- The Second Affiliated Hospital of Guangxi Medical University, Nanning, China
Objective: Given the discrepancy between the low utilization rate of hospice care services and the high willingness to choose hospice care, this study aims to identify the factors influencing the utilization among older adults. The findings will provide a foundation for interventions designed to enhance the growth of this service.
Design: A mixed-methods study of convergent parallel designs.
Methods: In the quantitative research phase, in January 2024, a convenience sampling method was used to recruit 350 terminally ill older individuals from three hospitals and three communities in Guangxi, China. Face-to-face surveys were conducted using a general information questionnaire, a Home Hospice Care Service Needs Questionnaire, and a Home Hospice Care Service Knowledge, Attitude, and Practice Scale. In the qualitative research phase, semi-structured interviews were conducted with 16 terminally ill older individuals to explore the barriers and facilitators to the utilization of home hospice care services.
Results: A total of 332 (94.86%) older individuals completed the survey, and 45 (13.55%) accepted home hospice care. The identified barriers to utilization included high physiological, psychological, and spiritual needs, as well as families’ feelings of guilt. The facilitators included being of advanced age (≥80 years), having chronic diseases, not needing a caregiver, having high social needs and knowledge scores, and perceiving a significant economic burden.
Conclusion: The utilization of home hospice care services by older adults is lower, which is influenced by both subjective and objective factors. The novel identification of ‘families’ guilty’ as a barrier underscores the need for targeted interventions that address emotional and psychological barriers within families. Policymakers should consider these factors when developing strategies to promote the development of home hospice care for older adults, ensuring that interventions are culturally sensitive and economically feasible.
1 Introduction
China’s aging process is accelerating, with the aged population expected to increase from 250 to 400 million by 2050, resulting in an aging rate exceeding 30% (1). As age increases, the risk of death increases and the ability to take care of themselves declines (2, 3). Among the older adults, 6.18 million were disabled, 82.34% were unable to look after themselves before they died (4, 5). Therefore, the quality of life for the older adult at the end of life is in urgent need of attention.
According to the report of the World Health Organization (6), globally, 25.7 million people need hospice care in the last year of life, with older adults accounting for over 69%. Due to the traditional Chinese cultural concept of ‘returning to one’s roots’ among Chinese older adults, approximately 87–89% of them pass away at home (7, 8). Home hospice care can improve the quality of life for older adults who die at home and their family members (9), reducing unnecessary hospitalizations and medical costs (10, 11). Therefore, studying home hospice care services for older adults is of great significance for improving the quality of life of older adults at the end of life.
According to the location of service, China’s hospice care service models include home hospice care and inpatient hospice care. Home hospice care mainly refers to terminally ill patients living at home, receiving basic life care from family members, and obtaining medical services or consultations from general practitioners and hospice care institutions to meet the needs of patients and their families (12). China has developed hospice care into a basic medical service, but its development started relatively late, with pilot programs beginning in 2017, and home hospice care services started even later (13). At present, China’s home hospice care service system is not mature and is unable to meet the needs of terminally ill older adults. Therefore, it is necessary to conduct more research. The willingness to utilize hospice care can promote its development (14). In South Korea, 88.9% of older adults at the end of life are willing to choose home hospice care (15); however, in China, 38.5% only (14). Compared with the global average, China’s utilization rate of hospice care services is even lower. Globally, 14% of people who need hospice care are able to receive such services, while in China, only 0.3% (15). In order to meet the needs of China’s large older population, it is necessary to explore the facilitators and barriers for older adults to utilize home hospice care services to promote the development of hospice care.
The development of hospice care in China is caught in a dilemma where there is a relatively high willingness but a low utilization rate of services (16). The reason for this dilemma is not just due to a lack of supply. In fact, the occupancy rate of hospice care beds is not high (15). Therefore, a systematic understanding of the factors influencing the utilization of home hospice care for terminally ill older adults could better facilitate its development. Existing research indicates that demographic characteristics, such as age (17, 18), health beliefs (19), economic income (20), perceived risk of illness (21), and attitudes toward death (22), influence the willingness or acceptance of hospice care services. It is evident that the factors influencing the utilization of hospice care encompass both objective and subjective elements. However, current research predominantly focuses on intentions, often employing either solely quantitative or qualitative methods, resulting in the study of factors influencing home hospice care utilization being somewhat limited. To comprehensively explore these factors and consider both objective conditions and subjective perceptions, it is essential to adopt a mixed-methods research approach.
The Andersen Model, a robust theoretical framework for analyzing the factors influencing the utilization of healthcare services, was proposed by American scholar Ronald Andersen (23). Therefore, guided by the Andersen Model, we employed a mixed-methods approach with a convergent parallel design to thoroughly investigate the associated factors of terminally ill older adults toward the utilization of home hospice care. This research aims to make up for the insufficiency of mixed-methods evidence in the research on factors influencing the utilization of home hospice care and provide actionable entry points to promote the development of home hospice care.
2 Theoretical framework
The Andersen Model posits that individual’s utilization healthcare services decided by the following three dimensions: predisposing factors, enabling factors, and need factors (23). Predisposing factors are characteristics that exist before an individual encounters a health problem, including demographic characteristics, social structure, health beliefs, and attitudes. Enabling factors are resources that facilitate or hinder access to healthcare services, including personal, family, and community resources. Need factors reflect the actual or perceived need for health services. Predisposing factors include demographic, social structure, and health belief variables. Enabling factors encompass personal, family, and social resources. Need factors involve the perception and evaluation of health status. After five revisions, the model can comprehensively explain health service utilization behavior (24).
3 Methods
3.1 Design
Our research team consists of 15 members, including two deputy chief physicians and five deputy chief nurses in the field of hospice care, seven graduate students, and one graduate advisor. Our research team was responsible for the design and implementation of the entire study. Due to the cultural background of taboo death in China (in Chinese culture, death is often considered a taboo topic, primarily due to the belief that discussing death brings bad luck or misfortune), this study adopted a mixed method of quantitative and qualitative research, which results can complement each other, enhancing the depth and breadth of the research on the associated factors of home hospice care for older adults. We conducted a convergent parallel design, meaning that both types of research were employed independently and simultaneously (25). The quantitative research was conducted using Paper-version questionnaires through one-on-one interviews, and the qualitative research was completed using semi-structured interviews. This study’s report refers to the Good Report of a Mixed-Methods Study (GRAMMS) (26).
3.2 Participants
In January 2024, a convenience sampling method was used to select 350 terminally ill older individuals from three hospitals and three communities in Guangxi, China, for the study. The surveyed hospitals and communities are all pilot sites for hospice care. For the qualitative study, the participants were recruited as follows: inclusion criteria included (1) older adult terminal patients (aged ≥60) or their primary caregivers who were deemed eligible for home hospice care by a physician and (2) those who provided informed consent to participate in the survey, and the exclusion criterion was individuals with communication difficulties. The inclusion criterion for the qualitative study was those who had completed the questionnaire and were willing to undergo a 20–30-min interview. According to logistic regression for sample size, at least 5–10 times the number of independent variables surveyed for the quantitative study is required and considered for a 10% sample loss (27). With 21 independent variables, the required sample size for the quantitative study was calculated to be 117–234 cases. The sample size for the qualitative study was based on the principle of saturation (28). Ultimately, a total of 332 (94.86%) terminally ill older individuals completed the questionnaire survey; 18 who failed to complete it were excluded, and 16 of them participated in qualitative interviews.
3.3 Research instruments
3.3.1 General information
Our research team designed a survey questionnaire to collect general information about terminally ill older individuals after a comprehensive literature review and group discussions. Guided by the Andersen Model, general data are divided into the following three categories with detailed content as follows: (1) predisposing factors, including gender, age, ethnicity, whether suffering from chronic diseases, and awareness of home-based hospice care; (2) Enabling factors, including marital status, place of residence, education level, monthly personal income (Chinese Yuan), method of medical payment, living arrangement, and type of primary caregiver; (3) need factors include the activities of daily living (ADL) score. The Barthel Index Scoring Scale is used for scoring. The Barthel Index, designed by American Florence Mahoney and Dorothy Barthel (29), is applied clinically and is a widely used tool internationally. The total score is 100 points, with higher scores indicating greater self-care ability and less dependency; a score of 100 means no dependency, 61–99 points indicate mild dependency, 41–60 points indicate moderate dependency, and ≤40 points indicate severe dependency. The nutritional risk of older adults was measured using nutritional risk screening (NRS 2002), which was proposed by Danish scholar Kondrup in 2002 (30). The total score of NRS 2002 consists of three parts: nutritional status impairment score, disease severity score, and age score (over 70 years old plus 1 point). The total score is 0–7 points. If the patient’s score reaches or exceeds 3 points, it is considered that there is a nutritional risk, and nutritional support is required.
3.3.2 Home hospice care service need scale
This scale was designed by our team, referring to China’s hospice care practice guidelines (31) and humanistic theories. The scale is divided into four dimensions: physiological needs (related to relieving symptoms, six items), psychological needs (related to helping patients cope with adverse emotional reactions, four items), social needs (related to individual social relations and support, seven items), and spiritual needs (related to patient’s beliefs, values and the pursuit of the meaning of life, four items), with a total of 21 items. The scoring uses a Likert 5-point scale as follows: Completely do not need (1 point), Occasionally need (2 points), Moderately need (3 points), Very much need (4 points), and Completely need (5 points). The total score is 21–105 points. The higher the total score, the greater the demand for home hospice care services. In our study, we confirmed that the scale has good reliability and validity when applied to terminally ill older adult individuals. Cronbach’s alpha is 0.949, and Scale-level Content Validity Index (S-CVI) is 0.923. See Appendix 1 for the scale.
3.3.3 Knowledge, attitude, and behavior of home hospice care scale
Before the survey, our team developed the scale guided by the knowledge theory, belief theory, and action theory of the Behavioral Change Wheel (BCW) (32). The scale uses a Likert 5-point scoring system as follows: Strongly agree (5 points), Agree (4 points), Uncertain (3 points), Disagree (2 points), and Strongly disagree (1 point). To enhance the reliability of the survey results, seven items were reverse-scored. The total score is 29–145 points. The higher the total score, the better understanding of home hospice care. This scale has good reliability and validity, too, with a Cronbach’s alpha of 0.947 and an S-CVI of 0.941. See Appendix 2 for the scale.
3.3.4 Interview outline
The interview outline was designed to focus on the psychological processes and associated factors involved in the use of home hospice care by older adults or their families, and it referenced relevant literature (33). The final version of the interview outline was modified and confirmed after conducting pre-interviews with two terminally ill older individuals to ensure the understandability and accessibility of the guide. The details are as follows: (1) How did you learn about home hospice care? What are your thoughts on it? (2) Why did you accept/refuse home hospice care services? (3) What barriers or difficulties have you encountered when receiving home hospice care services? (4) What are your needs for home hospice care services? (5) What suggestions do you have for the provision of home hospice care services?
4 Data collection
4.1 Quantitative data collection
Before the survey, uniform training was provided to the members of the research team. During the research process, the purpose and significance of the study were first introduced to the respondents. After obtaining their consent, the research team members conducted one-on-one interviews with each respondent using the questionnaire. After the interview, two researchers checked all the questionnaires, eliminated the questionnaires that were not completed and the answer rules, and then entered the data into the Excel table. Of them, 18 (5.14%) questionnaires were incomplete.
4.2 Qualitative data collection
Before the interview, staff from the hospice care institutions or hospitals communicated with the interviewees in advance. After the interviewees’ consent, two members of the research team conducted semi-structured interviews (one was responsible for the main interview, and the other was responsible for recording the interview dialogue, the interviewee’s expressions, and body language). The two members had received training in qualitative interviewing and participated in the collection and analysis of quantitative data. Hospitalized patients were interviewed in the hospital, while home-based patients were interviewed at their homes under the guidance of hospice care personnel. The interview environment was quiet and relaxed, with each interview lasting approximately 20–30 min. The interviewers asked questions according to the interview guide, listened carefully, refrained from making suggestions or leading the interviewee, and used reflective questions to allow the interviewee to express their feelings. If necessary, the interviewers provided supplementary descriptions of the concept of home hospice care and repeated and summarized the interviewee’s statements. Within 24 h of the interviews, the recording was converted into text, and the text data were returned to the interviewee for reading to ensure the accuracy of the data.
5 Data analysis
5.1 Quantitative data analysis
The SPSS version 27.0 was used for descriptive statistics and difference comparisons. Categorical data are represented by frequency (n) and percentage (%). Continuous data are expressed as mean ( ) and standard deviation (SD). In univariate analysis, comparisons of rates are made using the Chi-square test, and comparisons of means are made using the t-test. Multivariate analysis is conducted using logistic regression. Considering that the variable of education has a great OR value in the model, and it is reclassified or removed, primary school and below and junior high school are combined, and the sensitivity analysis is repeated by binary logistic regression. The significance level is set at α = 0.05 (two-tailed).
5.2 Qualitative data analysis and result integration
Directed content analysis was employed for data analysis. After importing the text into the Nvivo 14.0 software, the Anderson Model was used as the coding framework, and the coding process was carried out in the following steps: (1) repeatedly listening to the recordings and reading the transcribed texts to gain an overall sense; (2) identifying factors influencing the utilization of home hospice care by older adults, which is the open coding; (3) aggregating all codes and, through repeated comparison and categorization, grouping codes with the same attributes into the same category, which is the axial coding; (4) classifying themes into three dimensions: predisposing factors, enabling factors, and need factors, which is the selective coding. Finally, the results were integrated using the parallel data comparison method (34). First, quantitative and qualitative data were placed side by side for direct comparison of their consistencies and differences. The integrated results were then jointly presented in tables to illustrate the findings and meta-inferences. All the processes were performed independently and simultaneously by two researchers. In case of disagreement, our research team held a collective discussion and finally reached a conclusion, which ensured the logic and reliability of each topic.
6 Results
6.1 Common method bias
Harman single-factor method was used to test the common method bias (35). The results showed that the characteristic roots of the 9 factors were greater than 1, and the explained variation of the first factor was 30.06%, which was lower than the critical value of 40.00%. Therefore, it shows that there is no obvious common method bias in this study.
6.2 Quantitative results
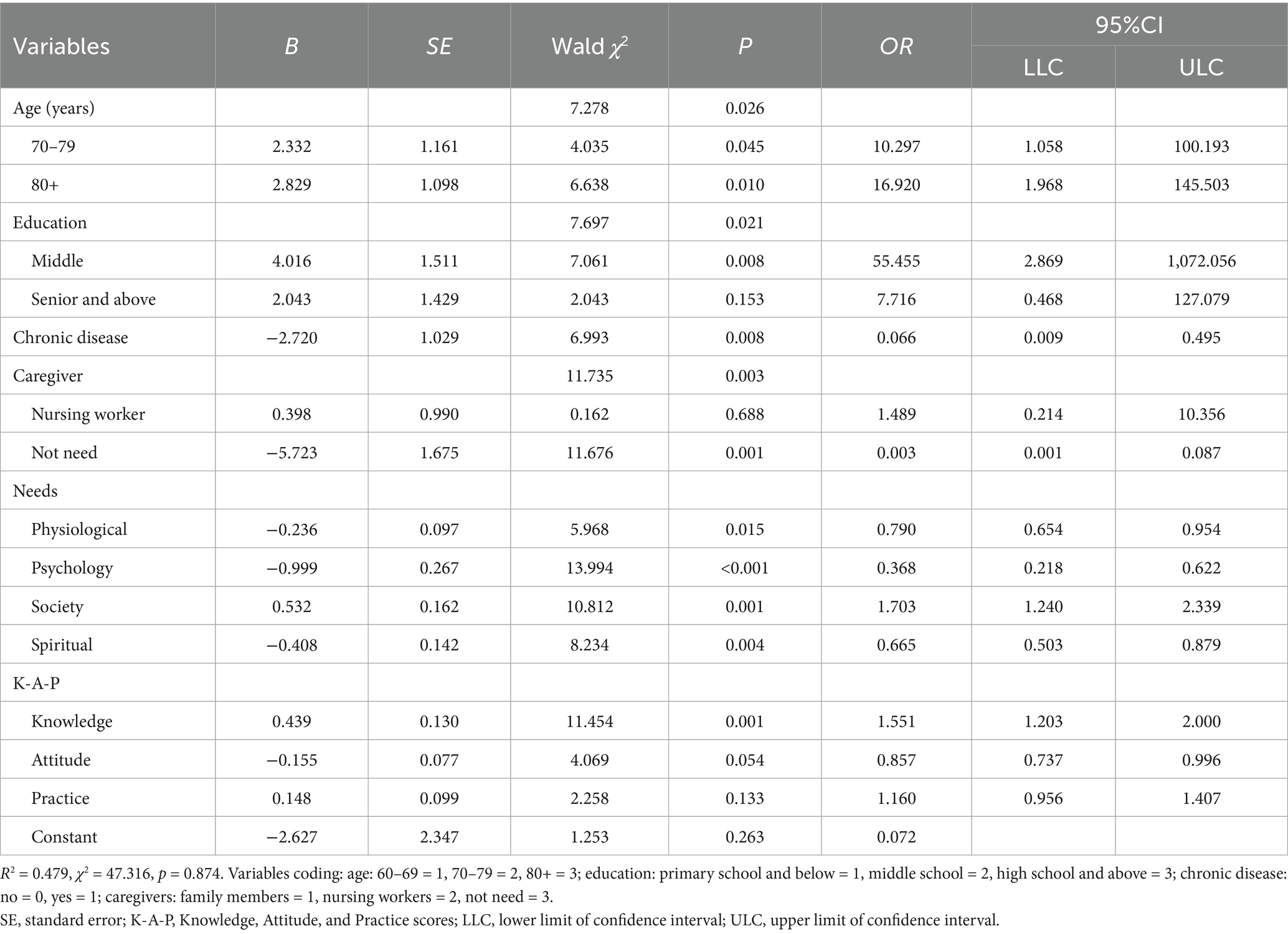
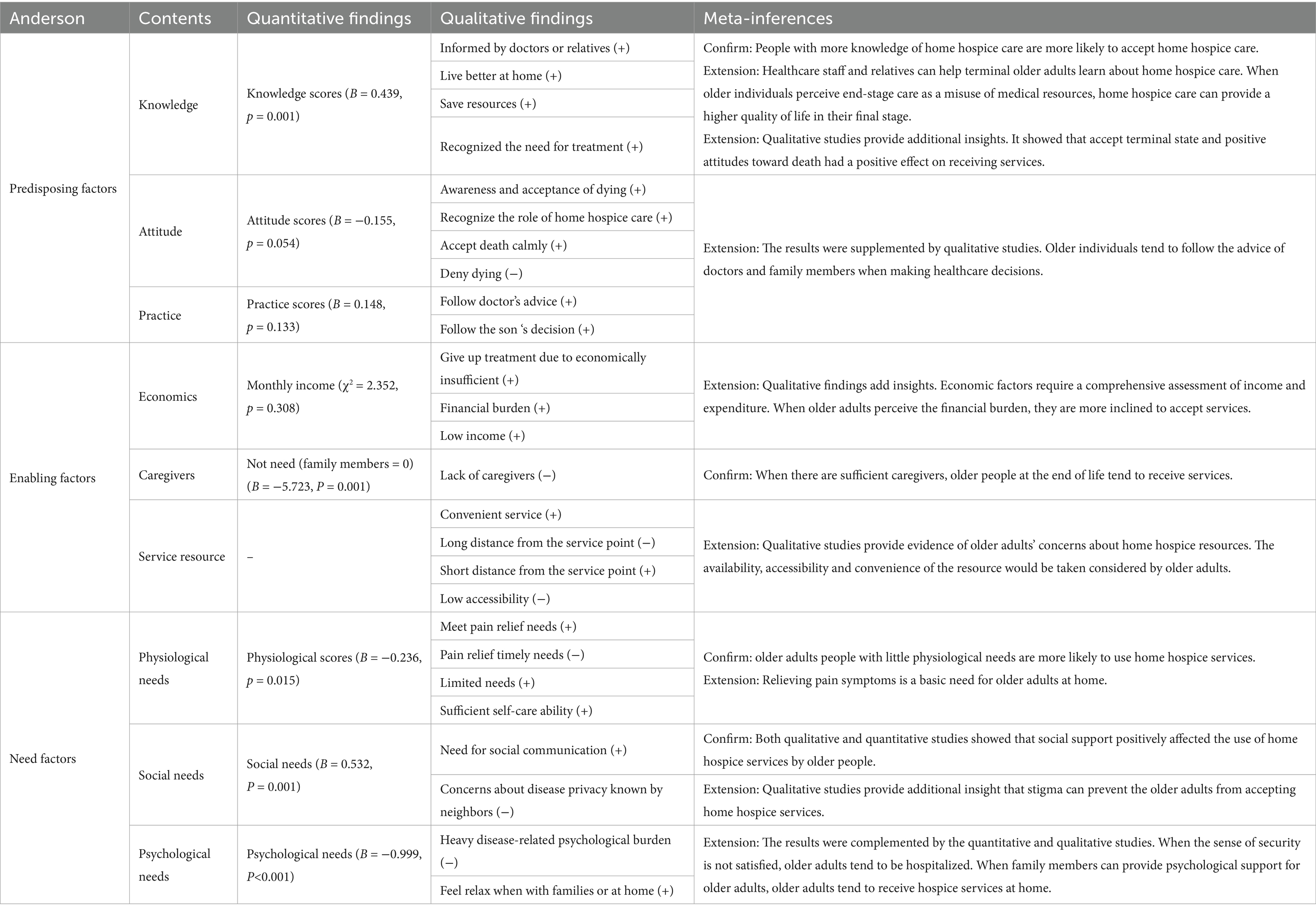
The average age of older adults was 70.73 years (SD = 10.12), ranging from 60 to 96 years old. A total of 45 (13.55%) older adults utilized home hospice care services. The Home Hospice Care Service Need Scale score was 24–100 (60.67 ± 19.91). The Knowledge, Attitude, and Behavior of Home Hospice Care Scale score was 32–124 (62.37 ± 17.80). Univariate analysis results showed that the utilization of home hospice care by older adults differed significantly in terms of age (F = 6.971, p = 0.008), type of caregiver (F = 30.981, p < 0.001), physiological needs scores (t = 9.995, p < 0.001), psychological needs scores (t = 12.901, p < 0.001), social needs scores (t = 4.069, p < 0.001), spiritual needs scores (t = 8.971, p < 0.001), knowledge scores (t = −9.442, p < 0.001), belief scores (t = −4.315, p < 0.001), and attitude scores (t = −10.418, p < 0.001). The general characteristics of older adults and the results of univariate analysis are presented in Table 1. Furthermore, binary logistic regression analysis was used to examine the associated factors of home hospice care service utilization, with detailed results shown in Table 2.
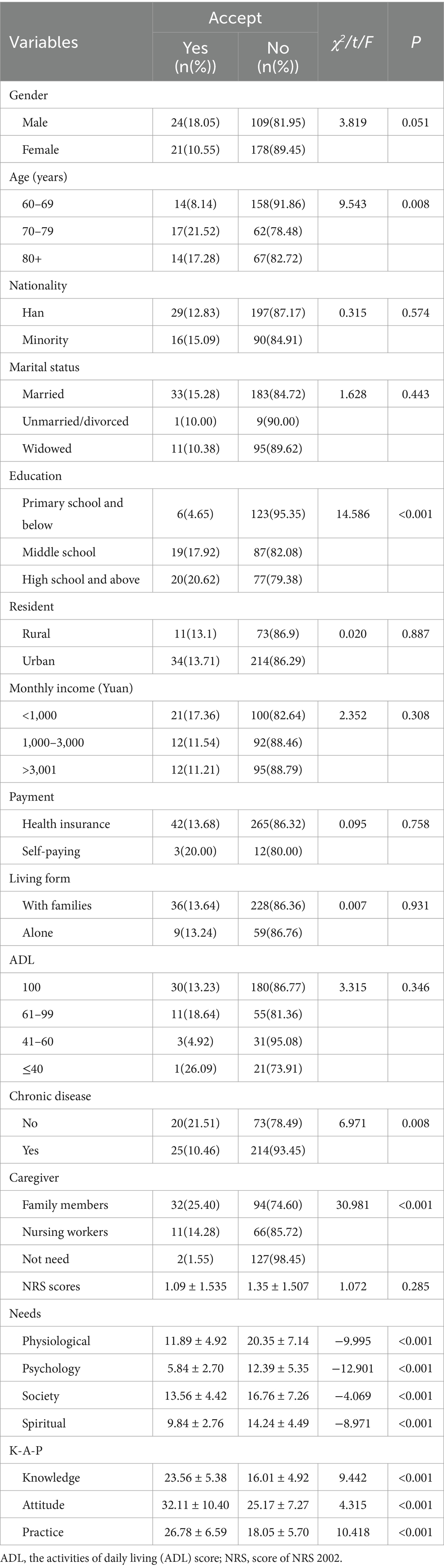
Table 1. Characteristics of participants and analysis of differences in home hospice care acceptance.
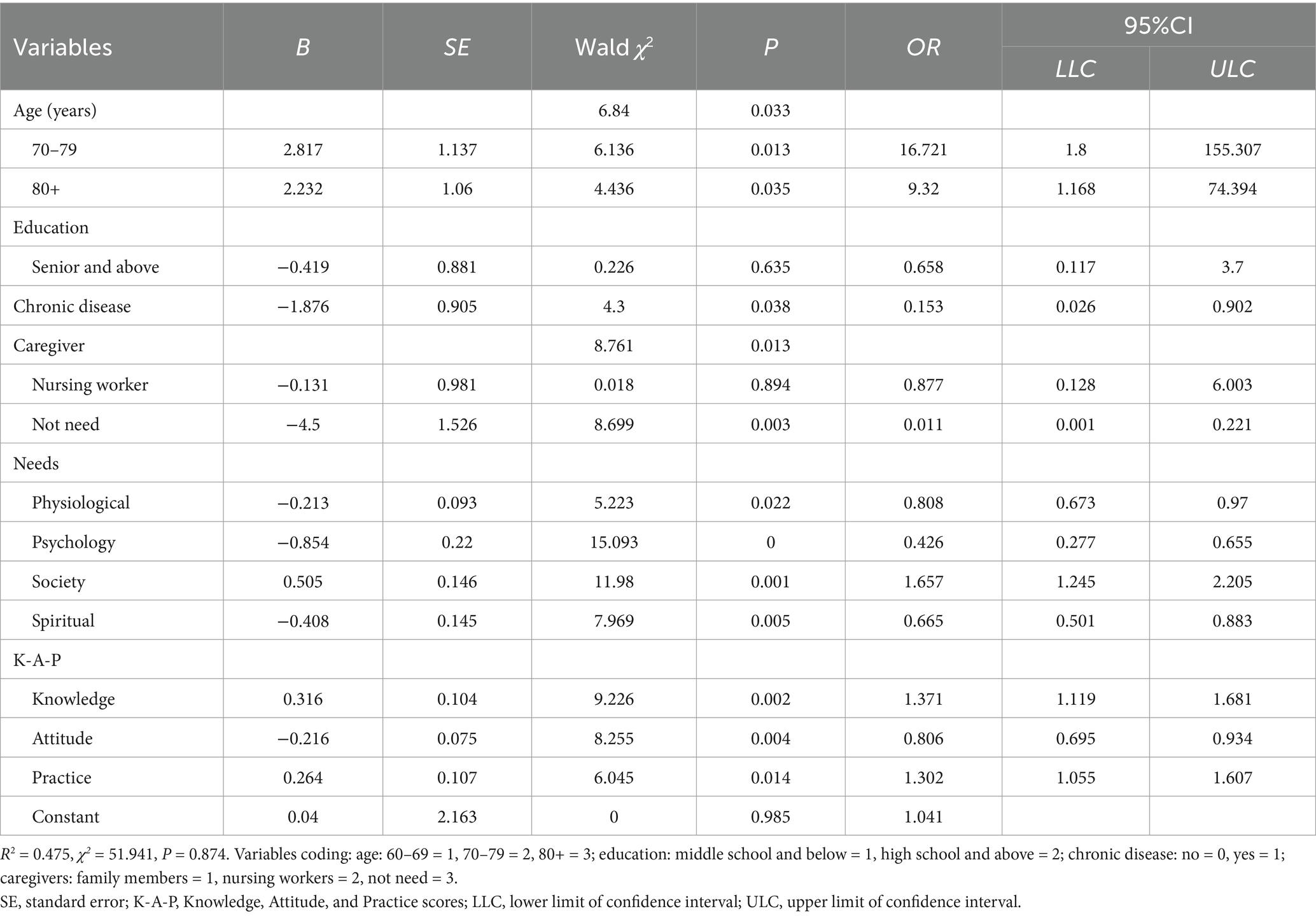
6.3 Sensitivity analysis
After merging the variable of education, the analysis showed that age, education, chronic disease, caregiver, physiological needs, psychological needs, social needs, spiritual needs, and knowledge, attitude, and practice are factors associated with utilization (P<0.05). When removed, the same results are shown, indicating that the results are robust (see Table 3).
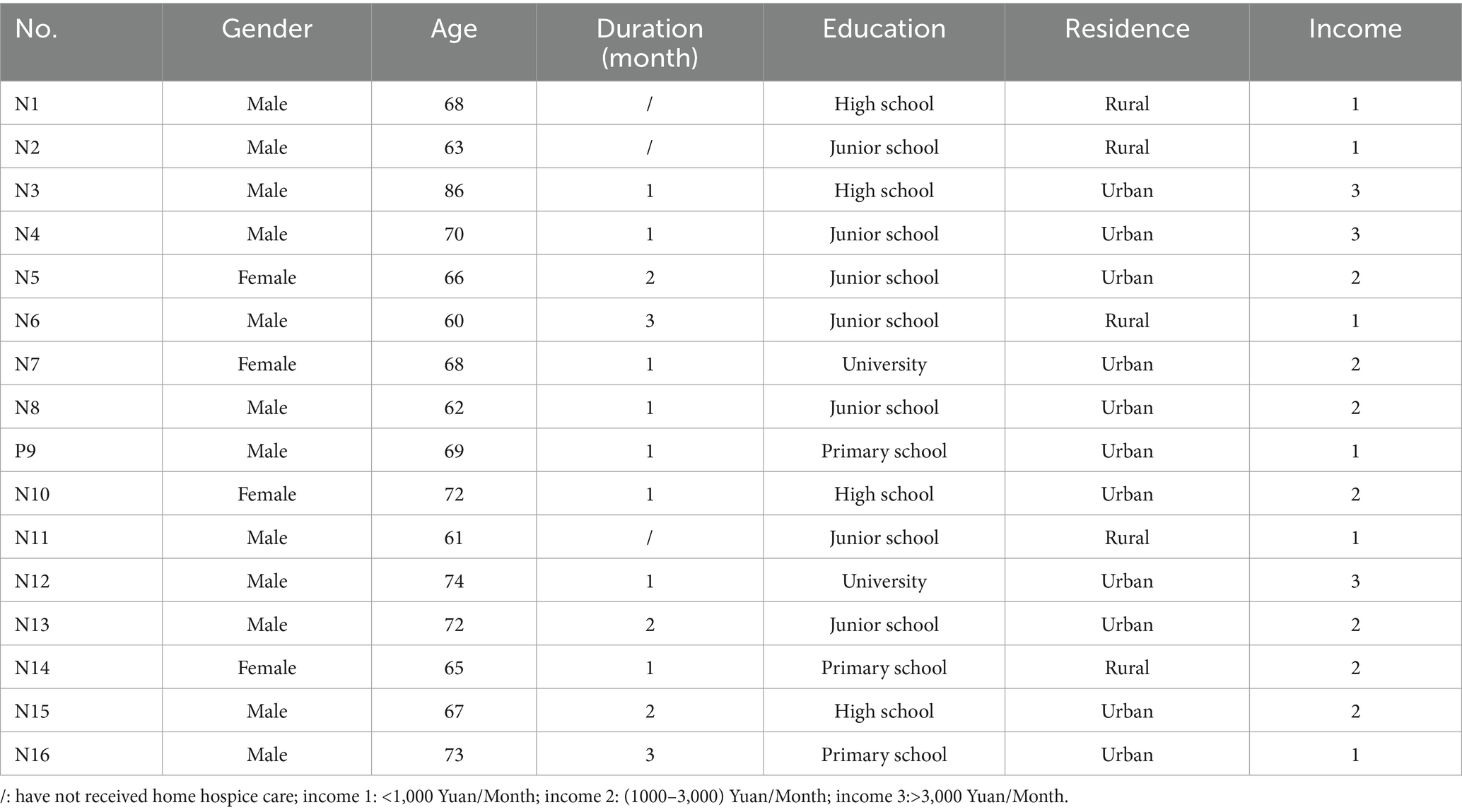
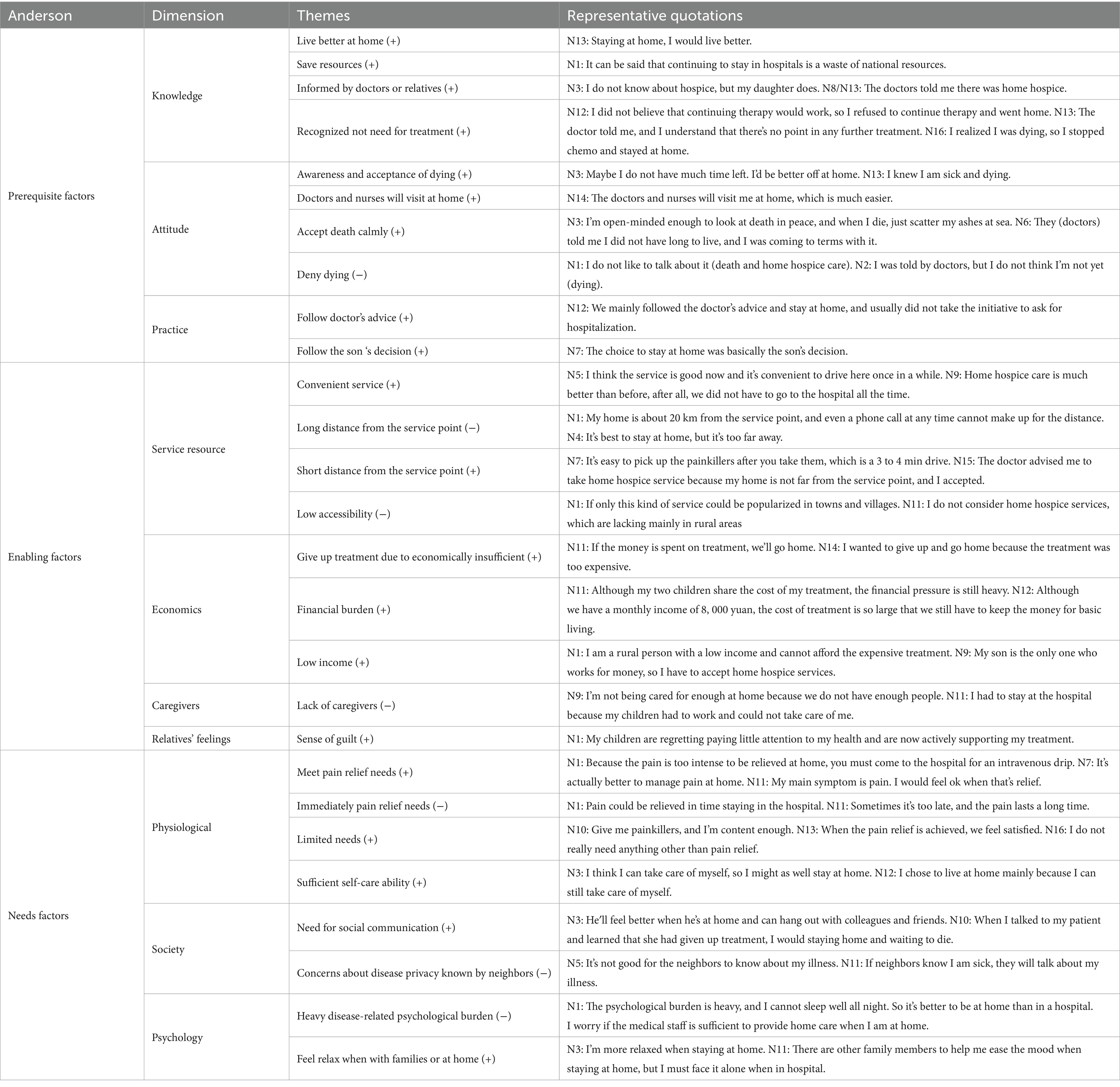
6.4 Qualitative research results
A total of 16 individuals participated in semi-structured interviews, with 13 (81.25%) utilizing home hospice care and three receiving treatment in the hospital, with an average age of 68.50 years (SD = 6.36). All were cancer patients, and their detailed characteristics are shown in Table 4. From the interviews, 29 factors influencing the utilization of home hospice care by terminally ill older individuals were identified. These associated factors were first categorized into physiological needs, psychological needs, social needs, knowledge, beliefs, and attitudes, and then all categories were grouped into the themes of predisposing factors, enabling factors, and need factors within the Andersen Model. Detailed information is presented in Table 5. The integrated results are detailed in Table 6.
7 Discussion
7.1 Predisposing factors associated with the utilization of home hospice care by the older adults
When exploring the predisposing factors for the utilization of home hospice care services among older adults, first, age is a factor that influences the use of home hospice care, which is similar to the findings of Kumar et al. (18). In our study, older people are more likely to choose home-based hospice care services, which may be related to their more ingrained ‘bottom-up’ concept and greater acceptance of death. Some researches also show that the proportion of older adults who chose to die at home is the highest (14.5 times that of hospitals, 3.4 times that of nursing institutions) (36), and their acceptance of death scores are also higher (37). Second, older adults with chronic diseases are also more inclined to utilize home hospice care services. This might be because these individuals have endured economic burdens for a long time, and home care is usually less expensive than hospitalization (38). However, qualitative research indicates that the factors are complex, including self-care ability and the pursuit of quality of life, which are relatively consistent with the existing research results (39, 40). In the future, methods such as longitudinal studies should be adopted to conduct more in-depth research on the utilization of palliative care services by older people in order to better understand the interaction of these factors and their impact on the utilization of services. More importantly, both quantitative and qualitative studies indicated that awareness and knowledge about home hospice care services were key factors in utilization. This factor positively influences the utilization behavior of older adults, which fully demonstrates the particular importance of doing well in promoting home hospice care. The qualitative study results supplement that older adults learn about home hospice care through doctors or families, with the role of doctors’ notification being more prominent, which is consistent with the research results of Lane et al. (41). Therefore, in the background of the cultural of taboos around death, promoting hospice care through doctors or families might be more significantly effective. In addition, the level of knowledge about home hospice care services (score status) also positively affects utilization behavior. The integrated results indicated that, in terms of knowledge about home hospice care, the subjective factors for older adults to utilize it were mainly recognizing that it can improve the quality of life and save medical resources. This finding reflects the terminally ill older adults’ pursuit of quality of life and less economic burden. However, old adults in the UK and the US are more aware of hospice care at home than in China, as they have raised public awareness of hospice care through extensive publicity and education (42). Therefore, to improve the acceptance of the service, enhance the awareness of home-based palliative care among the old adults and their families through community education, emphasize its advantages and economy would be advice in the future.
7.2 Enabling factors associated with the utilization of home hospice care by the older adults
First, who do not require caregivers is the enabling factor for older adults to use home-based hospice services, which is slightly different from the results in western countries where family caregivers are more willing to choose home-based services (43). The reason might be that the supply is insufficient in China, and most of the pressure of daily care is still borne by family caregivers, which is a huge caring burden when terminally ill older adults stay at home (44). Generally, the terminally older are also concerned about the quality and safety of care services (45). Therefore, it is necessary to strengthen the training of nursing staff, enrich nursing human resources, such as collaborative training between medical institutions and society, and increase efforts to train medical caregivers and older adult caregivers. In fact, the decision-making of families and the dying older is a complex issue that might be emotionally contradictory (46). Qualitative research shows that when families feel guilty due to lack of care, they tend to choose hospitalization with the intention of making up for the sense of guilt, as they might think that choosing hospice care is equivalent to giving up treatment (47). Therefore, it is also necessary to improve the understanding of relatives on death and hospice care. In the future, various forms of community education activities should be carried out, such as lectures, workshops, and brochures, to improve the awareness of the population. Third, a huge economic burden is an incentive, and evidence also shows that hospice services can reduce the cost of treatment (48). It is worth noting that assessing the specific income does not accurately predict the motivation for utilization. In the future, the subjective economic burden and objective income of the older and their families should be assessed at the same time. It is necessary to learn from some developed countries, such as South Korea and the UK, which provide financial support for the health services of hospice care and clarify the medical insurance reimbursement system (49). Additionally, home-based hospice care resources are an important motivational factor. In qualitative studies, older adults have indicated that the long distance between service locations and the lack of widespread resources are reasons they consider not to use home-based services. Terminally ill patients face a multitude of painful symptoms (50), especially those in the late stages of cancer. When resources to alleviate pain are not readily available, they might choose to be hospitalized. Therefore, attention should be paid to perfecting the rational allocation of distance and resources for home-based services by centering on community health services, with the main guidance from hospitals and auxiliary services from volunteers.
7.3 Demand factors associated with the utilization of home hospice care by the older adults
Interestingly, quantitative research has found that the higher the physiological and psychological needs, the less inclined they were to utilize home-based services. Qualitative research indicated that older adults did not have many needs for home-based services, which are urgent for pain relief. Home-based services are limited in China, with visits ranging from one time a month to one time a week, which hinders their ability to provide timely pain relief and a sense of security when symptoms arise (51). Therefore, home-based services are a good option when the demand is not high for older adults. Next, qualitative research findings further indicate that even within the context of limited services, family members’ psychological support is a facilitating factor for utilization. In the future, a comprehensive assessment of the varying degrees of needs of older adults, such as the most urgent, urgent, and general, should be conducted to first meet the most pressing needs and guide families in psychological nursing skills, making resource allocation more rational and service development feasible. However, when there is a high level of social needs, the likelihood of older adults utilizing them increases, and they also express a need for community interaction. Contrary to social demands, they have indicated that the negative attitudes of neighbors toward the end of life can hinder utilization behavior. Studies have shown (52) that disease stigma can lead to a sense of shame and social alienation in older adults. Participating in community activities and receiving support from the community can increase the happiness of older adults and reduce their feelings of loneliness. It also indicates that community support involving medical personnel can extend the time that older adult individuals spend at home. Therefore, it is possible to provide support for home-based older adult care through community death education and the establishment of informal organizations that include medical staff.
8 Limitations
The following are the limitations of our study. The older adults who utilized home hospice care in this study were mostly patients in the late stages of cancer, and the results may not be as representative of other terminally ill older adult individuals. Second, the study was conducted in a less economically developed province in western China, and the economic factors may differ from other regions. Therefore, future studies could expand the range of diseases and regions under investigation, employing stratified sampling based on disease types and regional economies to make the study results more representative. Third, this study is a cross-sectional survey and cannot reflect the psychological factors at different stages of terminally ill patients. Future longitudinal studies could explore the utilization trends and associated factors of home hospice care. Fourth, due to the need for patients to recall and the influence of patients’ social expectations, there is a certain recall bias and social expectation bias in the study. Finally, this cross-sectional study cannot establish a causal relationship.
9 Conclusion
In comparison with South Korea and China, the utilization rate in this study is only 13.55%, which fully demonstrates the gap between intention and acceptance. This further illustrates the significant importance of understanding the influencing factors. The factors influencing the utilization of home hospice care services by older adults are complex. The utilization of home-based services is influenced by both objective conditions and subjective intentions. Our study, guided by Andersen’s Health Services Utilization Model, employs mixed methods to explore the potential factors in the decision-making of terminally ill older individuals regarding home-based hospice care. Ultimately, the positive enabling factors for utilization by older adults are identified as advanced age, chronic illness, and good knowledge of it. The main positive enabling factors are caregivers being nursing staff, a significant perceived economic burden, and accessible care resources, while the negative factor is the emotional involvement of families. Positive needs factors include social needs, and negative ones include physical and psychological needs. These results provide a comprehensive framework for understanding the facilitators and barriers to the utilization of home-based hospice care services by terminally ill older adults. In the future, intervention strategies to increase the utilization rate of home-based hospice care for older adults can be formulated based on these associated factors.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: the materials in this article are from the author’s original research, and further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Second Affiliated Hospital of Guangxi Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JP: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation. XF: Formal analysis, Investigation, Writing – review & editing. XC: Data curation, Investigation, Writing – review & editing. LL: Investigation, Validation, Writing – review & editing. PD: Formal analysis, Investigation, Writing – review & editing. HW: Data curation, Visualization, Writing – review & editing. YC: Investigation, Supervision, Writing – review & editing. PH: Investigation, Validation, Writing – review & editing. DH: Investigation, Writing – review & editing. CL: Investigation, Writing – review & editing. YP: Investigation, Writing – review & editing. DF: Investigation, Project administration, Writing – review & editing. QP: Investigation, Methodology, Writing – review & editing. SL: Investigation, Project administration, Writing – review & editing. XP: Investigation, Resources, Writing – review & editing. LZ: Funding acquisition, Writing – review & editing. PT: Supervision, Validation, Writing – review & editing. HH: Funding acquisition, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by the research topic “Current Status and Solutions for the Utilization of Home-Based Hospice Care Services for the older adults in Guangxi from the Perspective of Healthy Aging” (22FRK004) and “China Life Care Association Humanistic Nursing Professional Committee Humanistic Nursing Research Projects” (RW2024ZD02).
Acknowledgments
The authors are very grateful to older adults individuals and their families who participated in this study, as well as the community and hospice workers who assisted us in organizing the survey with older adults.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1519712/full#supplementary-material
References
1. Chen, X, Giles, J, Yao, Y, Yip, W, Meng, Q, Berkman, L, et al. The path to healthy ageing in China: a Peking University-lancet commission. Lancet (London, England). (2022) 400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X
2. Moqri, M, and Snyder, M. Organ-specific aging and the risk of chronic diseases. Nat Med. (2023) 29:1068–9. doi: 10.1038/s41591-023-02338-z
3. Li, Z, Zhang, Z, Ren, Y, Wang, Y, Fang, J, Yue, H, et al. Aging and age-related diseases: from mechanisms to therapeutic strategies. Biogerontology. (2021) 22:165–87. doi: 10.1007/s10522-021-09910-5
4. Song, L, and Su, C. Research status and policy response on the quality of death for the elderly in China. Beijinciences. (2021) 6:119–28.
5. Tan, R. Analysis of the dental health status and changes among the elderly population in China—based on the sixth and seventh national population census data. Health Econ Res. (2023) 40:6–11.
6. WHO. Palliative care. p. Los cuidados paliativos constituyen un planteamiento que mejora la calidad de vida de los pacientes (adultos y niños) y sus allegados cuando afrontan problemas inherentes a una enfermedad potencialmente mortal; (2020)
7. Li, Z, Ding, Z, and Zhao, P. Comparison of functional disabilities, place of death and end-of-life medical expenditures among centenarians and non-centenarians in China: a series of cross-sectional studies. BMC Geriatr. (2023) 23:402. doi: 10.1186/s12877-023-04111-w
8. Li, Z, Hung, P, Shi, K, Fu, Y, and Qian, D. Association of rurality, type of primary caregiver and place of death with end-of-life medical expenditures among the oldest-old population in China. Int J Equity Health. (2023) 22:1. doi: 10.1186/s12939-022-01813-2
9. Wang, L, Li, Y, Zhao, R, Li, J, Gong, X, Li, H, et al. Influencing factors of home hospice care needs of the older adults with chronic diseases at the end of life in China: a cross-sectional study. Front Public Health. (2024) 12:1348214. doi: 10.3389/fpubh.2024.1348214
10. Wu, C, Ma, K, Liang, Y, Chung, W, and Wang, J. Exploring the effects of acceptable palliative care models on survival time and healthcare expenditure among patients with cancer: a national longitudinal population-based study. Suppor Care Cancer. (2024) 32:116. doi: 10.1007/s00520-023-08297-y
11. Wang, L, Li, Y, Zhao, R, Li, J, Gong, X, and Li, H. Development and validation of the home hospice care needs questionnaire for the dying old adult (HHCNQ-DE) in mainland China. Am J Hosp Palliat Care. (2024) 41:1391–9. doi: 10.1177/10499091231223486
12. Yin, Z, Li, J, Ma, K, Ning, X, Chen, H, Fu, H, et al. Development of palliative care in China: a tale of three cities. Oncologist. (2017) 22:1362–7. doi: 10.1634/theoncologist.2017-0128
13. Shim, HY, Park, JH, Kang, GH, and Kim, MJ. Adults above 65 years of intention to use homecare hospice and a study on the factors influencing the perception of hospice·palliative care service. Appl Nurs Res. (2023) 71:151684. doi: 10.1016/j.apnr.2023.151684
14. Yang, L, Zhou, Q, Hong, T, Zhang, L, and Che, H. Analysis on the willingness and influencing factors of choosing hospice care service institutions among among older people in Wuhu, China: a cross-sectional study. BMJ Open. (2024) 14:e83400. doi: 10.1136/bmjopen-2023-083400
15. Yao, N, Chen, H, and Lai, X. Hospice preference of the family decision-makers for cancer patients in China: an exploratory study. BMC Palliat Care. (2022) 21:222. doi: 10.1186/s12904-022-01112-1
16. Yang, M, and Zhuo, H. Development status and insights of palliative care in Taiwan. Med Philos. (2024) 45:50–4.
17. Tramontano, AC, Nipp, R, Kong, CY, Yerramilli, D, Gainor, JF, and Hur, C. Hospice use and end-of-life care among older patients with esophageal cancer. Health Sci Rep-US. (2018) 1:e76
18. Kumar, P, Casarett, D, Corcoran, A, Desai, K, Li, Q, Chen, J, et al. Utilization of supportive and palliative care services among oncology outpatients at one academic cancer center: determinants of use and barriers to access. J Palliat Med. (2012) 15:923–30. doi: 10.1089/jpm.2011.0217
19. Htut, Y, Shahrul, K, and Poi, PJH. The views of older Malaysians on advanced directive and advanced care planning: a qualitative study. Asia Pac J Public Health. (2007) 19:58–67. doi: 10.1177/101053950701900310
20. Lackan, NA, Ostir, GV, Freeman, JL, Mahnken, JD, and Goodwin, JS. Decreasing variation in the use of hospice among older adults with breast, colorectal, lung, and prostate cancer. Med Care. (2004) 42:116–22. doi: 10.1097/01.mlr.0000108765.86294.1b
21. Yoo, SH, Lee, J, Kang, JH, Maeng, CH, Kim, YJ, Song, E, et al. Association of illness understanding with advance care planning and end-of-life care preferences for advanced cancer patients and their family members. Support Care Cancer. (2020) 28:2959–67. doi: 10.1007/s00520-019-05174-5
22. Lim, MK, Lai, PSM, Lim, PS, Wong, PS, Othman, S, and Mydin, FHM. Knowledge, attitude and practice of community-dwelling adults regarding advance care planning in Malaysia: a cross-sectional study. BMJ Open. (2022) 12:e48314. doi: 10.1136/bmjopen-2020-048314
23. Babitsch, B, Gohl, D, and von Lengerke, T. Re-revisiting Andersen's behavioral model of health services use: a systematic review of studies from 1998–2011. Psychosoc Med. (2012) 9:Doc11. doi: 10.3205/psm000089
24. Lemming, MR, and Calsyn, RJ. Utility of the behavioral model in predicting service utilization by individuals suffering from severe mental illness and homelessness. Community Ment Health J. (2004) 40:347–64. doi: 10.1023/b:comh.0000035229.20557.5c
25. Piano, JWCV. Designing and conducting mixed methods research. Aust NZ J Publ Health. (2007) 31:388.
26. O'Cathain, A, Murphy, E, and Nicholl, J. The quality of mixed methods studies in health services research. J Health Serv Res Policy. (2008) 13:92–8. doi: 10.1258/jhsrp.2007.007074
27. Kim, S, Wand, J, Magana-Ramirez, C, and Fraij, J. Logistic regression models with unspecified low dose-response relationships and experimental designs for Hormesis studies. Risk Anal. (2021) 41:92–109. doi: 10.1111/risa.13588
28. Saunders, B, Sim, J, Kingstone, T, Baker, S, Waterfield, J, Bartlam, B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. (2018) 52:1893–907. doi: 10.1007/s11135-017-0574-8
29. Mahoney, FI, and Barthel, DW. Functional evaluation: the Barthel index. MD State Med J. (1965) 14:61–5.
30. Kondrup, J, Allison, SP, Elia, M, Vellas, B, and Plauth, M. ESPEN guidelines for nutrition screening 2002. Clin Nutr (Edinb). (2003) 22:415–21. doi: 10.1016/s0261-5614(03)00098-0
31. National Health and Family Planning Commission of the People's Republic of China. (2017). Notice on the issuance of the guidelines for palliative care practice (for trial implementation). Bulletin of the National Health and Family Planning Commission of the People's Republic of China, 2017(2).
32. Michie, S, van Stralen, MM, and West, R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
33. Lalani, N, and Cai, Y. Palliative care for rural growth and wellbeing: identifying perceived barriers and facilitators in access to palliative care in rural Indiana, USA. BMC Palliat Care. (2022) 21:25. doi: 10.1186/s12904-022-00913-8
34. Younas, A, Pedersen, M, and Durante, A. Characteristics of joint displays illustrating data integration in mixed-methods nursing studies. J Adv Nurs. (2020) 76:676–86. doi: 10.1111/jan.14264
35. Podsakoff, PM, MacKenzie, SB, Lee, J, and Podsakoff, NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
36. Regier, NG, Cotter, VT, Hansen, BR, Taylor, JL, and Wright, RJ. Place of death for persons with and without cognitive impairment in the United States. J Am Geriatr Soc. (2021) 69:924–31. doi: 10.1111/jgs.16979
37. Lei, L, Zhao, H, Ran, L, Wang, L, and Luo, Y. Influencing factors of attitudes towards death and demands for death education among community-dwelling Chinese older adults: a cross-sectional study. BMC Public Health. (2022) 22:1242. doi: 10.1186/s12889-022-13655-2
38. Smith, S, Brick, A, O'Hara, S, and Normand, C. Evidence on the cost and cost-effectiveness of palliative care: a literature review. Palliat Med. (2014) 28:130–50. doi: 10.1177/0269216313493466
39. Yang, Z, Hou, B, Chen, P, and Zhang, H. Preference and influencing factors of advance care planning for Chinese elderly patients with chronic diseases: a mixed-methods approach. J Hosp Palliat Nurs. (2021) 23:178–86. doi: 10.1097/NJH.0000000000000734
40. Lu, B, Zhang, R, and Chao, J. Health status and associated factors among the community-dwelling elderly women in China. Arch Gerontol Geriatr. (2018) 79:78–82. doi: 10.1016/j.archger.2018.08.005
41. Lane, T, Brereton, E, Nowels, C, McKeehan, J, Moss, M, and Matlock, DD. Surrogate informed consent: a qualitative analysis of surrogate decision makers' perspectives. Ann Am Thorac Soc. (2021) 18:1185–90. doi: 10.1513/AnnalsATS.202007-851OC
42. Zhou, W, Zhang, X, and Lyu, X. Monitoring utilisation patterns of home- and community-based services for healthy ageing: a cross-sectional study. BMC Geriatr. (2025) 25:291. doi: 10.1186/s12877-025-05918-5
43. Nysæter, TM, Olsson, C, Sandsdalen, T, Wilde-Larsson, B, Hov, R, and Larsson, M. Preferences for home care to enable home death among adult patients with cancer in late palliative phase – a grounded theory study. BMC Palliat Care. (2022) 21:49. doi: 10.1186/s12904-022-00939-y
44. Mertens, F, Vanderstichelen, S, Deveugele, M, Deliens, L, and Pype, P. Family carers' experiences regarding patient transfers between care settings in palliative care: an interview study. Ann Palliat Med. (2023) 12:767–82. doi: 10.21037/apm-23-20
45. Li, LZ, Yang, P, Singer, SJ, Pfeffer, J, Mathur, MB, and Shanafelt, T. Nurse burnout and patient safety, satisfaction, and quality of care: a systematic review and Meta-analysis. JAMA Netw Open. (2024) 7:e2443059. doi: 10.1001/jamanetworkopen.2024.43059
46. Mulcahy Symmons, S, Ryan, K, Aoun, SM, Selman, LE, Davies, AN, Cornally, N, et al. Decision-making in palliative care: patient and family caregiver concordance and discordance-systematic review and narrative synthesis. BMJ Support Palliat Care. (2023) 13:374–85. doi: 10.1136/bmjspcare-2022-003525
47. Flieger, SP, Chui, K, and Koch-Weser, S. Lack of awareness and common misconceptions about palliative care among adults: insights from a National Survey. J Gen Intern Med. (2020) 35:2059–64. doi: 10.1007/s11606-020-05730-4
48. Luta, X, Ottino, B, Hall, P, Bowden, J, Wee, B, Droney, J, et al. Evidence on the economic value of end-of-life and palliative care interventions: a narrative review of reviews. BMC Palliat Care. (2021) 20:89. doi: 10.1186/s12904-021-00782-7
49. Kim, K, Park, B, Gu, B, Nam, EJ, Kye, SH, and Choi, JY. The National Hospice and palliative care registry in Korea. Epidemiol Health. (2022) 44:e2022079. doi: 10.4178/epih.e2022079
50. Verkissen, MN, Hjermstad, MJ, Van Belle, S, Kaasa, S, Deliens, L, and Pardon, K. Quality of life and symptom intensity over time in people with cancer receiving palliative care: results from the international European palliative care cancer symptom study. PLoS One. (2019) 14:e222988. doi: 10.1371/journal.pone.0222988
51. Chen, S, Lai, X, Chen, L, and Xia, H. A general review of home palliative care services. Nurs Res. (2021) 35:3048–55.
Keywords: home hospice care, associated factors, Andersen model, terminally ill, older adults
Citation: Peng J, Feng X, Cao X, Lai L, Dong P, Wu H, Chai Y, Huang P, Hai D, Li C, Pan Y, Fan D, Pan Q, Lu S, Pan X, Zhang L, Tao P and Huang H (2025) Associated factors of home hospice care utilization by the terminally ill older adults: a mixed-methods study. Front. Public Health. 13:1519712. doi: 10.3389/fpubh.2025.1519712
Edited by:
Roger O’Sullivan, Institute of Public Health, IrelandReviewed by:
Lambert Zixin Li, National University of Singapore, SingaporeQian Huang, East Tennessee State University, United States
Erin Mauck, East Tennessee State University, United States
Copyright © 2025 Peng, Feng, Cao, Lai, Dong, Wu, Chai, Huang, Hai, Li, Pan, Fan, Pan, Lu, Pan, Zhang, Tao and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: HuiQiao Huang, aGhxQHNyLmd4bXUuZWR1LmNu
 Jie Peng
Jie Peng Xiaoling Feng
Xiaoling Feng Xiaoying Cao
Xiaoying Cao Lichong Lai
Lichong Lai Caili Li
Caili Li Pinyue Tao
Pinyue Tao