health behaviour in school-aged children (HBSC) study–methodology of the World Health Organization’s child and adolescent health study. J Health Monitoring. (2020) 5:88–102. doi: 10.25646/6904
2. Lazzeri, G, Ciardullo, S, Spinelli, A, Pierannunzio, D, Dzielska, A, Kelly, C, et al. The correlation between adolescent daily breakfast consumption and socio-demographic: trends in 23 European countries participating in the health behaviour in school-aged children study (2002–2018). Nutrients. (2023) 15:2453. doi: 10.3390/nu15112453
3. Inchley, J, Currie, D, Young, T, Samdal, O, Torsheim, T, Augustson, L, et al. Health behaviour in school-aged children (HBSC) study: international report from the 2013/2014 survey. Health Policy Child Adolesc. (2016) 7:1–277.
4. WHO. A health behaviour in school-aged children (HBSC) study and schools for health in Europe network (SHE) collaborative project for data-led health action planning in schools: Findings and reflections from three European pilot case studies. A health behaviour in school-aged children (HBSC) study and schools for health in Europe network (SHE) collaborative project for data-led health action planning in schools: Findings and reflections from three European pilot case studies. Geneva: WHO (2020).
5. Molcho, M, Bjarnason, T, Cristini, F, Gaspar de Matos, M, Koller, T, Moreno, C, et al. Foreign-born children in Europe: An overview from the health behaviour in school-aged children (HBSC) study. Geneva: International Organization for Migration Background Paper (IOM) (2009).
6. Burton, P, Daley, A, and Phipps, S. The well-being of adolescents in northern Canada. Child Indic Res. (2015) 8:717–45. doi: 10.1007/s12187-014-9252-8
7. Marquez, J. Gender differences in school effects on adolescent life satisfaction: Exploring cross-national variation. Child Youth Care Forum. (2024) 53:389–409. doi: 10.1007/s10566-023-09756-7
8. Daw, TM, Reid, NJ, Coulthard, S, Chaigneau, T, António, VM, Cheupe, C, et al. Life satisfaction in coastal Kenya and Mozambique reflects culture, gendered relationships and security of basic needs: implications for ecosystem services. Ecosyst Serv. (2023) 62:101532. doi: 10.1016/j.ecoser.2023.101532
9. Potrebny, T, Wiium, N, Haugstvedt, A, Sollesnes, R, Torsheim, T, Wold, B, et al. Health complaints among adolescents in Norway: a twenty-year perspective on trends. PLoS One. (2019) 14:e0210509. doi: 10.1371/journal.pone.0210509
10. Barabas, A, Nagy, AC, Pazmany, V, Molnarne, AKG, Agnes, N, Jona, G, et al. Comparison of the HBSC results of the Visegrad countries with the health behavior of Young people with disabilities living in Hungary: A Cross-sectional study. (2024).
11. Adhikari, P, Paudel, K, Bhusal, S, Gautam, K, Khanal, P, Adhikari, TB, et al. Health literacy and its determinants among school-going children: a school-based cross-sectional study in Nepal. Health Promot Int. (2024) 39:daae059. doi: 10.1093/heapro/daae059
12. Bucksch, J, Häußler, A, Schneider, K, Finne, E, Schmidt, K, Dadacynski, K, et al. Physical activity and dietary habits of older children and adolescents in Germany–Cross-sectional results of the 2017/18 HBSC study and trends. J. Health Monitoring. (2020) 5:21–36. doi: 10.25646/6900
13. Maltoni, J, Lisboa, CSM, Matos, MG, Teodoro, ML, and Neufeld, CB. Cultural adaptation of the health behaviour protocol in school-aged children for the brazilian reality. Psicologia: teoria e prática. (2019) 21:77–92. doi: 10.5935/1980-6906/psicologia.v21n3p77-92
15. Ojala, K, Tynjälä, J, Välimaa, R, Villberg, J, and Kannas, L. Overweight adolescents’ self-perceived weight and weight control behaviour: HBSC study in Finland 1994–2010. J Obes. (2012) 2012:180176. doi: 10.1155/2012/180176
16. Jáuregui, A, Pacheco-Miranda, S, Argumedo-García, G, Marron-Ponce, JA, Armando, G, Vargas-Meza, J, et al. Comprehensive evaluation of Salud escolar a health school program in Mexico: rationale, design and methods. Prev Med Rep. (2022) 25:101662. doi: 10.1016/j.pmedr.2021.101662
17. Nakabazzi, B, Wachira, L-JM, Oyeyemi, AL, Ssenyonga, R, and Onywera, VO. Prevalence and socio-demographic correlates of accelerometer measured physical activity levels of school-going children in Kampala city, Uganda. PLoS One. (2020) 15:e0235211. doi: 10.1371/journal.pone.0235211
18. Moradell, A, Santaliestra-Pasías, AM, Aparicio-Ugarriza, R, Huybrechts, I, Bertalanné Szommer, A, Forsner, M, et al. Are physical activity and sedentary screen time levels associated with food consumption in European adolescents? The HELENA study. J Am Nutr Assoc. (2023) 42:55–66. doi: 10.1080/07315724.2021.1978900
19. Chong, KH, Suesse, T, Cross, PL, Ryan, ST, Aadland, E, Aoko, O, et al. Pooled analysis of physical activity, sedentary behavior, and sleep among children from 33 countries. JAMA Pediatr. (2024) 178:1199–207. doi: 10.1001/jamapediatrics.2024.3330
20. Markova, G. The health culture of adolescents from Pleven. Bulgaria Health Educ Health Prom. (2024) 12:105–10. doi: 10.58209/hehp.12.1.105
21. Kotzeva, T, and Dimitrova, E. Risk Behaviours: tracking youth health and well-being in Bulgaria 2006–2018 In: A Heinen and R Samuel, editors. Wohlbefinden und Gesundheit im Jugendalter: Theoretische Perspektiven, empirische Befunde und Praxisansätze. Wiesbaden: Springer Fachmedien Wiesbaden (2022). 665–87.
22. Becker, HV. Understanding adolescent physical activity in the early nutrition transitioning country of Haiti. Washington, DC: Washington University in St. Louis (2018).
23. Geller, J, Starrs, M, Bartholomew, A, Kaliszak, S, and Kessenich, J. The health of Haitian schoolchildren: longitudinal effect of annual visits on growth. J Refugee Global Health. (2021) 4:2. doi: 10.55504/2473-0327.1070
24. Haug, E, Smith, ORF, Ng, K, Samdal, O, Marques, A, Borraccino, A, et al. Family structure and the association with physical activity—findings from 40 countries participating in the health behaviour in school-aged children (HBSC) study. PLoS One. (2024) 19:e0300188. doi: 10.1371/journal.pone.0300188
25. Mertens, SB, and Caskey, MM Young adolescent health and well-being. Health and well-being in the middle grades: research for effective middle level Education (2023).
26. Rafi, W. Academic health science centers and health disparities: A qualitative review of the intervening role of the electronic health record and social determinants of health. (2022).
27. Bromley, K, Sacks, DD, Boyes, A, Driver, C, and Hermens, DF. Health enhancing behaviors in early adolescence: an investigation of nutrition, sleep, physical activity, mindfulness and social connectedness and their association with psychological distress and wellbeing. Front Psych. (2024) 15:1413268. doi: 10.3389/fpsyt.2024.1413268
28. Currie, C, and Morgan, A. A bio-ecological framing of evidence on the determinants of adolescent mental health-a scoping review of the international health behaviour in school-aged children (HBSC) study 1983–2020. SSM-Population Health. (2020) 12:100697. doi: 10.1016/j.ssmph.2020.100697
29. Fismen, A-S, Smith, ORF, Helleve, A, Haug, E, Chatelan, A, Kelly, C, et al. Cross-national variation in the association between family structure and overweight and obesity: findings from the health behaviour in school-aged children (HBSC) study. SSM-Population Health. (2022) 19:101127. doi: 10.1016/j.ssmph.2022.101127
30. Potrebny, T, Nilsen, SA, Bakken, A, von Soest, T, Kvaløy, K, Samdal, O, et al. Secular trends in mental health problems among young people in Norway: a review and meta-analysis. Eur Child Adolesc Psychiatry. (2025) 34:69–81. doi: 10.1007/s00787-024-02371-4
31. Eriksson, C, and Stattin, H. Mental health profiles of 15-year-old adolescents in the Nordic countries from 2002 to 2022: person-oriented analyses. BMC Public Health. (2024) 24:2358. doi: 10.1186/s12889-024-19822-x
32. Borraccino, A, Berchialla, P, Dalmasso, P, Sciannameo, V, Vieno, A, Lazzeri, G, et al. Connectedness as a protective factor in immigrant youth: results from the health behaviours in school-aged children (HBSC) Italian study. Int J Public Health. (2020) 65:303–12. doi: 10.1007/s00038-020-01355-w
33. Kleszczewska, D, Porwit, K, Boberova, Z, Sigmund, E, Vasickova, J, and Paakkari, L. Adolescent health literacy and neighbourhood features: HBSC findings from Czech Republic, Poland, and Slovakia. Int J Environ Res Public Health. (2021) 18:7388. doi: 10.3390/ijerph18147388
34. Tt, B, de Looze, M, Lee, A, van den Eijnden, R, Stevens, G, and Fung, A. Social and economic indicators of psychological symptoms and life satisfaction among Dutch and Hong Kong adolescents: a cross-national HBSC study. Cross-Cult Res. (2024) 59:88–120. doi: 10.1177/10693971241231019
35. Currie, C, Díaz, AYA, Bosáková, L, and de Looze, M. The international family affluence scale (FAS): charting 25 years of indicator development, evidence produced, and policy impact on adolescent health inequalities. SSM-Population Health. (2024) 25:101599. doi: 10.1016/j.ssmph.2023.101599
36. Oksuz, I, Ozcan, MS, Dost-Gözkan, A, and Kisbu, Y. Health risk behaviors of adolescents in Europe: a latent profile analysis of health behavior in school-aged children survey data from 43 countries. J Adolesc Health. (2024) 76:115–21. doi: 10.1016/j.jadohealth.2024.08.001
37. Walsh, SD, Sela, T, De Looze, M, Craig, W, Cosma, A, Harel-Fisch, Y, et al. Clusters of contemporary risk and their relationship to mental well-being among 15-year-old adolescents across 37 countries. J Adolesc Health. (2020) 66:S40–9. doi: 10.1016/j.jadohealth.2020.02.012
38. Potrebny, T, Nilsen, SA, Bakken, A, von Soest, T, Kvaløy, K, Samdal, O, et al. Secular trends in mental health problems among young people in Norway: a review and meta-analysis. Eur Child Adolesc Psychiatry. (2024) 34:1–13.
39. Musić Milanović, S, Buoncristiano, M, Križan, H, Rathmes, G, Williams, J, Hyska, J, et al. Socioeconomic disparities in physical activity, sedentary behavior and sleep patterns among 6-to 9-year-old children from 24 countries in the WHO European region. Obes Rev. (2021) 22:e13209. doi: 10.1111/obr.13209
40. Roman-Juan, J, Roy, R, Jensen, MP, and Miró, J. The explanatory role of sedentary screen time and obesity in the increase of chronic back pain amongst European adolescents: the HBSC study 2002–2014. Eur J Pain. (2022) 26:1781–9. doi: 10.1002/ejp.2003
41. Berli, R, Sempach, C, and Herter-Aeberli, I. Risk factors and 20-year time-trend in childhood overweight and obesity in Switzerland: a repeated Cross-sectional study. Children. (2024) 11:1050. doi: 10.3390/children11091050
42. Currie, C. Inequalities in young people's health: HBSC international report from the 2005/2006 Survey. Geneva: World Health Organization (2008).
43. Marques, A, Demetriou, Y, Tesler, R, Gouveia, ÉR, Peralta, M, and Matos, MG. Healthy lifestyle in children and adolescents and its association with subjective health complaints: findings from 37 countries and regions from the HBSC study. Int J Environ Res Public Health. (2019) 16:292. doi: 10.3390/ijerph16183292
44. De Graaf, H, Vanwesenbeeck, I, and Meijer, S. Educational differences in adolescents' sexual health: a pervasive phenomenon in a national Dutch sample. J Sex Res. (2015) 52:747–57. doi: 10.1080/00224499.2014.945111
45. Madkour, AS, Farhat, T, Halpern, CT, Godeau, E, and Gabhainn, SN. Early adolescent sexual initiation as a problem behavior: a comparative study of five nations. J Adolesc Health. (2010) 47:389–98. doi: 10.1016/j.jadohealth.2010.02.008
46. de Graaf, H, Schouten, F, van Dorsselaer, S, Költő, A, Ball, J, Stevens, GW, et al. Trends and the gender gap in the reporting of sexual initiation among 15-year-olds: a comparison of 33 European countries. J Sex Res. (2024) 20:1–10. doi: 10.1080/00224499.2023.2297906
47. Imamura, M, Tucker, J, Hannaford, P, Da Silva, MO, Astin, M, Wyness, L, et al. Factors associated with teenage pregnancy in the European Union countries: a systematic review. Eur J Pub Health. (2007) 17:630–6. doi: 10.1093/eurpub/ckm014
48. Gromada, A, Rees, G, and Chzhen, Y. Worlds of influence: Understanding what shapes child well-being in rich countries. Innocenti Report Card 16. Florence: UNICEF Office of Research-Innocenti (2020).
49. WHO. The adolescent health indicators recommended by the global action for measurement of adolescent health: Guidance for monitoring adolescent health at country, regional and global levels. Geneva: World Health Organization (2024).
50. Brons, ME, Helbich, M, Elgar, FJ, Lenzi, M, Bolt, G, Dierckens, M, et al. School socioeconomic status and psychological complaints among adolescents in 44 countries: the mediating role of schoolwork pressure and classmate support and the moderating role of family SES and country-level income inequality. Soc Sci Med. (2024) 354:117062. doi: 10.1016/j.socscimed.2024.117062
51. Torchyan, AA, Houkes, I, and Bosma, H. Income inequality and socioeconomic differences in bullying perpetration among adolescents in post-communist countries of Europe: findings from the HBSC study. Prev Med Rep. (2024) 37:102540. doi: 10.1016/j.pmedr.2023.102540
52. Moor, I, Herke, M, Markert, J, Böhm, M, Reiß, F, Bilz, L, et al. Trends in health inequalities in childhood and adolescence in Germany: results of the HBSC study 2009/10–2022. J Health Monitoring. (2024) 9:79–98. doi: 10.25646/11876
53. Queral, J, Wargers, A, Tarro, L, Llauradó, E, Solà, R, and Jansen, W. Changes over time of fruit, vegetable and sweets consumption among European adolescents and associations with sociodemographic characteristics: an HBSC study. J Public Health. (2024) 46:392–402. doi: 10.1093/pubmed/fdae033
54. Dierckens, M, Deforche, B, De Clercq, B, Weinberg, D, Stevens, GW, Chatelan, A, et al. Country-level sociocultural context and socioeconomic inequalities in adolescent dietary behaviours: a multilevel analysis in 21 European countries. Appetite. (2024) 198:107339. doi: 10.1016/j.appet.2024.107339
55. Guthold, R, Stevens, GA, Riley, LM, and Bull, FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1· 6 million participants. Lancet Child Adolescent Health. (2020) 4:23–35. doi: 10.1016/S2352-4642(19)30323-2
56. Hulbert, S, Eida, T, Ferris, E, Hrytsenko, V, and Kendall, S. HBSC England National Report: Findings from the 2001–2022 HBSC study for England. Kent: University of Kent (2023).
57. López-Gil, JF, Mesas, AE, Álvarez-Bueno, C, Pascual-Morena, C, Saz-Lara, A, and Cavero-Redondo, I. Association between eating habits and perceived school performance: a cross-sectional study among 46,455 adolescents from 42 countries. Front Nutr. (2022) 9:797415. doi: 10.3389/fnut.2022.797415
58. Pedroni, C, Dujeu, M, Lebacq, T, Desnouck, V, Holmberg, E, and Castetbon, K. Alcohol consumption in early adolescence: associations with sociodemographic and psychosocial factors according to gender. PLoS One. (2021) 16:e0245597. doi: 10.1371/journal.pone.0245597
59. Holstein, BE, Andersen, A, Damsgaard, MT, Due, P, Bast, LS, and Rasmussen, M. Trends in socioeconomic differences in daily smoking among 15-year-old Danes 1991–2014. Scand J Public Health. (2020) 48:667–73. doi: 10.1177/1403494819848284
60. Helmer, SM, Burkhart, G, Matias, J, Buck, C, Engling Cardoso, F, and Vicente, J. “Tell me how much your friends consume”—personal, behavioral, social, and attitudinal factors associated with alcohol and cannabis use among European school students. Int J Environ Res Public Health. (2021) 18:1684. doi: 10.3390/ijerph18041684
61. Cosma, A, Bjereld, Y, Elgar, FJ, Richardson, C, Bilz, L, Craig, W, et al. Gender differences in bullying reflect societal gender inequality: a multilevel study with adolescents in 46 countries. J Adolesc Health. (2022) 71:601–8. doi: 10.1016/j.jadohealth.2022.05.015
62. Kim, SS, Craig, WM, King, N, Bilz, L, Cosma, A, Molcho, M, et al. Bullying, mental health, and the moderating role of supportive adults: a cross-national analysis of adolescents in 45 countries. Int J Public Health. (2022) 67:1604264. doi: 10.3389/ijph.2022.1604264
63. Stevely, AK, Gray, LA, Fairbrother, H, Fenton, L, Henney, M, Kersbergen, I, et al. A latent class analysis of international change and continuity in adolescent health and wellbeing: a repeat cross-sectional study. PLoS One. (2024) 19:e0305124. doi: 10.1371/journal.pone.0305124
64. Moore, G, Donaldson, C, Ouerghi, S, Hawkins, J, Anthony, R, Angel, L, et al. School and family level socioeconomic status, school connectedness and health and wellbeing among 9–11 year olds: Cross sectional analysis of the student health and wellbeing survey in Wales. Child Indic Res. (2024) 17:2769–87. doi: 10.1007/s12187-024-10179-6
65. Residori, C, Lopes Ferreira, J, Goedert Mendes, F, and Catunda, C. COVID-19 impact and trends in health of school-aged children from 2006-2022 in Luxembourg-report on the Luxembourg HBSC survey 2022. (2022).
66. Weinberg, D, Stevens, GW, Peeters, M, Visser, K, Frankenhuis, W, and Finkenauer, C. The role of social cognitions in the social gradient in adolescent mental health: a longitudinal mediation model. Dev Psychopathol. (2024) 36:953–66. doi: 10.1017/S0954579423000214
67. Mazur, J, Kleszczewska, DW, Porwit, K, Zawadzka, D, and Małkowska-Szkutnik, A. Quality of life in 13-year-olds depending on health status, residential neighbourhood deprivation and social capital-results from the polish HBSC study 2010-2018. Ann Agric Environ Med. (2023) 30:474–82. doi: 10.26444/aaem/161852
68. Cerqueira, A, Botelho Guedes, F, Gaspar, T, Godeau, E, and Gaspar de Matos, M. Shedding light on the lifestyle and participation of Portuguese adolescents with chronic conditions—data from the HBSC 2018 study. Children. (2022) 9:717. doi: 10.3390/children9111717
69. Lipari, D, Bocci, BM, Rivieri, C, Frongillo, E, Miserendino, A, Pammolli, A, et al. Trend of correlations between psychological symptoms and socioeconomic inequalities: HBSC cross-sectional study among Tuscan adolescents from 2006 to 2018. (2023).
70. Alferink, W. The influence of family support and living in an advantaged neighborhood on adolescent alcohol use in the Netherlands (2022).
71. Winter, K, Moor, I, Markert, J, Bilz, L, Bucksch, J, Dadaczynski, K, et al. Concept and methodology of the health behaviour in school-aged children (HBSC) study–insights into the current 2022 survey and trends in Germany. J Health Monitoring. (2024) 9:99–117. doi: 10.25646/11878
72. Gaspar, S, Guedes, FB, Cerqueira, A, Gaspar, T, Machado, MC, and de Matos, MG. Health literacy and medication health literacy in adolescents: highlights from HBSC/WHO. Eur J Educ. (2024) 59:e12686. doi: 10.1111/ejed.12686
73. Reiß, F, Behn, S, Erhart, M, Strelow, L, Kaman, A, Ottová-Jordan, V, et al. Subjective health and psychosomatic complaints of children and adolescents in Germany: results of the HBSC study 2009/10–2022. J Health Monitoring. (2024) 9:7–22. doi: 10.25646/11868
74. Roman-Juan, J, Jensen, MP, and Miró, J. Increases in sleep difficulties and psychological symptoms are associated with the increase of chronic back pain in adolescents: the HBSC study 2002 to 2018. J Pain. (2024) 25:407–17. doi: 10.1016/j.jpain.2023.09.004
75. Khan, A, Khan, SR, and Lee, E-Y. Association between lifestyle behaviours and mental health of adolescents: evidence from the Canadian HBSC surveys, 2002–2014. Int J Environ Res Public Health. (2022) 19:6899. doi: 10.3390/ijerph19116899
76. Leurent, B, Dodd, M, Allen, E, Viner, R, Scott, S, and Bonell, C. Is positive school climate associated with better adolescent mental health? Longitudinal study of young people in England. SSM-Mental Health. (2021) 1:100033. doi: 10.1016/j.ssmmh.2021.100033
77. Bellisario, V, Bono, R, Squillacioti, G, Caputo, M, Gintoli, I, Borracino, A, et al. Urbanization and greenness in HBSC survey: association with overweight and obesity in adolescents. Eur J Pub Health. (2020) 30:712. doi: 10.1093/eurpub/ckaa165.712
78. Abrams, R, Nordmyr, J, and Forsman, AK. Promoting sexual health in schools: a systematic review of the European evidence. Front Public Health. (2023) 11:1193422. doi: 10.3389/fpubh.2023.1193422
79. Niland, R, Flinn, C, and Nearchou, F. Assessing the role of school-based sex education in sexual health behaviours: a systematic review. Cogent Psychol. (2024) 11:2309752. doi: 10.1080/23311908.2024.2309752
80. Feng, B, Xu, K, and Zhou, P. Association between vigorous physical activity and life satisfaction in adolescents. Front Public Health. (2022) 10:944620. doi: 10.3389/fpubh.2022.944620
81. Inchley, JC, Stevens, GW, Samdal, O, and Currie, DB. Enhancing understanding of adolescent health and well-being: the health behaviour in school-aged children study. J Adolesc Health. (2020) 66:S3–5. doi: 10.1016/j.jadohealth.2020.03.014
82. Nagy-Pénzes, G, Vincze, F, Víghné Arany, Á, and Bíró, É. Impact of a primary school health promotion Programme on adolescents’ health behaviour and well-being. Children. (2024) 11:919. doi: 10.3390/children11080919
83. Roșioară, A-I, Năsui, BA, Ciuciuc, N, Sîrbu, DM, Curșeu, D, Pop, AL, et al. Status of healthy choices, attitudes and health education of children and Young people in Romania—a literature review. Medicina. (2024) 60:725. doi: 10.3390/medicina60050725
84. Chu, M, Lee, CY, Li, X, Zhao, Z, Gao, M, and Chiang, YC. Association of Friendly School and Family Contexts and reducing health risk behaviors among adolescents: a Cross-National Study in Europe, North America, and China. J Sch Health. (2024) 94:57–68. doi: 10.1111/josh.13331
85. Coene, B. The role of school climate in preventing cyberbully perpetration: Evaluating the impact of student-teacher relationships, classmate relationships, and friend support (2024).
86. Hardley, SH. Wellbeing for all: How a Scottish secondary school conceptualises health and wellbeing support for socioeconomically disadvantaged students. (2024).
87. Zheng, Y, Panayiotou, M, Currie, D, Yang, K, Bagnall, C, Qualter, P, et al. The role of school connectedness and friend contact in adolescent loneliness, and implications for physical health. Child Psychiatry Hum Dev. (2024) 55:851–60. doi: 10.1007/s10578-022-01449-x
88. Hoffman, LK. The relationship between student health behaviors, demographic variables and suicide: A secondary analysis of health behaviors in school-age children (HBSC 2009–2010). (2020).
89. Fairclough, SJ, Clifford, L, Foweather, L, Knowles, ZR, Boddy, LM, Ashworth, E, et al. Move well, feel good: feasibility and acceptability of a school-based motor competence intervention to promote positive mental health. PLoS One. (2024) 19:e0303033. doi: 10.1371/journal.pone.0303033
90. Goss, HR, Smith, C, Hickey, L, Issartel, J, Morrissey, J, Murrin, C, et al. Using co-design to develop a health literacy intervention with socially disadvantaged adolescents. Int J Environ Res Public Health. (2022) 19:4965. doi: 10.3390/ijerph19094965
91. Cefai, C, Simões, C, and Caravita, S. A systemic, whole-school approach to mental health and well-being in schools in the EU. (2021).
92. Markkanen, I. Students’ perceptions of the quality of school life, health, and health behaviours in Finnish comprehensive schools. Jyväskylä: University of Jyväskylä (2022).
93. Lazzeri, G, Ahluwalia, N, Niclasen, B, Pammolli, A, Vereecken, C, Rasmussen, M, et al. Trends from 2002 to 2010 in daily breakfast consumption and its socio-demographic correlates in adolescents across 31 countries participating in the HBSC study. PLoS One. (2016) 11:e0151052. doi: 10.1371/journal.pone.0151052
94. Havaei, F, Doull, M, and Saewyc, E. A trend analysis of sexual health behaviours of a national sample of Canadian adolescents using HBSC data from 2002–2014. Can J Hum Sex. (2019) 28:17–25. doi: 10.3138/cjhs.2018-0035
95. Young, H, Burke, L, and Nic, GS. Sexual intercourse, age of initiation and contraception among adolescents in Ireland: findings from the health behaviour in school-aged children (HBSC) Ireland study. BMC Public Health. (2018) 18:362–17. doi: 10.1186/s12889-018-5217-z
96. Vaičiūnas, T, Žemaitaitytė, M, Lange, S, Štelemėkas, M, Oja, L, Petkevičienė, J, et al. Trends in adolescent substance use: analysis of HBSC data for four eastern European countries, 1994–2018. Int J Environ Res Public Health. (2022) 19:15457. doi: 10.3390/ijerph192315457
97. Šumskas, L, Zaborskis, A, and Grabauskas, V. Social determinants of smoking, alcohol and drug use among Lithuanian school-aged children: results from 5 consecutive HBSC surveys, 1994–2010. Medicina. (2012) 48:87. doi: 10.3390/medicina48110087
98. Bezborodovs, Ņ, and Villeruša, A, Subjective health status, health behaviours, and high-risk behaviours as factors associated with adolescent mental health. SHS web of conferences (2024).
99. Sendatzki, S, Helmchen, RM, Moor, I, Sudeck, G, Dadaczynski, K, and Rathmann, K. Health literacy of students in Germany - results of the HBSC study 2022. J Health Monitoring. (2024) 9:23–41. doi: 10.25646/11870
100. Goedert Mendes, F, Lopes Ferreira, J, Residori, C, and Catunda, C. Health behaviours of school-aged children in Luxembourg-report on the Luxembourg HBSC survey 2022. (2022).
101. Barnett, E, and de Koning, K In: V Francis, editor. Health & HIV/AIDS education in primary & secondary schools in Africa & Asia. Policies, Practice & Potential: Case studies from Pakistan, India, Uganda, Ghana. Education Research. Budapest: ERIC (1995)
102. Chowa, G, Masa, R, Manzanares, M, and Bilotta, N. A scoping review of positive youth development programming for vulnerable and marginalized youth in low-and middle-income countries. Child Youth Serv Rev. (2023) 154:107110. doi: 10.1016/j.childyouth.2023.107110
103. John, NA, Stoebenau, K, Ritter, S, Edmeades, J, and Balvin, N, UNICEF Gender socialization during adolescence in low-and middle-income countries: Conceptualization, influences and outcomes. (2017).
104. Kim, SW. Meta-analysis of parental involvement and achievement in east Asian countries. Educ Urban Soc. (2020) 52:312–37. doi: 10.1177/0013124519842654
105. Hartas, D. Patterns of parental involvement in selected OECD countries: Cross-national analyses of PISA. Eur J Educ Res. (2015) 201688:185–95. doi: 10.12973/eu-jer.4.4.185
106. Lengle, JM. Intersectionality and adolescent dietary behavior in Flanders: An analysis of the interaction between family affluence, gender, and migration background (2021).
107. Currie, D, Samdal, O, Torsheim, T, and Augustson, L. Growing up unequal: gender and socioeconomic differences in young people's health and well-being In: J Inchley, D Currie, and T Young, editors. Health behaviour in school-aged children (HBSC) study: International report from the 2013/2014 survey. Geneva: World Health Organization (2016)
108. WHO. Growing up unequal: gender and socioeconomic differences in young people's health and well-being. Growing up unequal: gender and socioeconomic differences in young people's health and well-being. Geneva: World Health Organization (2016).
109. Organization WH. Spotlight on adolescent health and well-being. Findings from the 2017/2018 health behaviour in school-aged children (HBSC) survey in Europe and Canada. Int. Rep. (2020) 66:S1–2. doi: 10.1016/j.jadohealth.2020.03.024
110. Singh, S, Darroch, JE, and Frost, JJ. Socioeconomic disadvantage and adolescent women's sexual and reproductive behavior: the case of five developed countries. Fam Plan Perspect. (2001) 33:251. doi: 10.2307/3030192
111. Kendall, GE, van Eekelen, J, Mattes, E, and Li, J Children in harm’s way: A global issue as important as climate change. Forum on Public Policy (2009).
112. Cianconi, P, Betrò, S, and Janiri, L. The impact of climate change on mental health: a systematic descriptive review. Front Psych. (2020) 11:490206. doi: 10.3389/fpsyt.2020.00074
113. Berry, HL, Bowen, K, and Kjellstrom, T. Climate change and mental health: a causal pathways framework. Int J Public Health. (2010) 55:123–32. doi: 10.1007/s00038-009-0112-0
114. Reid Chassiakos, YL, Radesky, J, Christakis, D, Moreno, MA, Cross, C, Hill, D, et al. Children and adolescents and digital media. Pediatrics. (2016) 138:2593. doi: 10.1542/peds.2016-2593
115. Chatelan, A, Rouche, M, Kelly, C, Fismen, A-S, Pedroni, C, Desbouys, L, et al. Tax on sugary drinks and trends in daily soda consumption by family affluence: an international repeated cross-sectional survey among European adolescents. Am J Clin Nutr. (2023) 117:576–85. doi: 10.1016/j.ajcnut.2023.01.011
116. Silva, CF, Rocha, P, and Santos, P. Consumption of licit and illicit substances in Portuguese young people: a population-based cross-sectional study. J Int Med Res. (2018) 46:3042–52. doi: 10.1177/0300060518767588
117. Boniel-Nissim, M, Marino, C, Galeotti, T, Blinka, L, Ozoliņa, K, Craig, W, et al. A focus on adolescent social media use and gaming in Europe, Central Asia and Canada: Health behaviour in school-aged children international report from the 2021/2022 survey. Geneva: WHO (2024).
118. Abdoli, M, Scotto Rosato, M, Desousa, A, and Cotrufo, P. Cultural differences in body image: a systematic review. Soc Sci. (2024) 13:305. doi: 10.3390/socsci13060305
119. Lazzeri, G, Vieno, A, Charrier, L, Spinelli, A, Ciardullo, S, Pierannunzio, D, et al. The methodology of the Italian health behaviour in school-aged children (HBSC) 2018 study and its development for the next round. J Prev Med Hyg. (2022) 62:E926. doi: 10.15167/2421-4248/jpmh2021.62.4.2343
120. Samdal, O, Budin-Ljøsne, I, Haug, E, Helland, T, Kjostarova-Unkovska, L, Bouillon, C, et al. Encouraging greater empowerment for adolescents in consent procedures in social science research and policy projects. Obes Rev. (2023) 24:e13636. doi: 10.1111/obr.13636
121. Nesrallah, S, Klepp, KI, Budin-Ljøsne, I, Luszczynska, A, Brinsden, H, Rutter, H, et al. Youth engagement in research and policy: the CO-CREATE framework to optimize power balance and mitigate risks of conflicts of interest. Obes Rev. (2023) 24:e13549. doi: 10.1111/obr.13549
122. Ricardo, LIC, Wendt, A, dos Santos, CC, Mielke, GI, Brazo-Sayavera, J, Khan, A, et al. Gender inequalities in physical activity among adolescents from 64 global south countries. J Sport Health Sci. (2022) 11:509–20. doi: 10.1016/j.jshs.2022.01.007
123. Larson, KE, Nguyen, AJ, Solis, MGO, Humphreys, A, Bradshaw, CP, and Johnson, SL. A systematic literature review of school climate in low and middle income countries. Int J Educ Res. (2020) 102:101606. doi: 10.1016/j.ijer.2020.101606
124. Okoye, HU. Intersecting social statuses, health inequities, and macro-social influences on HIV risk behaviour among adolescents in sub-Saharan Africa: A structural determinants exploration. Vancouver, BC: University of British Columbia (2024).
125. Roberts, C, Currie, C, Samdal, O, Currie, D, Smith, R, and Maes, L. Measuring the health and health behaviours of adolescents through cross-national survey research: recent developments in the health behaviour in school-aged children (HBSC) study. J Public Health. (2007) 15:179–86. doi: 10.1007/s10389-007-0100-x
Keywords: adolescent health, cultural health paradigms, health surveys, social determinants of health, health policies
Citation: Alshahrani MS, Gannamaneni VK, Kakaraparthi VN, Alahmari KA, Alkhamis B, Reddy RS, Tedla JS, Dixit S, Kakaraparthi L and Nambi G (2025) Health behaviors in school-aged children: global trends in education, socioeconomic status, and adolescent health. Front. Public Health. 13:1514386. doi: 10.3389/fpubh.2025.1514386
Edited by:
Morteza Taheri, University of Tehran, IranReviewed by:
Maedeh Ahmadpour, PhD University of Tehran, IranRoya Khorrami Estakhri, Guilan University of Medical Sciences, Iran
Copyright © 2025 Alshahrani, Gannamaneni, Kakaraparthi, Alahmari, Alkhamis, Reddy, Tedla, Dixit, Kakaraparthi and Nambi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Venkata Nagaraj Kakaraparthi, dm5yYWpAa2t1LmVkdS5zYQ==
 Mastour Saeed Alshahrani
Mastour Saeed Alshahrani Vamsi Krishna Gannamaneni
Vamsi Krishna Gannamaneni Venkata Nagaraj Kakaraparthi
Venkata Nagaraj Kakaraparthi Khalid A. Alahmari
Khalid A. Alahmari Batool Alkhamis
Batool Alkhamis Ravi Shankar Reddy
Ravi Shankar Reddy Jaya Shanker Tedla
Jaya Shanker Tedla Snehil Dixit
Snehil Dixit Lalitha Kakaraparthi
Lalitha Kakaraparthi Gopal Nambi
Gopal Nambi