- 1Division of Population Health, Health Services Research and Primary Care, National Institute for Health and Care Research (NIHR) School for Primary Care Research, University of Manchester, Manchester, United Kingdom
- 2Division of Population Health, Health Services Research and Primary Care, Manchester Centre for Health Economics, University of Manchester, Manchester, United Kingdom
- 3Division of Population Health, Health Services Research and Primary Care, Centre for Biostatistics, University of Manchester, Manchester, United Kingdom
- 4Division of Pharmacy and Optometry, National Institute for Health and Care Research Greater Manchester Patient Safety Research Collaboration, University of Manchester, Manchester, United Kingdom
- 5Division of Informatics, Imaging and Data Sciences, University of Manchester, Manchester, United Kingdom
- 6Centre for Pharmacoepidemiology and Drug Safety, School of Health Sciences, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom
- 7School of Medicine, Keele University, Keele, United Kingdom
- 8Exeter Collaboration for Academic Primary Care, University of Exeter, Exeter, United Kingdom
- 9Primary Care Research Centre, University of Southampton, Southampton, United Kingdom
- 10Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, United Kingdom
- 11Royal College of General Practitioners Research and Surveillance Centre, London, United Kingdom
Background: Burnout is associated with career disengagement among general practitioners (GPs), but the underlying mechanisms of this association remain poorly understood.
Objective: This study examined the pathways linking burnout to career disengagement factors among GPs.
Methods: An 11-item online questionnaire, including validated abbreviated measures of burnout outcomes (single items on emotional exhaustion (EE) and depersonalisation), career disengagement factors (intention to quit patient care, work–life balance, presenteeism and job satisfaction), and demographic information, was distributed to a random sample of GPs in England between December 2019 and April 2020. Correlations between burnout outcomes and disengagement factors were assessed, followed by a path analysis using a generalized structural equation model, to examine directional relationships between burnout outcomes and survey variables.
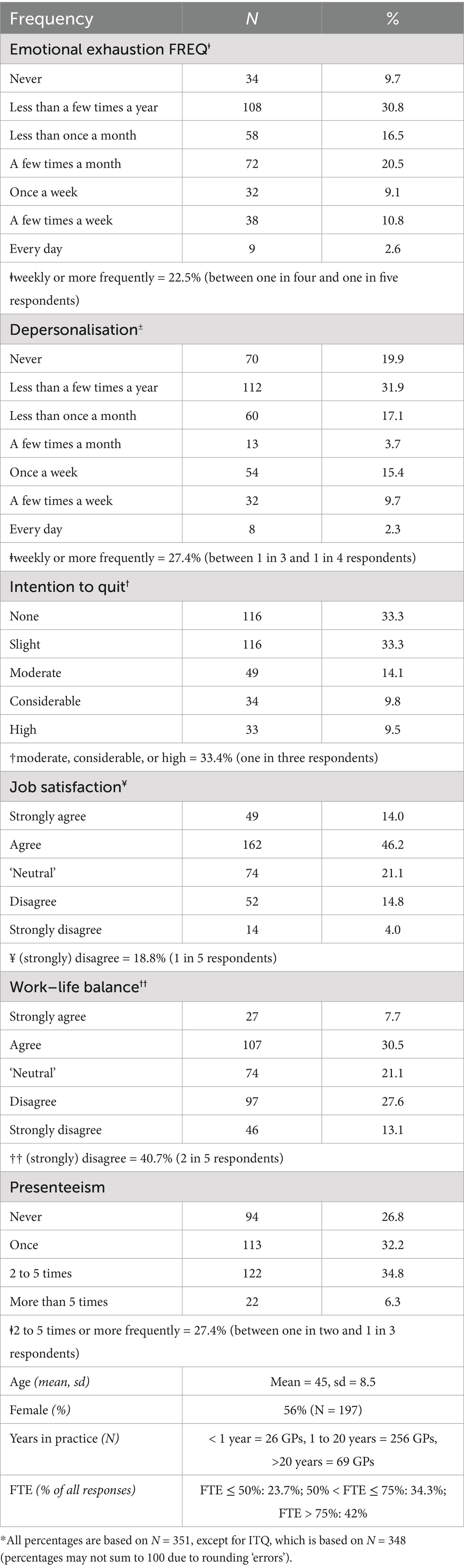
Results: A total of 351 GPs from 57 different medical practices completed the questionnaire. Up to one in four GPs (22.5%) experienced emotional exhaustion, while up to one in three (27.4%) experienced depersonalisation on a weekly basis. In addition, one in three GPs (33.3%) expressed a moderate-to-high intention to quit patient care within the next 5 years. Moreover, one in five GPs (18.8%) reported job dissatisfaction, two in five GPs (40.7%) indicated poor work–life balance, and up to one in two GPs (27.4%) reported presenteeism in the past year. In the path analysis, intention to quit patient care had significant direct associations with both job satisfaction and burnout and significant indirect associations (via burnout) with work–life balance and presenteeism. GP demographics were excluded from the path analysis because they exhibited very weak correlations with dimensions of burnout and work engagement factors.
Conclusion: These findings highlight the urgent need for interventions and policies aimed at addressing burnout and improving job satisfaction to retain GPs. In addition, improving work–life balance and reducing presenteeism could serve as effective early preventative measures to reduce burnout and job dissatisfaction and, in turn, retain GPs.
Introduction
There is substantial evidence, both internationally and within the United Kingdom (UK), indicating a workforce crisis in primary care (1, 2). More than half of general practitioners (GPs) have reported experiencing burnout symptoms, which has led many to disengage from practice by opting for part-time work, considering early retirement, or intending to quit medical practice (3–5). The Job Demands-Resources model offers a useful framework to understand how the imbalance between job demands (such as workload, emotional strain and poor work–life balance) and available resources (including job satisfaction) contributes to burnout and subsequent career disengagement (6). Common indicators of potential career disengagement, as outlined in recent frameworks (7), include low job satisfaction, presenteeism/absenteeism, poor work–life balance, and intention to quit patient care. However, intention to quit patient care was a strong indicator of actual turnover rates among healthcare professionals, including GPs (8, 9).
Research suggests that emotional exhaustion (EE), a dimension of burnout, is strongly associated with these career disengagement factors (5). International studies have demonstrated robust associations between burnout and career disengagement factors, such as job dissatisfaction, poor work–life balance, presenteeism, and turnover intention among healthcare workers (7, 10–13). For instance, low job satisfaction correlates with burnout in physicians, and those experiencing high burnout levels are more inclined to express the intention to quit patient care (10, 13, 14). However, formal path analyses that examine the strength and direction of these associations are scarce in the literature (15), particularly among GPs in UK general practices. Understanding these pathways is crucial for guiding policymakers in identifying the association between dimensions of burnout, career disengagement factors, and GP/practice factors that require urgent attention to improve GP retention rates (16).
In this study, a custom questionnaire was distributed to a random sample of GPs in England to investigate, through path analysis, the association between burnout (measured by emotional exhaustion and depersonalisation), demographic factors (age distribution, gender composition, time commitment, and years in practice), and career disengagement factors (including work–life balance, intention to quit patient care, presenteeism, and job satisfaction) among GPs.
Methods
Data collection
Study design and sample
This cross-sectional study was conducted in England based on responses from a GP questionnaire. The Royal College of General Practitioners (RCGP) Research and Surveillance Centre (RSC), which manages data collection and monitoring from over 2,000 general practices across England and Wales, facilitated the recruitment process for the research team between December 2019 and April 2020. The RCGP RSC sent invitation letters to practice managers at all practices in its network, inviting them to participate in an online survey hosted on the SurveyMonkey platform (17, 18).
The first 70 practices that volunteered were included in the study. The research team aimed to recruit approximately 350–400 GPs from these practices. The target number of GPs was determined based on available funding rather than a formal sample size calculation. Within each participating practice, deterministic sampling was employed in-house to mitigate potential selection bias. This approach assumes a random distribution based on discrete weighted samples and helps predict statistical moments that represent the properties of the overall distribution.
Questionnaire
The research team developed a cross-sectional questionnaire to examine burnout and career disengagement factors among GPs in England. The questionnaire consisted entirely of previously validated items (19–22).
The questionnaire comprised 11 items, including the following:
• A validated abbreviated scale from the Maslach Burnout Inventory (MBI), consisting of two items—emotional exhaustion and depersonalisation—was used. These items were measured on a 7-point ordinal scale (from never to every day), with higher scores indicating greater burnout. This abbreviated measure has been validated in many studies involving GPs and other clinicians (11, 23, 24). These two single items provide more meaningful insights into burnout among medical professionals compared to the full MBI (19). In addition, several studies have demonstrated that these two dimensions have the highest factor loadings in terms of their respective burnout domains (23, 25).
• Validated questions on intention to quit direct patient care, job satisfaction, work–life balance, and presenteeism (four items) were included. These items were sourced from previously published instruments that have been validated for their association with burnout (19–22).
• GP and practice characteristics such as age, gender, full-time equivalent (FTE), sum of FTE of all GPs in the practice and years worked in the practice (five items), were included.
The scales and items underwent discussion and agreed upon through consensus within the research group through patient and public involvement (PPI) and stakeholder engagement with GPs. The questionnaire is provided in Supplementary information S1. Completion of the questionnaire required 3–4 min. Participation in the questionnaire was voluntary, and written informed consent was obtained from all participants on the first page of the questionnaire. In December 2019, all general practice managers with valid email addresses received an email containing a link to the electronically administered questionnaire, which they were asked to circulate to GPs in their practices. All GPs, regardless of employment status (full-time, part-time, salaried, partners, or locums), were eligible to participate in the study. Non-respondents received reminders at 2-week and 4-week intervals, with data collection concluding in April 2020. The questionnaire link was personalized with a unique serial number but no personal identifiers. Participants who completed the questionnaire received a £20 payment reimbursement.
Statistical analyses
First, we summarized the age distribution, gender composition, time commitment, and years in practice of the respondents, along with the distribution of responses to key survey variables. Pairwise correlations between the two burnout dimensions and career disengagement factors were calculated using Kendall’s tau-b due to the ordinal nature of the data. To determine the presence of within-practice clustering in the responses to the survey questions, we calculated the intra-class correlation using a one-way ANOVA, which was calculated separately for all practices and for practices with at least two, three, five and seven responses. We used a multi-level ordered logistic regression to assess whether GP demographics had a discernible effect on career disengagement factors.
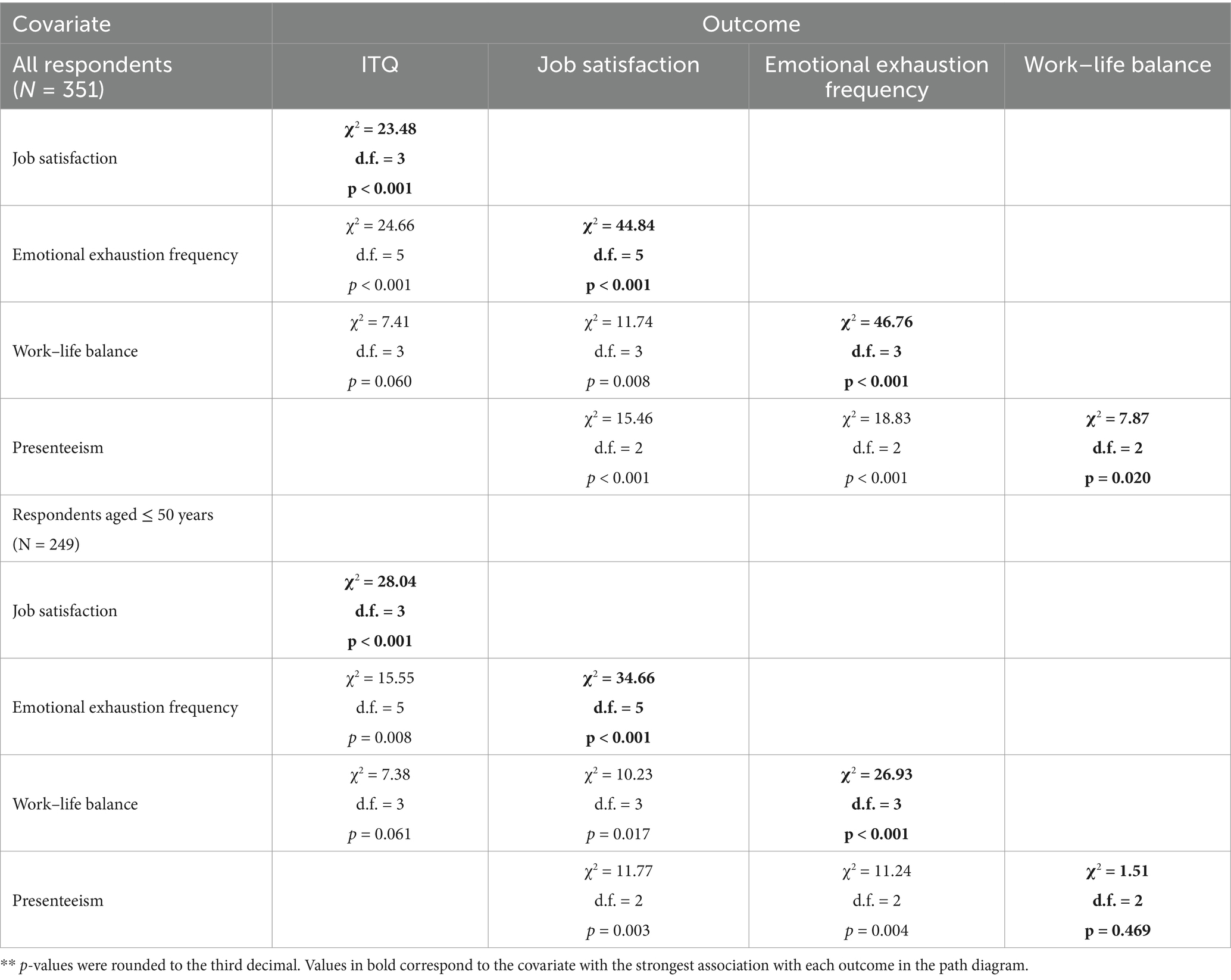
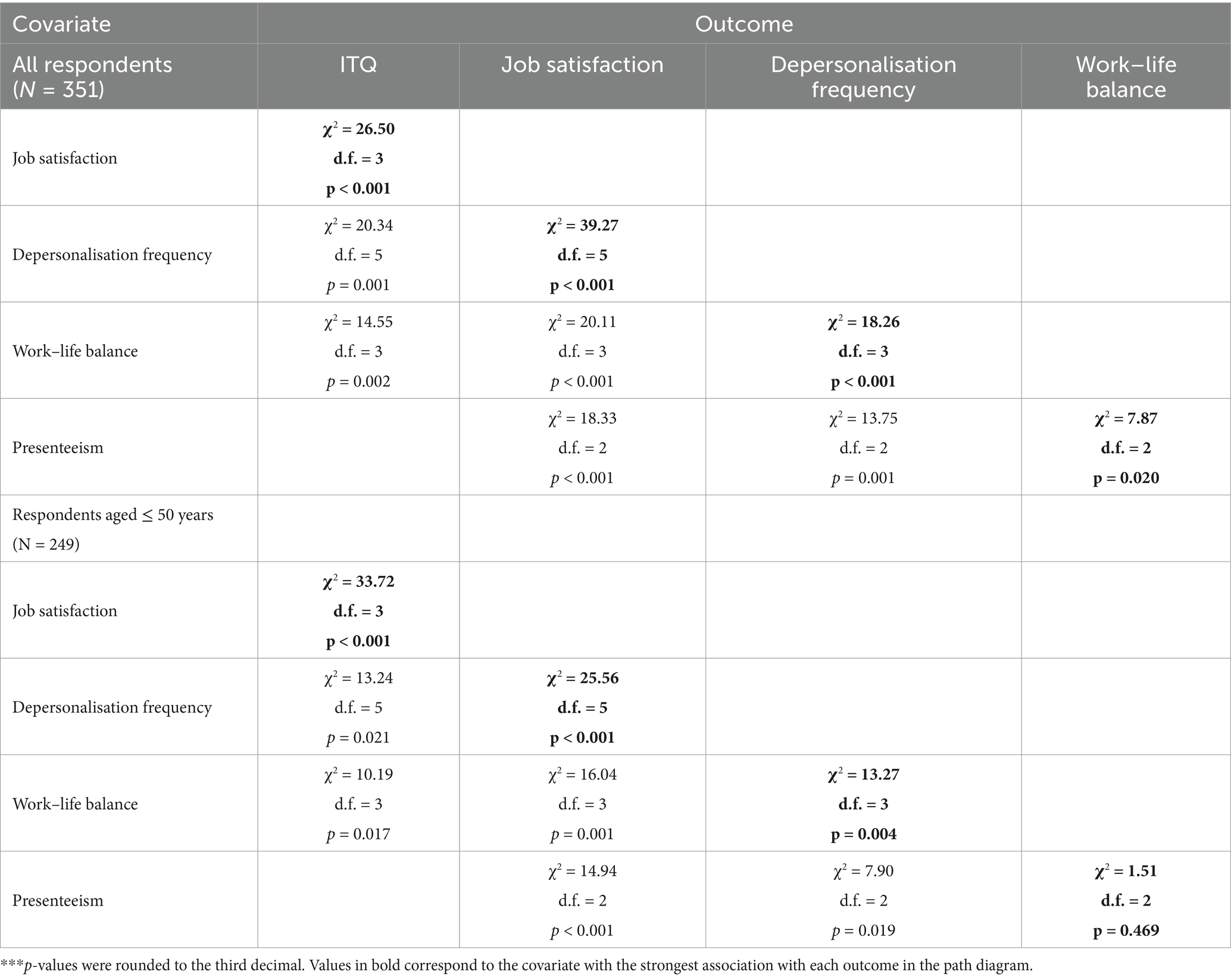
Next, we employed generalized structural equation modelling (GSEM) in Stata to examine pre-specified directional relationships between the survey variables, as depicted in the path diagram in Figure 1. Two models examining different burnout dimensions were utilized: one investigating the relationship between emotional exhaustion frequency and career disengagement factors and another exploring the relationship between depersonalisation frequency and career disengagement factors. As some of the variable scores were missing from the original survey, missing data were imputed using the R package ‘MICE: Multivariate Imputation by Chained Equations’ (26).
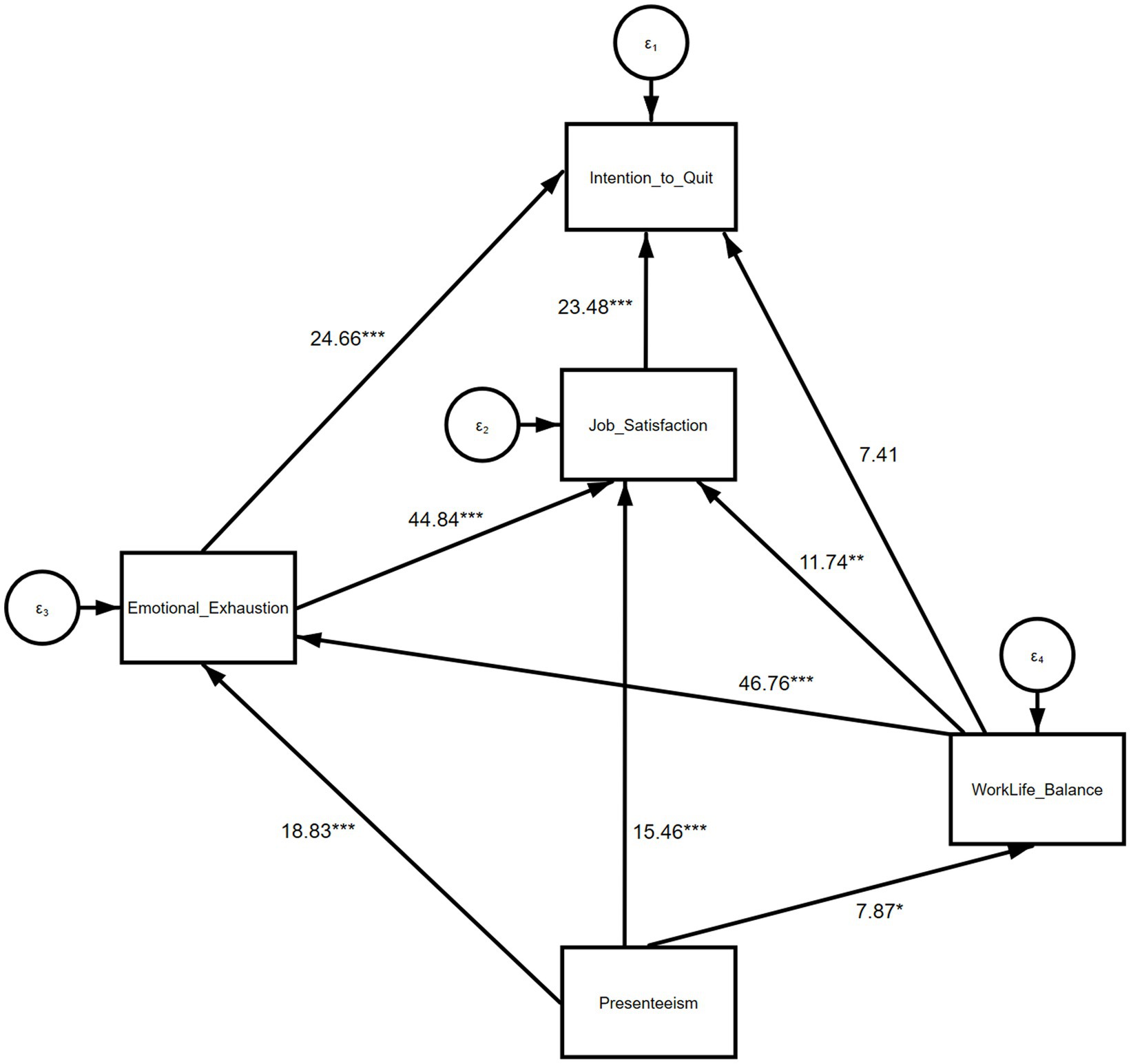
Figure 1. Structural model with emotional exhaustion frequency as the outcome†. †n = 351; values represent the chi-squared test for statistical significance, where **p ≤ 0.001, **p < 0.01, *p < 0.05.
GSEM enables the treatment of variables as ordinal within an ordered logistic regression; however, this approach entails estimating a large number of parameters. Model comparisons were based on log-likelihoods and available degrees of freedom, as conventional model-fit statistics are not applicable to GSEM. To streamline the model and prevent potential issues with convergence or estimation imprecision, GP demographic variables were omitted, as their inclusion could overly complicate the model (27). Due to the large number of estimated parameters, we performed chi-squared tests to assess the statistical significance of the associations between the response items and used p-values to identify the strongest associations of interest.
Furthermore, we considered models for the subset of GPs aged 50 years or younger, as this group was presumed to be less likely to express a desire to quit general practice due to retirement, potentially making them more inclined to report wanting to quit due to job-related factors. This approach allowed us to better focus on GPs whose intention to quit patient care were more likely to be related to job factors, such as burnout or work dissatisfaction.
Results
A total of 351 GPs from 57 general practices completed the bespoke questionnaire. The questionnaire was distributed to 67 practices, but 10 (15%) practices were excluded as only one GP registrar responded from these practices, and they were consulting at multiple locations, making it impossible to assign them a unique practice ID. The median response rate of the GPs across the 57 practices was 39% (range 12–91%). The average age of the participants was 45 years (SD = 8.5, range = 28 to 70), with 56% (196 out of 351) being female. Regarding work experience, 7.4% (26 GPs) had been in practice for less than 1 year, 73% (256 GPs) for 1 to 20 years, and 19.7% (69 GPs) for more than 20 years. Data analysis was based on 351 responses, except for the analysis that involved the intention to quit, which included 348 responses. The results are presented in Table 1, which indicated that between one in four (25%) and one in five (20%) GP participants reported feeling emotionally exhausted on a weekly basis, while between one in three (33%) and one in four (25%) GPs reported feeling callous toward other people at least once a week. Regarding career disengagement factors, one in three (33%) participants indicated having at least a moderate intention to quit direct patient care in the next 5 years, and one in five (20%) participants reported dissatisfaction with their career in general practice. In terms of work–life balance, two in five (40%) respondents indicated that their work schedule did not afford them enough time for personal/family life, and between one in two (50%) and one in three (33%) reported working while ill (presenteeism) at least 2–5 times over the last 12 months. We observed weak to moderate correlations between the key variables of interest (Supplementary Table S2) and very low intra-class correlation coefficients for the items in all four categories (i.e., all practices and practices with more than two, three, five or seven employed GPs) (Supplementary Table S3). The results from the multi-level ordered logistic regression exploring the effects of GP demographics on career disengagement factors indicated no statistically significant associations, as presented in Supplementary Table S1.
Path relationship between job satisfaction, burnout, and other career disengagement factors
The GSEM routine employed in our analysis does not enable reporting the usual indices of model fit. Instead, we present the final adjusted GSEM results, including the values of the chi-squared test for statistical significance, in Figure 1 (emotional exhaustion and career disengagement factors) and 2 (depersonalisation and career disengagement factors), as well as in Tables 2, 3. Due to the ordinal nature of the response variables, we focused on p-values and statistical significance to assess the overall association between any pair of variables, rather than the standardized path coefficients. All direct paths in the model (Figures 1, 2) demonstrated a significant association, except for the one between work–life balance and presenteeism in the model for GPs aged 50 or younger. Therefore, we focused on the strongest associations for each outcome, corresponding to the variable immediately below the outcome in the ‘hierarchy of prediction’ (Tables 2, 3).
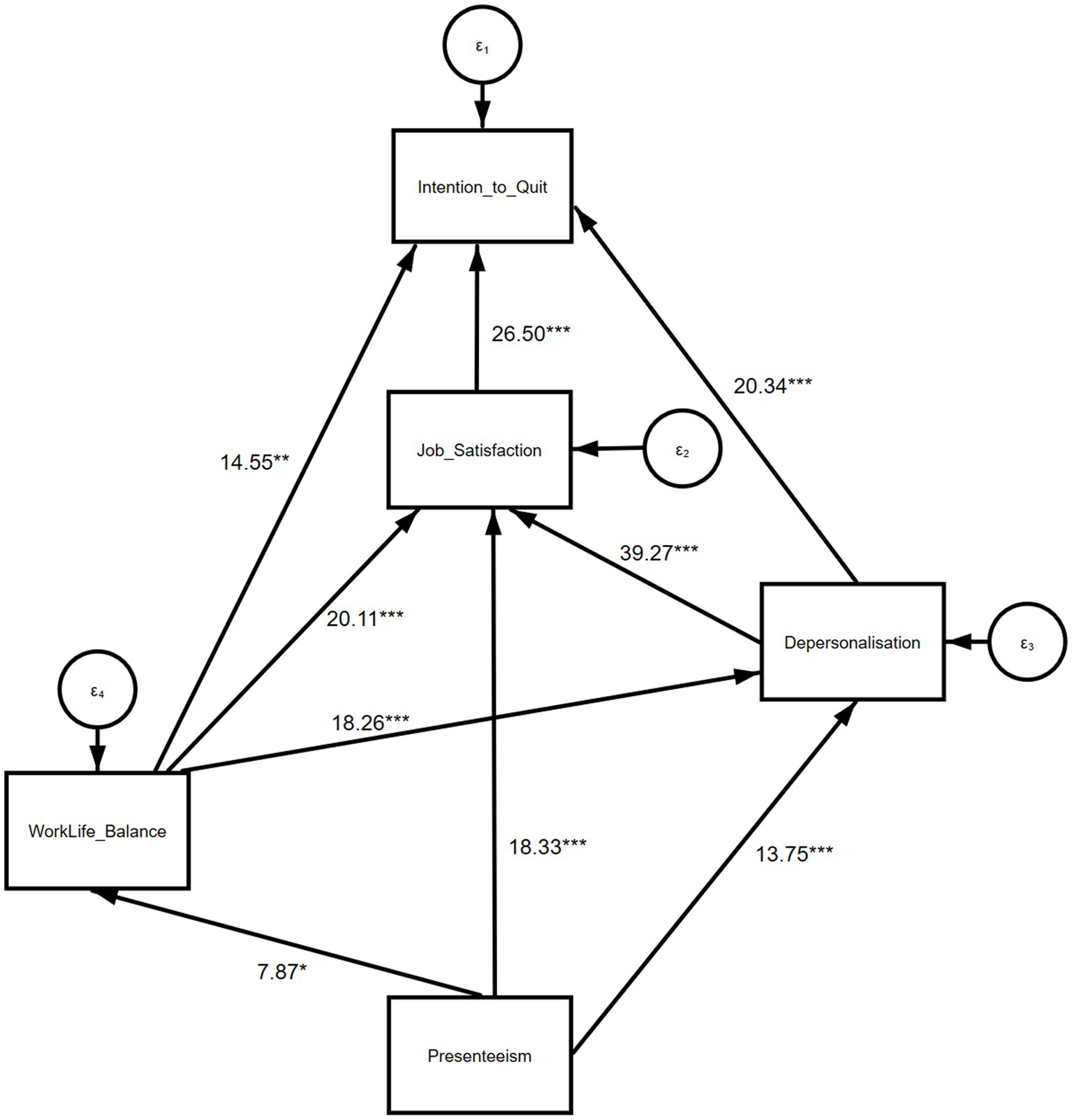
Figure 2. Structural model with depersonalisation frequency as the outcome††. ††n = 351; values represent the chi-squared test for statistical significance, where **p ≤ 0.001, **p < 0.01, *p < 0.05.
In the first model exploring the path relationship between emotional exhaustion and career disengagement factors (Figure 1), intention to quit patient care had the strongest association with job satisfaction (χ2 = 23.48, p < 0.001, df = 3), followed by emotional exhaustion (χ2 = 24.66, p < 0.001, df = 5). The association between the intention to quit patient care and work–life balance was weaker (χ2 = 7.41, p = 0.060, df = 3). Job satisfaction showed the strongest association with emotional exhaustion (χ2 = 44.84, p < 0.001, df = 5), but it was also significantly associated with work–life balance (χ2 = 11.74, p = 0.008, df = 3) and presenteeism (χ2 = 15.46, p < 0.001, df = 2). For emotional exhaustion, the strongest association was observed with work–life balance (χ2 = 46.76, p < 0.001, df = 3), followed by presenteeism (χ2 = 18.83, p < 0.001, df = 2), and for work–life balance, the strongest association was observed with presenteeism (χ2 = 23.48, p < 0.001, df = 2).
In the second model exploring the path relationship between depersonalisation and career disengagement factors (Figure 2), intention to quit patient care had the strongest association with job satisfaction (χ2 = 26.50, p < 0.001, df = 3), followed by depersonalisation (χ2 = 20.34, p = 0.001, df = 5) and work–life balance (χ2 = 14.55, p = 0.002, df = 3). We observed the strongest association between job satisfaction and depersonalisation (χ2 = 39.27, p < 0.001, df = 5). The associations between work–life balance (χ2 = 20.11, p < 0.001, df = 3) and presenteeism (χ2 = 18.33, p < 0.001, df = 2) were also strong, although comparatively weaker. For depersonalisation, the strongest association was observed with work–life balance (χ2 = 18.26, p < 0.001, df = 3), followed by presenteeism (χ2 = 13.75, p = 0.001, df = 2). Similar associations were found across the two models for the subgroup of GPs aged 50 or younger.
Discussion
Summary of the findings
Our study outlines a pathway that identifies a spectrum of associations, ranging from the most direct and immediate to the most indirect and distant, between burnout and career disengagement factors among GPs in England. We found that job satisfaction and the two dimensions of burnout (emotional exhaustion and depersonalisation) were the only direct and immediate factors associated with intention to quit patient care, which is considered the most proximal indicator of career disengagement. Other common career disengagement factors, such as work–life balance and presenteeism, were primarily associated with the intention to quit patient care indirectly through burnout. In addition, the demographic characteristics of GPs did not contribute to this pathway beyond career disengagement factors and burnout dimensions.
Strengths and limitations of the study
Our study employed advanced statistical techniques to explore the complex associations between burnout dimensions and career disengagement factors among GPs in England. However, several limitations should be noted. First, the cross-sectional study design precludes the establishment of causation, emphasising the need for future studies employing longitudinal data. Second, the response rate across practices was low (39%), although the rate is higher than that in most studies involving GP respondents (28, 29) and substantially higher than that in the UK’s Tenth National GP Work-life Survey in 2019 (30). For example, a large cross-sectional survey of burnout among physicians in the US (31) reported a response rate of approximately 20%, whereas the GP Work-life Survey had a cross-sectional response rate of 12% in 2019. However, we cannot rule out the possibility that our findings reflect only the perspectives of the participating GPs, rather than those of all practising GPs across the UK. Third, although the survey used validated items, the potential risk of selection and/or recall bias cannot be ruled out, especially if responding GPs had already been experiencing emotional exhaustion or depersonalisation in the preceding 12 months. While the demographic characteristics of the respondents broadly align with national statistics for GPs, the voluntary nature of the survey might have introduced selection bias. Therefore, caution should be exercised when generalising the findings to the wider GP workforce in England. Furthermore, the survey was distributed during the very early stages of the COVID-19 pandemic, which might have introduced unique stressors that influenced the GPs’ responses, particularly regarding burnout, disengagement, and intention to quit patient care (32). However, as major disruptions had not yet fully materialised during most of the data collection period, the early pandemic context should be considered when interpreting the results. Fourth, the distribution of the questionnaires at the onset of the COVID-19 pandemic might have influenced the responses due to increased workload pressures. Fifth, we used a two-item abbreviated measure of burnout to shorten the survey and reduce the risk of dropout. This measure has demonstrated excellent value in capturing overall burnout as well as emotional exhaustion and depersonalization dimensions of burnout in physicians. However, this measure did not include the personal accomplishment dimension of the MBI, and there might be additional benefits to including this dimension, especially when examining paths to positive outcomes such as fulfilment and motivation. We recommend replicating these findings using the full MBI measure. Moreover, we acknowledge that practice-and country-level factors, such as healthcare policies and organisational culture and teamwork (33), were not accounted for and might have influenced levels of burnout and career disengagement. Future research should incorporate these potential confounders for a more comprehensive understanding of the tested relationships.
Comparison with existing literature
Work stress and burnout in doctors are often associated with suboptimal patient safety (7, 14, 34) and career disengagement (14). However, little is known about the mechanisms underlying the association between burnout and career disengagement. Our findings support the Job Demands-Resources model by demonstrating that high levels of burnout (emotional exhaustion and depersonalisation) directly contribute to the intention to quit patient care, a critical indicator of career disengagement. The above model suggests that job demands, such as excessive workload and poor work–life balance, act as stressors that lead to burnout, which, in turn, exacerbates disengagement from patient care. Our study reinforces this finding by demonstrating that burnout is strongly associated with job dissatisfaction, which is the most direct factor linked to quitting intention.
In the UK, the primary care workforce has been severely affected by prolonged staff shortages, funding shortfalls, and poor planning (35). Recent studies have revealed an increasing number of doctors retiring or leaving direct patient care early in their careers (36). In addition, working during the COVID-19 pandemic has also increased burnout levels among GPs (37). Burnout and job satisfaction are known drivers of the intention to quit patient care among GPs (5, 15, 38). This study advances these findings by offering a potential pathway through which burnout dimensions and career disengagement factors intercorrelate among GPs. Our findings suggest that GP retention may be at immediate risk when burnout and job dissatisfaction are high, while poor work–life balance and presenteeism may serve as opportunities for early intervention to improve GP retention.
Job satisfaction is typically defined as an individual’s perceptions and evaluation of their job, and these perceptions are influenced by the demands, values and expectations associated with their job (15). We propose that GPs with higher job satisfaction are more enthusiastic about work and derive greater utility from role-related tasks, which, in turn, is likely to reduce their intention to quit. There is also evidence that burnout is driven by working conditions, such as excessive demands, toxic cultures, and poor working environments (18, 39, 40). GPs have one of the highest rates of poor work–life balance among medical professionals (41), likely influencing their decisions to reduce working hours and retire early in their careers (42, 43). Doctors may also have a higher threshold for recognising illness in themselves, often reserving sick leave for when their dependents are unwell (44). Building on these findings, we demonstrated that work–life balance and presenteeism have an indirect effect on the intention to quit patient care via emotional exhaustion and depersonalisation dimensions of burnout (45, 46). Some studies have suggested that perceived social support in the workplace is associated with lower levels of sickness presenteeism (47). It may be that interventions aimed at reshaping doctors’ attitudes toward work–life balance and sickness will have a positive impact on GP well-being and retention (48). Investing in such organisational changes is recommended by our findings.
Implications for research and practice
Job dissatisfaction and burnout are likely immediate indicators that GPs are at high risk of quitting direct patient care. High levels of burnout and job dissatisfaction may require urgent action to improve GP retention. Strategies such as fair compensation, professional development, and a supportive work environment could enhance job satisfaction. In addition, providing sufficient organisational support, including time and resources to implement stress management programmes and mental health support, can potentially reduce burnout and help retain GPs.
Poor work–life balance and presenteeism may serve as early indicators of the intention to quit, as they are associated with burnout and job dissatisfaction. Preventative measures, such as offering flexible working hours and fostering a supportive culture that encourages taking sick leave without stigma, can serve as early interventions to improve work–life balance and reduce presenteeism.
Interestingly, demographic factors of GPs do not significantly contribute to the path toward career disengagement. Therefore, efforts should focus on addressing work stress and the workplace environment.
Extending this pathway to include work culture and practice-level characteristics, as well as adopting a longitudinal approach with a larger sample of GPs and practices, is recommended. This finding would provide insights into how burnout, work culture, and other practice-specific characteristics influence self-reported intentions to quit patient care and actual career disengagement in GPs. These insights would also enable causal mechanisms to be established and subsequently to be more targeted and comprehensive interventions to enhance GP retention.
Data availability statement
The datasets presented in this article are not readily available because this study used pseudonymised patient-level data from the Oxford-Royal College of General Practitioner Research and Surveillance Centre (RSC). These data can be accessed for ethically approved research by applying via https://orchid.phc.ox.ac.uk/.
Ethics statement
The studies involving humans were approved by the project was reviewed by the University of Manchester’s research ethics committee before approval (IRAS ID: 268533). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CG: Project administration, Supervision, Writing – original draft, Writing – review & editing. MH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. AH: Conceptualization, Investigation, Methodology, Writing – review & editing. SZ: Investigation, Writing – review & editing. EK: Funding acquisition, Investigation, Writing – review & editing. DA: Funding acquisition, Investigation, Writing – review & editing. CC-G: Funding acquisition, Investigation, Writing – review & editing. RP: Funding acquisition, Investigation, Writing – review & editing. PL: Funding acquisition, Investigation, Writing – review & editing. SL: Funding acquisition, Investigation, Writing – review & editing. AZ: Funding acquisition, Investigation, Writing – review & editing. AE: Funding acquisition, Investigation, Writing – review & editing. MP: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study/project is funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research (project reference 411) and the National Institute for Health and Care Research Greater Manchester Patient Safety Research Collaboration (NIHR GM PSRC) (award number: NIHR204295). AH is funded by his NIHR fellowship. CCG is part funded by the NIHR WM ARC. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Conflict of interest
SL has received funding through his University from Astra-Zeneca, Ei-Lilly, GSK, Moderna, MSD, NovoNordisk, Sanofi, and Seqirus and has been a member of advisory boards for Astra-Zeneca, Sanofi, and Seqirus. SL is Director of the Oxford-RCGP RSC. DMA reports receiving research grants from AbbVie, Almirall, Celgene, Eli Lilly, Janssen, Novartis, UCB, and the Leo Foundation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1547102/full#supplementary-material
References
2. World Health Organisation. A Universal Truth No health without a workforce. Geneva: World Health Organisation (2013).
3. Royal College of General Practitioners. Fit for the future: retaining the GP workforce. Royal College of General Practitioners. (2022).
4. Owen, K, Hopkins, T, Shortland, T, and Dale, J. GP retention in the UK: a worsening crisis. Findings from a cross-sectional survey. BMJ Open. (2019) 9:e026048. doi: 10.1136/bmjopen-2018-026048
5. Scanlan, JN, and Still, M. Relationships between burnout, turnover intention, job satisfaction, job demands and job resources for mental health personnel in an Australian mental health service. BMC Health Serv Res. (2019) 19:62. doi: 10.1186/s12913-018-3841-z
6. Demerouti, E, Bakker, AB, Nachreiner, F, and Schaufeli, WB. The job demands-resources model of burnout. J Appl Psychol. (2001) 86:499–512. doi: 10.1037/0021-9010.86.3.499
7. Hodkinson, A, Zhou, A, Johnson, J, Geraghty, K, Riley, R, Zhou, A, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. (2022) 378:e070442. doi: 10.1136/bmj-2022-070442
8. Ki, J, and Choi-Kwon, S. Health problems, turnover intention, and actual turnover among shift work female nurses: Analyzing data from a prospective longitudinal study. PLoS One. (2022) 17:e0270958. doi: 10.1371/journal.pone.0270958
9. Hann, M, Reeves, D, and Sibbald, B. Relationships between job satisfaction, intentions to leave family practice and actually leaving among family physicians in England. Eur J Pub Health. (2011) 21:499–503. doi: 10.1093/eurpub/ckq005
10. Wang, H, Jin, Y, Wang, D, Zhao, S, Sang, X, and Yuan, B. Job satisfaction, burnout, and turnover intention among primary care providers in rural China: results from structural equation modeling. BMC Fam Pract. (2020) 21:1–10. doi: 10.1186/s12875-020-1083-8
11. Dyrbye, LN, West, CP, and Shanafelt, TD. Defining burnout as a dichotomous variable. J Gen Intern Med. (2009) 24:440. doi: 10.1007/s11606-008-0876-6
12. Willard-Grace, R, Knox, M, Huang, B, Hammer, H, Kivlahan, C, and Grumbach, K. Burnout and health care workforce turnover. Ann Fam Med. (2019) 17:36–41. doi: 10.1370/afm.2338
13. Shanafelt, TD, Hasan, O, Dyrbye, LN, Sinsky, C, Satele, D, Sloan, J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. (2015) 90:1600–13. doi: 10.1016/j.mayocp.2015.08.023
14. Shanafelt, TD, Balch, CM, Bechamps, G, Russell, T, Dyrbye, L, Satele, D, et al. Burnout and medical errors among American surgeons. Ann Surg. (2010) 251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3
15. Zhang, T, Feng, J, Jiang, H, Shen, X, Pu, B, and Gan, Y. Association of professional identity, job satisfaction and burnout with turnover intention among general practitioners in China: evidence from a national survey. BMC Health Serv Res. (2021) 21:1–11. doi: 10.1186/s12913-021-06322-6
16. Chilvers, R, Richards, SH, Fletcher, E, Aylward, A, Dean, S, Salisbury, C, et al. Identifying policies and strategies for general practitioner retention in direct patient care in the United Kingdom: a RAND/UCLA appropriateness method panel study. BMC Fam Pract. (2019) 20:1–12. doi: 10.1186/s12875-019-1020-x
17. Survey Monkey. (2022) Available online at: https://www.surveymonkey.co.uk/ (Accessed May 3, 2022).
18. Liu, W, Zhao, S, Shi, L, Zhang, Z, Liu, X, Li, L, et al. Workplace violence, job satisfaction, burnout, perceived organisational support and their effects on turnover intention among Chinese nurses in tertiary hospitals: a cross-sectional study. BMJ Open. (2018) 8:e019525. doi: 10.1136/bmjopen-2017-019525
19. West, CP, Dyrbye, LN, Sloan, JA, and Shanafelt, TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. (2009) 24:1318–21. doi: 10.1007/s11606-009-1129-z
20. Thun, S, Fridner, A, Minucci, D, and Løvseth, LT. Sickness present with signs of burnout: the relationship between burnout and sickness presenteeism among university hospital physicians in four European countries. Scand Psychol. (2014) 1:1. doi: 10.15714/scandpsychol.1.e5
21. Shanafelt, TD, Boone, S, Tan, L, Dyrbye, LN, Sotile, W, Satele, D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Aarch Int Med. (2012) 172:1377–85. doi: 10.1001/archinternmed.2012.3199
22. Neumann, JL, Mau, L-W, Virani, S, Denzen, EM, Boyle, DA, Boyle, NJ, et al. Burnout, moral distress, work–life balance, and career satisfaction among hematopoietic cell transplantation professionals. Biol Blood Marrow Transplant. (2018) 24:849–60. doi: 10.1016/j.bbmt.2017.11.015
23. Maslach, C, Jackson, S, and Leiter, M. The Maslach Burnout Inventory Manual In: CP Zalaquett and RJ Wood, editors. Evaluating Stress: A Book of Resources : The Scarecrow Press (1997). 191–218.
24. West, CP, Dyrbye, LN, Satele, DV, Sloan, JA, and Shanafelt, TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445–52. doi: 10.1007/s11606-012-2015-7
25. Vanheule, S, Rosseel, Y, and Vlerick, P. The factorial validity and measurement invariance of the Maslach burnout inventory for human services. Stress Health. (2007) 23:87–91. doi: 10.1002/smi.1124
26. Van Buuren, S, and Groothuis-Oudshoorn, K. Mice: multivariate imputation by chained equations in R. J Stat Softw. (2011) 45:1–67. doi: 10.18637/jss.v045.i03
27. Deng, L, Yang, M, and Marcoulides, KM. Structural equation modeling with many variables: a systematic review of issues and developments. Front Psychol. (2018) 9:580. doi: 10.3389/fpsyg.2018.00580
28. Bonevski, B, Magin, P, Horton, G, Foster, M, and Girgis, A. Response rates in GP surveys: trialling two recruitment strategies. Aust Fam Physician. (2011) 40:427–30.
29. Creavin, ST, Creavin, AL, and Mallen, CD. Do GPs respond to postal questionnaire surveys? A comprehensive review of primary care literature. Fam Pract. (2011) 28:461–7. doi: 10.1093/fampra/cmr001
30. Sutton, M, Checkland, K, Gibson, J, Moss, C, Spooner, S, and Walker, B. (2019). ‘Tenth national GP worklife survey 2019’. PruComm website. Available at: https://prucomm.ac.uk/projects/current-projects/tenth-gp-worklife-survey.html (Accessed December 10, 2023).
31. Tawfik, DS, Profit, J, Morgenthaler, TI, Satele, DV, Sinsky, CA, Dyrbye, LN, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. (2018) 93:1571–80. doi: 10.1016/j.mayocp.2018.05.014
32. Zhou, AY, Hann, M, Panagioti, M, Patel, M, Agius, R, Van Tongeren, M, et al. Cross-sectional study exploring the association between stressors and burnout in junior doctors during the COVID-19 pandemic in the United Kingdom. J Occup Health. (2022) 64:e12311. doi: 10.1002/1348-9585.12311
33. Williams, P, Jones, B, Aspen, C, Bird, T, Smylie, J, Touray, M, et al. Team climate, job satsfaction and burnout: results from a national survey of staff in general practice in England. Br J Gen Pract. (2024) 74:bjgp24X737877. doi: 10.3399/bjgp24X737877
34. Hodkinson, A, Zghebi, SS, Kontopantelis, E, Grigoroglou, C, Ashcroft, DM, Hann, M, et al. Association of strong opioids and antibiotics prescribing with GP burnout: a retrospective cross-sectional study. Br J Gen Pract. (2023) 73:e634–43. doi: 10.3399/BJGP.2022.0394
35. Beech, J, Bottery, S, Charlesworth, A, Evans, H, Gershlick, B, Hemmings, N, et al. Closing the gap. London: The Nuffield Trus (2019).
36. Sizmur, S, and Raleigh, V. The risks to care quality and staff wellbeing of an NHS system under pressure. The King's Fund. (2018):24.
37. Abdelhafiz, AS, Ali, A, Ziady, HH, Maaly, AM, Alorabi, M, and Sultan, EA. Prevalence, associated factors, and consequences of burnout among Egyptian physicians during COVID-19 pandemic. Front Pub Health. (2020) 8:590190. doi: 10.3389/fpubh.2020.590190
38. Angerer, P, Li, J, and Degen, C. Physicians’ intention to leave direct patient care: an integrative review. Hum Resour. Health. (2015) 13:74. doi: 10.1186/s12960-015-0068-5
39. Rothenberger, D. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. (2017) 60:567–76. doi: 10.1097/DCR.0000000000000844
40. Zhou, AY, Panagioti, M, Esmail, A, Agius, R, Van Tongeren, M, and Bower, P. Factors associated with burnout and stress in trainee physicians: a systematic review and meta-analysis. JAMA Netw Open. (2020) 3:e2013761-e. doi: 10.1001/jamanetworkopen.2020.13761
41. Shanafelt, TD, West, CP, Sinsky, C, Trockel, M, Tutty, M, Satele, DV, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. (2019) 94:1681–94. doi: 10.1016/j.mayocp.2018.10.023
42. Lown, M, Lewith, G, Simon, C, and Peters, D. Resilience: what is it, why do we need it, and can it help us? Br J Gen Pract. (2015) 65:e708–10. doi: 10.3399/bjgp15X687133
43. Sansom, A, Terry, R, Fletcher, E, Salisbury, C, Long, L, Richards, SH, et al. Why do GPs leave direct patient care and what might help to retain them? A qualitative study of GPs in south West England. BMJ Open. (2018) 8:e019849. doi: 10.1136/bmjopen-2017-019849
44. Chambers, C, Frampton, C, and Barclay, M. Presenteeism in the New Zealand senior medical workforce-a mixed-methods analysis. New Zeal Med J. (2017) 130:10–21.
45. Lui, JNM, Andres, EB, and Johnston, JM. Presenteeism exposures and outcomes amongst hospital doctors and nurses: a systematic review. BMC Health Serv Res. (2018) 18:985. doi: 10.1186/s12913-018-3789-z
46. Pit, SW, and Hansen, V. The relationship between lifestyle, occupational health, and work-related factors with presenteeism amongst general practitioners. Arch Environ Occup Health. (2016) 71:49–56. doi: 10.1080/19338244.2014.998329
47. Xi, X, Lu, Q, Lu, M, Xu, A, Hu, H, and Ung, COL. Evaluation of the association between presenteeism and perceived availability of social support among hospital doctors in Zhejiang, China. BMC Health Serv Res. (2020) 20:609. doi: 10.1186/s12913-020-05438-5
Keywords: burnout, general practice, workforce, structural equation modelling, well-being
Citation: Grigoroglou C, Hann M, Hodkinson A, Zghebi SS, Kontopantelis E, Ashcroft DM, Chew-Graham CA, Payne RA, Little P, de Lusignan S, Zhou AY, Esmail A and Panagioti M (2025) Associations between burnout and career disengagement factors among general practitioners: a path analysis. Front. Public Health. 13:1547102. doi: 10.3389/fpubh.2025.1547102
Edited by:
Niccolo Persiani, University of Florence, ItalyReviewed by:
Ognjen Brborovic, University of Zagreb, CroatiaJiří Vévoda, Palacký University Olomouc, Czechia
Copyright © 2025 Grigoroglou, Hann, Hodkinson, Zghebi, Kontopantelis, Ashcroft, Chew-Graham, Payne, Little, de Lusignan, Zhou, Esmail and Panagioti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christos Grigoroglou, Q2hyaXN0b3MuZ3JpZ29yb2dsb3VAbWFuY2hlc3Rlci5hYy51aw==
 Christos Grigoroglou
Christos Grigoroglou Mark Hann
Mark Hann Alexander Hodkinson
Alexander Hodkinson Salwa S. Zghebi1
Salwa S. Zghebi1 Carolyn A. Chew-Graham
Carolyn A. Chew-Graham Simon de Lusignan
Simon de Lusignan Anli Yue Zhou
Anli Yue Zhou Maria Panagioti
Maria Panagioti