- 1The Working Group to Analyze the Emergency Medical Care System in Osaka Prefecture, Osaka, Japan
- 2Division of Environmental Medicine and Population Sciences, Department of Social and Environmental Medicine, Osaka University Graduate School of Medicine, Suita, Japan
- 3Department of Traumatology and Acute Critical Medicine, Osaka University Graduate School of Medicine, Suita, Japan
- 4Osaka Prefectural Government, Osaka, Japan
- 5Rinku General Medical Center, Izumisano, Japan
Background: This study aimed to assess the influence of the COVID-19 pandemic on emergency medical services for older patients who were transported to hospitals by ambulance.
Methods: This descriptive retrospective study was conducted between January 2019 and December 2022, using the Osaka Emergency Information Research Intelligent Operation Network system. All patients aged ≥65 years who were transported by ambulance to hospitals in Osaka Prefecture for acute diseases were included. The outcomes were the number of older patients transported by ambulance, the number of difficulties obtaining patient acceptance at hospitals, and the number of deaths following hospitalization. We calculated the incidence rate ratio (IRR) and its associated 95% confidence interval (CI) for each year of the study period (2020, 2021, and 2022) using Poisson regression, with 2019 as the control year.
Results: Compared to 2019, the numbers of older patients transported for acute disease were 186,218 (IRR, 0.92; 95% CI: 0.92–0.93) in 2020, 186,955 (0.93, 0.92–0.93) in 2021, and 214,048 (1.06, 1.05–1.07) in 2022. Difficulty obtaining patient acceptance increased over time (6,668 in 2020, 9,894 in 2021, and 22,790 in 2022). The number of deaths were 8,660 (1.01, 0.98–1.04) in 2020, 9,754 (1.14, 1.10–1.17) in 2021, and 11,050 (1.29, 1.25–1.32) in 2022.
Conclusion: The number of older patients transported to emergency departments in Osaka Prefecture for acute diseases increased in 2022 compared with 2019. Difficulties obtaining patient acceptance and in-hospital deaths also increased over this period.
1 Introduction
Coronavirus disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was first identified in China in December 2019, before the infection spread rapidly worldwide (1). On March 11, 2020, the World Health Organization officially declared COVID-19 a pandemic (2). Although there were several known risk factors for developing severe COVID-19, older age was considered the primary one (3, 4). Mortality from COVID-19 was higher in older patients, and mortality increased with age (5, 6).
A number of reports have indicated that the COVID-19 pandemic had significant impacts on emergency medical services (EMSs) worldwide, often comprising longer transport times and worse outcomes following hospitalization (7–10). In Singapore during the pandemic (January–May 2020), the patients waited longer for EMS and pre-hospital return of spontaneous circulation was less likely (9). In Korea, multivariable logistic regression analysis showed that the COVID-19 pandemic was significantly associated with higher in-hospital mortality among patients in the emergency department (10). Older adults tend to make up a large proportion of patients in emergency departments. In Osaka Prefecture, Japan, for example, those aged ≥65 years account for approximately 60% of all patients transported to hospital emergency departments (11). Therefore, it may be important to evaluate the overall EMS system with a focus on older patients, as this group are generally more vulnerable than other age groups to health problems, yet may not have been transported quickly and appropriately to hospitals during the COVID-19 pandemic.
Osaka Prefecture is the largest metropolitan area in western Japan, with a population of approximately 8.8 million people. The annual number of ambulance calls in this region was 500,000 in 2019 (12, 13). The Osaka Emergency Information Research Intelligent Operation Network (ORION) system, a population-based emergency transport registration system in Osaka, includes pre-hospital care records and post-transport outcomes (14). This study aimed to describe the actual situation regarding emergency transportation of older patients to hospitals by EMS before and after the COVID-19 pandemic in Osaka Prefecture, and to assess the effect of the pandemic on this type of transportation, using the ORION database.
2 Materials and methods
2.1 Study design, population, and setting
This was a descriptive retrospective study with a period spanning January 1, 2019, to December 31, 2022. We used the database of the population-based registry of emergency department patients, comprising both ambulance and in-hospital records managed by ORION. This database is operated by Osaka Prefecture and covers all patients transported to critical care centers and emergency hospitals in the prefecture. Information concerning the ORION database has been previously described in detail (14, 15). Briefly, the ambulance crew at the scene operate the ORION smartphone application for each emergency patient. All data entered into the mobile app are recorded, including vital signs and the time between receipt of the request and admission to the hospital. The smartphone app data are then stored on the ORION cloud server. Cooperating with the dispatched ambulance crew, the data manager at each fire department directly enters and uploads the ambulance records for each emergency patient, which can then be linked to the app data. Operators at each hospital also directly input or upload patient data, such as diagnoses and outcomes, after patients are admitted, and the results compiled by the ORION system are fed back to each fire department and emergency hospital. The ORION system is installed in all fire departments and emergency hospitals in Osaka Prefecture. Its data are administrative records that are anonymized without specific personal information such as patient names, birth dates, and addresses. Therefore, the requirement to obtain informed patient consent was waived for this study. This study was approved by the ethics committee of Osaka University Graduate School of Medicine (approval no.: 15003). All procedures were conducted in accordance with the Declaration of Helsinki.
In 2020, 8,837,685 people lived in the 1905 km2 area of Osaka Prefecture. Of these, 2,441,984 (27.6%) were aged ≥65 years (12). This study defined older patients as those aged 65 years or older, according to the protocol used in previous related studies, and focused on this population (16).
2.2 Measurements
Reasons for ambulance calls were divided into: “fire accident,” “natural disaster,” “water accident,” “traffic accident involving car, ship, or aircraft,” “injury, poisoning, and disease caused by industrial accident,” “disease and injury caused by sports,” “other injury,” “trauma caused by assault,” “self-induced injury,” “acute disease,” and “others” (14, 15). Patients who were transported as inter-hospital relocations were excluded. We focused on patients whose reasons for calling an ambulance were “acute disease” and who were successfully transported and admitted to a hospital. We also focused on any difficulties patients experienced obtaining acceptance to hospitals, and defined such cases as those in which ambulance crews made ≥4 phone calls to the hospitals before obtaining patient acceptance, as well as those in which the crews stayed at the scene for >30 min, based on national standards (17). Post-hospitalization diagnoses were classified according to International Classification of Diseases, 10th Revision codes (ICD-10), which classified COVID-19 as category “U” (18). For the “surge” periods during which the COVID-19 epidemic spread through the region, Osaka Prefecture recorded the first surge between January 29, 2020 and June 13, 2020; second surge between June 14, 2020 and October 9, 2020; third surge between October 10, 2020 and February 28, 2021; fourth surge between March 1, 2021 and June 20, 2021; fifth surge between June 21, 2021 and December 16, 2021; sixth surge between December 17, 2021 and June 24, 2022; seventh surge between June 25, 2022 and September 26, 2022; and eighth surge between September 27, 2022 and May 8, 2023 (19).
2.3 Outcomes
The outcome measures of this study were the number of older patients transported to emergency departments for acute disease, the number of deaths among them, the number of difficulties obtaining patient acceptance from hospitals, and the time interval from ambulance call to arrival on scene. The patients’ outcomes after 21 days of hospitalization were also recorded and classified into four categories: continued hospitalization, discharged, changed hospital, and death.
2.4 Statistical analysis
Based on previous related studies, we used the 2019 outcome measures as a reference (i.e., the control period before the COVID-19 pandemic) and compared them by year and month for 2020 (the first year of the pandemic), 2021 (the second year), and 2022 (the third year) (11). We calculated the incidence rate ratio (IRR) and its associated 95% confidence interval (CI) by year and month for 2020, 2021, and 2022 using a Poisson regression model with 2019 serving as the control year and the census population of Osaka Prefecture in 2020 as the denominator (12). This is because the number of emergency transports in Osaka Prefecture was considered to be very low relative to its population. As there were no cases with an ICD-10 diagnosis of “U” in 2019, the IRRs for 2021 and 2022 were calculated based on 2020 for these cases. Difference in the time intervals from ambulance call to arrival on scene by year was assessed using a Jonckheere-Terpstra test. All statistical analyses were performed using STATA MP version 16.0 (StataCorp, College Station, TX, USA).
3 Results
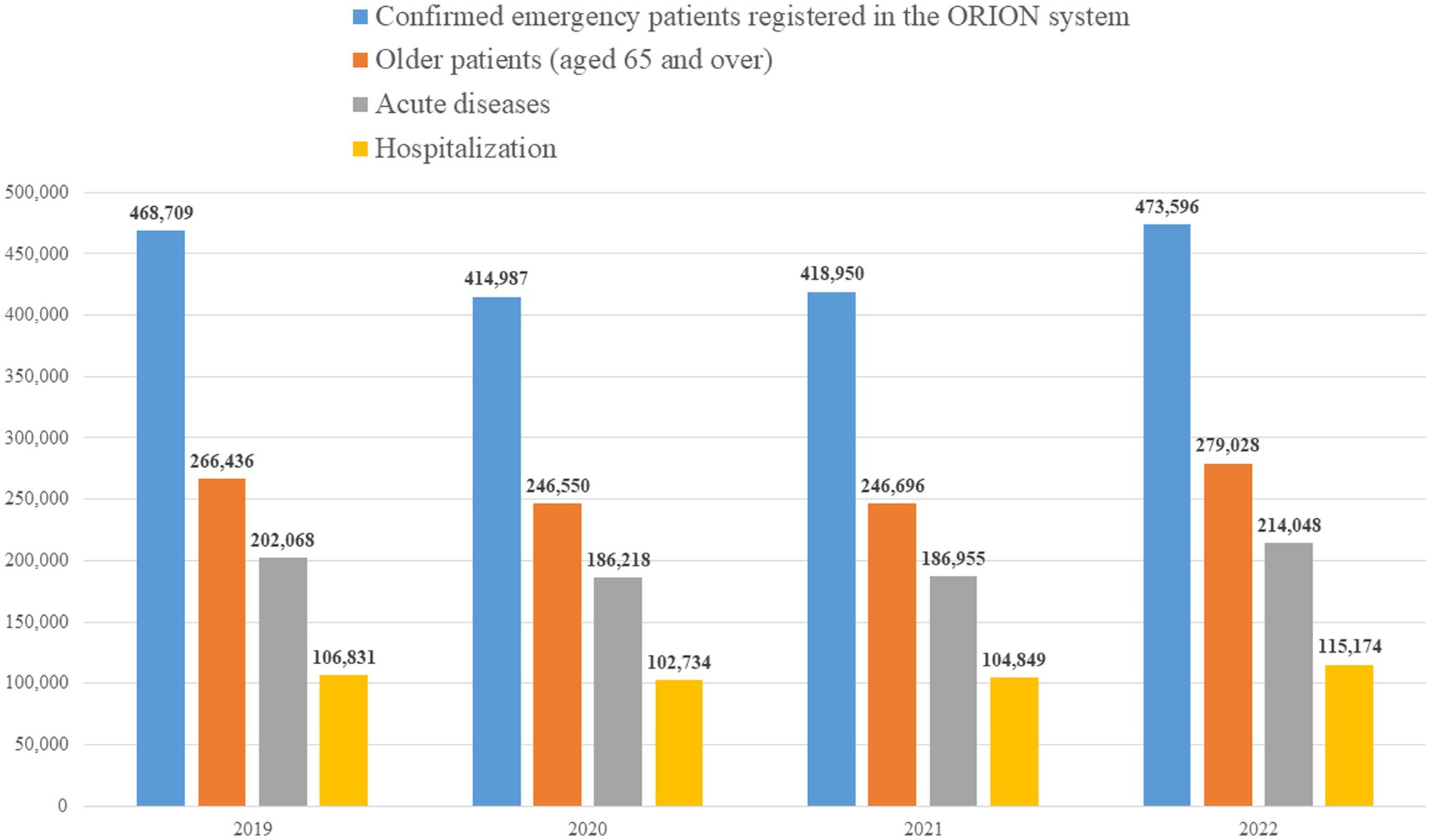
The numbers of older patients were 266,436 in 2019, 246,550 in 2020, 246,696 in 2021, and 279,028 in 2022 (Figure 1). The mean and standard deviation of the time intervals from ambulance call to arrival on scene were 7.4 ± 2.7 min in 2019, 7.5 ± 2.7 min in 2020, 7.9 ± 3.0 min in 2021, and 8.8 ± 4.4 min in 2022 and it increased significantly over year (P for trend < 0.05).
Table 1 shows the number of older emergency patients and IRRs (with associated 95% CIs) in each year, by reason for the ambulance call, in 2019–2022. For “acute disease” as the reason for calling an ambulance, the number of emergency patients decreased significantly in 2020 (IRR: 0.92, 95% CI: 0.92–0.93) and in 2021 (IRR: 0.93, 95% CI: 0.92–0.93) compared with 2019; however, it increased significantly in 2022 (IRR: 1.06, 95% CI: 1.05–1.07).
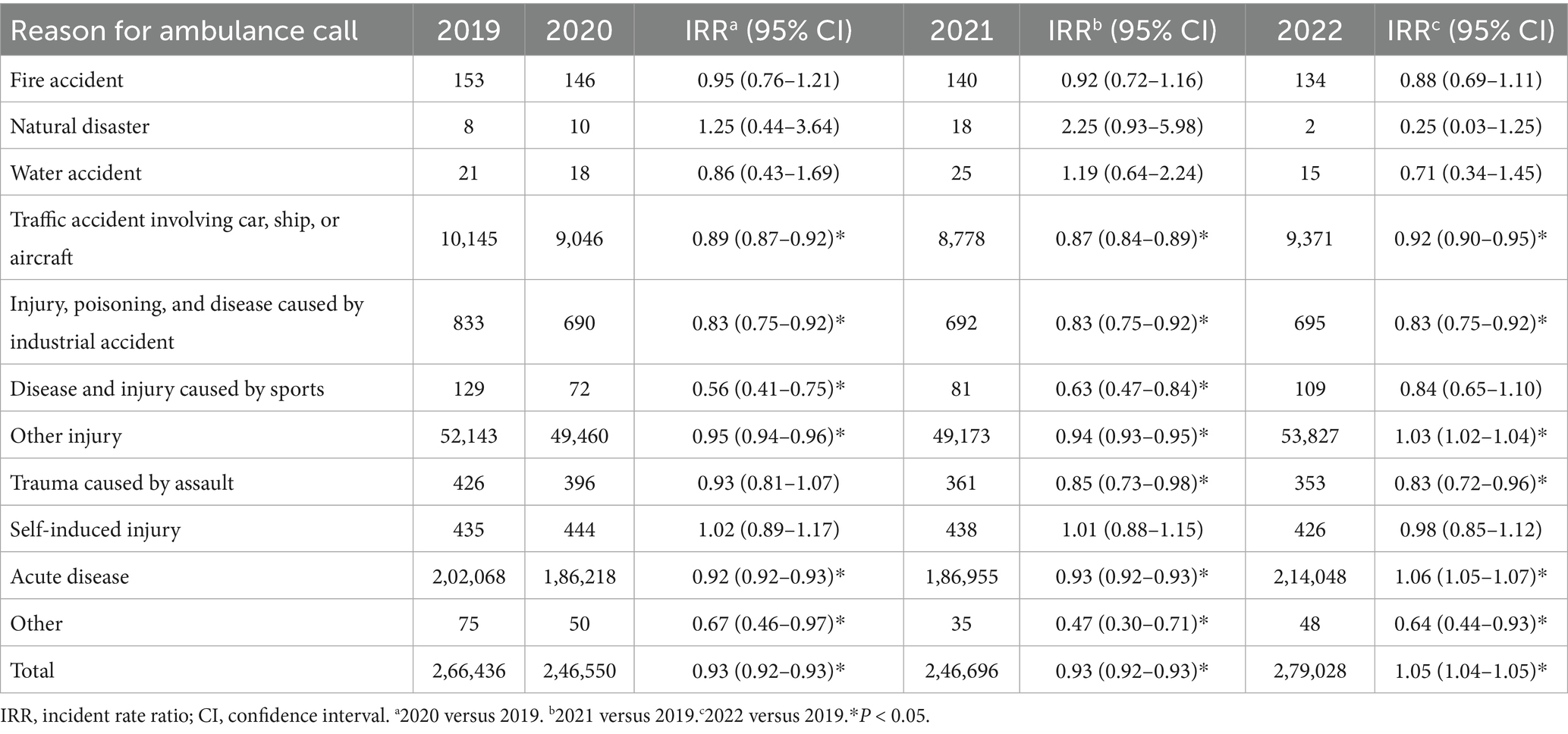
Table 1. The number of emergency patients registered in the Osaka emergency information research intelligent operation network system in 2019–2022.
The number of older emergency patients transported for acute disease, their admissions, and the IRRs (95% CIs) for each month in 2019–2022 are shown in Table 2. Significant increases in older emergency patients transported for acute diseases were seen in July 2022, which corresponds to the seventh COVID-19 surge in Japan, when compared to July 2019, and December 2022, which corresponds to the eighth surge, when compared to December 2019. The number of hospitalized older patients transported for acute disease decreased significantly in 2020 (IRR: 0.96, 95% CI: 0.95–0.97) and 2021 (IRR: 0.98, 95% CI: 0.97–0.99), compared to 2019; however, it increased significantly in 2022 (IRR: 1.08, 95% CI: 1.07–1.09). In 2022, significant increases were observed in almost every month compared with that in 2019.
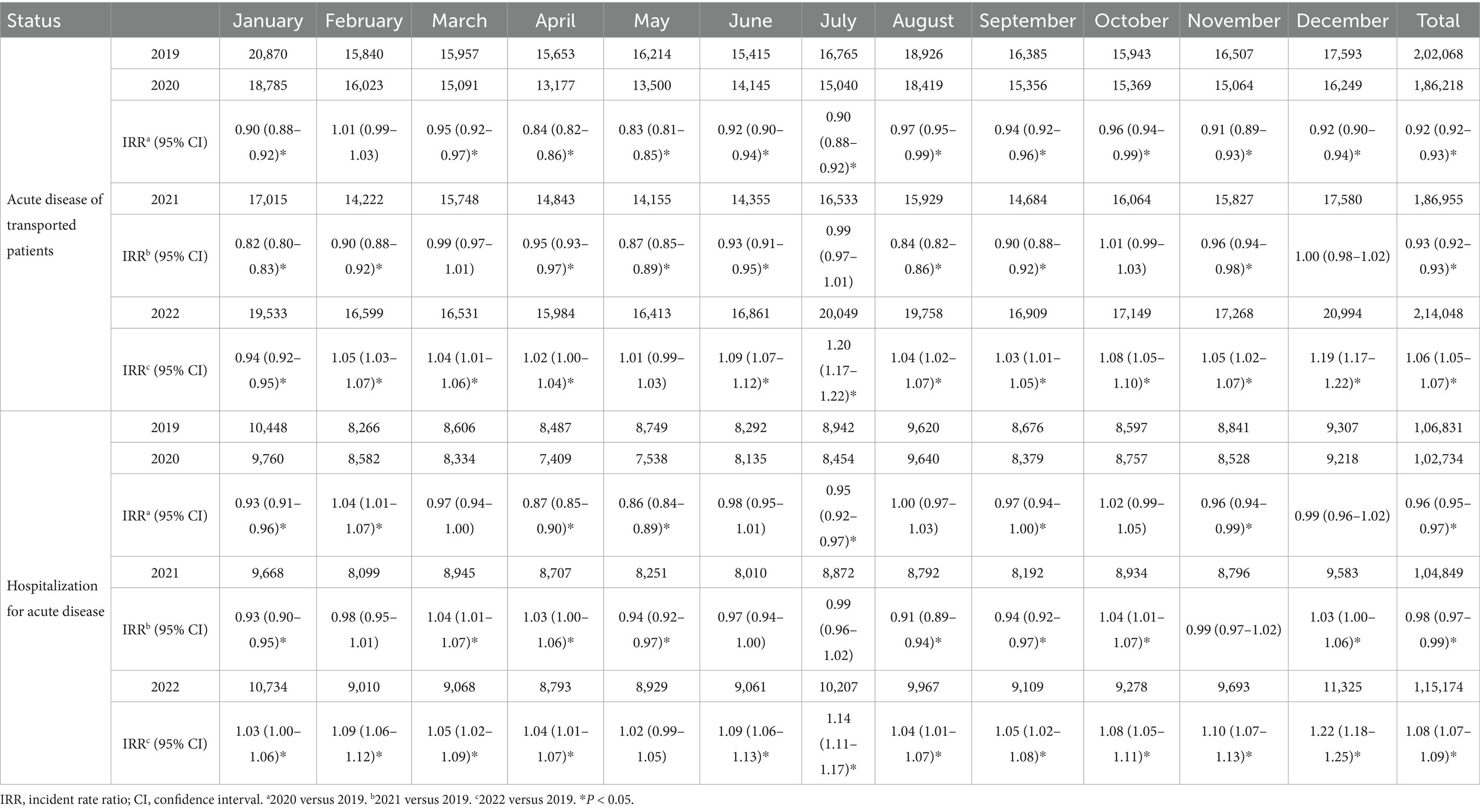
Table 2. The number of patients transported to emergency departments for acute diseases and hospitalized in Osaka in 2019–2022.
The number of difficulties obtaining patient acceptance from hospitals increased significantly in 2020 (IRR: 1.43, 95% CI: 1.38–1.49), 2021 (IRR: 2.13, 95% CI: 2.05–2.20), and 2022 (IRR: 4.90, 95% CI: 4.74–5.05) compared to 2019 (Table 3). Compared to 2019, the number of difficulties obtaining patient acceptance from hospitals increased significantly in all months of 2022. This was particularly true in August, corresponding to the seventh surge, and December, during the eighth surge. Similar results were observed for the hospitalized cases.
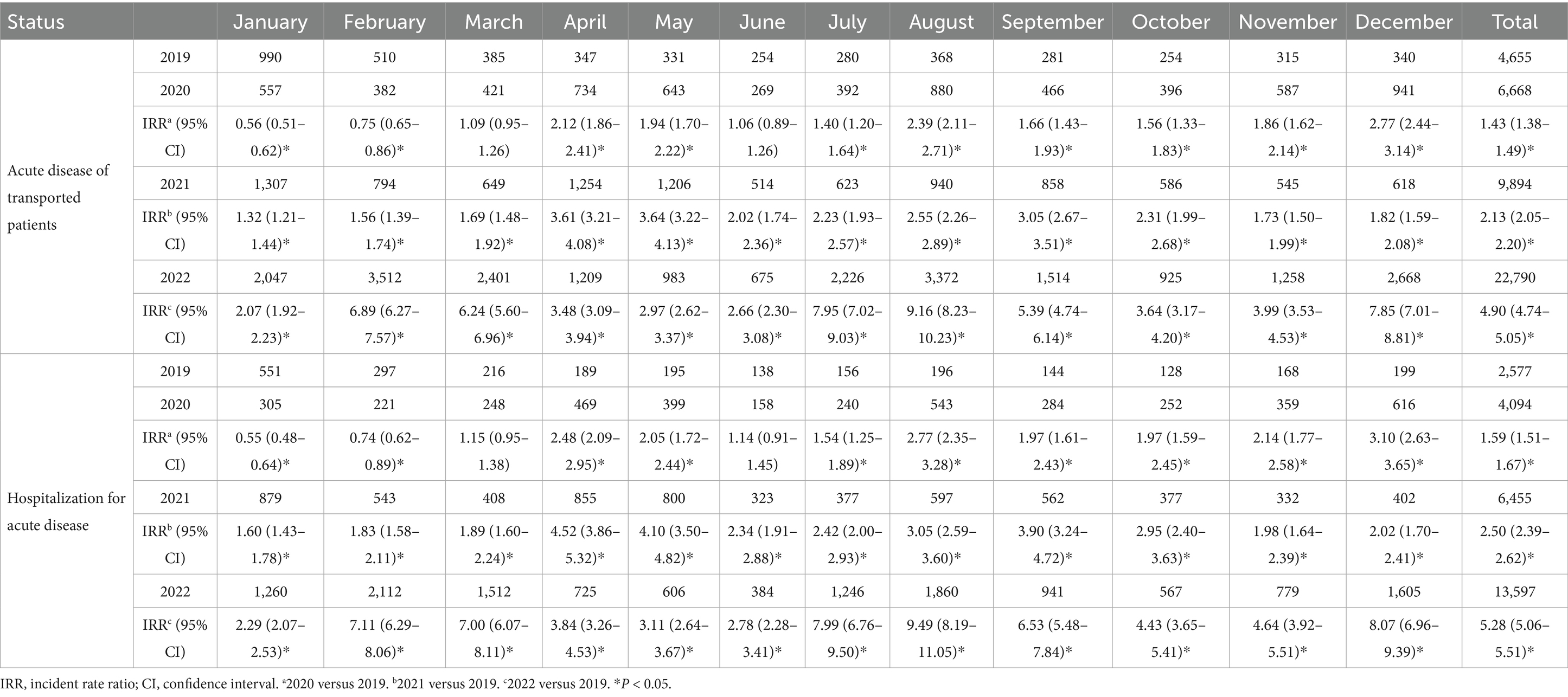
Table 3. Difficulties obtaining patient acceptance for patients transported to emergency departments for acute diseases and subsequently hospitalized in Osaka in 2019–2022.
Table 4 shows the patient outcomes 21 days after hospitalization. The number of discharges decreased significantly in 2020 (IRR: 0.93, 95% CI: 0.92–0.94) and 2021 (IRR: 0.91, 95% CI: 0.90–0.92), compared to 2019; however, it remained comparable in 2022 (IRR: 1.01, 95% CI: 1.00–1.02). The number of continued hospitalizations increased significantly in 2022 compared with 2019 (IRR: 1.11, 95% CI: 1.09–1.12). The number of deaths increased significantly in 2021 (IRR: 1.14, 95% CI: 1.10–1.17) and 2022 (IRR: 1.29, 95% CI: 1.25–1.32). This tendency was seen in almost all months of 2022 compared to the corresponding months in 2019, with particularly higher increases in February, which corresponds to the sixth surge, August, representing the seventh surge, and December, during the eighth surge.
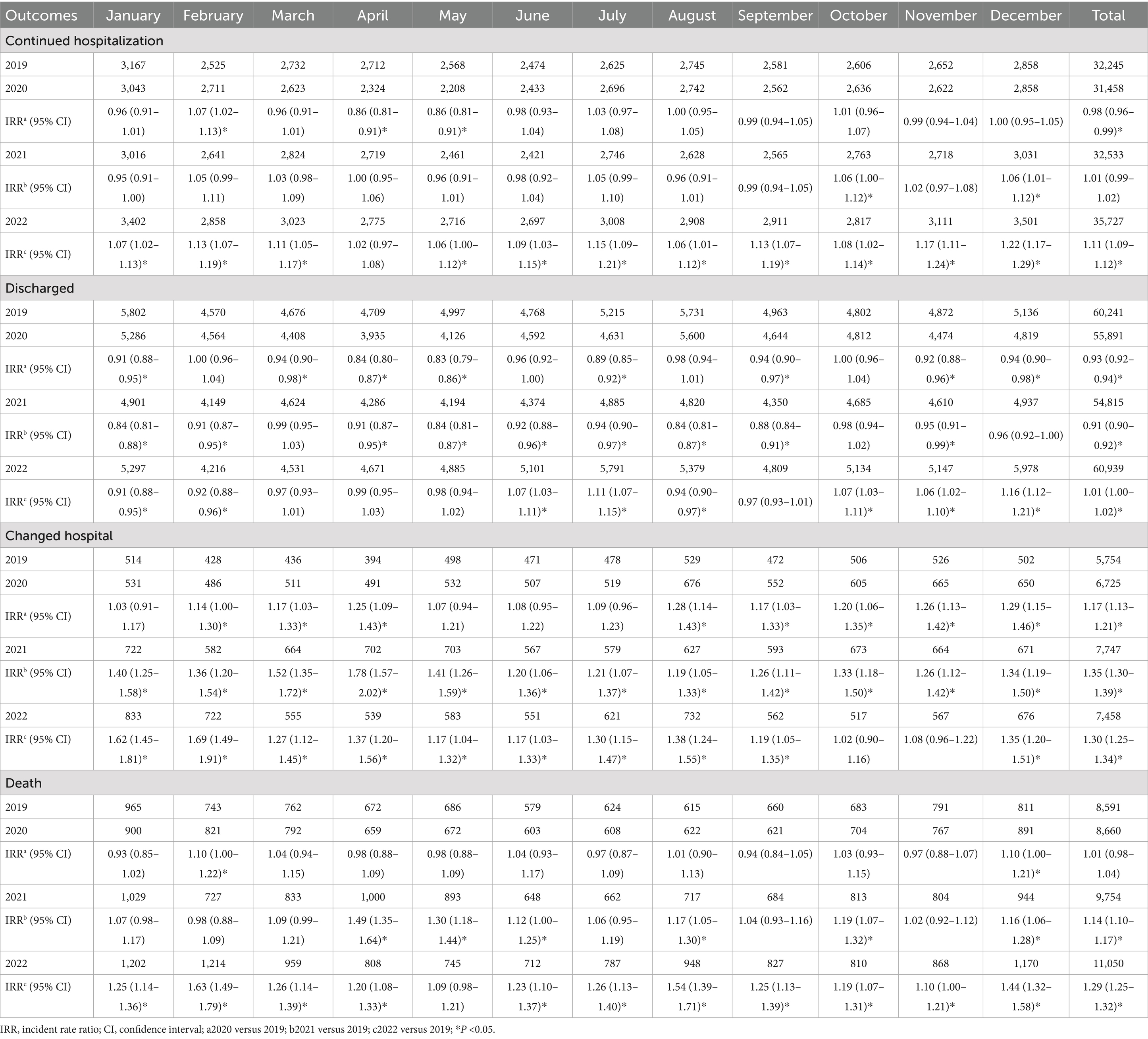
Table 4. Outcomes of patients transported to emergency departments in Osaka for acute diseases, at 21 days following hospitalization, in 2019–2022.
The numbers of hospitalizations for COVID-19 (U) were 1,051 in 2020, 3,933 in 2021, and 12,791 in 2022. Significant increases were observed in 2021 and 2022, compared to 2020 (Table 5). The diagnostic classifications of the older emergency patients who were transported to hospitals for acute diseases and died thereafter are shown in Table 6. The numbers of deaths attributed to COVID-19 (U) were 102 in 2020, 568 in 2021, and 920 in 2022. Significant increases were observed in 2021 and 2022, compared to 2020. In terms of deaths caused by other diseases, the numbers of several diseases increased significantly in 2022 compared with 2019, including diseases of the circulatory system, diseases of the respiratory system, and diseases of the digestive system.
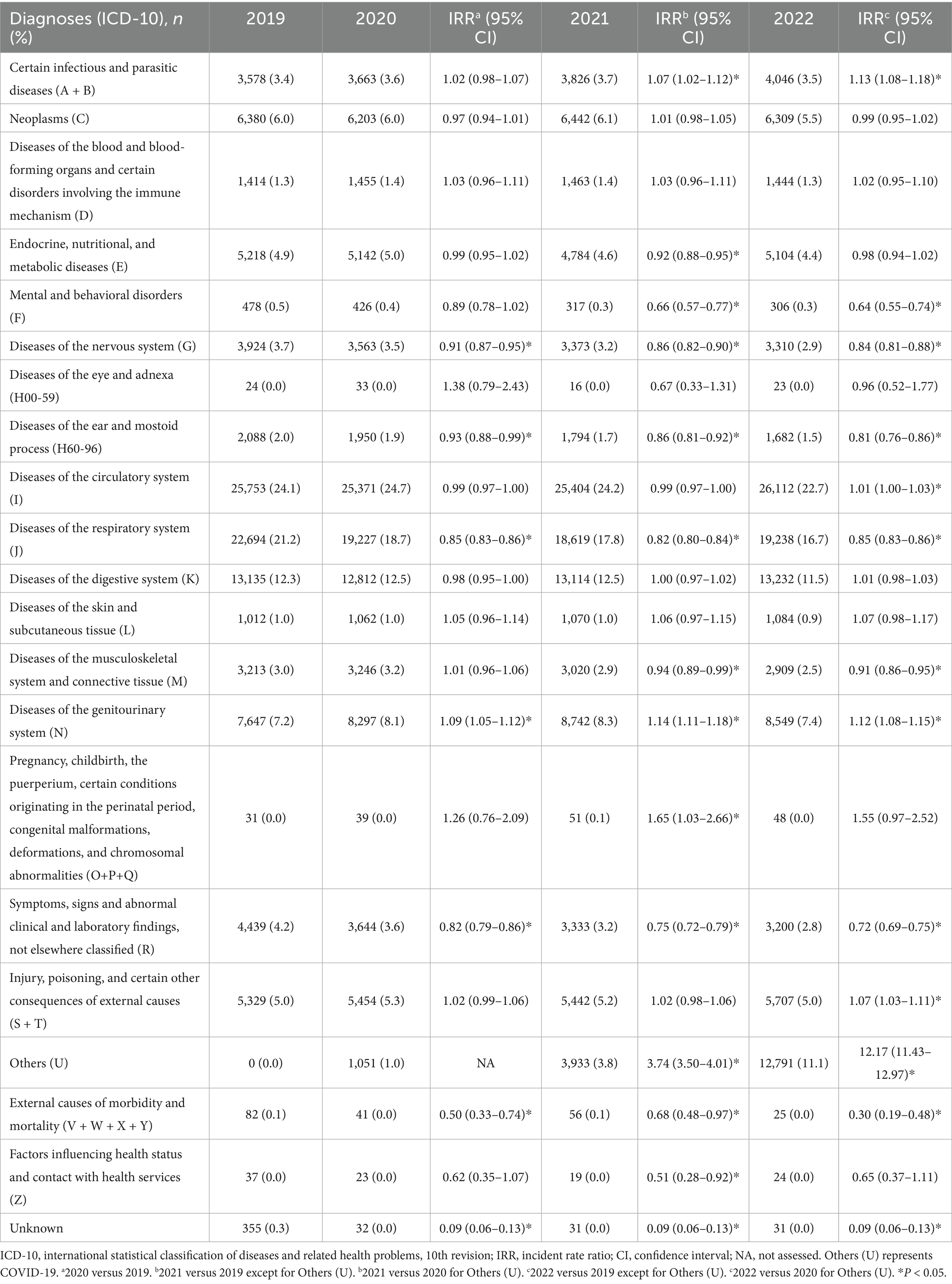
Table 5. Diagnoses of hospitalized patients transported to emergency departments in Osaka for acute diseases in 2019–2022.
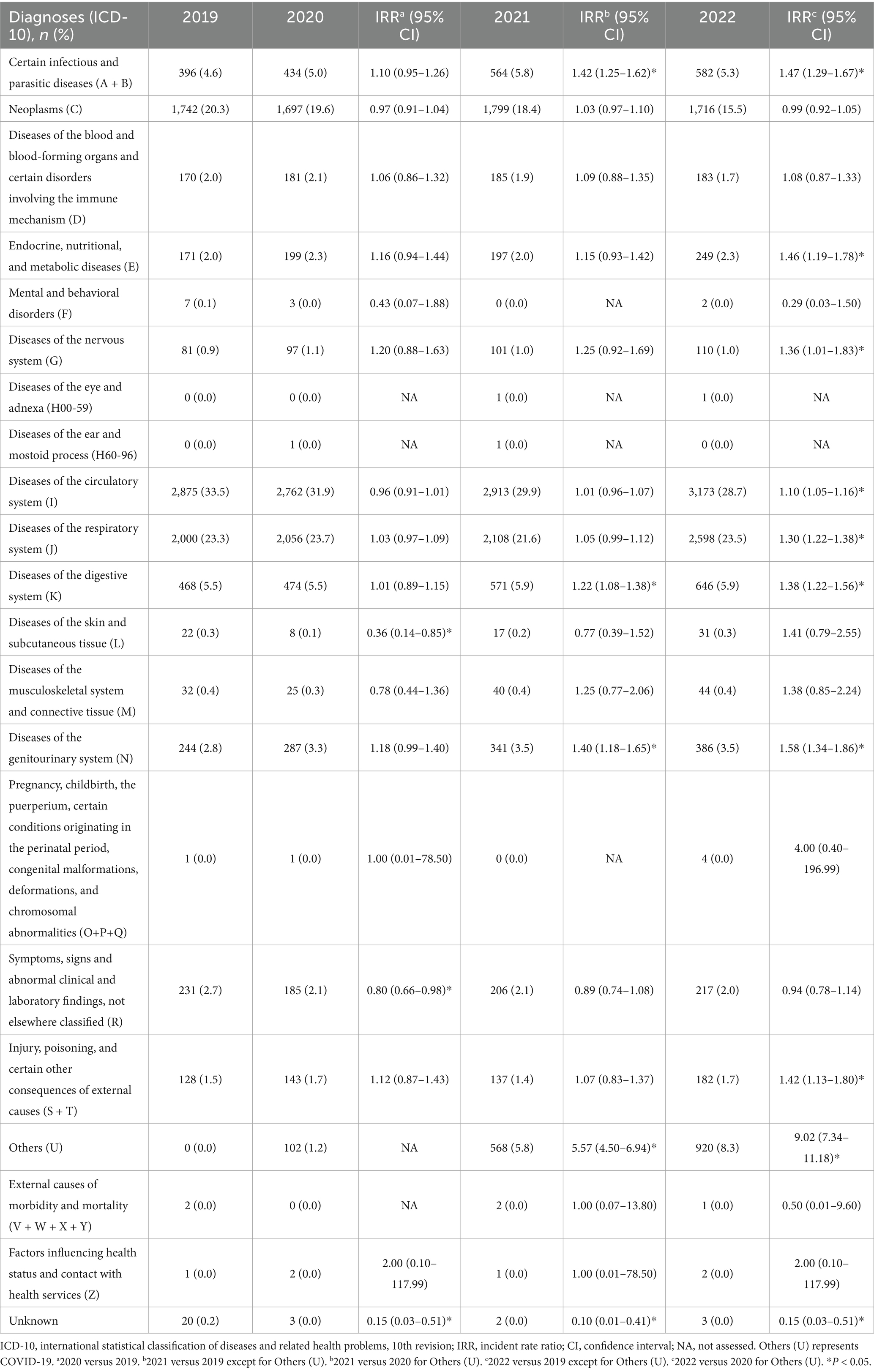
Table 6. Diagnoses of patients transported to emergency departments in Osaka for acute diseases and died following hospitalization in 2019–2022.
4 Discussion
Using the population-based ORION registry, this descriptive study revealed the reality regarding older patients transported by ambulance to emergency departments in Osaka Prefecture, Japan in 2019–2022. The number of emergency patients, number of emergency patients transported for acute diseases, and the number of emergency patients transported for acute diseases who were later hospitalized all decreased in 2020 and 2021 compared with 2019, but were higher in 2022. This population-based descriptive study regarding the influence of the COVID-19 pandemic on EMS in older patients is expected to prove useful for healthcare systems and policy planning.
The number of emergency transports increased in 2022 vs. 2019, with the majority being for acute diseases. The number of older emergency patients transported because of acute diseases decreased in 2020 and 2021, but increased in 2022. A similar trend was observed during the Severe Acute Respiratory Syndrome outbreak in 2003 (20). This change might have been related to a return to normal social life, including the removal of behavioral restrictions, fewer people wearing masks, and an increase in the number of patients with COVID-19.
However, the number of difficulties obtaining acceptance from hospitals for emergency patients transported for acute disease gradually increased after the COVID-19 pandemic. The number of older emergency patients who were transported for acute diseases and later died in hospital also increased in 2021 and 2022 vs. 2019. In particular, the number of deaths from cardiovascular, respiratory, and gastrointestinal diseases increased in 2022. Even before the COVID-19 pandemic, emergency department crowding was reported to be related to increased deaths (21). A previous Japanese study showed that this increase in older emergency patients had a direct significant negative effect on emergency department overcrowding (22). Several studies have reported that patient outcomes were affected by the COVID-19 pandemic (7, 23–25). The pandemic reportedly increased the number of cases that were difficult to transport, the time required for initial responses from EMSs, and caused some patients to refrain from seeking medical care over fear of COVID-19 infection (7, 26–28). Older patients are more vulnerable to health problems; therefore, these factors may have increased the number of people who became seriously ill and worsened their prognoses. The time intervals from ambulance call to arrival on scene increased over year in this study. However, the definitive reasons for the increase in the number of deaths following emergency hospitalization after the COVID-19 pandemic are unclear, because data regarding emergency procedures, particularly for cardiovascular, respiratory, and gastrointestinal diseases after hospital arrival, were unavailable for this study. It is essential to continue monitoring changes in the number of emergency patients transported to hospitals, as well as their number of deaths. Regular assessments of the impact of the COVID-19 pandemic on the EMS system can be used to formulate EMS system plans for future pandemics and disasters. Based on the lessons learned from this experience, it would be useful to prepare for future pandemics by, for example, expanding consultation services that can be used before calling for EMS, educating residents on the proper use of ambulances, and establishing a task force within the government to respond to such situations.
In our study, the number of hospitalizations and deaths caused by COVID-19 among older emergency patients significantly increased over the study period. In 2022, when the Omicron variant of the SARS-CoV-2 virus became dominant, the mortality rate of COVID-19 declined among all patients, including older ones (29). On the other hand, the number of confirmed COVID-19 cases increased significantly in Osaka Prefecture, from 30,000 in 2020 to 170,000 in 2021, then 2,340,000 in 2022 (30). The increase in the number of hospitalizations and deaths caused by COVID-19 in this study was likely attributable to the greater impact of the increase in the number of COVID-19 cases. Older patients with COVID-19 accounted for 10% of all hospitalized patients in 2022, placing a significant overall burden on EMS. Further studies are warranted to determine the long-term transition characteristics of older patients with COVID-19 who are transported to emergency hospitals.
This study was subject to several key limitations worth noting. First, the ORION registry records patient data concerning patients who are transported to emergency hospitals and emergency critical care centers in Osaka Prefecture but does not register data regarding emergency patients who are transported to non-emergency medical institutions in the prefecture or to medical institutions outside of the prefecture. Second, we had no information on disease severity or the treatments received by our cohort of emergency patients within the hospitals they were admitted to. Finally, patient-related factors such as medical history, and social factors such as the person who called for EMS, hospital capacity, and regional differences in EMS operations, may influence patient prognoses; however, these factors were not included in this study (31–33).
5 Conclusion
The number of older patients transported to emergency departments in Osaka Prefecture for acute diseases decreased in 2020 and 2021, but increased in 2022. The number of difficulties obtaining patient acceptance from hospitals for these patients increased as COVID-19 spread through the region. By 2022, the number of deaths from acute diseases, including cardiovascular, respiratory, and gastrointestinal diseases, also increased. Continuous monitoring will be necessary to assess future changes.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the data supporting the findings of this study are available from the Osaka Prefectural government; however, the availability of these data is restricted. The data cannot be shared publicly because of the Protection Ordinance for Personal Information law in Osaka Prefecture. They may be accessible to qualified researchers who apply for access and are approved by the technical committee. Requests to access these datasets should be directed to https://www.pref.osaka.lg.jp/o100030/iryo/qq/orion_teikyo.html.
Ethics statement
This study was approved by the Ethics Committee of Osaka University Graduate School of Medicine (approval no.: 15003). The ORION data are administrative records that are anonymized without specific personal information. Therefore, the requirement to obtain informed patient consent was waived for this study.
Author contributions
KT: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. YK: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Visualization, Writing – review & editing. TK: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Software, Validation, Writing – original draft, Writing – review & editing. HD: Conceptualization, Methodology, Resources, Writing – review & editing. JO: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing – review & editing. TM: Conceptualization, Data curation, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Fire and Disaster Prevention Technologies Program (grant no.: 21584490).
Acknowledgments
We are deeply indebted to all of the Emergency Medical Service personnel and concerned physicians in Osaka Prefecture, and to the Osaka Medical Association for their indispensable cooperation and support. This study was supported by the Osaka University Center of Medical Data Science and Advanced Clinical Epidemiology Investigator’s Research Project, which provided insights and expertise.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wiersinga, WJ, Rhodes, A, Cheng, AC, Peacock, SJ, and Prescott, HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. (2020) 324:782–93. doi: 10.1001/jama.2020.12839
2. Cucinotta, D, and Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
3. Bonanad, C, García-Blas, S, Tarazona-Santabalbina, F, Sanchis, J, Bertomeu-González, V, Fácila, L, et al. The effect of age on mortality in patients with COVID-19: a Meta-analysis with 611,583 subjects. J Am Med Dir Assoc. (2020) 21:915–8. doi: 10.1016/j.jamda.2020.05.045
4. Romero Starke, K, Petereit-Haack, G, Schubert, M, Kämpf, D, Schliebner, A, Hegewald, J, et al. The age-related risk of severe outcomes due to COVID-19 infection: a rapid review, Meta-analysis, and Meta-regression. Int J Environ Res Public Health. (2020) 17:5974. doi: 10.3390/ijerph17165974
5. Tanaka, K, Zha, L, Kitamura, T, Katayama, Y, Takeuchi, T, Komukai, S, et al. Characteristics and outcomes of older patients with coronavirus disease 2019 in Japan. Geriatr Gerontol Int. (2021) 21:629–35. doi: 10.1111/ggi.14207
6. Kim, L, Garg, S, O'Halloran, A, Whitaker, M, Pham, H, Anderson, EJ, et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the US coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET). Clin Infect Dis. (2021) 72:e206–14. doi: 10.1093/cid/ciaa1012
7. Katayama, Y, Tanaka, K, Kitamura, T, Dohmi, H, Masui, J, Hirose, T, et al. Incidence and outcome of patients with difficulty in hospital acceptance during COVID-19 pandemic in Osaka prefecture, Japan: a population-based descriptive study. Acute Med Surg. (2023) 10:e880. doi: 10.1002/ams2.880
8. Kovach, CP, and Perman, SM. Impact of the COVID-19 pandemic on cardiac arrest systems of care. Curr Opin Crit Care. (2021) 27:239–45. doi: 10.1097/MCC.0000000000000817
9. Lim, SL, Shahidah, N, Saffari, SE, Ng, QX, Ho, AFW, Leong, BS, et al. Impact of COVID-19 on out-of-hospital cardiac arrest in Singapore. Int J Environ Res Public Health. (2021) 18:3646. doi: 10.3390/ijerph18073646
10. Kim, C, Lee, J, Cho, Y, Oh, J, Kang, H, Lim, TH, et al. The impact of the COVID-19 pandemic on in-hospital mortality in patients admitted through the emergency department. Clin Exp Emerg Med. (2023) 10:92–8. doi: 10.15441/ceem.22.359
11. Katayama, Y, Tanaka, K, Domi, H, Masui, J, Nakao, S, Tachino, J, et al. Outcome of emergency patients transported by ambulance during the COVID-19 pandemic in Osaka prefecture, Japan: a population-based descriptive study. Front Public Health. (2024) 11:1322236. doi: 10.3389/fpubh.2023.1322236
12. Population of Osaka prefecture in 2020. Osaka: Osaka Prefectural government. Available online at: https://www.pref.osaka.lg.jp/attach/42622/00426107/R2kokutyo_osakahu_kakuhou_toukeihyo.pdf (Accessed May 21, 2024).
13. Katayama, Y, Tanaka, K, Kitamura, T, Takeuchi, T, Nakao, S, Nitta, M, et al. Incidence and mortality of emergency patients transported by emergency medical service personnel during the novel Corona virus pandemic in Osaka prefecture, Japan: a population-based study. J Clin Med. (2021) 10:5662. doi: 10.3390/jcm10235662
14. Okamoto, J, Katayama, Y, Kitamura, T, Sado, J, Nakamura, R, Kimura, N, et al. Profile of the ORION (Osaka emergency information research intelligent operation network system) between 2015 and 2016 in Osaka, Japan: a population-based registry of emergency patients with both ambulance and in-hospital records. Acute Med Surg. (2018) 6:12–24. doi: 10.1002/ams2.371
15. Katayama, Y, Kitamura, T, Kiyohara, K, Iwami, T, Kawamura, T, Izawa, J, et al. Improvements in patient acceptance by hospitals following the introduction of a smartphone app for the emergency medical service system: a population-based before-and-after observational study in Osaka City, Japan. JMIR Mhealth Uhealth. (2017) 5:e134. doi: 10.2196/mhealth.8296
16. Orimo, H, Ito, H, Suzuki, T, Araki, A, Hosoi, T, and Sawabe, M. Reviewing the definition of “elderly”. Geriatr Gerontol Int. (2006) 6:149–58. doi: 10.1111/j.1447-0594.2006.00341.x
17. Fire and Disaster Management Agency. Survey on the difficulty in hospital acceptance during the novel corona virus pandemic. Tokyo: The publisher name is Fire and Disaster Management Agency. Available online at: https://www.fdma.go.jp/disaster/coronavirus/items/coronavirus_kekka.pdf (Accessed May 21, 2024).
18. Centers for Disease Control and Prevention. (2025). New ICD-10-CM code for the 2019 novel coronavirus (COVID-19). Atlanta: Centers for Disease Control and Prevention.Available online at: https://www.cdc.gov/nchs/data/icd/Announcement-New-ICD-code-for-coronavirus-3-18-2020.pdf (Accessed May 21, 2024).
19. Results related to COVID-19 in Osaka up to the 8th surge. Osaka: Osaka Prefectural government. Available online at: https://www.pref.osaka.lg.jp/attach/23711/00456341/16sankou16.pdf (Accessed May 21, 2024).
20. Heiber, M, and Lou, WY. Effect of the SARS outbreak on visits to a community hospital emergency department. CJEM. (2006) 8:323–8. doi: 10.1017/s148180350001397x
21. Morley, C, Unwin, M, Peterson, GM, Stankovich, J, and Kinsman, L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One. (2018) 13:e0203316. doi: 10.1371/journal.pone.0203316
22. Kawano, T, Nishiyama, K, Anan, H, and Tujimura, Y. Direct relationship between aging and overcrowding in the ED, and a calculation formula for demand projection: a cross-sectional study. Emerg Med J. (2014) 31:19–23. doi: 10.1136/emermed-2012-202050
23. Chung, H, Namgung, M, Lee, DH, Choi, YH, and Bae, SJ. Effect of delayed transport on clinical outcomes among patients with cardiac arrest during the coronavirus disease 2019 pandemic. Australas Emerg Care. (2022) 25:241–6. doi: 10.1016/j.auec.2021.11.006
24. Surek, A, Ferahman, S, Gemici, E, Dural, AC, Donmez, T, and Karabulut, M. Effects of COVID-19 pandemic on general surgical emergencies: are some emergencies really urgent? Level 1 trauma center experience. Eur J Trauma Emerg Surg. (2021) 47:647–52. doi: 10.1007/s00068-020-01534-7
25. Nakao, S, Masui, J, Katayama, Y, Kitamura, T, and Matsuoka, T. Impact of coronavirus disease 2019 on the mortality of patients who received emergency transportation: a population-based cross-sectional study. Acute Med Surg. (2023) 10:e813. doi: 10.1002/ams2.813
26. Laukkanen, L, Lahtinen, S, Liisanantti, J, Kaakinen, T, Ehrola, A, and Raatiniemi, L. Early impact of the COVID-19 pandemic and social restrictions on ambulance missions. Eur J Pub Health. (2021) 31:1090–5. doi: 10.1093/eurpub/ckab065
27. Chen, Y, Zhong, B, Jiang, Q, Chen, Y, He, W, Lai, N, et al. The impact of the COVID-19 pandemic on the care of pulmonary hypertension patients outside the Hubei province in China. Pulm Circ. (2022) 12:e12130. doi: 10.1002/pul2.12130
28. Di Bidino, R, and Cicchetti, A. Impact of SARS-CoV-2 on provided healthcare. Evidence from the emergency phase in Italy. Front Public Health. (2020) 8:583583. doi: 10.3389/fpubh.2020.583583
29. Adjei, S, Hong, K, Molinari, NM, Bull-Otterson, L, Ajani, UA, Gundlapalli, AV, et al. Mortality risk among patients hospitalized primarily for COVID-19 during the omicron and Delta variant pandemic periods-United States, April 2020-June 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:1182–9. doi: 10.15585/mmwr.mm7137a4
30. Ministry of Health, Labour, and Welfare. (2024). Open data source about COVID-19. Tokyo: Ministry of Health, Labour and Welfare. Available online at: https://www.mhlw.go.jp/stf/covid-19/open-data.html (Accessed May 21, 2024).
31. Palomeras, E, Fossas, P, Quintana, M, Monteis, R, Sebastián, M, Fábregas, C, et al. Emergency perception and other variables associated with extra-hospital delay in stroke patients in the Maresme region (Spain). Eur J Neurol. (2008) 15:329–35. doi: 10.1111/j.1468-1331.2008.02082.x
32. Katsomboon, K, Sindhu, S, Utriyaprasit, K, and Viwatwongkasem, C. Factors associated with 24-hour clinical outcome of emergency patients; a cohort study. Arch Acad Emerg Med. (2022) 10:e30. doi: 10.22037/aaem.v10i1.1590
Keywords: COVID-19 pandemic, death, emergency transportation, incidence, older patients
Citation: Tanaka K, Katayama Y, Kitamura T, Domi H, Oda J and Matsuoka T (2025) Impact of the COVID-19 pandemic on the emergency transportation of older patients: a population-based descriptive study in Osaka prefecture, Japan. Front. Public Health. 13:1515635. doi: 10.3389/fpubh.2025.1515635
Edited by:
Kamyar Asadipooya, University of Kentucky, United StatesReviewed by:
Amit Tak, RVRS Medical College, IndiaFariba Afrin Irany, University of North Texas, United States
Copyright © 2025 Tanaka, Katayama, Kitamura, Domi, Oda and Matsuoka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yusuke Katayama, b3Jpb24xM0BocC1lbWVyZy5tZWQub3Nha2EtdS5hYy5qcA==
 Kenta Tanaka1,2
Kenta Tanaka1,2 Yusuke Katayama
Yusuke Katayama Tetsuhisa Kitamura
Tetsuhisa Kitamura Tetsuya Matsuoka
Tetsuya Matsuoka