- 1Mental Health and Wellbeing Research Group, Vrije Universiteit Brussel, Laarbeeklaan, Belgium
- 2Department of Public Health, Vrije Universiteit Brussel, Laarbeeklaan, Belgium
- 3Kenniscentrum Kinderrechten, Ghent, Belgium
- 4Awel, Schaarbeek, Belgium
Few studies have investigated whether children, adolescents, and young adults (aged 10–25 years) had access to professional mental health aid when they desired it during the coronavirus disease 2019 (COVID-19) pandemic. An online survey was conducted in Flanders, Belgium, to examine professional mental health aid access (PMHAA). In total, 982 respondents were included, of whom the majority were between 13 and 15 years old (44.8%) and female (81.4%). Of these, 64.8% felt a need for PMHAA. Of those wanting PMHAA, only 29.6% had an appointment with a mental health professional. Those who did not have PMHAA mostly did not do so because of fear of stigma (54%), not knowing where to search for professional mental health aid (38.2%), and finding the aid to be too expensive (12.9%). This study’s findings indicate a large unmet need for professional mental health aid during the COVID-19 pandemic among people aged between 10 and 25 years old. There is a need for a campaign to reduce mental health stigma in this population.
1 Introduction
During the COVID-19 pandemic, several government measures were taken to stop the spread of the virus. In many countries, social distancing was introduced, and work shifted from physical locations to online settings. Young people had to attend their classes online, as schools were closed. Although the mortality caused by the virus decreased over time, the COVID-19 measures also seemingly had other consequences. Studies have demonstrated that children, adolescents, and young adults experienced more issues with their wellbeing and mental health than before the start of the pandemic (1–6). This encompassed, among other things, an increase in depressive, stress, or anxiety symptoms compared to before COVID-19 (1–3, 7). Furthermore, studies have indicated that the likelihood of child abuse and maltreatment increased during the pandemic (8–11). Regarding suicidal ideation and behavior, studies provide conflicting evidence: some find higher rates of suicide and suicidal ideation among children, adolescents, and young adults, while others report the opposite (12, 13).
Consequently, there was an increased need for professional mental health aid access (PMHAA). However, due to COVID-19 restrictions, there were fewer possibilities to obtain such access (14–17). This was, as was the case in schools, professional mental health aid was limited as much as possible in physical form. The provision of professional mental health aid often shifted to virtual settings, which likely hindered some individuals from PMHAA (e.g., due to a lack of internet access) (18–20). Therefore, unsurprisingly, several studies have demonstrated unmet health needs among children, adolescents, and young adults during COVID-19 (21–24).
In the context of Flanders, it remains somewhat unclear whether there were unmet mental health aid needs or not, and if so, what the magnitude of this problem is. One study indicated that adolescents and young adults in Belgium generally had less access to services (21). However, the minimum age in that study was 15 years old and thus did not provide information for those younger than 15. Furthermore, the reasons for the lack of mental health access often remained unclear and understudied. Studies on PMHAA remain important to find out how mental health literacy and knowledge can be improved among young adults, as this remains a sorely understudied topic (25).
This study investigates access to professional mental health aid (PMHHA) specifically among children, adolescents, and young adults (between 10 and 25 years old) during the COVID-19 pandemic in Flanders. There is a strong need for such studies because this is a vulnerable group that is at risk of developing mental health issues (7).
2 Method
2.1 Population and design
In 2021, the population in Flanders that was between 10 and 25 years old was 1,084,135 (26). Approximately 16.3% had some form of mental health disorder (27). An online cross-sectional survey was developed in cooperation with Awel (a youth help line in Flanders) and Kenniscentrum Kinderrechten (in English: “Children’s Rights Knowledge Centre”), an organization that strives to strengthen and acknowledge the position of children in society. Central to this approach is the respect for and guarantee of their rights. Data collection occurred from 2 February to 2 March 2021. During this period, COVID-19 measures were still strict, with meetings with other people only allowed up to 10 people and only outside, and physical education was still not allowed. Cookies were used in the online survey to prevent multiple answers from the same individual.
The survey was developed in several phases: First, questions were evaluated with employees of Awel and WAT WAT, together with a pilot group of several adolescents and children, to verify whether questions were understandable for children, adolescents, and young adults. Then, adjustments were made to questions according to their feedback, such as the reduction of the number of questionnaire items, removing as many Likert scales as possible, and adding multiple-choice questions. Afterward, a copywriter of Ambrassade, another website targeting youth, simplified questions that were too complex in formulation. All questions were only available in Dutch. This was done as the partners who agreed to spread the survey were all Flemish organizations, and thus only provided information to youth in Dutch.
The link to the survey was put on several websites of several organizations for the wellbeing of adolescents and young adults in Flanders, such as Awel, Kenniscentrum Kinderrechten, WAT WAT, and Ambrassade. Awel is a Flemish organization that aims at low-threshold online conversations with youth about any topic, ranging from school, friendship, to mental health issues. During 2021, when data collection occurred, Awel had 28,886 contacts with youth, which was 2% more than in 2020 (28). Kenniscentrum Kinderrechten, WAT WAT, and Ambrassade are websites where young adults can search for information about various themes/subjects, including rights, mental health issues, and sexuality. Kenniscentrum Kinderrechten does not have children and youth as its primary target group. They mainly focus on practice, policy, and research. People who work for, by, or about children and young people. Through their website, they reach these people and, in a secondary way, also children, young people, and young adults themselves.
2.2 Measures
The survey had a complex structure as there were many different pathways to answering it, as illustrated in Figure 1. Collected demographics were age, gender, and living situation. Age categories included 7–9, 10–12, 13–15, 16–17, 18–19, 20–25, and 25+. Living situation was categorized as “living with one parent at a time (e.g., parents are divorced),” “I live in the same house as my parents,” “I live in another family than with my parents (e.g., foster parents, grandparents,…),” “I live in a group (e.g., hospital, asylum centre…),” “I live alone (e.g., student home),” and “I live in another way (free text field).” Gender had options “boy,” “girl,” “other,” or “no answer.” Several questions were only answerable with “yes” or “no,” especially those concerning PMHAA: “Did you have the need to talk with a professional, such as a therapist, psychiatrists, or psychologist?,” “Did you have a talk with a professional?,” “Do you still feel the need for professional help?,” “Did you go to professional aid before COVID-19?,” and “Were you satisfied with the aid you received?”
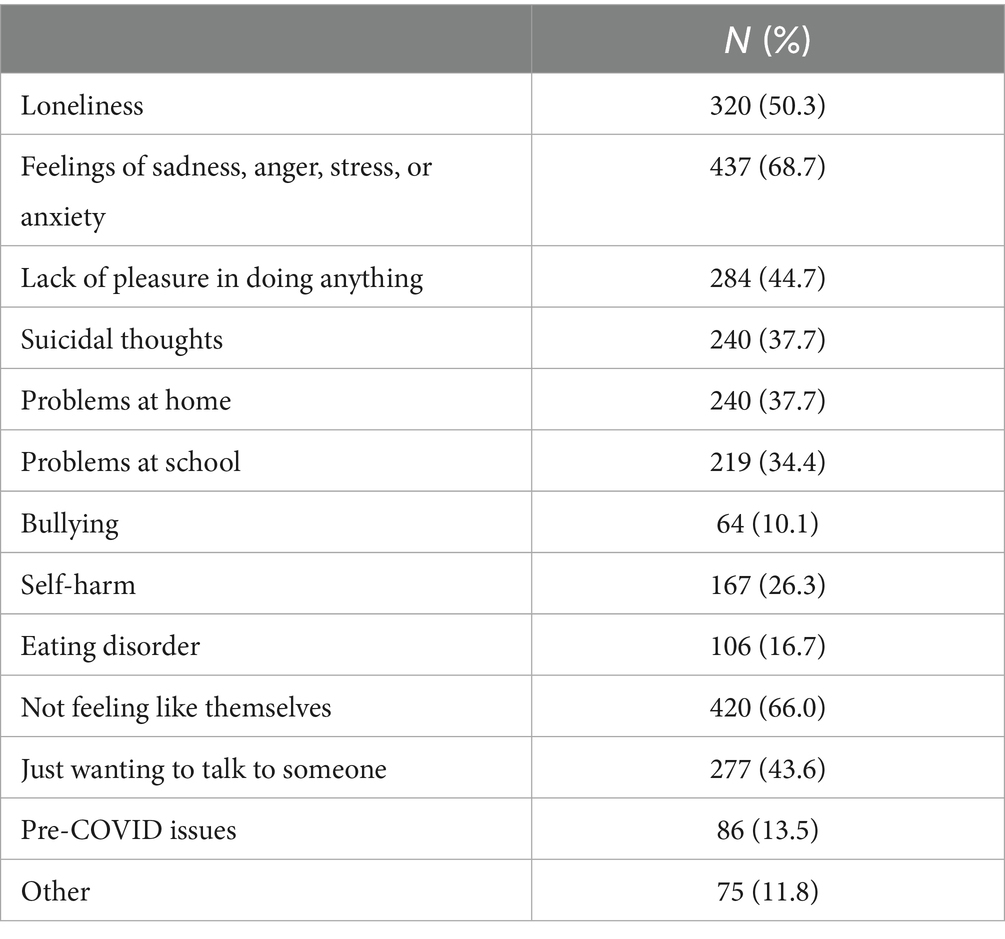
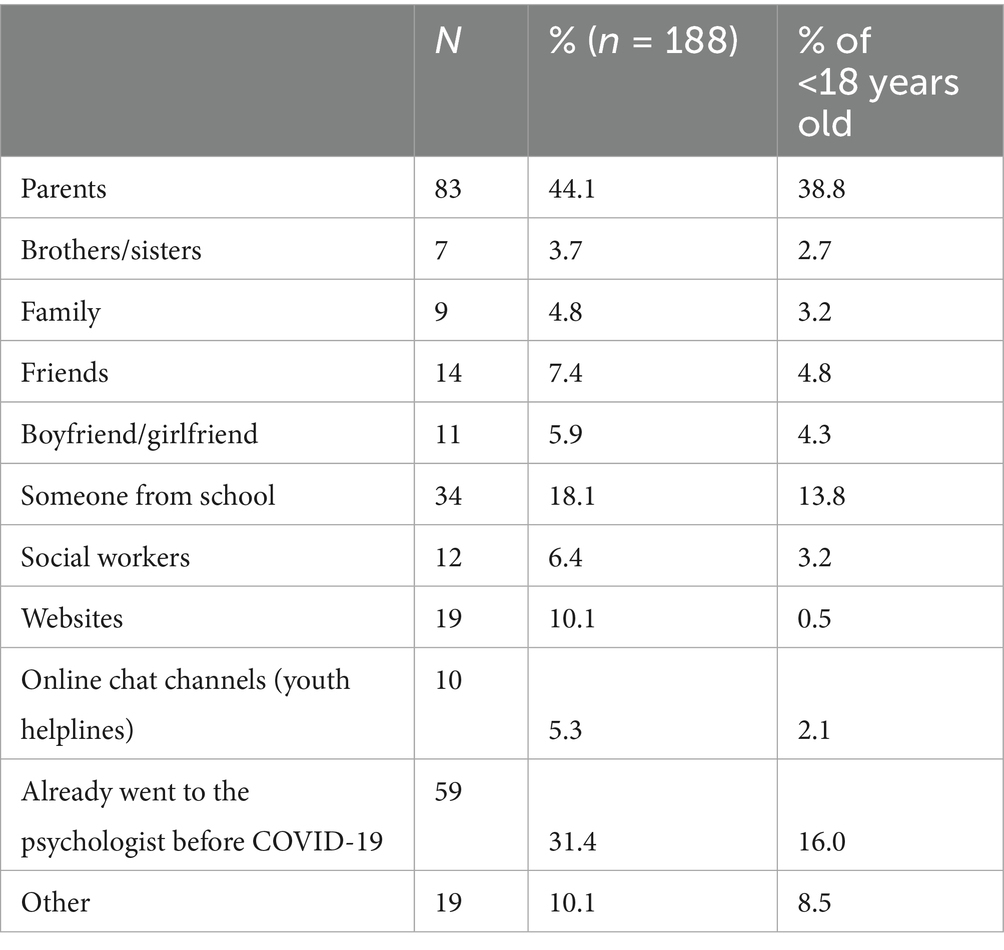
The following questions were multiple-choice questions, where multiple answers were possible. “Why did you want to talk with a professional?” was answerable with statements on emotional problems (“I felt lonely,” “I felt sad, angry, stressed, anxious,” “I had no pleasure anymore in doing things,” “I had suicidal thoughts,” and “I wasn’t feeling good about myself”), situational problems (“I had problems at home,” “I had problems at school,” and “I was being bullied”), and behavioral problems (“I was hurting myself (e.g., automutilation)” and “I had/have an eating disorder”). Other options were “I just wanted to talk with someone” and “Other,” which was an open-text field. “How did you find this professional?” was answerable with “Parents,” “Brothers/sisters,” “Family,” “Friends,” “Girl/boyfriend,” “Student counseling,” “Online,” “Youth helplines (e.g., Awel),” and “I went to professional aid before COVID.”
For those who did not need professional aid: “If you needed to find professional help, would you know where to find it?” was answerable with “I would not know where to find it,” “I would ask help to family/friends,” “I would ask help in school,” “I already know someone that provides professional aid,” “I would seek help online,” and “I would ask aid through online-aid (e.g., Awel, Tele-onthaal).” Tele-onthaal is an organization anyone can call or contact for any subject.
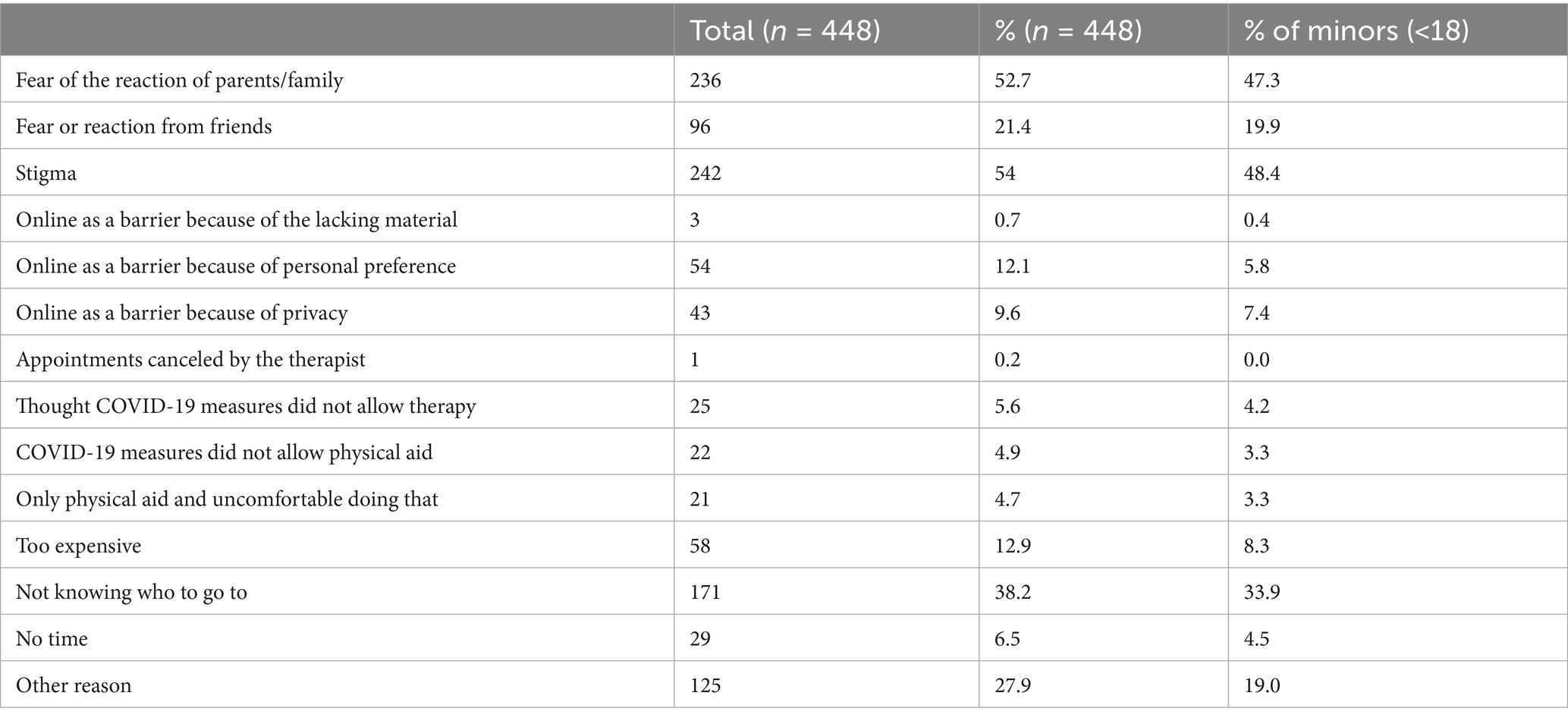
For those who did not talk to a professional: “Why did you not seek out help?” was answerable with “Fear of the reaction of parents/family,” “Fear of the reaction of friends,” “It was online and I do not have the necessary material to do that,” “It was only online and I did not want to do it like that,” “It was online and I did not have a place at home to do it privately,” “My therapist told me he/she could not do it,” “I thought it was not possible because of the COVID-measures,” “The measures did not allow me to go there physically,” “It was only possible physically, and I did not feel comfortable doing that,” “Too expensive,” “I did not know where to go,” “No time,” and “Other reason,” which was completable as a free-text field.
Perceived stigma was assessed by asking if respondents feared negative reactions from (a) parents/family or (b) friends; an affirmative response to either was counted as stigma.
“Who did you talk to about your problems?” was answerable with “My parents,” “My brother/sister,” “My friends,” “My classmates,” “A teacher,” “Student counseling,” “Youth helplines (e.g., Awel),” “No one,” and “Other,” which was a free-text field.
For those that received aid, but were not satisfied with it: “Why were you not satisfied?,” with answering options “It was only online and I do not like it online,” “It was only online and I had problems with getting on the internet,” “It was too expensive,” “I did not feel understood,” “It was a physical conversation and I did not feel comfortable with this,” “It was too short,” and “Other reason” (open text field).
One question was in the form of a Likert scale. “Was this talk online or offline?” was answerable with “Completely online,” “Mostly online, but sometimes physical,” “Partly online, partly physical,” “Mostly physical, but sometimes online,” and “Completely physical.”
2.3 Analysis
Those who were older than 25 years of age were excluded. Similarly, those who did not provide an answer to the question about age were removed. Finally, we excluded all those who did not complete the question about whether or not they needed aid. Descriptive statistics were calculated with Pearson’s chi-squared test when comparing groups. Open-text fields were summarized and reported descriptively.
2.4 Ethics
This study was approved by the ethics committee of the VUB/UZ Brussels (B.U.N. 1432021000442). Respondents first got an introduction screen explaining the aims of the study with the assurance that any response given would be processed and presented anonymously. At the end of the survey, respondents received information on how to contact Awel or WAT WAT if they were in need of information or help.
3 Results
3.1 Demographics
In total, 1,079 people completed the survey. After excluding those of unknown age and without information on the need for professional aid, respectively, 982 respondents remained. As can be seen in Table 1, the large majority of respondents were female (81.4%). The majority were between 10 and 15 years old (66.7%). The largest age category was between 13 and 15 years old (44.8%).
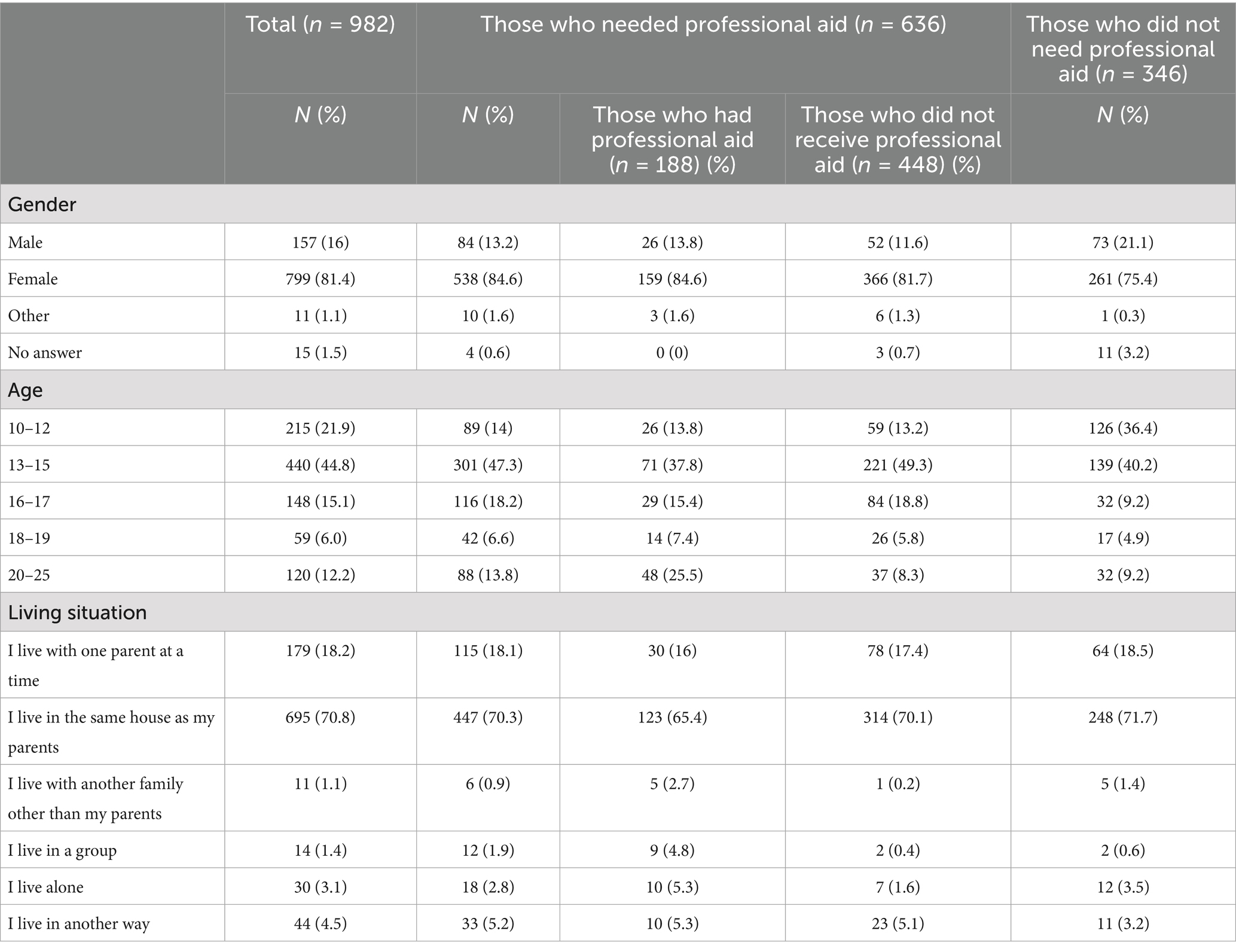
Table 1. Characteristics of children and adolescents responding to the online survey of mental health needs and access during COVID-19.
3.2 Needing professional aid
Among the respondents, 636 (64.8%) reported that they felt a need for PMHAA. Girls generally stated to experience a greater need than boys (84.4 and 13.2%) (p < 0.001). The majority of those between 13 and 25 reported needing aid, while this was only a minority among those between 10 and 12 (85.9 and 14%) (p < 0.001) (see Table 1). The main reasons for needing PMHAA were not feeling like themselves (66%), lack of pleasure in doing anything (44.7%); feelings of sadness, anger, stress, or anxiety (68.7%); and loneliness (50.3%). In total, 26.3% of respondents reported that they were hurting themselves, and 37.7% stated that they had suicidal thoughts. Issues at home (37.7%) appeared to be another frequently mentioned reason for needing PMHAA. Of 13.5% of those needing professional mental health aid, these issues were for which they were already in treatment before COVID-19 (see Table 2).
Of those reporting that they needed a conversation with a professional, 188 (29.6%) had an appointment, with 59 of them already going to a professional before the COVID-19 pandemic (31.4% of 188). Others found aid through student counseling (18.1%) or parents (44.1%) (see Table 3). For 48.9%, the aid they received was entirely in person, with only 12.8% having completed online sessions. The majority were satisfied with this approach, and only 25.5% indicated that they were dissatisfied. The reason for dissatisfaction was varied, with the most frequent answer being that the respondent did not feel understood (4.8%).
3.3 Needing, but not seeking professional aid
Of the 636 that needed PMHAA, the majority (n = 448; 70.4% of 636) reported not having an appointment. Children and adolescents (10–17 years) more often had no professional aid (74.3%) than young adults (18–25 years) (50.4%) (see Table 1). The most frequently mentioned reasons for not having an appointment were fear of negative reactions from parents and family (52.7%) and not knowing where to search for professional aid (38.2%). Stigma was present among 54% respondents, with most of these being females (46.7% of 448 respondents). It was present mostly among minors (48.4%), and those between 13 and 15 years old (30.6%) experienced stigma more than other age groups. (see Table 4). Other reasons included that it was too expensive (12.9%), 5.6% thought it was not possible due to the COVID-19 measures, and 4.9% did not go because of the COVID-19 measures. However, 12.1% indicated that they did not seek out psychological aid because it was only possible through online media.
Those who completed the open text field (27.9%) indicated reasons such as not wanting to overburden their parents (3.1%), fear of making the appointment (3.4%), feeling their issues were not serious enough (1.1%), fear of being mocked by family (1.3%), and long waiting lists (0.9%). To cope with their issues, most talked to friends (33.4%), though a large proportion also did not talk to anyone (38.2%). Of those that needed a professional but eventually did not, 75.2% still needed to have a talk with a professional.
3.4 Not needing any professional aid
In total, 346 (35.2%) respondents had no need for PMHAA. We asked them who they would reach out to for help finding professional aid if needed. The majority of respondents indicated family or friends (37% of 346), though 29.2% also would seek help online.
4 Discussion
This study investigated the mental health needs of children, adolescents, and young adults during the COVID-19 pandemic. Our findings reveal a substantial prevalence of unmet professional mental health needs among the respondents. Those individuals who sought mental health assistance during the pandemic were mostly those who were already engaged in such services prior to the outbreak, and mostly older participants (+18) sought mental health assistance. Conversely, younger participants (below 18 years old) expressed a desire for professional mental health support but refrained from seeking help for various reasons. The most frequently cited factors were stigma (54%), lack of awareness about available professional aid (38.2%), and financial constraints (12.9%). While some respondents (12.1%) mentioned not needing aid when online psychological assistance was the only option, COVID-19 measures were rarely identified as a direct hindrance to seeking aid. Those who did not seek professional mental healthcare often did not talk to anyone about their mental health issues (38.2%).
This study’s findings align with research conducted in other countries during the COVID-19 pandemic. For instance, a survey encompassing young adults from Canada and France reported that 50.7% expressed a need for mental health services, although a majority did not access them (24). Stigma emerged as the primary barrier to access to professional mental health aid in our study. Despite Belgium having a fairly well-developed mental health system, stigma predominantly hindered minors from reaching out to the system (25, 29, 30). This suggests that the challenges surrounding mental healthcare and youth persistently existed both before and after the onset of COVID-19. However, the pandemic potentially exacerbated the issue by introducing online therapy, which some respondents found problematic. Encouragingly, those who predominantly received mental healthcare online reported comparable levels of satisfaction with the therapy as those who exclusively received in-person therapy.
Among those younger than 18 years old, there is a markedly lower reported need for mental health aid among 10–12-year-olds. This could indicate genuinely lower incidence of psychosocial distress in pre-adolescents, but might also reflect under-recognition of mental health needs in this age group. Thus, this might indicate a need for more mental health literacy. However, it is difficult to make broad conclusions about this finding due to lower survey engagement by younger children.
This study revealed that individuals aged 18 and older, along with those who had established prior contact with therapists, were more successful in seeking out mental health aid. This pattern mirrors findings in studies on adults, indicating that those with pre-existing engagement with mental health experts were better positioned to access professional services during the pandemic compared to individuals who developed mental health concerns amid the COVID-19 crisis (20, 31). This is not surprising, as studies have shown the strong link between the need for professional mental health and the actual seeking of mental health aid, when possible (32).
Another noteworthy challenge identified was respondents’ lack of awareness regarding where to seek mental health aid. This confusion may partly arise from Belgium’s intricate mental health system (33). To address this issue, it might be beneficial to introduce educational modules in schools to inform youth about where to find and how to access professional mental health aid. Nevertheless, the implementation of such initiatives remains unclear due to the scarcity of robust longitudinal studies (25). Despite improving familiarity with the mental health system, financial concerns persist as a substantial barrier, as evident in other studies (34). It is all the more surprising, however, since in general therapy sessions in Belgium are free for the first session (33). It shows that taking away financial barriers is not enough to increase access to mental health aid.
The study’s limitations include its cross-sectional design, precluding causal inferences or follow-up investigations. Moreover, the convenience sampling method used for the online survey hampers its representativeness. For example, girls are overrepresented in the sample. The manner of data collection, using sites that are aimed at helping youth with various problems and questions, may also indicate a bias toward respondents who already wanted aid. Additionally, Belgium, and Flanders in particular, generally have a quite high burden of mental health disorders, making the results in this study probably not directly comparable with other countries (35). Finally, the questionnaire’s simplicity restricted in-depth exploration. Related to that, the concept of “stigma” as operationalized in this study does not fully capture the full complexity of stigma. Nevertheless, the strengths of this study lie in its status as one of the few to assess youth’s access to professional mental health aid during COVID-19, particularly with a substantial sample size and a wide age range.
Future studies should assess further the access of youth to professional mental health aid. Clearly, this is an issue that will not go away with time, as it was already noticed before COVID-19 and during COVID-19. In addition, studies should also look at how youth helplines may aid in addressing the issues that youth encounter. It may be that youth helplines are more low-threshold and thus easier to access for youth, while having the same effect. However, to our knowledge, no such studies exist that have evaluated whether youth helplines can aid in this. Either way, it is clear that solutions have to be sought out to address this clear problem.
5 Conclusion
In summary, our study underscores the difficulties faced by individuals aged 10 to 25 in accessing professional mental health support, with the underlying barriers being largely consistent with factors predating the COVID-19 pandemic. We propose public health campaigns aimed at enhancing mental health literacy among youth, providing them with guidance on accessing professional mental health aid, and combating the stigma associated with mental health issues. Furthermore, addressing financial obstacles is crucial. While progress has been made in reducing mental healthcare costs in Belgium in recent years, further steps should be taken (33).
Finally, the large percentage of respondents who did not talk to anyone about their issues is rather surprising. Social support from friends and family remains one of the most important buffers against the development of mental health issues (36, 37). A campaign to reduce mental health stigma can increase the social support people receive, and thus would in fact reduce the number of people who have to seek professional mental health aid, and would lower the threshold of seeking professional mental health aid for those who need it.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by ethics committee of the VUB/UZ Brussels. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because online survey where anonimity was guaranteed.
Author contributions
EM: Writing – original draft, Writing – review & editing. LV: Writing – original draft, Writing – review & editing. HD: Writing – original draft, Writing – review & editing. SV: Writing – original draft, Writing – review & editing. KK: Writing – original draft, Writing – review & editing. SD: Writing – original draft, Writing – review & editing. JB: Writing – original draft, Writing – review & editing. RO: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We wish to thank all respondents and everyone who contributed to this survey, the group of adolescents who provided feedback, and the employees of Awel, Kenniscentrum Kinderrechten, WAT WAT, and Ambrassade who helped with the set-up, creation of the survey, and the spread of the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li, B, Ng, K, Tong, X, Zhou, X, Ye, J, and Yu, JJ. Physical activity and mental health in children and youth during COVID-19: a systematic review and meta-analysis. Child Adolesc Psychiatry Ment Health. (2023) 17:92. doi: 10.1186/s13034-023-00629-4
2. Leung, XY, Kavanagh, AM, Quang, QT, Shields, M, and Aitken, Z. A systematic review of the impact of the COVID-19 pandemic on the mental health of adolescents and young people with disabilities aged 15–29 years. BMC Public Health. (2023) 23:1390. doi: 10.1186/s12889-023-16260-z
3. Ludwig-Walz, H, Dannheim, I, Pfadenhauer, LM, Fegert, JM, and Bujard, M. Anxiety increased among children and adolescents during pandemic-related school closures in Europe: a systematic review and meta-analysis. Child Adolesc Psychiatry Ment Health. (2023) 17:74. doi: 10.1186/s13034-023-00612-z
4. Burdzovic, AJ, and Brunborg, GS. Self-reported mental and physical health among Norwegian adolescents before and during the COVID-19 pandemic. JAMA Netw Open. (2021) 4:e2121934. doi: 10.1001/jamanetworkopen.2021.21934
5. Mei, F, and Wang, Z. Trends in mental health: a review of the most influential research on depression in children and adolescents. Ann General Psychiatry. (2024) 23:36. doi: 10.1186/s12991-024-00520-2
6. Pettersen, JH, Hannigan, LJ, Gustavson, K, Lund, IO, Pearson, RM, Jensen, P, et al. COVID-19 pandemic quarantines and mental health among adolescents in Norway. JAMA Netw Open. (2024) 7:e2422189. doi: 10.1001/jamanetworkopen.2024.22189
7. Madigan, S, Racine, N, Vaillancourt, T, Korczak, DJ, Hewitt, JMA, Pador, P, et al. Changes in depression and anxiety among children and adolescents from before to during the COVID-19 pandemic. JAMA Pediatr. (2023) 177:567. doi: 10.1001/jamapediatrics.2023.0846
8. Sharma, S, Wong, D, Schomberg, J, Knudsen-Robbins, C, Gibbs, D, Berkowitz, C, et al. COVID-19: differences in sentinel injury and child abuse reporting during a pandemic. Child Abuse Negl. (2021) 116:104990. doi: 10.1016/j.chiabu.2021.104990
9. Lee, H, and Kim, E. Global prevalence of physical and psychological child abuse during COVID-19: a systematic review and meta-analysis. Child Abuse Negl. (2023) 135:105984. doi: 10.1016/j.chiabu.2022.105984
10. Vermeulen, S, Alink, LRA, and van Berkel, SR. Child maltreatment during school and childcare closure due to the COVID-19 pandemic. Child Maltreat. (2023) 28:13–23. doi: 10.1177/10775595211064885
11. Massiot, L, Launay, E, Fleury, J, Poullaouec, C, Lemesle, M, Guen, CG, et al. Impact of COVID-19 pandemic on child abuse and neglect: a cross-sectional study in a French child advocacy Center. Child Abuse Negl. (2022) 130:105443. doi: 10.1016/j.chiabu.2021.105443
12. Horita, N, and Moriguchi, S. COVID-19, young people, and suicidal behaviour. Lancet Psychiatry. (2023) 10:484–5. doi: 10.1016/S2215-0366(23)00159-1
13. ZHU, S, ZHUANG, Y, LEE, P, and WONG, PWC. The changes of suicidal ideation status among young people in Hong Kong during COVID-19: a longitudinal survey. J Affect Disord. (2021) 294:151–8. doi: 10.1016/j.jad.2021.07.042
14. Villarreal-Zegarra, D, Segovia-Bacilio, P, Paredes-Angeles, R, Vilela-Estrada, AL, Cavero, V, and Diez-Canseco, F. Provision of community mental health care before and during the COVID-19 pandemic: a time series analysis in Peru. Int J Soc Psychiatry. (2023) 69:5026. doi: 10.1177/00207640231185026
15. Duden, GS, Gersdorf, S, and Stengler, K. Global impact of the COVID-19 pandemic on mental health services: a systematic review. J Psychiatr Res. (2022) 154:354–77. doi: 10.1016/j.jpsychires.2022.08.013
16. Stepanova, E, Thompson, A, Yu, G, and Fu, Y. Changes in mental health services in response to the COVID-19 pandemic in high-income countries: a rapid review. BMC Psychiatry. (2024) 24:103. doi: 10.1186/s12888-024-05497-6
17. Vandamme, J, Beerten, SG, Crèvecoeur, J, Van den Bulck, S, Aertgeerts, B, Delvaux, N, et al. The impact of the COVID-19 pandemic on the registration and care provision of mental health problems in general practice: registry-based study. JMIR Public Health Surveill. (2023) 9:e43049. doi: 10.2196/43049
18. Chen, JA, Chung, W-J, Young, SK, Tuttle, MC, Collins, MB, Darghouth, SL, et al. COVID-19 and telepsychiatry: early outpatient experiences and implications for the future. Gen Hosp Psychiatry. (2020) 66:89–95. doi: 10.1016/j.genhosppsych.2020.07.002
19. Reay, RE, Looi, JC, and Keightley, P. Telehealth mental health services during COVID-19: summary of evidence and clinical practice. Australas Psychiatry. (2020) 28:514–6. doi: 10.1177/1039856220943032
20. Rojnic Kuzman, M, Vahip, S, Fiorillo, A, Beezhold, J, Pinto da Costa, M, Skugarevsky, O, et al. Mental health services during the first wave of the COVID-19 pandemic in Europe: results from the EPA ambassadors survey and implications for clinical practice. Eur Psychiatry. (2021) 64:e41. doi: 10.1192/j.eurpsy.2021.2215
21. Rens, E, Michielsen, J, Dom, G, Remmen, R, and Van den Broeck, K. Clinically assessed and perceived unmet mental health needs, health care use and barriers to care for mental health problems in a Belgian general population sample. BMC Psychiatry. (2022) 22:455. doi: 10.1186/s12888-022-04094-9
22. Gorfinkel, LR, Snell, G, Long, D, del Casal, M, Wu, J, Schonert-Reichl, K, et al. Access to mental health support, unmet need and preferences among adolescents during the first year of the COVID-19 pandemic. Health Promot Chronic Dis Prev Can. (2023) 43:182–90. doi: 10.24095/hpcdp.43.4.03
23. Adams, SH, Schaub, JP, Nagata, JM, Park, MJ, Brindis, CD, and Irwin, CE. Young adult anxiety or depressive symptoms and mental health service utilization during the COVID-19 pandemic. J Adolesc Health. (2022) 70:985–8. doi: 10.1016/j.jadohealth.2022.02.023
24. Coulaud, P, Jesson, J, Bolduc, N, Ferlatte, O, Jenkins, E, Bertrand, K, et al. Young adults’ mental health and unmet service needs in the context of the COVID-19 pandemic across Canada and France. Community Ment Health J. (2023) 59:222–32. doi: 10.1007/s10597-022-01000-1
25. Thornicroft, G, Mehta, N, Clement, S, Evans-Lacko, S, Doherty, M, Rose, D, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. (2016) 387:1123–32. doi: 10.1016/S0140-6736(15)00298-6
26. Statistiek Vlaanderen. (2025) Population by age and gender 2025. https://www.vlaanderen.be/en/statistics-flanders/population/population-by-age-and-gender (Accessed February 21, 2025).
27. For a Healthy Belgium. (2023). Adolescent mental health 2023. Available online at: https://www.healthybelgium.be/en/health-status/mental-health/adolescent-mental-health?utm_source=chatgpt.com (Accessed February 21, 2025).
28. VRT. (2021). Jongerenlijn “Awel” kreeg opnieuw 2 procent meer oproepen in 2021, corona niet de hoofdoorzaak van kopzorgen 2021. Available online at: https://www.vrt.be/vrtnws/nl/2022/02/04/corona-niet-de-hoofdoorzaak-voor-sombere-gedachten-bij-jongeren/ (Accessed February 21, 2025).
29. Nobre, J, Oliveira, AP, Monteiro, F, Sequeira, C, and Ferré-Grau, C. Promotion of mental health literacy in adolescents: a scoping review. Int J Environ Res Public Health. (2021) 18:9500. doi: 10.3390/ijerph18189500
30. Telesia, L, Kaushik, A, and Kyriakopoulos, M. The role of stigma in children and adolescents with mental health difficulties. Curr Opin Psychiatry. (2020) 33:571–6. doi: 10.1097/YCO.0000000000000644
31. Yu, E, Xu, B, and Sequeira, L. Determinants of e-mental health use during COVID-19: cross-sectional Canadian study. J Med Internet Res. (2022) 24:e39662. doi: 10.2196/39662
32. Codony, M, Alonso, J, Almansa, J, Bernert, S, de Girolamo, G, de Graaf, R, et al. Perceived need for mental health care and service use among adults in Western Europe: results of the ESEMeD project. Psychiatr Serv. (2009) 60:1051–8. doi: 10.1176/ps.2009.60.8.1051
34. Moroz, N, Moroz, I, and D’Angelo, MS. Mental health services in Canada: barriers and cost-effective solutions to increase access. Healthc Manage Forum. (2020) 33:282–7. doi: 10.1177/0840470420933911
35. Muysewinkel, E, Vesentini, L, Van Deynse, H, Gisle, L, Smith, P, Bruggeman, H, et al. Trauma exposure, social support and mental health in the general population in Belgium. Eur J Investig Health Psychol Educ. (2024) 14:2047–56. doi: 10.3390/ejihpe14070136
36. Meherali, S, Punjani, N, Louie-Poon, S, Abdul Rahim, K, Das, JK, Salam, RA, et al. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health. (2021) 18:3432. doi: 10.3390/ijerph18073432
Keywords: mental health services, mental health, COVID-19, youth, stigma
Citation: Muysewinkel E, Vesentini L, Van Deynse H, Vanclooster S, Kinderrechten K, Devarwaere S, Bilsen J and Van Overmeire R (2025) Professional mental health aid for children, adolescents, and young adults during COVID-19 in Flanders, Belgium. Front. Public Health. 13:1527141. doi: 10.3389/fpubh.2025.1527141
Edited by:
Cheng Ren, University at Albany, United StatesReviewed by:
Dana Vrajitoru, Indiana University South Bend, United StatesSoumya Basu, Monash University, Australia
Márton Bagyura, University of Pécs, Hungary
Emeka Duru, The University of Utah, United States
Copyright © 2025 Muysewinkel, Vesentini, Van Deynse, Vanclooster, Kinderrechten, Devarwaere, Bilsen and Van Overmeire. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Roel Van Overmeire, cm9lbC52YW4ub3Zlcm1laXJlQHZ1Yi5iZQ==
†These authors have contributed equally to this work
 Emilie Muysewinkel1,2
Emilie Muysewinkel1,2 Helena Van Deynse
Helena Van Deynse Stephanie Vanclooster
Stephanie Vanclooster Johan Bilsen
Johan Bilsen Roel Van Overmeire
Roel Van Overmeire