- 1School of Nursing, Jiangxi Medical College, Nanchang University, Nanchang, China
- 2Department of General Surgery, The First Affiliated Hospital of Nanchang University, Nanchang, China
Introduction: Frailty is prevalent among preoperative gastric cancer (GC) patients and significantly affects surgical risk and long-term recovery. Family health may hold substantial potential for mitigating frailty, although the mechanisms underlying this effect remain unclear. This study aims to investigate the impact of family health on frailty in preoperative GC patients, and the mediating effects of health literacy and physical activity.
Methods: A total of 240 patients scheduled for radical gastrectomy at a tertiary hospital in China were surveyed using Family Health Scale (FHS), Health Literacy Scale (HLS-SF), International Physical Activity Questionnaire (IPAQ-7), and Tilburg Frailty Indicator (TFI). Data were analyzed using independent t-tests, χ2 tests, Pearson’s correlation, and binary logistic regression. Mediation analysis with Structural Equation Modeling (SEM) was then applied to explore the relationships between variables.
Results: Family health in preoperative GC patients was negatively correlated with frailty (r = −0.791, p < 0.01) and positively correlated with both health literacy (r = 0.806, p < 0.01) and physical activity (r = 0.464, p < 0.01). Mediating effect analysis indicated that the direct effect of family health on frailty was −0.837, while health literacy and physical activity served as partial mediators in this relationship, with indirect effects of −0.332 and −0.095 (both p < 0.01), respectively. The mediating effects accounted for 33.83% of the total effect.
Conclusion: Family health directly affects frailty and also exerts an indirect impact through the mediators of health literacy and physical activity. These findings suggest that healthcare professionals should focus on vulnerable populations with low family health and implement family-centered preoperative frailty interventions. Guiding GC patients to improve health literacy and engage in personalized family-based exercises can help delay or reverse preoperative frailty, promoting long-term recovery outcomes.
1 Introduction
According to the latest data released by the International Agency for Research on Cancer (IARC), there are approximately 968,000 new cases of gastric cancer (GC) and 660,000 deaths globally (1). In China, GC ranks third in both incidence and mortality among all cancers, with an overall 5-year survival rate of less than 50%, making it a significant public health concern (2). Currently, surgical resection remains the preferred approach for achieving radical cure and improving long-term survival in GC patients. As the population ages at an unprecedented rate, individuals aged 60 and older now account for 70.8% of all GC cases, with an increasing proportion of patients in this age group undergoing gastrectomy. However, due to a combination of factors such as aging, tumor-related metabolic disturbances, and nutritional and skeletal muscle abnormalities, preoperative GC patients often exhibit frailty symptoms, including weight loss, fatigue, reduced grip strength and decreased pace (3). Frailty refers to a homeostatic imbalance of dysfunction, decreased physiological reserve, increased vulnerability, and decreased anti-stress capacity after a stressor event (4), and is clinically dynamic and reversible (5). A systematic review (6) reported that the incidence of frailty in GC patients ranges from 10 to 71%, with an overall prevalence of 29%. Preoperative frailty not only increases surgical risks (7), but also predisposes patients to a range of adverse health outcomes postoperatively, including increased complications, prolonged hospital stays, disability, and mortality, which significantly affect long-term recovery (8, 9). Therefore, preoperative frailty management in GC patients is crucial.
In recent years, the concept of “family health” has garnered increasing attention within the academic community, with a growing number of studies both domestically and internationally focusing on family-based health promotion and disease management (10, 11). “Family health” refers to a resource at the family unit level, arising from the interplay of the health, abilities, behaviors, personalities, and interactions of each family member, as well as the family’s physical, social, emotional, economic, and medical resources (12). Numerous studies have underscored the indispensable role of families in providing care for individuals with chronic diseases, disabilities, and frailty. In fact, the economic value generated by family-based caregiving is estimated to be 2–6 times greater than that of formal healthcare systems (13). Despite this substantial contribution, the potential of family-centered approaches to mitigate frailty, optimize public health resource allocation, and curtail healthcare costs remains largely untapped. Currently, domestic frailty management strategies predominantly concentrate on individual-level interventions, thereby overlooking the family as a central health-promoting entity.
Health literacy and physical activity, as modifiable cognitive and behavioral factors, have demonstrated efficacy in improving individual frailty outcomes, offering a crucial avenue for understanding the relationship between family health and frailty. Health literacy is defined as the ability of individuals to access, comprehend, and utilize basic health information to promote their own health (14). This capability is often influenced by factors such as family structure, income level, and the educational background of family members (15). Research indicates that low health literacy is associated with patients’ inadequate understanding of their disease status and poor self-care abilities, which can adversely affect disease management and health outcomes in individuals with chronic conditions (16). Therefore, enhancing patients’ health literacy is anticipated to help prevent the onset of preoperative frailty. Furthermore, physical activity is a key and significant indicator of bodily functions. Research has demonstrated that supportive interactions and shared values regarding healthy behaviors within a family can influence the level of physical activity individuals engage in Wunsch et al. (17). Previous studies have also established that exercise frequency serves as a crucial predictor of frailty (18). However, previous research has yet to explore the mediating effects of these factors in the context of how family health influences preoperative frailty.
In this study, we hypothesized that family health is negatively associated with frailty, and that health literacy and physical activity partially mediate the relationship between the two. To test this hypothesis, we conducted a cross-sectional survey at a tertiary hospital in China. The study aimed to provide clinicians with a cost-effective and evidence-based strategy to reduce preoperative frailty risk in GC patients while offering theoretical insights for the development of family-friendly healthcare policies and support systems, particularly in the face of an aging population and increasingly strained healthcare resources.
2 Materials and methods
2.1 Study design and participants
This cross-sectional study was conducted in accordance with STROBE Statement (19). A convenience sampling method was employed to select 240 patients scheduled for radical gastrectomy at the First Affiliated Hospital of Nanchang University in China, between November 2023 and April 2024. Inclusion criteria include: Aged ≥ 18 years; A confirmed diagnosis of primary GC according to the China Standardization for Diagnosis and Treatment of Gastric Cancer (2022 edition) (20); United States Society of anesthesiologists (ASA) classification (21) Class I–III; Waiting for the first radical gastrectomy at our hospital. Exclusion criteria included: preoperative chemoradiotherapy; Concomitant other primary malignancies or serious medical diseases; critically ill and in the acute phase; Have a history of psychiatric illness or cognitive dysfunction; Severe limitations in hearing, vision, or speech impairment. The sample size was determined based on the empirical criterion that the sample size for Structural Equation Modeling (SEM) should be ≥150 (22). All study subjects gave informed consent and voluntarily participated in this study.
2.2 Survey instruments
2.2.1 General information questionnaire
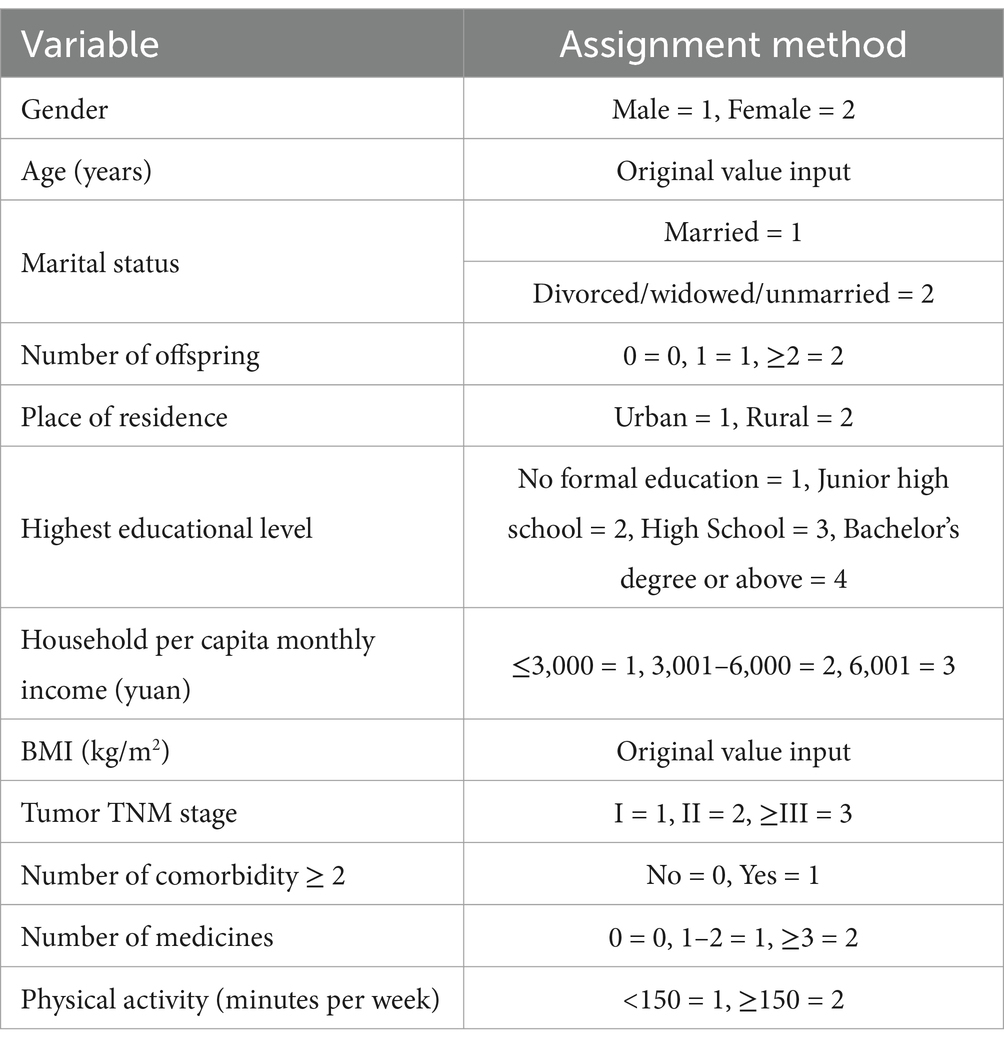
The General Information Questionnaire was designed to collect general demographic and health-related data of patients. Demographic data include gender, age, marital status, number of offspring, place of residence, highest educational level, household per capita monthly income, etc.; Health-related information included Body Mass Index (BMI), tumor TNM stage, number of comorbidity and number of medicines.
2.2.2 Family health scale (FHS)
The FHS was developed by Crandall et al. (23) and revised into Chinese by Wang et al. (24), to assess participants’ family health functioning. The scale includes 4 dimensions of family social and emotional wellbeing process, social approach to family health, family health resources, and social support outside the family, with a total of 10 items, and is scored on a 5-level Likert scale (1 = strongly disagree, 2 = somewhat disagree, 3 = neither agree nor disagree, 4 = somewhat agree, 5 = strongly agree), with questions 6, 9, and 10 being scored backwards. The total score of the scale is between 10 and 50 points, and the higher the score, the better the level of family health. The Cronbach’s α coefficient was 0.830 for the Chinese version of the scale. This study Cronbach’s α coefficient of 0.814.
2.2.3 Health literacy scale short form (HLS-SF4)
Originally developed by Duong et al. (15) and subsequently adapted and simplified by domestic scholars Sun et al. (25). It was simplified to a 4-item version using Classical Test Theory and the Mokken model to measure public health literacy. The HLS-SF4 comprises three dimensions: healthcare, health promotion, and disease prevention. It utilizes a 4-point Likert scale for scoring (1 = very difficult, 2 = difficult, 3 = easy, 4 = very easy), with total scores ranging from 4 to 16, where a higher scores indicate a greater level of health literacy. The HLS-SF4 has demonstrated strong reliability and validity, with a Cronbach’s α coefficient of 0.842 and an intraclass correlation coefficient (ICC) for criterion validity of 0.892 (95% CI: 0.886–0.899), making it a reliable and concise tool for measuring health literacy. In our research, the Cronbach’s α coefficient for the HLS-SF4 was 0.801.
2.2.4 The international physical activity questionnaire (IPAQ-7)
The IPAQ-7 (26) assesses participants’ activities in terms of heavy physical activity, moderate physical activity, and walking in the past week. It contains a total of 7 items. The exercise duration is calculated by summing all the activity time (minutes). Physical activity levels were assessed based on previous studies, with 150 min of exercise per week deemed to be a healthy benchmark (27). If individuals engaged in physical activity for less than 150 min per week, their activity levels were not considered sufficient.
2.2.5 Tilburg frailty indicator (TFI)
The TFI developed by Netherlands Tiburg University scholar Gobbens et al. (28) based on the frailty integration model, including 3 dimensions of physical frailty, psychological frailty and social frailty, a total of 15 self-report items, 11 items in the scale are “yes, no” dichotomous options, which are scored 0 or 1 respectively, and the remaining 4 items are “yes, sometimes, no” tricategorical options, with intermediate values 0.5 points. The total score of the scale is the sum of the scores of each item, with a range of 0–15 points, and ≥ 5 points are frailty, and the higher the score, the more severe the frailty. The TFI scale has been validated by domestic scholars, showing good reliability and validity (29). In this study, the Cronbach’s α coefficient was 0.830.
2.3 Survey methodology
A one-on-one, face-to-face questionnaire survey was conducted with GC patients 24 h before surgery by systematically trained surveyors. Prior to the survey, the purpose and methodology of completing the questionnaires were clearly explained to the patients using standardized guidance, and data collection commenced only after obtaining informed consent. For participants who were physically weak or had low educational levels and were unable to complete the questionnaires independently, investigators read the questions aloud one by one and recorded the responses on their behalf. After completing the questionnaire, participants were informed of their responses to verify accuracy, and any discrepancies were addressed by repeating the questions and answers as necessary. A total of 240 questionnaires were distributed, and 223 valid responses were collected, yielding an effective response rate of 92.92%.
2.4 Statistical methods
Data were entered into Excel using a two-person double-entry verification method. SPSS 26.0 and Amos 23.0 software were employed for data organization and statistical analysis. Measurement data conforming to a normal distribution were expressed as Mean ± Standard Deviation (SD). The independent samples t-test was employed for group comparisons. Enumeration data were presented as frequencies and percentages, with the χ2 test applied for analysis. Point-biserial correlation was used to analyze the relationship between the binary variable and continuous variables, while Pearson’s correlation coefficient was employed for the relationships among the continuous variables. Variables that demonstrated statistically significant differences in univariate analysis were included in a binary logistic regression analysis, with a significance level set at α = 0.05. In the analysis of mediating effects using SEM, frailty was treated as the dependent variable, family health as the independent variable, and health literacy and physical activity as mediating variables. The bootstrap method was utilized for significance testing; a 95% confidence interval that did not include 0 indicated the establishment of a partial mediation effect.
3 Results
3.1 General demographic data of preoperative GC patients and single factor analysis of frailty
A total of 223 patients were included in this study, of which the age of the survey group was (64.41 ± 9.75) years, mainly older adult patients. There were 147 males (65.9%) and 76 females (34.1%). As shown in Table 1, frailty scores varied by age, gender, highest educational level, household per capita monthly income, tumor TNM stage, number of comorbidity, number of medicines, and physical activity (p < 0.05).

Table 1. General demographic data of preoperative GC patients and single factor analysis of frailty (n = 223).
3.2 Family health, health literacy and frailty scale and its dimension scores of preoperative GC patients
The scores of the 3 scales and their dimensions are shown in Table 2. Among 223 preoperative GC patients, 103 (46.2%) were frail and 120 (53.8%) were non-frail.
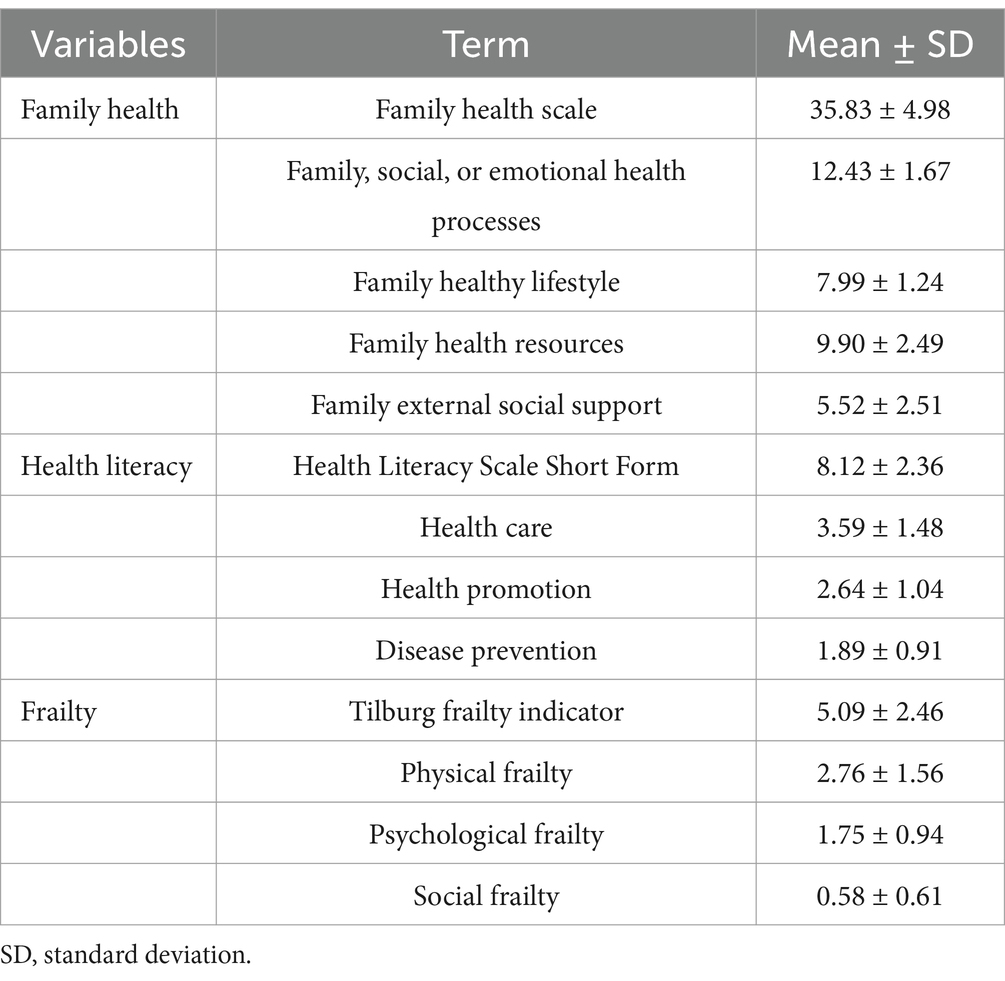
Table 2. Family health, health literacy and frailty scale and its dimension scores of preoperative GC patients (n = 223).
3.3 Correlation analysis of family health, health literacy, physical activity and frailty in preoperative GC patients
Correlation analysis showed that family health was negatively correlated with frailty (r = −0.791, p < 0.01) and positively correlated with both health literacy (r = 0.806, p < 0.01) and physical activity (r = 0.464, p < 0.01), as shown in Table 3.
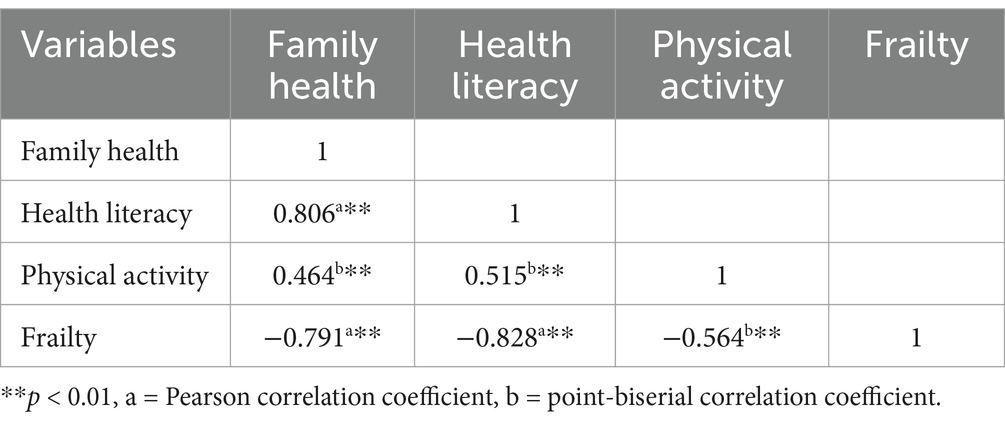
Table 3. Correlation analysis of family health, health literacy, physical activity and frailty in preoperative GC patients.
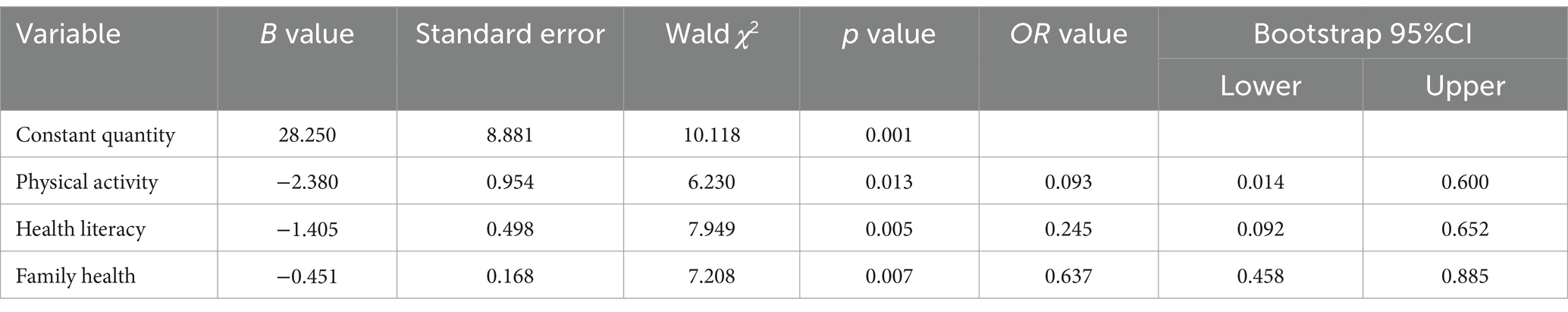
3.4 Multivariate regression analysis of frailty in preoperative GC patients
Multivariate regression analysis used the frailty score as the dependent variable, and the variables with statistically significant differences in the univariate analysis included the independent variables. The specific variable assignments are listed in Table 4. The results of the analysis showed that physical activity, health literacy, and family health were the influencing factors for frailty in preoperative GC patients (p < 0.01; Table 5).
3.5 Mediating effects of family health, health literacy and physical activity on frailty in preoperative GC patients
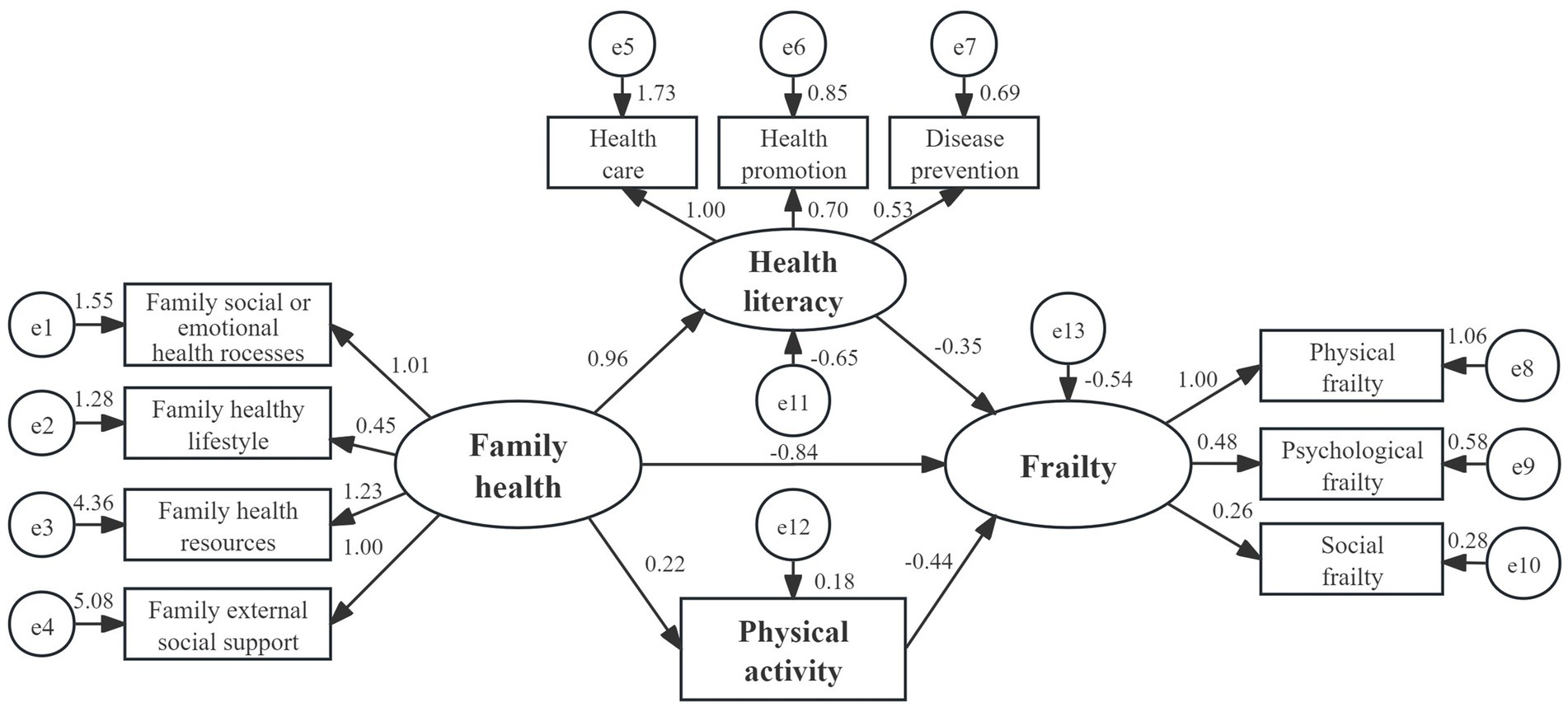
A structural equation model was constructed using Amos 23.0 software. Family health was taken as independent variable, health literacy and physical activity as intermediate variable, and frailty as dependent variable. Maximum likelihood method was used to fit the hypothetical model. The results showed that the model fit well: χ2/df = 3.121, RMSEA = 0.049, IFI = 0.919, TLI = 0.873, CFI = 0.918. The confidence interval for the mediating effect was then calculated using the bias corrected Bootstrap method, limiting 5,000 repeated samples to construct a 95% bias corrected confidence interval. The results showed that the indirect effects of family health through health literacy (95% CI = −0.597 to −0.032), physical activity (95% CI = −0.232 to −0.033) and frailty were significant, the mediating effect value is −0.332 and −0.095 (both p < 0.01), accounting for 33.83% of the total effect; meanwhile, the direct effect of family health to frailty is also significant (95% CI = −1.401 to −0.549), the effect value is −0.837 (p < 0.01), accounting for 66.17% of the total effect (Figure 1 and Table 6).
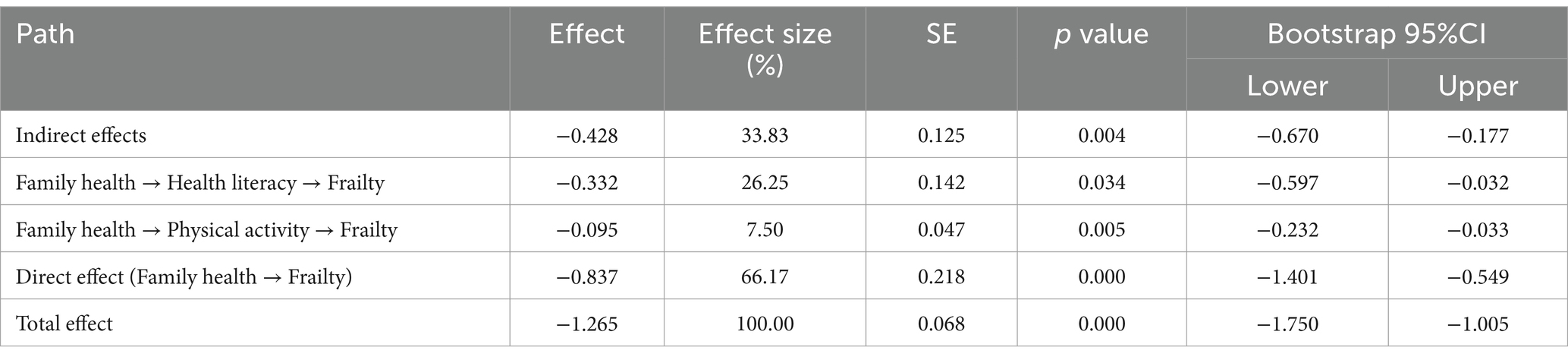
Table 6. Mediating effects of family health, health literacy and physical activity on frailty in preoperative GC patients.
4 Discussion
To our knowledge, this is the first study to investigate the effects of family health, health literacy, and physical activity on the frailty state of preoperative GC patients. The results demonstrate that family health has a direct negative effect on frailty, and health literacy and physical activity partially mediate the relationship between family health and frailty.
In this study, the prevalence of frailty among preoperative GC patients was 46.2%, with several previous studies reporting similar or lower rates (8, 30). These variations may be attributed to different national circumstances, frailty assessment tools and underlying concepts of frailty. The TFI scale utilized in this study is widely recognized for its effectiveness in the clinical multidimensional assessment of frailty, thereby enhancing the rigor and reliability of our findings. Furthermore, preoperative health promotion and prehabilitation are key strategies for improving cancer care outcomes (31) and enhance the efficiency of medical resource utilization (32). Studies have shown that early prehabilitation in preoperative frail patients is more likely to reduce surgical risks and promote long-term recovery compared to those with postoperative frailty (7). Therefore, the findings of this study provide a valuable intervention strategy for managing preoperative frailty.
The mediating effect model of this study revealed a significant direct effect between family health and frailty, with an effect size of −0.837, which accounted for 66.17% of the total effect. This indicates that a higher level of family health can effectively prevent or delay the onset and progression of frailty, acting as a protective buffer. Previous research has demonstrated a positive direct effect of family functioning on patients’ chronic disease management and health-related quality of life (33). These findings are consistent with our results, which may be attributed to factors such as emotional communication within the family, lifestyle choices of family members, access to family health resources, and external family support (24). Our study hypothesizes that positive emotional bonding among family members enhances mental resilience and coping skills in patients with GC, thereby improving their frailty condition. Chew et al. (34) also found that healthy family emotional dynamics foster resilience and are linked to improved mental and physical health outcomes, such as reduced depression and chronic pain. Additionally, health habits developed in a family environment can significantly enhance patients’ health knowledge and encourage the active adoption of healthy lifestyles, ultimately improving overall health status and mitigating the progression of frailty. Furthermore, family health resources influence the availability and quality of medical support for patients facing illness (35). Strong family health resources, coupled with external social support, enable patients to access and utilize health information more effectively, thereby better managing their frailty condition. Therefore, family health plays a crucial role in the management of frailty in preoperative GC patients.
However, current frailty research predominantly concentrates on individual-level factors, such as rehabilitation exercises, nutritional optimization, multi-component interventions, and individualized geriatric care models (7, 36). This suggests that healthcare professionals should broaden their understanding of family health, optimize and strengthen the internal relationships of patients with preoperative GC, and enhance external support for patients’ families, thereby promoting effective preoperative frailty management. Moreover, as family health serves as a negative predictor of frailty risk, clinical efforts should prioritize populations with vulnerable family health, including patients from low-income backgrounds and those with unstable family structures, such as individuals living alone, single parents, and intergenerational families. Early identification of high-risk frailty groups among preoperative GC patients, along with targeted preoperative rehabilitation measures, can significantly improve frailty status.
This study demonstrated that the negative impact of family health on frailty in preoperative GC patients can be moderated by health literacy and physical activity, with a total indirect effect value of −0.428, representing 33.83% of the overall effect. This indicates that both health literacy and physical activity play a crucial role in the relationship between family health and frailty in this patient population. Previous research (37, 38) has identified health literacy as a significant mediator between family health and outcomes such as wellbeing, family burden, and self-management among chronic disease patients, aligning with the findings of this study. Rothbaum et al. (39) describe the family as a cohesive social unit that functions like a system, autonomously establishing rules and responsibilities. In this context, it is essential for families to guide members experiencing frailty in enhancing their health literacy, which is considered a fundamental family responsibility. This study found a significant negative relationship between physical activity and the risk of frailty, corroborating previous reports (27, 40). It is speculated that, given the impaired physiological reserves of preoperative patients with GC, inadequate physical activity may further elevate inflammatory biomarkers, leading to disturbances in the body’s internal environment and nutrient loss. This, in turn, can adversely affect muscle mass, function, and strength, ultimately reducing physical activity levels and body weight, thereby contributing to frailty (41).
Against the backdrop of accelerating population aging and increasingly strained healthcare resources, this study proposes that clinical staff shift their focus from difficult-to-modify frailty biomarkers emphasized in previous research to modifiable cognitive and behavioral factors. We advocate integrating family health education and family-empowered physical activity programs into preoperative frailty management protocols for GC patients. Specifically, by enhancing patients’ understanding of health knowledge and motivation for physical activity, we encourage family members to assist in delivering systematic, evidence-based physical activity programs that include resistance training, aerobic activity, and balance exercises. This intervention strategy offers both practicality and cost-effectiveness, reducing the risk of preoperative frailty while alleviating pressure on formal healthcare systems. It aligns clearly with United Nations Sustainable Development Goal (SDG) 3 “Good Health and Well-Being” (42). By positioning families as fundamental units of health promotion, our research provides scientific evidence for achieving health equity and efficient resource utilization—key objectives outlined in SDG targets 3.4 “Reduce non-communicable disease risks” and 3.8 “Achieve universal health coverage.”
5 Limitations and future research
This study has several limitations: first, it was conducted solely in a tertiary hospital in China, which may restrict the representativeness and generalizability of the parallel mediating effect model; future multi-center studies are recommended to improve these aspects. Second, as a cross-sectional study, while it explored the potential mechanisms by which family health influences frailty through parallel mediation analysis, the actual causal relationships require further investigation through prospective longitudinal studies. Third, the two mediating variables in this study—health literacy and physical activity—accounted for 33.83% of the total effect of family health on frailty, suggesting their roles are limited. Family health is a holistic concept associated with individual health, integrating fundamental elements such as family structure, function, and social networks (35). Likewise, frailty is a complex, multi-dimensional state influenced by various physiological, psychological, and social factors (43). Future research is recommended to broaden its scope by incorporating additional health behavior factors related to frailty, such as nutritional intake and emotional self-regulation, and to explore more potential pathways through which family health may influence frailty. This will provide a more comprehensive basis for developing family-centered, multi-collaborative preoperative frailty intervention programs.
6 Conclusion
The analysis of the mediating effects in this study indicates that family health has both direct and indirect predictive effects on the risk of frailty, with health literacy and physical activity serving as partial mediators. Therefore, it is recommended that healthcare professionals prioritize vulnerable groups with compromised family health, such as patients from low socioeconomic backgrounds or with unstable family structures. Implementing preoperative rehabilitation measures that focus on family involvement can guide patients in enhancing their health literacy and increasing their physical activity levels, thereby effectively reducing the risk of frailty in preoperative GC patients and promoting long-term rehabilitation outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving humans were approved by the Medical Ethics Research Committee of the First Affiliated Hospital of Nanchang University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HX: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. CH: Conceptualization, Writing – review & editing, Resources. YG: Data curation, Writing – review & editing. XM: Formal analysis, Writing – review & editing. ZX: Supervision, Writing – review & editing. JG: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the 2022 Science and Technology Plan of the Health and Health Commission of Jiangxi Province (202211348) and the project “Development of a Virtual Simulation System for Chronic Diseases” (HX202305080003).
Acknowledgments
The authors express gratitude for the invaluable contributions of the participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bray, F, Laversanne, M, Sung, H, Ferlay, J, Siegel, RL, Soerjomataram, I, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2024) 74:229–63. doi: 10.3322/caac.21834
2. He, F, Wang, S, Zheng, R, Gu, J, Zeng, H, Sun, K, et al. Trends of gastric cancer burdens attributable to risk factors in China from 2000 to 2050. Lancet Reg Health West Pac. (2024) 44:101003. doi: 10.1016/j.lanwpc.2023.101003
3. Liang, H, and Hu, A. Frailty and long-term survival of patients with gastric cancer: a meta-analysis. Front Oncol. (2023) 13:1239781. doi: 10.3389/fonc.2023.1239781
4. Hoogendijk, EO, Afilalo, J, Ensrud, KE, Kowal, P, Onder, G, and Fried, LP. Frailty: implications for clinical practice and public health. Lancet. (2019) 394:1365–75. doi: 10.1016/S0140-6736(19)31786-6
5. Deng, Y, Zhang, K, Zhu, J, Hu, X, and Liao, R. Healthy aging, early screening, and interventions for frailty in the elderly. Biosci Trends. (2023) 17:252–61. doi: 10.5582/bst.2023.01204
6. Tang, W-Z, Tan, Z-K-K, Qiu, L-Y, Chen, J-Q, and Jia, K. Prevalence and unfavorable outcome of frailty in older adults with gastric cancer: a systematic review and meta-analysis. Support Care Cancer. (2024) 32:115. doi: 10.1007/s00520-024-08306-8
7. Cappe, M, Laterre, P-F, and Dechamps, M. Preoperative frailty screening, assessment and management. Curr Opin Anaesthesiol. (2023) 36:83–8. doi: 10.1097/ACO.0000000000001221
8. Ding, L, Miao, X, Jiang, X, Chen, L, Lu, J, Zhu, H, et al. Adverse outcomes and health-ecological influencing factors of preoperative frailty among elderly patients with gastric cancer. J Cancer Res Clin Oncol. (2023) 149:7043–51. doi: 10.1007/s00432-023-04651-z
9. Sakurai, K, Kubo, N, Hasegawa, T, Tamamori, Y, Kuroda, K, Iseki, Y, et al. Risk factors of “loss of independence” in elderly patients who received gastrectomy for gastric cancer. Gastric Cancer. (2023) 26:638–47. doi: 10.1007/s10120-023-01376-3
10. Midgley, W, Mizen, A, Bailey, R, Hollinghurst, J, Hollinghurst, R, Lyons, RA, et al. How does the environment in and around the home affect social care and health outcomes for older people? A national longitudinal dynamic cohort study. Lancet. (2023) 402:S69. doi: 10.1016/S0140-6736(23)02096-2
11. Kuhlthau, KA, Ames, SG, Ware, A, Hoover, CG, Wells, N, and Shelton, C. Research on family health and children and youth with special health care needs. Acad Pediatr. (2022) 22:S22–7. doi: 10.1016/j.acap.2021.07.019
12. Feinberg, M, Hotez, E, Roy, K, Ledford, CJW, Lewin, AB, Perez-Brena, N, et al. Family health development: a theoretical framework. Pediatrics. (2022) 149:e2021053509I. doi: 10.1542/peds.2021-053509I
13. Collins, TL, Yong, KW, Marchetti, MT, Miller, KL, Booths, B, and Falvey, JR. The value of home health physical therapy. Home Healthc Now. (2019) 37:145–51. doi: 10.1097/NHH.0000000000000760
14. Nutbeam, D, and Lloyd, JE. Understanding and responding to health literacy as a social determinant of health. Annu Rev Public Health. (2021) 42:159–73. doi: 10.1146/annurev-publhealth-090419-102529
15. Duong, TV, Aringazina, A, Kayupova, G, Null, N, Pham, TV, Pham, KM, et al. Development and validation of a new short-form health literacy instrument (HLS-SF12) for the general public in six Asian countries. Health Lit Res Pract. (2019) 3:e91–e102. doi: 10.3928/24748307-20190225-01
16. Abd Kadir, NA, Azzeri, A, Mohd Noor, MI, Kefeli, Z, Abdullah, MF, Ramlee, MNA, et al. Health literacy status among community in the protected area: a protocol for systematic review and meta-analysis. Medicine (Baltimore). (2023) 102:e33590. doi: 10.1097/MD.0000000000033590
17. Wunsch, K, Fiedler, J, Hubenschmid, S, Reiterer, H, Renner, B, and Woll, A. An mHealth intervention promoting physical activity and healthy eating in a family setting (SMARTFAMILY): randomized controlled trial. JMIR Mhealth Uhealth. (2024) 12:e51201. doi: 10.2196/51201
18. Yang, X, Li, S, Xu, L, Liu, H, Li, Y, Song, X, et al. Effects of multicomponent exercise on frailty status and physical function in frail older adults: a meta-analysis and systematic review. Exp Gerontol. (2024) 197:112604. doi: 10.1016/j.exger.2024.112604
19. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, Vandenbroucke, JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
20. National Health Commission of The People's Republic of China. Standardization for diagnosis and treatment of gastric cancer (2022 edition). Chinese J Digest Surg. (2022) 21:1137–64. doi: 10.3760/cma.j.cn115610-20220726-00432 (in Chinese)
21. Rosenblatt, WH, and Yanez, ND. A decision tree approach to airway management pathways in the 2022 difficult airway algorithm of the American society of anesthesiologists. Anesth Analg. (2022) 134:910–5. doi: 10.1213/ANE.0000000000005930
22. Sun, X, Shi, Y, Wang, X, Zhou, R, and Deng, W. Diabetes-related stress in older adults with type 2 diabetes and chronic complication: multiple effects of social-ecological support on self-management behavior. Medicine (Baltimore). (2024) 103:e37951. doi: 10.1097/MD.0000000000037951
23. Crandall, A, Weiss-Laxer, NS, Broadbent, E, Holmes, EK, Magnusson, BM, Okano, L, et al. The family health scale: reliability and validity of a short- and long-form. Front Public Health. (2020) 8:587125. doi: 10.3389/fpubh.2020.587125
24. Wang, F, Wu, Y, Sun, X, Wang, D, Ming, W-K, Sun, X, et al. Reliability and validity of the Chinese version of a short form of the family health scale. BMC Prim Care. (2022) 23:108. doi: 10.1186/s12875-022-01702-1
25. Sun, X, Chen, K, Wu, Y, Tang, J, Wang, F, Sun, X, et al. Development of a short version of the health literacy scale based on classical test theory and item response theory. China Gen Pract. (2024) 27:2931–40. (in Chinese). doi: 10.12114/j.issn.1007-9572.2023.0072
26. Hu, B, Lin, LF, Zhuang, MQ, Yuan, ZY, Li, SY, Yang, YJ, et al. Reliability and relative validity of three physical activity questionnaires in Taizhou population of China: the Taizhou longitudinal study. Public Health. (2015) 129:1211–7. doi: 10.1016/j.puhe.2015.03.024
27. Mok, A, Khaw, K-T, Luben, R, Wareham, N, and Brage, S. Physical activity trajectories and mortality: population based cohort study. BMJ. (2019) 365:l2323. doi: 10.1136/bmj.l2323
28. Gobbens, RJJ, van Assen, MALM, Luijkx, KG, Wijnen-Sponselee, MT, and Schols, JMGA. The Tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc. (2010) 11:344–55. doi: 10.1016/j.jamda.2009.11.003
29. Dong, L, Liu, N, Tian, X, Qiao, X, Gobbens, RJJ, Kane, RL, et al. Reliability and validity of the Tilburg frailty indicator (TFI) among Chinese community-dwelling older people. Arch Gerontol Geriatr. (2017) 73:21–8. doi: 10.1016/j.archger.2017.07.001
30. Zhao, B, Zhang, S, Chen, Y, Zhang, T, and Zhang, C. Risk factors for preoperative frailty in older patients with gastric cancer: a systematic review and meta-analysis. Support Care Cancer. (2024) 32:450. doi: 10.1007/s00520-024-08654-5
31. Maselli, D. Strategies for tobacco-free survivorship after breast cancer: the possible weaving of preoperative care and public health policies. Public Health Nurs. (2024) 41:403–5. doi: 10.1111/phn.13293
32. Munir, MM, Woldesenbet, S, and Pawlik, TM. Trajectory analysis of healthcare use before and after gastrointestinal cancer surgery. J Am Coll Surg. (2024) 240:24–33. doi: 10.1097/XCS.0000000000001212
33. Cavaliere, C, Damiao, J, Pizzi, M, and Fau, L. Health, well-being, and health-related quality of life following COVID-19. OTJR (Thorofare N J). (2023) 43:188–93. doi: 10.1177/15394492221111733
34. Chew, J, Carpenter, J, and Haase, AM. Young people’s experiences of living with epilepsy: the significance of family resilience. Soc Work Health Care. (2018) 57:332–54. doi: 10.1080/00981389.2018.1443195
35. Ramaswami, SB, Jensen, T, Berghaus, M, De-Oliveira, S, Russ, SA, Weiss-Laxer, N, et al. Family health development in life course research: a scoping review of family functioning measures. Pediatrics. (2022) 149:e2021053509J. doi: 10.1542/peds.2021-053509J
36. Walston, J, Buta, B, and Xue, Q-L. Frailty screening and interventions: considerations for clinical practice. Clin Geriatr Med. (2018) 34:25–38. doi: 10.1016/j.cger.2017.09.004
37. Lopes, RT, Neves, ÉTB, Dutra, LC, Gomes, MC, Paiva, SM, Abreu, MHNGD, et al. Socioeconomic status and family functioning influence oral health literacy among adolescents. Rev Saude Publica. (2020) 54:30. doi: 10.11606/s1518-8787.2020054001842
38. Champlin, S, Hoover, DS, and Mackert, M. Family health in adult education: a missing piece of the health literacy puzzle. Health Lit Res Pract. (2019) 3:S75–8. doi: 10.3928/24748307-20190624-03
39. Rothbaum, F, Rosen, K, Ujiie, T, and Uchida, N. Family systems theory, attachment theory, and culture. Fam Process. (2002) 41:328–50. doi: 10.1111/j.1545-5300.2002.41305.x
40. Angulo, J, El Assar, M, Álvarez-Bustos, A, and Rodríguez-Mañas, L. Physical activity and exercise: strategies to manage frailty. Redox Biol. (2020) 35:101513. doi: 10.1016/j.redox.2020.101513
41. Taylor, JA, Greenhaff, PL, Bartlett, DB, Jackson, TA, Duggal, NA, and Lord, JM. Multisystem physiological perspective of human frailty and its modulation by physical activity. Physiol Rev. (2023) 103:1137–91. doi: 10.1152/physrev.00037.2021
42. Sachs, JD. From millennium development goals to sustainable development goals. Lancet. (2012) 379:2206–11. doi: 10.1016/S0140-6736(12)60685-0
Keywords: gastric cancer, preoperative care, frailty, family health, health literacy, physical activity, mediating role
Citation: Xin H, He C, Gu Y, Ma X, Xiang Z and Gong J (2025) The association between family health and frailty in preoperative patients with gastric cancers: the mediating role of health literacy and physical activity. Front. Public Health. 13:1541688. doi: 10.3389/fpubh.2025.1541688
Edited by:
Klara Komici, University of Molise, ItalyReviewed by:
Gagan Matta, Gurukul Kangri University, IndiaRima Kregzdyte, Lithuanian University of Health Sciences, Lithuania
Copyright © 2025 Xin, He, Gu, Ma, Xiang and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chaozhu He, MTMwNzAyNDYyNjdAMTYzLmNvbQ==
 Hanjia Xin
Hanjia Xin Chaozhu He
Chaozhu He Yingying Gu1
Yingying Gu1