- 1Shandong Academy of Occupational Health and Occupational Medicine, Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan, China
- 2Shandong Center for Disease Control and Prevention, Jinan, China
- 3Harbin Second Hospital, Harbin, China
Objective: Numerous studies have explored the correlation between dietary patterns and the risk of hypertension, yet the findings have remained indeterminate. We performed a meta-analysis to evaluate how various dietary patterns relate to hypertension risk in the Chinese population.
Methods: Relevant articles published from 1 January 2004 to 14 March 2024 in five databases (PubMed, Scopus, Web of Science, CNKI, and VIP) were searched. Fixed or random-effects models were employed to estimate the multivariable-adjusted odds ratios (ORs) and 95% confidence intervals (CIs) comparing the highest and lowest categories of dietary patterns.
Results: In total, 22 articles were incorporated into the meta-analysis. The pooled results indicated a reduced likelihood for hypertension in the highest compared to the lowest category of the traditional southern Chinese pattern (OR = 0.95, 95% CI: 0.92–0.97, p < 0.001). In addition, compared to the lowest category of fruit and dairy pattern, the risk of the highest category had a 25% reduction in hypertension risk (OR = 0.75, 95% CI: 0.64–0.89, p = 0.001). Nevertheless, there was no significant correlation between the animal food pattern and the odds of hypertension (OR = 1.06, 95% CI: 0.98–1.15, p = 0.171).
Conclusion: The traditional southern Chinese pattern as well as the fruit and dairy pattern was a protective factor for hypertension. High-quality, large-scale studies are needed to confirm the findings of the current meta-analysis further.
1 Introduction
Hypertension (HTN) is one of the most prevalent chronic diseases and one of the principal causes of public health issues, leading to a huge healthcare burden worldwide (1). Cardiovascular disease, chronic kidney disease, and cognitive impairment are common complications of HTN (2–4). According to the World Health Organization, approximately 1.28 billion adults aged 30–79 years worldwide are afflicted with HTN in 2023, with less than half (42%) receiving a diagnosis and treatment (5). The prevalence and overall burden of HTN are increasing on a global scale, particularly in low- and middle-income nations (6). Data from the China Chronic Disease and Risk Factor Surveillance indicates that 27.5% of Chinese adults are affected by HTN, with low rates of awareness and treatment among those diagnosed (7).
It is widely recognized that HTN is subject to a combination of genetic susceptibility and environmental factors (8). Diverse non-pharmacological strategies have been proposed to prevent and control HTN, such as weight reduction, healthy eating patterns, moderate alcohol intake, exercise enhancement, dietary sodium restriction and potassium supplementation (9). Numerous studies have shown that the intake of individual nutrients or foods, such as sodium (10), lycopene (11), and soy (12), are strongly associated with lower blood pressure. However, there are interactions among different foods or nutrients, and a single evaluation of the health effect of nutrients or a specific food cannot adequately and realistically reflect the comprehensive impact of the overall dietary situation on human health (13). Therefore, dietary pattern, which is a combination of multiple foods, is regarded as a more accurate indicator of overall food consumption and nutritional condition. In fact, the Dietary Approaches to Stop Hypertension (DASH) diet has been demonstrated to be efficacious in reducing the risk of HTN and has been proposed for HTN management (14).
As a result of rapid economic development, the dietary pattern of Chinese adults has changed significantly, as evidenced by a decrease in the consumption of vegetables and cereals, an increase in the consumption of animal foods (of which pork dominates), and a slight increase in the consumption of eggs, fish, and dairy products (15). In recent years, scholars in China have paid increasing attention to the correlation between dietary patterns and the likelihood of HTN (16–19). Nevertheless, the findings from these studies have shown a lack of consistency. Therefore, we carried out a revised meta-analysis of observational studies to provide epidemiological evidence on how dietary patterns relate to the risk of HTN.
2 Materials and methods
2.1 Searching strategy
This article followed the PRISMA Standard guidelines (20). An exhaustive literature retrieval was undertaken through PubMed, Scopus, Web of Science, CNKI, and VIP database from 1 January 2004 to 14 March 2024. The subsequent key words and medical subject headings were implemented during the search: (diet pattern OR dietary pattern OR dietary patterns OR food pattern OR food patterns OR eating pattern OR eating patterns) AND (hypertension OR high blood pressure OR high blood pressures) AND (adults OR adult) AND (Chinese OR China). What’s more, we conducted a comprehensive evaluation of the reference lists of pertinent studies in order to identify additional studies.
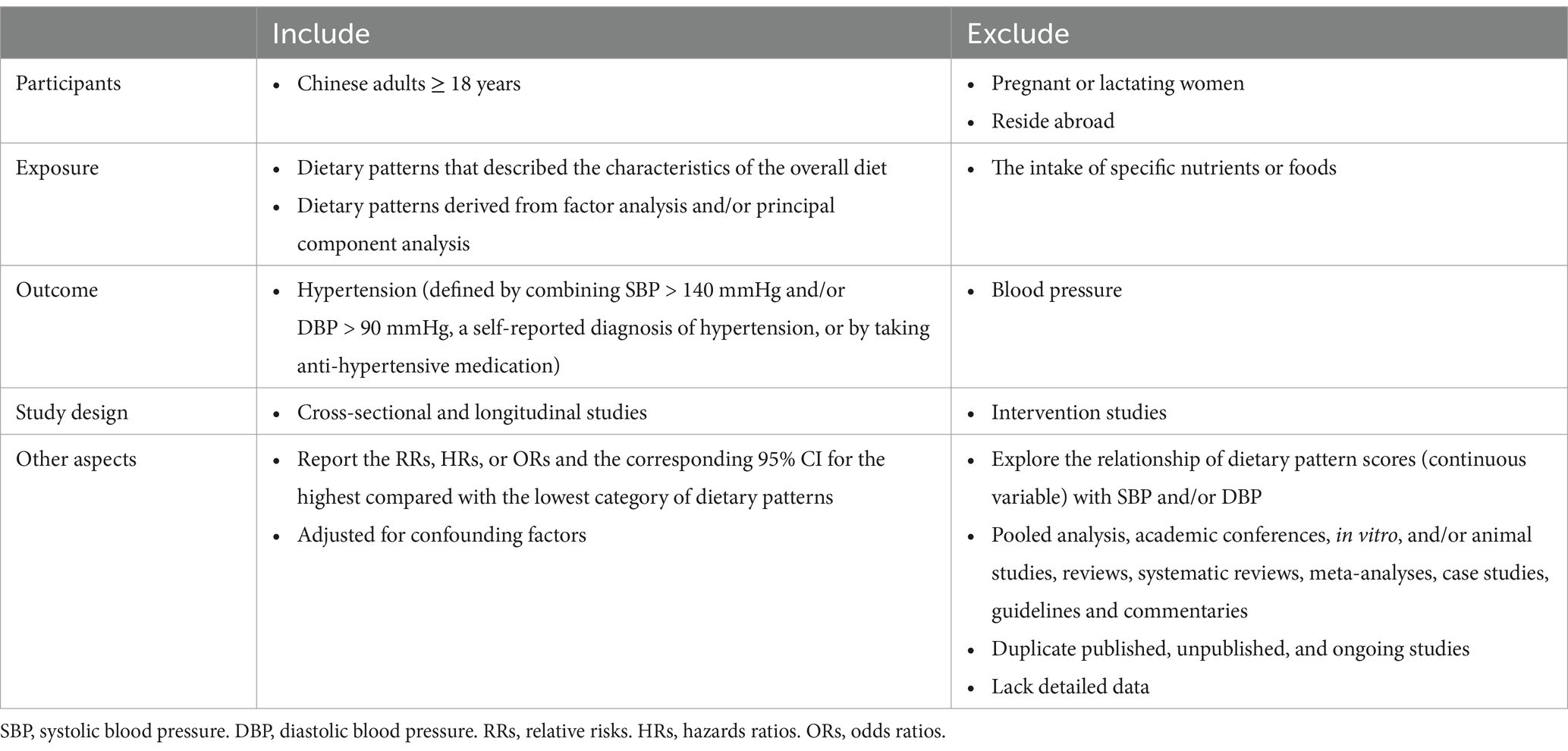
2.2 Eligibility criteria
Articles that were in the original report and met the criteria in Table 1 were eligible for inclusion the meta-analysis. To minimize error, only the dietary patterns with similar factor loadings of foods were selected.
2.3 Data extraction
Three researchers autonomously reviewed the literature, gathered the data, and verified it for accuracy. In case of discrepancies, a consensus should be reached through consultation with a fourth party. The subsequent information was extracted for each specified study: first author’s surname, publication year, study design, number of participants, characteristics of population, diet assessment method, dietary patterns identified and potential confounders adjusted in analysis. With respect to multiple estimates, those with adjustment for the most confounding factors were chosen.
2.4 Quality assessment
The quality of the identified studies were evaluated using the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (21). The evaluation tool comprises 14 criteria of equal weight, resulting in a maximum of fourteen points being assigned to each study. A score below 7 implied a high risk of bias, while a score between 7 and 10 suggested a moderate risk, and a score of 11–14 was deemed as low risk.
2.5 Statistical analysis
To assess HTN risk in the highest compared to the lowest category of the traditional southern Chinese pattern, the fruit and dairy pattern and the animal food pattern, we implemented this meta-analysis. The I2 and Q statistic were employed to determine statistical heterogeneity (22). I2 ≤ 50% and p > 0.10 suggested no heterogeneity among studies, and a fixed-effects model (Mantel–Haenszel method) was employed. Conversely, a random-effects model (DerSimonian and Laird method) was utilized (23). Multivariable adjusted odds ratios (ORs) with 95% confidence intervals (CIs) from each study were weighted and combined to calculate the summary OR and its 95% CI. We further carried out subgroup analysis based on study design (cross-sectional and cohort), sample size (≥ 5,000 and < 5,000), and with or without adjustment for several confounders to assess whether the differences affected our study conclusions. The robustness of the results was demonstrated by leave-one-out sensitivity analysis. Egger’s test, Begg’s test, and funnel plots were implemented to evaluate publication bias (24, 25). If substantial publication bias was identified, the trim-and-fill method was implemented to mitigate it (26). All statistical analyses were conducted with STATA version 17.0 (StataCorp LLC, College Station, TX 77845, USA). All p values were two-tailed, and p values < 0.05 were deemed as statistically significant, except where otherwise specified.
3 Results
3.1 Study selection
After a primary search, we screened 1,966 articles in total, of which 304 duplicates were deleted. Then, we eliminated 1,581 articles by going through the titles and abstracts whose study population, topic, or outcomes were deemed irrelevant. We excluded 59 articles after performing a thorough review of the remaining 81. Ultimately, 22 articles were eligible for inclusion in this meta-analysis. The flowchart of the stu2dy selection procedure is illustrated in Figure 1.
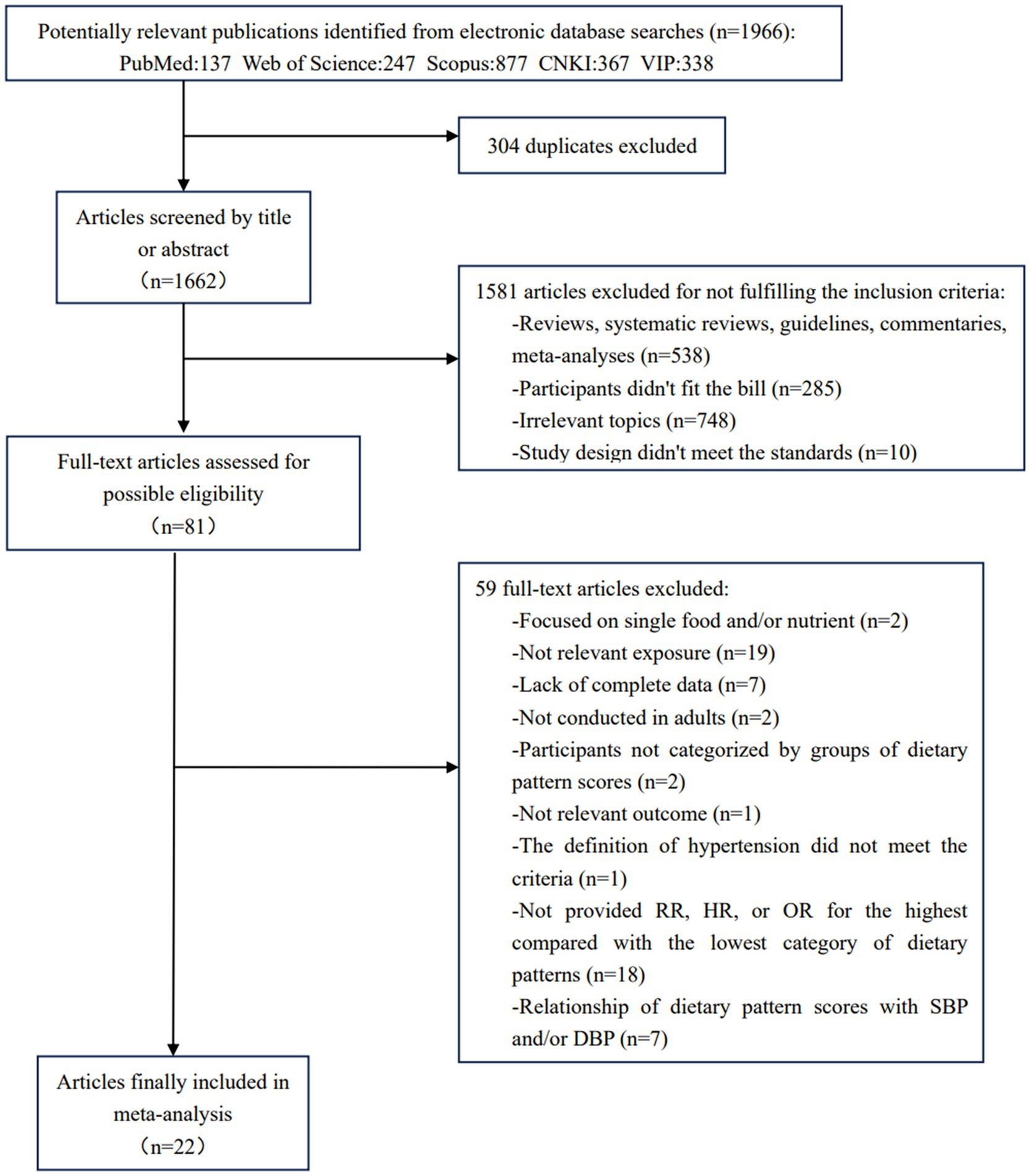
Figure 1. Flow chart of study selection. PubMed, Public Medicine. CNKI, China national knowledge infrastructure. VIP, VIP Database for Chinese Technical Periodicals. RR, relative risk. HR, hazard ratio. OR, odds ratio. SBP, systolic blood pressure. DBP, diastolic blood pressure.
3.2 Study characteristics
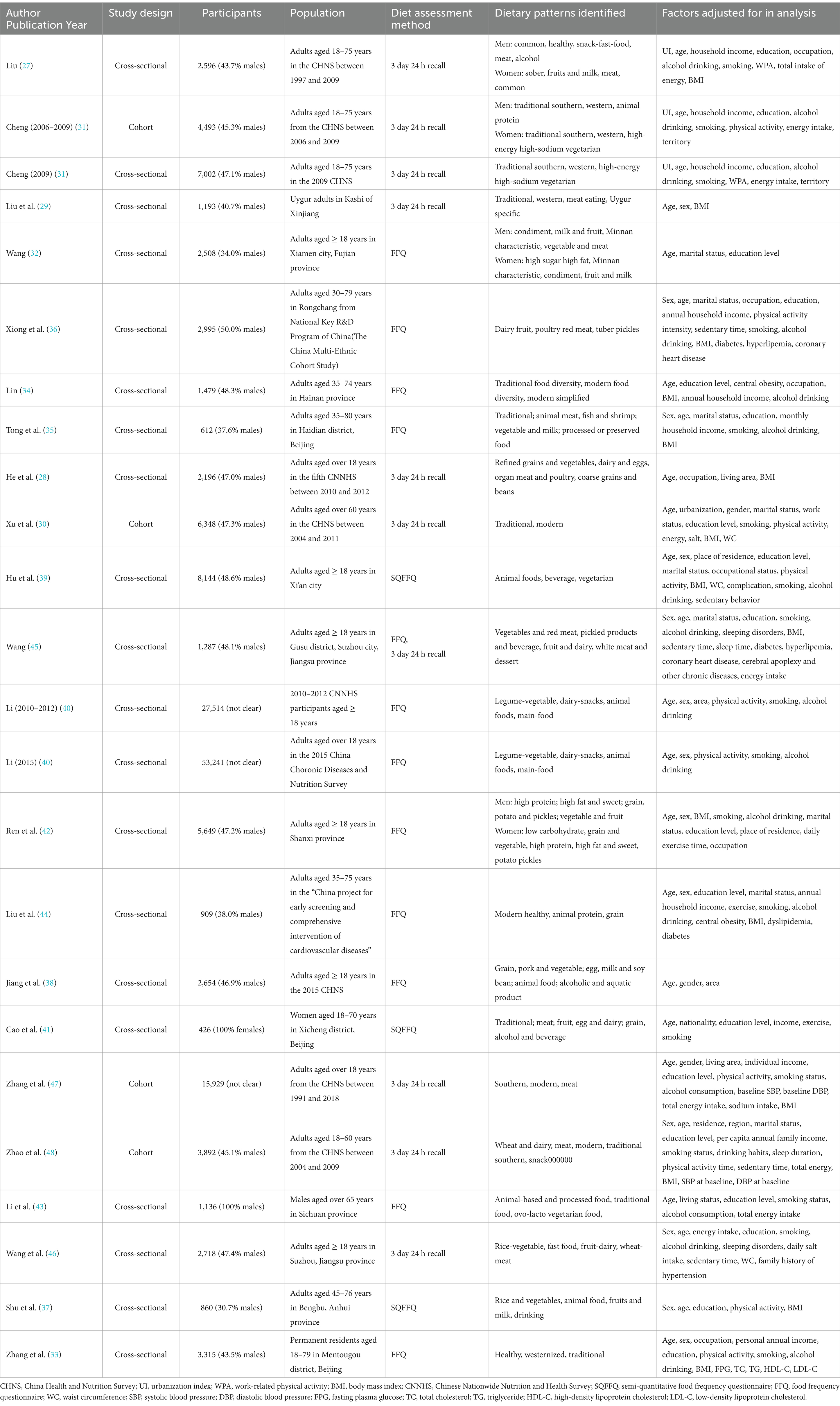
The features of the identified 22 articles (27–48) are depicted in Table 2. Among them, one article (40) reported the results of two cross-sectional studies. Another article (31) conducted both a cross-sectional study and a cohort study. Consequently, the present meta-analysis comprised 20 cross-sectional studies (27–29, 31–46) and 4 longitudinal studies (30, 31, 47, 48). The papers were released from 2011 to 2023. Of these, five articles (27, 28, 31, 32, 42) analyzed the relationship between HTN and dietary patterns in gender-specific populations, and the remaining 17 articles (29, 30, 33–41, 43–48) examined the general population. The sample sizes of these investigations varied from 426 to 53,241. Dietary data were collected using a 3-day 24-h dietary review in 9 articles (27–31, 45–48), a food frequency questionnaire in 11 articles (32–36, 38, 40, 42–45), and a semi-quantitative food frequency questionnaire in 3 articles (37, 39, 41).
3.3 Quality assessment
All four of the included cohort studies were found to have high methodological quality (Table 3). By contrast, the remaining 20 cross-sectional studies were classified as having a medium risk of bias. The absence of temporal separation between exposures and outcomes was the main cause of bias risk in the cross-sectional researches.
3.4 Traditional southern Chinese pattern and hypertension
Of the 24 studies, 13 identified the ‘traditional southern Chinese diet’ as a dietary pattern; 3 of them were longitudinal studies (30, 31, 47) and the remaining 10 were cross-sectional studies (27, 28, 31, 34, 35, 37, 38, 41, 45, 46). Although this dietary pattern had been defined differently in different studies, in general, the traditional southern Chinese pattern was distinguished by substantial consumption of rice and vegetables, as well as moderate amounts of animal foods, especially pork. The forest plot in Figure 2A displays the risk of HTN in individuals with the highest category of this dietary pattern compared to the lowest category. A fixed-effects model was employed for data analysis, as no significant heterogeneity was observed (I2 = 10.7%, p = 0.329). The combined outcome demonstrated that greater adherence to traditional southern Chinese pattern was associated with a lower risk of HTN (OR = 0.95, 95% CI: 0.92–0.97, p < 0.001).
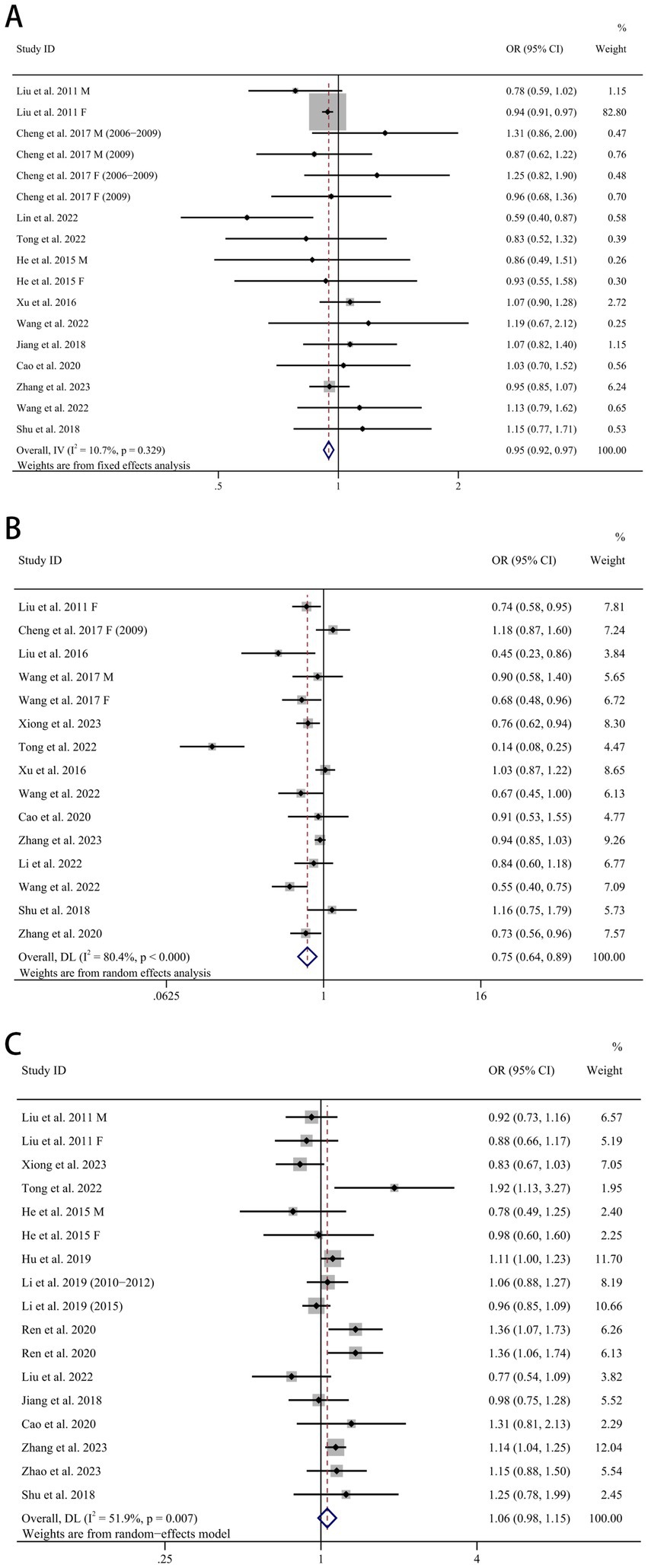
Figure 2. Forest plots of dietary patterns and hypertension. (A) Chinese traditional southern dietary pattern and hypertension, (B) fruit and dairy dietary pattern and hypertension, (C) animal food dietary pattern and hypertension. OR, odds ratio. CI, confidence interval. M, male. F, female.
3.5 Fruit and dairy pattern and hypertension
Of the 24 studies, 14 identified the ‘fruit and dairy pattern’ as a dietary pattern; 2 of them were longitudinal studies (30, 47) and the remaining 12 were cross-sectional studies (27, 29, 31–33, 35–37, 41, 43, 45, 46). The fruit and dairy pattern tended to be highly loaded with fruit, milk and dairy products. A significantly reduced risk of HTN in the highest compared to the lowest category of the fruit and dairy pattern was apparent in Figure 2B (OR = 0.75, 95% CI: 0.64–0.89, p = 0.001), despite the considerable heterogeneity (I2 = 80.4%, p < 0.001). A random-effects model was implemented to integrate all investigations.
3.6 Animal food pattern and hypertension
Of the 24 studies, 14 identified the ‘animal food pattern’ as a dietary pattern; 2 of them were longitudinal studies (47, 48) and the remaining 12 were cross-sectional studies (27, 28, 35–42, 44). The animal food pattern was characterized to have high factor loadings for foods including pork and other livestock meat, poultry, animal organs, aquatic products/seafood, processed and cooked meat and eggs. The meta-analysis found no relationship between animal food pattern and HTN (OR = 1.06, 95% CI: 0.98, 1.15, p = 0.171) (Figure 2C). The random-effects model was employed to evaluate the data from these investigations due to the substantial heterogeneity (I2 = 51.9%, p = 0.007).
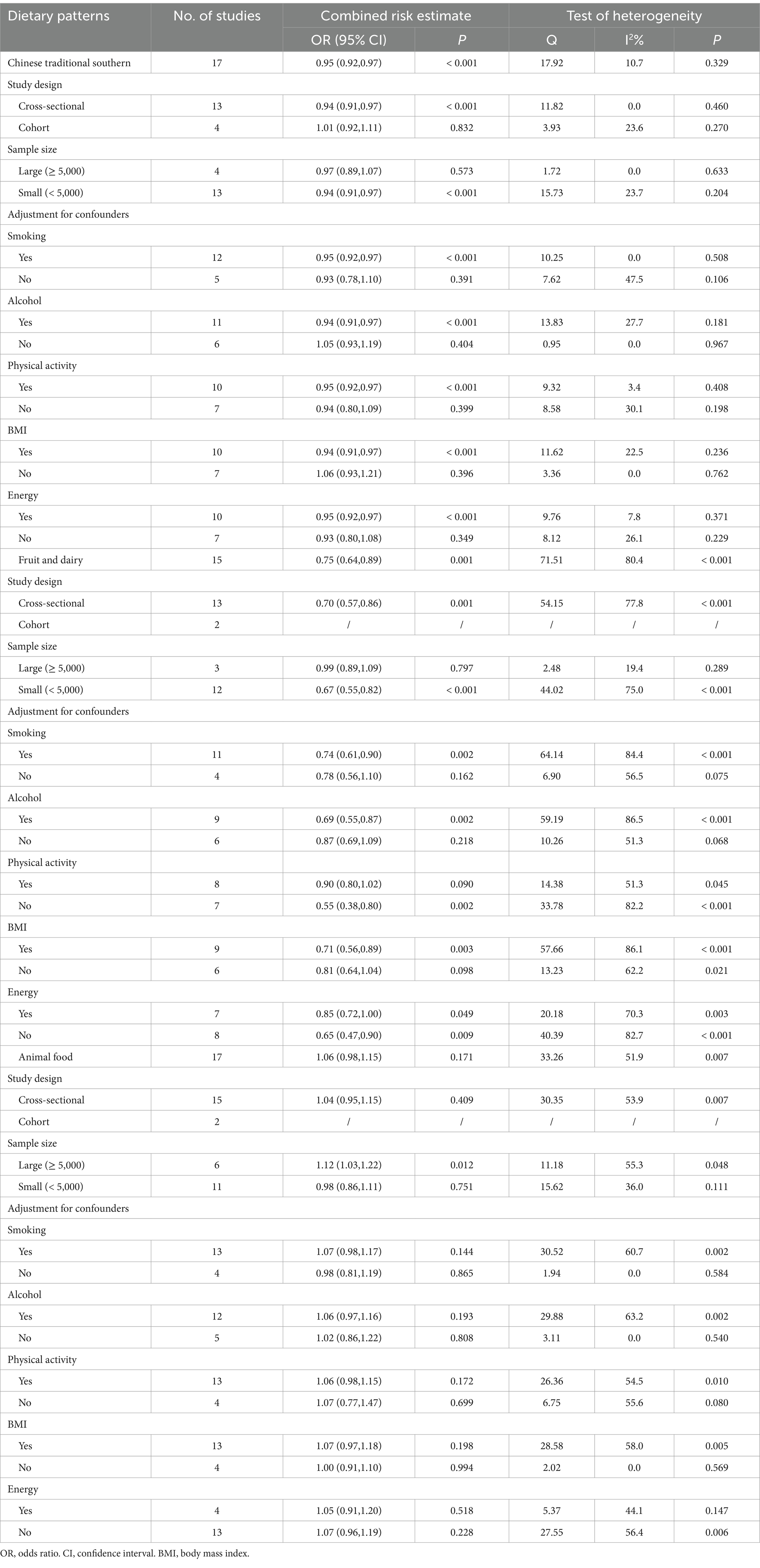
3.7 Subgroup analysis
A subgroup analysis was carried out in order to further explore the correlation among dietary patterns and HTN risk (Table 4). We found that dietary patterns and HTN were influenced by study design, sample size, and whether or not to adjust for multiple confounders. The negative association of the traditional southern Chinese pattern with HTN was evident in studies with cross-sectional designs, small sample sizes, and corrections for smoking, alcohol, physical activity, body mass index (BMI), or energy. The correlation between fruit and dairy pattern and HTN was more pronounced in studies with cross-sectional designs, small sample sizes, and corrections for smoking, alcohol, and BMI, but not for physical activity. In addition, we discovered a substantial positive correlation between animal food pattern and HTN in studies with a large sample size. As the impact of these variables is significantly in determining the linkage between dietary patterns and HTN risk, their disparities could potentially account for the observed heterogeneity across different studies.
3.8 Sensitivity analysis
In the analysis of the traditional southern Chinese pattern, the results were unstable, which became statistically non-significant on the exclusion of the study of Liu (27) Female (OR = 0.97, 95% CI: 0.91–1.04) (Figures 3A,B). For the fruit and dairy pattern and animal food pattern, the overall statistical significance of the meta-analysis did not change after the deletion of any individual study, indicating that the results were stable and credible (Figures 3C,D).
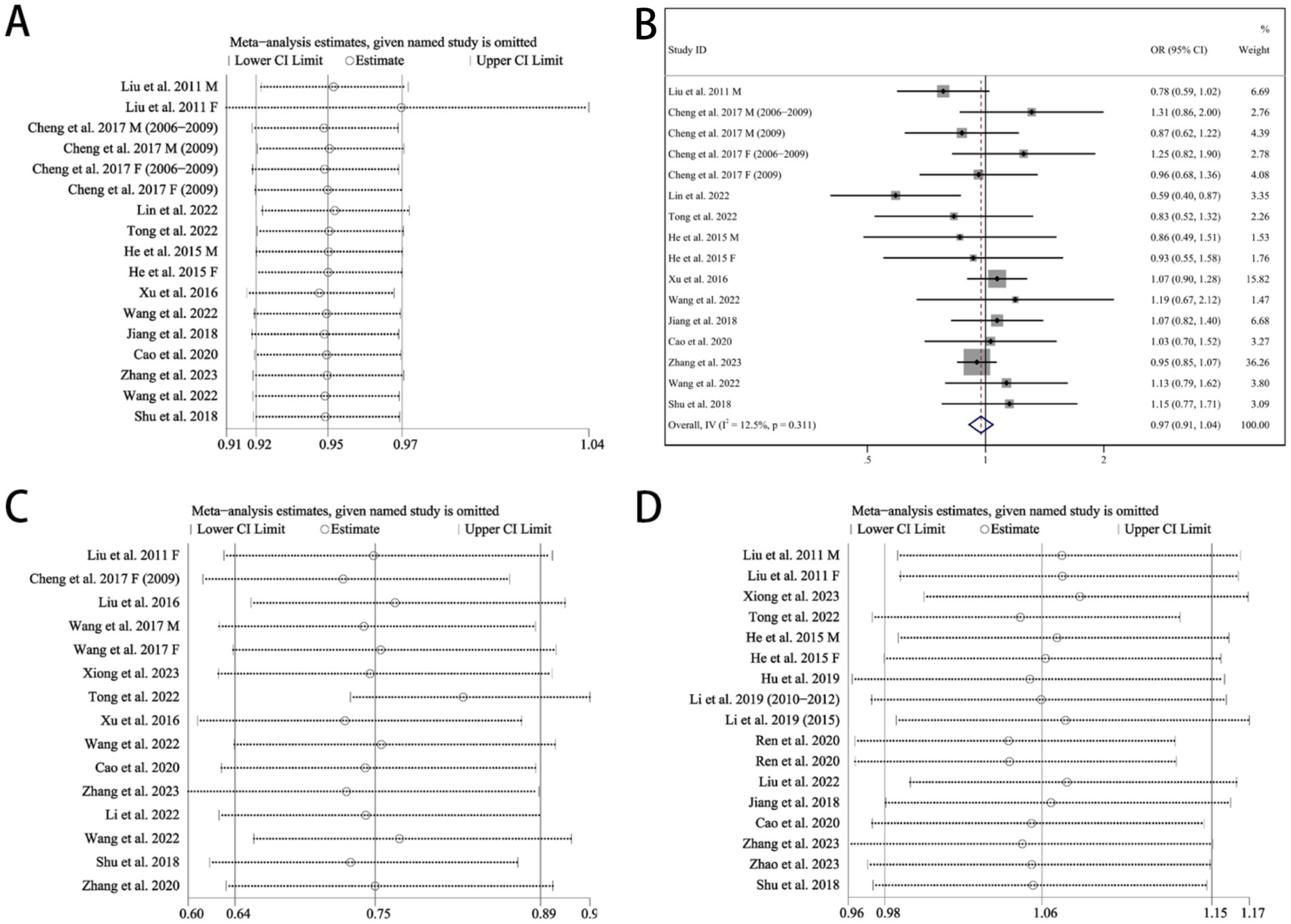
Figure 3. Sensitivity analysis. (A) Chinese traditional southern dietary pattern, (B) forest plots of Chinese traditional southern dietary pattern and hypertension after omitting the study of Liu (27) Female, (C) fruit and dairy dietary pattern, (D) animal food dietary pattern. OR, odds ratio. CI, confidence interval. M, male. F, female.
3.9 Publication bias
No publication bias occurred in the traditional southern Chinese pattern studies (Begg’s test p = 0.484, Egger’s test p = 0.452) (Figure 4A) and animal food pattern studies (Begg’s test p = 0.837, Egger’s test p = 0.793) (Figure 4C) according to Begg’s and Egger’s tests. Despite the notable publication bias in the research on fruit and dairy pattern (Begg’s test p = 0.092, Egger’s test p = 0.046) (Figure 4B), the correlation continued to be significant following the inclusion of four more studies through the trim-and-fill method (OR = 0.64, 95% CI: 0.52–0.78, p < 0.001) (Figure 4D).
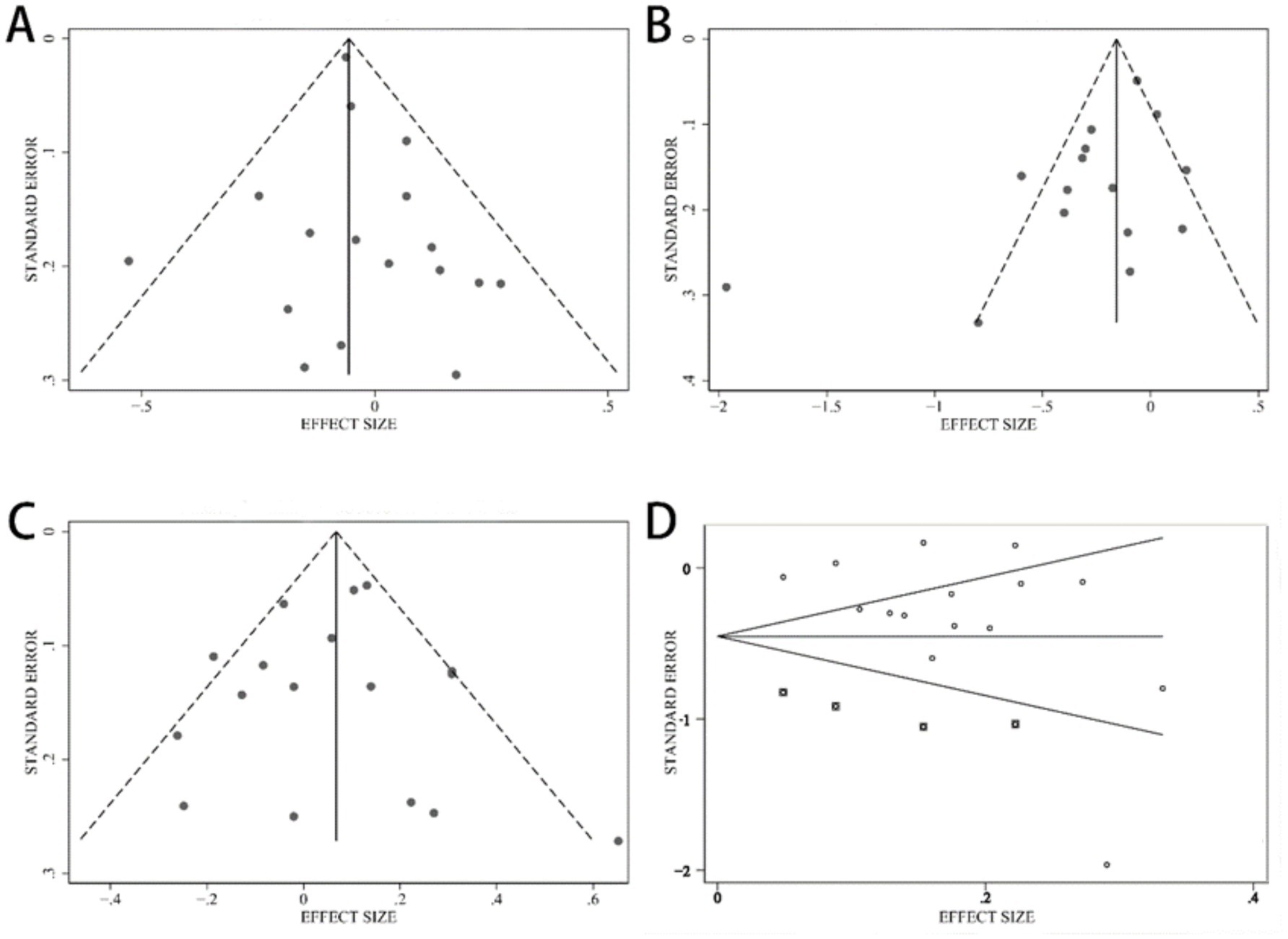
Figure 4. Funnel plot. (A) Chinese traditional southern dietary pattern, (B) fruit and dairy dietary pattern before using the trim-and-fill method, (C) animal food dietary pattern, (D) fruit and dairy dietary pattern after using the trim-and-fill method, and the boxes represent the filled studies.
4 Discussion
As far as we know, this meta-analysis provides the most up-to-date findings on how dietary patterns impact the likelihood of developing HTN among Chinese adults. In the current study, the results indicated that the traditional southern Chinese pattern and the fruit and dairy pattern were relevant to a lower risk of HTN, whereas the animal food pattern had nothing to do with HTN risk. We incorporated data from 24 observational studies that involved 159,096 participants in this analysis.
Although different definitions are used, the traditional southern Chinese pattern consists mainly of grains (especially rice), vegetables, and meat (especially pork). It seems probable that the consumption of these foods is a significant contributor to the observed influence on HTN risk, especially vegetables. Vegetable consumption and HTN risk were discovered to be negatively correlated in a meta-analysis involving eight cohorts (49). Vegetables are a valuable source of dietary fiber, vitamins, minerals and phytochemicals (50). A systematic review conducted by Vitrag and his colleagues showed that a positive association was consistently observed between increased dietary fiber intake and lower BP levels (51). Dietary fiber affects blood pressure by forming a viscous gel in the gastrointestinal tract, delaying glucose absorption and digestion, and improving blood sugar control (52). Furthermore, the gut flora can ferment dietary fiber to synthesize short-chain fatty acids (SCFAs), which have the ability to reduce BP (53, 54). Relevant meta-analyses revealed that serum vitamin C concentration was oppositely related to both systolic blood pressure (SBP) and diastolic blood pressure (DBP) (55), and vitamin C supplementation could reduce SBP by −3.0 mmHg (95% CI, −4.7 to −1.3 mmHg; p = 0.001) over the short term (56). As an effective antioxidant and free radical scavenger, vitamin C can reduce the damage of oxidative stress to vascular endothelial cells (57–60). In addition, vitamin C potentiates the synthesis and bioactivity of endothelial nitric oxide (NO) (a vital antioxidant and vasodilator) by increasing intracellular tetrahydrobiopterin (61, 62). Vitamin E also reduces BP through a number of mechanisms and its main biological function is antioxidant (63–65). Vegetables are good sources of magnesium and potassium, whose role in the regulation of BP is well established in previous studies (66–68). The mechanisms of potassium’s hypotensive effect include: promoting sodium excretion in urine, endothelium-dependent vasodilation, increasing endothelial NO production, and inhibiting the sympathetic nervous system (69). It has been reported that magnesium ions can directly stimulate the production of prostacyclin and NO, induce vasodilation, act as a natural calcium channel blocker, decrease intracellular calcium and sodium, and thus reduce peripheral vascular resistance and BP (70). The flavonoids and carotenoids contained in vegetables regulate BP by their ability to inhibit free radicals, reduce reactive oxygen species-induced damage, reduce oxidative stress and inflammatory responses, and increase NO bioavailability and bioactivity (71, 72). A dose–response meta-analysis of prospective cohort studies showed that compared to non-flavonoid consumption, the risk of incident HTN was reduced by 3% (relative risk (RR): 0.97, 95% CI: 0.94–0.99) at 500 mg/d intake (73). A meta-analysis by Behzadi et al. (74) revealed that carotenoid supplementation prominently reduced SBP (weighted mean difference (WMD), −2.492 mmHg; 95% Cl, −4.52, −0.47; p = 0.016) and DBP (WMD, −1.60 mmHg; 95% Cl, −2.73, −0.47; p = 0.005). A meta-analysis carried out by Jiang and others (75) with 23 articles determined that traditional Chinese dietary patterns characterized were related to a lower risk of obesity, which was regarded as a crucial risk factor for HTN.
Compared to the lowest category of the fruit and dairy pattern, the highest category had a 25% reduction in HTN risk in our findings. This beneficial association can be explained by the beneficial influence of fruit and milk on BP. Recently, Madsen and his colleagues conducted a meta-analysis including 18 prospective studies and demonstrated that fruit intake was connected to a decrease HTN risk (RR: 0.91, 95% CI: 0.85–0.97) (76). Fruits are rich in potassium, magnesium, vitamin C, folate, flavonoids, and carotenoids, which are thought to reduce BP by enhancing endothelial function, modulating baroreflex sensitivity, promoting vasodilation, and boosting antioxidant activity (58, 72, 73, 77–79). Recent meta-analysis carried out by Chen and his co-workers, hinted that total dairy intake was linked to a diminished HTN risk (RR for highest compared with lowest level of intake: 0.91, 95% CI: 0.86–0.95; RR for 1 serving/d increase: 0.96, 95% CI: 0.94–0.97) (80). It has been proposed that the beneficial effects of milk and dairy products on HTN are attributed to a number of ingredients such as calcium, potassium, or lactate tripeptides (81–83). Dietary calcium can regulate BP by secreting parathyroid hormone, promoting sodium ion excretion, regulating the sympathetic nervous system, and changing intracellular free calcium levels (84). During milk fermentation, bioactive peptides are produced that inhibit angiotensin-converting enzyme, thereby maintaining normal BP (85).
Our findings showed no significant correlation between the animal food pattern and HTN. Our results contradicted some former studies that suggested a positive correlation between this dietary pattern and HTN risk (35, 39, 42, 47). This null relationship might have various reasonable causes. Above all, it may be due to interactions between different food categories. Numerous studies have confirmed that red meat consumption (especially processed red meat) and poultry consumption are related to an incremental risk of HTN, whereas the intake of fish or eggs is inversely connected with HTN risk, so the harmful effects may be offset by the protective effects of other food groups (86–89). Secondly, the intake of different parts of the same food was unknown, and the complex effects of various components after entering the body were unknown, which need to be further explored. For example, livestock meat is an excellent source of fat supply and a provider of high-quality protein (89). It has been reported that the protein hydrolysates of meat and muscle have strong vasopressor activity (90). A research completed by Zhou and others has proven that there is a window of consumption (at appropriate levels) of proteins, whether from fish, eggs, red meat sources (including unprocessed) or poultry sources, in which the risk of HTN is low (91). Thirdly, the zero correlation may lie in the fact that the sample size of the survey was not large enough. Subgroup analysis implied a significant positive correlation between HTN and the animal food pattern in studies with larger sample sizes. Compared to studies with large sample sizes, studies with small sample sizes have lower statistical validity and are more susceptible to extreme values or outliers affecting the overall results. More studies with larger sample sizes are needed to determine the true impact of the animal food pattern on the risk and severity of HTN. Finally, it pertained to a number of potential confounding factors that we did not take into consideration or that we were unable to quantify, such as cooking methods.
First of all, there was significant heterogeneity in the included studies. This could be attributed to extensive differences in the collection and analysis of dietary data, inconsistent adjustment of multifarious confounders, and the recognition of dietary patterns. While we endeavored to align the factor loads of included studies as closely as possible, the practical factor loads of the identical foods in semblable dietary patterns were never precisely consistent across studies. In subgroup analyses, we also observed that study design, sample size, adjustments for smoking, alcohol, physical activity, BMI, or energy had a significant impact on the dietary patterns and HTN. However, limited by the amount of research included, we were unable to investigate all possible sources of heterogeneity. Secondly, cross-sectional designs were employed in the majority of studies, which are more prone to recall and selection bias than cohort designs, particularly in case of diet recall bias. Furthermore, the cross-sectional studies were not suitable for causal reasoning and did not permit the evaluation of any potential trends. Thirdly, all studies included in this meta-analysis were conducted in China, and as dietary intake is influenced by ethnic, geographic, and social factors, the results cannot be extended to all populations. Last but not least, the instability of the results in sensitivity analysis of the traditional southern Chinese dietary pattern suggested that additional pertinent articles are required to delve into this connection. In the fruit and dairy pattern studies, publication bias was identified. Nonetheless, the inverse association remained significant after the pruning and filling method was used.
5 Conclusion
The results of our meta-analysis showed that Chinese traditional southern dietary pattern and fruit and dairy dietary pattern were strongly associated with the risk of HTN. Higher adherence to these two dietary patterns may be beneficial in reducing the risk of HTN. However, there was no evidence to indicate the level of risk of high, moderate or low risk of HTN based on dietary patterns. Subgroup analyses showed that the negative association between these two dietary patterns and the risk of HTN was influenced by study design, sample size, and multiple potential confounders. Future high-quality prospective studies with larger sample sizes and strict control of confounders are needed to further validate our findings and explore their dose–response relationships.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
XW: Conceptualization, Methodology, Software, Writing – review & editing, Data curation, Formal analysis, Validation, Writing – original draft. JL: Conceptualization, Data curation, Methodology, Software, Writing – original draft. ZW: Conceptualization, Data curation, Methodology, Software, Writing – original draft. SC: Conceptualization, Data curation, Methodology, Software, Writing – original draft. JM: Conceptualization, Data curation, Methodology, Writing – original draft. MC: Conceptualization, Data curation, Methodology, Writing – original draft. YY: Conceptualization, Data curation, Methodology, Writing – original draft. GW: Conceptualization, Methodology, Project administration, Software, Supervision, Writing – review & editing. WL: Conceptualization, Methodology, Project administration, Software, Supervision, Writing – review & editing. ZD: Conceptualization, Methodology, Project administration, Software, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Key Research and Development Program of China [grant number 2022YFC2503202], National Natural Science Foundation of China (NSFC) [grant numbers 81602893, 81872575], Natural Science Foundation of Shandong Province [grant numbers ZR2015YL049, ZR2021MH218, ZR2022MH184 and ZR2024QH001]; Shandong Province Medical and Health Technology Development Plan [grant number 202104020224, 202212040403, 202312010854]; Shandong Province Traditional Chinese Medicine Science and Technology Plan [grant numbers, 2021M151, Z-2023114], and Jinan Science and Technology Plan [grant number 202328074] and the innovation Project of Shandong Academy of Medical Science.
Acknowledgments
We acknowledge the significant efforts of each and every author.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
2. Fuchs, FD, and Whelton, PK. High blood pressure and cardiovascular disease. Hypertension. (2020) 75:285–92. doi: 10.1161/HYPERTENSIONAHA.119.14240
3. Burnier, M, and Damianaki, A. Hypertension as cardiovascular risk factor in chronic kidney disease. Circ Res. (2023) 132:1050–63. doi: 10.1161/CIRCRESAHA.122.321762
4. Santisteban, MM, Iadecola, C, and Carnevale, D. Hypertension, neurovascular dysfunction, and cognitive impairment. Hypertension. (2023) 80:22–34. doi: 10.1161/HYPERTENSIONAHA.122.18085
5. World Health Organization. Hypertension (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/hypertension (Accessed May 20, 2024).
6. Mills, KT, Stefanescu, A, and He, J. The global epidemiology of hypertension. Nat Rev Nephrol. (2020) 16:223–37. doi: 10.1038/s41581-019-0244-2
7. Zhang, M, Wu, J, Zhang, X, Hu, C, Zhao, Z, Li, C, et al. Prevalence and control of hypertension in adults in China, 2018. Chinese J Epidemiol. (2021) 42:1780–9. doi: 10.3760/cma.j.cn112338-20210508-00379
8. Priviero, F. Epigenetic modifications and fetal programming: molecular mechanisms to control hypertension inheritance. Biochem Pharmacol. (2023) 208:115412. doi: 10.1016/j.bcp.2023.115412
9. Carey, RM, Moran, AE, and Whelton, PK. Treatment of hypertension: a review. JAMA. (2022) 328:1849–61. doi: 10.1001/jama.2022.19590
10. Gupta, DK, Lewis, CE, Varady, KA, Su, YR, Madhur, MS, Lackland, DT, et al. Effect of dietary sodium on blood pressure: a crossover trial. JAMA. (2023) 330:2258–66. doi: 10.1001/jama.2023.23651
11. Mozos, I, Stoian, D, Caraba, A, Malainer, C, Horbańczuk, JO, and Atanasov, AG. Lycopene and vascular health. Front Pharmacol. (2018) 9:521. doi: 10.3389/fphar.2018.00521
12. Mosallanezhad, Z, Mahmoodi, M, Ranjbar, S, Hosseini, R, Clark, CCT, Carson-Chahhoud, K, et al. Soy intake is associated with lowering blood pressure in adults: a systematic review and Meta-analysis of randomized double-blind placebo-controlled trials. Complement Ther Med. (2021) 59:102692. doi: 10.1016/j.ctim.2021.102692
13. Wang, S, Meckling, KA, Marcone, MF, Kakuda, Y, and Tsao, R. Synergistic, additive, and antagonistic effects of food mixtures on Total antioxidant capacities. J Agric Food Chem. (2011) 59:960–8. doi: 10.1021/jf1040977
14. Theodoridis, X, Chourdakis, M, Chrysoula, L, Chroni, V, Tirodimos, I, Dipla, K, et al. Adherence to the dash diet and risk of hypertension: a systematic review and Meta-analysis. Nutrients. (2023) 15:3261. doi: 10.3390/nu15143261
15. Huang, L, Wang, Z, Wang, H, Zhao, L, Jiang, H, Zhang, B, et al. Nutrition transition and related health challenges over decades in China. Eur J Clin Nutr. (2021) 75:247–52. doi: 10.1038/s41430-020-0674-8
16. Wang, N, Hong, X, Wang, Z, and Xu, F. Study of relation between dietary patterns and hypertension among residents by dietary pattern analysis. Jiangsu J Prevent Med. (2015) 26:35–8. doi: 10.13668/j.issn.1006-9070.2015.05.012
17. Wang, C, Lan, L, Yang, C, Jiang, G, Wang, R, and Zhao, N. Relationship between hypertension and dietary patterns in residents of Harbin City. Occupat Health. (2017) 33:2377–9. doi: 10.13329/j.cnki.zyyjk.2017.0710
18. Chen, M, Xu, Y, Wang, X, Shan, S, and Cheng, G. Association between the prudent dietary pattern and blood pressure in Chinese adults is partially mediated by body composition. Front Nutr. (2023) 10:1131126. doi: 10.3389/fnut.2023.1131126
19. Zheng, PF, Shu, L, Zhang, XY, Si, CJ, Yu, XL, Gao, W, et al. Association between dietary patterns and the risk of hypertension among Chinese: a cross-sectional study. Nutrients. (2016) 8:239. doi: 10.3390/nu8040239
20. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The Prisma 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. (2021) 18:e1003583. Epub 2021/03/30. doi: 10.1371/journal.pmed.1003583
21. National Heart Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (2021). Available online at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Accessed April 23, 2024).
22. Higgins, JPT, and Thompson, SG. Quantifying heterogeneity in a Meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
23. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in Meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
24. Begg, CB, and Mazumdar, M. Operating characteristics of a rank correlation test for publication Bias. Biometrics. (1994) 50:1088–101.
25. Egger, M, Davey, SG, Schneider, M, and Minder, C. Bias in Meta-analysis detected by a simple. Graph Test BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
26. Duval, S, and Tweedie, R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication Bias in Meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341x.2000.00455.x
27. Liu, A. Chinese Adults' dietary patterns and their relationship with hypertension among residents in nine provinces (1997~2009). [Doctoral thesis]. Beijing: Chinese Center for Disease Control and Prevention (2011).
28. He, D, Yang, M, Zhang, R, Am, X, Huang, L, Huang, E, et al. Dietary patterns associated metabolic syndrome in Chinese adults. Biomed Environ Sci. (2015) 28:370–3. doi: 10.3967/bes2015.051
29. Liu, J, Yao, H, Zhang, L, Lazhati, G, Gu, K, Kedeerayi, M, et al. Study on the relationship between dietary patterns and metabolic syndrome and its components in Xinjiang Uygur population. J Hygiene Res. (2016) 45:725–32. doi: 10.19813/j.cnki.weishengyanjiu.2016.05.032
30. Xu, X, Byles, J, Shi, Z, McElduff, P, and Hall, J. Dietary pattern transitions, and the associations with Bmi, waist circumference, weight and hypertension in a 7-year follow-up among the older Chinese population: a longitudinal study. BMC Public Health. (2016) 16:743. doi: 10.1186/s12889-016-3425-y
31. Cheng, M. Dietary patterns and their association with metabolic syndrome among adults in China (2006–2009). [Doctoral thesis]. Beijing: Chinese Center for Disease Control and Prevention (2017).
32. Wang, X. Study on the correlation between dietary patterns and metabolic syndrome among residents in Xiamen. [Master’s thesis]. Fujian: Xiamen University (2017).
33. Zhang, T, Na, X, Zhu, Z, Zhou, J, Chen, Y, Zhou, G, et al. Relationship between dietary patterns and the prevalence and control of hypertension among residents in Mentougou District of Beijing. Chinese journal of. Health Educ. (2020) 36:129–33. doi: 10.16168/j.cnki.issn.1002-9982.2020.02.008
34. Lin, L. Relationship between dietary behavior and hypertension in middle-aged and elderly residents in Hainan Province. [Master’s thesis]. Hainan: Hainan Medical University (2022).
35. Tong, G, Gao, X, Xu, R, Qin, Y, Huang, L, Wang, X, et al. Relationship between dietary pattern and risk of suffering from hypertension in physical examinees aged 35 years and above in Haidian District of Beijing. Pract Prevent Med. (2022) 29:906–11. doi: 10.3969/j.issn.1006-31.10.2022.08.003
36. Xiong, H, Ju, D, Qiu, J, Shu, Q, Yu, J, and Tang, D. Correlation analysis between different dietary patterns and hypertension based on population survey. Modern Prevent Med. (2023) 50:1026–31. doi: 10.20043/j.cnki.MPM.202208158
37. Shu, L, Lu, X, and Li, X. Relationship of different dietary patterns with dyslipidemia and hypertension among middle-aged and elderly residents in Bengbu City in 2014-2015. J Hygiene Res. (2018) 47:554–61. doi: 10.19813/j.cnki.weishengyanjiu.2018.04.003
38. Jiang, M, Lai, S, Lin, S, and Huang, Z. Relationship between dietary patterns and metabolic syndrome among adult residents in Fujian Province. Acta Nutrimenta Sinica. (2018) 40:439–44. doi: 10.13325/j.cnki.acta.nutr.sin.2018.05.009
39. Hu, M. The prevalence and control of hypertension and its correlation with health-related behaviors among adult in Xi'an City. [Doctoral thesis]. Shaanxi: Air Force Medical University (2019).
40. Li, Y. The associations between dietary intake and metabolic syndrome prevalence. [Doctoral thesis]. Beijing: Chinese Center for Disease Control and Prevention (2019).
41. Cao, L, Xu, J, Zhang, Y, and Xue, Y. Relationship between dietary patterns and common chronic diseases among female residents of a Community in Beijing. China Food Nutr. (2020) 26:84–8. doi: 10.19870/j.cnki.11-3716/ts.2020.04.019
42. Ren, Z, Zhao, J, Chen, J, Zhang, R, Wang, M, Liang, J, et al. The study on the association between dietary pattern and the incidence of hypertension in different genders in Shanxi Province. Chinese J Dis Control Prevent. (2020) 24:754–60. doi: 10.16462/j.cnki.zhjbkz.2020.07.003
43. Li, T, Xie, J, Shuai, P, Huang, J, and He, B. Dietary patterns, skeletal muscle mass loss, and cardiovascular risk among elderly men: a preliminary cross-sectional study in Sichuan Province. Environ Res. (2022) 208:112719. doi: 10.1016/j.envres.2022.112719
44. Liu, L, Sun, M, Lin, W, Wu, X, Li, Y, and Pan, B. Relationship between dietary patterns and chronic non-communicable diseases among middle aged and old people in old urban region of Guangzhou City. Occupat Health. (2022) 38:626–30. doi: 10.13329/j.cnki.zyyjk.2022.0095
45. Wang, C. Study on the associations of dietary patterns and sleep disorders with hypertension among adult residents in Gusu District. Suzhou [Master’s thesis]. Suzhou: Soochow University (2022).
46. Wang, C, Zheng, Y, Zhang, Y, Liu, D, Guo, L, Wang, B, et al. Dietary patterns in association with hypertension: a community-based study in eastern China. Front Nutr. (2022) 9:926390. doi: 10.3389/fnut.2022.926390
47. Zhang, J, Du, W, Huang, F, Li, L, Bai, J, Wei, Y, et al. Longitudinal study of dietary patterns and hypertension in adults: China health and nutrition survey 1991–2018. Hypertens Res. (2023) 46:2264–71. doi: 10.1038/s41440-023-01322-x
48. Zhao, JK, Guo, WJ, Wang, JP, and Wang, T. Exploring the Association of Dietary Patterns with the risk of hypertension using principal balances analysis and principal component analysis. Public Health Nutr. (2023) 26:160–70. doi: 10.1017/S136898002200091X
49. Wu, L, Sun, D, and He, Y. Fruit and vegetables consumption and incident hypertension: dose-response Meta-analysis of prospective cohort studies. J Hum Hypertens. (2016) 30:573–80. doi: 10.1038/jhh.2016.44
50. Sarkar, T, Salauddin, M, Roy, S, Chakraborty, R, Rebezov, M, Shariati, MA, et al. Underutilized green leafy vegetables: frontier in fortified food development and nutrition. Crit Rev Food Sci Nutr. (2023) 63:11679–733. doi: 10.1080/10408398.2022.2095555
51. Tejani, VN, Dhillon, SS, Damarlapally, N, Usman, NUB, Winson, T, Basu, RP, et al. The relationship between dietary Fiber intake and blood pressure worldwide: a systematic review. Cureus. (2023) 15:e46116. doi: 10.7759/cureus.46116
52. Aleixandre, A, and Miguel, M. Dietary Fiber in the prevention and treatment of metabolic syndrome: a review. Crit Rev Food Sci Nutr. (2008) 48:905–12. doi: 10.1080/10408390701761886
53. Makki, K, Deehan, EC, Walter, J, and Bäckhed, F. The impact of dietary Fiber on gut microbiota in host health and disease. Cell Host Microbe. (2018) 23:705–15. doi: 10.1016/j.chom.2018.05.012
54. Hu, T, Wu, Q, Yao, Q, Jiang, K, Yu, J, and Tang, Q. Short-chain fatty acid metabolism and multiple effects on cardiovascular diseases. Ageing Res Rev. (2022) 81:101706. doi: 10.1016/j.arr.2022.101706
55. Ran, L, Zhao, W, Tan, X, Wang, H, Mizuno, K, Takagi, K, et al. Association between serum vitamin C and the blood pressure: a systematic review and Meta-analysis of observational studies. Cardiovasc Ther. (2020) 2020:4940673–11. doi: 10.1155/2020/4940673
56. Lbban, E, Kwon, K, Ashor, A, Stephan, B, Idris, I, Tsintzas, K, et al. Vitamin C supplementation showed greater effects on systolic blood pressure in hypertensive and diabetic patients: an updated systematic review and Meta-analysis of randomised clinical trials. Int J Food Sci Nutr. (2023) 74:814–25. doi: 10.1080/09637486.2023.2264549
57. Ashor, AW, Siervo, M, Lara, J, Oggioni, C, Afshar, S, and Mathers, JC. Effect of vitamin C and vitamin E supplementation on endothelial function: a systematic review and Meta-analysis of randomised controlled trials. Br J Nutr. (2015) 113:1182–94. doi: 10.1017/S0007114515000227
58. Morelli, MB, Gambardella, J, Castellanos, V, Trimarco, V, and Santulli, G. Vitamin C and cardiovascular disease: an update. Antioxidants. (2020) 9:1227. doi: 10.3390/antiox9121227
59. Tamari, Y, Nawata, H, Inoue, E, Yoshimura, A, Yoshii, H, Kashino, G, et al. Protective roles of ascorbic acid in oxidative stress induced by depletion of superoxide dismutase in vertebrate cells. Free Radic Res. (2013) 47:1–7. doi: 10.3109/10715762.2012.734916
60. Ellulu, MS. Obesity, cardiovascular disease, and role of vitamin C on inflammation: a review of facts and underlying mechanisms. Inflammopharmacology. (2017) 25:313–28. doi: 10.1007/s10787-017-0314-7
61. Heller, R, Unbehaun, A, Schellenberg, B, Mayer, B, Werner-Felmayer, G, and Werner, ER. L-ascorbic acid potentiates endothelial nitric oxide synthesis via a chemical stabilization of tetrahydrobiopterin. J Biol Chem. (2001) 276:40–7. doi: 10.1074/jbc.M004392200
62. Huang, A, Vita, JA, Venema, RC, and Keaney, JF. Ascorbic acid enhances endothelial nitric-oxide synthase activity by increasing intracellular tetrahydrobiopterin. J Biol Chem. (2000) 275:17399–406. doi: 10.1074/jbc.M002248200
63. Qi, S, Luo, X, Liu, S, Ling, B, Si, M, and Jin, H. Effect of vitamin B (2), vitamin C, vitamin D, vitamin E and folic acid in adults with essential hypertension: a systematic review and network Meta-analysis. BMJ Open. (2024) 14:e074511. doi: 10.1136/bmjopen-2023-074511
64. Amponsah-Offeh, M, Diaba-Nuhoho, P, Speier, S, and Morawietz, H. Oxidative stress, antioxidants and hypertension. Antioxidants. (2023) 12:281. doi: 10.3390/antiox12020281
65. Miyazawa, T, Burdeos, GC, Itaya, M, Nakagawa, K, and Miyazawa, T. Vitamin E: regulatory redox interactions. IUBMB Life. (2019) 71:430–41. doi: 10.1002/iub.2008
66. Filippini, T, Naska, A, Kasdagli, MI, Torres, D, Lopes, C, Carvalho, C, et al. Potassium intake and blood pressure: a dose-response Meta-analysis of randomized controlled trials. J Am Heart Assoc. (2020) 9:e015719. doi: 10.1161/JAHA.119.015719
67. Filippini, T, Violi, F, D'Amico, R, and Vinceti, M. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and Meta-analysis. Int J Cardiol. (2017) 230:127–35. doi: 10.1016/j.ijcard.2016.12.048
68. Han, H, Fang, X, Wei, X, Liu, Y, Jin, Z, Chen, Q, et al. Dose-response relationship between dietary magnesium intake, serum magnesium concentration and risk of hypertension: a systematic review and Meta-analysis of prospective cohort studies. Nutr J. (2017) 16:26. doi: 10.1186/s12937-017-0247-4
69. Ekmekcioglu, C, Elmadfa, I, Meyer, AL, and Moeslinger, T. The role of dietary potassium in hypertension and diabetes. J Physiol Biochem. (2016) 72:93–106. doi: 10.1007/s13105-015-0449-1
70. Romani, AMP. Beneficial role of mg (2+) in prevention and treatment of hypertension. Int J Hypertens. (2018) 2018:9013721. doi: 10.1155/2018/9013721
71. Sánchez, M, Romero, M, Gómez-Guzmán, M, Tamargo, J, Pérez-Vizcaino, F, and Duarte, J. Cardiovascular effects of flavonoids. Curr Med Chem. (2019) 26:6991–7034. doi: 10.2174/0929867326666181220094721
72. Abbasian, F, Alavi, MS, and Roohbakhsh, A. Dietary carotenoids to improve hypertension. Heliyon. (2023) 9:e19399. doi: 10.1016/j.heliyon.2023.e19399
73. Li, T, Zhao, Y, Yuan, L, Zhang, D, Feng, Y, Hu, H, et al. Total dietary flavonoid intake and risk of Cardiometabolic diseases: a dose-response Meta-analysis of prospective cohort studies. Crit Rev Food Sci Nutr. (2024) 64:2760–72. doi: 10.1080/10408398.2022.2126427
74. Behzadi, M, Akbarzadeh, M, Mohammadi, SM, Rabiee, M, and Bideshki, MV. Effect of carotenoid supplementation on blood pressure in adults: a grade-assessed systematic review and dose-response Meta-analysis of randomized controlled trials. Nutr Rev. (2024) 83:13–28. doi: 10.1093/nutrit/nuad172
75. Jiang, K, Zhang, Z, Fullington, LA, Huang, TT, Kaliszewski, C, Wei, J, et al. Dietary patterns and obesity in Chinese adults: a systematic review and meta-analysis. Nutrients. (2022) 14:4911. doi: 10.3390/nu14224911
76. Madsen, H, Sen, A, and Aune, D. Fruit and vegetable consumption and the risk of hypertension: a systematic review and Meta-analysis of prospective studies. Eur J Nutr. (2023) 62:1941–55. doi: 10.1007/s00394-023-03145-5
77. Staruschenko, A. Beneficial effects of high potassium: contribution of renal basolateral K(+) channels. Hypertension. (2018) 71:1015–22. doi: 10.1161/HYPERTENSIONAHA.118.10267
78. Houston, M. The role of magnesium in hypertension and cardiovascular disease. J Clin Hypertens. (2011) 13:843–7. doi: 10.1111/j.1751-7176.2011.00538.x
79. Asbaghi, O, Salehpour, S, Rezaei, KM, Bagheri, R, Ashtary-Larky, D, Nazarian, B, et al. Folic acid supplementation and blood pressure: a grade-assessed systematic review and dose-response Meta-analysis of 41, 633 participants. Crit Rev Food Sci Nutr. (2023) 63:1846–61. doi: 10.1080/10408398.2021.1968787
80. Chen, Z, Ahmed, M, Ha, V, Jefferson, K, Malik, V, Ribeiro, PAB, et al. Dairy product consumption and cardiovascular health: a systematic review and Meta-analysis of prospective cohort studies. Adv Nutr. (2022) 13:439–54. doi: 10.1093/advances/nmab118
81. Houston, MC, and Harper, KJ. Potassium, magnesium, and calcium: their role in both the cause and treatment of hypertension. J Clin Hypertens. (2008) 10:3–11. doi: 10.1111/j.1751-7176.2008.08575.x
82. Fekete, ÁA, Givens, DI, and Lovegrove, JA. Casein-derived Lactotripeptides reduce systolic and diastolic blood pressure in a Meta-analysis of randomised clinical trials. Nutrients. (2015) 7:659–81. doi: 10.3390/nu7010659
83. Jayedi, A, and Zargar, MS. Dietary calcium intake and hypertension risk: a dose-response Meta-analysis of prospective cohort studies. Eur J Clin Nutr. (2019) 73:969–78. doi: 10.1038/s41430-018-0275-y
84. Hatton, DC, and McCarron, DA. Dietary calcium and blood pressure in experimental models of hypertension. A Review. Hypertension. (1994) 23:513–30. doi: 10.1161/01.hyp.23.4.513
85. Rai, AK, Sanjukta, S, and Jeyaram, K. Production of angiotensin I converting enzyme inhibitory (ace-I) peptides during Milk fermentation and their role in reducing hypertension. Crit Rev Food Sci Nutr. (2017) 57:2789–800. doi: 10.1080/10408398.2015.1068736
86. Zhang, Y, and Zhang, DZ. Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens. (2018) 32:507–17. doi: 10.1038/s41371-018-0068-8
87. Allen, TS, Bhatia, HS, Wood, AC, Momin, SR, and Allison, MA. State-of-the-art review: evidence on red meat consumption and hypertension outcomes. Am J Hypertens. (2022) 35:679–87. doi: 10.1093/ajh/hpac064
88. Brosolo, G, Da Porto, A, Marcante, S, Picci, A, Capilupi, F, Capilupi, P, et al. Omega-3 fatty acids in arterial hypertension: is there any good news? Int J Mol Sci. (2023) 24:9520. doi: 10.3390/ijms24119520
89. Huang, WY, Davidge, ST, and Wu, J. Bioactive natural constituents from food sources-potential use in hypertension prevention and treatment. Crit Rev Food Sci Nutr. (2013) 53:615–30. doi: 10.1080/10408398.2010.550071
90. Ahhmed, AM, and Muguruma, M. A review of meat protein hydrolysates and hypertension. Meat Sci. (2010) 86:110–8. doi: 10.1016/j.meatsci.2010.04.032
Keywords: dietary pattern, hypertension, meta-analysis, Chinese adults, prevalence
Citation: Wu X, Liu J, Wang Z, Chen S, Ma J, Cao M, Yang Y, Wu G, Li W and Du Z (2025) Dietary patterns and hypertension in Chinese adults: a systematic review and meta-analysis. Front. Public Health. 13:1539359. doi: 10.3389/fpubh.2025.1539359
Edited by:
Jan Mohammad Mir, Islamic University of Science and Technology, IndiaReviewed by:
Ezequiel Pinto, University of Algarve, PortugalNisar A. Dangroo, Islamic University of Science and Technology, India
Copyright © 2025 Wu, Liu, Wang, Chen, Ma, Cao, Yang, Wu, Li and Du. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guangjian Wu, bml1bml1MTAyODg4ODhAMTYzLmNvbQ==; Wentao Li, bGl3ZW50YW83MEAxNjMuY29t; Zhongjun Du, ZHV6ajE5ODFAMTYzLmNvbQ==; ZHV6aG9uZ2p1bkBzZGZtdS5lZHUuY24=
 Xi Wu1
Xi Wu1 Shangya Chen
Shangya Chen Zhongjun Du
Zhongjun Du