- 1School of Nursing, Health Science Center, Xi’an Jiaotong University, Xi’an, China
- 2School of Nursing, Qiqihar Medical University, Qiqihar, China
- 3Department of Neurosurgery, Qiqihar First Hospital, Qiqihar, China
Background and objectives: Although the global human immunodeficiency virus (HIV) infection rate has decreased in recent years, the proportion and number of HIV-infected individuals aged 18–24 years has increased. The main mode of HIV transmission is sexual, a large proportion of the infected population are college students, and numerous health education activities have been implemented to prevent HIV infection, where mastery of relevant knowledge greatly improves. Nevertheless, the effectiveness of necessary protective measures is not ideal during actual behavior, indicating insufficient conversion of prevention knowledge to behavioral. To understand the factors and interactions that influence preventive behavior, we conducted a cross-sectional exploratory study.
Materials and methods: Participants (n = 1,111) were students from Heilongjiang Province. A survey questionnaire was distributed through online social platforms. The questionnaire collected data on sociodemographic variables, perception of infection risk (PIR), perceived benefits of preventive behavior (PBPB), perceived disorders of preventive behavior (PDPB), attitudes of preventive behavior (APB), and behavior of wearing condoms (BWC).
Results: BWC did not differ significantly according to gender, academic qualification pursued, or subject major (p ≥ 0.05), but did differ significantly based on sexual orientation, receiving HIV infection prevention education, and commercial and casual sexual behaviors. No significant correlation was detected between PIR and APB (p ≥ 0.05), while PBPB and APB were significantly positively and PDPB and APB significantly negatively correlated (p < 0.05). Further, there was no significant correlation between PBPB and BWC (p ≥ 0.05), while PIR and APB were positively correlated with BWC (p < 0.05), and there was a negative correlation between PDPB and BWC (p < 0.05). APB did not mediate between PDPB and BWC, but APB partially mediated between PDPB and BWC, accounting for approximately 9.96% of the total effect value, and played a fully mediating role (100%) between PBPB and BWC.
Conclusion: Our analysis indicates that PBPB acts on BWC through APB, PIR directly affects BWC, and PDPB can directly affect BWC, while also influencing BWC through APB. Future efforts to increase PBPB, PIR, and APB, reduce PDPB, and promote the use of condoms in sexual behavior among college students are warranted.
1 Introduction
Human immunodeficiency virus (HIV) infection continues to impose a heavy burden and remains a major public health issue (1). To date, there is no effective vaccine to prevent (2), and no effective medication to cure HIV (3); however, viral load and disease progression speed can be controlled through medication (4). Hence, prevention remains the most important measure to control the number of HIV infections.
After years of effort, HIV infection in China demonstrates an overall low prevalence trend (5, 6); however, the proportion and numbers of HIV-infected individuals aged 18–24 years has increased, rather than decreasing (7). The affected population includes many college students (8), and there is a risk of further HIV infection spread to the intimate partners of infected individuals, which would inevitably generate public health pressure (9). Pre exposure prevention and post exposure prevention, as effective prevention strategies, can significantly reduce the risk of infection (10–14). Early diagnosis and treatment can help infected individuals receive timely medical intervention and reduce the risk of virus transmission (14). In summary, the comprehensive use of pre-and post exposure prevention, voluntary counseling and testing, risk behavior management, condom use, and early intervention strategies can effectively prevent the spread of HIV (14).
The main route of HIV infection among college students is sexual transmission (15), and a considerable proportion of HIV infection cases are due to individuals not wearing condoms during sexual intercourse (16, 17). Over many years, health education aimed at preventing HIV infection has been vigorously implemented, and these educational activities have achieved significant results in enhancing the knowledge of college students about HIV infection prevention and AIDS-related awareness (18); however, necessary protective measures are often not taken proactively during actual sexual behavior, indicating insufficient conversion of prevention knowledge at the behavioral level (19). This phenomenon prompted us to explore where the “gap” between knowledge dissemination and practical protective behavior arises.
The aim of this study was to establish a theoretical model using structural equation modeling to explain the factors influencing of behavior of wearing condoms (BWC) among college students who engage in sexual activity, as well as the relationships between identified influencing factors. Our research results provide basic data that can improve health education and intervention strategies for preventing HIV infection among college students.
1.1 Theoretical model construction and research hypotheses
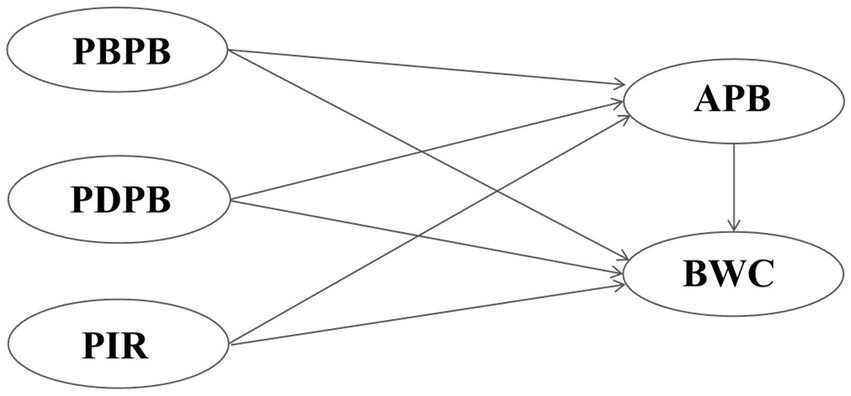
The health belief model (20, 21) is a widely used theory of individual behavior change. Health beliefs (22) also have strong predictive effects on behavior, as follows: First, the perception of diseases, which, in our study, equated to an individual’s perception of possible HIV infection; Second, the perception of preventive behavior, mainly including its benefits during sexual activity (such as using condoms to reduce the risk of HIV transmission) and the perception of obstacles (such as the impact of condoms on sexual pleasure or difficulty in obtaining them), which collectively affect an individual’s attitudes toward preventive behavior. The knowledge, attitude, practice model is a classic theory used to explain and predict healthy behaviors (23). This model suggests that behavior change is a progressive process, from acquiring knowledge to forming attitudes, and then to actual action (24). Attitude is an important intermediate link between knowledge and practical behavior. There are two facets of attitude in this context (25): attitude toward the disease, referring to an individual’s understanding of the severity and potential risks of HIV infection; and attitude toward preventive behavior, referring to an individual’s trust in the effectiveness of preventive measures, such as wearing condoms during sexual activity. Although both facets of attitude have predictive effects on behavior, research suggests that attitudes toward preventive behavior are more important (26). Therefore, in this study we mainly considered attitudes toward preventive behavior. If individuals firmly believe that preventive measures can effectively prevent the spread of HIV, they are more likely to translate them into practical protective actions, thereby reducing the risk of infection. In summary, we explored perception of infection risk (PIR) about HIV, perceived benefits of preventive behavior (PBPB), perceived disorders of preventive behavior (PDPB), and attitudes of preventive behavior (APB), as factors potentially affecting behavior of wearing condoms (BWC); constructed a theoretical model (Figure 1); and tested research hypotheses as follows:
H1: PIR exerts a positive effect on APB.
H2: PBPB exerts a positive effect on APB.
H3: PDPB exerts a negative effect on APB.
H4: PIR exerts a positive effect on BWC.
H5: PBPB exerts a positive effect on BWC.
H6: PDPB exerts a negative effect on BWC.
H7: APB exerts a positive effect on BWC.
2 Materials and methods
2.1 Ethics and consent
This study was approved by the Ethics and Research Review Committee of Qiqihar Medical University in China ([2021]150); the date of approval was 8 November, 2021. All participants in the study provided informed consent.
2.2 Study population and design
In China, young students aged 18–24 are mainly college students and junior college students, while considering the impact of medical background on HIV prevention knowledge. This study selected junior college and college students, and who majoring in medicine and non-medical fields as research subjects. For the convenience of questionnaire distribution and data collection, universities in the author’s city of work and nearby cities were selected for the survey.
A cross-sectional anonymous online survey of students aged ≥ 18 years from five universities in Qiqihar, Daqing, Harbin in Heilongjiang Province, who filled out the questionnaire with informed consent and had no reading or questionnaire barriers, was conducted from November 2023 to December 2023. The survey questionnaire was distributed through online social platforms (WeChat and QQ) and automatically collected after completion.
2.3 Questionnaire design
The survey questionnaire was proofread and revised by a panel of experts in relevant fields, including disease prevention experts, behavioral psychologists, and statisticians. The first version of the questionnaire was pre surveyed among 30 medical students, and based on the pre survey results, some ambiguous items were modified, resulting in 23 questions. The questionnaire usually took < 10 min to complete.
The questionnaire comprised the following parts: (1) sociodemographic variables, including gender, education level, subject major, sexual orientation, whether received health education to prevent HIV infection, whether engaged in commercial sexual activity, and whether engaged in casual sexual activity; (2) Perception of infection risk (3 items), perceived benefits of preventive behavior (3 items), perceived disorders of preventive behavior (4 items), and attitudes of preventive behavior (5 items); and (3) Behavior of wearing condoms (1 item). Behavior of wearing condoms refers to whether participants have used condoms throughout their most recent sexual intercourse before the survey. Among the sexual transmission routes of HIV, vaginal intercourse and anal intercourse are the main transmission routes (27, 28). Therefore, in this study, sexual intercourse refers to both vaginal and anal intercourse.
This study included perception of infection risk, perceived benefits of preventive behavior, perceived disorders of preventive behavior, attitudes of preventive behavior, and 7 sociodemographic variables, totaling 11 independent variables. The sample size was taken as 10 times the number of independent variables, and considering 20% of invalid questionnaires, at least 138 people need to be included in this study. To ensure the stability and accuracy of structural equation modeling analysis, the sample size should be greater than 200 (29). Based on the above two considerations, the sample size of this study was designed to be at least 200 people.
2.4 Variables and measurements
Each item in perception of infection risk, perceived benefits of preventive behavior, perceived disorders of preventive behavior, and attitudes of preventive behavior was scored on a 5-point Likert scale, with a score of 1 indicating strong disagreement and a score of 5 indicating strong agreement. Behavior of wearing condoms was transformed to a binary variable (1 = yes and 0 = no), to facilitate analysis. “yes” indicates that participants had used condoms throughout their most recent sexual intercourse before the survey.“no” means not using or not using condoms throughout the entire process when engaging in sexual activity before the survey.
2.5 Questionnaire reliability
In this study, the calculated Cronbach’s alpha and Kaiser-Meyer-Olkin values for the questionnaire were 0.786 and 0.859, respectively, indicating that the instrument is valid and reliable for data-gathering activities (30).
2.6 Statistical analysis
The software packages SPSS 21.0 and Analysis of Moment Structures 26.0 were used for statistical analyses. Calculation of descriptive statistics, correlation analysis, and structural equation modeling (SEM) were conducted. The fit of the SEM was tested using chi-square/degrees of freedom (χ2/DF) and root mean square error of approximation (RMSEA) analyses, where 1 < χ2/DF < 3 and RMSEA < 0.05 indicated a better fit. Comparative fit index (CFI), Tucker-Lewis index (TLI), and incremental fit index (IFI) served as incremental fit indices, where CFI > 0.95, TLI > 0.95, and IFI > 0.95 indicated better fit (30). A p-value of < 0.05 was considered statistically significant.
3 Results
3.1 Demographic data and behavior of wearing condoms
Students participating in the pre survey were not included in the final sample. A total of 21,445 questionnaires were collected, among which 1,111 college students reported engaging in sexual activity. Among the 1,111 sexually active individuals mean ± standard deviation age was 19.45 ± 1.309 years, the median age of participants was 19 years (range, 18–25 years), and 613 (55.18%) were male. Further, 292 (26.28%) were pursuing a college degree, 554 (49.86%) were medical majors, 32 (3.15%) had same-sex orientation, 1,032 (92.89%) had heterosexual orientation, 44 (3.96%) had bisexual orientation, 1,017 (91.54%) had received health education related to HIV infection prevention, 26 (2.34%) had undertaken commercial sexual activity, and 107 (9.63%) had engaged in casual sexual activity.
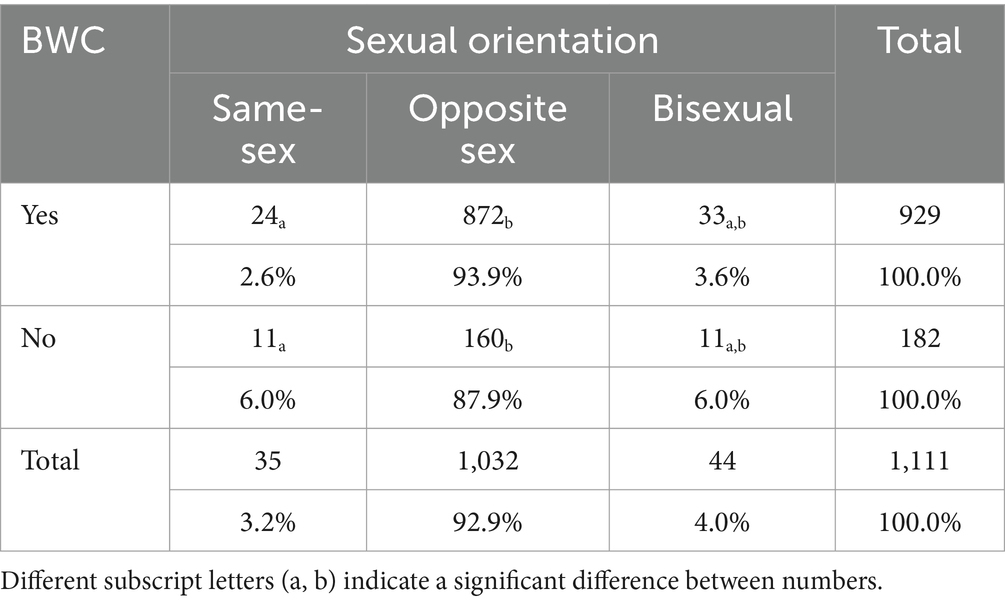
Behavior of wearing condoms did not differ significantly (p > 0.05) according to gender, academic qualifications pursued, or subject major; however, behavior of wearing condoms differed significantly (p < 0.05) among individuals with differing sexual orientation. The proportion of people with heterosexual orientation who reported wearing condoms during sexual relations was significantly higher than that of people with homosexual orientation (p < 0.05), while the differences between the group with bisexual orientation and those with other orientations were not significant (p > 0.05). Behavior of wearing condoms differed significantly between respondents who did and did not receive health education related to HIV infection prevention, between those who did and did not report engaging in commercial sexual activity, and between those who did and did not engage in casual sexual activity (p < 0.05). See Tables 1, 2 for details.
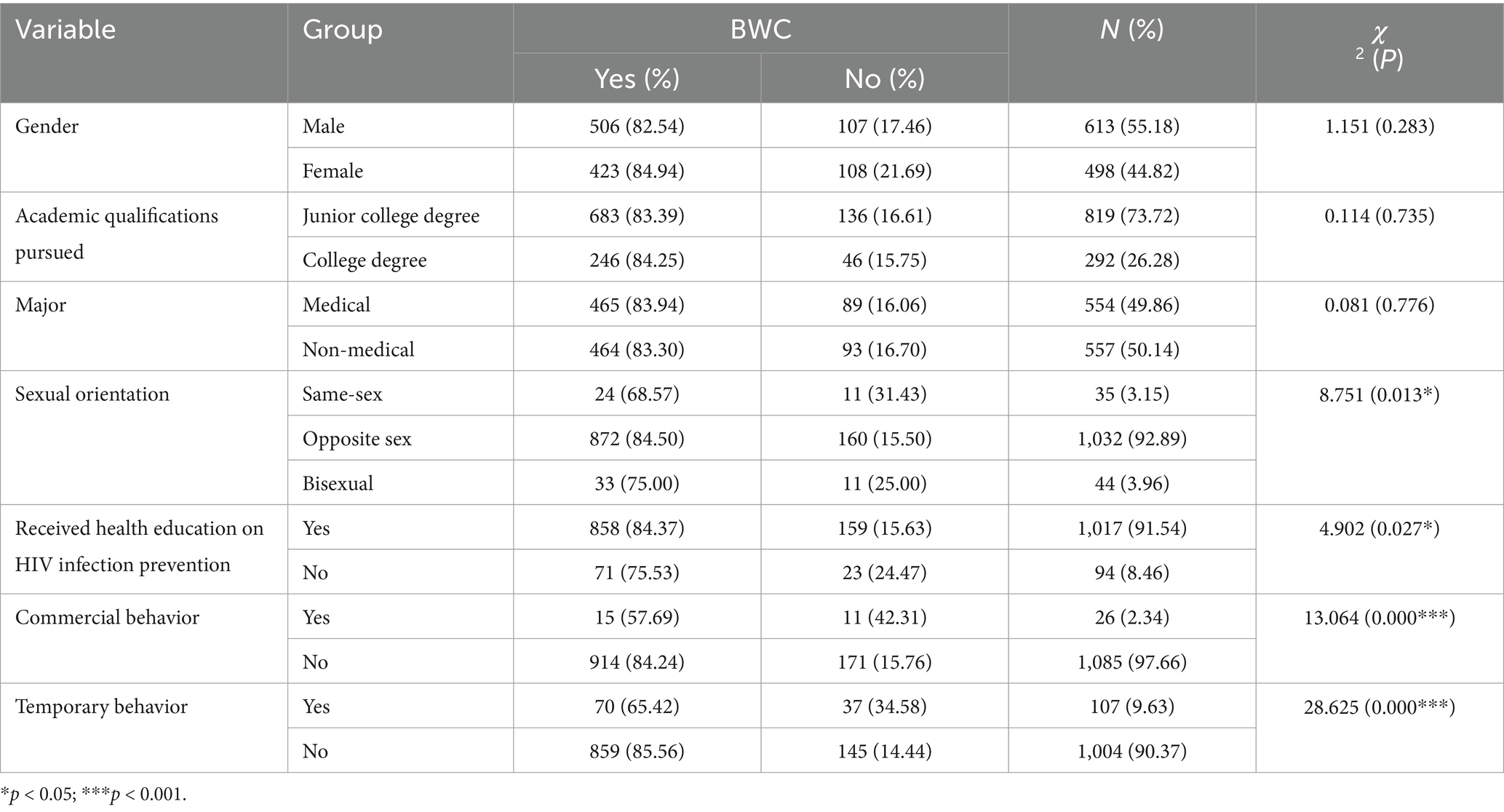
Table 1. Summary statistics of BWC according to participant sociodemographic characterization (n = 1,111).
3.2 SEM fitting index results
Analysis of the fit of the SEM generated in our study demonstrated that χ2/DF was 2.900, RMSEA was 0.041, CFI was 0.991, TLI was 0.988, and IFI was 0.991, indicating that the overall fit of the research model was acceptable.
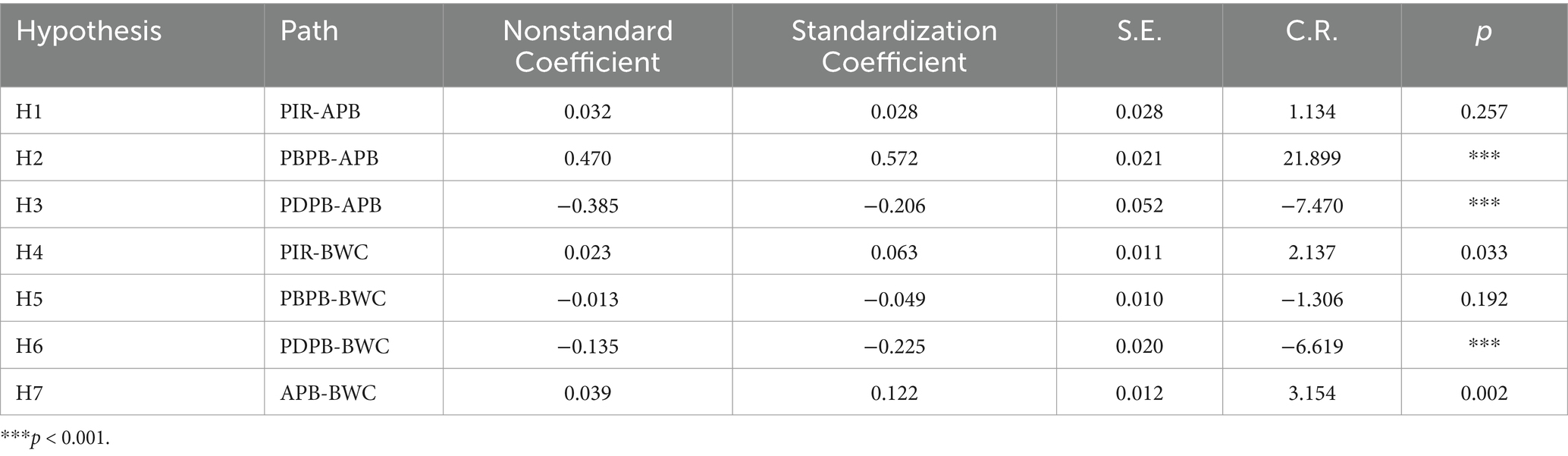
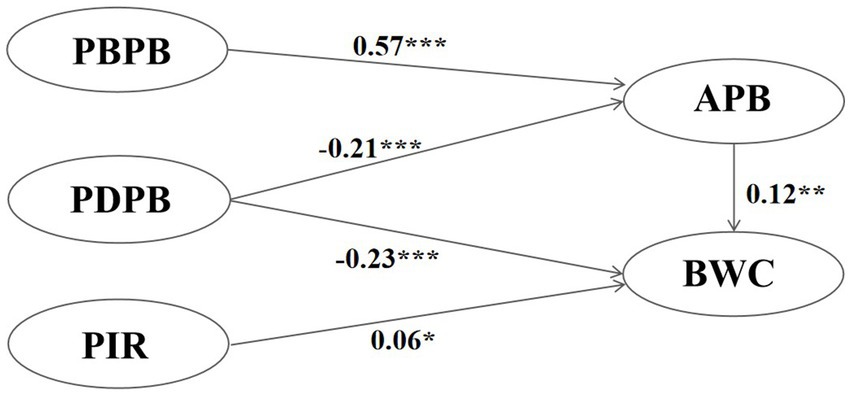
3.3 Model analysis results
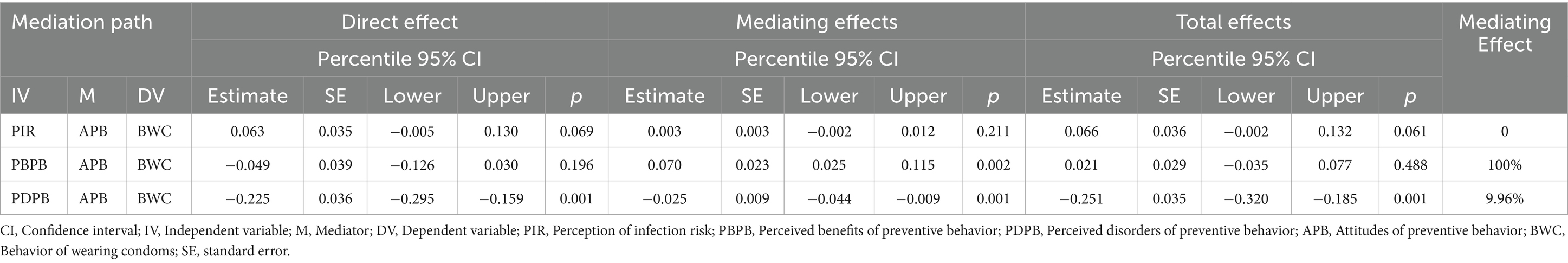
Path analysis demonstrated that perception of infection risk had a significant positive impact on behavior of wearing condoms, supporting H4, but had no effect on attitudes of preventive behavior, which does not support H1. Perceived benefits of preventive behavior had a significant positive effect on attitudes of preventive behavior, supporting H2, but no effect on behavior of wearing condoms, which did not support H5. Perceived disorders of preventive behavior had significant negative impacts on attitudes of preventive behavior and behavior of wearing condoms, supporting H3 and H6. Attitudes of preventive behavior had significant positive impact on behavior of wearing condoms, thus supporting H7. Hypothesis test results are presented in Table 3, and the results of deleting unsupported paths are shown in Figure 2.
As shown in Table 4, attitudes of preventive behavior did not play a mediating role between perception of infection risk and behavior of wearing condoms, but attitudes of preventive behavior played a fully mediating role (100%) between perceived benefits of preventive behavior and behavior of wearing condoms. Further, attitudes of preventive behavior played a partial mediating role between perceived disorders of preventive behavior and behavior of wearing condoms, accounting for approximately 6.9% of the total effect.
4 Discussion
4.1 General sociological factors influencing condom use among sexually active college students
The use of condoms during sexual activity is among the most effective means of preventing HIV infection (31); however, various factors influence condom use among college students. In this study, we found no significant difference in behavior of wearing condoms according to gender in respondents engaged in casual sexual relationships, indicating relatively consistent protective behaviors in both men and women in this context. Although traditional beliefs may suggest that men are less willing to use condoms (32), our research findings do not support this hypothesis, indicating that gender is no longer a key factor in this behavioral choice.
No significant difference in behavior of wearing condoms score was detected between respondents undertaking junior college degrees and those studying for college degrees, suggesting that education level was not a decisive factor affecting use of condoms among college students. Further, no significant difference in protective awareness was detected between undergraduate students and those who had received higher education, which may be related to the fact that all college students receive HIV prevention and health education.
Moreover, we found no significant difference in behavior of wearing condoms on comparison of medical and non-medical students. Although medical students study more health-related courses, and theoretically have a deeper understanding of HIV and sexually transmitted infections (33), this cognitive advantage was not translated into significantly higher rates of condom use. These findings indicate that, even for college students with a medical background, behavioral changes do not occur spontaneously due to accumulation of professional knowledge, and the effectiveness of behavioral interventions requires further efforts.
Sexual orientation is an important variable affecting behavior of wearing condoms among college students. In this study, we found that the proportion of heterosexual college students using condoms during sexual intercourse was significantly higher than that of homosexual college students. This finding may be related to the fact that heterosexual individuals receive more sexual health education focused on preventing sexually transmitted diseases (such as HIV) and unintended pregnancies (34), while homosexual individuals, especially male homosexual individuals, receive less attention in traditional sex education systems and may lack systematic education on sexual health, resulting in a lower rate of safety measure implementation. In addition, trust and dependence on partners are often strong within homosexual groups (35), and individuals may reduce their use of condoms due to strong emotional trust relationships (36); however, we found no significant difference in the proportion of condom use among bisexual individuals during sexual activity relative to those in the other groups.
Commercial and casual sexual activity also had a significant impact on behavior of wearing condoms. Students who did not engage in commercial sexual activity had a significantly higher frequency of using condoms in casual relationships than those who did engage in commercial sexual activity. A higher proportion of college students who did not engage in casual sexual activity also reported using condoms, possibly due to impulsivity in temporary situations and a lack of stable emotional connections, which may lead to a failure to fully consider safety precautions.
The effect of health education on HIV infection prevention in promoting behavior of wearing condoms was also very significant. The proportion of students who had received HIV-related health education that reported using condoms during sexual activity was significantly higher than that of students who had not received such education. This finding indicates that systematic and sustained health education is crucial for enhancing awareness of protective sexual behavior among college students (37), and is an effective health intervention. The effects of health education include the improvement of knowledge. Insufficient knowledge might not be able to apply all preventive measures to reduce the spread of HIV (38). However, a study found that condom use had nothing to do with HIV knowledge (39). Therefore, the strategy of health education should be adjusted (40).
4.2 Impacts of perception of infection risk, perceived benefits of preventive behavior, and perceived disorders of preventive behavior on attitudes of preventive behavior
The results of this study demonstrated no significant correlation between perception of infection risk and attitudes of preventive behavior. We speculate that, when individuals are aware of the risk of HIV infection but fail to fully internalize this perception as a motivation to increase their willingness to act, or are limited by external factors, such as environment and social pressure, their attitude toward wearing condoms will not significantly improve.
Perceived benefits of preventive behavior was positively correlated with attitudes of preventive behavior. This finding suggests that, if college students can clearly understand the specific benefits of wearing condoms during sexual activity, such as effectively preventing HIV infection, reducing sexually transmitted infections, and contraception (36), their attitude toward wearing condoms during sexual activity will be more positive. Strengthening education and publicity to remind individuals that condoms are a simple, easily accessible, and efficient protective tool will help increase their rate of practical use during relevant behaviors (41).
Our research identified a negative correlation between perceived disorders of preventive behavior and attitudes of preventive behavior. Perceived behavioral disorders refer to various practical or social difficulties that individuals experience during sexual activity (23), such as the use of condoms affecting sexual pleasure, partner unwillingness to cooperate, and the inconvenience of purchasing and carrying condoms, among others (42). The stronger the perception of these obstacles, the more negative an individual’s attitude toward wearing condoms will be. This result indicates that it is not only lack of knowledge that hinders widespread condom use, but also the perception of obstacles in real life situations that significantly impact protective psychology influencing sexual behavior. Therefore, reducing perceived disorders of preventive behavior will be a key step in improving condom use, and efforts should be made to eliminate negative behavioral barriers perceived by students in their psychological and socio-cultural contexts, helping them overcome obstacles, and encouraging the use of condoms in sexual relationships.
4.3 Impact of perception of infection risk, perceived benefits of preventive behavior, perceived disorders of preventive behavior, and attitudes of preventive behavior on behavior of wearing condoms
Our research found that perception of infection risk was an important predictor of behavior of wearing condoms. Perception of infection risk refers to an individual’s subjective assessment of their risk of exposure to HIV infection. If individuals believe they are at a higher risk of contracting HIV, they are more inclined to take preventive measures, such as wearing condoms, during sexual activity (43). In this study, we found a significant positive correlation between perception of infection risk and behavior of wearing condoms during sexual behavior, indicating that individuals with stronger perception of infection risk were more likely to insist on condom use during sexual activity. This finding is consistent with previous research (44), indicating that increasing an individual’s perception of infection risk can effectively promote safe sexual behavior. Therefore, future health education efforts should strengthen guidance on perception of infection risk to help provide a clearer understanding of the potential health threats posed by unsafe sexual behavior.
Perceived benefits of preventive behavior is often considered a driving factor in healthy behavior patterns; however, in this study, we did not detect a significant correlation between perceived benefits of preventive behavior and behavior during sexual activity. Although many people are theoretically aware that wearing condoms can effectively prevent HIV and other sexually transmitted diseases (45), this awareness has not been directly translated into practical safety behaviors. This phenomenon may be related to the complexity of behavior. Even if individuals accept the benefits of condoms at a cognitive level, during sexual behavior, the behavioral benefits may not play a decisive role in all situations, due to various factors, such as emotions, situations, partner attitudes, or immediate decisions. Hence, simply emphasizing the benefits of behavior may not be sufficient to encourage individuals to form stable healthy behaviors, and it may be necessary to combine intervention measures with other factors, particularly in efforts to reduce individual behavioral disorders and cultivate specific attitudes.
Perceived disorders of preventive behavior has an equally important impact on behavior of wearing condoms during sexual behavior and was negatively correlated with condom use in this study. When individuals feel that there are specific obstacles influencing their behavior, they are more inclined not to use condoms. Common obstacles include the impact of condoms on sexual pleasure, partner unwillingness to cooperate, inconvenience of obtaining and using condoms, and potential social awkwardness (46). These practical and subjective barriers often lead individuals to avoid using condoms during sexual activity. Our results also indicate that, although individuals may be aware of the benefits and importance of wearing condoms, these barriers significantly weaken their willingness to engage in protective behavior. This finding emphasizes the importance of reducing behavioral disorders in future health interventions, and particularly cultivating the ability of individuals to overcome relevant barriers to ensure that they can choose to take protective measures when facing these challenges.
This study also found that attitudes of preventive behavior during sexual activity was an important factor affecting behavior of wearing condoms, and that attitudes were positively correlated with reported behavior. This finding suggests that, when individuals hold a more positive attitude toward wearing condoms, they are more likely to choose to use condoms during sexual activity. Therefore, a positive attitude can encourage individuals to use condoms during sexual activity (47, 48). This finding provides further evidence supporting the need for future prevention interventions to focus on shaping and strengthening positive attitudes toward condom use, so that individuals not only accept the benefits of condoms at a cognitive level, but also can truly put these attitudes into practice at a behavioral level.
4.4 The mediating role of attitudes of preventive behavior between perception of infection risk, perceived benefits of preventive behavior, perceived disorders of preventive behavior, and behavior of wearing condoms
Our analysis also showed that attitudes of preventive behavior did not play a mediating role between perception of infection risk and behavior of wearing condoms, indicating that, although individuals may have positive or negative attitudes toward the act of wearing condoms, these attitudes fail to further mediate the impact of risk perception on actual behavior in the chain of action. That is, a strong sense of risk is sufficient to prompt individuals to take action, as demonstrated in other similar studies (49), while changes in attitude do not play a decisive role.
The results of our research show that, although individuals may be aware of the many benefits of wearing condoms, this perceived benefits of preventive behavior does not directly prompt them to take safety measures during sexual activity; however, we found that attitudes of preventive behavior plays a fully mediating role between perceived benefits of preventive behavior and behavior of wearing condoms during sexual relationships. This discovery suggests that, in future health interventions, there is a need to educate individuals both about the benefits of condom use (50) and, more importantly, cultivate and enhance their positive attitudes, to ensure higher condom use rates and effectively prevent the spread of HIV.
In this study, attitudes of preventive behavior played a partial mediating role between perceived disorders of preventive behavior and behavior of wearing condoms during sexual relations, accounting for approximately 9.96% of the total effect value. Hence, although perceived disorders of preventive behavior mainly reduces condom use through direct action, a positive attitude toward condom use can alleviate the negative impact of behavioral disorders to some extent (51). For example, even if individuals perceive certain barriers to using condoms, if they have a positive attitude toward wearing condoms, they may still be able to overcome these barriers and choose to use condoms during sexual activity (52).
5 Conclusion
Our evidence suggests that attitudes of preventive behavior does not mediate between perception of infection risk and behavior of wearing condoms among sexually active college students, while attitudes of preventive behavior does have a partial mediating role between perceived disorders of preventive behavior and behavior of wearing condoms and plays a fully mediating role between perceived benefits of preventive behavior and behavior of wearing condoms. Therefore, in health education, it is necessary to enhance awareness of perception of infection risk, perceived benefits of preventive behavior, and attitudes of preventive behavior, as well as reducing perceived disorders of preventive behavior, thereby improving behavior of wearing condoms and reducing the risk of HIV infection among college students through sexual activity.
6 Limitations and outlook
This study has certain limitations that can be addressed in future research. This study focuses on the use of condoms among Chinese college students engaged in sexual activities. No attention was paid to other prevention behaviors such as voluntary counseling and testing, early diagnosis, early treatment, HIV pre exposure prevention and post exposure prevention. Although the use of condoms is one of the traditional and effective methods for preventing the spread of HIV. However, in the comprehensive intervention strategy for HIV prevention, the synergistic effect of multiple methods has played an indispensable role in reducing the risk of virus transmission and improving the health level of the population. Pre exposure prophylaxis (PrEP) and post exposure prophylaxis (PEP), which involve the use of antiviral drugs in advance, can significantly reduce the risk of HIV infection. Voluntary Counseling and Testing (VCT) can detect HIV infected individuals early, promote early diagnosis and treatment, and reduce virus transmission. Future research will focus on voluntary counseling and testing, early diagnosis, early treatment, pre exposure prevention and post exposure prevention of HIV.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics and Research Review Committee of Qiqihar Medical University; The author is from this institution. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LQ: Conceptualization, Methodology, Project administration, Writing – original draft, Writing – review & editing. RG: Data curation, Formal Analysis, Writing – original draft. YQ: Investigation, Writing – review & editing. XL: Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the “Qiqihar Science and Technology Plan Joint Guidance Project” of Qiqihar Municipal Bureau in 2022 (No. LSFGG-2022052).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1544564/full#supplementary-material
Abbreviations
APB, Attitudes of preventive behavior; BWC, Behavior of wearing condoms; CS, College students; CFI, Comparative fit index; HIV, Human immunodeficiency virus; IFI, Incremental fit index; PBPB, Perceived benefits of preventive behavior; PDPB, Perceived disorders of preventive behavior; PIR, Perception of infection risk; RMSEA, Root mean square error of approximation; SEM, Structural equation modeling; TLI, Tucker-Lewis index.
References
1. Ghosn, J, Taiwo, B, Seedat, S, Autran, B, and Katlama, C. HIV Lancet. (2018) 392:685–97. doi: 10.1016/S0140-6736(18)31311-4
2. Klasse, PJ, and Moore, JP. Reappraising the value of HIV-1 vaccine correlates of protection analyses. J Virol. (2022) 96:e0003422. doi: 10.1128/jvi.00034-22
3. Frediansyah, A, Sofyantoro, F, Alhumaid, S, AlMutair, A, Albayat, H, Altaweil, HI, et al. Microbial natural products with antiviral activities, including anti-SARS-CoV-2: a review. Molecules. (2022) 27:4305. doi: 10.3390/molecules27134305
4. Acquired Immunodeficiency Syndrome Professional Group. Society of infectious diseases; Chinese Medical Association. Chinese guidelines for diagnosis and treatment of human immunodeficiency virus infection/acquired immunodeficiency syndrome (2024 edition). Chin Med J. (2024) 137:2654–80. doi: 10.1097/CM9.0000000000003383
5. Wu, ZY. China’s HIV/AIDS prevention and treatment is facing new situations and challenges. Chin J Public Health. (2011) 27:1505–7. doi: 10.11847/zgggws2011-27-12-01
6. Wu, Z, Chen, J, Scott, SR, and McGoogan, JM. History of the HIV epidemic in China. Curr HIV/AIDS Rep. (2019) 16:458–66. doi: 10.1007/s11904-019-00471-4
7. Wu, ZY. The situation and strategies for AIDS prevention and control in schools in our country. Chin J Sch Health. (2015) 36:1604–5. doi: 10.16835/j.cnki.1000-9817.2015.11.004
8. Huang, Y. Survey on condom awareness and use among post-95 higher vocational college students--taking a higher vocational college in Yiwu as an example. Popular Sci. (2018) 5:131–2. doi: 10.16728/j.cnki.kxdz.2018.05.119
9. Li, G, Jiang, Y, and Zhang, L. HIV upsurge in China’s students. Science. (2019) 364:711. doi: 10.1126/science.aay0799
10. Abdool Karim, SS, Baxter, C, and Abdool, KQ. Advancing HIV prevention using tenofovir-based pre-exposure prophylaxis. Antivir Ther. (2022) 27:13596535211067589. doi: 10.1177/13596535211067589
11. Inciarte, A, Leal, L, Masfarre, L, Gonzalez, E, Diaz-Brito, V, Lucero, C, et al. Post-exposure prophylaxis for HIV infection in sexual assault victims. HIV Med. (2020) 21:43–52. doi: 10.1111/hiv.12797
12. Patel, P, Celum, C, and Bekker, LG. Implementation of HIV prevention strategies globally. Lancet HIV. (2023) 10:e492–4. doi: 10.1016/S2352-3018(23)00139-X
13. Mohan Harjai, M, Sharma, R, Menon, PK, Nagpal, BM, and Singh, Y. Surgeon and HIV infection: post exposure prophylaxis: need of the hour. Med J Armed Forces India. (2000) 56:328–31. doi: 10.1016/S0377-1237(17)30221-6
14. Wu, ZY, and Scott, SR. Human immunodeficiency virus prevention strategies in China. Chin Med J. (2020) 133:318–25. doi: 10.1097/CM9.0000000000000647
15. Bracq, L, Xie, M, Benichou, S, and Bouchet, J. Mechanisms for cell-to-cell transmission of HIV-1. Front Immunol. (2018) 9:260. doi: 10.3389/fimmu.2018.00260
16. Liu, TJ, Wang, GX, Zhang, XY, Mu, YJ, Xing, YR, Kan, Z, et al. The correct use of condoms by college students who engage in sexual activity and its influencing factors. Chin J AIDS STD. (2019) 25:968–969+975. doi: 10.13419/j.cnki.aids.2019.09.26
17. Jones, J, Sullivan, PS, and Curran, JW. Progress in the HIV epidemic: identifying goals and measuring success. PLoS Med. (2019) 16:e1002729. doi: 10.1371/journal.pmed.1002729
18. Dodd, S, Widnall, E, Russell, AE, Curtin, EL, Simmonds, R, Limmer, M, et al. School-based peer education interventions to improve health: a global systematic review of effectiveness. BMC Public Health. (2022) 22:2247. doi: 10.1186/s12889-022-14688-3
19. Rodrigues, VCDC, Lopes, GF, Silveira, GEL, Sousa, IB, Sena, MM, Lopes, TSS, et al. Factors associated with the knowledge and attitude of adolescents regarding male condom use. Rev Bras Enferm. (2021) 74:e20190452. doi: 10.1590/0034-7167-2019-0452
20. Zampetakis, LA, and Melas, C. The health belief model predicts vaccination intentions against COVID-19: a survey experiment approach. Appl Psychol Health Well Being. (2021) 13:469–84. doi: 10.1111/aphw.12262
21. Rosenstock, IM, Strecher, VJ, and Becker, MH. Social learning theory and the health belief model. Health Educ Q. (1988) 15:175–83. doi: 10.1177/109019818801500203
22. Yu, B, Han, JY, Yang, SF, Dong, PJ, and Yang, SJ. Influence of different types of AIDS knowledge on AIDS-related health beliefs of junior college students. Chin J Health Educat. (2020) 36:733–7. doi: 10.16168/j.cnki.issn.1002-9982.2020.08.012
23. Bettinghaus, EP. Health promotion and the knowledge-attitude-behavior continuum. Prev Med. (1986) 15:475–91. doi: 10.1016/0091-7435(86)90025-3
24. Bukuluki, P, Wandiembe, SP, Kisaakye, P, Kiwujja, V, Kajungu, C, and Mugwanya, W. The sexual behavior of young people living with a disability: findings from the KAP study in northern Uganda. Front Reprod Health. (2023) 5:1065437. doi: 10.3389/frph.2023.1065437
26. Dopelt, K, Radon, P, and Davidovitch, N. Environmental effects of the livestock industry: the relationship between knowledge, attitudes, and behavior among students in Israel. Int J Environ Res Public Health. (2019) 16:1359. doi: 10.3390/ijerph16081359
27. Ouattara, LA, Vann, NC, and Doncel, GF. Ex vivo HIV infection model of Cervico-vaginal and rectal tissue. Methods Mol Biol. (2022) 2407:157–72. doi: 10.1007/978-1-0716-1871-4_12
28. Yu, M, Xu, J, Jiang, G, Li, Z, Song, W, Gong, H, et al. Correlates of HIV-infection among men who have sex with men: results from a community-based, cross-sectional study in Tianjin. China AIDS Care. (2019) 31:1574–9. doi: 10.1080/09540121.2019.1612004
29. Yan, Y, and Wang, T. Medical statistics. Fifth ed. Beijing: People’s Health Publishing House (2020). 384 p.
30. Wu, ML. Structural equation modelling: Operations and applications of AMOS. Chongqing: Chongqing University Press. (2010) p: 52–53.
31. Budhwani, H, Hearld, KR, Hasbún, J, Franklin, SG, Vashi, BG, Cataldo, NA, et al. Assessing human immunodeficiency virus (HIV) prevention through knowledge and condom use among female sex workers at the border of Haiti and Dominican Republic. AIDS Patient Care STDs. (2020) 34:477–83. doi: 10.1089/apc.2020.0148
32. Tremelling, J, All, A, Lleras, L, Cancel, A, Jenkins, D, Pina, C, et al. Poor quality male latex condoms found in Dominican Republic: quality assurance evaluation and public health impact. PLoS One. (2019) 14:e0210150. doi: 10.1371/journal.pone.0210150
33. Sun, X, Fan, L, Chang, C, and Shi, Y. HIV/AIDS related perception and behavior: a comparative study among college students of different majors in China. Int J Nurs Sci. (2020) 7:S74–9. doi: 10.1016/j.ijnss.2020.07.010
34. Poteat, T, Cooney, E, Malik, M, and Restar, A. Dangerfield DT 2nd, white J. HIV prevention among cisgender men who have sex with transgender women. AIDS Behav. (2021) 25:2325–35. doi: 10.1007/s10461-021-03194-z
35. Mitchell, JW, Harvey, SM, Champeau, D, and Seal, DW. Relationship factors associated with HIV risk among a sample of gay male couples. AIDS Behav. (2012) 16:404–11. doi: 10.1007/s10461-011-9976-0
36. Elshiekh, HF, Hoving, C, and de Vries, H. Exploring determinants of condom use among university students in Sudan. Arch Sex Behav. (2020) 49:1379–91. doi: 10.1007/s10508-019-01564-2
37. Santos, VP, Coelho, MTÁD, Macário, EL, and Oliveira, TCDS. Is there a relationship between students’ knowledge of HIV/AIDS ways of transmission and their responses regarding their proximity to people living with HIV/AIDS? Ciencia & Saude Coletiva. (2017) 22:2745–52. doi: 10.1590/1413-81232017228.25892015
38. Licata, F, Angelillo, S, Nobile, CGA, Di Gennaro, G, and Bianco, A. Understanding individual barriers to HIV testing among undergraduate university students: results from a cross-sectional study in Italy. Front Med (Lausanne). (2022) 9:882125. doi: 10.3389/fmed.2022.882125
39. Stutts, LA, Robinson, PA, Witt, B, and Terrell, DF. Lost in translation: college students' knowledge of HIV and PrEP in relation to their sexual health behaviors. J Am Coll Heal. (2022) 70:561–7. doi: 10.1080/07448481.2020.1757679
40. Licata, F, Angelillo, S, Oliverio, A, Di Gennaro, G, and Bianco, A. How to safeguard university students against HIV transmission? Results of a cross-sectional study in southern Italy. Front Med (Lausanne). (2022) 9:903596. doi: 10.3389/fmed.2022.903596
41. De Torres, RQ. Facilitators and barriers to condom use among Filipinos: a systematic review of literature. Health Promot Perspect. (2020) 10:306–15. doi: 10.34172/hpp.2020.49
42. Rios-Zertuche, D, Cuchilla, J, Zúñiga-Brenes, P, Hernández, B, Jara, P, Mokdad, AH, et al. Alcohol abuse and other factors associated with risky sexual behaviors among adolescent students from the poorest areas in Costa Rica. Int J Public Health. (2017) 62:271–82. doi: 10.1007/s00038-016-0859-z
43. Han, J, Bouey, JZ, Wang, L, Mi, G, Chen, Z, He, Y, et al. PrEP uptake preferences among men who have sex with men in China: results from a National Internet Survey. J Int AIDS Soc. (2019) 22:e25242. doi: 10.1002/jia2.25242
44. Fauk, NK, Kustanti, CY, Liana, DS, Indriyawati, N, Crutzen, R, and Mwanri, L. Perceptions of determinants of condom use behaviors among male clients of female sex workers in Indonesia: a qualitative inquiry. Am J Mens Health. (2018) 12:666–75. doi: 10.1177/1557988318756132
45. Arendt, F, Hauck, P, Mayr, J, and Negwer, F. Anti-stigma HIV-related social advertising: no evidence for side effects on condom use. Health Commun. (2019) 34:135–8. doi: 10.1080/10410236.2017.1384435
46. Okeke, SR. "I always prefer to withdraw than use a condom": contextualising condomless sex among east Asian and sub-Saharan African international students in Sydney. Arch Public Health. (2022) 80:20. doi: 10.1186/s13690-021-00777-z
47. Voyiatzaki, C, Venetikou, MS, Papageorgiou, E, Anthouli-Anagnostopoulou, F, Simitzis, P, Chaniotis, DI, et al. Awareness, knowledge and risky behaviors of sexually transmitted diseases among young people in Greece. Int J Environ Res Public Health. (2021) 18:10022. doi: 10.3390/ijerph181910022
48. Youssef, L, Hallit, S, Sacre, H, Salameh, P, Cherfan, M, Akel, M, et al. Correction: knowledge, attitudes and practices towards people living with HIV/AIDS in Lebanon. PLoS One. (2021) 16:e0259359. doi: 10.1371/journal.pone.0259359
49. Musche, V, Kohler, H, Bäuerle, A, Schweda, A, Weismüller, B, Fink, M, et al. COVID-19-related fear, risk perception, and safety behavior in individuals with diabetes. Healthcare (Basel). (2021) 9:480. doi: 10.3390/healthcare9040480
50. Yao, J, Wan, YY, and Yuan, XX. Investigation on status quo of condom cognition and sexual behavior among 1897 college students in a university. Chin J School Doctor. (2022) 36:660–3. Available at: https://kns.cnki.net/kcms2/article/abstract?v=IVqNFfq6ZnJIuXFd7fRILKi2OufWllFWrvdFzgJKTR_tJQLXMFRkbtUrqElpCvhCbUUDJpNcj5JYQvnqduhDkKt1ck-omUIxXLHlvQQ6RuzzUaRhk5HaP7W0APvZbr4patjZX8-bVyVrjf6T3ce4t5Dc_xmqF2wY8lK8VKMsEuUGpqYyaZ9ipg==&uniplatform=NZKPT&language=CHS
51. Elamouri, F, Rockstroh, JK, Kratoo, W, Miyahara, Y, and Pumpaibool, T. HIV/AIDS knowledge and attitudes towards HIV and condom use among internally displaced Libyan males. Is there a need to implement sex education? HIV Res Clin Pract. (2024) 25:2305554. doi: 10.1080/25787489.2024.2305554
Keywords: college students, sexual behaviors, perception of infection risk, perceived disorders of preventive behavior, perceived benefits of preventive behavior, attitudes of preventive behavior, behavior of wearing condoms, HIV
Citation: Qi L, Guo R, Qu Y and Li X (2025) A cross-sectional survey about behavior of wearing condoms among college students who engage in sexual activity: the mediating role of attitudes of preventive behavior. Front. Public Health. 13:1544564. doi: 10.3389/fpubh.2025.1544564
Edited by:
Augustine Talumba Choko, Malawi-Liverpool-Wellcome Trust Clinical Research Programme, MalawiReviewed by:
Ketan Chitnis, UNICEF United Nations International Children’s Emergency Fund, United StatesFrancesca Licata, University Magna Graecia of Catanzaro, Italy
Copyright © 2025 Qi, Guo, Qu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaomei Li, cm9zZWxlZUB4anR1LmVkdS5jbg==
 Li Qi
Li Qi Ronghuang Guo2
Ronghuang Guo2 Yi Qu
Yi Qu