- 1Center for Research for Infant Birth and Survival, Wichita, KS, United States
- 2Department of Pediatrics, University of Kansas School of Medicine-Wichita, Wichita, KS, United States
- 3Kansas Infant Death and SIDS (KIDS) Network, Wichita, KS, United States
- 4Department of Obstetrics and Gynecology, University of Kansas School of Medicine-Wichita, Wichita, KS, United States
Introduction: The Kansas Infant Death and SIDS (KIDS) Network facilitates a two-day conference certifying Safe Sleep Instructors to provide standardized trainings based on the American Academy of Pediatrics (AAP) Safe Sleep Recommendations. Within one-year of certification, Safe Sleep Instructors are tasked with (a) disseminating safe sleep education to 10 professionals or parent/caregivers; and (b) hosting one Safe Sleep Community Baby Shower or 10 Safe Sleep Crib Clinics.
Methods: A retrospective study was implemented to assess the impact of the Safe Sleep Instructor certification program using data from participants trained in Fiscal Year 2022. Data was assessed using the RE-AIM framework and aspects of the Kirkpatrick Evaluation Model. Reach and Effectiveness were evaluated at the conference, as were Kirkpatrick Reaction and Learning. Adoption and Implementation, and Kirkpatrick Behavior, were assessed through post-conference activities. Maintenance was measured based on Safe Sleep Instructor recertification the following year.
Results: Results suggested the Safe Sleep Instructor certification was successful in terms of Reach, Effectiveness, Implementation and Maintenance, and Kirkpatrick Evaluation Model. Adoption was less than expected.
Conclusion: Utilizing dissemination and implementation science allowed for identification of strengths and limitations regarding the Safe Sleep Instructor program promoting the AAP Safe Sleep Recommendations. Modification to program requirements and expectations, post-conference support for activities, and increased ability to tailor to community needs may enhance Adoption efforts. In addition, Safe Sleep Instructors must have capacity, resources, expertise, and institutional support. Future studies are needed to assess characteristics that impact Adoption to enhance promotion of the AAP Safe Sleep Recommendations.
1 Introduction
Since the 1990s the American Academy of Pediatrics (AAP) has recommended evidence-based interventions (EBI) to reduce sudden unexpected infant death (SUID). Recommendations include strategies such as placing infants in supine position, on a safety-approved sleep surface (e.g., bassinet, crib) in a tobacco-free environment (1, 2). Despite known risk reduction strategies, SUID is the leading cause of mortality between 28 days and 1 year of life, impacting 3,400 infants annually in the United States (3).
Most SUIDs, also termed sleep-related infant deaths, include external risk factors which may have contributed to the death (3). While public awareness campaigns (4) and community-based interventions (5–7) promote knowledge and address barriers, the burden of providing safe sleep interventions to families often falls on physicians and clinicians (e.g., nurses, midwives) (2). Efforts in the clinical setting have had some success, with families who receive advice from healthcare professionals more likely to report following safe sleep practices (8–10). However, many factors impact safe sleep behaviors including knowledge; convenience; perceived quality of infant sleep; perceived infant safety, comfort, and susceptibility; and cultural factors (11–19). Further, professionals do not always provide complete or consistent safe sleep information (8, 9, 20, 21), and some groups distrust advice from healthcare professionals (8, 11, 17, 22, 23). For example, persons with low income (8, 11, 22, 23) or of Black/African American (8, 17) descent may be wary of advice due to historical discrimination or systemic racism (24). Translational science is needed to determine effective strategies to promote SUID risk-reduction strategies and to address barriers to safe sleep practices (25).
In Kansas, the SUID rate is higher than the national average (120 infant deaths per 100,000 live births compared to 92 infant deaths; 2016–2020 data) (3). To promote SUID risk reduction strategies and ensure consistent safe sleep messages across the spectrum of perinatal services (8, 11, 18, 26, 27), an infrastructure to educate professionals and families across the state was needed. The Kansas Infant Death and SIDS (KIDS) Network and the University of Kansas School of Medicine-Wichita (KUSM-W) Center for Research for Infant Birth and Survival (CRIBS) partnered to develop an innovative strategy to scale-up safe sleep education interventions in Kansas. The Safe Sleep Instructor (SSI) certification program was developed to embed local experts across the state to provide education on the AAP safe sleep recommendations and to promote a culture of safe infant sleep (28).
No identified studies utilize an implementation science framework to assess the impact of interventions to promote uptake of the AAP Safe Sleep Recommendations. As such, the purpose of this study was to assess the impact of the SSI certification program in enhancing dissemination of the AAP Safe Sleep Recommendations across a rural state.
2 Materials and methods
2.1 Overall design
A retrospective study using the RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) framework (29, 30) was implemented based on data from the Safe Sleep Instructor cohort certified during Fiscal Year 2022. In addition, portions of the Kirkpatrick Evaluation Model were employed to clarify training effectiveness (31). This project involved secondary analysis of deidentified program data collected by KIDS Network staff for program reporting purposes; as such, the University of Kansas Medical Center Human Subjects Committee did not require ethics approval for the study.
2.2 SSI training program
The 2-day in-person conference to certify new SSIs consisted of didactics, hands-on demonstrations, video, small group activities, expert panel discussions and large group discussions provided by SSI Faculty (CRS, CS, AH, MT, SK, ZK) (26, 32). On day one, the curriculum covered data trends regarding sleep-related infant deaths and the AAP Safe Sleep Recommendations (1, 2). SSI trainees learned how to provide standardized education on the AAP Safe Sleep Recommendations to professionals (professional training) and caregivers (parent/caregiver training). The SSI training also included strategies on how to identify and engage community champions to build organizational partnerships to reach learners. SSI trainees were instructed on how to perform a Safe Sleep Crib Demonstration (33). This involved setting up a portable crib and using safe (e.g., wearable blanket) and unsafe (e.g., loose blanket, pillow) items with a doll to actively demonstrate how to create a safe sleep environment. This hands-on activity allowed SSI trainees to build skills and critically think about application of the AAP Safe Sleep Recommendations, as well as learn a demonstration method to employ when educating about infant safe sleep. SSI trainees engaged in small group dialog related to addressing social and cultural barriers to following the AAP Safe Sleep Recommendations.
On day two, SSI trainees learned how to educate persons in the perinatal period through a Safe Sleep Community Baby Shower (CBS) (26). Curriculum included how to identify and collaborate with key partners (e.g., hospitals, clinics, community programs, churches, local breastfeeding and tobacco cessation experts); identify priority populations (e.g., race/ethnicity, zip code); engage priority populations (e.g., partnering with organizations, community or religious leaders, existing events); identify and understand local infant mortality data; develop grant proposals for material supports (e.g., food/beverage, location rental fees, cribs for attendees); manage event logistics; engage vendors (e.g., hospital, insurance providers, oral health providers); collect data; and conduct evaluations. For SSIs from small, rural communities with access to fewer pregnant persons, or those who need to connect with participants virtually, instructions were shared for hosting a smaller event, referred to as a Safe Sleep Crib Clinic (CC) (33). A bereaved family was also invited to share their experience and to issue a call to action to disseminate safe sleep information.
To be certified, the SSI trainee was required to pass a knowledge assessment (score ≥ 90%) and successfully conduct a Crib Demonstration (score ≥ 90%). Those who did not meet the a priori level for certification were provided remediation by KIDS Network staff until they were successful. Once certified, SSIs were expected to complete the following within 1 year: (a) disseminate safe sleep education to at least 10 professionals or parent/caregivers; (b) host a Safe Sleep Community Baby Shower or 10 Safe Sleep Crib Clinics; and (c) submit pre/post-test data for these trainings. No compensation is provided to the SSIs by the KIDS Network for these dissemination efforts.
Each year certified SSIs attend a recertification webinar to learn new information (e.g., data, research, updated AAP recommendations) related to SUID and receive revised training materials to maintain their certification.
2.3 Data sources
2.3.1 Conference evaluation
Reach and Effectiveness were evaluated at the 2-day SSI conference using data collected by KIDS Network staff. Reach included the number of new SSIs certified and the number of professions represented in the training. No minimum educational or employment qualifications were required to become an SSI, however priority was given to those employed in a maternal/infant health-related field and who indicated supervisor approval to embed SSI activities into their job duties. SSI training participants were recruited across the state of Kansas through email invitations distributed by the KIDS Network, Kansas Department of Health and Environment (KDHE) and other maternal and infant health partners. Promotion and recruitment were also done at the KDHE Home Visiting Conference, Annual Governor’s Conference for the Prevention of Child Abuse and Neglect, Annual Kansas Governor’s Public Health Conference, Kansas Perinatal Community Collaboratives, Safe Kids Kansas Coalitions, local Integrated Referral and Intake System (IRIS) quarterly meetings, Emergency Medical Services for Children (EMSC) Advisory Committee Meetings, Kansas State University Extension Services and Community Health Worker Program. Communities with high rates of infant mortality, based on vital statistics reports (34) were contacted directly (e.g., health department, hospital, home visiting program, Department of Children and Families) to recruit training participants. In addition, participants external to Kansas were invited through national conference presentations (e.g., National Parents as Teachers Conference; Cribs for Kids; Safe Kids Worldwide Childhood Injury Prevention Convention), the American Association of SIDS Prevention Physicians (AASPP) listserv and meetings with the Minnesota Public Health Department, Halo Innovations, and Mississippi SIDS and Infant Safety Alliance.
Effectiveness was measured using a 10-item SSI Training Test administered pre- and post-conference. The test was developed by SSI faculty to measure knowledge related to the AAP Safe Sleep Recommendations. All participants completed the pre-and post-tests at the beginning of the conference and immediately following. The tests included the same 10 multiple choice questions, in modified order, which addressed the definition of SUID and specific AAP recommendations.
Effectiveness was also measured by SSI trainee ability to complete a Crib Demonstration with at least 90% fidelity. SSI Faculty used a 10-item checklist which included nine priority points to address during the demonstration (e.g., on back, why loose blankets are not safe, wearable blanket as alternative to loose blankets) and a list from which the SSI Faculty selected a supplemental questions to ask (e.g., where to get a crib, how to know if it was safe/had been recalled).
To further assess conference impact a post-conference evaluation was administered to all attendees. Reaction and Learning were assessed based on the Kirkpatrick Evaluation Model (31). For Reaction, relevance of the topics presented, whether the training was worthwhile, and satisfaction were measured, all with 5-point rating scales (5-representing positive endorsement). Learning was measured with 5-point Likert-type scales addressing the following: gained insight into safe infant sleep; materials were understandable; information was new; felt prepared to implement; and likelihood of providing safe sleep education.
2.3.2 Post-conference evaluation
Following the SSI conference, certified SSIs recruited participants to attend professional training(s), parent/caregiver training(s), CBS(s) and/or CC(s) in their communities. Adoption included the percentage of certified SSIs who: (1) conducted one or more Professional Trainings; (2) conducted one or more Parent/Caregiver Trainings; (3a) facilitated one or more CBS; (3b) facilitated one or more CC; (4) facilitated post-conference trainings at requested levels. In addition, Kirkpatrick Behavior examined SSIs who conducted no post-conference trainings (31).
Implementation was measured based on knowledge change between pre-and post-tests for Professional Trainings, Parent/Caregiver Trainings, CBSs, and CCs. All pre- and post-tests were developed by SSI Faculty to measure knowledge related to the AAP Safe Sleep Recommendations.
• Professional Training Tests: 10-item matched pre- and post-tests, similar to the SSI Training Tests but with less complex questions.
• Parent/Caregiver Training Tests: 3-item unmatched pre- and post-test assessed knowledge related to (1) infant sleep position, (2) sleep location and (3) items in the sleep environment.
• CBS/CC Tests: a 3-item matched pre- and post-test of knowledge related to (1) infant sleep position, (2) sleep location and (3) items in the sleep environment were collected.
2.3.3 Maintenance
Finally, Maintenance was measured using data collected by KIDS Network staff regarding the proportion of SSIs certified in Fiscal Year 2022 who attended the recertification training and certified for the following year (Fiscal Year 2023).
2.4 Data analysis
KIDS Network staff collected, deidentified and entered conference evaluation data into a secure online database. Post-conference data were collected, deidentified, and entered into a secure online database by certified SSIs following each training. Participants were encouraged to complete the pre-and post-tests in their entirety. However, due to the voluntary nature respondents had the right to skip questions. Missing data were removed from analysis. All reported data were collected for SSIs trained in Fiscal Year 2022 (Fall 2021 cohort: October 1, 2021–September 30, 2022; Spring 2022 cohort: June 1, 2022–May 31, 2023).
Descriptive statistics were summarized using frequencies (percentages) and means (standard deviations). The 10-item SSI Training Tests and Professional Training Tests were coded as correct vs. incorrect. Differences were evaluated by Wilcoxon Signed Rank Test. The 3-item Parent/Caregiver Training Tests were coded as safe vs. unsafe and evaluated by the Mann–Whitney U-Test. The 3-item CB and CC Test responses were coded as safe vs. unsafe, and comparisons were made using McNemar for paired dichotomous variables. Alpha=0.05 for all. Statistical analyses were performed using SPSS for Windows, Version 26.0 (IBM Corp).
3 Results
3.1 SSI conference
3.1.1 RE-AIM: reach
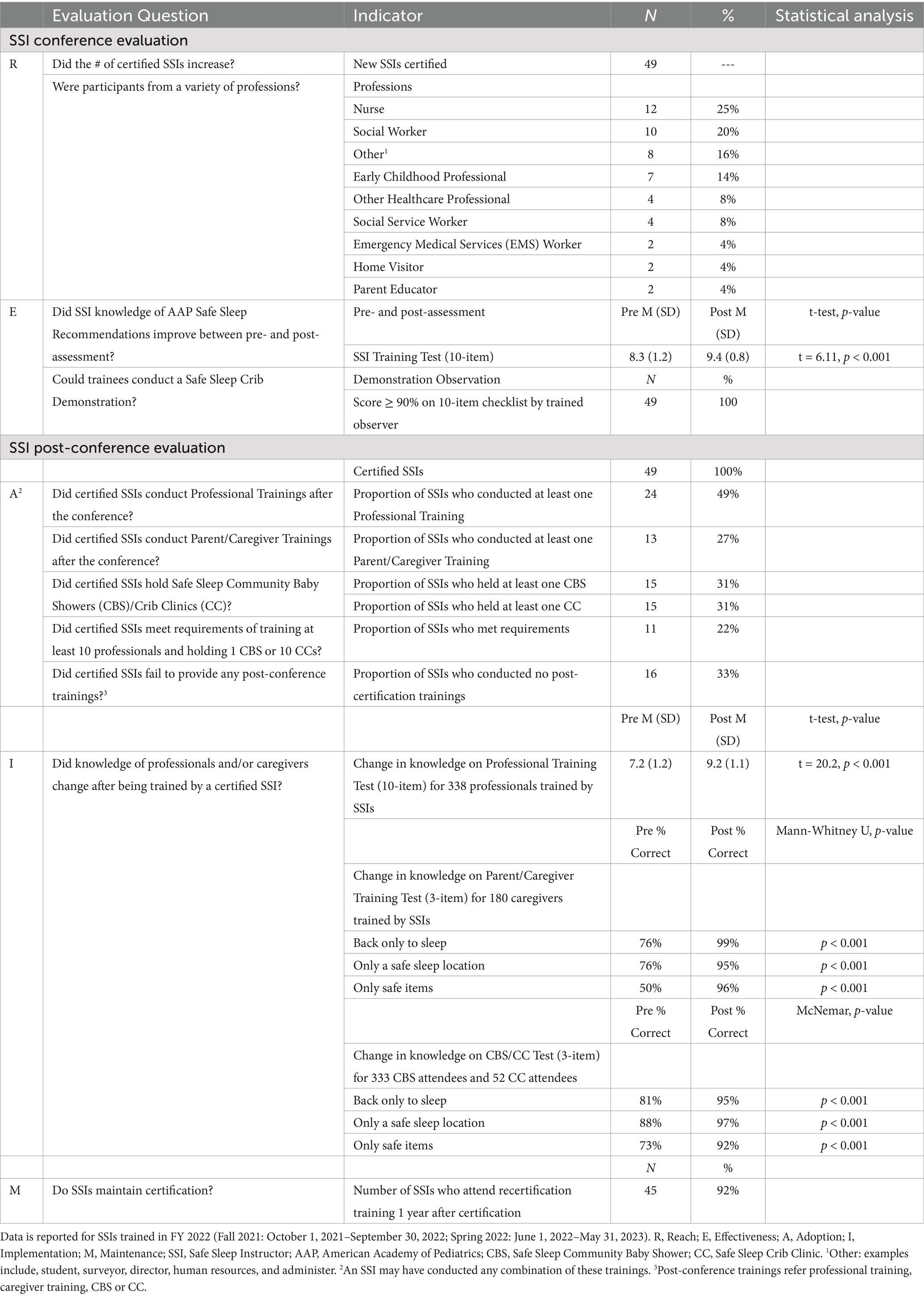
Sixty-four individuals registered for the Fall 2021 (n = 28) and Spring 2022 (n = 36) trainings, and 49 (77%) attended. Of these, 21 (43%) attended the Fall training and 28 (57%) attended the Spring training. SSI trainees represented nine professions as detailed in Table 1.
3.1.2 RE-AIM: effectiveness
Forty-four SSI trainees passed the SSI Training post-test with a score of 90% or greater. Five trainees (4 Fall; 1 Spring) scored less than 90% and received remediation. All participants passed the crib demonstration with a score of 90% or greater. All 49 trainees certified as SSIs.
3.1.3 Kirkpatrick: reaction
All 49 (100%) SSI trainees completed the post-conference evaluation. Overall, trainees agreed the topics were relevant (M = 4.98; SD = 0.14) and the training was worthwhile (M = 4.96; SD = 0.20). Trainees were very satisfied with the training (M = 4.94; SD = 0.24).
3.1.4 Kirkpatrick: learning
On the evaluation, SSI trainees reported the materials presented were understandable (M = 4.96; SD = 0.20), most information was new (M = 3.92; SD = 1.05) and they gained insight into safe infant sleep (M = 4.88; SD = 0.33). Trainees were extremely likely to intend to provide safe sleep education in their community (M = 4.92; SD = 0.27). When asked about post-conference training requirements, trainees felt prepared to facilitate a Parent or Caregiver Training (M = 4.78; SD = 0.46), a Professional Training (M = 4.63; SD = 0.60), a Safe Sleep Crib Clinic (M = 4.73; SD = 0.53), and a Safe Sleep Community Baby Shower (M = 4.41; SD = 0.81).
3.2 Post-conference
3.2.1 RE-AIM: adoption
Since certification, 24 (49%) SSIs conducted professional trainings, of those, 16 (67%) trained at least 10 professionals. Thirteen (27%) SSIs conducted parent/caregiver trainings and of these, 6 (46%) trained at least 10 parent/caregivers. Fifteen (31%) SSIs hosted at least one CBS. Fifteen (31%) SSIs facilitated CCs, with 4 (27%) facilitating at least 10. Eleven (22%) SSIs completed the post-conference trainings at levels requested.
3.2.2 Kirkpatrick: behavior
Of the 49 SSIs certified, 16 (33%) conducted no post-certification trainings.
3.2.3 RE-AIM: implementation
After being trained by a certified SSI, statistically significant increases in participant knowledge were observed between Professional Training (n = 338), Parent/Caregiver Training (n = 180), and CBS/CC (n = 385) pre- and post-tests.
3.2.4 RE-AIM: maintenance
Forty-five (92%) SSIs recertified for Fiscal Year 2023. Of the 33 SSIs who provided at least one training, 31 (94%) recertified. Of the 16 who conducted no post-certification trainings, 14 (89%) recertified with commitment to provide trainings at requested levels in Fiscal Year 2023.
4 Discussion
Despite promotion of evidence-based risk reduction strategies for nearly 30 years, SUID remains a primary cause of infant mortality. Many sleep-related deaths are likely due to modifiable factors. The Kansas State Child Death Review Board reported 98% of SUID deaths in 2020 had external contributing factors such as unsafe sleep location (35). While safe sleep interventions have shown some success (17), implementation science is needed to facilitate the translation of the AAP Safe Sleep Recommendations into behavioral practice (25).
This study offers a preliminary application of dissemination and implementation science to the promotion of the AAP Safe Sleep Recommendations through a train-the-trainer program. In terms of RE-AIM (29, 30), findings regarding SSI program success were mixed. Reach (SSIs trained), Effectiveness (change in knowledge of SSIs), Implementation (change in knowledge of those trained by SSIs) and Maintenance (recertification of SSIs) were high, suggesting merits in terms of ability to build a program infrastructure for dissemination of safe sleep education. However, Adoption (post-certification trainings provided by SSIs) fell far below expectations with 22% of SSIs providing training at the required levels. Based on Kirkpatrick Behavior (31), 33% of certified SSIs engaged in no post-certification activity suggesting no individual or organizational impact from the SSI training for those participants.
Low Adoption, when training effectiveness has been established, is an indicator that program modifications are needed to ensure uptake. Variables impacting Adoption are likely multifaceted and involve a confluence of program, individual, organizational and environmental factors. Most SSIs were able to engage in some level of post-certification training, but few achieved the number requested. In terms of individual factors, the variables assessed related to Kirkpatrick Reaction and Learning (31), such as perceived relevance and confidence, were high for all trainees. Differences in SSIs’ professions may have acted as a facilitator or barrier in training certain audiences or engaging in different training formats. Other demographic or individual characteristics not measured may have also impacted Adoption but were beyond the scope of this study.
In terms of environmental factors, population density may have limited access to both professionals and perinatal persons in frontier areas of Kansas. Further, during FY22, some COVID-19 restrictions were still in effect and may have limited ability to conduct trainings and community events, especially for pregnant participants (32, 36–38). It is also possible that other community-level factors, such as cultural beliefs about infant sleep, impacted SSIs’ ability to engage the local populace.
Many SSIs engaged in certification due to their job (39), therefore, organizational factors must also be taken into consideration regarding Adoption. For example, many healthcare and public health organizations experienced reductions in maternal/infant services due to shifting of staff responsibilities to focus on COVID-related activities (e.g., vaccination, enhance safety measures) (36). While priority was given to SSI applicants who expressed organizational support, the level of institutional buy-in for safe sleep initiatives was not assessed. Competing or conflicting priorities at the organizational level may have also impacted an SSI’s ability to conduct trainings. Strategies to improve Adoption should address perceived value of providing safe sleep training from organization/employer’s perspective. Examination of additional characteristics, including organization size, type and structure may further elucidate barriers to engaging in post-conference dissemination.
To increase Adoption, SSIs must have the capacity, resources and expertise necessary to comply with program requirements. These factors are necessary to ensure program fidelity, so all SSIs deliver consistent messages regarding safe infant sleep practices. Evaluation of Adoption in subsequent years can help determine whether challenges were pandemic-related or reflect additional barriers in disseminating safe sleep education. Qualitative interviews with current SSIs may also help identify barriers and facilitators to Adoption. Mixed methods designs are particularly useful for initiatives where the goal is to learn about adaptability and use (40), which can support informed decision-making about implementation and translation (41). In addition to interviews, observation of SSIs conducting training (e.g., CBS) may identify program structure or contextual factors that could help improve post-certification dissemination activities. A better understanding of impediments to Adoption may assist with identifying pragmatic ways to tailor the program in different settings.
Once SSI needs are better understood, program modifications should be considered in determining the best way to increase Adoption. For example, within the SSI program, there may be benefits to offering “tracts” where SSIs specialize in educating either professionals or families as many SSIs had success with one group but not the other. Allowing for adaptability of the program, to better meet the needs of SSIs and their organizations is necessary to enhance program effectiveness. Throughout the certification training, SSIs are challenged to consider adaptations to best meet their community needs, such as addressing local cultural beliefs and identifying key partners to reach priority populations. However, the lower levels of Adoptions suggest broader adaptations of the SSI program may be needed, especially as the program is integrated into new settings.
It may also be useful to partner with external organizations whose staff are seeking SSI certification to establish policies and infrastructure to ensure institutional support for success. For example, hospitals that have or are working on the Cribs for Kids’ National Safe Sleep Hospital Certification (42) may benefit from having an SSI on staff. The Hospital Certification requires a system-wide policy, annual staff training, education to families and provision of cribs to families in need, all of which could be supported by a certified SSI. Better understanding partnership opportunities can facilitate program changes most likely to increase Adoption by SSIs.
With over 35,000 births in Kansas annually, it will be necessary to reach a critical mass to eliminate sleep-related infant deaths. Utilizing implementation science strategies to enhance Adoption is necessary to strengthen sustainability of the program as cost of retaining SSIs is much lower than identifying and certifying new trainees. In addition to strategies outlined above, behavioral measures regarding professional dissemination of safe sleep information following training by an SSI, and use of safe sleep practices following Safe Sleep CBS/CCs could be incorporated into future studies. Iterative applications of the RE-AIM framework and Kirkpatrick Evaluation Model should be applied to determine impact of strategies to increase Adoption over the course of program implementation (29–31).
4.1 Limitations
This study has several limitations. The SSI conference took place in, and most participants were from, a Midwestern state in the US. This may impact generalizability of findings related to conferences in other locations. Evaluation of Reach was limited as the distribution of SSI certification training invitations included listservs and professional groups that could not be quantified, and recipients were encouraged to share the invitation with others. Many of the variables assessed were collected based on self-report (e.g., self-assessed knowledge change, behavioral intentions) and may have been impacted by social desirability bias. There was no follow-up to assess long-term knowledge change (professionals, parents/caregivers) or behavior change (perinatal persons) following training by the SSIs. Kirkpatrick Results (31) were unable to be assessed with program data, however future reports on state Pregnancy Risk Assessment Monitoring System (PRAMS) findings related to infant sleep practices may offer some insight. In addition, the ultimate outcome of this intervention, reduced SUID rates, was beyond the scope of this evaluation due to the delay in availability of infant mortality data. Long-term SUID trends will be monitored, using state vital statistics reports, though causation cannot be assumed.
5 Conclusion
This study offers a preliminary application of dissemination and implementation science to the promotion of the AAP Safe Sleep Recommendations through a train-the-trainer program. Utilizing the RE-AIM framework and Kirkpatrick Evaluation Model allowed investigators to apply well-established models to clearly identify strengths and limitations of the current program (29–31). The SSI certification was successful in terms of Reach, Effectiveness, Implementation and Maintenance. Kirkpatrick Reaction and Learning also had positive findings. Adoption was less than expected. Enhancing adaptability of the certification requirements may increase success and sustainability of the program. Further refinement of program expectations enhanced post-conference support for Adoption activities, and opportunities for tailoring may enhance Adoption efforts. Future studies will further assess characteristics that impact Adoption in order to enhance promotion of SUID risk reduction strategies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
CA-S: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. CS: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing. AH: Conceptualization, Formal analysis, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. MT: Conceptualization, Investigation, Methodology, Writing – review & editing. SK: Conceptualization, Writing – review & editing. ZK: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This project is supported in part by the Kansas Department of Health and Environment’s Bureau of Family Health Maternal and Child Health Services Block Grant #B04MC30614 funded by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS). This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government. This project is also supported in party by Grant 1R13HS027541-01A1 from the Agency for Healthcare Research and Quality (AHRQ). The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.
Abbreviations
AAP, American Academy of Pediatrics; SUID, Sudden unexpected infant death; SSI, Safe Sleep Instructor; RE-AIM Framework, Reach, Effectiveness, Adoption, Implementation, and Maintenance framework; CBS, Safe Sleep Community Baby Shower; CC, Safe Sleep Crib Clinic; COVID-19, Coronavirus disease 2019.
References
1. Moon, RY, Carlin, RF, and Hand, ITask Force on Sudden Infant Death Syndrome and the Committee on Fetus and Newborn. Evidence base for 2022 updated recommendations for a safe infant sleeping environment to reduce the risk of sleep-related infant deaths. Pediatrics. (2022) 150:e2022057991. doi: 10.1542/peds.2022-057991
2. Moon, RY, Carlin, RF, and Hand, ITask Force on Sudden Infant Death Syndrome and the Committee on Fetus and Newborn. Sleep-related infant deaths: updated 2022 recommendations for reducing infant deaths in the sleep environment. Pediatrics. (2022) 150:e2022057990. doi: 10.1542/peds.2022-057990
3. Centers for Disease Control and Prevention. Sudden unexpected infant death and sudden infant death syndrome: data and statistics. (2021). Available at: https://www.cdc.gov/sudden-infant-death/data-research/data/?CDC_AAref_Val=https://www.cdc.gov/sids/data.htm (Accessed May 26, 2023).
4. National Institute of Child Health and Human Development, US Department of Health and Human Services. Safe to sleep: public education campaign. (2021). Available online at: https://safetosleep.nichd.nih.gov/ (Accessed April 28, 2021).
5. Moon, RY, Oden, RP, and Grady, KC. Back to sleep: an educational intervention with women, infants, and children program clients. Pediatrics. (2004) 113:542–7. doi: 10.1542/peds.113.3.542
6. Moon, RY, Hauck, FR, and Colson, ER. Safe infant sleep interventions: what is the evidence for successful behavior change? Curr Pediatr Rev. (2016) 12:67–75. doi: 10.2174/1573396311666151026110148
7. Salm Ward, TC, and Balfour, GM. Infant safe sleep interventions, 1990-2015: a review. J Community Health. (2016) 41:180–96. doi: 10.1007/s10900-015-0060-y
8. Von Kohorn, I, Corwin, MJ, Rybin, DV, Heeren, TC, Lister, G, and Colson, ER. Influence of prior advice and beliefs of mothers on infant sleep position. Arch Pediatr Adolesc Med. (2010) 164:363–9. doi: 10.1001/archpediatrics.2010.26
9. Hirai, AH, Kortsmit, K, Kaplan, L, Reiney, L, Warner, L, Parks, SE, et al. Prevalence and factors associated with safe infant sleep practices. Pediatrics. (2019) 144:e20191286. doi: 10.1542/peds.2019-1286
10. Robida, D, and Moon, RY. Factors influencing infant sleep position: decisions do not differ by SES in African-American families. Arch Dis Child. (2012) 97:900–5. doi: 10.1136/archdischild-2011-301360
11. Colson, ER, McCabe, LK, Fox, K, Levenson, S, Colton, T, Lister, G, et al. Barriers to following the back-to-sleep recommendations: insights from focus groups with inner-city caregivers. Ambul Pediatr. (2005) 5:349–54. doi: 10.1367/A04-220R1.1
12. Vilvens, HL, Vaughn, LM, Southworth, H, Southworth, H, Denny, SA, and Gittelman, MA. Personalising safe sleep messaging for infant caregivers in the United States. Health Soc Care Community. (2020) 28:891–902. doi: 10.1111/hsc.12920
13. Ajao, TI, Oden, RP, Joyner, BL, and Moon, RY. Decisions of black parents about infant bedding and sleep surfaces: a qualitative study. Pediatrics. (2011) 128:494–502. doi: 10.1542/peds.2011-0072
14. Caraballo, M, Shimasaki, S, Johnston, K, Tung, G, Albright, K, and Halbower, AC. Knowledge, attitudes, and risk for sudden unexpected infant death in children of adolescent mothers: a qualitative study. J Pediatr. (2016) 174:78–83.e2. doi: 10.1016/j.jpeds.2016.03.031
15. Gaydos, LM, Blake, SC, Gazmararian, JA, Woodruff, W, Thompson, WW, and Dalmida, SG. Revisiting safe sleep recommendations for African-American infants: why current counseling is insufficient. Matern Child Health J. (2015) 19:496–503. doi: 10.1007/s10995-014-1530-z
16. Joyner, BL, Oden, RP, Ajao, TI, and Moon, RY. Where should my baby sleep: a qualitative study of African American infant sleep location decisions. J Natl Med Assoc. (2010) 102:881–9. doi: 10.1016/s0027-9684(15)30706-9
17. Moon, RY, Oden, RP, Joyner, BL, and Ajao, TI. Qualitative analysis of beliefs and perceptions about sudden infant death syndrome in African-American mothers: implications for safe sleep recommendations. J Pediatr. (2010) 157:92–97.e2. doi: 10.1016/j.jpeds.2010.01.027
18. Oden, RP, Joyner, BL, Ajao, TI, and Moon, RY. Factors influencing African American mothers' decisions about sleep position: a qualitative study. J Natl Med Assoc. (2010) 102:870–80. doi: 10.1016/s0027-9684(15)30705-7
19. Zoucha, R, Walters, CA, Colbert, AM, Carlins, E, and Smith, E. Exploring safe sleep and SIDS risk perception in an African-American community: focused ethnography. Public Health Nurs. (2016) 33:206–13. doi: 10.1111/phn.12235
20. Moon, RY, Kington, M, Oden, R, Iglesias, J, and Hauck, FR. Physician recommendations regarding SIDS risk reduction: a National Survey of pediatricians and family physicians. Clin Pediatr. (2007) 46:791–800. doi: 10.1177/0009922807303894
21. Thornhill-Scott, F, Dong, F, Redmond, M, and Ablah, E. Physician practices regarding SIDS in Kansas. Clin Pediatr. (2017) 56:759–65. doi: 10.1177/0009922816684597
22. Pease, A, Ingram, J, Blair, PS, and Fleming, PJ. Factors influencing maternal decision-making for the infant sleep environment in families at higher risk of SIDS: a qualitative study. BMJ Paediatr Open. (2017) 1:e000133. doi: 10.1136/bmjpo-2017-000133
23. Mosley, JM, Daily Stokes, S, and Ulmer, A. Infant sleep position: discerning knowledge from practice. Am J Health Behav. (2007) 31:573–82. doi: 10.5555/ajhb.2007.31.6.573
24. Taylor, J, Novoa, C, Hamm, K, and Phadke, SThe Center for American Progress. Eliminating racial disparities in maternal and infant mortality: a comprehensive policy blueprint. (2019). Available online at: www.americanprogress.org/article/eliminating-racial-disparities-maternal-infant-mortality/ (Accessed February 1, 2024).
25. Overpeck, MD, Cruz, TH, and McKenzie, LB. Advancing safe sleep for infants through translational research. Inj Prev. (2013) 19:442–2. doi: 10.1136/injuryprev-2013-041083
26. Ahlers-Schmidt, CR, Schunn, C, Engel, M, Dowling, J, Neufeld, K, and Kuhlmann, S. Implementation of a statewide program to promote safe sleep, breastfeeding and tobacco cessation to high risk pregnant women. J Community Health. (2019) 44:185–91. doi: 10.1007/s10900-018-0571-4
27. Colson, ER, Levenson, S, Rybin, D, Calianos, C, Margolis, A, Colton, T, et al. Barriers to following the supine sleep recommendation among mothers at four centers for the women, infants, and children program. Pediatrics. (2006) 118:e243–50. doi: 10.1542/peds.2005-2517
28. Ahlers-Schmidt, CR, Schunn, C, Kuhlmann, S, Kuhlmann, Z, and Engel, M. Developing a state-wide infrastructure for safe sleep promotion. Sleep Health. (2017) 3:296–9. doi: 10.1016/j.sleh.2017.05.010
29. Glasgow, RE, Harden, SM, Gaglio, B, Rabin, B, Smith, ML, Porter, GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. (2019) 7:64. doi: 10.3389/fpubh.2019.00064
30. Glasgow, RE, Vogt, TM, and Boles, SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. (1999) 89:1322–7. doi: 10.2105/ajph.89.9.1322
31. Kirkpatrick, DL, and Kirkpatrick, JD. Evaluating training programs: The four levels (Third Edition). San Francisco: Berrett-Koehler Publishers Inc (2006).
32. Ahlers-Schmidt, CR, Schunn, C, Hervey, AM, Torres, AM, Torres, M, Sage, C, et al. Infant safe sleep promotion: increasing capacity of child protective services employees. Int J Environ Res Public Health. (2021) 18:4227. doi: 10.3390/ijerph18084227
33. Ahlers-Schmidt, CR, Schunn, C, Hervey, AM, and Torres, M. Safe sleep crib clinics: promoting risk reduction strategies for sudden unexpected infant death. PEC Innovation. (2024) 6:100370. doi: 10.1016/j.pecinn.2024
34. Kansas Department of Health and Environment (KDHE). Kansas Infant Mortality & Stillbirth Report, 2020. (2022). Available online at: www.kdhe.ks.gov/DocumentCenter/View/24431/Infant-Mortality-Report-2020-PDF (Accessed May 26, 2023).
35. Kansas State Child Death Review Board. 2022 Annual Report (2020 Data). (2022). Available online at: https://www.ag.ks.gov/home/showpublisheddocument/10878/638461048654200000 (Accessed May 26, 2023).
36. Ahlers-Schmidt, CR, Hervey, AM, Neil, T, Kuhlmann, S, and Kuhlmann, Z. Concerns of women regarding pregnancy and childbirth during the COVID-19 pandemic. Patient Educ Couns. (2020) 103:2578–82. doi: 10.1016/j.pec.2020.09.031
37. Blebu, BE, Kuppermann, M, Coleman-Phox, K, Karasek, D, Lessard, L, and Chambers, BD. A qualitative exploration of experiences accessing community and social services among pregnant low-income people of color during the COVID-19 pandemic. Womens Health. (2023) 19:19. doi: 10.1177/17455057231156792
38. Pasadino, F, DeMarco, K, and Lampert, E. Connecting with families through virtual perinatal education during the COVID-19 pandemic. MCN Am J Matern Child Nurs. (2020) 45:364–70. doi: 10.1097/NMC.0000000000000665
39. RE-AIM: Improving Public Health Relevance and Population Health Impact. Improving adoption. (2023). Available online at: https://re-aim.org/learn/what-is-re-aim/adoption/improving-adoption/ (Accessed May 26, 2023).
40. Worthen, BR, Sanders, JR, and Fitzpatrick, JL. Program evaluation: Alternative approaches and practical guidelines (2nd Edition). New York: Longman Pub Group (1996).
41. Cross, JE, Dickmann, E, Newman-Gonchar, R, and Fagan, JM. Using mixed-method design and network analysis to measure development of interagency collaboration. Am J Eval. (2009) 30:310–29. doi: 10.1177/1098214009340044
42. Cribs for Kids. The National Safe Sleep Hospital Certification Program. (2024). Available online at: https://cribsforkids.org/hospitalcertification/ (Accessed November 18, 2024)
Keywords: RE-AIM framework, implementation science, safe sleep education, sudden unexpected infant death (SUID), sleep-related death
Citation: Ahlers-Schmidt CR, Schunn C, Hervey AM, Torres M, Kuhlmann S and Kuhlmann Z (2025) Using the Reach, Effectiveness, Adoption, Implementation, and Maintenance framework to evaluate a state-wide safe infant sleep education program for continuous improvement. Front. Public Health. 13:1540451. doi: 10.3389/fpubh.2025.1540451
Edited by:
Jeanine Young, University of the Sunshine Coast, AustraliaReviewed by:
John Pascoe, Wright State University, United StatesViviana Elizabeth Rodriguez, Institute for Clinical Effectiveness and Health Policy (IECS), Argentina
Copyright © 2025 Ahlers-Schmidt, Schunn, Hervey, Torres, Kuhlmann and Kuhlmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carolyn R. Ahlers-Schmidt, Y3NjaG1pZHQzQGt1bWMuZWR1
 Carolyn R. Ahlers-Schmidt
Carolyn R. Ahlers-Schmidt Christy Schunn
Christy Schunn Ashley M. Hervey1,2
Ashley M. Hervey1,2