- 1Yunnan Provincial Key Laboratory of Public Health and Biosafety, Kunming Medical University, Kunming, China
- 2School of Public Health, Kunming Medical University, Kunming, China
- 3Department of Infectious Diseases and Hepatology, The First Affiliated Hospital of Kunming Medical University, Kunming, China
Background: Injection of drug abuse could result in infectious disease, and adverse childhood experiences (ACEs) possibly are associated with infectious disease. However, there is a paucity of literature on a direct or indirect relationship between ACEs, injection of drug use and infectious disease. We thus identified the pathway of influence of ACEs in adulthoods and injection of drug use on infectious disease by structural equation models (SEM).
Methods: A cross-sectional study was conducted by respondent driving sampling and consecutive sampling among people who use drugs in southwest of China in 2021. R software 4.2.1 was used to conduct descriptive, univariate, and SEM analysis.
Results: There were 404 participants in total, with an average age of 34 and most males (98.3%) and minorities (79.6%). 95.5% of respondents experienced ACEs with 46.6% of reporting 4 or more ACEs. Correlations in SEM showed that infectious disease might be directly positively affected by injection of drug use (β = 0.184), and directly negatively affected by ACEs (β = −0.188). Age (β = 0.029), Ethnic (β = −0.021), Education (β = 0.019), Gender (β = 0.022), Sex partners (β = −0.017), and ACEs (β = −0.029) might have indirect effects on infectious disease.
Conclusion: ACEs might be a direct or indirect predictor for infectious disease in adulthood, injection of drug use might be a risk factor and moderate other factors of infection of infectious disease. Strategies for creating a positive home environment, minimizing traumatic or stressful childhood experiences, and increasing awareness of the risks associated with drug injection use are all ways to lower the chances of contracting infectious diseases.
1 Introduction
Prevalence of Acquired Immune Deficiency Syndrome (AIDS), Hepatitis B virus (HBV), and Hepatitis C virus (HCV) among drug users were higher especially in the border areas. Approximately 284 million people have used drugs, 14.8 million people who injected drugs (PWID) with 15.2% of HIV infection, 38.8% of HCV and 8.4% of HBV (1). Among PWID, the HIV prevalence was 28 times higher than in the rest of the global adult population with an estimated 68 and 83% condomless sex in the US and Nampula/Nakala, respectively, (2–4). Furthermore, 7.7% of HIV and HCV-positive rates among drug users in China’s border areas thus exceeding the national level of 4.8% (5).
Additionally, poly-drug usage and injection drug use (IDU) were significantly risk factors associated with blood-borne virus diseases that accounted for 43% of future HCV infection up to 79% in high-income countries globally (1, 6–8). Individuals who inject multiple substances exhibited higher levels of risk behaviors and prevalence of sexually transmitted infections (STIs) compared to single users (7, 9), with an increased risk of HIV and Syphilis infection and transmission among men who have sex with men (MSM) (10). Co-infection with syphilis spirochetes was associated with increased HIV viral load and decreased CD4 T-cell counts (11), which HIV infection could impact the normal progression of HBV and HCV (12, 13). Therefore, there existed complex associations between poly-drug uses, IDU and blood-borne viruses’ diseases. More importantly, poly-drug use and IDU may increase the likelihood of engaging in unsafe sexual behaviors like having multiple sexual partners and condomless sex that are major contributors to increased risk of contracting HIV, HCV and syphilis (6, 14, 15). Evidence showed that consistent condom use reduced the risk of contracting the virus by 10–20 times when exposed, compared to inconsistent, non-use or those who had multiple sexual partners (16–18), with an estimated 0.3% risk of HIV transmission and ratios ranging from 2.08 to 2.94 association between stimulant use and unprotected sex and multiple sexual partners (6, 19).
Moreover, adverse Childhood Experiences (ACEs) are associated with risky behaviors related to substance abuse in adulthood with increased risk of HIV and other STIs (20–22). On average, adults were more likely to contract STIs and report association between ACEs and polydrug pattern and alcohol abuse (23, 24), with ACEs being an independent risk of HIV (21, 25). It is essential to explore the pathways through which ACEs affect infectious diseases in adults while controlling for other influencing factors as evidence remains insufficient regarding the associations of ACEs with infectious diseases.
Cross-border activities independently contribute to the increased prevalence of HIV, HBV, HCV, and syphilis. Literature review suggested that cross-border sexual activities were independent predictors of STIs (17), with four times higher HIV prevalence among mobile population than that of the general population in Cambodia, Myanmar, southern China, Vietnam to Thailand with 19.0% HIV-1among Burmese injecting drug users (Yunnan-mIDUs) living in Yunnan (26–28). Migration and mobility were often connected to vulnerability factors like substance use, social exclusion, stigma, and limited access to healthcare or social security services which could increase the chances of HIV transmission (29). However, the relationship among them is not clear. Further exploration of the pathways through which these risk factors act is warranted.
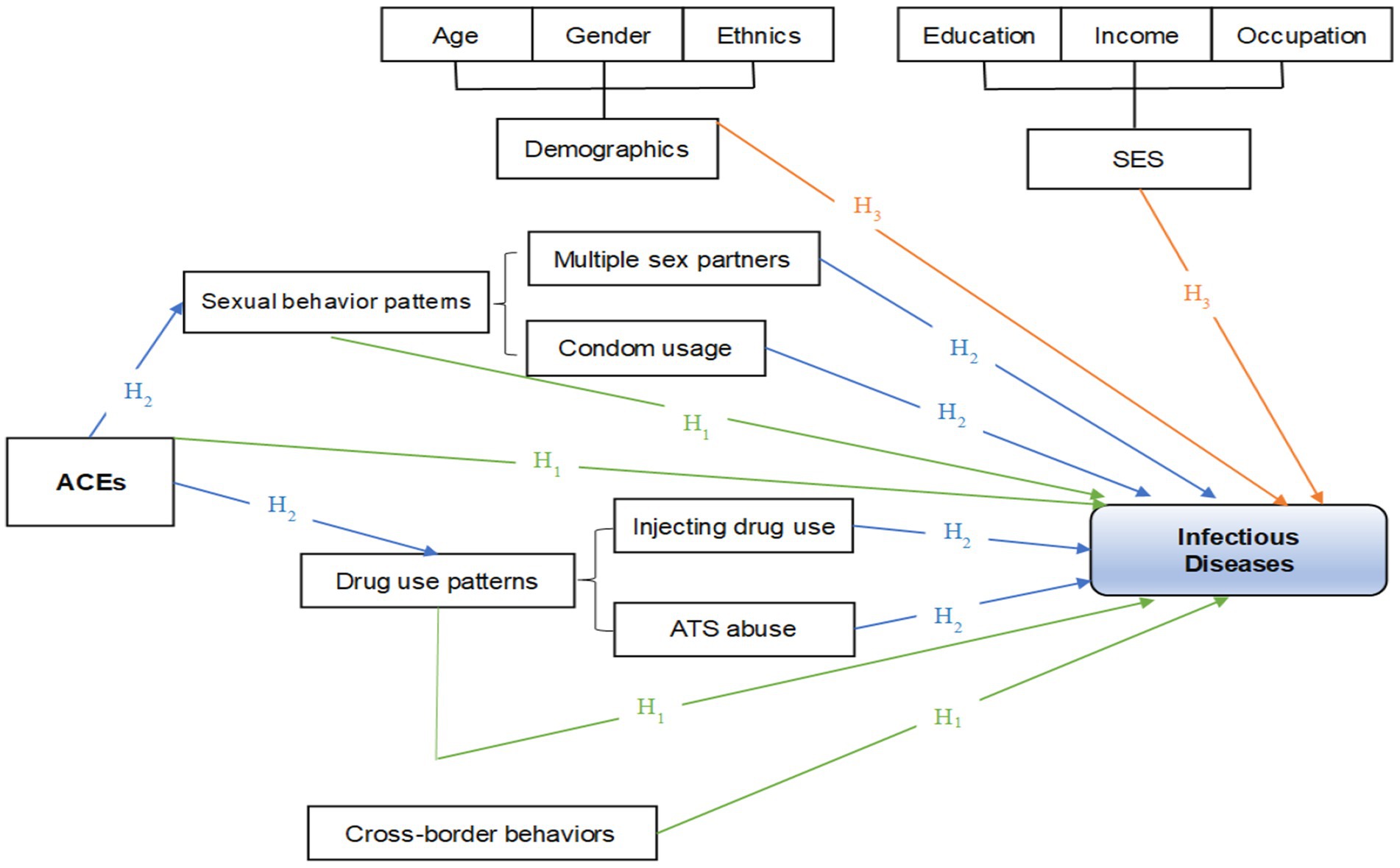
While the associations between drug use and infectious diseases are well-established, the potential role of ACEs as both direct and indirect predictors of infection remains insufficiently examined, particularly in under-resourced border regions. We proposed that IDU and ACEs may act as mediating variables in infectious diseases. Structural Equation Modeling (SEM), a more advanced form of regression analysis and strategy (30), was used to simultaneously estimate the direct and indirect pathways from ACEs and IDU to sexually transmitted infectious diseases in adulthood, and to account for latent and observed variable interrelationships. If these intermediary variables can be confirmed, and the causes of the infectious disease pattern are well-documented, future interventions should prioritize addressing early experiences. We hypothesize the following: (1) IDU and ATS use can directly predict infectious diseases in adulthood; (2) having multiple sexual partners and inconsistent condom use can directly predict infectious diseases in adulthood; (3) exposure to ACEs in childhood can directly or indirectly predict infectious diseases in adulthood; (4) cross-border activities can predict infectious diseases (Figure 1).
Our targets aimed to expand upon previous studies and complement them with factors that may contribute to a better understanding of the association between ACEs and drug use. Concretely, we explored the pathways by which ACEs affect infectious diseases in adulthood and the possible moderating effects of injection of drug use in samples from the southwest of China.
2 Methods
2.1 Study setting
A cross-sectional study was conducted by respondent driving sampling and consecutive sampling among adults who used drugs in Jinghong city, Xishuangbanna Autonomous Prefecture, Yunnan Province from January to July 2021. The inclusion criteria were that participants older than 18 and have used injectable drugs or stimulants during the previous 6 months. Individuals who were unable to participate for medical or psychiatric reasons were omitted. Self-administered questionnaires were primarily used to gather data from eligible participants. For further information on the study setup, participants, sampling, data collection, and processing, refer to our previous publication (31).
2.2 Measurements
The questionnaires were used to measure demographics, socio-economic status (SES), cross-border behaviors, ACEs, patterns of sexual behavior, use of illegal addictive drugs and usage patterns. Additionally, the presence of infectious diseases was also collected.
Sex was defined according to external anatomy. Cross-border activity was defined as having experience with going abroad. Sexual behavior patterns included condom use and having multiple sexual partners. Condom usage referred to whether a condom was used during sexual intercourse (vaginal intercourse, oral sex, anal sex, etc.) and multiple sexual partners were identified by the number of sexual partners at the same time, including modes of sexual intercourse with boy/girlfriends, spouses, sex workers, and others. IDU was assessed by asking participants if they had a history of injecting drug use in adulthoods. Infectious disease status was determined based on clinical records indicating physician-diagnosed cases of HIV/AIDS, hepatitis B, hepatitis C, and syphilis. To assess ACEs, a standardized methodology was utilized, incorporating items from the Childhood Trauma Questionnaire (CTQ-SF) (32) and a portion of the items from the USA’s National Survey on Alcohol and Related Conditions-III (33). Nine questions were selected that related to experiences of adverse family events, including neglected daily care, verbal abuse, incidents of sexual abuse, failure to provide medical care, emotional neglect, disapproval, physical violence, an uncaring family climate, and family disruption due to substance use. The questions were adapted to the Chinese context, reviewed and finalized by experts, and pilot tested. Participants were asked to respond to each question on the ACEs questionnaire with either “Yes” or “No.”
2.3 Variables
The dependent variable was any HIV/HBV/HCV/Syphilis infection. Demographic variables included age, sex (male = 0, female = 1), ethnicity (Han = 0, minority = 1), and marital status (unmarried = 0, married = 1). SES included occupation (unemployed = 0, employed = 1), education (≤primary school = 0, ≥junior high school = 1), and monthly income. Among them, age and average income were continuous variables. Other factors included cross-border behaviors (non-cross-border = 0, cross-border = 1), condom usage (No = 0, Yes = 1), number of sex partners was continuous variables. Furthermore, ACEs scores varying from 0 to 9 were utilized to assess the overall impact of various ACEs, with higher scores implying more severe exposure to ACEs. It can be fragmented down into four levels: none (zero), mild (1, 2), moderate (3), and severe (equal to or greater than 4).
2.4 Data management and statistical analysis
Epi data 3.1 was utilized for data management, and R software 4.2.1 was used for data analysis. For comparison of risk levels in univariate analysis, chi-square and rank sum tests were applied. SEM was employed to investigate direct and indirect effects and associations between variables. A p-value below 0.05 was considered statistically significant.
3 Results
3.1 Distribution of socio-economic-demographics
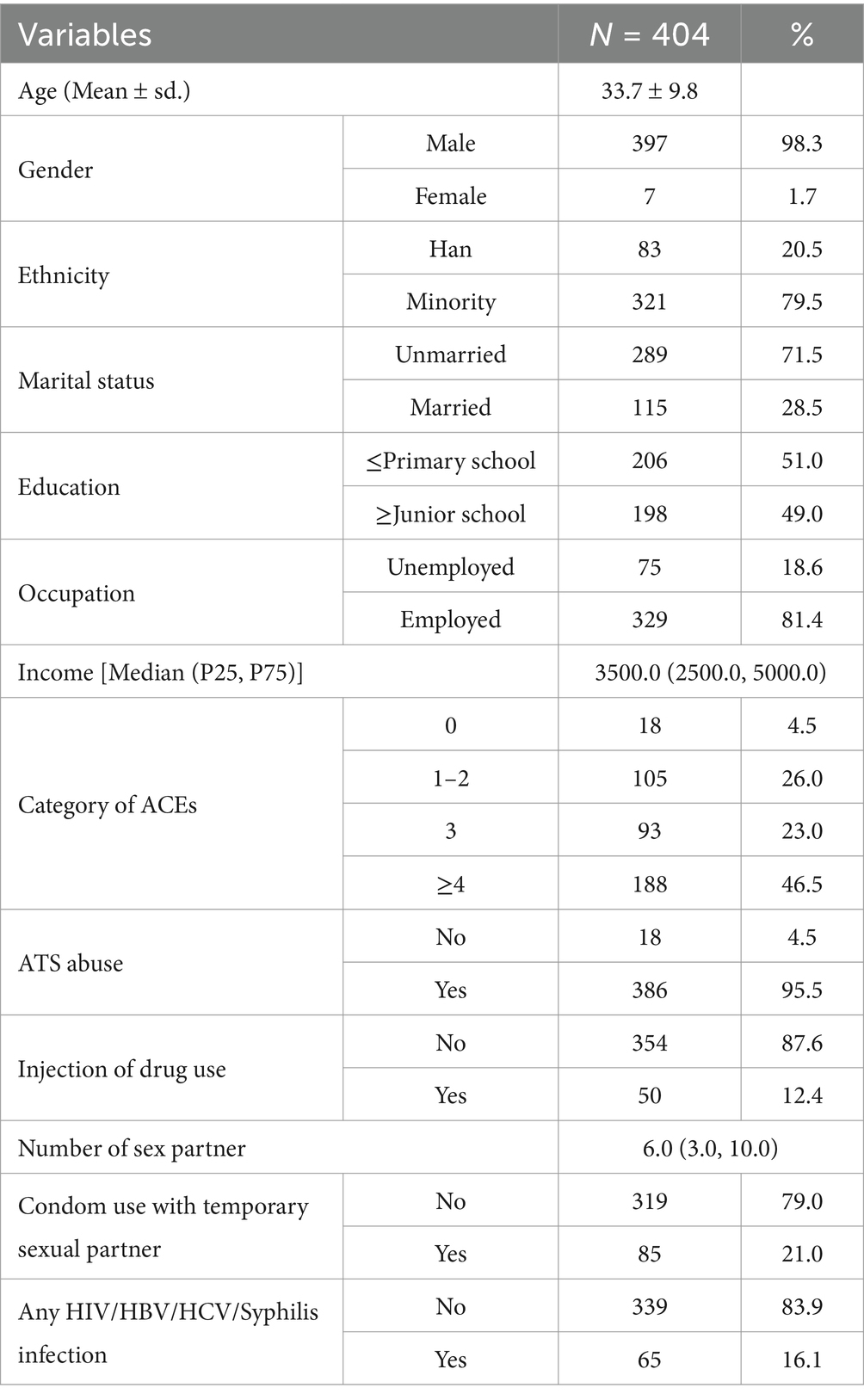
404 people who used drugs included 397 males and 7 females with mean age of 33.7 years old, 79.5% of ethnic minority, 71.5% of unmarried and employed accounting for 81.4%. 95.5% of respondents experienced ACEs with 46.5% of reporting 4 or more ACEs. 95.5 and 12.4% of respondents were ATS abuser and injection of drug user, respectively. The average values for monthly income and number of sex partner were 3500.0 (2500.0, 5000.0), and 6.0 (3.0, 10.0) respectively. 16.1% of respondents was infected by sexual transmitted diseases (Table 1).
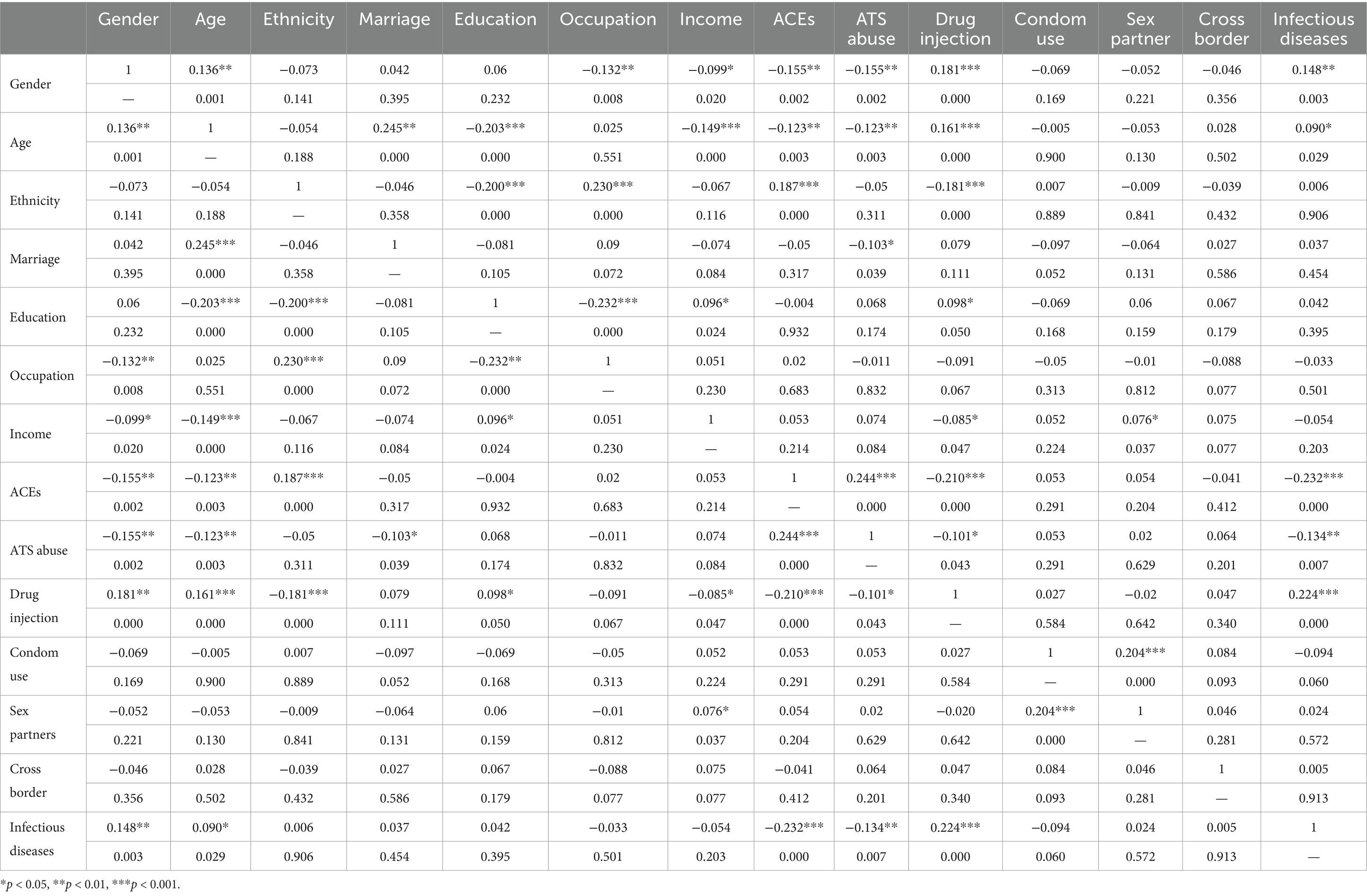
3.2 Correlations between variables in SEM
Drug injection was positively related to gender (p < 0.001), age (p < 0.001), education (p = 0.05) and infectious diseases (p < 0.001) but negatively related to ethnicity (p < 0.001), income (p < 0.05), ACEs (p < 0.001) and ATS abuse (p < 0.05). ATS abuse was negatively related to gender (p < 0.01), age (p < 0.01), marriage (p < 0.05) and infectious disease (p < 0.01) but positively related to ACEs (p < 0.001). Infectious disease was positively related to gender (p < 0.01) and age (p < 0.05) but negatively related to ACEs (p < 0.001) (details refer to Table 2).
3.3 Predictors of infectious disease by SEM
The final structural model fitted the current data well, Chi-square = 41.828 (df = 34, p = 0.167), Root Mean Square Error of Approximation (RMSEA) = 0.024 (90% CI: 0.000, 0.045), Adjusted Goodness of Fit Index (AGFI) = 0.962, and Comparative Fit Index (CFI) = 0.962. Figure 2 showed that Infectious disease was positively affected by drug injection (β = 0.184), and negatively affected by ACEs (β = −0.188). Drug injection was positively associated with education (β = 0.102), age (β = 0.159), gender (β = 0.120) and negatively associated with ACEs (β = −0.146) and ethnic (β = −0.116). ATS abuse was positively affected by ACEs (β = 0.244) and negatively associated with gender (β = −0.166) and ethnic (β = −0.101). The details of other associations between variables studied were showed in Figure 2.
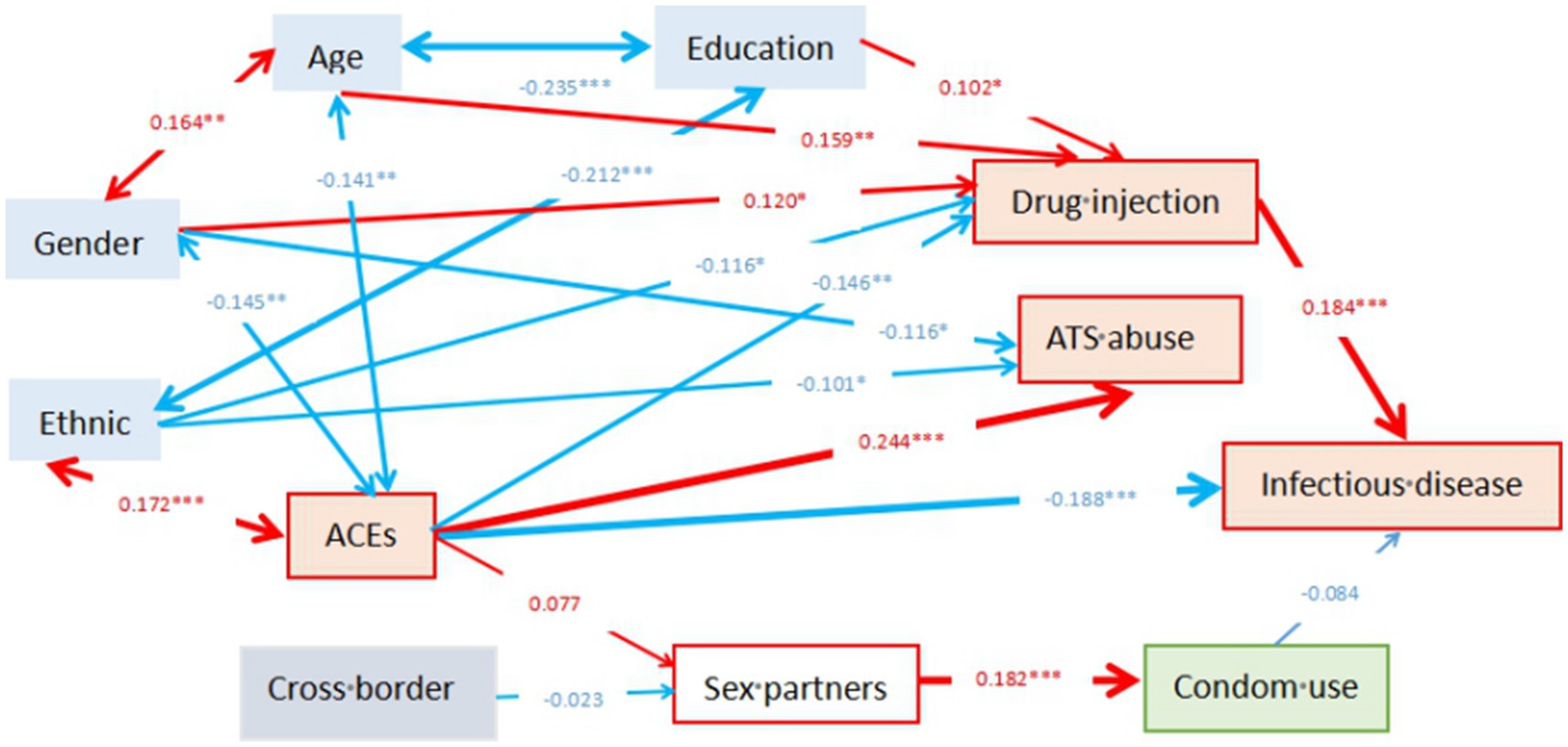
Figure 2. Pathways illustrating the effects of adverse childhood experiences and drug injection on infectious diseases among drug-using adults. Parameters in this figure are standardized value. The significant level for path coefficients was set at *p < 0.05, **p < 0.01, ***p < 0.001.
4 Discussion
Exposure to ACEs in childhood could predict infectious diseases in adulthood through both direct and indirect negative effects on infectious diseases by positively impacting the adult injection of drug use. Meanwhile, drug use injection also had a direct positive effect on infectious diseases while condom use was not associated with infectious diseases. Delving into demographics, it turns out that age, gender, ethnicity and education might subtly influence infectious disease by shifting behaviors related to injecting drug use.
Our findings support the first hypothesis that IDU was directly associated with infectious diseases and a higher risk of HIV and HCV prevalence which was consistent with other studies (1, 34–36). Nevertheless, studies have also showed 30–40% were not exposed to HCV in high-risk settings with IDU (37). There was a high risk of contracting a blood-borne virus through IDU as the use of contaminated needles, syringes, or drug injection equipment was the main cause of HIV and HCV infection (34). The Xishuangbanna region is traditionally an area of high rate of IDU, the transmission of infection through unprotected sexual intercourse may sometimes be ignored in the context of infectious diseases caused by IDU.
ACEs exposure could predict infectious diseases in adulthood, through both indirect and direct negative effects on infectious diseases by positively affecting adult injection of drug use. Previous findings that ACEs were associated with poor health outcomes in adulthood, such as increased risk of HIV and other sexually transmitted diseases (22, 38, 39). Whereas our study found ACEs contributed to a directly negative effect on sexually transmitted infections. One possible explanation for this finding is the concept of “benign resilience,” an unquantified resilience mechanism that mitigates the long-term effects of ACEs and reduces the likelihood of risky behaviors in adulthood, thereby reducing the risk of infectious diseases (38, 40). And, in Anhui Province, China, 44.6% of methamphetamine users reported negative childhood events (41). On the other hand, ACEs indirectly predict infectious diseases through drug injection as a mediator in our study. Firstly, drug injection was negatively associated with ACEs. In contrast, other scholars found that IDU in adulthood was strongly associated with ACEs, and that early childhood maltreatment led to increased risk of substance abuse, as well as being a possible victim and perpetrator of HIV risk behaviors (42–44). The characteristic of individuals with ACEs to holistically avoid negative health and social outcomes associated with childhood was called resilience, which was said to reduce the adverse effects (45). The target population of this study may establish the negative outcomes associated with drug injection while growing up, thereby reducing the likelihood of IDU in adulthood. Moreover, ACEs exposure did not indirectly predict infectious diseases by condom use as a mediator, which was totally contrary with our hypothesis. Previous studies have shown that ACEs were related to a lack of condom use and a higher number of sexual partners (46, 47). The possible reason may be the low detection rate of infectious diseases in the target population of this study. Notably, these infectious diseases can alter the immune system, leading to more severe health consequences and disease burdens in the long effects. It needs more explore the long effects rather than the relationship between ACEs and infectious diseases. One other possible explanation is that the presence of a suppression effect. Suppression occurs when the inclusion of a mediating or confounding variable in the model changes the direction or magnitude of the direct relationship between the independent and dependent variables.
Education, age, and gender might be positively associated with injecting drug use. Age and education exhibited correlation, as older adults tend to have lower levels of education, possibly due to economic or developmental reasons that prevented them from receiving education in their youth. Furthermore, older and better educated individuals were more likely to engage in drug injection, which aligns with other studies that have shown higher rates of blood-borne virus infections among older adults with a history of injecting drug use (8). Moreover, women may have a higher likelihood of injecting drugs and subsequently developing infectious diseases, while men with ACEs were also more prone to drug injection. Previous research has indicated that women were more susceptible to be affected by multiple forms of abuse and poor mental health outcomes that later manifest as IDU (42). These findings suggest that women may be at elevated risk for both ACE exposure and subsequent high-risk behaviors such as IDU, which can in turn increase vulnerability to infectious diseases. While the sample was male-dominated overall, the pathways observed in the model underscore the importance of addressing gender-specific trauma and substance use trajectories in prevention efforts. Ethnicity showed a negative association with drug injection, which may be attributed to the fact that the study area was predominantly inhabited by ethnic minority populations. The relatively lower rates of injection among these groups could reflect cultural or social protective factors, whereas Han Chinese individuals, though fewer in number locally, may experience increased psychosocial stressors leading to higher vulnerability to IDU.
On the other hand, the study did not provide enough evidence to validate our second hypothesis regarding the relationship between sexual behavior and infectious diseases. Although sexual risk factors were not associated with the HIV epidemic, majority (73%) of adult stimulant users in the United States involved in risky sexual behaviors with only 38% consistent condoms use (48). Conversely, another study alluded that an increase in the number of condomless anal sex partners could explain why MSM and those who primarily injected methamphetamine were more likely to be diagnosed with syphilis and HIV, and association between women who engage in sex works and condom use more often (7). Meanwhile, the association between cross-border behavior and infectious diseases also could not be elucidated. This may be because cross-border behavior, although common in border areas and with frequent cross-border marriages, was not a significant mobility factor due to the presence of stable, long-term residence in one village per country. A previous study also showed no significant differences in HIV, HCV, and syphilis infection rates between Chinese and Myanmar nationalities, possibly indicating that the high-risk sexual behaviors among individuals in cross-border marriages do not differ significantly in the long term. This observation may also be influenced by local infectious disease prevention and control policies, such as the equal entitlement of foreign women in cross-border marriages to resident health insurance and basic public health services (49).
There were several weaknesses in this study. Firstly, ACEs were assessed via self-recall, which could introduce information bias. Secondly, the cross-sectional design could hamper the ability to derive causation. Furthermore, SEM revealed pathways that were not comprehensive, as there were few directly observed variables and no potential variables considered that could influence exposure and outcome, thus limiting causal interpretation. Lastly, the study was confined to drug users receiving treatment, lacking a control group of non-drug users, and the majority of participants were Dai male patients, thereby restricting the generalizability of the findings.
5 Conclusion
ACEs might be a direct or indirect predictor for infectious disease in adulthood, injection of drug use might be a risk factor and moderate other factors of infectious disease. Subsequent cohort studies should be conducted to further explore the causal relationship between them.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Kunming Medical University Ethics Review Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
MZ: Data curation, Formal analysis, Software, Writing – original draft, Writing – review & editing. JH: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. JMY: Supervision, Writing – review & editing. JY: Investigation, Supervision, Writing – review & editing. JL: Conceptualization, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The survey was supported by National Natural Science Foundations of China (72274086 and 81760617); Applied Basic Research Projects of Yunnan Province (202301AY070001-258); and Reserve Talents Program for Young and Middle-aged Academic and Technical Leaders of Yunnan Province (202205AC160064). They were not involved in the design of the study, collection, analysis, and interpretation of data, and in writing the manuscript.
Acknowledgments
The authors thank all participants agreed to participate in this study and are appreciative of Professor Jianhua Fan of Center for Disease Control and Prevention, Xishuangbanna Dai Autonomous Prefecture and Professor Dongli Feng of Center for Disease Control and Prevention in Jinghong for supporting the fieldworks.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Degenhardt, L, Webb, P, Colledge-Frisby, S, Ireland, J, Wheeler, A, Ottaviano, S, et al. Epidemiology of injecting drug use, prevalence of injecting-related harm, and exposure to Behavioural and environmental risks among people who inject drugs: a systematic review. Lancet Glob Health. (2023) 11:e659–72. doi: 10.1016/S2214-109X(23)00057-8
2. Sharma, V, Tun, W, Sarna, A, Saraswati, LR, Pham, MD, Thior, I, et al. Prevalence and determinants of unprotected sex in intimate partnerships of men who inject drugs: findings from a prospective intervention study. Int J STD AIDS. (2019) 30:386–95. doi: 10.1177/0956462418802142
3. Handanagic, S, Finlayson, T, Burnett, JC, Broz, D, and Wejnert, C. Hiv infection and Hiv-associated behaviors among persons who inject drugs - 23 metropolitan statistical areas, United States, 2018. MMWR Morb Mortal Wkly Rep. (2021) 70:1459–65. doi: 10.15585/mmwr.mm7042a1
4. Semá Baltazar, C, Horth, R, Boothe, M, Sathane, I, Young, P, Chitsondzo Langa, D, et al. High prevalence of Hiv, Hbsag and anti-Hcv positivity among people who injected drugs: results of the first bio-behavioral survey using respondent-driven sampling in two urban areas in Mozambique. BMC Infect Dis. (2019) 19:1022. doi: 10.1186/s12879-019-4655-2
5. Wang, J, Wu, T, Tang, X, Zhang, C, Luo, H, Song, L, et al. Analysis of HIV combined with syphilis and HCV infection among drug users in Kunming during 2012 to 2021. Chin J AIDS STD. (2023) 29:210–3. doi: 10.13419/j.cnki.aids.2023.02.19
6. Su, S, Mao, L, Zhao, J, Chen, L, Jing, J, Cheng, F, et al. Epidemics of Hiv, Hcv and syphilis infection among synthetic drugs only users, heroin-only users and poly-drug users in Southwest China. Sci Rep. (2018) 8:6615. doi: 10.1038/s41598-018-25038-y
7. Dumchev, K. Challenges of sexually transmitted infections and sexual health among people who inject drugs. Curr Opin Infect Dis. (2022) 35:55–60. doi: 10.1097/QCO.0000000000000801
8. Cai, Y, Dai, Z, Wen, S, and Bhandari, R. Risk factors associated with infection of blood-borne virus among people who used methamphetamine. BMC Infect Dis. (2020) 20:742. doi: 10.1186/s12879-020-05464-y
9. Schneider, KE, White, RH, Musci, RJ, O'Rourke, A, Kilkenny, ME, Sherman, SG, et al. The relationship between polysubstance injection drug use, Hiv risk behaviors, and interest in pre-exposure prophylaxis (prep) among people who inject drugs in rural West Virginia. J Stud Alcohol Drugs. (2020) 81:740–9. doi: 10.15288/jsad.2020.81.740
10. Zhao, T, Chen, G, Sun, C, Gong, X, Li, H, and Fu, G. The epidemic of Hiv and syphilis and the correlation with substance abuse among men who have sex with men in China: a systematic review and Meta-analysis. Front Public Health. (2023) 11:1082637. doi: 10.3389/fpubh.2023.1082637
11. Refugio, ON, and Klausner, JD. Syphilis incidence in men who have sex with men with human immunodeficiency virus comorbidity and the importance of integrating sexually transmitted infection prevention into Hiv care. Expert Rev Anti-Infect Ther. (2018) 16:321–31. doi: 10.1080/14787210.2018.1446828
12. Chan, DPC, Sun, H-Y, Wong, HTH, Lee, S-S, and Hung, C-C. Sexually acquired hepatitis C virus infection: a review. Int J Infect Dis. (2016) 49:47–58. doi: 10.1016/j.ijid.2016.05.030
13. Semá Baltazar, C, Boothe, M, Kellogg, T, Ricardo, P, Sathane, I, Fazito, E, et al. Prevalence and risk factors associated with Hiv/hepatitis B and Hiv/hepatitis C co-infections among people who inject drugs in Mozambique. BMC Public Health. (2020) 20:851. doi: 10.1186/s12889-020-09012-w
14. Haider, MR, Kingori, C, Brown, MJ, Battle-Fisher, M, and Chertok, IA. Illicit drug use and sexually transmitted infections among Young adults in the us: evidence from a nationally representative survey. Int J STD AIDS. (2020) 31:1238–46. doi: 10.1177/0956462420950603
15. Daskalopoulou, M, Rodger, A, Phillips, AN, Sherr, L, Speakman, A, Collins, S, et al. Recreational drug use, Polydrug use, and sexual behaviour in Hiv-diagnosed men who have sex with men in the Uk: results from the cross-sectional Astra study. Lancet HIV. (2014) 1:e22–31. doi: 10.1016/S2352-3018(14)70001-3
16. Xia, D, Chen, Y, Chang, R, Xu, C, Yu, X, Liu, Y, et al. Psychosocial problems and Condomless anal sex among transgender women in two cities of China: study based on the Syndemic framework. Int J Environ Res Public Health. (2022) 19:6161. doi: 10.3390/ijerph192316161
17. Kampman, CJG, Hoebe, CJPA, Koene, R, Kamp, L, Jansen, K, Koedijk, FDH, et al. Sexually transmitted infections in male heterosexual Dutch clients who visited German cross-border female sex workers; a 3 year retrospective study. BMC Public Health. (2020) 20:1182. doi: 10.1186/s12889-020-09240-0
18. Okiria, AG, Achut, V, McKeever, E, Bolo, A, Katoro, J, Arkangelo, GC, et al. High Hiv and syphilis prevalence among female sex workers and sexually exploited adolescents in Nimule town at the border of South Sudan and Uganda. PLoS One. (2023) 18:e0266795. doi: 10.1371/journal.pone.0266795
19. Feelemyer, JP, Richard, E, Khan, MR, Scheidell, JD, Caniglia, EC, Manandhar-Sasaki, P, et al. Does the association between stimulant use and high risk sexual behavior vary by injection drug use, sexual minority status, or Hiv infection status? A Meta-analysis. AIDS Behav. (2023) 27:2883–90. doi: 10.1007/s10461-023-04012-4
20. Rivas-Rivero, E, and Bonilla-Algovia, E. Adverse childhood events and substance misuse in men who perpetrated intimate partner violence. Int J Offender Ther Comp Criminol. (2022) 66:876–95. doi: 10.1177/0306624X211013519
21. Hall, DL, Batchelder, AW, Fitch, CJ, Glynn, TR, Ironson, G, Mizrach, H, et al. Posttraumatic cognitions and Condomless sex among men who have sex with men (Msm) with a history of childhood sexual abuse: the role of avoidance coping. AIDS Behav. (2023) 27:667–72. doi: 10.1007/s10461-022-03801-7
22. Pulerwitz, J, McClair, T, Gottert, A, Shabangu, P, Cawood, C, Chipeta, E, et al. Effects of Men's lifetime adverse events experience on violence, Hiv risk, and wellbeing: insights from three countries. AIDS. (2022) 36:S99–S108. doi: 10.1097/QAD.0000000000003224
23. Hughes, K, Bellis, MA, Sethi, D, Andrew, R, Yon, Y, Wood, S, et al. Adverse childhood experiences, childhood relationships and associated substance use and mental health in Young Europeans. Eur J Pub Health. (2019) 29:741–7. doi: 10.1093/eurpub/ckz037
24. Hughes, K, Bellis, MA, Hardcastle, KA, Sethi, D, Butchart, A, Mikton, C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and Meta-analysis. Lancet Public Health. (2017) 2:e356–66. doi: 10.1016/S2468-2667(17)30118-4
25. VanderEnde, K, Chiang, L, Mercy, J, Shawa, M, Hamela, J, Maksud, N, et al. Adverse childhood experiences and Hiv sexual risk-taking behaviors among Young adults in Malawi. J Interpers Violence. (2018) 33:1710–30. doi: 10.1177/0886260517752153
26. Rakkapao, N, Kiattisaksiri, P, and Samakkekarom, R. Knowledge, attitudes, and Hiv/Aids risk behaviors of Myanmar migrant Workers in Thailand. GHMJ. (2019) 3:84–94. doi: 10.35898/ghmj-33581
27. He, H, Zhang, J, and Xiu, D. China’s migrant population and health. China Popul Dev Stud. (2019) 3:53–66. doi: 10.1007/s42379-019-00032-7
28. Chen, X, Zhou, Y-H, Ye, M, Wang, Y, Duo, L, Pang, W, et al. Burmese injecting drug users in Yunnan play a pivotal role in the cross-border transmission of Hiv-1 in the China-Myanmar border region. Virulence. (2018) 9:1195–204. doi: 10.1080/21505594.2018.1496777
29. Rocha-Jiménez, T, Morales-Miranda, S, Fernández-Casanueva, C, Silverman, JG, Zúñiga, ML, Goldenberg, SM, et al. Migration and mobility: correlates of recent HIV testing among substance using female sex Workers at the Mexico-Guatemala Border. AIDS Behav. (2022) 26:1467–76. doi: 10.1007/s10461-021-03501-8
30. Lee, S-Y, and Song, X-Y. Bayesian analysis of structural equation models with dichotomous variables. Stat Med. (2003) 22:3073–88. doi: 10.1002/sim.1544
31. Li, J, Li, M, Zhang, Y, Li, J, Zhao, Y, Lu, R, et al. Amphetamine-type stimulants use and socio-economic factors associated with hepatitis C antibody positivity among border drug users in south of China. Front Public Health. (2022) 10:998768. doi: 10.3389/fpubh.2022.998768
32. Bernstein, DP, Stein, JA, Newcomb, MD, Walker, E, Pogge, D, Ahluvalia, T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
33. Grant, BF, Goldstein, RB, Saha, TD, Chou, SP, Jung, J, Zhang, H, et al. Epidemiology of Dsm-5 alcohol use disorder: results from the National Epidemiologic Survey on alcohol and related conditions III. JAMA Psychiatry. (2015) 72:757–66. doi: 10.1001/jamapsychiatry.2015.0584
34. Joshi, N, Chandane Tak, M, and Mukherjee, A. The involvement of Micrornas in Hcv and Hiv infection. Ther Adv Vaccines Immunother. (2022) 10:25151355221106104. doi: 10.1177/25151355221106104
35. Bosetti, D, Mugglin, C, Calmy, A, Cavassini, M, Stöckle, M, Braun, D, et al. Risk factors and incidence of sexually transmitted infections in the Swiss Hiv cohort study. Open Forum Infect Dis. (2022) 9:ofac592. doi: 10.1093/ofid/ofac592
36. Shayan, SJ, Nazari, R, and Kiwanuka, F. Prevalence of HIV and HCV among injecting drug users in three selected who-Emro countries: a meta-analysis. Harm Reduct J. (2021) 18:59. doi: 10.1186/s12954-021-00505-4
37. Mateu-Gelabert, P, Sabounchi, NS, Guarino, H, Ciervo, C, Joseph, K, Eckhardt, BJ, et al. Hepatitis C virus risk among Young people who inject drugs. Front Public Health. (2022) 10:835836. doi: 10.3389/fpubh.2022.835836
38. Ashton, K, Davies, AR, Hughes, K, Ford, K, Cotter-Roberts, A, and Bellis, MA. Adult support during childhood: a retrospective study of trusted adult relationships, sources of personal adult support and their association with childhood resilience resources. BMC Psychol. (2021) 9:101. doi: 10.1186/s40359-021-00601-x
39. Wade, R, Cronholm, PF, Fein, JA, Forke, CM, Davis, MB, Harkins-Schwarz, M, et al. Household and community-level adverse childhood experiences and adult health outcomes in a diverse urban population. Child Abuse Negl. (2016) 52:135–45. doi: 10.1016/j.chiabu.2015.11.021
40. Js, L, Li, J, You, J, and Lu, R. Research about adverse childhood experiences and behavior of lnjection drug use among border drug users. J Kunming Med Univ. (2022) 43:35–40.
41. Chen, Y, Zhang, J, and Sun, Y. The relationship between childhood abuse and depression in a sample of Chinese people who use methamphetamine. Int J Clin Health Psychol. (2019) 19:181–8. doi: 10.1016/j.ijchp.2019.06.003
42. Abajobir, AA, Kisely, S, Williams, G, Clavarino, A, Strathearn, L, and Najman, JM. Gender-based differences in injecting drug use by Young adults who experienced maltreatment in childhood: findings from an Australian birth cohort study. Drug Alcohol Depend. (2017) 173:163–9. doi: 10.1016/j.drugalcdep.2016.12.027
43. Liu, M, Luong, L, Lachaud, J, Edalati, H, Reeves, A, and Hwang, SW. Adverse childhood experiences and related outcomes among adults experiencing homelessness: a systematic review and Meta-analysis. Lancet Public Health. (2021) 6:e836–47. doi: 10.1016/S2468-2667(21)00189-4
44. Macleod, J, Hickman, M, Jones, HE, Copeland, L, McKenzie, J, De Angelis, D, et al. Early life influences on the risk of injecting drug use: case control study based on the Edinburgh addiction cohort. Addiction. (2013) 108:743–50. doi: 10.1111/add.12056
45. Bellis, MA, Hardcastle, K, Ford, K, Hughes, K, Ashton, K, Quigg, Z, et al. Does continuous trusted adult support in childhood impart life-course resilience against adverse childhood experiences - a retrospective study on adult health-harming Behaviours and mental well-being. BMC Psychiatry. (2017) 17:110. doi: 10.1186/s12888-017-1260-z
46. Kidman, R, Breton, E, Behrman, J, and Kohler, H-P. A prospective study on adverse childhood experiences and Hiv-related risk among adolescents in Malawi. AIDS. (2022) 36:2181–9. doi: 10.1097/QAD.0000000000003377
47. Song, W, and Qian, X. Adverse childhood experiences and teen sexual behaviors: the role of self-regulation and school-related factors. J Sch Health. (2020) 90:830–41. doi: 10.1111/josh.12947
48. Meade, CS, Towe, SL, Xu, Y, and Rainer, C. Hiv prevalence and associated risks in a respondent-driven sample of illicit stimulant users in a southern United States City. AIDS Behav. (2020) 24:2336–46. doi: 10.1007/s10461-020-02793-6
49. Xu, CP, Du, BL, Hou, Y, Shi, NL, Wang, W, Yang, YC, et al. The prevalence of Hiv, hepatitis C virus and syphilis and related factors among cross-border couples in Mangshi County, Dehong Dai and Jingpo autonomous prefecture of Yunnan Province from 2017 to 2019. Zhonghua Yu Fang Yi Xue Za Zhi. (2022) 56:1101–6. doi: 10.3760/cma.j.cn112150-20211029-01001
Keywords: injection of drug use, adverse childhood experiences, infectious disease, structural equation models, border
Citation: Zhang M, He J, Young JM, You J and Li J (2025) Impact pathways of adverse childhood experiences on infectious diseases among substance abusers in border regions: structural equation modeling. Front. Public Health. 13:1518607. doi: 10.3389/fpubh.2025.1518607
Edited by:
Hai-Feng Pan, Anhui Medical University, ChinaReviewed by:
Stefano Ferracuti, Sapienza University of Rome, ItalyPei Wang, Fudan University, China
Copyright © 2025 Zhang, He, Young, You and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Li, b25seWppbmcyMDA1QGhvdG1haWwuY29t
†These authors have contributed equally to this work
 Mingmei Zhang
Mingmei Zhang Jianhui He2†
Jianhui He2† Jing You
Jing You