- 1Department of Internal Medicine, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates
- 2Department of Anesthesiology, Hospital Clínic de Barcelona, Universitat de Barcelona, Barcelona, Spain
- 3Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain
- 4Centro de Investigación Biomédica en Red Salud Mental (CIBERSAM), Madrid, Spain
- 5Donation and Transplantation Institute, Barcelona, Spain
Introduction: Organ transplantation is a vital treatment for end-stage organ failure. However, the shortage of available organs remains a significant challenge worldwide. This study aimed to explore university students’ willingness to donate organs, including their views on brain death, in the United Arab Emirates (UAE).
Methods: The study is cross-sectional survey on the respondents’ knowledge of, attitudes toward, and perceived barriers to and facilitators of organ donation. A total of 521 students completed the survey. Chi-square tests and logistic regression models were used to identify the factors associated with their willingness to donate their organs after death.
Results: Most of the respondents (69%) were willing to donate their organs after death, and 79% were willing to donate their organs to a loved one during their lifetime. However, only 42.8% accepted brain death as equivalent to death. The most reported reasons behind the respondents’ willingness to donate organs were the belief that it is something everyone should do (adjusted odds ratio [aOR]: 4.68) and a responsibility to help loved ones (aOR: 2.63). Meanwhile, the significant barriers to organ donation included a preference for whole-body burial (aOR: 0.079), religious objections (aOR: 0.195), and family objections (aOR: 0.326).
Discussion: University students in the UAE show a positive attitude toward organ donation. However, significant barriers, including family and religious objections, remain to be addressed. Increasing public awareness about brain death and establishing mechanisms for securing family consent in advance are crucial steps for the successful implementation of a deceased organ donation program in the UAE.
Introduction
Organ transplantation is vital for end-stage organ failure, but rising demand has caused an organ shortage and growing waiting lists (1). In 2021, the Global Observatory on Donation and Transplantation reported organ availability at less than 10% of global demand, with most donations from deceased donors (2). In the UAE, deceased organ donation remains low despite an increasing number of patients awaiting kidney transplants (2–4).
Given the severe shortage of organs for donation in the country, a federal decree (5/2016) has been issued for the regulation of human organ transplantation. In 2017, the Ministry of Health and Prevention issued the first decree, defining the diagnostic criteria, rules, and procedures regulating the determination of death based on neurological criteria and subsequently updated it in 2022 (5). A recent systematic review reported that in the Middle East, up to half of the studied population were willing to donate their organs. However, the respondents’ knowledge regarding organ donation and their willingness to donate organs varied widely between studies (6). Another recent survey of residents in the UAE found that only 36% of the participants were aware that organ donation after death is allowed legally in UAE (7). Furthermore, there is limited information regarding the barriers and facilitators of organ donation among UAE residents.
As in most Arab and Eastern countries, health-related decisions in the UAE are shared family affairs; in many instances, family members provide social and supportive care for their sick family member (8). Moreover, people’s ideas and beliefs regarding illness; disease treatment; and the holiness of the human body, life, and death affect their decision-making and consent regarding donation after death (9–11).
In Eastern culture, death is an ominous matter; previous studies have highlighted that the fear of dehumanizing the body’s dignity, and the fear of the unknown prevents people from signing up for organ donation (11, 12). They also highlighted the importance of obtaining family members’ approval in signing up for organ donation. Moreover, a higher level of education and social media exposure could increase awareness and the willingness to donate organs (11, 13). Individuals with higher levels of education are more likely to perceive organ donation as a humane and noble act and are thus more likely to sign up for organ donation after death (14–19). Since the Federal Decree-Law No. 5 of 2016 on Regulation of Human Organs and Tissue Transplantation allowing and regulating organ transplantation between live and deceased donors was implemented in 2016, more than 110 deceased patients in the UAE have donated their organs. However, most of the donors were non-citizens and therefore number of donors among citizens remains low (2–4). Therefore, this study aimed to explore the willingness of university students in the UAE to donate their organs after death, including their views on brain death. We hypothesized that inadequate knowledge about donations processes, death by neurological criteria and unfavorable attitudes toward deceased donation may explain the low donation rates. Understanding the contextual factors that affect the deceased organ donation program will help in tailoring the awareness program to address family concerns about deceased organ donation. It will also guide policymakers in developing a contextual holistic approach to decrease the wastage of potential organs due to delay in consent and the counseling process.
Materials and methods
The UAE is a confederation of seven emirates. The population is multiethnic, with the majority (85%) being expatriate temporary workers (20). This study was conducted at UAE University because it is a federal public university that enrolls more than 13,000 students from all seven emirates (Figure 1). The study was approved by the Social Sciences Research Ethics Committee of UAE University (ERS_2018_5842).

Figure 1. Distribution of the population, UAE University students, and study respondents across the UAE.
A self-administered questionnaire was designed based on previous studies (21–23) and comprised three parts: (1) participants’ demographics and socioeconomic status; (2) their knowledge, attitude, and willingness to donate organs after brain death; and (3) the perceived barriers and facilitators for deceased organ donation.
The questionnaire was reviewed by three experts to assess the face validity of the survey items and to provide feedback regarding the clarity and conciseness of the questions. The ambiguous issues were corrected and then a pilot test was conducted using a test group of university students (n = 10). No problems were identified in the pilot study; therefore, no further changes were made to the questionnaire. The questionnaire was then posted online using Research Electronic Data Capture (REDCap), a secure web-based application that allows respondents to answer questions while preventing duplicate responses. Additionally, REDCap includes features that ensure data integrity and participant confidentiality, such as audit trails, real-time data validation, encryption, and customizable user permissions (24).
Next, REDCap was used to send invitations to students’ university e-mails on March 3, 2019. Three weekly reminders were sent to nonresponders who received the invitations. The responses were collected during the four-week period from March 3, 2019 to April 4, 2019. The first page of the survey contained information about the study’s rationale and statements ensuring respondents’ confidentiality. The participants were given the choice to decline or consent to accept the participation and proceeded to answer the survey questions. The survey questions allowed for no response as an option for every question, and the participants could stop participation at any time.
It was estimated that a sample size of 385 would provide correct information regarding respondents’ willingness to donate organs within a 5% margin of error at a 95% confidence level. The sample size was calculated using the following formula: N = Z2pq/d2, assuming a population proportion of 0.5 and an unlimited population size1.
The participants’ demographic characteristics were summarized using descriptive statistics. Continuous variables were summarized as means with standard deviations, whereas categorical variables were summarized as counts and percentages. The association between responses and variables related to participants’ demographics, knowledge, attitude, and willingness to donate organs after brain death and perceived barriers and facilitators for deceased organ donation was examined. A chi-squared test for comparing proportions was used to test the null hypothesis (i.e., there was no difference in the characteristics of participants who were willing to be, not willing to be, and unsure about being organ donors). Univariate and multivariable logistic regression models were constructed to determine the association of participants’ characteristics that could affect the decision to donate an organ. The statistical difference of the categorical variables was assessed using chi-square tests. Logistic regression analysis was then used to explore main factors affecting willingness to donate organs. Demographic variables that had a p-value <0.05 following the chi-squared test, and those that had a known association with organ donation hesitancy were included in a multivariate regression model. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. A complete case analysis approach was applied in the regression analysis, where only participants with complete data for the variables included in each model were analyzed. Since all covariates are fully observed, there is no loss of information regarding the predictors. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS V.26.0, IBM, Chicago, Illinois, USA).
Results
Characteristics of the study respondents
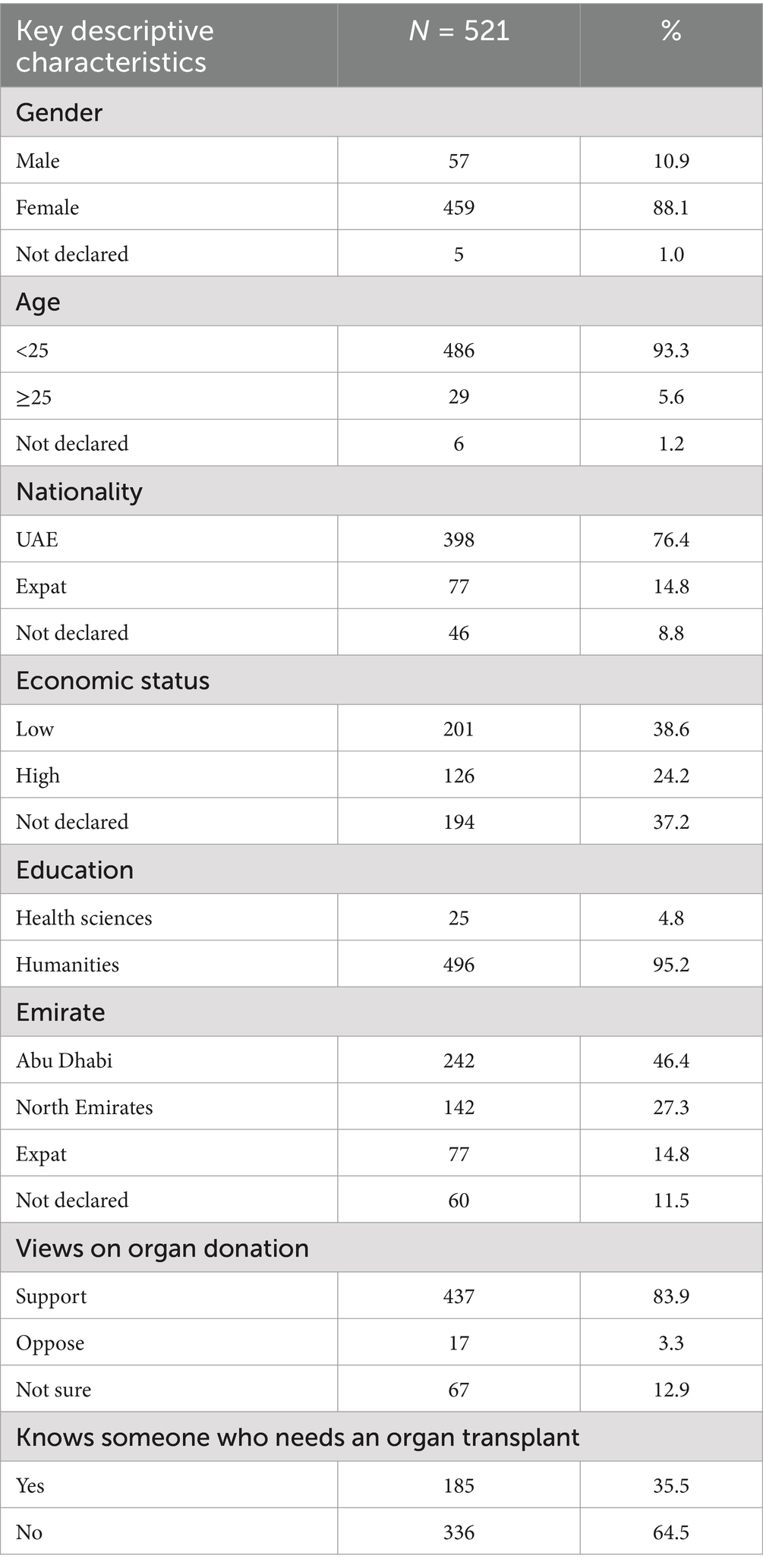
Of the 800 students who received the survey, 521 agreed to participate and completed the survey (response rate: 65.1%). The demographic characteristics of the study participants and their geographical distribution by emirate are shown in Table 1. The cohort of 521 students was found to be representative of the population distribution in the seven emirates (Table 1, Figure 1).
Most respondents were Emirati nationals (~76%) and female (~88%), with a nonmedical background (humanities: 496 [95.2%]). Most of the respondents supported organ donation as a medical treatment (84%). Approximately one-third of the respondents knew someone who needed an organ transplant or already had an organ transplant (Table 1).
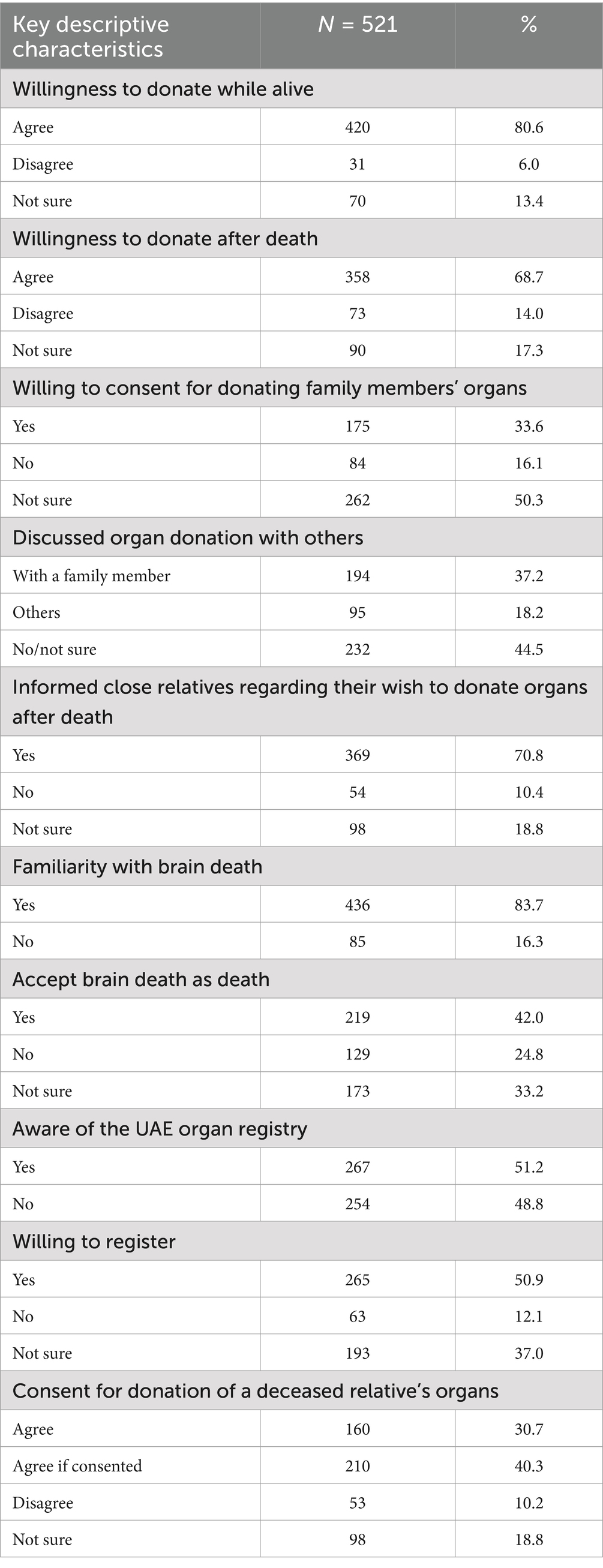
Approximately 33% of the respondents were not aware or unsure about the existence of an organ donation program in the UAE (Table 2). Others had learned about the UAE organ donation program primarily through media and awareness campaigns. A few respondents had learned about the program in schools.
Willingness and attitude toward organ donation
Most respondents (79%) were willing to donate their organs to a loved one during their lifetime (Table 2). In addition, most (69%) of the respondents were willing to donate their organs after death. However, 50% of respondents hesitated to consent for donating a family member’s organ after their death. Approximately 55% of the respondents had discussed the topic of organ donation, most of the time, they discussed this issue with a family member (Table 2). They discussed being a donor and their opinions on organ donation (Table 2). When the topic was not discussed, it was usually because it never came up during conversations (Table 2).
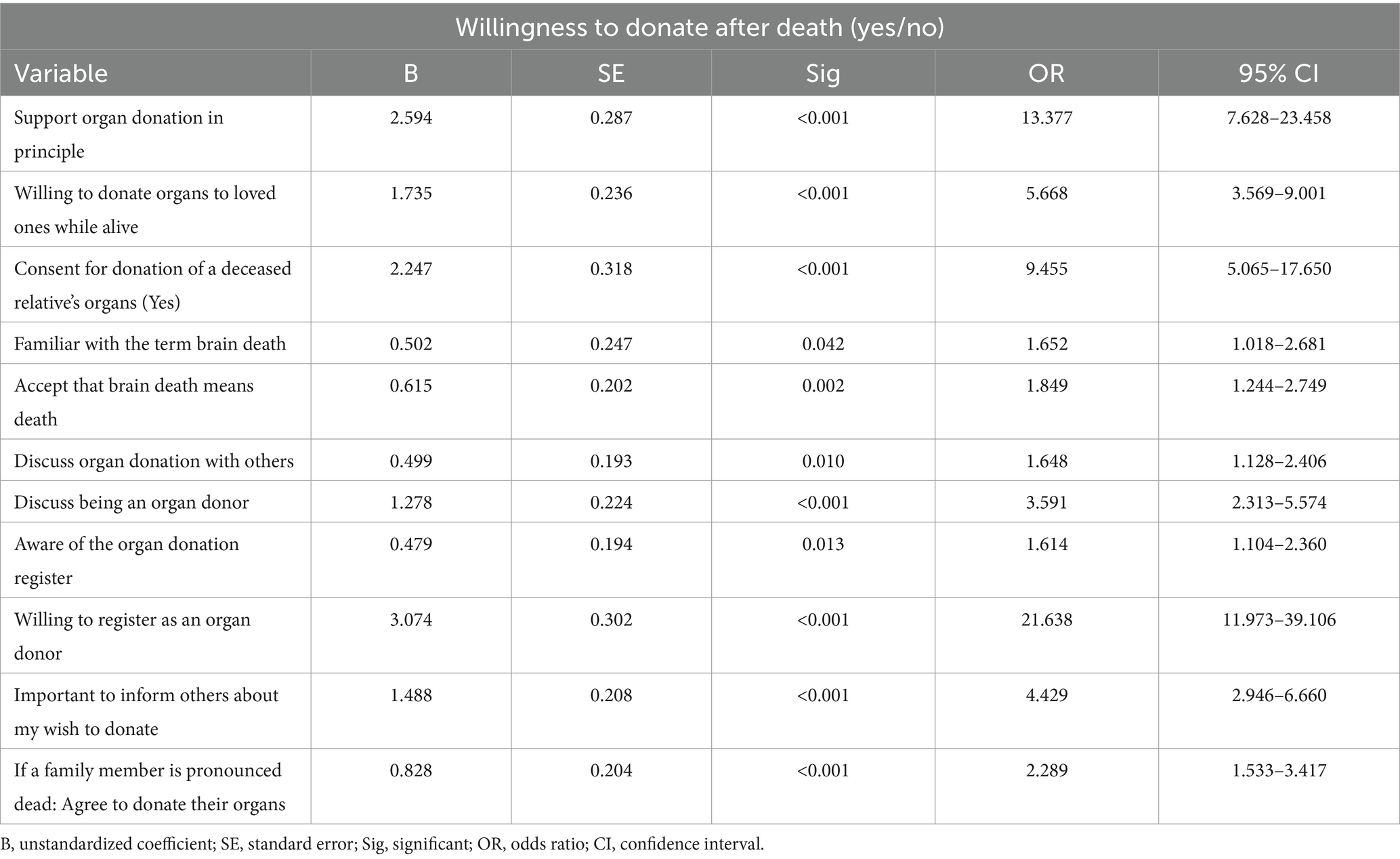
The characteristics of respondents who were willing to donate their organs after death are shown in Table 3. The willingness for organ donation was significantly higher among those who were willing to donate their organs while alive, those who registered as organ donors, those who consented for the donation of a deceased relative’s organs, and those who had expressed their wishes to donate after death.
Perception and attitude toward brain death
Most of the respondents were familiar with the term brain death (83.7%). However, only 42.8% of respondents accepted brain death as equivalent to death (Table 2), with the main reason for rejecting brain death as death being that the individual still had a heartbeat.
Willingness to register for organ donation
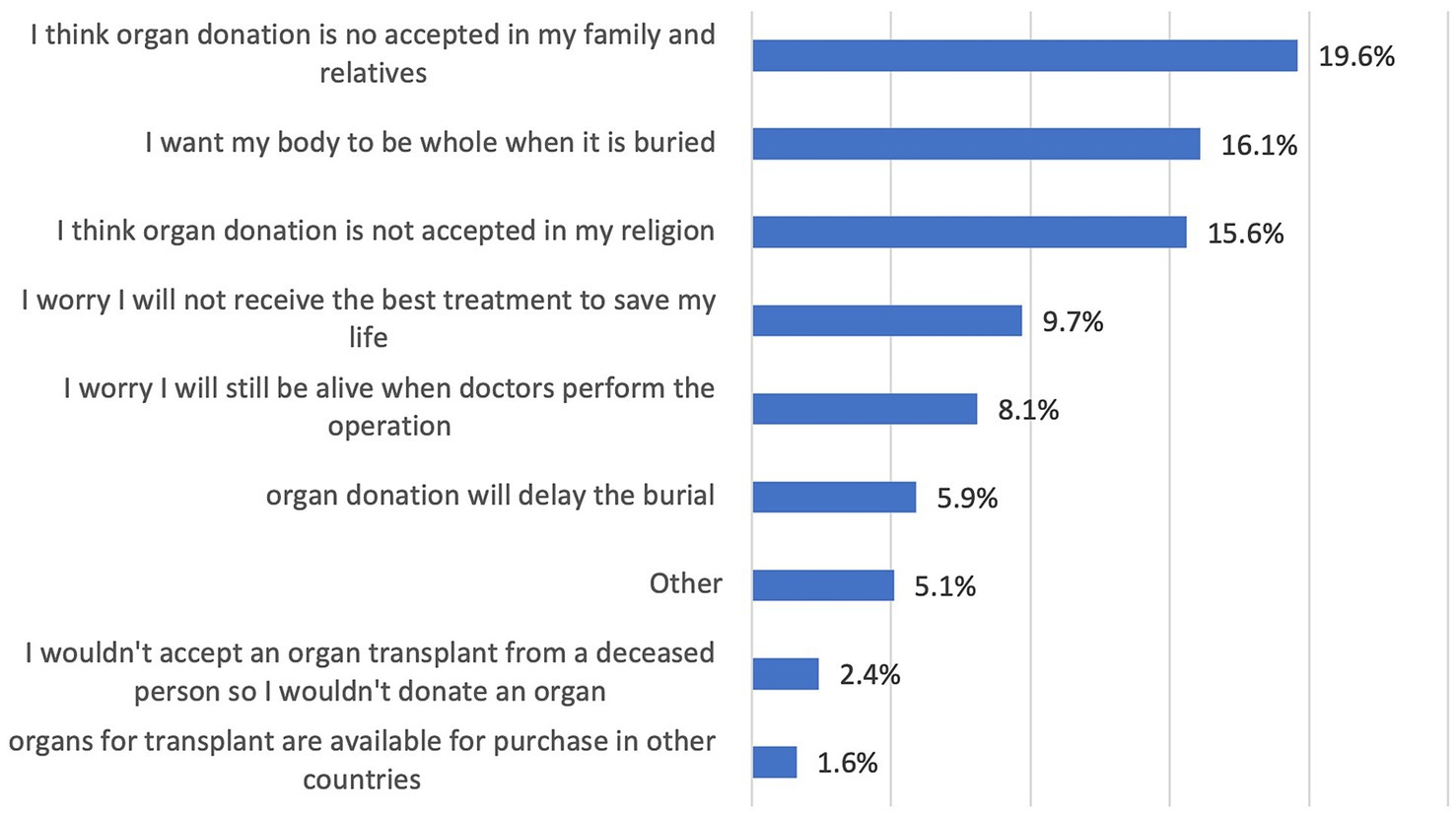
Approximately 51% of respondents were aware of the existence of the UAE register for organ donation and were willing to register for organ donation after death (Table 2). However, 19.6% mentioned that they would consider their family members’ opinions before registering as organ donors (Figure 2).
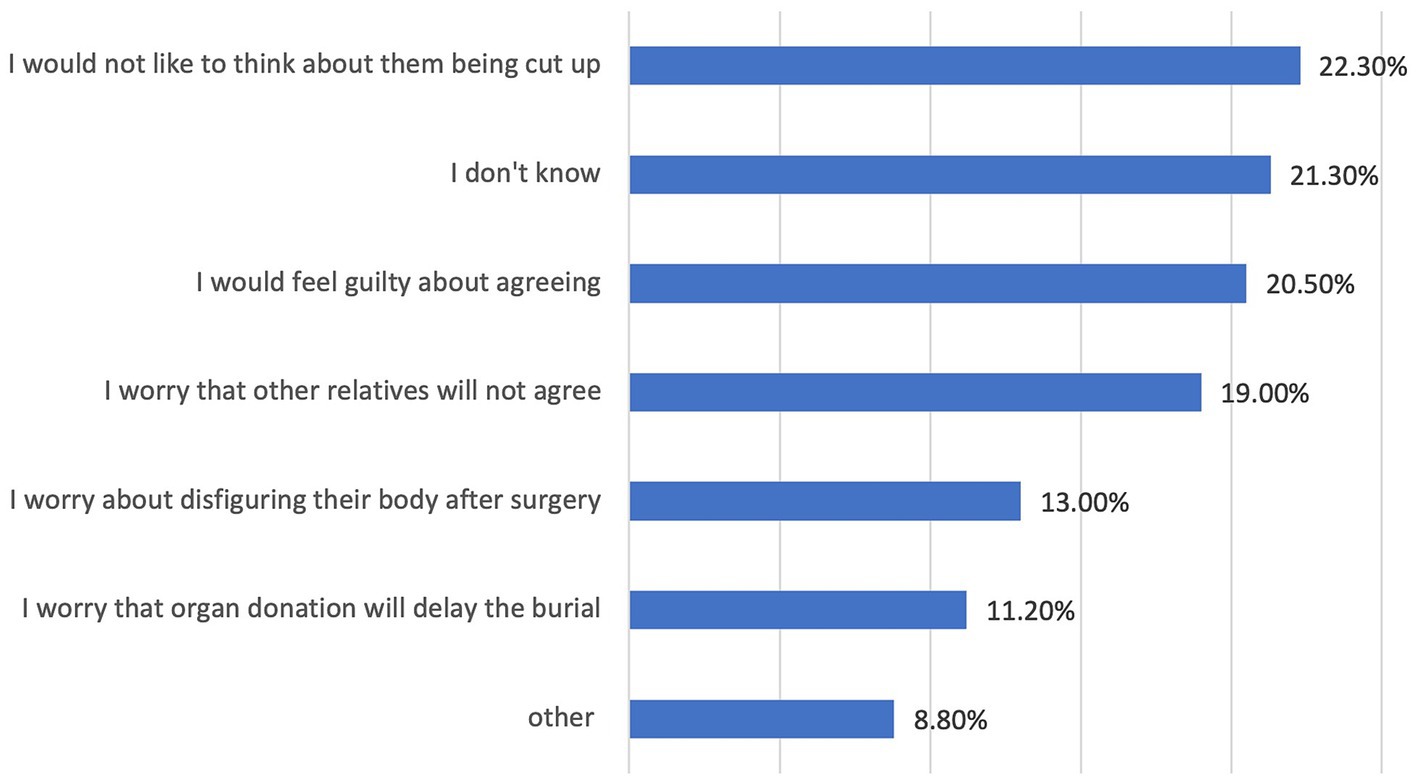
Approximately 71% of respondents agreed that it is important to inform people close to them about their wish to donate organs after death, and many would agree for a family member to donate their organs only if they had expressed their wishes or consent in writing to a register (Table 2). Because of personal beliefs or sociocultural reasons, 29% of respondents either disagreed or were hesitant to agree to donate the organs of a family member (Figure 3).
Perceived facilitators and barriers toward organ donation
Almost all respondents perceived organ donation as a good act that should be promoted (82.7%) and could save someone’s life (93.3%). Nevertheless, many respondents were unlikely to register as an organ donor even if their families had no objection (26.3%). Many respondents did not believe that organ donation would be rewarded by God (38.6%), and few respondents believed that organ donation is permitted in Islam (23.4%) and would be accepted in the UAE society (20.2%).
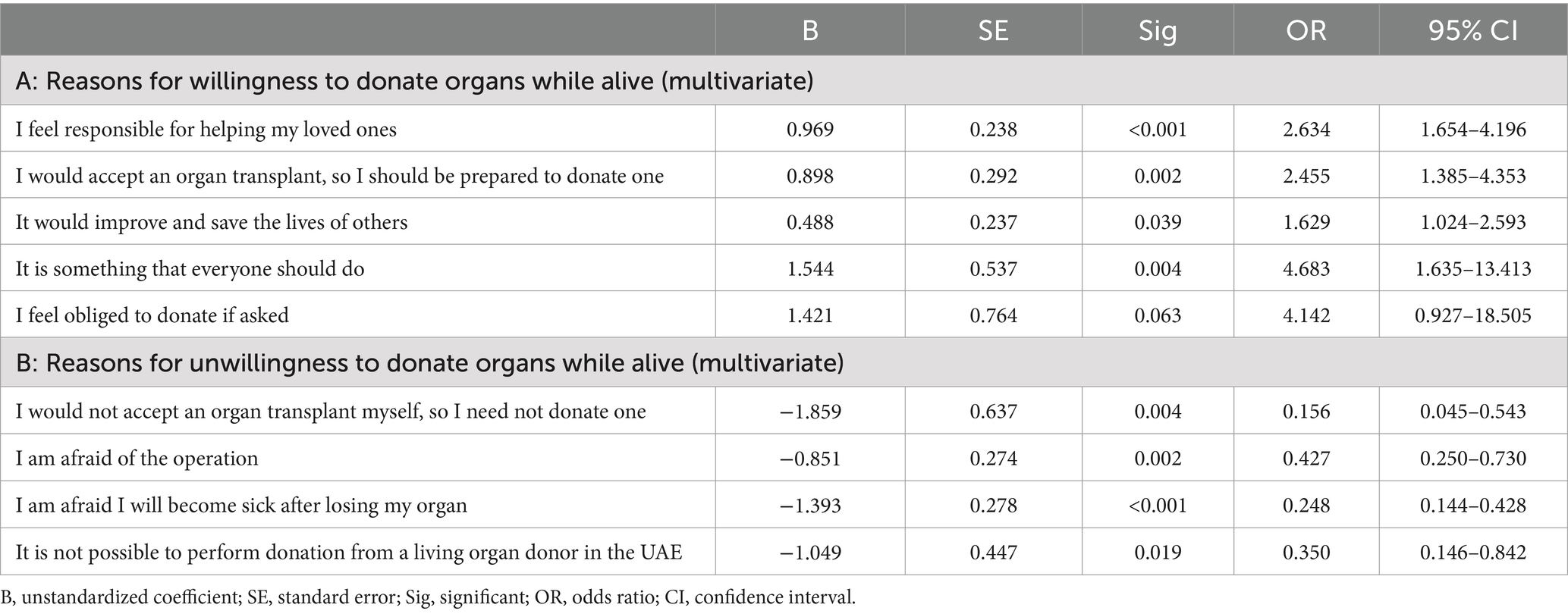
Predictors toward organ donation while alive
The most reported reasons of respondents for their willingness to donate organs while alive were altruism and feeling obligated to help family members (Table 4). The most commonly selected responses were that the respondents believed that organ donation is something that everyone should do (adjusted OR [aOR]: 4.68; 95% CI: 1.635–13.413); that it is a responsibility to help a loved one (aOR: 2.63; 95% CI: 1.654–4.196); that it should be done as respondents would like to accept an organ transplant themselves (aOR: 2.45; 95% CI: 1.385, 4.353); and that it will save others’ lives (aOR: 1.63; 95% CI: 1.024, 2.593).
Respondents who were hesitant to donate organs frequently cited fear of the operation or of losing an organ. The reported reasons for being unwilling to donate organs included the participants attitude against accepting deceased organ transplantation (aOR: 0.156; 95% CI: 0.045–0.543), fear of sickness (OR: 0.248; 95% CI: 0.144–0.428), unavailability of donating organs while living in the UAE (aOR: 0.35; 95% CI: 0.146–0.842), and fear of the operation (OR: 0.43; 95% CI: 0.250–0.730).
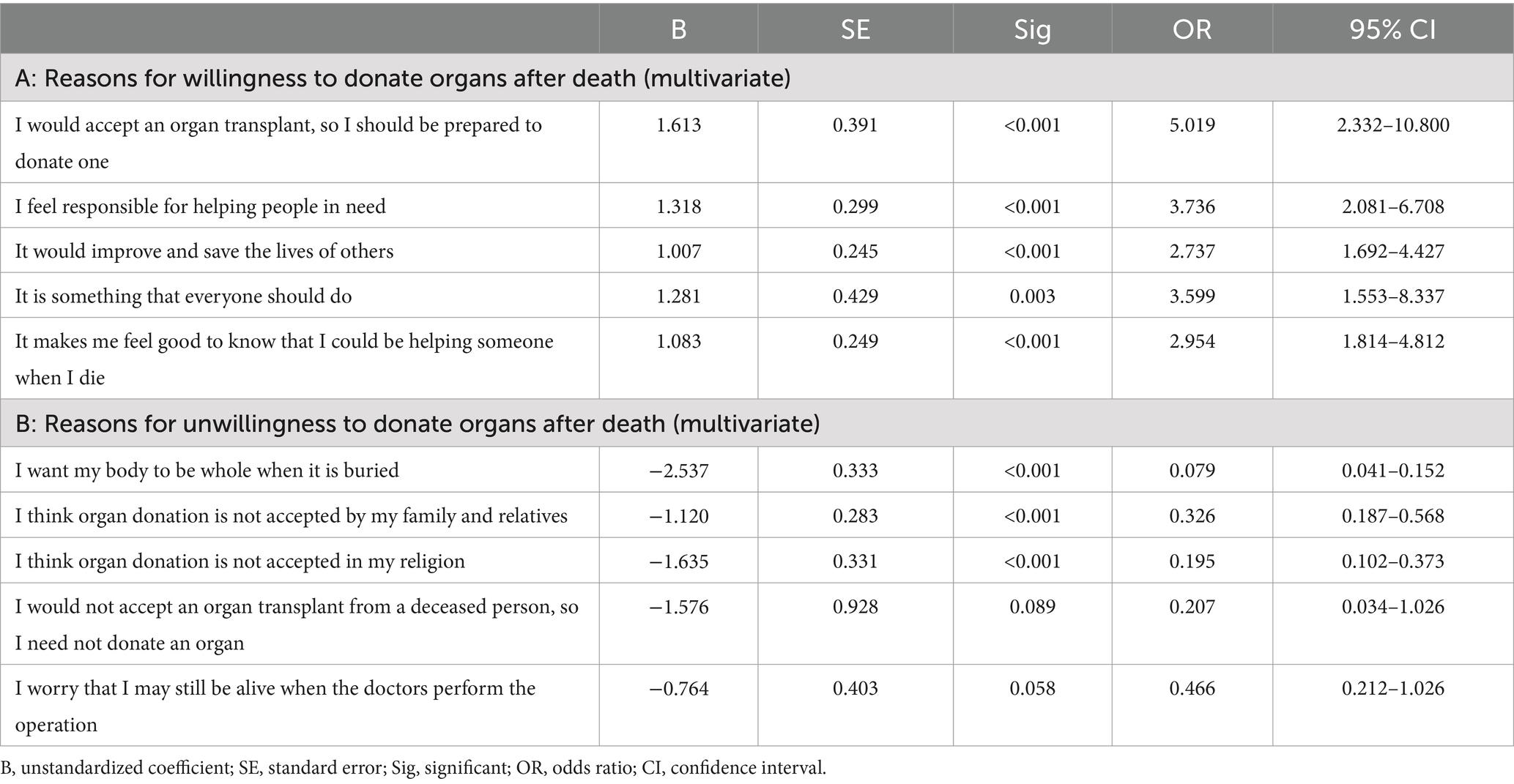
Predictors toward organ donation after death
The characteristics of respondents who were willing to donate organs after death are shown in Table 3. The reported reasons for the willingness to donate organs after death included altruism and the obligation to help family members. The respondents who were hesitant to donate their organs after death were primarily hesitant because of sociocultural and religious beliefs (Table 5). The odds to donate organs after death decreased by 92.1% (aOR: 0.079; 95% CI: 0.041–0.152), 80.5% (aOR: 0.195; 95% CI: 0.102–0.373), and 67.4% (aOR: 0.326; 95% CI: 0.187–0.568) for participants who wanted their whole body to be buried after death, those who had religious objections, and those who had family objections, respectively.
Discussion
This study aimed to explore the perceived facilitators and barriers toward organ donation in the UAE. Although most participants had a positive attitude toward organ donation and were willing to donate their organs to a loved one while alive, they were less likely to donate after death. Commonly cited reasons for declining consent for organ donation included fear of family refusal, moral objections to taking human organs after death, concerns about body disfigurement, and religious beliefs. The study’s findings align with previous research conducted elsewhere, which highlights that religious beliefs and cultural reasons are significant barriers to the acceptance of deceased organ donation in the Middle East (6, 13, 25).
The present study included university students, who typically have higher levels of education and are more likely to be open to sociocultural changes (14). Our findings concur with a similar study involving university students in Turkey. In that study, willingness to donate organs among university students was associated with receiving education on the topic, previous discussions with family and friends, awareness of existing organ donation program, willingness to receive an organ if needed and being registered as organ donors (26). While many participants demonstrated knowledge of brain death, a significant portion did not equate brain death with actual death. Instead, most participants accepted death only when the heart and breathing ceased or when all body organs stopped functioning. The prevailing belief that death cannot be declared if the heart is still beating underscores the need for targeted educational efforts about what brain death truly means as an irreversible cessation of all brain activity and is legally recognized as death. The confusion induced by the link of brain death concept with organ donation is highlighted by our study findings of a paradoxical correlation between participants acceptance of brain death as equivalent to death and their willingness to donate after death (27). Therefore, dissociating brain death from organ donation discussions might be prudent for the success of organ donation program in this setting. Multifaceted outreach initiatives that clarify religious, clinical, and legal perspectives on death based on neurological criteria, could improve public understanding of brain death. Collaborating with religious leaders and cultural influencers to provide accurate information about organ donation may provide culturally sensitive support to medical teams approaching families for organ donation authorization (27).
Although many respondents were willing to donate their organs after death (69%), 50% of participants in our study expressed hesitation in consenting to donate a deceased relative’s organs. Family participation in decisions to donate organs after death is a norm in society, and their consent is often shaped by sociocultural and religious beliefs (8, 12, 14). This hesitation can create ethical dilemmas related to respecting the autonomy of the deceased, managing the emotional burden on families, and ensuring cultural sensitivity (27, 28). Additionally, it can lead to delays in decision-making, potentially affecting the success of organ transplantation efforts. Addressing this issue requires public awareness initiatives that encourage open discussions about organ donation within families and promote the documentation of individual donation preferences (29, 30).
Religious and sociocultural beliefs are commonly cited barriers for consenting for organ donation after death (31). Individuals who are willing to register as donors would seek the consent of family members and perhaps religious figures before registering as organ donors (32, 33). The Islamic perspective on organ donation and transplantation has been extensively reviewed; overall, the religion has a positive attitude toward this subject (34). However, this view might not be widely prevalent. For example, a survey of clerics in Turkey showed poor knowledge of and attitudes toward organ donation (35). Thus, it is important to address cultural issues during organ retrieval and provide information about the process of organ retrieval in a way that aligns with cultural needs (e.g., declaring death, not delaying the burial, and preserving the body after retrieval). These findings also emphasize the importance of educating the public regarding the process of organ retrieval and how healthcare professionals consider cultural needs (12). A recent systematic review with narrative synthesis exploring barriers and facilitators of deceased organ donation among Muslims living in various communities globally identified the following five themes as important: knowledge, willingness to donate, community influence, bodily influence and religious beliefs (36). Furthermore, it is important for the public to be informed that a person has died when an official declaration of brain death is made (33).
Participants who believed that organ donation may be rewarded by God were more likely to register as a donor, highlighting the impact of religious belief on attitude toward organ donation (11, 12). In addition, a mechanism is needed to establish an early interaction with family members of potential donors facilitate the family consenting process and facilitating successful organ donation process (37). Furthermore, 10% of respondents reported fear of not receiving appropriate treatment as a barrier for registering as an organ donor (Figure 2). Donor rights are among the priorities for policymakers in the UAE as in the updated and more detailed Federal Decree by Law No. (25) of 2023 Concerning Donation and Transplantation of Human Organs and Tissues (38).
The strengths of our study are as follows: First, the study fills a gap in the literature regarding public knowledge regarding organ donation in the UAE and the barriers and facilitators to organ donation in the country. Second, the study adheres to recognized standards for formulating self-administered questionnaires, improving the robustness of the findings (39). Third, the study’s sample represents a fair distribution of respondents over the UAE’s seven emirates, improving the generalizability of the findings. Notably, however, this study also has some limitations, including a small sample size; a closed sampling frame (students at UAE University), which may not be representative of society; and low representation of males (10.9%). Low response rate is a common concern for surveys which can affect the strength of findings and increase bias. In our study, the response rate of 65%, despite being low, is above the suggested rate of 45% for online survey (40). Several factors may explain the poor response rates of males compared to females including organ transplantation topic itself (41). For example, a survey on this topic done in Turkey, a country that shares similar social and cultural beliefs as ours, 84% of respondents were females (42). This suggests that topic might not be of interest to males. Additionally, research has indicated that females generally respond more frequently to online surveys compared to their male counterparts, possibly due to differences in engagement with academic research and survey participation (43, 44). Therefore, a mixed-method approach for data collection that allows free-text answers, qualitative in-depth interviews including family members, or focus group discussions, can provide valuable additional information.
The concept of brain death is still foreign among Arab and eastern societies. The low rate of acceptance of the diagnosis of brain death is related to the existing gap between medical knowledge, legality of brain death, religious views, and the public acceptance of diagnosis of the brain death. This complicated by the central influence of family in any heath care related decision-making process. The notion that an individual is dead, according to medical definition, while the heart is still beating causes a lot of turbulence between the patient’s family and the caring physician. To resolve this issue, the medical community can improve understanding through consistent, simplified language, dissociating brain death from organ donation, and recognizing the emotions tied to discussions of brain death. The educational effort should focus on to increase public overall awareness of brain death as a medical condition. Furthermore, there is a need to form clear practical guidelines related to the diagnosis of brain death and subsequently guidelines related to the withdrawal of artificial support in these patients.
In conclusion, the study findings shed light on the limited acceptance of brain death and the need to obtain family consent for deceased organ donation. The public’s sociocultural view of death needs to evolve for deceased organ donation rates to improve. A structured approach, including early, empathetic communication with families of potential deceased donors, is essential. This should provide clear information about brain death, address cultural and religious concerns, and offer necessary religious and culturally support to the family. Additionally, preemptive education and involvement of trusted community leaders can help to improve understanding of brain death concept as terminal death. Future research on the best policy strategies and best practices for obtaining consent for deceased organ donation is needed.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Social Sciences Research Ethics Committee of UAE University (ERS_2018_5842). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. GA-B: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. RV: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. OB: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This paper was supported by the Office of Assistant Dean for Research of College of Medicine & Health Sciences at the United Arab Emirates University for publication fees.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1551380/full#supplementary-material
Footnotes
References
1. Algahim, MF, and Love, RB. Donation after circulatory death: the current state and technical approaches to organ procurement. Curr Opin Organ Transplant. (2015) 20:127–32. doi: 10.1097/MOT.0000000000000179
2. WHO-ONT. Those 2022 data are based on the global observatory on donation and transplantation (GODT) data. Geneva: WHO (2022).
3. Amouzegar, A, Abu-Alfa, AK, Alrukhaimi, MN, Bello, AK, Ghnaimat, MA, Johnson, DW, et al. International Society of Nephrology Global Kidney Health Atlas: structures, organization, and services for the management of kidney failure in the Middle East. Kidney Int Suppl. (2011) 11:e47–56. doi: 10.1016/j.kisu.2021.01.002
4. Vachharajani, T, Jasuja, S, AlSahow, A, GA, SM, Al-Aradi, AH, Salmi, A I, et al. Current status and future of end-stage kidney disease in gulf cooperation council countries: challenges and opportunities. Saudi J Kidney Dis Transpl. (2021) 32:1073–88. doi: 10.4103/1319-2442.338281
5. Prevention MoHa. (2022). Translation of the Minesterial decision no. (19) of 2022, concerning the criteria for the diagnosis od death. Available online at: https://mohap.gov.ae/assets/6d39e921/Translation%20of%20th%20Ministerial%20Decision%20No%2019%20of%202022%20Concerning%20the%20Criteria%20for%20the%20Diagnosis%20of%20Death.pdf.aspx2022 (Accessed March 31, 2025).
6. Mekkodathil, A, El-Menyar, A, Sathian, B, Singh, R, and Al-Thani, H. Knowledge and willingness for organ donation in the middle eastern region: a Meta-analysis. J Relig Health. (2020) 59:1810–23. doi: 10.1007/s10943-019-00883-x
7. Janahi, FK, Al Rais, A, Al Rukhaimi, M, Khamis, AH, and Hickey, D. Public awareness of knowledge, belief, and attitude regarding organ donation and organ transplantation: a National Survey from the United Arab Emirates. Transplant Proc. (2018) 50:2932–8. doi: 10.1016/j.transproceed.2018.08.006
8. Shahidi, J. Not telling the truth: circumstances leading to concealment of diagnosis and prognosis from cancer patients. Eur J Cancer Care. (2010) 19:589–93. doi: 10.1111/j.1365-2354.2009.01100.x
9. Shaheen, FA, and Souqiyyeh, MZ. Factors influencing organ donation and transplantation in the Middle East. Transplant Proc. (2000) 32:645–6. doi: 10.1016/S0041-1345(00)00929-5
10. Shaheen, FA, and Souqiyyeh, MZ. Increasing organ donation rates from Muslim donors: lessons from a successful model. Transplant Proc. (2004) 36:1878–80. doi: 10.1016/j.transproceed.2004.08.090
11. Woodman, A, Waheed, KB, Rasheed, M, and Ahmad, S. Current state of ethical challenges reported in Saudi Arabia: a systematic review & bibliometric analysis from 2010 to 2021. BMC Med Ethics. (2022) 23:82. doi: 10.1186/s12910-022-00816-6
12. Woodman, A, Al-Jamea, LH, Zahrani, EMA, Elsafi, SH, Waheed, KB, Al-Yami, FS, et al. Knowledge, attitude, and behavior toward organ donation and transplantation among medical students in the Eastern Province of Saudi Arabia. Transplant Proc. (2022) 54:1690–6. doi: 10.1016/j.transproceed.2022.05.034
13. Hajjar, WM, Bin Abdulqader, SA, Aldayel, SS, Alfardan, AW, and Alzaidy, NI. Knowledge, attitudes, and beliefs toward organ donation among social media users. Transplant Proc. (2016) 48:2418–22. doi: 10.1016/j.transproceed.2016.02.097
14. AbuAlhommos, AK, AlSaeed, AA, AlMutayib, M, Althuwaini, RF, Alshehab, SS, and Alsuwailem, NS. Assessment of community knowledge of and attitude toward organ donation in Saudi Arabia. Transplant Proc. (2023) 55:7–12. doi: 10.1016/j.transproceed.2022.09.036
15. Abdulrazeq, F, Matsumoto, MM, Zourob, M, Al-Dobai, A, Zeyad, K, Marwan, N, et al. Barriers in knowledge and attitudes regarding organ donation among urban Jordanian population. Saudi J Kidney Dis Transpl. (2020) 31:624–38. doi: 10.4103/1319-2442.289449
16. Al-Qerem, W, Carter, N, and Ling, J. Attitudes to organ donation and transplantation: an insight from Jordan. Exp Clin Transplant. (2022) 20:602–8. doi: 10.6002/ect.2021.0419
17. Alobaidi, S. Beliefs and intention to organ donation in Saudi Arabia: an online cross-sectional survey. Healthcare. (2023) 11:716. doi: 10.3390/healthcare11121716
18. Seddiq, M, Uddin, RH, Mohammed, M, Khalaf, I, Mohammed, A, Akbar, M, et al. Knowledge, attitudes, and willingness regarding organ donation in a Muslim country: a report from the United Arab Emirates. Saudi J Kidney Dis Transpl. (2023) 34:482–94. doi: 10.4103/sjkdt.sjkdt_464_20
19. Althunayyan, AM, Alsadun, AH, Alrumayh, F, and Alsulaim, L. Assessment of knowledge and attitudes toward organ donation in the Qassim region, Saudi Arabia. Cureus. (2025) 17:e77768. doi: 10.7759/cureus.77768
20. The United Arab Emirates' Government Portal. (2022). Fact sheet. Available online at: https://u.ae/en/about-the-uae/fact-sheet.
21. El-Shoubaki, H, and Bener, A. Public knowledge and attitudes toward organ donation and transplantation: a cross-cultural study. Transplant Proc. (2005) 37:1993–7. doi: 10.1016/j.transproceed.2005.03.014
22. Mohamed, E, and Guella, A. Public awareness survey about organ donation and transplantation. Transplant Proc. (2013) 45:3469–71. doi: 10.1016/j.transproceed.2013.08.095
23. Hammad, S, Alnammourah, M, Almahmoud, F, Fawzi, M, and Breizat, AH. Questionnaire on brain death and organ procurement. Exp Clin Transplant. (2017) 15:121–3. doi: 10.6002/ect.mesot2016.O115
24. Harris, PA, Taylor, R, Thielke, R, Payne, J, Gonzalez, N, and Conde, JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
25. Iniesta-Sepulveda, M, Lopez-Navas, AI, Gutierrez, PR, Ramirez, P, and Rios, A. The willingness to donate organs in medical students from an international perspective: a Meta-analysis. Transpl Int. (2022) 35:10446. doi: 10.3389/ti.2022.10446
26. Sengul, S, and Sahin, MK. The willingness and attitudes of medical students regarding organ donation and transplantation: a cross-sectional study from Turkey. Rev Assoc Med Bras. (2022) 68:1631–7. doi: 10.1590/1806-9282.20220307
27. Berzelak, N, Avsec, D, and Kamin, T. Reluctance and willingness for organ donation after death among the Slovene general population. Zdr Varst. (2019) 58:155–63. doi: 10.2478/sjph-2019-0020
28. Li, AH, Al-Jaishi, AA, Weir, M, Lam, NN, Maclean, J, Dhanani, S, et al. Familial consent for deceased organ donation among immigrants and long-term residents in Ontario, Canada: a population-based retrospective cohort study. Can J Kidney Health Dis. (2017) 4:2054358117735564. doi: 10.1177/2054358117735564
29. Grossi, AA, Cabrini, L, Redaelli, P, Manfrin, E, et al. Cognitive and non-cognitive factors affecting decision-making about deceased organ donation in Italy: a systematic review. Minerva Anestesiol. (2024) 90:931–8. doi: 10.23736/S0375-9393.24.18098-4
30. Volz Wenger, A, and Szucs, TD. Predictors of family communication of one's organ donation intention in Switzerland. Int J Public Health. (2011) 56:217–23. doi: 10.1007/s00038-010-0139-2
31. Almohsen, SS, Alobaishy, SM, Alghammas, NI, Albulayhi, SK, Alrashid, SM, Aljamal, RY, et al. Attitudes and beliefs on organ donation among students in a university in Central Saudi Arabia. Saudi Med J. (2016) 37:591. doi: 10.15537/smj.2016.5.14701
32. Alam, AA. Public opinion on organ donation in Saudi Arabia. Saudi J Kidney Dis Transpl. (2007) 18:54–9.
33. Siminoff, LA, Gordon, N, Hewlett, J, and Arnold, RM. Factors influencing families' consent for donation of solid organs for transplantation. JAMA. (2001) 286:71–7. doi: 10.1001/jama.286.1.71
34. Ali, A, Ahmed, T, Ayub, A, Dano, S, Khalid, M, El-Dassouki, N, et al. Organ donation and transplant: the Islamic perspective. Clin Transpl. (2020) 34:e13832. doi: 10.1111/ctr.13832
35. Keten, HS, Keten, D, Ucer, H, Cerit, M, Isik, O, Miniksar, OH, et al. Knowledge, attitudes, and behaviors of mosque imams regarding organ donation. Ann Transplant. (2014) 19:598–603. doi: 10.12659/AOT.891370
36. Al-Abdulghani, A, Vincent, BP, Randhawa, G, Cook, E, and Fadhil, R. Barriers and facilitators of deceased organ donation among Muslims living globally: an integrative systematic review. Transplant Rev. (2024) 38:100874. doi: 10.1016/j.trre.2024.100874
37. El Hennawy, HM, Safar, O, Thamer, A, Asiri, A, Abdullah, HS, Alhadi, WA, et al. Knowledge, attitude, and barriers toward deceased organ donation among health care professionals and medical students in southern Saudi Arabia: a cross-sectional study. Exp Clin Transplant. (2023) 21:772–8. doi: 10.6002/ect.2023.0166
38. President of the United Arab Emirates. (2023). Federal Decree by Law No. (25) of 2023 Concerning Donation and Transplantation of Human Organs and Tissues, Available online at: https://uaelegislation.gov.ae/en/legislations/2135/download#:~:text=1%2D%20It%20is%20prohibited%20to%20remove%20and%20transplant%20any%20organ,up%20to%20the%20fourth%20degree.
39. Burns, KE, Duffett, M, Kho, ME, Meade, MO, Adhikari, NK, Sinuff, T, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. (2008) 179:245–52. doi: 10.1503/cmaj.080372
40. Goodfellow, LT. An overview of survey research. Respir Care. (2023) 68:1309–13. doi: 10.4187/respcare.11041
41. Story, DA, and Tait, AR. Survey research. Anesthesiology. (2019) 130:192–202. doi: 10.1097/ALN.0000000000002436
42. Soylu, D, Ozdemir, A, and Soylu, A. Does religious attitude affect organ donation and transplantation? Transpl Immunol. (2022) 71:101555. doi: 10.1016/j.trim.2022.101555
43. Greenlaw, C, and Brown-Welty, S. A comparison of web-based and paper-based survey methods: testing assumptions of survey mode and response cost. Eval Rev. (2009) 33:464–80. doi: 10.1177/0193841X09340214
Keywords: Organ donation (topic area), public awareness, organ transplant, predictors, attitudes
Citation: Alshamsi F, Al-Bluwi GSM, Valero R and Bakoush O (2025) Attitudes toward organ donation among university students in the United Arab Emirates: a cross-sectional survey. Front. Public Health. 13:1551380. doi: 10.3389/fpubh.2025.1551380
Edited by:
Denise Lo, Emory University, United StatesReviewed by:
Roberto Scendoni, University of Macerata, ItalyMustafa Kursat Sahin, Ondokuz Mayıs University, Türkiye
Copyright © 2025 Alshamsi, Al-Bluwi, Valero and Bakoush. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Omran Bakoush, b21yYW4uYmFrb3VzaEB1YWV1LmFjLmFl
†ORCID: Ricard Valero, https://orcid.org/0000-0001-7875-9496
 Fayez Alshamsi
Fayez Alshamsi Ghada S. M. Al-Bluwi
Ghada S. M. Al-Bluwi Ricard Valero
Ricard Valero Omran Bakoush
Omran Bakoush