- 1Psychiatry Department, Massachusetts General Hospital, Boston, MA, United States
- 2Department of Neurology, Harvard Medical School, Boston, MA, United States
- 3Recovery Inspired Opportunities, Boston, MA, United States
- 4Alcohol Research Group/Public Health Institute, Emeryville, CA, United States
- 5Black Faces Black Voices, Rochester, MN, United States
- 6Faces & Voices of Recovery, Washington, DC, United States
Objective: Racial and ethnic disparities exist in opioid-related overdose death rates and engagement with substance use disorder (SUD) treatment. Emerging peer recovery support services (PRSS) show promise in engaging and supporting marginalized populations. Recovery community centers (RCCs) are an important and growing source of community-based PRSS. Our goal was to examine if RCCs serving Black, Hispanic/Latino, or other racial/ethnic communities successfully engage marginalized populations in their community and if there are differences in the service models and functioning of RCCs serving different racial/ethnic communities.
Methods: We conducted exploratory secondary analyses of a nationwide survey of RCC directors (n = 122), in which directors described their RCC in terms of logistics, footprints, service model, linkages, services, and attitudes toward medication treatment. Analysis of variance and chi-square tests were used to compare RCCs serving different communities (i.e., Black, Hispanic/Latino, Other) on these variables, where “serving a Black/Hispanic/Latino community” was operationally defined as being in a ZIP code with more than double the national prevalence of Black (13.6%) and Hispanic/Latino (19.1%) individuals in the United States.
Results: On average, the median [IQR] percentage of Black participants within RCCs serving Black communities was 45% [30–63%] (51% of residents in the RCCs' ZIP codes were Black); in RCCs serving Hispanic/Latino communities, 50% [28–60%] of RCC participants were Hispanic/Latino (57% of residents in the RCCs' ZIP codes were Hispanic/Latino). Across 70 variables describing the RCCs' service model and functioning, only two statistically significant differences emerged between RCCs serving Black, Hispanic/Latino, and other communities, using an alpha of 0.05. RCCs differed in offering 12-step mutual aid groups (lowest in RCCs serving Hispanic/Latino communities; p = 0.03) and the existence of direct collaboration with clinical sites providing medications for opioid use disorder (MOUD, most common in RCCs serving Black communities; p = 0.03).
Conclusion: The overall RCC model appears to be consistent across racial/ethnic settings in terms of footprints, model of care, services offered, connection to relevant systems and organizations, and attitudes toward medications. Given the commonly observed racial/ethnic disparities in SUD care, the robustness of the RCC model across communities is promising.
Introduction
Racially minoritized communities have been disproportionately affected by the opioid epidemic. Although there were more total overall deaths among non-Hispanic/Latino Whites relative to all other ethnic groups between 1999 and 2017, there was a more drastic rise in opioid-related overdose deaths among Hispanic/Latino and non-Hispanic/Latino Black individuals. Age-adjusted opioid-related death rates increased from 3.5 overdoses per 100,000 people (Hispanic/Latino and Black individuals) in 1999 to 6.8 (Hispanic/Latino individuals) and 12.9 (Black individuals) per 100,000 in 2017 (1). These disparities were amplified during the COVID-19 pandemic. In 2020, the overdose death rate among Black individuals surpassed that of White individuals for the first time since 1999, with Black individuals estimated to have a 16.3% higher overdose death rate (2). While opioids remain a leading driver of substance use-related mortality, research over the past years highlights a disproportionate rise in alcohol (3), amphetamine, cannabis (4), and cocaine-related deaths (5) among Black and Hispanic individuals compared to White individuals.
The U.S. Department of Health and Human Services (HHS) has acknowledged the need to advance racial equity in access to health care, treatment receipt within the justice system, and drug policy for underserved populations (6). Unfortunately, ongoing racial/ethnic disparities exist for treatment. Substance use disorder (SUD) treatment settings are subject to systemic racial barriers (e.g., stigma, distrust), which have hindered them in effectively engaging and retaining non-Hispanic/Latino Black populations, resulting in lower rates of treatment utilization, treatment completion, and equitable medication access to medications for opioid use disorder (MOUDs; e.g., buprenorphine, methadone) (7–13). Structural inequities, rooted in historical discrimination and marginalization, are intensified by social stigma, racial biases, and government-driven punitive measures against people who use substances such as opioids, alcohol, cocaine, methamphetamine, heroin, and cannabis. These barriers have disproportionately affected communities of color (12, 14, 15). Existing literature highlights the impact of discrimination-induced psychological stress and its linkage with problematic substance use (12, 16). Structural and societal conditions have continued to perpetuate disparities in the quality of and access to healthcare, education, economic stability, and community resources (e.g., food, shelter, and medical needs). Indeed, poor socioeconomic conditions have been highlighted as contributors to lower treatment completion rates in Black and Hispanic/Latino populations compared to White populations in formal treatment settings (17–19). These factors, referred to as social determinants of health, are crucial to consider when highlighting the disproportionate rates of substance-use mortality for ethnic and racially minoritized populations (20–22).
The concept of recovery has increasingly shifted toward a more inclusive definition that recognizes its multifaceted nature. The Substance Abuse and Mental Health Services Administration's (SAMHSA) working definition describes recovery as “a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential”. This definition emphasizes four key dimensions that support long-term recovery: health, home, purpose, and community (23). Recovery from SUD may not be achieved through clinical treatment for SUD alone; people follow diverse trajectories from SUD to recovery or remission, including through the help of mutual aid groups, treatment, and the provision of recovery support services (19). The need for recovery support services as part of clinical treatment or as a stand-alone path to recovery initiation and maintenance has given rise to peer recovery support services (PRSS), which are peer-driven non-clinical services delivered by trained peers, often called “peer recovery specialists” or “recovery coaches”. Although little research has been conducted to date, available studies suggest that PRSS have the potential to improve engagement in clinical treatment, as well as in other recovery-oriented settings (e.g., recovery community centers, transitional outpatient, and residential treatment centers) (24). A recent systematic review found that PRSS in hospital settings was found to facilitate linkages to treatment and follow-up care/support (24). Additionally, a positive relationship has been observed between PRSS participation and MOUD initiation, increased treatment retention, and greater treatment satisfaction. These studies point to the potential importance of PRSS in the recovery process, yet further research is needed, particularly regarding its delivery within the context of racial and ethnic disparities in SUD treatment and recovery.
One type of PRSS that may be particularly promising in addressing health disparities is recovery community centers (RCCs). RCCs are brick and mortar buildings that provide a “one-stop-shop” for recovery support services (25). Located within their communities, RCCs welcome all pathways of recovery and uphold and promote safe spaces for individuals regardless of the services they choose to engage with (25, 26). They provide a variety of services, including recovery coaching, support group meetings, relapse prevention skills-building, opioid and/or harm reduction services, technology and internet access, employment and job training linkages, assistance with basic needs and social services, substance-free recreational activities, health and nutrition programs, and civic participation (27). Beyond substance use disorders, RCCs also address behavioral and process addictions through SMART Recovery meetings, a mutual-help program grounded in cognitive behavioral therapy that explicitly supports recovery from behavioral addictions such as gambling, overeating, or internet use, thus supporting individuals across diverse recovery pathways (28). A nationwide survey of RCCs (n = 122) found that all offered support for alcohol and drug-related issues, while nearly 70% of RCCs also addressed “other addictions” and mental health concerns (29). Additionally, an online survey of RCC participants indicated that over 80% of RCC members engaged in polysubstance use, with opioids (32.7%) and alcohol (26.8%) reported as the most common primary substance (25).
RCCs provide extensive internal and external resources that can help individuals initiate and sustain recovery, and are an essential component in improving quality of life outside of clinical care (30). RCCs provide recovery support services that are especially useful to those in low-income communities who experience disparities in access to formal SUD treatment (29). Thus, RCCs may offer a more accessible and engaging support system for racially minoritized individuals by addressing key social determinants of health. Unlike traditional clinical settings, which primarily focus on SUD treatment, RCCs seemingly adopt a holistic approach—connecting individuals to essential social determinants of health that directly impact long-term recovery and stability. By integrating these broader support services, RCCs recognize that sustained recovery is not solely a medical issue (26, 27) but is deeply tied to structural inequities pertaining to socioeconomic health that disproportionately affect racially minoritized communities.
Importantly, RCCs appear to be able to engage ethnic and racially minoritized groups (29). This sets them apart not only from formal treatment settings, as described above but also from some of the more traditional PRSS. For example, recent membership surveys of Alcohol Anonymous (AA) and Narcotics Anonymous (NA) have shown relatively low engagement of Black and Hispanic/Latino people (3–13%) (31, 32). RCCs, on the other hand, may provide a welcoming environment to address disparities and increase recovery resources among Black and Hispanic/Latino populations (29). In this secondary data analysis of a nationwide survey of RCCs (29), we examine if the RCC service model shows a pattern of ethnic/racial disparities that is frequently observed in other SUD and opioid use disorder treatment and recovery settings. In particular, we utilize existing data to test if differences exist between RCCs serving Black, Hispanic/Latino, and other communities in terms of their reach, organizational capacity, service model, interconnectivity with other SUD-relevant organizations, and their attitudes toward MOUDs.
Methods
Sample
This is a secondary data analysis of a sample of RCC directors or delegates who participated in a nationwide survey of RCCs known at the time of the survey (29). Of the 198 RCCs contacted, 122 RCCs responded and completed the survey (122/198, 62% response rate) (29). We asked the directors of RCCs or their delegates to report on the logistics, footprint, model of care, demographics of RCC attendees, services provided, and linkages established at their RCCs (29). For the study, RCCs were defined as: “Brick and mortar places located within the heart of a community that serves as a central recovery hub by providing a variety of support services for people in or seeking recovery” (29).
Procedure
For this secondary data analysis, we differentiated three different kinds of RCCs: RCCs serving Black communities, Hispanic/Latino communities, and other communities. To make these determinations, we utilized the publicly available physical address data for all RCCs in conjunction with 2021 U.S. Census ZIP code tabulation data on race and ethnicity (33). Our operational definition for RCCs serving a Black or Hispanic/Latino community was any RCC located in a ZIP code with more than double the U.S. national prevalence of Black (13.6%) or Hispanic/Latino (19.1%) individuals, respectively (33). Specifically, we defined an RCC as serving a Black community if it was located in a ZIP code in which more than 27.2% of the residents reported being Black, as per the U.S. Census; we defined an RCC as serving a Hispanic/Latino community if more than 38.2% of the residents reported being Hispanic/Latino, as per the U.S. Census. For RCCs with both high Black and Hispanic/Latino prevalence (n = 4), we grouped them according to their higher percentage. We selected this cutoff to capture ZIP codes with a substantial proportion of Black and Hispanic individuals. The 'other' category includes RCCs serving predominantly White populations as well as those serving racially/ethnically mixed or non-specified populations. Using a threshold set at twice the national percentage provides a more meaningful criterion for identifying RCCs that are more closely representative of and inclusive of these racial and ethnic groups.
Study data were collected and managed using the Research Electronic Data Capture (REDCap) system, hosted at Mass General Brigham. REDCap is a secure, web-based, and HIPAA-compliant software platform designed to support data capture for research studies (34). Study staff sent email invitations to the directors of each RCC and followed up via phone calls on three or more different days to remind participants to complete surveys, as needed. RCC leadership was offered $50 to complete the survey; 41 (34%) opted out of remuneration. The Mass General Brigham Institutional Review Board reviewed and approved all study procedures.
Measures
RCC logistics, footprints, model of care, and demographics (Table 1) were assessed with multiple choice items and open-ended questions. To describe the demographics of the people served by their RCC, RCC directors or delegates were asked to estimate the percentage of RCC members per given category for age, gender, race, and ethnicity, as shown in Table 1. For example, when reporting on the age of their RCC members, RCC directors were asked to estimate the percentage of RCC members who were aged “under 18 years”, “18–24 years”, “25–59 years”, and “60+ years”. If percentages did not add up to 100%, the survey platform alerted them and asked for a correction (34). These estimates are based on reports from RCC delegates rather than intake forms or verified data, as many RCCs do not require formal sign-up or intake processes for individuals accessing walk-in services in these community-based settings.
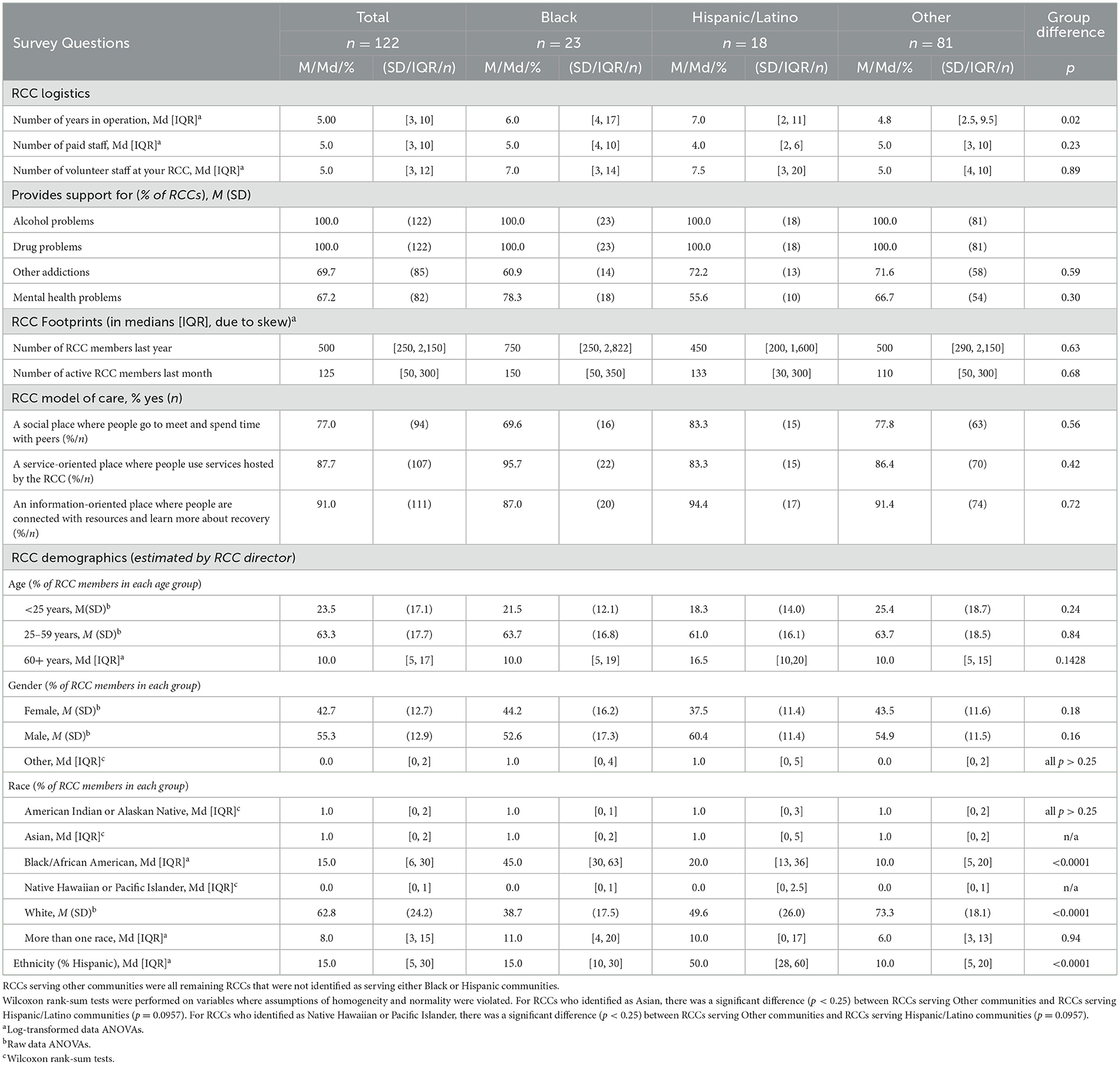
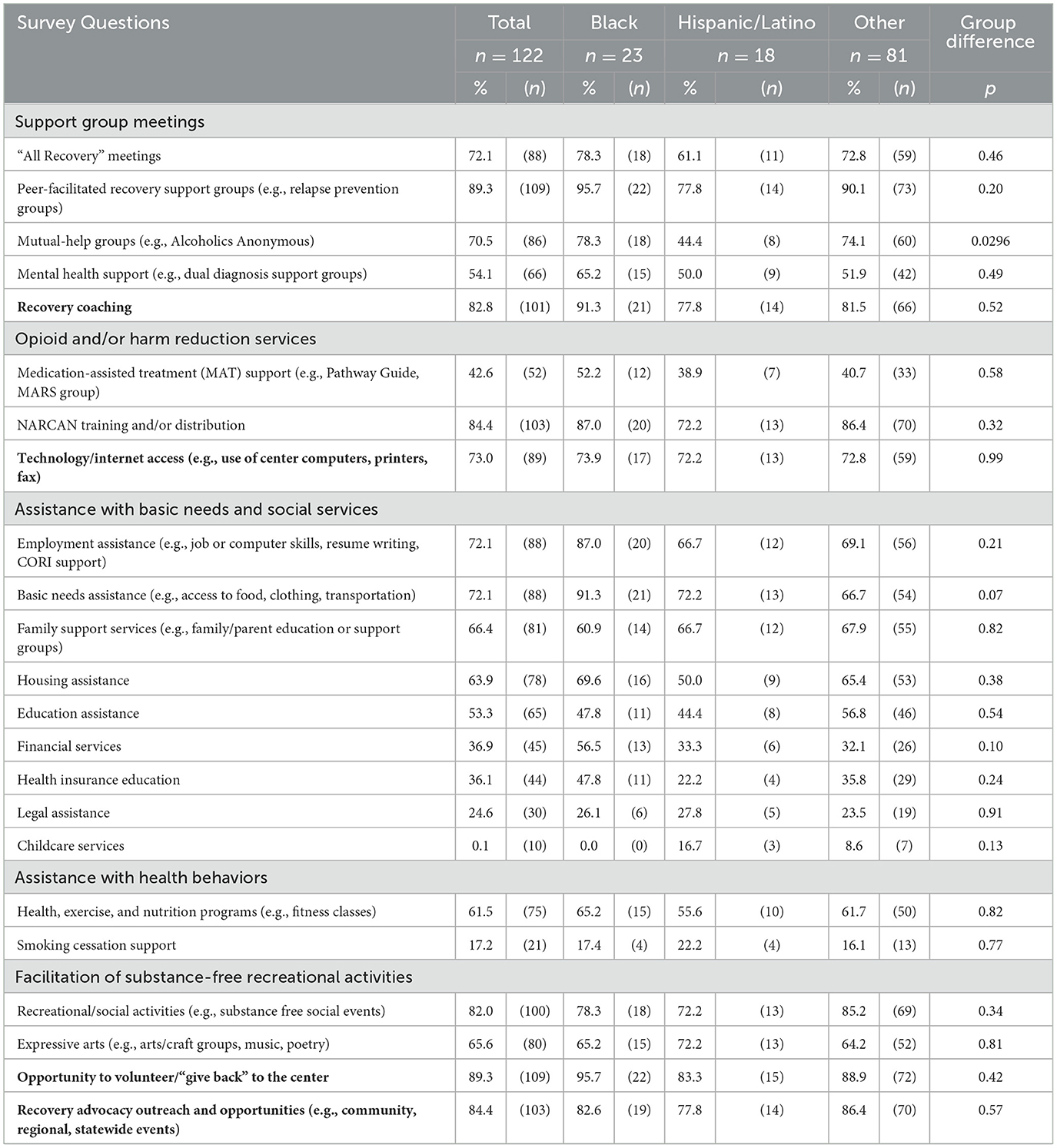
Table 1. RCC logistics, footprints, model of care, and demographics across RCCs that serve different communities.
For RCC services (Table 2), RCC directors or delegates used a checklist (yes/no) to indicate the services their RCC provided. This checklist was derived from earlier research on RCCs located in the northeast of the U.S. (25, 35, 36). To describe the degree to which RCCs interacted with other organizations, they were asked: “Does your RCC currently have linkages to any of the following?”, and then were provided with checkboxes for a variety of types of organizations (as shown in Table 3).
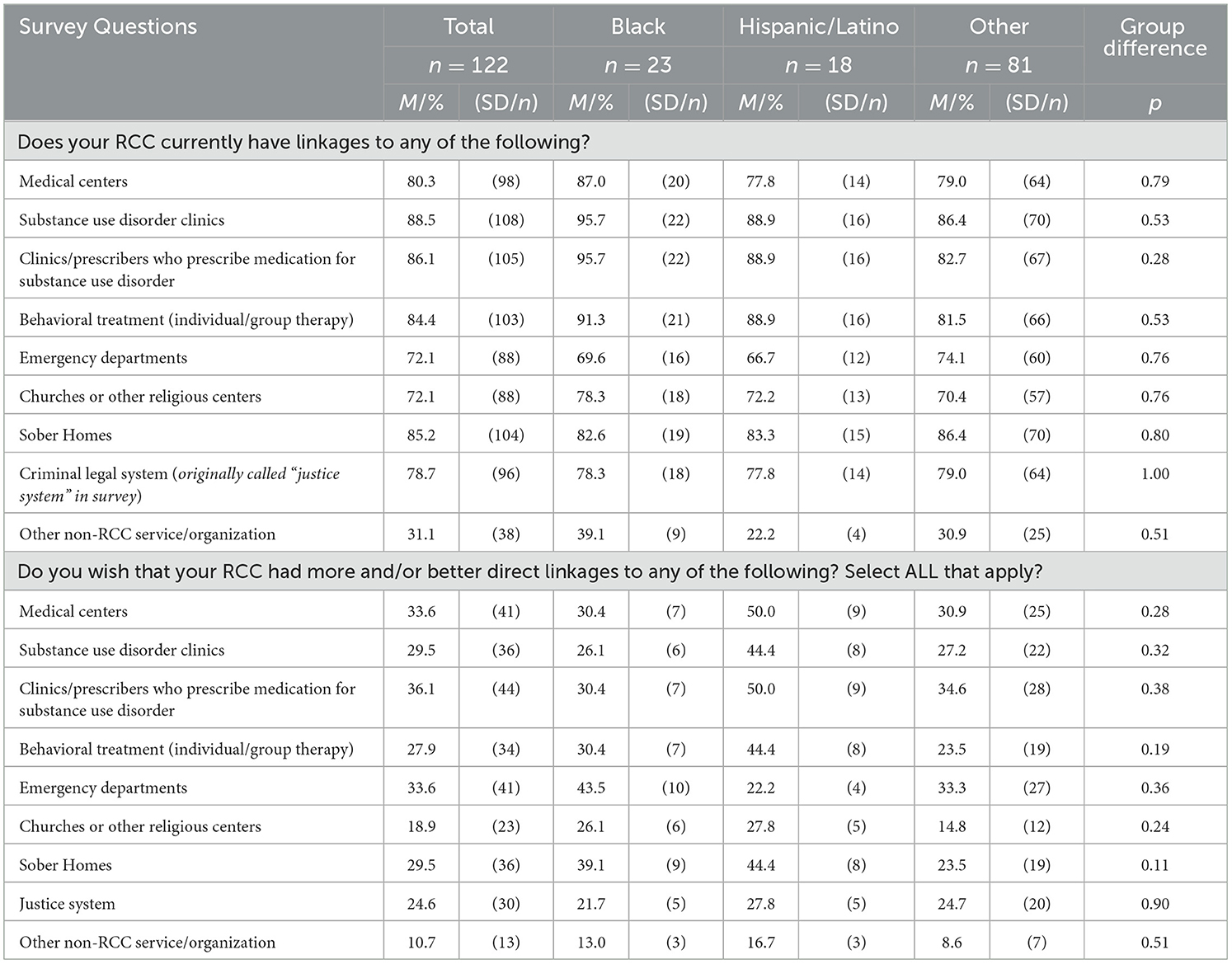
Table 3. Organizations and systems RCCs connect with in fulfilling their mission across RCCs serving different communities.
RCC directors were also asked to provide feedback on their RCC's approach to SUD medication treatment in general (Table 4). We asked: “How open is your RCC to medication-assisted treatment?” with answer options rated on a 1–5 scale, ranging from 1 (“not open at all”) to 5 (“extremely open”). We then asked RCC directors and delegates to indicate in a checklist how they handled MOUDs specifically (“How does your RCC handle medications for opioid use disorder? Select ALL that apply”; response options are shown in Table 4).
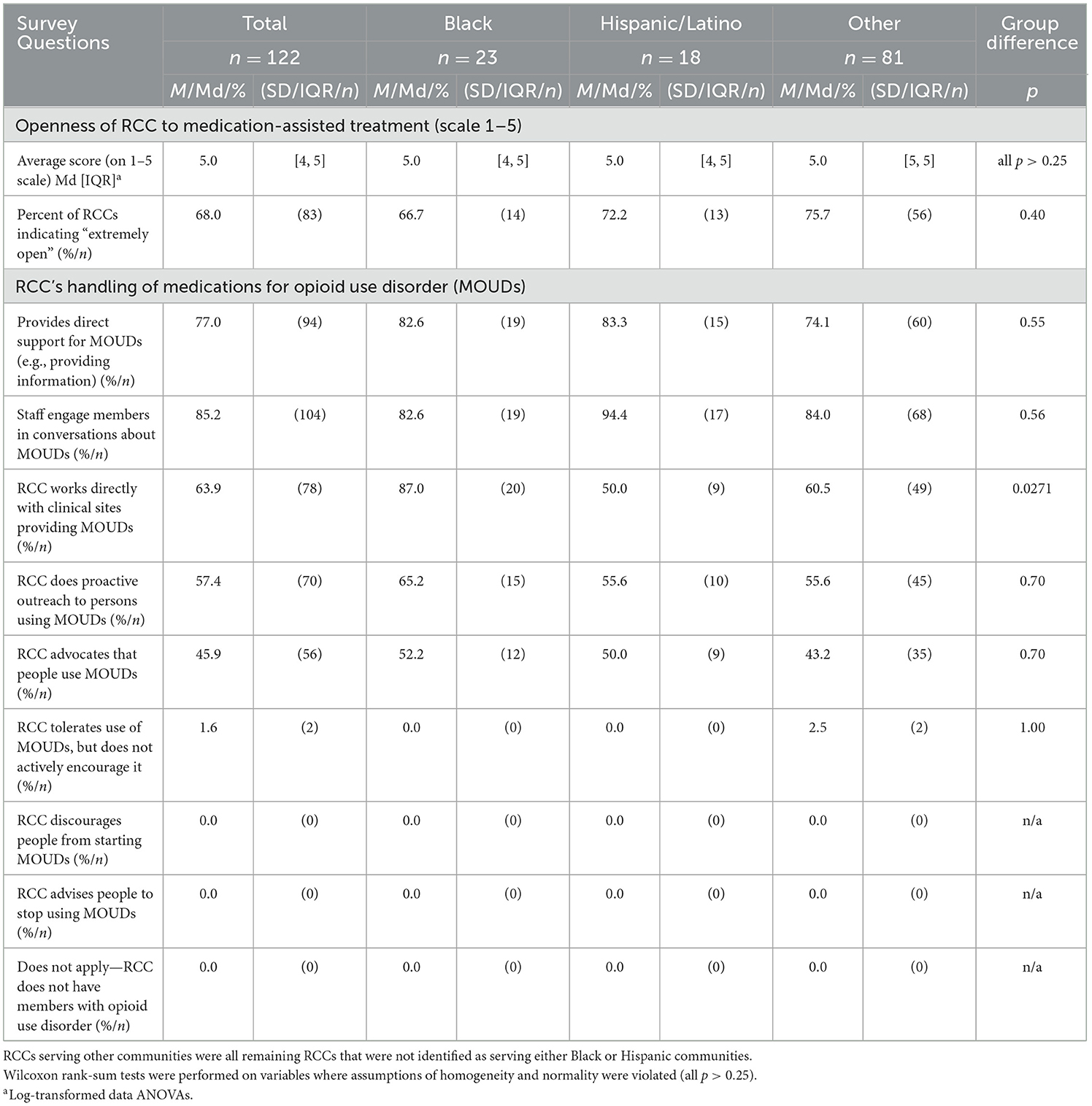
Table 4. RCC attitudes toward medication assisted recovery across RCCs serving different communities.
Analytic strategy
To compare RCCs serving primarily Black (n = 23) vs. Hispanic/Latino (n = 18) vs. other communities (n = 81), we calculated descriptive statistics [i.e., means (M) with standard deviations (SD) for continuous variables; medians (Md) with interquartile ranges [IQR] for continuous variables with substantial skew; and percentages (%) with sample sizes (n) for categorical data (yes/no)] for survey items. For variables where RCC directors or their delegates estimated percentages for their RCC (i.e., RCC member percentages in different age, gender, race, and ethnicity categories), we treated the percentage estimates provided by RCCs as continuous variables. For continuous and count variables, we conducted group comparison tests via one-way analysis of variance (ANOVA); where necessary, we log-transformed data to better meet the assumptions of homogeneity of variance and normality (37, 38). For continuous variables with substantial skew even after log-transformation [e.g., “Other” genders, American Indian or Alaskan Native race, Asian race, and Native Hawaiian or Pacific Islander race, as well as for the variable Openness of RCC to medication-assisted treatment (scale 1–5)], we used non-parametric Wilcoxon rank-sum tests to test pairwise group differences (for details, see Supplementary material). For categorical variables, we used chi-square tests to compare RCCs serving primarily Black, Hispanic/Latino, or other communities. Due to the exploratory nature of these analyses, we did not adjust the group effect tests for multiple comparisons. For group difference tests that showed overall group differences at a significance level of p < 0.25 (a common threshold in screening for univariate predictors) (39), we conducted follow-up pairwise comparisons to further evaluate specific group differences (40, 41). We adjusted the pairwise group differences for multiple comparisons using the Holm-Bonferroni procedure at a significance level of α = 0.05 to detect differences (42).
Results
Engagement of Black and Hispanic/Latino individuals in RCC participation
To descriptively assess equity in RCC engagement, we compared the proportion of Black and Hispanic/Latino participants reported by RCCs to the racial/ethnic composition of the communities in which the RCCs are located. While not a causal analysis, this comparison offers preliminary insight into whether RCCs are reaching racially minoritized populations at or above expected levels based on local demographics. RCCs serving Black and Hispanic/Latino communities successfully engaged Black and Hispanic/Latino individuals in recovery support services. That is, of RCCs serving Black communities, the median [IQR] percentage of RCC participants who were Black was 45% [30–63%], compared to an average of 51% (SD = 21) of Black people living in the surrounding zip code. Similarly, in RCCs serving Hispanic/Latino communities, the percentage of RCC participants who were Hispanic was 50% [28–60%], compared to 56.8% (SD = 16.6) Hispanic/Latino people living in the surrounding zip code. Paired t-tests of these differences (i.e., RCC participant racial/ethnic prevalence vs. local zip code racial/ethnic prevalence) were not significant (p = 0.18) for RCCs serving Black communities, p = 0.06 for RCCs serving Hispanic/Latino communities).
Differences in other demographics
A significant difference was found in the number of years RCCs had been in operation across the groups (p = 0.02, based on an ANOVA of log-transformed data). Median [IQR] years in operation were 6 (4–17) for RCCs serving Black communities, 7 (2–11) for RCCs serving Hispanic/Latino communities, and 4.8 [2.5–9.5] for RCCs serving other communities, respectively. Although no pairwise comparisons reached statistical significance after adjustment, the comparison between RCCs serving Black communities and those serving other communities approached significance and accounted for most of the observed group-level difference (p = 0.08).
Differences in services and service model
Across 52 characteristics, including 23 possible services offered (Table 2), 18 possible linkages provided (Table 3), and 11 descriptors of how RCCs handled medication assisted recovery (Table 4), only two statistically significant overall group differences emerged between RCCs serving Black, Hispanic/Latino, and other communities. Of note, given an alpha of 0.05, 2–3 significant differences (i.e., 5%) would be expected to emerge by chance. Importantly, RCCs in this sample demonstrate an all-encompassing approach to supporting long-term recovery. A notable number of RCCs reported providing support for addictions apart from substance use (69.7%; Table 1) and mental health problems (67.2%; Table 1). Where the literature has demonstrated that co-morbidities often occur in SUD and other addictions, such as mental health problems (43), RCCs provide resources that address all aspects of recovery, suggesting a comprehensive approach to acknowledging and supporting the many facets and complexities of sustaining recovery.
The two differences observed were in the offering of 12-step groups (p = 0.0296; Table 2) and linkages to clinics that provide MOUDs (p = 0.0271; Table 4). Offering 12-step mutual aid groups (e.g., Alcoholics Anonymous) was least common in RCCs serving Hispanic/Latino communities (44.4%) and considerably more common among RCCs serving Black communities (78.3%; p = 0.05) and other communities (74.1%; p = 0.04); there was no difference in the prevalence of offering 12-step groups between RCCs serving Black or other communities (p = 0.69). In terms of linkage to medication, direct collaboration with clinical sites providing MOUDs was most common in RCCs serving Black communities (87.0%) compared to RCCs serving Hispanic/Latino communities (50.0%; p = 0.03) or other communities (60.5%; p = 0.04); there was no difference in the prevalence of direct collaboration with clinical sites providing MOUDs between RCCs serving Hispanic/Latino or other communities (p = 0.42).
Exploratory post-hoc analysis
Exploratory Holm-Bonferroni adjusted post-hoc analysis, triggered by group difference tests with a p < 0.25, showed additional differences in aiding with basic needs (Table 2) and social services (Table 3). Namely, although non-significant, RCCs serving Black communities demonstrated a greater ability to provide basic needs assistance (e.g., access to food, clothing, transportation; 91.3% of RCCs) compared to RCCs serving other communities (66.7% of RCCs; p = 0.06) and were more likely to provide financial services (56.5% for RCCs serving Black communities) compared RCCs serving other communities (32.1%; p = 0.06).
Lastly, while we were unable to detect any differences in the prevalence of current linkages between RCCs and other organizations and systems that RCCs connect with in fulfilling their mission (all p > 0.25; Table 3), there were two differences in the prevalence of RCC directors or their delegates who wished they had more and/or better direct linkages. Across all options for linkages except emergency departments, directors and delegates of RCCs serving Hispanic/Latino communities more frequently expressed a desire for expanded and improved linkages. Particularly, RCCs serving Hispanic/Latino communities were more likely to express a wish for more and better linkages to behavioral treatment (i.e., individual/group therapy; 44.4%) and sober homes (44.4%) compared to RCCs serving other communities (behavioral treatment: 23.5%, p = 0.0718; sober homes: 23.5%, p = 0.0718), with RCCs serving Black communities at intermediate prevalences that showed no difference to either of the other types of communities (all p > 0.10).
Discussion
In conducting this secondary data analysis examining RCCs in Black, Hispanic/Latino, and other communities, we found that while each RCC is unique, the overall service and support model in the RCCs included in this sample appears to be consistent across racial/ethnic community settings. This consistency includes their range of operation, model of care, services offered, connection and linkages to relevant systems and organizations, director openness, support, and engagement with participants utilizing MOUDs, regardless of demographic composition. RCCs have gained attention as a valuable recovery support service and community resource over the past two decades (44). Given that there are a limited number of RCCs, future research should further examine how RCCs serving specific racially minoritized individuals may be pivotal connections to lessen the gap between treatment and sustained recovery. RCCs operate in environments where racial disparities are commonly observed. However, within our sample, we do not see evidence of service and support disparities among RCCs serving Black, Hispanic/Latino, and other communities—an encouraging finding. Further research is needed to establish this.
We noted two specific differences in linkages between RCCs and other systems and organizations that support or work with people seeking or in recovery. The first was that mutual aid organization linkage was significantly lower at RCCs serving Hispanic/Latino communities than at RCCs serving either Black or other communities. This reflects a national trend in which Black individuals attend mutual-help groups at slightly higher rates than Hispanic/Latino individuals (45–47). The more encouraging second difference was that direct collaborations between RCCs with clinical sites providing MOUDs were most common in RCCs serving Black communities (87.0% of RCCs). As previously noted, structural inequities and racial biases within SUD treatment systems have led to lower treatment engagement by Black individuals; however, our results show that RCCs serving Black communities may be actively seeking connections with MOUD clinics, which may be a pivotal step to reducing disparities in treatment seeking behaviors. Further research is needed to explore how connections between community-oriented supports, such as RCCs, and evidence-based treatment approaches, including mutual-help groups and MOUD clinics, may enhance recovery stability beyond traditional treatment settings.
Another set of interesting observations was that RCCs serving Black communities tended to provide basic needs assistance and financial services more frequently than other communities. While these results were not statistically significant, they may indicate that RCCs might be particularly responsive to the needs of their surrounding communities due to their reliance on community-based staffing, including PRSS, and their community-oriented treatment model. Given the disparities in health insurance coverage and financial resources among Black communities (16, 17), RCCs may be more inclined to prioritize financial assistance and access-related services to effectively address these barriers. The provision of such services can have meaningful impacts on the lives of recipients by helping them meet their basic needs and reducing barriers to their ongoing recovery. For instance, the provision of transportation assistance may enable recipients to attend recovery-related services and activities or hold jobs; the provision of clothing assistance may enable recipients to start and keep jobs and enhance their sense of dignity and self-worth; the provision of childcare services can help recipients regain or keep custody of their children, provide greater flexibility in attending recovery-related activities, and increase their ability to work and pay rent (48). Future research should examine if this increased service assistance was provided in response to greater economic need in the specific local communities they serve or whether this may indicate an unmet need in RCCs serving other communities. More work is needed to quantify the numerous benefits of these supportive services in helping individuals in recovery build recovery capital and enable more RCCs to offer these services.
Notably, 19–36% of all RCCs expressed a desire for more and better linkages to existing systems and organizations, most commonly to medical centers, clinics/prescribers who prescribe medication for substance use disorders, and emergency departments. RCCs serving Hispanic/Latino communities were, furthermore, particularly interested in more and better linkages to behavioral treatment providers and sober homes. More work is needed to strengthen and increase these existing linkages while ensuring that the organizations and systems that are already linked offer language-compatible and culturally appropriate services for Hispanic/Latino individuals seeking or in recovery. A study on substance use treatment barriers among Latino, White, and Black participants with SUD found that, compared to White and Black individuals, Latinos expressed more pronounced narratives about attitudinal norm barriers tied to cultural factors and stigma, emphasizing the need for culturally informed services beyond Spanish language support (49). Substance use treatment providers and counselors must actively recognize how systemic racism shapes the institutions in which they operate and critically reflect on how their own racial identity may influence power dynamics in care delivery. By integrating ongoing cultural competency training, providers can develop a deeper understanding of the historical and structural inequities affecting racially minoritized communities, ensuring that care is culturally responsive and informed (15, 16).
In general, we found that the overall service model of RCCs varies little across racial/ethnic community settings. For example, we did not find that RCCs serving Black communities functioned drastically different in terms of services provided from RCCs serving Hispanic/Latino communities or RCCs serving other communities. RCCs serving Black, Hispanic/Latino, and other communities appeared to adhere to a model that offered a variety of recovery support services in addition to educational and social services and activities. Future research should incorporate acceptability measures to establish the perceived agreement and satisfaction of the RCC model across diverse racial and ethnic groups. High rates of racially minoritized individuals expect and experience racial discrimination and medical mistrust of traditional systems of substance use treatment leading to delayed and lower engagement in care (50). More research should be done to see if newer substance use treatment models like RCCs—rooted in community-oriented, socioeconomic care, and peer support—may support lower perceived and experienced racial discrimination, increasing acceptability and treatment outcomes (e.g., engagement and completion rates). Indeed, past research has highlighted the ability of PRSS to support low-income ethnic and racially minoritized individuals in their recovery journey in a community resource center (51). PRSS was able to help individuals in this setting who were interested in addressing their substance use by assisting them in overcoming barriers to care and by linking them to substance use treatment. Fifty-two percentage of individuals who were linked to treatment remained in treatment at the 30-day follow-up period (51). Additionally, PRSS has shown effectiveness in engaging individuals in harm-reduction services such as syringe exchange programs, which are important in reducing the potential for overdoses and infections (52) and are notably highlighted as an important service to help address substance use health disparities (12). Given this past research, which speaks to the potential of PRSS, and our findings demonstrating RCC engagement of marginalized communities, the RCC model indicates promise to be an important resource for long-term recovery support service. Additionally, while stigma might hinder marginalized populations from engaging in treatments like medications for SUD, previous studies have shown that RCCs are both welcoming to individuals taking medications and have connections with more formal healthcare settings, such as clinics that provide these medications (29). These findings suggest that RCCs provide promise for helping to overcome racial and ethnic disparities in SUD treatment and long-term recovery.
Limitations
This secondary data analysis was conducted using data that was collected in 2022. Since then, the number of RCCs in the United States has continued to increase (i.e., in 2022, our team was able to identify 198 RCCs nationwide, 122 of which participated in this survey; we have since then learned of 39 more RCCs, which is likely an underestimate of how many more RCCs have opened their doors since 2022). This means that not all existing RCCs nationwide were captured in the survey (29). Due to this growth, previously non-existent disparities within the RCC framework may have emerged. The significance of any group differences found need to be interpreted with caution: the number of variables we examined was high, which increases the risk of Type I error (false positives), especially given the number of p-values reported near the conventional threshold (p < 0.05). However, in this first study to examine potential racial/ethnic disparities in the context of RCCs, we aimed to include all possible leads ensuring that all differences identified could be examined for replicability in future studies. At the same time, the dataset was relatively small (n = 122), thereby providing limited statistical power to detect group differences, especially for comparisons between RCCs serving Black (n = 23) and Hispanic/Latino (n = 18) communities. Additionally, this survey assessed characteristics of RCCs through self-reporting from RCC directors or delegates, which may not capture the fullness of the RCC model, footprint, services, or linkages. Future studies should prioritize obtaining more objective or observational data on RCCs as the data collection infrastructure in RCCs develops.
This survey did not assess engagement in cultural activities held at RCCs, which may be an important factor for engaging Black and Hispanic/Latino communities (36). Lastly, the data were limited regarding the provision of harm reduction tools and information. This survey only asked about Narcan (naloxone) training and/or distribution; other services, such as the provision of clean syringes or fentanyl test strips, were not assessed. Future research should examine the ability of RCCs to support harm reduction approaches in a landscape of variably restrictive state legislations and community attitudes, which may illuminate different pathways and opportunities for reducing stigma around harm reduction and reducing harm in the community (53, 54).
Conclusion
Our results indicate that RCCs successfully engage Black and Hispanic/Latino people with their services and activities. This is an important contribution, given widespread racial/ethnic disparities in accessing and engaging with SUD treatment. These results strengthen the rationale for the current rapidly growing investment in RCCs and the services they offer, providing hope for closing currently existing gaps in providing SUD-related recovery support and care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the (patients/participants OR patients/participants legal guardian/next of kin) was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
DD: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Visualization. AF: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. AW: Investigation, Writing – review & editing. SH: Conceptualization, Data curation, Methodology, Writing – review & editing. LH: Conceptualization, Methodology, Writing – review & editing. MR: Investigation, Writing – review & editing. JJ: Writing – review & editing. JO: Conceptualization, Methodology, Writing – review & editing. AM: Conceptualization, Methodology, Writing – review & editing. VR: Conceptualization, Methodology, Writing – review & editing. PR: Conceptualization, Methodology, Writing – review & editing. PM: Conceptualization, Methodology, Writing – review & editing. BH: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by grants from the National Institute on Drug Abuse (R24 DA051988: PI Bettina B. Hoeppner; K02DA056613: PI Bettina B. Hoeppner; K01DA055768: PI Lauren A. Hoffman).
Acknowledgments
The authors would like to thank all the directors and staff of recovery community centers (RCCs) nationwide who made this study possible by answering our phone calls, assisting us in identifying RCCs, and completing the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1532488/full#supplementary-material
References
1. Drake J, Charles C, Bourgeois JW, Daniel ES, Kwende M. Exploring the impact of the opioid epidemic in Black and Hispanic communities in the United States. Drug Sci Policy Law. (2020) 6:428. doi: 10.1177/2050324520940428
2. Friedman J, Hansen H. Black and native overdose mortality overtook that of white individuals during the COVID-19 pandemic. JAMA Psychiatry. (2022) 79:379–81. doi: 10.1001/jamapsychiatry.2022.0004
3. Lee H, Singh GK. Racial and ethnic disparities in monthly trends in alcohol-induced mortality among US adults from January 2018 through December 2021. Am J Drug Alcohol Abuse. (2023) 49:450–7. doi: 10.1080/00952990.2023.2208728
4. Mowbray O, Purser G, Tennant E, Paseda O. Substance use related violent deaths among racial/ethnic groups in the United States. Addict Behav. (2022) 133:107384. doi: 10.1016/j.addbeh.2022.107384
5. Yunusa IA-O, Farhadi K, Karaye IM. Racial, ethnic, and regional disparities in cocaine-involved overdose deaths in the US, 1999-2020. J Racial Ethn Health Disparities. (2024) 11:441–50. doi: 10.1007/s40615-023-01531-7
6. U.S. Department of Health and Human Services. Overdose Prevention Strategy. (2024). Available online at: https://www.hhs.gov/overdose-prevention/background (accessed March 14, 2024).
7. Jordan A, Mathis M, Haeny A, Funaro M, Paltin D, Ransome Y. An evaluation of opioid use in black communities: a rapid review of the literature. Harv Rev Psychiatry. (2021) 292:108–30. doi: 10.1097/HRP.0000000000000285
8. Stahler GJ, Mennis J, Baron DA. Racial/ethnic disparities in the use of medications for opioid use disorder (MOUD) and their effects on residential drug treatment outcomes in the US. Drug Alcohol Depend. (2021) 226:108849. doi: 10.1016/j.drugalcdep.2021.108849
9. Stein BD, Dick AW, Sorbero M, Gordon AJ, Burns RM, Leslie DL, et al. A population-based examination of trends and disparities in medication treatment for opioid use disorders among medicaid enrollees. Subst Abus. (2018) 394:419–25. doi: 10.1080/08897077.2018.1449166
10. Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. (2019) 769:979–81. doi: 10.1001/jamapsychiatry.2019.0876
11. Stahler G, Mennis J. Treatment outcome disparities for opioid users: are there racial and ethnic differences in treatment completion across large US metropolitan areas? Drug Alcohol Depend. (2018) 190:170–8. doi: 10.1016/j.drugalcdep.2018.06.006
12. Farahmand P, Arshed A, Bradley Mark V. Systemic racism and substance use disorders. Psychiatr Ann. (2020) 50:494–8. doi: 10.3928/00485713-20201008-01
13. Acevedo A, Panas L, Garnick D, Acevedo-Garcia D, Miles J, Ritter G, et al. Disparities in the treatment of substance use disorders: Does where you live matter? J Behav Health Serv Res. (2018) 45:533–49. doi: 10.1007/s11414-018-9586-y
14. Netherland J, Hansen H. The war on drugs that wasn't: wasted whiteness, “dirty doctors,” and race in media coverage of prescription opioid misuse. Cult Med Psychiatry. (2016) 404:664–86. doi: 10.1007/s11013-016-9496-5
15. Nuriddin A, Mooney G, White AIR. Reckoning with histories of medical racism and violence in the USA. Lancet. (2020) 396:949–51. doi: 10.1016/S0140-6736(20)32032-8
16. Matsuzaka S, Knapp M. Anti-racism and substance use treatment: addiction does not discriminate, but do we? J Ethn Subst Abuse. (2020) 19:567–93. doi: 10.1080/15332640.2018.1548323
17. Saloner B, Lê Cook B. Blacks and hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Affairs. (2013) 311:135–45. doi: 10.1377/hlthaff.2011.0983
18. Cooper RL, MacMaster S, Rasch R. Racial differences in retention in residential substance abuse treatment: the impact on African American men. Res Social Work Prac. (2010) 202:183–90. doi: 10.1177/1049731509338936
19. Burlew K, McCuistian C, Szapocznik J. Racial/ethnic equity in substance use treatment research: the way forward. Addict Sci Clin Pract. (2021) 16:50. doi: 10.1186/s13722-021-00256-4
20. Kariisa M, Davis NL, Kumar S, Seth P, Mattson CL, Chowdhury F, et al. Vital signs: drug overdose deaths, by selected sociodemographic and social determinants of health characteristics–25 states and the District of Columbia, 2019–2020. MMWR Morb Mortal Wkly Rep. (2022) 71:940–7. doi: 10.15585/mmwr.mm7129e2
21. Substance Abuse and Mental Health Services Administration. The Opioid Crisis and the Black/African American Population: An Urgent Issue. Publication No. PEP20-Q15 05-02-001. Office of Behavioral Health Equity. Rockville, MD: Substance Abuse and Mental Health Services Administration (2020).
22. Substance Abuse and Mental Health Services Administration. The Opioid Crisis and the Hispanic/Latino Population an Urgent Issue. Publication No. PEP20-05-02-Q15 002. Office of Behavioral Health Equity. Rockville, MD: Substance Abuse and Mental Health Services Administration (2020).
23. Substance Abuse and Mental Health Services Administration. SAMHSA's Working Definition of Recovery. Rockville, MD: Substance Abuse and Mental Health Services Administration (2012).
24. Eddie D, Hoffman L, Vilsaint C, Abry A, Bergman B, Hoeppner B, et al. Lived experience in new models of care for substance use disorder: a systematic review of peer recovery support services and recovery coaching. Front Psychol. (2019) 10:1052. doi: 10.3389/fpsyg.2019.01052
25. Kelly JF, Stout RL, Jason LA, Fallah-Sohy N, Hoffman LA, Hoeppner BB. One-stop shopping for recovery: an investigation of participant characteristics and benefits derived from US recovery community centers. Alcohol Clin Exp Res. (2020) 443:711–21. doi: 10.1111/acer.14281
26. Jason LA, Salomon-Amend M, Guerrero M, Bobak TJ, O'Brien JF, Soto-Nevarez A. The emergence, role, and impact of recovery support services. Alcohol Res. (2021) 41:04. doi: 10.35946/arcr.v41.1.04
27. Haberle BJ, Conway S, Valentine P, Evans AC, White WL, Davidson L. The recovery community center: a new model for volunteer peer support to promote recovery. J Groups Addict Recover. (2014) 93:257–70. doi: 10.1080/1556035X.2014.940769
28. Recovery Research Institute. (n.d.). Recovery Community Centers. Boston, MA: Massachusetts General Hospital. Available online at: https://www.recoveryanswers.org/resource/recovery-community-centers/ (Accessed May 23, 2025).
29. Hoeppner BB, Simpson HV, Weerts C, Riggs MJ, Williamson AC, Finley-Abboud D, et al. A nationwide survey study of recovery community centers supporting people in recovery from substance use disorder. J Addict Med. (2024) 18:274–81. doi: 10.1097/ADM.0000000000001285
30. Best D, Laudet A. The Potential of Recovery Capital. (2010). Available online at: https://facesandvoicesofrecovery.org/wp-content/uploads/2019/06/The-Potential-of-Recovery-Capital.pdf (accessed March 14, 2024).
31. Narcotics Anonymous World Services, Inc. 2018 Narcotics Anonymous Membership Survey. (2018). Available online at: https://www.na.org/wp-content/uploads/2024/06/2301-Membership-Survey-English-2018-11-19.pdf (accessed October 2, 2024).
32. Alcoholics Anonymous (2022). 2022 Membership Survey. Available online at: https://www.aa.org/membership-survey-2022 (accessed October 2, 2024).
33. United States Census Bureau. QuickFacts United States. Washington, DC: U.S. Department of Commerce (n.d). Available online at: https://www.census.gov/quickfacts/fact/table/US/RHI225222 (Accessed January 16, 2024).
34. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The redcap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
35. Kelly JF, Fallah-Sohy N, Vilsaint C, Hoffman LA, Jason LA, Stout RL, et al. New kid on the block: an investigation of the physical, operational, personnel, and service characteristics of recovery community centers in the United States. J Subst Abuse Treat. (2020) 111:1–10. doi: 10.1016/j.jsat.2019.12.009
36. Kelly JF, Fallah-Sohy N, Cristello J, Stout RL, Jason LA, Hoeppner BB. Recovery community centers: characteristics of new attendees and longitudinal investigation of the predictors and effects of participation. J Subst Abuse Treat. (2021) 124:108287. doi: 10.1016/j.jsat.2021.108287
37. Zygmont CS. Managing the assumption of normality within the general linear model with small samples: guidelines for researchers regarding if, when and how. TQMP. (2023) 19:302–32. doi: 10.20982/tqmp.19.4.p302
38. Shatz I. Assumption-checking rather than (just) testing: the importance of visualization and effect size in statistical diagnostics. Behav Res Methods. (2024) 56:826–45. doi: 10.3758/s13428-023-02072-x
39. Nordstokke D, Stelnicki AM. Pairwise comparisons. In:Michalos AC, , editor. Encyclopedia of Quality of Life and Well-being Research. Dordrecht: Springer Netherlands (2014). p. 4575–6.
40. LibreTexts Statistics. Introduction to Pairwise Comparisons. (2021). Available online at: https://stats.libretexts.org/Workbench/PSYC_2200%3A_Elementary_Statistics_for_Behavioral_and_Social_Science_(Oja)_WITHOUT_UNITS/11%3A_BG_ANOVA/11.05%3A_Introduction_to_Pairwise_Comparisons (accessed November 10, 2024).
41. Hosmer DW, Lemeshow S. Model-building strategies and methods for logistic regression. In:Shewhart WA, Wilks, SS, , editor. Applied Logistic Regression. Hoboken, NJ: John Wiley & Sons, Inc (2000). p. 91–142.
42. Chen SY, Feng Z, Yi X. A general introduction to adjustment for multiple comparisons. J Thorac Dis. (2017) 9:1725–9. doi: 10.21037/jtd.2017.05.34
43. Lai HMX, Cleary M, Sitharthan T, Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: a systematic review and meta-analysis. Drug Alcohol Depend. (2015) 154:1–13. doi: 10.1016/j.drugalcdep.2015.05.031
44. Office of National Drug Control Policy. National Drug Control Strategy. (2022). Available online at: https://www.whitehouse.gov/wp-content/uploads/2022/04/National-Drug-Control-2022Strategy.pdf (accessed February 1, 2024).
45. Mauro PM, Kaur N, Askari MS, Keyes KM. Alcohol or drug self-help use among adults in the United States: age, period, and cohort effects between 2002 and 2018. Int J Ment Health Addict. (2023) 8:1–15. doi: 10.1007/s11469-023-01012-2
46. Zemore SE, Gilbert PA, Pinedo M, Tsutsumi S, McGeough B, Dickerson DL. Racial/ethnic disparities in mutual help group participation for substance use problems. Alcohol Res. (2021) 411:03. doi: 10.35946/arcr.v41.1.03
47. Zemore SE, Mericle AA, Martinez P, Bergman BG, Karriker-Jaffe KJ, Patterson D, et al. Disparities in alcoholics anonymous participation from 2000 to 2020 among U.S. residents with an alcohol use disorder in the national alcohol survey. J Stud Alcohol Drugs. (2024) 851:32–40. doi: 10.15288/jsad.23-00086
48. Jones AE, Walters JE, Brown AR. Over the hills and through the hollers: how one program is assisting residents of appalachian with opioid use recovery. J Appalach Health. (2023) 43:71–86. doi: 10.13023/jah.0403.05
49. Pinedo M, Zemore S, Rogers S. Understanding barriers to specialty substance abuse treatment among latinos. J Subst Abuse Treat. (2018) 94:1–8. doi: 10.1016/j.jsat.2018.08.004
50. Hall OT, Jordan A, Teater J, Dixon-Shambley K, McKiever ME, Baek M, et al. Experiences of racial discrimination in the medical setting and associations with medical mistrust and expectations of care among black patients seeking addiction treatment. J Subst Abuse Treat. (2022) 133:108551. doi: 10.1016/j.jsat.2021.108551
51. Kleinman MB, Doran K, Felton JW, Satinsky EN, Dean D, Bradley V, et al. Implementing a peer recovery coach model to reach low-income, minority individuals not engaged in substance use treatment. Subst Abus. (2021) 42:726–34. doi: 10.1080/08897077.2020.1846663
52. Ashford RD, Curtis B, Brown AM. Peer-delivered harm reduction and recovery support services: Initial evaluation from a hybrid recovery community drop-in center and syringe exchange program. Harm Reduct J. (2018) 15:52. doi: 10.1186/s12954-018-0258-2
53. Ramprashad A, Burnett GM, Welsh C. Harm reduction: not dirty words any more. Psychiatr Clin North Am. (2022) 45:529–46. doi: 10.1016/j.psc.2022.04.005
54. ASTHO. Legal Mapping of Harm Reduction Laws and Overdose Prevention Center Legislation. (2023). Available online at: https://www.astho.org/globalassets/report/legal-mapping-of-harm-reduction-laws-and-overdose-prevention-center-legislation.pdf (accessed July 2, 2024).
Keywords: recovery, recovery community centers, treatment models, disparities (health racial), community recovery capital
Citation: DeCristofaro D, Futter A, Williamson A, Hoeppner SS, Hoffman LA, Riggs MJ, Joseph J, Ojeda J, Mericle AA, Rao V, Rutherford PX, McCarthy P and Hoeppner BB (2025) Comparing recovery community centers (RCCs) serving Black, Hispanic/Latino, and other communities: an exploratory secondary data analysis of a nationwide survey of RCC directors. Front. Public Health 13:1532488. doi: 10.3389/fpubh.2025.1532488
Received: 22 November 2024; Accepted: 09 June 2025;
Published: 02 July 2025.
Edited by:
Susan M. Snyder, Georgia State University, United StatesReviewed by:
Olaniyi Olayinka, University of Texas Health Science Center at Houston, United StatesSarel Ohayon, Bar-Ilan University, Israel
Corinne A. Beaugard, Boston Medical Center, United States
Nicholas Guenzel, University of Nebraska Medical Center, United States
Copyright © 2025 DeCristofaro, Futter, Williamson, Hoeppner, Hoffman, Riggs, Joseph, Ojeda, Mericle, Rao, Rutherford, McCarthy and Hoeppner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bettina B. Hoeppner, YmhvZXBwbmVyQG1naC5oYXJ2YXJkLmVkdQ==
 Diadora DeCristofaro
Diadora DeCristofaro Allison Futter
Allison Futter Alivia Williamson
Alivia Williamson Susanne S. Hoeppner
Susanne S. Hoeppner Lauren A. Hoffman
Lauren A. Hoffman Marion J. Riggs2
Marion J. Riggs2 Amy A. Mericle
Amy A. Mericle Vinod Rao
Vinod Rao Philip X. Rutherford
Philip X. Rutherford Bettina B. Hoeppner
Bettina B. Hoeppner