- 1Department of Health and Rehabilitation Sciences, Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia
- 2Department of Physical Therapy, Jazan University, Jazan, Saudi Arabia
Background: Frailty and depression are common conditions in older adults, but their coexistence and combined impact on physical activity and quality of life remain understudied, particularly in Saudi Arabia.
Objective: To examine the independent associations of depression, frailty, and their coexistence with physical activity levels and quality of life among Saudi older adults.
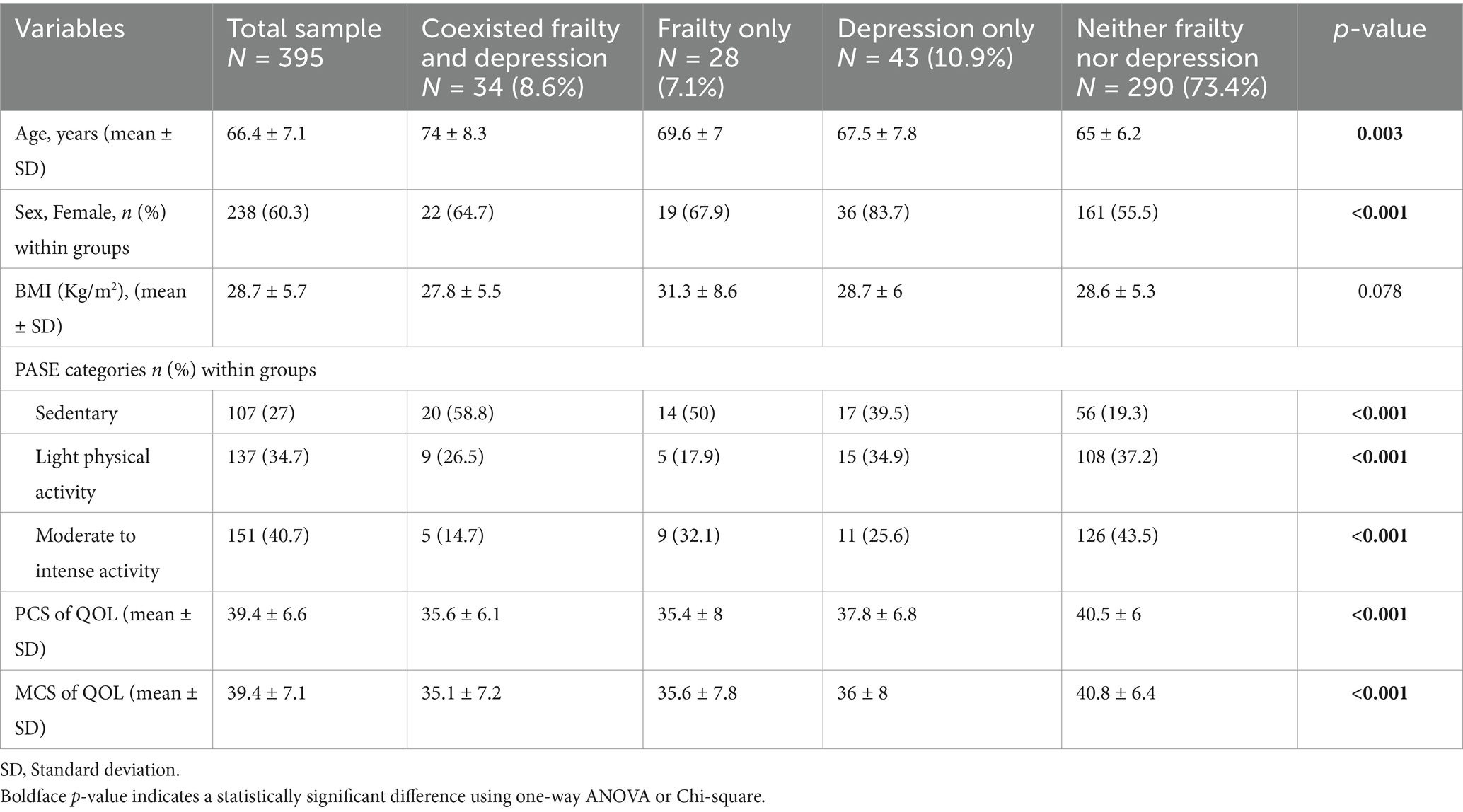
Methods: A cross-sectional study was conducted among 395 community-dwelling adults aged 60 years and older (mean age 66.4 ± 7.1 years, 60% women) in Saudi Arabia. Frailty was assessed using the FRAIL scale, depression using the Patient Health Questionnaire 9 (PHQ-9), physical activity using the Physical Activity Scale for the Elderly (PASE), and quality of life using the SF-12. Participants were categorized based on the results of FRAIL and PHQ-9 scale into four groups: coexisting frailty and depression, frailty only, depression only, or neither.
Results: The prevalence of coexisting frailty and depression was 8.6%. Participants with coexisting frailty and depression were more likely to be sedentary (OR = 4.37, 95% CI: 1.41–13.55, p = 0.011) compared to those without frailty or depression. Frailty only group (β = −3.55, p = 0.003) and coexisting frailty and depression (β = −2.55, p = 0.033) were significantly associated with lower physical quality of life. Depression, frailty, and their coexistence were all significantly associated with lower mental quality of life (p < 0.001 for all).
Conclusion: The coexistence of frailty and depression in older adults is associated with a higher likelihood of sedentary behavior and lower quality of life. These findings highlight the need for comprehensive geriatric assessments and targeted interventions addressing both physical and mental health in older adults.
Introduction
The aging population is rapidly growing worldwide. Approximately 703 million people were aged 65 years and older in 2019, and this figure is predicted to grow substantially to about 1.5 billion by 2050 (1). In Saudi Arabia, the older population is expected to rise from the 9.5% in 2035 to 18% of the entire population by the year 2050.
The aging process, a complex phenomenon involves psychological, biochemical, and functional changes that cause a decline in physiological and functional capacities, leading to frailty. Frailty is increasingly among older adults, with more than half of the older adult population in Saudi Arabia experiencing some degree of this condition (1). A recent cross-sectional study reported that 21.4% of older adults in Riyadh were frail, while 47.3% were pre-frail (1). The key factors independently associated with frailty among Saudi older adult include age, living alone, cognitive impairment, and multimorbidity (1). The prevalence of frailty was significantly (p < 0.001) associated with falls among Saudi older adults and frail older adult have 5.37 times higher number of falls compared with non-frail individuals (2). Frailty increases vulnerability to negative health outcomes, such as fatigue, weakness, disability, falls, hospitalization, imposing significant healthcare burdens and contributing to depression (3, 4).
Depression a major mental health issue among older adults and is often linked to physical decline, cognitive impairment, and reduced quality of life (QoL) (5). Recent studies found that 42.4% of older adults aged 60 years and older in Saudi Arabia exhibited depressive symptoms (6). The prevalence of depressive symptoms was higher among older adult diagnosed with chronic conditions (6). A systematic review and meta-analysis of 24 studies highlighted that depression was at approximately fourfold increased odds among frail older adults (7). The co-existence of depression and frailty leads to worse outcomes such as accelerated cognitive impairment, increased morbidity and mortality, and a declined QoL, emphasizing the need to explore potential modifiable factors associated with both conditions (7).
In this sense, proposed that physical activity (PA) may play a crucial role in promoting and preserving mental health by potentially mitigating the negative impacts of stress (8). According to the Physical Activity Guidelines for Americans, adults should perform at least 150 min to 300 min a week of moderate-intensity, or 75 min to 150 min a week of vigorous-intensity aerobic physical activity (9). A large-scale community-based study among 26,000 families in Saudi Arabia reported that only 17.4% of adults meet the minimum recommended physical activity levels and those aged ≥65 years old was the lowest practitioners of physical activity (10). The most common reason for not practicing physical activity was lack of desire (33.50%) (10). A recent literature review investigating the relationship between PA and depression revealed that there is an inverse relationship between PA and depression in older adults (11). However, none of the studies included in this review studied the association between sedentary behavior and depression. Further, the recommendation of this review mentioned that “reciprocal relationships between PA and depression in older adults still need more research to be replicated” (11).
Empirical evidence indicated that consistent engagement in PA, particularly moderate-to-vigorous physical activity (MVPA) (e.g., exercise, sports, and brisk walking) has been linked to reduced levels of depression in older adults (12). Similarly, a randomized control trial reported that multicomponent exercise program have a significant impact in reducing frailty (p < 0.001) and reversing frailty to pre-frailty in the older population (13).
Despite the known benefits of PA, little attention has been paid to the combined impact of frailty and depression on PA levels and QoL among older adults. Given the cultural and lifestyle differences in Saudi Arabia, it is essential to investigate these associations to addresses these modifiable factors and inform tailored interventions that can improve mental health, and frailty symptoms of older adults, ultimately enhancing their overall quality of life.
Therefore, the present study aimed to primarily examine the independent association of depression, frailty and their coexistence with PA levels among community-dwelling older adults in Saudi Arabia. The secondary aim was to investigate the independent association of depression, frailty and their coexistence with QoL among Saudi older adults. The results of the study may help healthcare professionals to understand the interplay association between coexisted frailty and depression and both PA and QoL, and thereby design an appropriate modifiable intervention to reduce their impact and improve overall QoL.
Methods
Study design
A cross-sectional study was conducted to examine the association between depression, frailty and coexisted frailty and depression and both PA level and QoL among community-dwelling older adults in Saudi Arabia.
Data collection procedures
Adults’ community-dwellers were recruited to participate in the study. Participants were eligible if they were aged ≥ 60 years, able to read and write in Arabic, and were Saudi citizens. The data collection was conducted in-person by ten independent trained physiotherapy researchers (between March–September 2022). Many community locations were used for recruitment including malls, mosques, and social places.
Data were collected using a two-part, standardized form designed by the research team for the purpose of the study. The first part of the form contained questions related to demographics including age, gender, and body mass index (BMI). The second part of the form aimed to gather clinical data using standardized outcome measure including PA level, depression symptoms and QoL. All research assistants were trained on data collection. The validation process was taken place through randomly validating the results with some of the included participants through phone call. All data were collected via written questionnaires or interviews. The collected data were anonymized and confidentially protected. The recruited participants received a participant information sheet (includes study aim, procedure, their rights to withdraw anytime, and the assurance of the privacy of the collected data) and have an opportunity to ask anything about the study before participation. All participants signed an informed consent form in accordance with the Declaration of Helsinki. This study was approved by the Research Ethics Committee at Prince Sattam bin Abdulaziz University (No. RHPT/022/010).
Outcome measures
Frailty
The Arabic version of the FRAIL scale is a 5-domain scale designed to evaluate physical frailty (14). These domains include resistance, fatigue, illness, ambulation, and weight loss. Scores on the scale range from 0 to 5, with 0 representing the best condition and 5 indicating the worst. The total FRAIL scale score is computed by summing up the scores from each of the five domains. A score of 3 to 5 indicates frailty, 1 to 2 indicates pre-frailty, and a score of 0 indicates no frailty. Arabic FRAIL scale demonstrated good diagnostic accuracy for frailty (AUC = 0.71) using the Fried Frailty Index as the criterion measure (14).
Depressive symptoms
The Arabic version of the Patient Health Questionnaire 9 (PHQ-9) was used to assess depressive symptoms in this study (15). This questionnaire is a valid scale for detecting suspected cases of depression and anxiety in the general population as well as for assessing the severity of these mental diseases. PHQ-9 demonstrated a good reliability and validity in both original and Arabic versions (15, 16). The Arabic PHQ-9 showed good internal consistency with Cronbach’s alpha of 0.857 (15). All items in the Arabic version were correlated with the total scale to a good degree (lowest r = 0.378) (15).
PHQ-9 includes 9 questions related to depressive symptoms. These questions were used to investigate several domains of depression, including anhedonia, depressed mood, sleep problems, fatigue, change in appetite, decreased self-esteem, concentration disturbance, psychomotor disorder, and suicidal thoughts. Each question was rated on a 4-point scale (0–3): “not at all = 0,” “several days = 1,” “more than half the days = 2,” and “nearly every day = 3.” The total score of the PHQ-9 is the sum of the 9-item scores and ranges between 0 and 27. In the current study, participants were classified as having depressive symptoms when the PHQ-9 score was ≥10 (17, 18).
Physical activity level
The Arabic version of Physical Activity Scale for the Elderly (PASE) was used to measure PA level (19, 20). PASE is a self-reported scale comprised of 12 items evaluates PA over a week focusing on participation in leisure activities, sports, and recreation, categorized by frequency and duration. Activities primarily involving a seated position, such as work (paid or unpaid), were recorded in total hours per week. Housework (light and heavy), lawn work/yard care, home repair, outdoor gardening, and caregiving for others were marked as dichotomous variables (“yes” or “no”). The total PASE score was calculated by summing all activities, with the time spent in each activity (hours/week) or participation in an activity (yes/no) multiplied by empirically derived item weights. The total PASE score range from 0 to 793; higher scores indicate greater PA. The PASE score was stratified in tertiles: 0 to 40 (sedentary), 41 to 90 (light physical activity) and more than 90 (moderate to intense activity) (21). The Arabic version of PASE demonstrated a good psychometric property. The internal consistency of the Arabic PASE components was good (Cronbach’s alpha 0.70–0.75), and the reliability of the components was excellent (ICC2,1 0.90–0.98) (19).
Quality of life
Health-related quality of life (QoL) was assessed using SF-12 (22). The SF-12 is a self-reported multipurpose measure of QoL derived from the SF-36 and contains only 12 items. The 12 items divided into two domains: Physical Component Summary (PCS) and the Mental Component Summary (MCS). The PCS focused on measuring the following QoL concepts: general health, mobility, physical activity limitations, stair climbing ability, and work limitations due to physical issues or pain. Whilest the MCS focuses on emotional aspects such as depression, anxiety, social activity, and the impact of feelings on productivity. The total QoL scores for PCS and MCS ranged from 0 to 100, where higher scores indicate better quality of life. The SF-12 have a good psychometric properties in different age groups, including older adults (23). The Arabic version have a good reliability with a high Cronbach’s alpha for the two components: MCS (α = 0.707) and PCS (α = 0.743) (24).
Sample size calculation
The sample has been calculated based on previous evidence related to the prevalence of frailty in Saudi Arabia (1). The reported prevalence of frailty and pre-frailty was 21.4 and 47.3%. There is no study investigated the prevalence of depressive symptoms or a combination of frailty and depression in older adults in Saudi Arabia. Therefore, we calculated the sample size using this formula [N = Z2 P(1−P)/d2]. Where N = sample size, Z = Z score statistic for a level of confidence (1.96), P = the prevalence of frailty, and d = the degree of precision (0.05). The sample size was estimated to be 330. Therefore, we recruited 395 participants accounting for possible missing data.
Statistical analysis
Descriptive statistics (mean, standard deviation, number, and percentage) were used to examine participants demographics and clinical characteristics. Differences between the groups (depression only, frailty only and coexisted frailty and depression) were determined by one-way ANOVA or Chi-square tests.
Multiple binomial logistic regression was utilized to examine the association between each group (depression only, frailty only and coexisted frailty and depression) and categories for PA level. Results are presented as odds ratios (OR) with 95% confidence intervals (95% CI) after controlling for covariates including age, sex, and BMI in this model.
Multiple linear regression was conducted to examine the association between each group (depressive only, frailty only and coexisted frailty and depression) and QOL. Two models were created, one for the PCS and the other model for the MCS after controlling for covariates including age, sex, and BMI. p-value was set at 0.05, and all the analyses used IBM SPSS for Mac version 29.0 (SPSS Inc. Chicago, IL).
Results
Participant characteristics
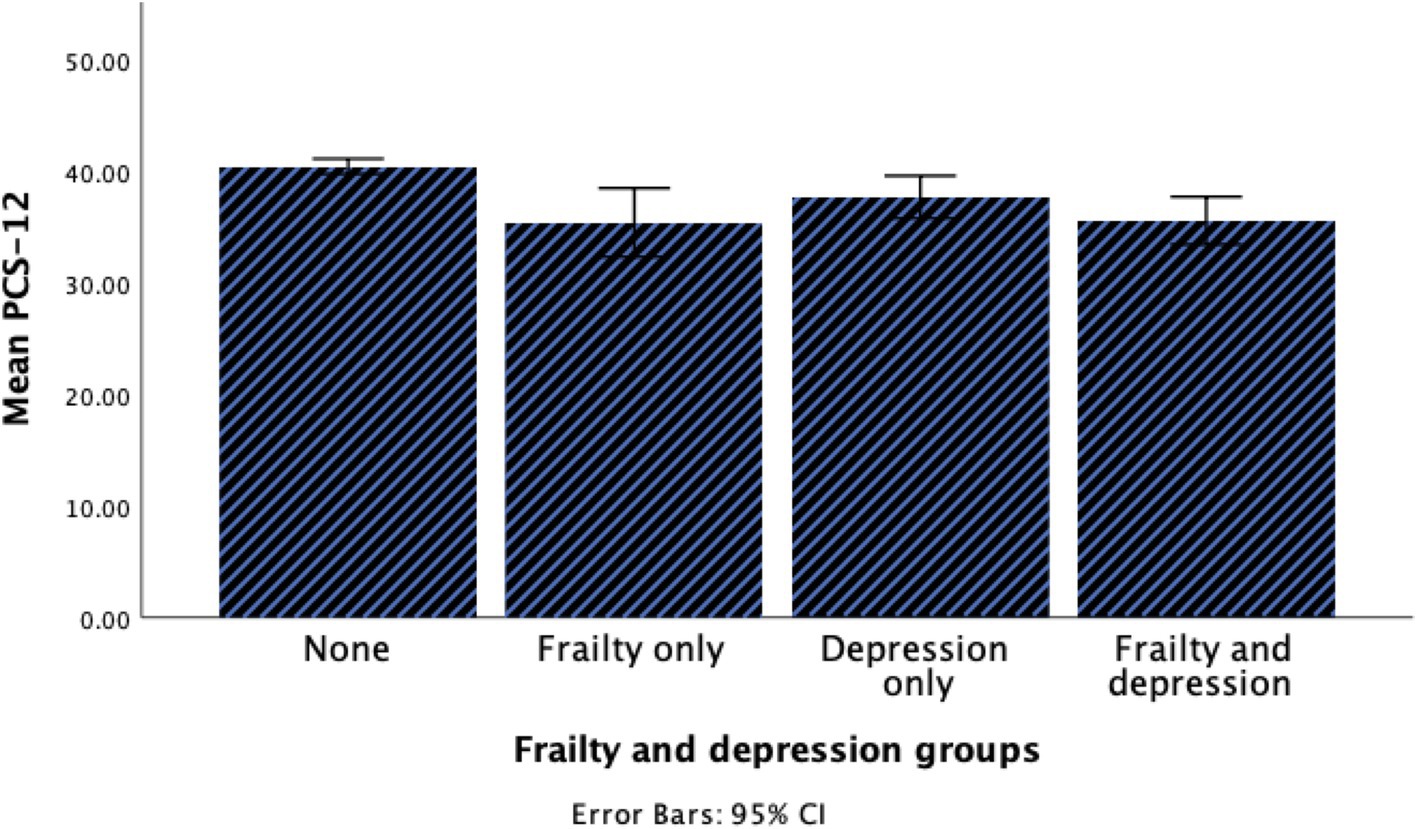
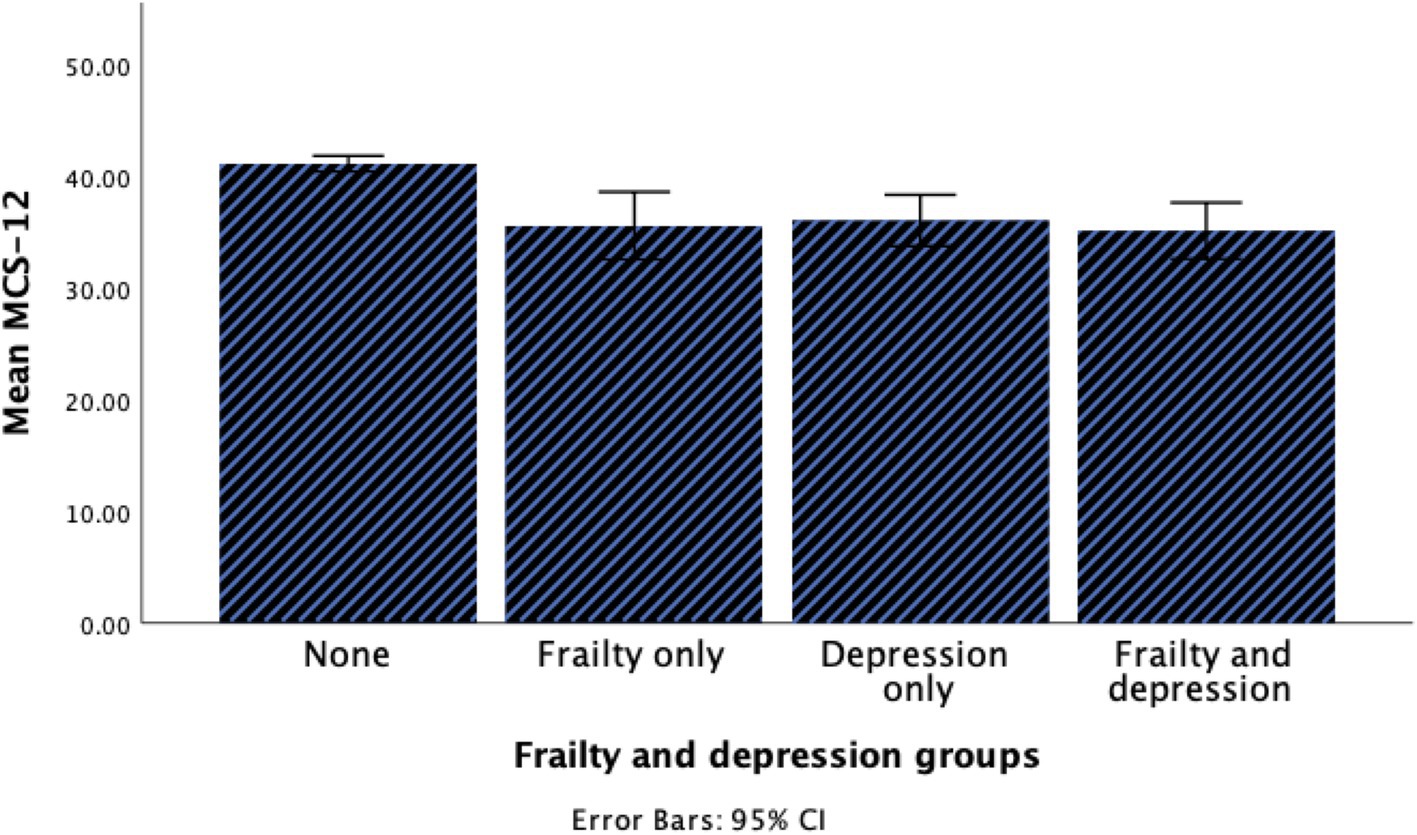
A total of 395 older adults participated in the current study. The demographic and clinical characteristics of the participants are summarized in Table 1. In brief, age, sex, quality of life, and level of PA were significantly different between groups. The prevalence of coexisting frailty and depression was 8.6% among participants. Participants with coexisting frailty and depression were notably older, and more than half of them exhibited a sedentary level of PA. Furthermore, coexisting frailty and depression group had lower scores in both PCS and MCS compared to other groups as illustrated in Figures 1, 2.
Summary of main findings
This study examined the association between frailty, depression, and their coexistence with levels of physical activity and quality of life among community-dwelling older adults in Saudi Arabia. The Key findings reveal that those with co-existing frailty and depression were significantly more sedentary (OR = 4.37, 95% CI: 1.41–13.55, p = 0.011) having lower physical (PCS) and mental (MCS) quality-of-life scores compared with other groups. Depression and frailty independently contributed to lower quality of life. While physical component quality of life (PCS) had a more apparent association with frailty, the mental component (MCS) was more associated with depression.
Association between groups and categories of physical activity level
Table 2 presents the results of multinomial logistic regression examining the association between frailty, depression, and coexisting frailty and depression with different levels of PA (PASE categories). The regression model has been adjusted for potential confounding factors, including age, sex, and BMI.
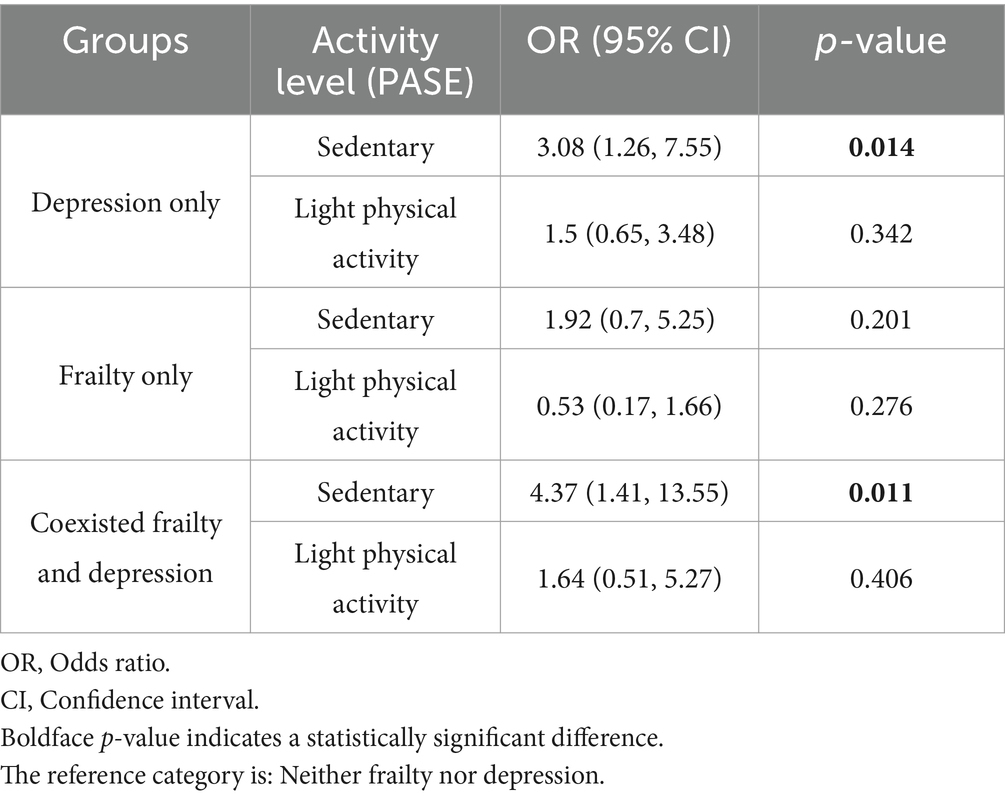
Table 2. Multinomial logistic regression for the association between each group with level of physical activity (PASE).
The results demonstrate a significant association between PA levels and the presence of depression or a coexistence of depression and frailty. Participants with depressive symptoms were significantly more likely to be sedentary (OR = 3.08, 95% CI: 1.26–7.55, p = 0.014) compared to those without frailty or depression. Additionally, coexisted frailty and depression group showed a significant association with PA level, and participants in this group were more likely to be sedentary (OR = 4.37, 95% CI: 1.41–13.55, p = 0.011). However, frailty alone showed no significant associations (p > 0.05) with sedentary or light PA levels.
Association between groups and quality of life
Tables 3, 4 presents the results of the multiple linear regression examining the association between frailty, depression, and coexisting frailty and depression with physical (PCS) and mental (MCS) subscales and of quality of life. The regression models have been adjusted for potential confounding factors, including age, sex, and BMI.
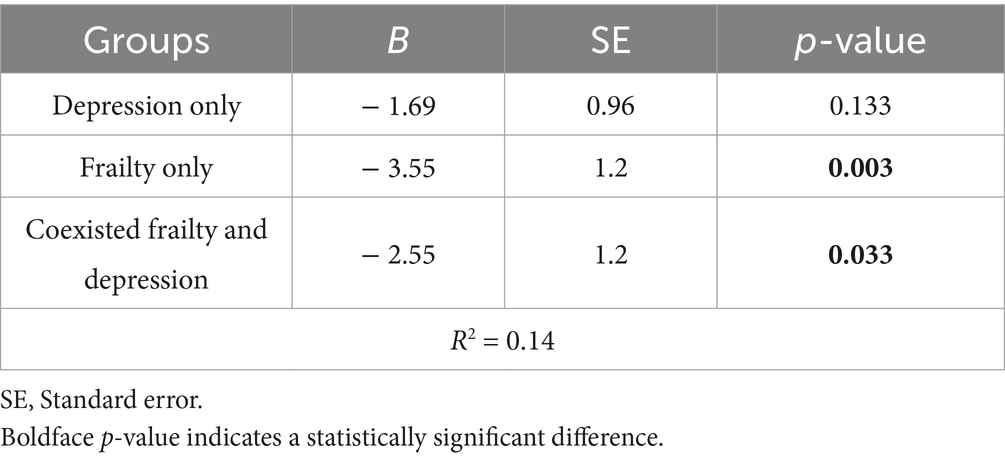
Table 3. Multiple linear regression for the association between each group with PCS of the quality of life (SF12).
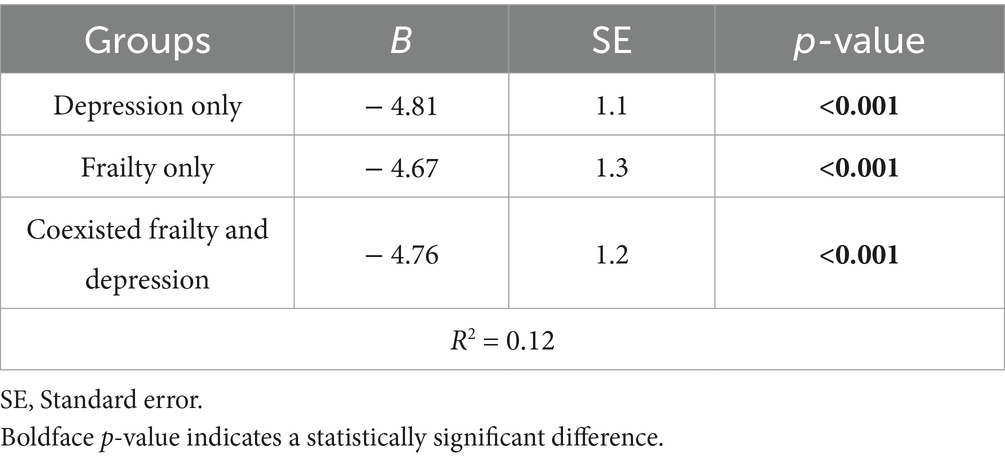
Table 4. Multiple linear regression for the association between each group with MCS of the quality of life (SF12).
Both groups, the frailty only and the coexisting frailty and depression group, were associated with lower values in the physical component summary (PCS) as shown in Table 3. The association results indicated a negative association of frailty with the physical quality of life (PCS) (B = −3.65, SE = 1.2, p = 0.003). Further, the association results suggested that coexisting frailty and depression affect the PCS score negatively (B = −2.53, SE = 1.2, p = 0.033). However, depression alone showed no significant associations with PCS score (p = 0.133), suggesting that depression independently may not significantly affect the physical domain of QoL.
For the mental component summary (MCS), all groups (frailty, depression, and coexisting frailty and depression) were significantly negatively associated with MCS scores (p < 0.001) as shown in Table 4. Frailty only group was significantly negatively associated with MCS score (B = −4.67, SE = 1.3, p < 0.001), indicating that frailty has a negative influence on mental well-being. Similarly, depression only group had the greatest negative association with MCS score (B = −4.81, SE = 1.1, p < 0.001), suggesting that depression is a major factor contributing to poor mental QoL. In addition, the frailty and depression coexisting were negatively associated with MCS score (B = −4.76, SE = 1.2, p < 0.001), emphasizing the role of both conditions in the deterioration of mental QoL.
Overall, frailty mainly affects the physical component of QoL; whilest depression has a stronger negative impact on mental component of QoL. The coexisting frailty and depression have a negative effect on both physical and mental quality of life.
Discussion
Main findings
This study aimed to explore the association between frailty, depression, or their coexistence with PA level. Further, it investigated the independent association between depression, frailty and coexisted frailty and depression with physical and mental quality of life among older adults. The findings revealed that a significant decline in PA level in depression and coexisting frailty and depression group as both of them are significantly associated with higher likelihood of being sedentary. Additionally, frailty alone and coexisting frailty and depression significantly reduce the physical aspect of quality of life (PCS). in the other hand, both frailty and depression, whether independently or coexisting, significantly reduce the mental aspect of quality of life (MCS).
Comparison with existing literature
The current study findings align with recent research that demonstrated a significant association between PA level as measured by total PASE score and depression (rs = −0.371, p < 0.001) in older adults in Taiwan (25). The association between PA level and depression could be bidirectional as shown in a large cross-sectional study that analysed data from 14 European countries (26). A data from 32,392 European late middle-aged to older adults showed that moderate and vigorous PA at least once a week is negatively associated with the score of depression (p < 0.001) (26). In addition, results from a recent cross-sectional study conducted in China among 1,180 older adults (aged ≥ 60 years) found that lower PA levels were significantly associated with depressive symptoms among older women (B = 1.35, p < 0.001) (27).
On the other hand, frailty alone was not significantly associated with the PA levels in our findings, although previous studies conducted in Brazil and Taiwan shown that frailty associated with low levels of PA (25, 28). In Brazil, a longitudinal study evaluated the relationship between physical activity levels, sedentary behavior, and frailty among older adults found that low PA levels and excessive sedentary behavior (≥540 min per day) were associated with a higher prevalence of frailty (PR = 2.83, p = 0.01) (28). In Taiwan, the result of a cross-sectional study investigated the associations between physical activity and frailty indicated that frailty associated (rs = −0.423, p < 0.001) with the total PASE score in older adult population (25). This disagreement between studies and our findings could be raised from the differences in the prevalence of frailty in the study’s population as only 7.1% of our sample have frailty, whereas frailty was more prevalent in the Taiwanese study sample, affecting 22.6% of participants (25).
Robust associations were found between various QoL domains (PCS and MCS) and frailty, as well as coexisting frailty and depression. However, depression alone showed a significant negative association only with the mental domain of QoL. This finding aligns with a previous literature that reported a negative correlation between frailty and QoL (4, 29–31). A systematic review and meta-analysis investigating the relationship between frailty and QoL among community-dwelling older adults revealed significantly higher PCS score on the SF-36 scale in non-frail group compared to those with frailty (30). Furthermore, a cross-sectional study used a multinomial logistic analysis of 573 individuals aged over 65 years old and lived in Spain identified the factors associated with QoL in community-dwelling older adults (29). Their results noted that frailty was the most strongly associated factor with diminished QoL, significantly affecting both the MCS and PCS. The odds of older adults having a low PCS were seven times greater for those who were frail (OR = 7.43, 95% CI = 2.13–25.82) compared to those who were robust. Similarly, the odds of having a low MCS were three times greater for those who were frail (OR = 3.2, 95% CI = 1.21–8.46) compared to those who were robust.
On the other hand, our finding is partially consistent with previous literature investigating the association between depression and QoL (32, 33). A systematic review and meta-analysis of longitudinal studies investigating the longitudinal association between depression and QoL showed that individuals with baseline depressive disorders had significantly (p < 0.01) lower PCS and MCS scores at follow-up compared to those without baseline depression, with medium and large effect sizes, respectively (30). Additionally, recent research among older adults in Greece suggested a significant independent association between frailty and depression with the physical domain of QoL (32). Their results indicated a decline in the physical domain of QoL as frailty and depression increased. However, they found that the mental domain of QoL was associated with depression scores but not with frailty. The differences between our findings and previous research could be due to the different scales used to measure depression, frailty, and QoL (32). Furthermore, the age of the sample in previous studies included younger participants (age range: 18–65) which could affect the prevalence of frailty and depression among participants (32, 33).
The interrelationships between frailty, depression, physical activity, and quality of life
The findings of our study align with the theoretical framework that conceptualize frailty and depression as interacting geriatric syndromes that are influenced by overlapping common biological and functional pathways (34, 35).
The negative association between coexisting frailty and depression with the sedentary level of PA is not surprising given the overlap of frailty characteristics, depressive symptoms with reduction in PA. Frailty and depression are among the most strongly comorbid illness; with approximately 40% of frail older adults having depression and approximately 40% of people with late-life depression are frail (7). This bidirectional association between frailty and depression highlighted in two landmark studies by Fried and colleagues and Lakey and colleagues (3, 35). Fried and colleagues found a significant difference (p < 0.001) in depression among alder adults with 31% of frail older adults have depression compared to 3% of non-frail elders (3).
Using data from the Women’s Health Initiative Observational Study (n = 33,324), Lakey and colleagues reported that non-frail women with high depressive symptom scores were 2.19 times likely to become frail over 3 years than women without depressive symptoms (35).
These cross-sectional associations are supported by longitudinal studies further demonstrating this bidirectional risk (36, 37). A longitudinal study among 2,717 older adults found that older adults with depressive symptoms are more likely to develop frailty than nondepressed individuals (2.6 increased hazard) over an average follow-up period of 5.9 years (36). Conversely, a large scale (n = 25,771 older adults) 5-years longitudinal study found that pre-frail older adults had an 1.86 higher odds of depression, and frail older adult had more than twice the odds (OR = 2.46) compared to non-frail individuals (37).
Our study expands upon the previous literature by demonstrating that the coexisting frailty and depression associated with the decline in PA levels and reduction in QoL more than either condition alone. The interrelationship between frailty, depression, physical activity, and quality of life in older adults has been documented in previous literature (38, 39). A cross-sectional study explored the mediating effects of daily physical activity on the relationship between frailty and QoL in Taiwanese older adults (39). Their results demonstrate that daily physical activity mediated the relationship between frailty and QoL and higher physical activity correlated with lower frailty scores and better QoL. More recently, a cross-sectional study involving 235 pre-frail/frail older adults explored the interplay between frailty, physical function, physical activity and their impact on the QoL and depressive status in older adults with frailty (38). The findings revealed a significant correlation between QoL and aspects of physical frailty. Better QoL score was associated with low fatigue, high gait speed and higher engagement in light physical activity. Furthermore, worsening depressive symptoms was associated with slow gait speed and low level of physical activity. Their findings suggested that physical activity is a key contributor to improve quality of life and reduce depressive symptoms in older adults with frailty.
Proposed mechanisms
The overlap between depression and frailty could be explained by the shared biological mechanisms that result in increased vulnerability and negative health outcomes in older adults. Brown et al. proposed that late life depression and frailty is the result results from shared biological mechanisms, including mitochondrial dysfunction, dopamine dysregulation, and chronic inflammation (34). Changes in mitochondrial function are apparent with age and characterized by reduced adenosine triphosphate (ATP) production, leading to fatigue, mobility decline, and an increase in oxidative stress. This mitochondrial dysfunction has been identified to be linked with reduced activity levels and depression. Another possible mechanism was dopamine dysfunction, particularly diminished levels of D1/D2 receptors in both the caudate and the putamen in older adults. This decrease is associated with decreased motor speed and worsening in frontal functioning, thereby exacerbate both conditions. Chronic inflammation, with raised levels of pro-inflammatory cytokines such as IL-6 and TNF-α, and C-reactive protein (CRP), affect the central nervous system—specifically, dopaminergic function in the basal ganglia, which may result in depression, fatigue, and cognitive and motor slowing. Chronic inflammatory state contributes to specific characteristics of frailty including low energy, decreased muscle mass and strength, cognitive impairments, reinforcing the bidirectional relationship between depression and frailty (34).
Clinical implications
The strong association between coexistence of frailty and depression with the sedentary PA level and reduced QoL among community-dwelling older adults have significant clinical implications. The complexity of health issues among older adults especially with the coexistent frailty and depression implies that healthcare providers must adopt a multidisciplinary approach in managing these population. In routine geriatric assessment, regular evaluation of frailty and depressive symptoms, physical activity levels, and quality of life is necessary to inform the design of targeted interventions. A collaborative multidisciplinary program that addresses both mental and physical health is recommended. These may include mental health support (e.g., cognitive-behavioral therapy) to help in addressing the psychological barriers to physical activity and reduce sedentary behavior in this population. Engaging in regular physical activity program including aerobic, resistance, balance, and flexibility exercises plays a beneficial role in reducing frailty, enhancing physical function, decreasing psychological distress, and improving overall mental well-being (8, 13, 39).
In addition, health education could help in raising the awareness about the symptoms of frailty and depression and how physical exercise could mitigate their impact. Furthermore, motivational strategies and lifestyle interventions to enhance physical active lifestyle are recommended to promote a healthy aging, reduce the impact of frailty and depression, and thereby improve the quality of life.
Study contributions and limitations
This study is one of the first to specifically examine the coexistence of frailty and depression and their combined impact on PA and QoL in older adults. The study contributes to the existing literature by quantifying the associations between frailty, depression, their coexistence with the PA levels and QoL in an older adult Saudi Arabian population. The results highlights the importance of developing a multidisciplinary interventions to address the impact of both frailty and depression and emphasize the QoL of older adults. Nevertheless, several limitations of this study should be acknowledged. First, the assessment of PA, depressive symptoms and QoL relied on self-reported measures, which may be subject to reporting bias. Second, the sample was recruited from a specific region of Saudi Arabia, which may limit the generalizability of results to other populations or cultural contexts. Further, the cross-sectional design of this study limits the ability to infer causality between frailty, depression, their coexistence, and the lower scores of QoL or PA.
Conclusion
The novel contribution of this study is the focus on the combined impact of the coexisting frailty and depression on physical activity and quality of life among Saudi older adults. This study demonstrates a significant association between depression and coexisting frailty and depression with the sedentary level of PA among older adults. Individuals with coexisting frailty and depression were over four times more likely to be sedentary compared to those without either condition (OR = 4.37, 95% CI: 1.41–13.55). Furthermore, frailty, depression, their coexistence significantly associated with a decline in MCS of QoL. The lower score of MCS was associated with the frailty and coexisting frailty and depression groups. Individuals with coexisting frailty and depression had a 2.55-point decrease in MCS score compared to those without either condition (B = −2.55, p = 0.033). These findings highlight the need for multidimensional geriatric assessments including frailty and depressive symptoms evaluation to identifying modifiable risk factors associated with low levels of PA and QoL. Designing of a targeted interventions should be considered by multidisciplinary healthcare team (i.e., medical doctors and physiotherapists) to reduce the influence of frailty and depression in older adults and improve QoL. Moreover, public health policies should support the implementation of motivational strategies to raise an awareness about the impact of coexisting frailty and depression, promote a healthy lifestyle and address the barriers to physical activity.
While this study provides valuable insights, it is important to acknowledge its limitations, including its cross-sectional nature. Further research is required to establish causality through longitudinal studies that provide deeper insights into how coexisting frailty and depression influence PA and QoL over time in older adults. Furthermore, inclusion of additional measures such as Basal Metabolic Rate (BMR) and biomarkers (e.g., cortisol) might assist in gaining deeper insights into the physiological mechanisms underpinning the coexisting frailty and depression, and their effect on physical activity levels.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by this study was conducted following the Declaration of Helsinki and was approved by the Research Ethics Committee of Prince Sattam Bin Abdulaziz University (No. RHPT/022/010, approval date: 01-03-2022). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NA: Conceptualization, Data curation, Writing – original draft. BA: Funding acquisition, Methodology, Writing – original draft. MA: Methodology, Writing – review & editing. AhA: Investigation, Supervision, Writing – review & editing. AqA: Formal analysis, Validation, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors extend their appreciation to Prince Sattam bin Abdulaziz University for funding this research work through the project number (PSAU/2024/03/30969).
Acknowledgments
The authors extend their appreciation to Prince Sattam bin Abdulaziz University for funding this research work through the project number (PSAU/2024/03/30969).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Alqahtani, BA, Alenazi, AM, Alshehri, MM, Osailan, AM, Alsubaie, SF, and Alqahtani, MA. Prevalence of frailty and associated factors among Saudi community-dwelling older adults: a cross-sectional study. BMC Geriatr. (2021) 21:185. doi: 10.1186/s12877-021-02142-9
2. Alqahtani, BA, and Alenazi, AM. Assessing the impact of frailty on fall risk in older adults: evidence from Saudi Arabia. J Res. (2025) 4, 1–5. doi: 10.57197/JDR-2025-0004
3. Fried, LP, Tangen, CM, Walston, J, Newman, AB, Hirsch, C, Gottdiener, J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.M146
4. Godin, J, Armstrong, JJ, Wallace, L, Rockwood, K, and Andrew, MK. The impact of frailty and cognitive impairment on quality of life: employment and social context matter. Int Psychogeriatr. (2019) 31:789–97. doi: 10.1017/S1041610218001710
5. Bai, W, Zhang, J, Smith, RD, Cheung, T, Su, Z, Ng, CH, et al. Inter-relationship between cognitive performance and depressive symptoms and their association with quality of life in older adults: a network analysis based on the 2017–2018 wave of Chinese longitudinal healthy longevity survey (CLHLS). J Affect Disord. (2023) 320:621–7. doi: 10.1016/j.jad.2022.09.159
6. Alabdulgader, A, Mobarki, AO, AlDuwayrij, A, Albadran, A, Almulhim, MI, and Almulhim, A. Depression screening for the geriatric population visiting primary healthcare centers in the eastern region of Saudi Arabia. Cureus. (2021) 13:e17971. doi: 10.7759/cureus.17971
7. Soysal, P, Veronese, N, Thompson, T, Kahl, KG, Fernandes, BS, Prina, AM, et al. Relationship between depression and frailty in older adults: a systematic review and meta-analysis. Ageing Res Rev. (2017) 36:78–87. doi: 10.1016/j.arr.2017.03.005
8. Mahindru, A, Patil, P, and Agrawal, V. Role of physical activity on mental health and well-being: a review. Cureus. (2023) 15:e33475. doi: 10.7759/cureus.33475
9. Piercy, KL, and Troiano, RP. Physical activity guidelines for Americans from the US Department of Health and Human Services. Circ Cardiovasc Qual Outcomes. (2018) 11:e005263. doi: 10.1161/CIRCOUTCOMES.118.005263
10. Alqahtani, BA, Alenazi, AM, Alhowimel, AS, and Elnaggar, RK. The descriptive pattern of physical activity in Saudi Arabia: analysis of national survey data. Int Health. (2021) 13:232–9. doi: 10.1093/inthealth/ihaa027
11. Zhang, S, Xiang, K, Li, S, and Pan, HF. Physical activity and depression in older adults: the knowns and unknowns. Psychiatry Res. (2021) 297:113738. doi: 10.1016/j.psychres.2021.113738
12. Callow, DD, Arnold-Nedimala, NA, Jordan, LS, Pena, GS, Won, J, Woodard, JL, et al. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am J Geriatr Psychiatry. (2020) 28:1046–57. doi: 10.1016/j.jagp.2020.06.024
13. Sadjapong, U, Yodkeeree, S, Sungkarat, S, and Siviroj, P. Multicomponent exercise program reduces frailty and inflammatory biomarkers and improves physical performance in community-dwelling older adults: a randomized controlled trial. Int J Environ Res Public Health. (2020) 17:3760. doi: 10.3390/ijerph17113760
14. Alqahtani, BA, and Nasser, TA. Assessment of frailty in Saudi community-dwelling older adults: validation of measurements. Ann Saudi Med. (2019) 39:197–204. doi: 10.5144/0256-4947.2019.197
15. AlHadi, AN, AlAteeq, DA, al-Sharif, E, Bawazeer, HM, Alanazi, H, AlShomrani, AT, et al. An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann General Psychiatry. (2017) 16:32. doi: 10.1186/s12991-017-0155-1
16. Sun, Y, Fu, Z, Bo, Q, Mao, Z, Ma, X, and Wang, C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. (2020) 20:474. doi: 10.1186/s12888-020-02885-6
17. Almegbas, NR, Almutairi, GR, Alosaimi, RM, Alqahtani, MA, Batook, SG, Alfageh, IA, et al. Fatigue and cognitive decline associated with depressive symptoms among community-dwelling adults. Inquiry. (2023) 60:469580231153524. doi: 10.1177/00469580231153524
18. Manea, L, Gilbody, S, and McMillan, D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184:E191–6. doi: 10.1503/cmaj.110829
19. Alqarni, AM, Vennu, V, Alshammari, SA, and Bindawas, SM. Cross-cultural adaptation and validation of the Arabic version of the physical activity scale for the elderly among community-dwelling older adults in Saudi Arabia. Clin Interv Aging. (2018) 13:419–27. doi: 10.2147/CIA.S157007
20. Washburn, RA, Smith, KW, Jette, AM, and Janney, CA. The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol. (1993) 46:153–62. doi: 10.1016/0895-4356(93)90053-4
21. Covotta, A, Gagliardi, M, Berardi, A, Maggi, G, Pierelli, F, Mollica, R, et al. Physical activity scale for the elderly: translation, cultural adaptation, and validation of the Italian version. Curr Gerontol Geriatr Res. (2018) 2018:8294568. doi: 10.1155/2018/8294568
22. Ware, J Jr, Kosinski, M, and Keller, SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34:220–33. doi: 10.1097/00005650-199603000-00003
23. Jakobsson, U. Using the 12-item short form health survey (SF-12) to measure quality of life among older people. Aging Clin Exp Res. (2007) 19:457–64. doi: 10.1007/BF03324731
24. Haddad, C, Sacre, H, Obeid, S, Salameh, P, and Hallit, S. Validation of the Arabic version of the "12-item short-form health survey" (SF-12) in a sample of Lebanese adults. Arch Public Health. (2021) 79:56. doi: 10.1186/s13690-021-00579-3
25. Huang, TY, Chou, MY, Liang, CK, Lin, YT, Chen, RY, and Wu, PF. Physical activity plays a crucial role in multidomain intervention for frailty prevention. Aging Clin Exp Res. (2023) 35:1283–92. doi: 10.1007/s40520-023-02412-z
26. Marques, A, Bordado, J, Peralta, M, Gouveia, ER, Tesler, R, Demetriou, Y, et al. Cross-sectional and prospective relationship between physical activity and depression symptoms. Sci Rep. (2020) 10:16114. doi: 10.1038/s41598-020-72987-4
27. Wang, Y, Wang, X, Zhu, X, Sun, Y, Han, B, and Chen, T. Physical activity, physical frailty and depressive symptoms among Chinese male and female older adults: do different indicators make a difference? Front Public Health. (2023) 11:11. doi: 10.3389/fpubh.2023.1280952
28. da Silva, VD, Tribess, S, Meneguci, J, Sasaki, JE, Garcia-Meneguci, CA, Carneiro, JAO, et al. Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health. (2019) 19:709. doi: 10.1186/s12889-019-7062-0
29. Blanco-Reina, E, Valdellós, J, Ocaña-Riola, R, García-Merino, MR, Aguilar-Cano, L, Ariza-Zafra, G, et al. Factors associated with health-related quality of life in community-dwelling older adults: a multinomial logistic analysis. J Clin Med. (2019) 8:1810. doi: 10.3390/jcm8111810
30. Crocker, TF, Brown, L, Clegg, A, Farley, K, Franklin, M, Simpkins, S, et al. Quality of life is substantially worse for community-dwelling older people living with frailty: systematic review and meta-analysis. Qual Life Res. (2019) 28:2041–56. doi: 10.1007/s11136-019-02149-1
31. Siriwardhana, DD, Weerasinghe, MC, Rait, G, Scholes, S, and Walters, KR. The association between frailty and quality of life among rural community-dwelling older adults in Kegalle district of Sri Lanka: a cross-sectional study. Qual Life Res. (2019) 28:2057–68. doi: 10.1007/s11136-019-02137-5
32. Argyriou, C, Dimitriadou, I, Saridi, M, Toska, A, Lavdaniti, M, and Fradelos, EC. Assessment of the relation between depression, frailty, nutrition and quality of life among older adults: findings from a cross-sectional study in Greece. Psychogeriatrics. (2024) 24:1065–74. doi: 10.1111/psyg.13160
33. Hohls, JK, König, HH, Quirke, E, and Hajek, A. Anxiety, depression and quality of life—a systematic review of evidence from longitudinal observational studies. Int J Environ Res Public Health. (2021) 18:12022. doi: 10.3390/ijerph182212022
34. Brown, PJ, Rutherford, BR, Yaffe, K, Tandler, JM, Ray, JL, Pott, E, et al. The depressed frail phenotype: the clinical manifestation of increased biological aging. Am J Geriatr Psychiatry. (2016) 24:1084–94. doi: 10.1016/j.jagp.2016.06.005
35. Lakey, SL, LaCroix, AZ, Gray, SL, Borson, S, Williams, CD, Calhoun, D, et al. Antidepressant use, depressive symptoms, and incident frailty in women aged 65 and older from the Women's Health Initiative observational study. J Am Geriatr Soc. (2012) 60:854–61. doi: 10.1111/j.1532-5415.2012.03940.x
36. Chang, CC, Wu, CS, Tseng, HY, Lee, CY, Wu, IC, Hsu, CC, et al. Assessment of incident frailty hazard associated with depressive symptoms in a Taiwanese longitudinal study. Int Psychogeriatr. (2022) 34:61–70. doi: 10.1017/S1041610221000806
37. Marconcin, P, Barak, S, Ferrari, G, Gouveia, ÉR, de Maio Nascimento, M, Willig, R, et al. Prevalence of frailty and its association with depressive symptoms among European older adults from 17 countries: a 5-year longitudinal study. Int J Environ Res Public Health. (2022) 19:14055. doi: 10.3390/ijerph192114055
38. Casals, C, Corral-Pérez, J, Ávila-Cabeza-de-Vaca, L, González-Mariscal, A, Carrión-Velasco, Y, Rodríguez-Martínez, MC, et al. Exploring the interplay of frailty, physical function, physical activity, nutritional status, and their association with quality of life and depressive symptoms in older adults with the frailty phenotype. Int J Geriatr Psychiatry. (2024) 39:e6078. doi: 10.1002/gps.6078
Keywords: frailty, depression, physical activity, quality of life, older adult
Citation: Alhwoaimel NA, Alqahtani BA, Alshehri MM, Alhowimel AS and Alenazi AM (2025) Coexisting frailty and depression associated with low physical activity and quality of life in Saudi community-dwelling older adults: a cross-sectional study. Front. Public Health. 13:1531101. doi: 10.3389/fpubh.2025.1531101
Edited by:
Silvia Giovannini, Catholic University of the Sacred Heart, ItalyReviewed by:
Ferdinando Franzoni, University of Pisa, ItalyJúlio César André, Faculdade de Medicina de São José do Rio Preto, Brazil
Copyright © 2025 Alhwoaimel, Alqahtani, Alshehri, Alhowimel and Alenazi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bader A. Alqahtani, ZHJhbHFhaHRhbmliYUBnbWFpbC5jb20=
 Norah A. Alhwoaimel
Norah A. Alhwoaimel Bader A. Alqahtani
Bader A. Alqahtani Mohammed M. Alshehri
Mohammed M. Alshehri Ahmed S. Alhowimel
Ahmed S. Alhowimel Aqeel M. Alenazi
Aqeel M. Alenazi