- 1The First Hospital of Jinzhou Medical University, Jinzhou, Liaoning, China
- 2School of Nursing, Jinzhou Medical University, Jinzhou, Liaoning, China
- 3Department of Editorial (Social Sciences Edition), Jinzhou Medical University, Jinzhou, China
Objective: Exploring the Relationship between Hearing Loss, psychological well-being, and Depressive Symptoms in Rural older adults: Validating the Mediating Role of psychological well-being in the Impact of Hearing Loss on Depressive Symptoms to Provide a Theoretical Basis for Improving the Mental Health of Rural older adults.
Methods: The study focuses on 5,273 rural older individuals aged 65 and above, using data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS) database. Hearing loss was assessed through self-report. Psychological well-being was evaluated using the Current Situation Assessment and Personality Emotional Characterization from the database. Depressive symptoms were measured using the short form of the Center for Epidemiologic Studies Depression Scale (CESD-10). The analysis involved using SPSS 27.0 and PROCESS v4.1 to conduct correlation analysis, regression analysis, and mediation effect analysis.
Results: The depressive symptoms score for rural older individuals was (13.02 ± 4.48), and the psychological well-being score was (19.13 ± 2.47). There was a negative correlation between depressive symptoms and psychological well-being (r = −0.123, p < 0.001), there was a negative correlation between depressive symptoms and hearing loss (r = −0.086, p < 0.001). A negative correlation was also observed between hearing loss and psychological well-being (r = −0.060, p < 0.001). Psychological well-being mediates the effect of hearing loss on depressive symptoms among rural older individuals.
Conclusion: Hearing loss in rural older individuals exerts both direct effects on depressive symptoms and indirect effects through the mediating role of psychological well-being. Specifically, the impairment of auditory function not only exacerbates emotional distress, but also diminishes psychological adaptability, thereby creating a dual pathway for depression development.
1 Introduction
In recent years, the prevalence and disability rates of hearing loss among the older adults have been rising, leading to a significant disease burden. Data indicate that in 2019, approximately 1.57 billion people worldwide had hearing loss, accounting for 20% of the global population (1). Hearing loss not only reduces quality of life but also contributes to the development of diseases such as dementia (2). Depression is one of the most common mental disorders among the older adults, with a prevalence of 20.0% among older adults in China (3). Depression is a leading cause of disability in the older adults, severely impacting their physical and mental health and adding stress to family and social relationships, thereby increasing the socioeconomic burden (4). Consequently, preventing depression in older adults is of significant public health importance.
Current research indicates a significant association between hearing loss and depressive symptoms. Studies have found that hearing loss can lead to social isolation, communication difficulties, and reduced self-esteem, which in turn increases the risk of depressive symptoms (5, 6). For rural older populations, where living conditions, medical resources, and social support are relatively limited, the impact of hearing loss and depressive symptoms may be even more pronounced. Psychological well-being reflects an individual’s emotional stability and adaptability in the face of stress and challenges. Hearing loss not only affects depressive symptoms but also negatively impacts psychological well-being. The communication barriers and reduced social interactions caused by hearing loss can lead to anxiety, loneliness, and identity crises, which weaken psychological well-being (7, 8). Research suggests that individuals with hearing loss exhibit lower emotional stability and adaptability under stress, resulting in reduced psychological well-being (9). Good psychological well-being can help individuals better cope with life’s pressures and challenges, thereby reducing the risk of depressive symptoms (10). Studies show that individuals with higher levels of psychological well-being have a significantly lower incidence of depressive symptoms compared to those with lower levels of psychological well-being (11).
Emerging evidence highlights that the relationship between hearing loss and depressive symptoms in older adults extends beyond psychosocial pathways to involve shared pathophysiological mechanisms. Neurobiologically, age-related hearing loss may accelerate cortical atrophy in brain regions critical for emotional regulation, impairing top-down control over negative affective states and heightening vulnerability to depression (12, 13). Additionally, chronic auditory deprivation disrupts neuroplasticity, potentially altering dopaminergic and serotonergic pathways implicated in mood disorders (14).
Peripherally, hearing loss is associated with systemic inflammation, marked by elevated pro-inflammatory cytokines, which are independently linked to depressive symptomatology (15). Furthermore, the increased cognitive load required to compensate for auditory deficits may overburden neural resources, exacerbating stress responses via hypothalamic–pituitary–adrenal (HPA) axis dysregulation and chronic cortisol elevation—a known risk factor for depression (16). Vascular comorbidities, common in aging populations, may also mediate this relationship by contributing to both auditory dysfunction and cerebrovascular damage in mood-regulating circuits (17, 18). These intertwined mechanisms suggest that hearing loss and depressive symptoms may mutually reinforce one another through bidirectional neurophysiological disruptions.
Based on existing research, this study hypothesizes that diminished psychological well-being (i.e., low mental health) mediates the effect of hearing loss on depressive symptoms. Specifically, hearing loss may increase the risk of depressive symptoms indirectly by reducing psychological well-being, rather than merely correlating with mental health as a broad construct. Using data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), this study explores the relationships among hearing loss, psychological well-being, and depressive symptoms in rural older individuals. The aim is to verify the mediating role of low psychological well-being in the pathway linking hearing loss to depressive symptoms, providing a scientific basis for developing targeted mental health interventions.
2 Methods
2.1 Study participants
The data used in this study were sourced from the 8th wave of the CLHLS project conducted by Peking University. The CLHLS is one of the most extensive and longest-running social science surveys in China, spanning from 1998 to 2018 and covering 23 provinces, municipalities, and autonomous regions. The cumulative sample size reached 113,000 participants. The 8th wave was conducted from 2017 to 2018 and included 15,874 individuals. The inclusion criteria for this study were as follows: (1) rural older individuals aged 65 and above; (2) availability of results from the Center for Epidemiologic Studies Depression Scale (CES-D-10); (3) availability of psychological well-being data; and (4) availability of hearing loss data. A total of 8,780 non-rural older individuals, 619 individuals without responses for depressive symptoms, and 1,202 individuals without responses for psychological well-being were excluded. A total of 5,273 rural older individuals met the inclusion criteria and were selected as the study population.
2.2 Research tools
1. Assessment of depressive symptoms: in this study, depressive symptoms were screened using the short version of the Center for Epidemiologic Studies Depression Scale (CES-D-10). This scale includes 10 items designed to assess depressive symptoms experienced by older individuals over the past week. Each item is scored from 0 to 3, with 2 items requiring reverse scoring. The total score ranges from 0 to 30, with a score of ≥10 indicating the presence of depressive symptoms and a score of <10 indicating their absence. The CES-D-10 has been widely used for screening depressive symptoms in older populations in China, demonstrating good reliability and validity with a Cronbach’s alpha coefficient of 0.78 (19, 20).
2. Hearing loss in this study was assessed through self-reported information from participants, a method validated in previous research (21, 22). Participants were first asked, “Do you have a disability involving deafness or partial deafness?” with responses coded as 0 (no impairment) or 1 (presence of impairment). To enhance assessment validity, we supplemented this measure with data on hearing aid usage by asking: “Do you currently use any hearing assistance devices (e.g., hearing aids or cochlear implants)?” Participants reporting hearing aid use were analyzed separately as a subgroup and included as a covariate in sensitivity analyses to account for potential mitigation of hearing impairment effects.
3. Assessment of psychological well-being: based on established indicators and calculation methods from previous studies (23–26), we developed the assessment for psychological well-being. This study evaluated psychological well-being through questions in the “Current Situation Assessment and Personality Emotional Traits” questionnaire, which captures older individuals’ subjective views on their overall quality of life and living standards, thereby providing a measure of psychological well-being. The survey included three questions reflecting positive emotions: “How do you feel about your life right now?,” “Can you think about what’s happening?,” and “Do you feel energetic?” Negative emotions were assessed with three questions: “Do you feel ashamed, regretful, or guilty about things you have done?,” “Do you feel angry at people or things you dislike?,” and “Do you often feel people around you are untrustworthy?” Responses to the positive emotion questions were reverse scored, from “very good” (5 points) to “very poor” (1 point). In contrast, the negative emotion questions were scored directly, with “always” scoring 1 point and “never” scoring 5 points. This standardization facilitated data measurement and calculation. Scores for positive and negative emotions each ranged from 3 to 15, with an overall psychological well-being score ranging from 6 to 30. Higher scores indicate better psychological well-being. In this research, the scale showed strong internal consistency, with a Cronbach’s α value of 0.860.
2.3 Data analysis
Data were analyzed using SPSS version 27.0. Quantitative data were expressed as mean ± standard deviation, while qualitative data were reported as frequency and composition ratio. Pearson correlation analysis was conducted to examine the relationships among hearing loss, psychological well-being, and depressive symptoms in rural older individuals. The mediation effect of psychological well-being between hearing loss and depressive symptoms was analyzed using the Process 4.1 plugin, with the Bootstrap method applied to test the mediation effect through 5,000 resampling iterations to calculate the 95% confidence interval. A p < 0.05 was considered statistically significant.
3 Results
3.1 Demographic information of rural older adults
The results of this study show that the age range of participants was 67–117 years, with an average age of 82.8 ± 11.1 years. Gender distribution included 2,343 males (46.1%) and 2,930 females (53.9%). Ethnicity distribution was as follows: 3,992 Han Chinese (75.7%) and 1,281 individuals from other ethnic groups (24.3%). Educational levels were categorized as follows: primary school or below for 1,859 individuals (35.3%), middle school for 972 individuals (18.4%), and high school or above for 2,442 individuals (46.3%). Marital status showed that 2,912 participants (55.2%) were without a spouse, while 2,361 participants (44.8%) had a spouse. Additionally, 929 participants (17.6%) were smokers, and 856 participants (16.2%) consumed alcohol.
3.2 Psychological well-being and depressive symptom scores and the relationship between hearing impairment, psychological well-being and depressive symptoms in rural older adults
The depressive symptom score among rural older individuals was 13.02 ± 4.48, and the psychological well-being score was 19.13 ± 2.47. There was a negative correlation between depressive symptom scores and psychological well-being (r = −0.123, p < 0.001) and a negative correlation between depressive symptom scores and hearing loss (r = −0.086, p < 0.001). Additionally, there was a negative correlation between hearing loss and psychological well-being (r = −0.060, p < 0.001) (Table 1).
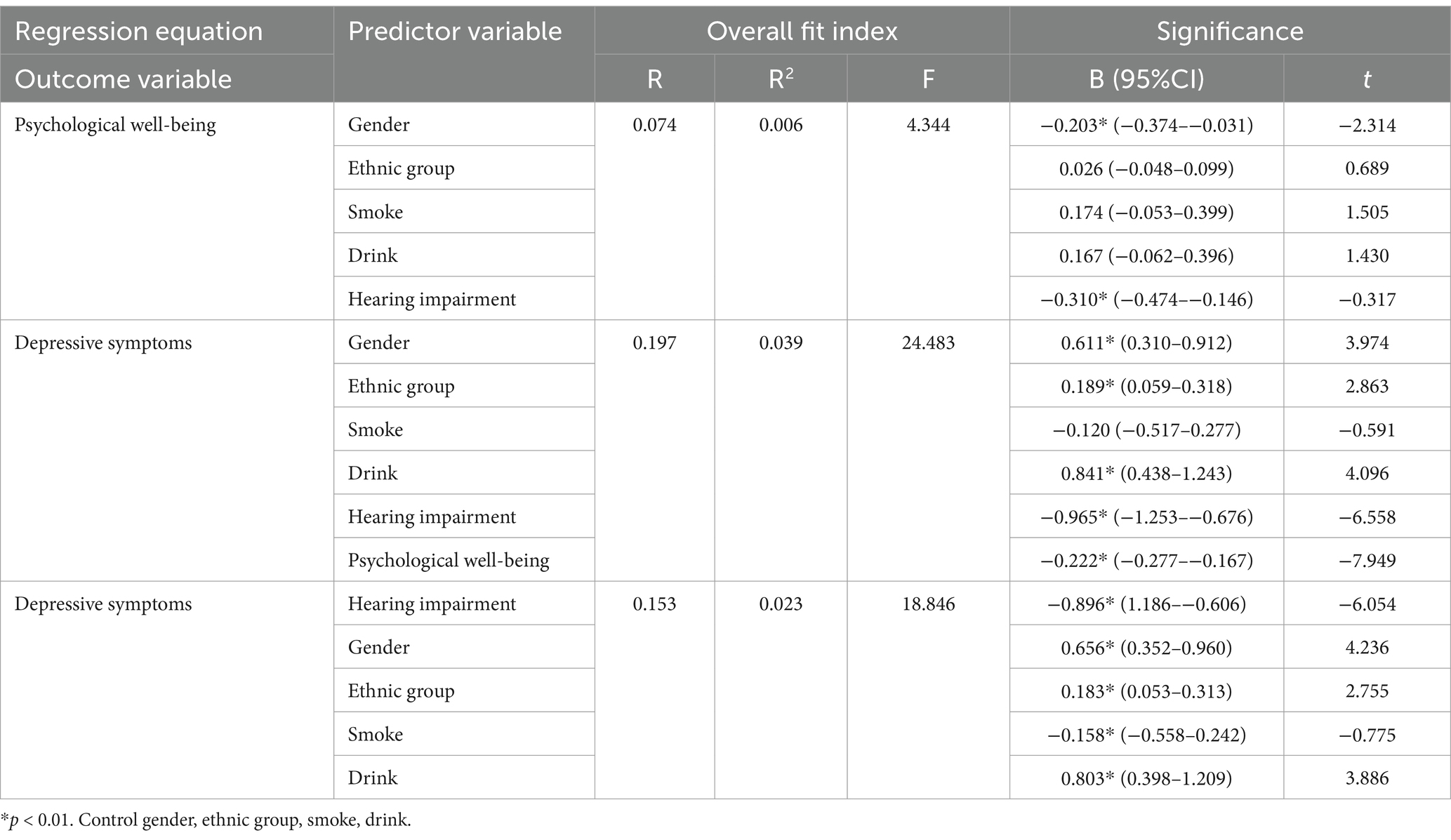
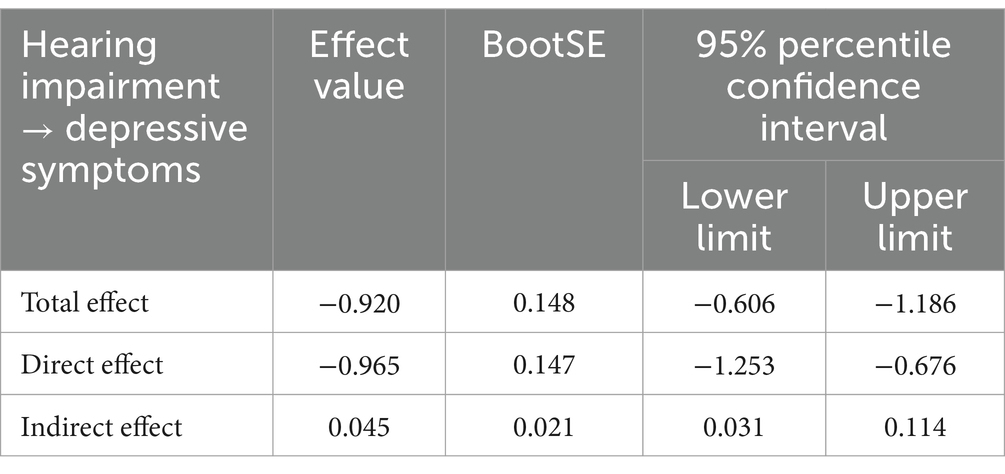
Table 1. Analysis of the mediating effect of psychological well-being among rural older adults between the effects of hearing impairment on depressive symptoms.
3.3 Analysis of the mediating effect of psychological well-being between hearing impairment and depressive symptoms
A mediation model was constructed with hearing loss as the predictor variable, depressive symptoms as the outcome variable, and psychological well-being as the mediating variable. Mediation analysis was conducted using Model 4 of the SPSS Process component. The results indicated that hearing loss had a significant negative predictive effect on depressive symptoms (β = −0.965, p < 0.001), while psychological well-being had a significant negative predictive effect on depressive symptoms (β = −0.222, p < 0.001). Additionally, hearing loss significantly negatively predicted psychological well-being (β = −0.203, p < 0.001). These results are shown in Table 2, and the path coefficients among the variables are illustrated in Figure 1.
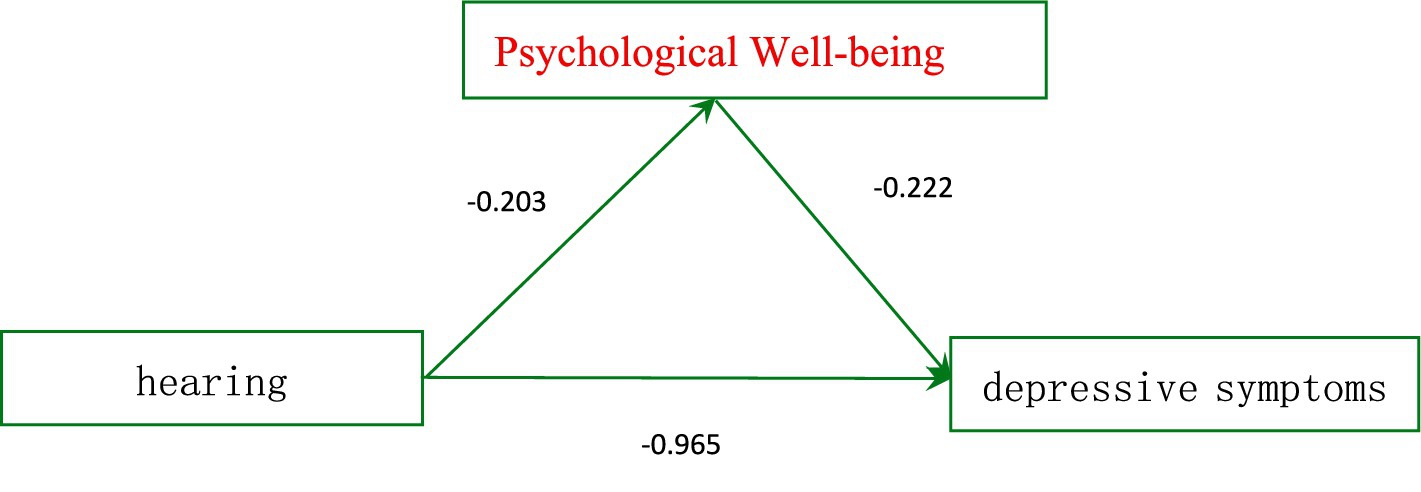
Figure 1. Mediating effect of psychological well-being in the effect of hearing impairment on depressive symptoms.
To further examine the mediation effect, a bias-corrected nonparametric percentile Bootstrap method, as provided by Hayes, was applied with 5,000 resamples and a 95% confidence interval. The results (see Table 2) revealed a significant indirect effect of hearing loss on depressive symptoms through psychological well-being (mediation effect = 0.045, SE = 0.021), with a 95% confidence interval [0.031, 0.114] that did not include zero, indicating that psychological well-being mediated the relationship between hearing loss and depressive symptoms among rural older individuals. The mediation effect accounted for 4.9% of the total effect.
4 Discussion
The results of this study indicate a negative correlation between hearing loss and depressive symptoms among rural older individuals (r = −0.086, p < 0.001), suggesting that more severe hearing loss may be associated with higher scores of depressive symptoms. The impact of hearing loss on depressive symptoms in the older adults is complex; in addition to increased social isolation and psychological burden, hearing loss may also lead to declining physical health, increased risk of chronic diseases, and poorer sleep quality—all physiological factors linked to depression (13, 27).
A negative correlation was found between hearing loss and psychological well-being (r = −0.060, p < 0.001), indicating that worsening hearing loss may affect psychological well-being in older individuals. Due to the cognitive load required to cope with hearing difficulties, psychological well-being may become compromised (28). Hearing loss can diminish self-efficacy, impacting confidence and ability to face challenges, thereby lowering psychological well-being levels (29). Additionally, psychological well-being scores among rural older individuals were negatively correlated with depressive symptoms (r = −0.123, p < 0.001), meaning that lower psychological well-being scores were associated with more severe depressive symptoms. This negative correlation reflects the potential influence of psychological well-being on depressive symptoms. In rural older populations, psychological well-being encompasses not only emotional stability but also adaptability to life’s challenges and self-regulation mechanisms. Studies indicate that poor psychological well-being may hinder effective emotional regulation, thereby increasing the risk of depressive symptoms (30). Furthermore, with aging, cognitive function in the older adults gradually declines, particularly affecting cognitive flexibility and decision-making ability, which increases susceptibility to depression. This finding is supported by studies, such as those by Kuo et al. (31).
Psychological well-being plays an important role in mitigating the impact of hearing loss on depressive symptoms among rural older individuals. Firstly, it enhances emotional regulation, helping individuals cope more effectively with the negative emotional responses caused by hearing loss. This includes cognitive regulation of emotions and emotional expression, enabling older individuals to face various life challenges and stresses more resiliently (32–36). Additionally, good psychological well-being helps protect mental resources, including cognitive abilities, emotional support, and coping strategies, reducing the potential depletion of these resources due to hearing loss. This protective effect helps maintain a more stable emotional state and higher life satisfaction among older individuals (37).
Furthermore, psychological well-being strengthens social support networks (such as family, friends, and community), providing emotional security and tangible support. This support and connection not only help older individuals better cope with the psychological stress and loneliness associated with hearing loss but also reduce the occurrence of depressive symptoms (38).
The analysis above demonstrates that psychological well-being plays a crucial mediating role in alleviating the impact of hearing loss on depressive symptoms among rural older individuals. A deeper understanding of these mechanisms and pathways can aid in developing targeted interventions to improve mental health and quality of life for the older adults. Based on this, the following measures are proposed to reduce depressive symptoms in rural older populations:
Prioritize personalized hearing aid fitting, auditory rehabilitation training, and regular hearing assessments to directly mitigate neurobiological stress responses caused by sensory deprivation. Implement cognitive-behavioral therapy (twice weekly) and digital emotion regulation training alongside auditory rehabilitation. Use virtual reality (VR) to simulate social scenarios for auditory-emotional integration exercises.
Establish a “Hearing-Friendly Community” certification program, mandating loop amplification systems in public spaces (39). Develop dialect-adaptive hearing aids and deploy interdisciplinary teams (audiologists + rural social workers + AI technicians) for monthly in-home device maintenance and psychological evaluation (40).
Design dual-task protocols combining auditory discrimination and cognitive exercises, enhanced by transcranial direct current stimulation (tDCS) to boost auditory cortex plasticity. Implement EEG biofeedback systems for real-time emotion regulation, dynamically adjusting intervention intensity based on neural activity.
Launch an intergenerational communication app that automatically optimizes grandchildren’s speech for high-frequency enhancement. Create a “Sound Memory Museum” digital platform using reminiscence therapy to rebuild auditory self-efficacy.
Apply machine learning to predict hearing loss trajectories, initiating 6-month preemptive cognitive reserve enhancement for high-risk individuals. Establish a rural auditory biobank to investigate gene–environment interactions affecting depression susceptibility.
5 Limitation
While this study provides valuable insights into the relationship between hearing loss, psychological well-being, and depressive symptoms in rural older individuals, several limitations should be acknowledged.
A noteworthy consideration is the potential role of suppression effects in the relationship between hearing loss, psychological well-being, and depressive symptoms. While our findings highlight psychological well-being as a mediator that amplifies the association between hearing loss and depressive symptoms (i.e., hearing loss reduces psychological well-being, which in turn exacerbates depressive symptoms), suppression effects may arise if unaccounted variables indirectly oppose the total effect. For instance, certain factors (e.g., compensatory social engagement or adaptive coping strategies triggered by hearing loss) could theoretically counteract the negative psychological consequences, creating a suppression mechanism where the indirect effect opposes the direct or total effect (41). Although our current model did not identify such suppression pathways, this possibility underscores the complexity of psychosocial mechanisms in aging populations. Future studies should explicitly test for suppression effects using moderated mediation or countervailing pathway analyses to disentangle these dynamics.
The data used in this study are cross-sectional, meaning that only a snapshot of the participants’ conditions was captured at a single point in time. As a result, the causality between hearing loss, psychological well-being, and depressive symptoms cannot be definitively established. Longitudinal studies would be beneficial in providing a clearer understanding of the temporal relationships between these variables and in identifying causal pathways.
Hearing loss in this study was assessed based on self-reported data, which may be subject to recall bias or misclassification. Participants’ perceptions of their hearing abilities may not fully reflect the actual severity of their hearing loss, as they might not accurately recognize or report the extent of their hearing difficulties. Future studies should consider objective hearing assessments (e.g., audiometric testing) to validate self-reported hearing loss and obtain more accurate data.
The assessment of psychological well-being was based on a questionnaire that captured subjective views on quality of life and emotional traits. While this tool demonstrated strong internal consistency, it remains a self-report measure, which can be influenced by individual perceptions, mood states, or social desirability bias. Additionally, the scale might not capture all dimensions of psychological well-being, and future research could benefit from incorporating more comprehensive measures that assess additional factors such as life satisfaction, social connectedness, and coping strategies.
This study focused specifically on rural older individuals, and the findings may not be generalizable to urban populations or to older individuals in other geographic regions of China or internationally. Rural populations often face unique social, economic, and healthcare challenges that may not be reflective of those encountered by urban older populations. Thus, caution is needed when interpreting these results in a broader context.
Although this study accounted for key variables such as depressive symptoms and hearing loss, there may be other potential confounders that were not included in the analysis. Factors such as socioeconomic status, social support, chronic illnesses, and access to healthcare could also play a significant role in the relationship between hearing loss, psychological well-being, and depressive symptoms. Future research should consider including these variables to further refine our understanding of the interplay between these factors.
While the study sample of 5,273 rural older individuals is substantial, the inclusion criteria focused specifically on older individuals with available data for depressive symptoms, psychological well-being, and hearing loss. As a result, there may be selection bias in the sample, potentially excluding individuals who may be more vulnerable to depressive symptoms but who were not included due to missing data or other reasons. Efforts to address missing data and ensure a more representative sample in future studies could enhance the generalizability of the findings.
Despite these limitations, this study provides important insights into the role of psychological well-being in the relationship between hearing loss and depressive symptoms among rural older individuals, suggesting potential avenues for future research and interventions aimed at improving the mental health of this population.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
The data from CLHLS survey already obtained the ethical approval and informed consent and was approved by the Ethics Committee of Peking University (IRB00001052-13074). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
QS: Writing – review & editing. ZJ: Writing – original draft, Writing – review & editing. ZX: Data curation, Writing – review & editing. MZ: Data curation, Writing – review & editing. XZ: Data curation, Writing – review & editing. TL: Data curation, Writing – review & editing. SZ: Data curation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Support Program for Liaoning Province Social Science Planning Fund Youth Project (L24BSH004).
Acknowledgments
This research utilized data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS). We appreciate the support of the project team.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. GBD Hearing Loss Collaborators. Hearing loss prevalence and years lived with disability, 1990-2019: findings from the global burden of disease study. Lancet. (2021) 397:996–1009. doi: 10.1016/S0140-6736(21)00516-X
3. Pang, WD, Ren, JJ, and Zhao, Y. Research progress on the relationship between hearing loss and dementia. Chin J Otol. (2022) 20:319–23. doi: 10.3969/j.issn.1672-2922.2022.02.029
4. Xu, SS, Hou, C, Han, X, Hu, Y, Yang, H, Shang, Y, et al. Adverse health consequences of undiagnosed hearing loss at middle age: a prospective cohort study with the UK biobank. Maturitas. (2023) 174:30–8. doi: 10.1016/j.maturitas.2023.05.002
5. Tang, T, Jiang, JL, and Tang, XF. Prevalence of depressive symptoms among older adults in China: a systematic review and meta-analysis. J Affect Disord. (2021) 293:379–90. doi: 10.1016/j.jad.2021.06.050
6. Friedrich, MJ. Depression is the leading cause of disability around the world. JAMA. (2017) 317:1517. doi: 10.1001/jama.2017.3826
7. Jiang, F, Kuper, H, Zhou, CC, Qin, W, and Xu, L. Relationship between hearing loss and depression symptoms among older adults in China:the mediating role of social isolation and loneliness. Int J Geriatr Psychiatry. (2022) 37:123–50. doi: 10.1002/gps.5729
8. Ye, X, Zhu, DW, Gao, JM, Chen, SY, and He, P. The impact of hearing on the depression of older Chinese adults. Popul Dev. (2019) 25:66–74.
9. Dobrota, SD, Biggs, ML, Pratt, S, Popat, R, and Odden, MC. The association of hearing problems with social network strength and depressive symptoms: the cardiovascular health study. Age Ageing. (2022) 51:afac181. doi: 10.1093/ageing/afac181
10. Huang, H, Wang, J, Jiang, CQ, Zhu, F, Jin, YL, Zhu, T, et al. Hearing loss and depressive symptoms in older Chinese: whether social isolation plays a role. BMC Geriatr. (2022) 22:3311. doi: 10.1186/s12877-022-03311-0
11. Cosh, S, Carriere, I, Delcourt, C, Helmer, C, and Consortium, TS. A dimensional approach to understanding the relationship between self-reported hearing loss and depression over 12 years: the Three-City study. Aging Ment Health. (2021) 25:954–61. doi: 10.1080/13607863.2020.1727845
12. Uhlmann, RF, Larson, EB, Rees, TS, Koepsell, TD, and Duckert, LG. Relationship of hearing impairment to dementia and cognitive dysfunction in older adults. JAMA. (1989) 261:1916–9. doi: 10.1001/jama.1989.03420130084028
13. Rutherford, BR, Brewster, K, Golub, JS, Kim, AH, and Roose, SP. Sensation and psychiatry: linking age-related hearing loss to late-life depression and cognitive decline. Am J Psychiatry. (2018) 175:215–24. doi: 10.1176/appi.ajp.2017.17040423
14. Golub, JS, Brewster, KK, Brickman, AM, Ciarleglio, AJ, Kim, AH, Luchsinger, JA, et al. Association of audiometric age-related hearing loss with depressive symptoms among Hispanic individuals. JAMA Otolaryngol Head Neck Surg. (2019) 145:132–9. doi: 10.1001/jamaoto.2018.3270
15. Lassale, C, Vullo, P, Cadar, D, Batty, GD, Steptoe, A, and Zaninotto, P. Association of inflammatory markers with hearing impairment: the English longitudinal study of ageing. Brain Behav Immun. (2020) 83:112–9. doi: 10.1016/j.bbi.2019.09.020
16. Fu, X, Liu, B, Wang, S, Robert, H, and Dona, MP. The relationship between hearing loss and cognitive impairment in a Chinese elderly population, the baseline analysis. Front Neurosci. (2021) 15:749273. doi: 10.3389/fnins.2021.749273
17. Oussoren, FK, Schermer, TR, van Leeuwen, RB, and Bruintjes, TD. Cardiovascular risk factors, cerebral small vessel disease, and subsequent risk of stroke in patients with idiopathic sudden sensorineural hearing loss: systematic review and Meta-analyses of the current literature. Audiol Neurootol. (2024) 29:1–29. doi: 10.1159/000530686
18. Hovaldt, HB, Nielsen, T, and Dammeyer, J. Validity and reliability of the major depression inventory for persons with dual sensory loss. Innov Aging. (2018) 2:igy010. doi: 10.1093/geroni/igy010
19. Zhao, M, Wang, Y, Wang, S, Yang, Y, Li, M, and Wang, K. Association between depression severity and physical function among Chinese nursing home residents: the mediating role of different types of leisure activities. Int J Environ Res Public Health. (2022) 19:3543. doi: 10.3390/ijerph19063543
20. Xu, R, Liu, Y, Mu, T, Ye, Y, and Xu, C. Determining the association between different living arrangements and depressive symptoms among over-65-year-old people: the moderating role of outdoor activities. Front Public Health. (2022) 10:954416. doi: 10.3389/fpubh.2022.954416
21. Amieva, H, and Ouvrard, C. Does treating hearing loss in older adults improve cognitive outcomes? A review. J Clin Med. (2020) 9:805. doi: 10.3390/jcm9030805
22. Ma, W, Zhang, Y, Li, X, Liu, S, Gao, Y, Yang, J, et al. High-frequency hearing loss is associated with anxiety and brain structural plasticity in older adults. Front Aging Neurosci. (2022) 14:821537. doi: 10.3389/fnagi.2022.821537
23. Jiang, K, and Chen, Y. Can parent-child living together improve the well-being of the elderly? Evident based on CLHLS data. Popul. J. (2016) 38:77–86. doi: 10.16405/j.cnki.doi:1004-129X.2016.06.008-en
24. Jiang, Z, Xu, Z, Zhou, M, Zhang, H, and Zhou, S. The mediating role of psychological equilibrium in the relationship between dietary variety and self-reported health among older adults in rural China. Sci Rep. (2025) 15:4240. doi: 10.1038/s41598-025-88835-2
25. Jiang, Z, Xu, Z, Zhou, M, Huijun, Z, and Zhou, S. The influence of healthy eating index on cognitive function in older adults: chain mediation by psychological balance and depressive symptoms. BMC Geriatr. (2024) 24:904. doi: 10.1186/s12877-024-05497-x
26. Bishop, NJ, and Zuniga, KE. Egg consumption, multi-domain cognitive performance, and short-term cognitive change in a representative sample of older U.S. Adults J Am Coll Nutr. (2019) 38:537–46. doi: 10.1080/07315724.2019.1566035
27. Lin, FR, Metter, EJ, O'Brien, RJ, Resnick, SM, Zonderman, AB, and Ferrucci, L. Hearing loss and incident dementia. Arch Neurol. (2011) 68:214–20. doi: 10.1001/archneurol.2010.362
28. Hazan, V, Tuomainen, O, Tu, L, Kim, J, Davis, C, Brungart, D, et al. How do aging and age-related hearing loss affect the ability to communicate effectively in challenging communicative conditions? Hear Res. (2018) 369:33–41. doi: 10.1016/j.heares.2018.06.009
29. Iwagami, M, Kobayashi, Y, Tsukazaki, E, Watanabe, T, Sugiyama, T, Wada, T, et al. Associations between self-reported hearing loss and outdoor activity limitations, psychological distress and self-reported memory loss among older people: analysis of the 2016 comprehensive survey of living conditions in Japan. Geriatr Gerontol Int. (2019) 19:747–54. doi: 10.1111/ggi.13708
30. Kuo, PL, Di, J, Ferrucci, L, et al. Analysis of hearing loss and physical activity among US adults aged 60-69 years. JAMA Netw Open. (2021) 4:e215484. doi: 10.1001/jamanetworkopen.2021.5484
31. Jiang, ZQ, Zhou, SX, Huang, MN, Sun, Q, Wang, DD, et al. Study on the relationship between homebound, depression, and cognitive function among rural empty-nest elderly. J Nurs Educ. (2024) 39:313–6. doi: 10.16821/j.cnki.hsjx.2024.03.016
32. Jiang, ZQ, Zhou, SX, and Sun, R. The relationship between personality characteristics, social support and subjective well-being of empty-nest elderly. Modern Prev Med. (2020) 47:2396–9.
33. Jiang, ZQ, Zhou, SX, Tang, KT, Yao, C, Wang, YD, Zhao, LC, et al. The mediating effect of psychological resilience on the alienation and subjective well-being of rural empty-nest elderly. Journal of. Nurs Sci. (2021) 36:89–94.
34. Jiang, Z, Zhou, S, Huang, M, Sun, Q, Wang, DD, Zhang, LL, et al. Study on the status of self-care ability and influencing factors among rural empty-nest elderly. J Nursing. (2024) 39:92–9.
35. Jiang, Z, Zhou, S, and Zhou, X. The influence of psychological resilience on self-care ability among rural empty-nest elderly. Chin J Behav Med Brain Sci. (2024) 33:347–51. doi: 10.3760/cma.j.cn371468-20230824-00065
36. Yu, S, Guo, N, Zheng, C, Song, Y, and Hao, J. Investigating the association between outdoor environment and outdoor activities for seniors living in old residential communities. Int J Environ Res Public Health. (2021) 18:7500. doi: 10.3390/ijerph18147500
37. Yin, Z, Brasher, MS, Kraus, VB, Lv, Y, Shi, X, and Zeng, Y. Dietary diversity was positively associated with psychological resilience among elders: a population-based study. Nutrients. (2019) 18:650. doi: 10.3390/nu11030650
38. MacKinnon, DP, Krull, JL, and Lockwood, CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. (2000) 1:173–81. doi: 10.1023/a:1026595011371
39. Swanepoel, W. Advancing equitable hearing care: innovations in technology and service delivery. Folia Phoniatr Logop. (2023) 75:201–7. doi: 10.1159/000530671
40. Kaspar, A, Pifeleti, S, and Driscoll, C. The role of health promotion in the development of ear and hearing health services in the Pacific Islands: a literature review. SAGE Open Med. (2021) 9:2050312121993287. doi: 10.1177/2050312121993287
Keywords: rural older adults, hearing loss, psychological well-being, mediation effect, depressive symptoms
Citation: Sun Q, Jiang Z, Xu Z, Zhou M, Zhang X, Liu T and Zhou S (2025) Exploring the role of psychological well-being in the impact of hearing loss on depressive symptoms in rural older adults. Front. Public Health. 13:1545483. doi: 10.3389/fpubh.2025.1545483
Edited by:
Anthony Vee Yee Alexander Chong, Monash University Malaysia, MalaysiaReviewed by:
Sten Olof Martin Hellström, Karolinska Institutet (KI), SwedenXinxing Fu, Capital Medical University, China
Changqing Sun, Zhengzhou University, China
Copyright © 2025 Sun, Jiang, Xu, Zhou, Zhang, Liu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qi Sun, bG55eHlqenFAc2luYS5jb20=
 Qi Sun1*
Qi Sun1* Zhaoquan Jiang
Zhaoquan Jiang Zhaoxu Xu
Zhaoxu Xu